- 1MAP Centre for Urban Health Solutions, Li Ka Shing Knowledge Institute, St. Michael's Hospital, Toronto, ON, Canada
- 2Harvard Medical School, Boston, MA, United States
- 3Applied Health Research Centre, Li Ka Shing Knowledge Institute, St. Michael's Hospital, Toronto, ON, Canada
- 4Dalla Lana School of Public Health, University of Toronto, Toronto, ON, Canada
- 5Centre for Addiction and Mental Health, Toronto, ON, Canada
- 6Department of Psychiatry, University of Toronto, Toronto, ON, Canada
- 7Department of Medicine, University of Toronto, Toronto, ON, Canada
Purpose: We examined the housing trajectories of homeless people with mental illness over a follow-up period of 6 years and the association of these trajectories with food security. We then examined the modifying role of psychopathology and alcohol and substance use disorders in this association.
Materials and Methods: We followed 487 homeless adults with mental illness at the Toronto site of the At Home/Chez-Soi project—a randomized trial of Housing First. Food security data were collected seven times during the follow-up period. Psychopathology (Colorado Symptom Index score) and alcohol and substance use disorders were assessed at baseline. Housing trajectories were identified using group-based trajectory modeling. Logistic regression was used to estimate the association between housing trajectory groups and food security.
Results: Three housing trajectory groups were identified: rapid move to consistent stable housing (34.7%), slow and inconsistent housing (52.1%), and never moved to stable housing (13.2%). Individuals included in the rapid move to consistent housing trajectory group had higher odds of remaining food secure compared with those in the never moved to stable housing trajectory group over the follow-up period [AOR 2.9, 95% CI: 1.3–6.6, P-value: 0.009]. However, when interactions were considered, this association was significant among those with moderate psychopathology but not severe psychopathology. Individuals with substance use disorder and in the never moved to stable housing group had the lowest food security status.
Discussion: Severe psychopathology and substance use disorders modified the association between housing trajectories and food security.
International Standard Randomized Control Trial Number Register (ISRCTN42520374).
Introduction
Homelessness (living without stable, safe, permanent, appropriate housing or the immediate prospect, means and ability of acquiring it (1) is detrimental for almost every life dimension of affected individuals. Being homeless is a crucial stress factor for well-being as it reflects severe material deprivation and, in addition, erodes mental, cognitive, and physical health (2–8); exposes individuals to risky conditions and behaviors [e.g., violence, bad meteorological conditions, discrimination; (9, 10)]; and precludes access to such basic services as sanitation, healthcare, water, or food (11–13).
Access to food is a consistent unmet need of homeless populations. Compared with the general population, homeless individuals have lower food security (14), lower nutrient intake, and diet insufficiency (15, 16). Homeless individuals typically cannot access kitchens to prepare meals and preserve perishable foods (17, 18), forcing them to depend on fast food, shelter or community meals, and even food waste to meet their needs or to remain hungry (19–21). The intertwinement of homelessness with mental illness and substance use worsens access to food because it generates competing needs for purchasing medications and substances (22–25).
Housing First (HF) interventions—generally including rent supplements and mental health support services—have been implemented internationally to facilitate exit from homelessness to stable housing while also providing social and health services to support housing stability and enhance health and well-being (26, 27). Studies in Canada and the United States demonstrate the effectiveness of HF interventions in promoting rapid exit from homelessness (28–30). However, two main concerns have been raised about these interventions. First, exiting homelessness remains a complex and non-linear process (31–33). Although some individuals who participate in HF interventions move rapidly and remain stably housed, others are either less successful in remaining stably housed or are never able to become stably housed (31, 32). These different housing trajectories affect and reflect other aspects of the lives of homeless adults. A study by Kerman et al. finds that housing trajectories shape patterns of social services use, independent of whether individuals are in the intervention or standard treatment arms (34). For example, participants who achieved sustained housing stability across both intervention and standard treatment groups have similar patterns of emergency department use, hospitalization, inpatient psychiatric admission, or food bank use. Within the intervention group, social and health services use was largely different among subgroups of individuals with different housing patterns.
Second, as for several mental health outcomes, HF interventions seem to have limited effect on quality of life of homeless individuals, including the satisfaction of some basic needs, such as food security, which is at the physiological level of Maslow's pyramid of needs and well-being (35–37). Previous analysis of HF in five Canadian cities over a 2-year period showed that access to stable housing was not sufficient to improve food security among individuals with mental illness (37). However, the heterogeneity of housing trajectories was not adequately accounted for in that study.
Here, we examine patterns of exiting homelessness to stable housing (housing trajectory groups) among homeless individuals with mental illness participating in the Toronto At Home/Chez Soi Study over a follow-up period of 6 years (38). This long follow-up period provided enough time to observe consistent changes over time, contrary to previous analyses that were limited to 2 years (31, 33, 39). Second, we ask whether these housing trajectory groups were associated with food security of study participants over the study period. Finally, we investigated whether the association between housing trajectory groups and food security differed across the severity of psychopathology and alcohol and substance use disorders. We hypothesized that a rapid move to stable housing was associated with consistent food security over the follow-up period and that this association was weaker among participants with severe psychopathology and alcohol and substance use disorders.
Materials and Methods
AH/CS Intervention
This study used data from the Toronto site of the At Home/Chez Soi (AH/CS) study, which was a randomized trial that compared the HF intervention (provision of mental health support services, such as assertive community treatment or intensive case management, plus rent supplement) to treatment as usual (TAU) (access to social, housing, and health services available in the community) (40). Participants were recruited from Toronto community agencies, shelters, clinics, and directly from the street between October 2009 and July 2011. The Toronto AH/CS participants were initially followed for 2 years (Phase I) between October 2009 and July 2013. In 2013, the study received additional funding to extend its follow-up period from January 2014 to March 2017 (Phase II) for a total follow-up period of approximately 6 years. Detailed information on study recruitment, design, population, and measurement instruments is reported elsewhere (41).
Four inclusion criteria were used to select AH/CS study participants: (1) being 18 years of age or older, (2) being absolutely homeless or precariously housed, (3) having a diagnosed severe mental disorder, and (4) not being served by assertive community treatment or an intensive case management program. Prior to randomization, participants were stratified by their level of needs for mental health services as high needs (HN) and moderate needs (MN). The level of need for mental health services was assessed using a combined algorithm that included having a psychotic disorder or bipolar affective disorder with psychotic symptoms [based on the Mini International Neuropsychiatric Interview 6.0 (MINI)], low community functioning [based on the Multnomah Community Ability Scale (MCAS)], presence of a comorbid substance use disorder, and prior history of hospitalizations and incarcerations (40–43). Out of the 575 Toronto participants, 197 participants met criteria to be classified as HN and 378 as MN. Then, according to their level of need, participants were randomly assigned to either the HF treatment or TAU. Participants assigned to the treatment group with HN received HF support services with assertive community treatment (ACT), and those with MN received HF support services with intensive case management (ICM) treatment. Participants assigned to the TAU group continued to have access to housing and social and health support services locally available in their communities.
Ethical considerations
The Toronto AH/CS study received approval from the St. Michael's Hospital Research Ethics Board (Canada), and all participants gave informed written consent to participate in the AH/CS study. The AH/CS study is also registered with the International Standard Randomized Control Trial Number Register (ISRCTN42520374).
Measures and Operational Definitions
Stable Housing
We captured stable housing through a residential timeline follow-back calendar (RTLFB) questionnaire (31, 44), which was administered every 3 months (Phase I) or 6 months (Phase II) to track the number of days living/sleeping in different types of housing accommodations. An accommodation was defined to be stable housing if the participant had tenancy rights or was expected to remain in the same accommodation for more than 6 months. For each follow-up year, participants were classified as being stably housed if they remained in stable housing for at least 75% of RTLFB-accounted days over a calendar year.
Consistent Food Security
The modified version of the U.S. Adult Food Security Survey Module (US FSSM) [U.S. Department of Agriculture, Economic Service Research (45) U.S. Adult Food Security Survey Module: Three-Stage Design, with Screeners, 2012] was used to assess the food security status of each participant over the 30 days prior to interview time points. Data were gathered every 6 months during phase I and every 12 months during phase II up to seven times across the 6-year follow-up period. This instrument has been validated in previous studies to assess food security for individuals experiencing homelessness (46–48). It contains 10 items related to food access, and the code responses were summed up to compute the food security score. This score ranges from 0 to 10 and classifies food security status into two main groups: food secure [those with high food security (score = 0) and marginal food security (score = 1–2)] and food insecure [those with low food security (score = 3–5), and very low food security (score = 6–10)] (37, 49, 50).
Participants were classified as being consistently food secure over the follow-up time if they were in the “food secure” group for more than 50% of the duration of their follow-up interviews. For example, a participant with four follow-up interviews had to be food secure at least three times (more than 50%) to be classified as consistently food secure. To ensure that participants had a minimum follow-up number of interviews for the analysis, we excluded those who had fewer than three food security interviews (n = 88).
Covariates
HF Intervention
Because the present study is embedded within an HF intervention, we considered the indicator of HF treatment (HF vs. TAU) as a covariate to adjust for the housing trajectory groups over the follow-up period.
Other covariates included sociodemographic variables (age at baseline (in years), self-reported gender (classified as male or not male), ethno-racial group membership [ethno-racial and not ethno-racial group), and marital status (single or not)], number of children under 18 years, and lifetime duration of homelessness prior to study enrolment (<3 and ≥3 years). No other gender categories were considered because there were fewer than 10 non-binary individuals in our sample. Participants were asked whether they used a food bank in the last 6 months prior to food security interviews, and we counted the number of times over the follow-up period.
Modifier Variables
Severe psychopathology
We used the Colorado Symptom Index score (CSI) at baseline to assess for the effect of psychopathology on food security (40, 51). CSI is a widely used self-report measure of psychiatric symptomatology and includes 14 items. Participants were asked how often they experienced specific psychiatric symptoms, such as “How often have you felt nervous, tense, worried, frustrated, or afraid?” or “How often have your voices, thoughts, or feelings interfered with your doing things?” Their responses were graded using a five-point Likert-items rated from “not at all” (1) to “at least every day” (5). Total scores ranged from 14 to 70, and higher scores indicated more severe psychiatric symptoms. Previous studies show that this index has high internal consistency (Cronbach's alpha = 0.92) (52, 53). CSI was dichotomized using a preestablished clinical threshold 30 or higher to indicate individuals with high (1) or low (0) psychopathology severity (52).
Alcohol and Substance disorders
Alcohol and non-alcohol substance use disorders were identified separately based on DSM-IV criteria using the MINI 6.0 and were evaluated at the time participants were screened for entering the study (40, 54).
Statistical Methods
We used group-based trajectory modeling to identify patterns of exiting homelessness to stable housing over the 6-year follow-up period (55). This modeling technique allows for the identification of clusters of individuals who followed a similar housing trajectory over time (56). Assuming a logistic distribution of housing stability, it uses intercept and time as change parameters to estimate latent trajectory groups. For the shape of trajectory groups, we tested different polynomial growth factors (linear, quadratic, and cubic time factors) and determined the optimal number of trajectory groups through the Bayesian information criterion (BIC). To determine the best-fit trajectory shapes, we used the average posterior probability measure and the weighted odds of correct classification (OCC) (55). Afterward, the model was adjusted for HF intervention group membership. All models were estimated using the module Traj in Stata 15 (55).
Next, we used logistic regression models to estimate odds ratios and 95% confidence intervals for the association between housing trajectory groups and consistent food security over the 6-year follow-up period. Then, we adjusted the model including the following covariates: age, self-reported gender, ethno-racial group membership, marital status, number of children under 18 years, lifetime duration of homelessness, food bank use, severe psychopathology, alcohol use disorder, and substance use disorder. To assess the modifying effect of severe psychopathology and alcohol and substance use disorders, we reestimated the model with interaction terms, and the interaction graphs are presented. All statistical analyses were performed with Stata version 15 (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC.).
Results
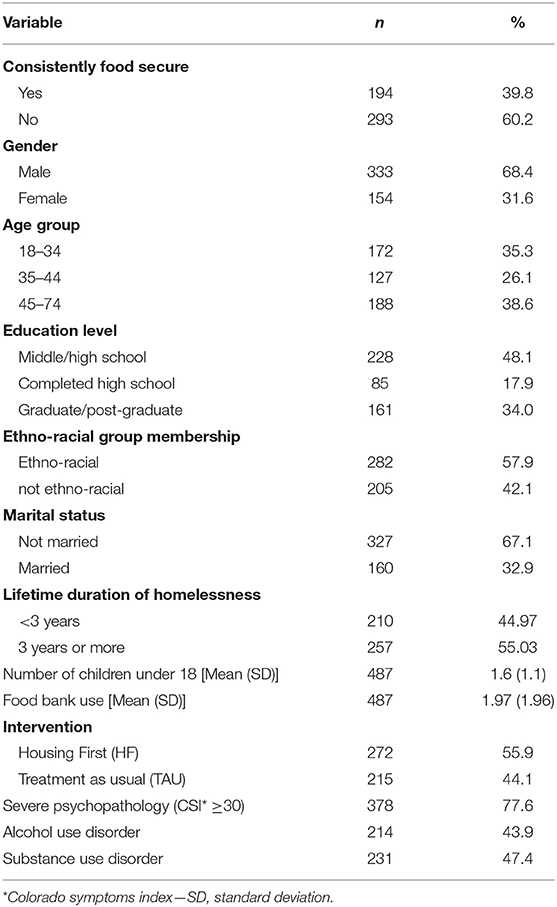
Sample characteristics are summarized in Table 1. Of 487 participants, 39.8% were consistently food secure (with high or marginal food security status) over the study period. Severe psychopathology was present in 77.6%, and 43.9 and 47.4% had alcohol and substance use disorders, respectively.
Housing Trajectories
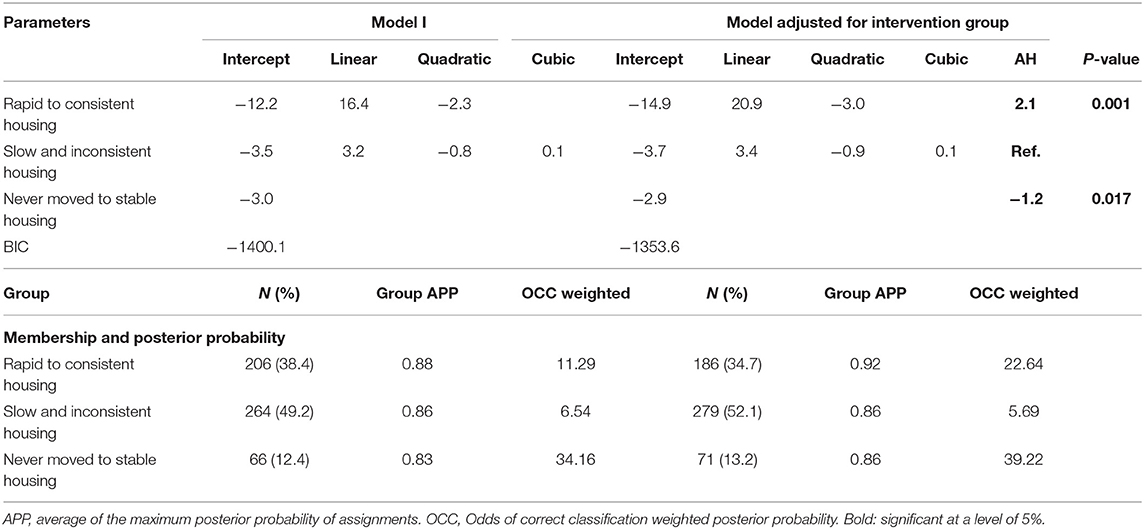
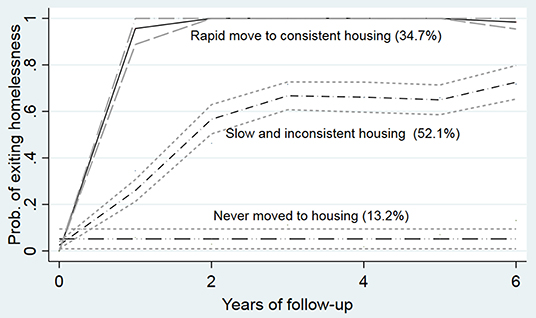
Three housing trajectory groups were identified: a rapid move to consistent stable housing trajectory with a quadratic form, a slow and inconsistent housing trajectory with a cubic form, and a never moved to stable housing trajectory (see Table 2 and Figure 1). Of the 487 participants, 34.7% of participants were classified in the rapid move to consistent stable housing group and 52.1% in the slow and inconsistent housing group; 13.2% never moved to stable housing during the study period. The BIC fit statistics confirmed this model as the best fit model (BIC for the two-group model = −1416.08; BIC3 = −1400.10, and BIC4 = −1455.53). The average posterior probability (>0.70) and the OCC-weighted posterior portability (>5) also indicate good fit. The adjusted model demonstrates that the HF intervention influences the trajectories, mainly by increasing the probability of having a rapid move to consistent housing and decreasing the probability of never moving or slow compared with the slow and inconsistent housing trajectory. Average posterior probabilities and two of the OCC-weighted posterior probabilities indicate improvement after the adjustment.
Housing Trajectory and Consistent Food Security
Compared with those in the never moved to stable housing trajectory, those in the rapid move to consistent housing stability group were more likely to be consistently food secure, AOR 2.9 [95% CI (1.3–6.6)] (see Table 3). Likewise, those with severe psychopathology and a substance use disorder were less likely to be consistently food secure (AOR 0.39 [95% CI (0.24–0.63)]) and 41% (AOR 0.59 [95% CI (0.37–0.95)]), respectively.
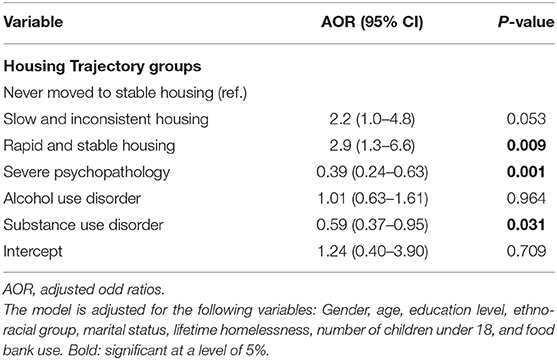
Table 3. Multivariable logistic regressions for consistent food security and housing trajectory groups adjusted for baseline characteristics.
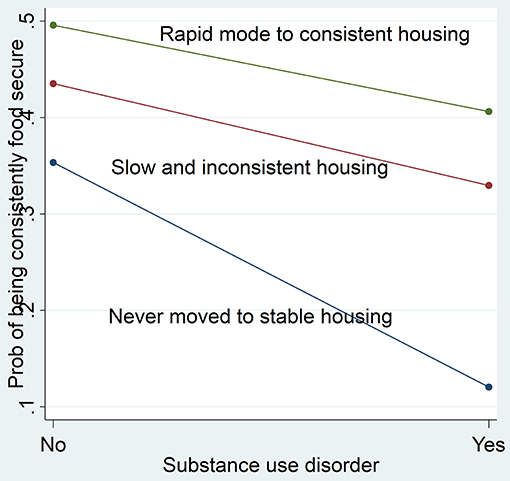
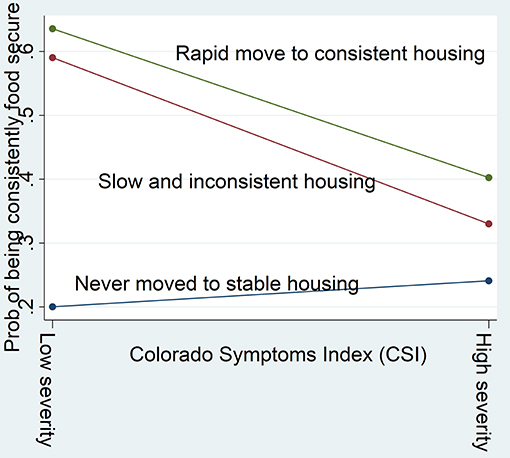
Modification Effects of Psychopathology and Substance Use Disorder
As shown in Figure 2, among participants with low psychopathology, those who moved to housing (rapid move to consistent housing and slow and inconsistent housing) were 40% more likely to be consistently food secure compared with those who never moved to stable housing. Conversely, among participants with severe psychopathology, no difference is observed between the housing trajectory groups. Likewise, those with no alcohol or substance use disorders and who never moved to stable housing were least likely to be consistently food secure (Figure 3). No modification effect was observed for alcohol use disorder.
Discussion
This study examined housing trajectories and their association with food security among homeless adults with mental illness in a large urban center. Three housing trajectory groups were identified: a rapid move to consistent housing group, a slow and inconsistent housing group, and a never moved to stable housing group. These results corroborate findings from previous studies on the complexity of exiting homelessness. Adair et al., using data from the multisite at Home/Chez Soi study of HF, found different housing trajectories over a 2-year period, including a group of almost no time housed (29%); a group of rapid and sustained housing (33%); and several small groups, such as slow and sustained housing, early housing, and gradually lost, rapid gain, and steep decline (31). Another study among homeless youth in Los Angeles County identified three trajectories over a 2-year period, a consistently sheltered group, a group with a high probability of finding and maintaining shelter over time, and a last group who remained inconsistently sheltered over a long term (33). Contrary to these studies conducted over a period up to 2 years, our study looked at pathways out of homeless to housing over a period of 6 years.
Our results indicate that providing housing is only one step toward supporting people experiencing homelessness by helping them leave streets and shelters and entering a residence. However, even after achieving housing, these individuals face several personal, economic, and social challenges and extreme poverty that can impede their achievement of long-term housing stability (32, 57–59). Moving into stable housing is accompanied by additional living costs (e.g., paying for utilities) that compete with other basic needs (e.g., food), rendering individuals vulnerable to eviction and repeated homelessness.
Our results also show that individuals in the rapid move to consistent housing group were more likely to be food secure compared with those in the never moved to stable housing group over the follow-up period. However, this association disappeared for those with severe psychopathology. Furthermore, those with substance use disorders and in the never moved to stable housing group were least likely to be food secure. Our results support findings from a recent study conducted by O'Campo et al. (37) on the role of housing stability as a key determinant of food security. Our findings offer new insight into the complexity of how pathways out of homelessness interact with mental health and substance use disorders to prevent individuals from achieving food security. The combination of a difficult housing trajectory with mental illness might prevent employment, forcing individuals to make trade-offs between food security, stable housing (e.g., rent), and other basic needs (59–61).
There are several study limitations to note. First, food security data may be affected by recall bias, which might influence the accuracy of reported findings. Second, there were not enough follow-up interviews to consistently assess food security over the entire study period. More food security interviews over the same follow-up period would have required reducing the time interval between interviews. Finally, this study focuses on homeless adults who have mental illness and is also limited to an only site, Toronto City, and cannot be generalized to all homeless adults.
Notwithstanding these limitations, this study provides a comprehensive view of the complexity of exiting homelessness to stable housing and its influence on food security. The analysis also offers insight into how psychopathology and substance use disorders contribute to poor food security even after homeless people achieve long-term housing stability. This study has two main policy implications. First, housing interventions must focus on achieving housing stability over a long period of time with special attention on factors that increase risk for unsuccessful housing trajectories. Second, it is important to enhance housing interventions with food security programs to better address the food needs of homeless adults with severe psychopathology and substance use disorders.
Data Availability Statement
Data cannot be made publicly available for both ethical and legal reasons. They were collected from randomized trial implemented within a hospital setting, St. Michael's Hospital in Toronto, which conferred the participants the status of patient. Data also contain information related to mental health status of the participants. Data collection, use, and disclosure are governed by the Personal Health Information Protection Act (PHIPA, 2004) and must not be disclosed without their written informed consent, as was stated in the written informed consent form by law. As the study addresses a specific and small subpopulation, any combination of three to four variables can facilitate the identification of some participants. Nonetheless, Home/Chez Soi Toronto Data will be available to investigators for studies that have received approval from research ethics boards. Study proposals and data access requests should be sent to Evie Gogosis at ZXZpZS5nb2dvc2lzQHVuaXR5aGVhbHRoLnRv.
Ethics Statement
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Research Ethics Board of St. Michael's Hospital (Canada). Written informed consent was obtained from all subjects/patients. The At Home/Chez-Soi study is registered with the International Standard Randomized Control Trial Number Register (ISRCTN42520374). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JL, CM-L, and PO'C conceived and designed the present research study. JL conducted the final statistical analysis, interpreted the data, and wrote the first manuscript draft. CM-L, RW, RN, and ML assisted in the study design, interpretation of the results, and revision of the first manuscript draft. PO'C, VS, and SH were also the principal investigators of the AH/CS study, Toronto site. All the co-authors revised and approved the present final manuscript version. All authors contributed to the interpretation of the results and critical revision and edition of the final manuscript.
Funding
This At Home/Chez Soi research demonstration project was made possible through a financial contribution from Health Canada provided to Mental Health Commission of Canada. This study was financially supported from research grants from Ontario Ministry of Health and Long Term Care (HSRF#259), and the Canadian Institute of Health Research (CIHR MOP-130405). Initials of authors who received Grants: HSRF #259: VS and SH CIHR operating grant: MOP-130405: VS, PO'C, and SH. JL acknowledges support from the Canadian Institute of Health Research-Institute of Population and Public fellowship award in Research & Knowledge Translation on Urban Housing and Health (201910RAT-435231-65841) in partnership with Canada Mortgage and Housing Corporation.
Disclaimer
The funding institutions had no role in the study design, collection, analysis, and interpretation of the data or the preparation, revision, or approval of the present manuscript. The views expressed in this publication are the views of the authors.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the At Home/Chez Soi participants whose willingness to share their lives, experiences, and stories with us made this project possible. We also thank the At Home/Chez-Soi project team, site coordinators, and service providers, who have contributed to the design, implementation, and follow-up of the project at the Toronto site. This manuscript has been released as a preprint at Research Square, Lachaud et al. (38).
References
1. Gaetz S, Barr C, Friesen A, Harris B, Hill C, Kovacs-Burns K, et al. Canadian Definition of Homelessness. Available online at: https://www.homelesshub.ca/sites/default/files/COHhomelessdefinition.pdf (accessed December 30, 2020).
2. Childress S, Reitzel LR, Maria DS, Kendzor DE, Moisiuc A, Businelle MS. Mental Illness and substance use problems in relation to homelessness onset. Am J Health Behav. (2015) 39:549–55. doi: 10.5993/AJHB.39.4.11
3. Davidson D, Chrosniak LD, Wanschura P, Flinn JM. Indications of reduced prefrontal cortical function in chronically homeless adults. Commun Mental Health J. (2014) 50:548–52. doi: 10.1007/s10597-013-9664-9
4. Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in Western countries: systematic review and meta-regression analysis. PLoS Med. (2008) 5:1670–81. doi: 10.1371/journal.pmed.0050225
5. Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. (2014) 384:1529–40. doi: 10.1016/S0140-6736(14)61132-6
6. Hwang SW. Is homelessness hazardous to your health? Can J Public Health. (2002) 93:407–10. doi: 10.1007/BF03405026
7. Pluck G, Lee KH, David R, Macleod DC, Spence SA, Parks RW. Neurobehavioural and cognitive function is linked to childhood trauma in homeless adults. Br J Clin Psychol. (2011) 50:33–45. doi: 10.1348/014466510X490253
8. Romaszko J, Cymes I, Dragańska E, Kuchta R, Glińska-Lewczuk K. Mortality among the homeless: causes and meteorological relationships. PLoS ONE. (2017) 12:e0189938. doi: 10.1371/journal.pone.0189938
9. Gaetz S. Safe streets for whom? Homeless youth, social exclusion, and criminal victimization. Can J Criminol Crim Just. (2004) 46:423–56. doi: 10.3138/cjccj.46.4.423
10. Skosireva A, O'Campo P, Zerger S, Chambers C, Gapka S, Stergiopoulos V. Perceived discrimination among homeless adults with mental illness in health care settings. BMC Health Serv Res. (2014) 14:376. doi: 10.1186/1472-6963-14-376
11. Baggett TP, O'Connell JJ, Singer DE, Rigotti NA. The unmet health care needs of homeless adults: a national study. Am J Public Health. (2010) 100:1326–33. doi: 10.2105/AJPH.2009.180109
12. Gozdzik A, Salehi R, O'Campo P, Stergiopoulos V, Hwang SW. Cardiovascular risk factors and 30-year cardiovascular risk in homeless. BMC Public Health. (2015) 15:165. doi: 10.1186/s12889-015-1472-4
13. Khandor E, Mason K, Chambers C, Rossiter K, Cowan L, Hwang SW. Access to primary health care among homeless adults in Toronto, Canada: results from the Street Health survey. Open Med. (2011) 5, e94–e103.
14. Baggett TP, Singer DE, Rao SR, O'Connell JJ, Bharel M, Rigotti NA. Food insufficiency and health services utilization in a national sample of homeless adults. J Gen Int Med. (2011) 26, 627–34. doi: 10.1007/s11606-011-1638-4
15. Tarasuk V, Dachner N, Poland B, Gaetz S. Food deprivation is integral to the ‘hand to mouth' existence of homeless youths in Toronto. Public Health Nutrition. (2009) 12:1437–42. doi: 10.1017/S1368980008004291
16. Tarasuk V, Dachner N, Li J. Homeless youth in Toronto are nutritionally vulnerable. J Nutrition. (2018) 135:1926–33. doi: 10.1093/jn/135.8.1926
17. Herault N, Ribar DC. Food insecurity and homelessness in the Journeys Home survey. J Hous Econ. (2017) 37:52–66. doi: 10.1016/j.jhe.2017.05.001
18. O'Flaherty B. Individual homelessness: entries, exits, and policy. J Hous Econ. (2012) 21:77–100. doi: 10.1016/j.jhe.2012.04.006
19. Geller L. Putting Housing First. Canadian Nurse (2014). Avcailable online at: https://www.canadian-nurse.com/articles/issues/2014/june-2014/putting-housing-first (accessed September 30, 2020).
20. Parpouchi M, Moniruzzaman A, Rezansoff SN, Russolillo A, Somers JM. Characteristics of adherence to methadone maintenance treatment over a 15-year period among homeless adults experiencing mental illness. Addict Behav Rep. (2017) 6:106–11. doi: 10.1016/j.abrep.2017.09.001
21. Rezansoff SN, Moniruzzaman A, Fazel S, Procyshyn R, Somers JM. Adherence to antipsychotic medication among homeless adults in Vancouver, Canada: a 15-year retrospective cohort study. Soc Psychiatry Psychiatr Epidemiol. (2016) 51:1623–32. doi: 10.1007/s00127-016-1259-7
22. Baer TE, Scherer EA, Fleegler EW, Hassan A. Food insecurity and the burden of health-related social problems in an urban youth population. J Adolesc Health. (2015) 57:601–7. doi: 10.1016/j.jadohealth.2015.08.013
23. Jessiman-Perreault G, McIntyre L. The household food insecurity gradient and potential reductions in adverse population mental health outcomes in Canadian adults. SSM Populat Health. (2017) 3:464–72. doi: 10.1016/J.SSMPH.2017.05.013
24. Martin MS, Maddocks E, Chen Y, Gilman SE, Colman I. Food insecurity and mental illness: disproportionate impacts in the context of perceived stress and social isolation. Public Health. (2016) 132:86–91. doi: 10.1016/j.puhe.2015.11.014
25. Tarasuk V, Mitchell A, Dachner N. Household Food Insecurity in Canada 2014. Toronto, ON: Research to identify policy options to reduce food insecurity (PROOF) (2016).
26. Goering PN, Streiner DL. Putting housing first: the evidence and impact. Can J Psychiatry. (2015) 60:465–6. doi: 10.1177/070674371506001101
27. Tsemberis S, Gulcur L, Nakae M. Housing first, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. Am J Public Health. (2004) 94:651–6. doi: 10.2105/AJPH.94.4.651
28. Aubry T, Goering P, Veldhuizen S, Adair CE, Bourque J, Distasio J, et al. A multiple-city RCT of housing first with assertive community treatment for homeless canadians with serious mental illness. Psychiatr Serv. (2016) 67:275–81. doi: 10.1176/appi.ps.201400587
29. O'Campo P, Stergiopoulos V, Nir P, Levy M, Misir V, Chum A, et al. How did a Housing First intervention improve health and social outcomes among homeless adults with mental illness in Toronto? Two-year outcomes from a randomised trial. BMJ Open. (2016) 6:e010581. doi: 10.1136/bmjopen-2015-010581
30. Stergiopoulos V, Hwang SW, Gozdzik A, Nisenbaum R, Latimer E, Rabouin D, et al. Effect of scattered-site housing using rent supplements and intensive case management on housing stability among homeless adults with mental illness: a randomized trial. J Am Med Assoc. (2015) 313:905–15. doi: 10.1001/jama.2015.1163
31. Adair CE, Streiner DL, Barnhart R, Kopp B, Veldhuizen S, Patterson M, et al. Outcome trajectories among homeless individuals with mental disorders in a multisite randomised controlled trial of housing first. Can J Psychiatry. (2017) 62:30–9. doi: 10.1177/0706743716645302
32. Patterson ML, Moniruzzaman A, Somers JM. History of foster care among homeless adults with mental illness in Vancouver, British Columbia: a precursor to trajectories of risk. BMC Psychiatry. (2015) 15:32. doi: 10.1186/s12888-015-0411-3
33. Tevendale HD, Comulada WS, Lightfoot MA. Finding shelter: two-year housing trajectories among homeless youth. J Adolesc Health. (2011) 49:615–20. doi: 10.1016/j.jadohealth.2011.04.021
34. Kerman N, Sylvestre J, Aubry T, Distasio J. The effects of housing stability on service use among homeless adults with mental illness in a randomized controlled trial of housing first. BMC Health Serv Res. (2018) 18:190. doi: 10.1186/s12913-018-3028-7
35. Lachaud J, Mejia-Lancheros C, Wang R, Wiens K, Nisenbaum R, Stergiopoulos V, et al. Mental and substance use disorders and food insecurity among homeless adults participating in the At Home/Chez Soi Study. PLoS ONE. (2020) 15:e0232001. doi: 10.1371/journal.pone.0232001
36. Lester D. Measuring Maslow's Hierarchy of Needs. Psychological Reports. (2013) 113:15–7. doi: 10.2466/02.20.PR0.113x16z1
37. O'Campo P, Hwang SW, Gozdzik A, Schuler A, Kaufman-Shriqui V, Poremski D, et al. Food security among individuals experiencing homelessness and mental illness in the at Home/Chez Soi Trial. Public Health Nutr. (2017) 20:2023–33. doi: 10.1017/S1368980017000489
38. Lachaud J, Mejia-Lancheros C, Liu M, Wang R, Nisenbaum R, Stergiopoulos V, et al. Severe psychopathology and substance use disorder modify the association between housing trajectories and food security among homeless adults. Res Square [Preprint]. (2020) 1–18. doi: 10.21203/rs.3.rs-26111/v1
39. Aubry T, Klodawsky F, Coulombe D. Comparing the housing trajectories of different classes within a diverse homeless population. Am J Commun Psychol. (2012) 49:142–55. doi: 10.1007/s10464-011-9444-z
40. Goering PN, Streiner DL, Adair C, Aubry T, Barker J, Distasio J, et al. The at Home/Chez Soi trial protocol: a pragmatic, multi-site, randomised controlled trial of a Housing First intervention for homeless individuals with mental illness in five Canadian cities. BMJ Open. (2011) 1:e000323. doi: 10.1136/bmjopen-2011-000323
41. Hwang SW, Stergiopoulos V, O'Campo P, Gozdzik A. Ending homelessness among people with mental illness: the at Home/Chez Soi randomized trial of a Housing First intervention in Toronto. BMC Public Health. (2012) 12:787. doi: 10.1186/1471-2458-12-787
42. Barker S, Barron N, McFarland BH, Bigelow DA, Carnahan T. A community ability scale for chronically mentally Ill consumers: part II. Applications. Commun Mental Health J. (1994) 30:459–72. doi: 10.1007/bf02189063
43. van Vliet IM, de Beurs. E. [The MINI-International Neuropsychiatric Interview. A brief structured diagnostic psychiatric interview for DSM-IV en ICD-10 psychiatric disorders]. Tijdschr Psychiatr. (2007) 49:393–7.
44. Tsemberis S, McHugo G, Williams V, Hanrahan P, Srefancic A. Measuring homelessness and residential stability: the residential time-line follow-back inventory. J Commun Psychol. (2007) 35:29–42. doi: 10.1002/jcop.20132
45. U.S. Department of Agriculture, Economic Service Research. US Adult Food Security Survey Module: Three-Stage Design, with Screeners (2012).
46. D'andreamatteo C and Slater J. Measuring food security in canadian homeless adult men. Can J Diet Pract Res. (2018) 79:42–5. doi: 10.3148/cjdpr-2017-026
47. Gundersen C, Engelhard EE, Crumbaugh AS, Seligman HK. Brief assessment of food insecurity accurately identifies high-risk US adults. Public Health Nutr. (2017) 20:1367–71. doi: 10.1017/S1368980017000180
48. Holland AC, Kennedy MC, Hwang SW. The assessment of food security in homeless individuals : a comparison of the Food Security Survey Module and the Household Food Insecurity Access Scale. Public Health Nutr. (2011) 14:2254–9. doi: 10.1017/S1368980011001327
49. Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Security, Revised 2000. Measuring food security in the United States: reports of the federal interagency food security measurement project. United States Department of Agriculture (2000). Available online at: https://www.fns.usda.gov/guide-measuring-household-food-security-revised-2000 (accessed April 15, 2021).
50. United States Department of Agriculture Economic Research Security. Definition of Food Security (2018). Available online at: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security.aspx (accessed December 30, 2020).
51. Conrad KJ, Yagelka JR, Matters MD, Rich AR, Williams V, Buchanan M. Reliability and validity of a modified Colorado Symptom Index in a national homeless sample. Mental Health Serv Res. (2001) 3:141–53. doi: 10.1023/A:1011571531303
52. Boothroyd RA, Chen HJ. The psychometric properties of the Colorado Symptom Index. Administr Policy Mental Health Mental Health Serv Res. (2008) 35:370–8. doi: 10.1007/s10488-008-0179-6
53. Shern DL, Wilson NZ, Coen AS, Patrick DC, Foster M, Bartsch DA, et al. Client outcomes II: longitudinal client data from the Colorado treatment outcome study. Milbank Q. (1994) 72:123. doi: 10.2307/3350341
54. Sheehan D, Lecrubier Y, Harnett-Sheehan K, Janavs J, Weiller E, Hergueta T, et al. the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. (1998) 59(Suppl. 20), 22–3. doi: 10.1016/S0924-9338(99)80239-9
55. Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Ann Rev Clin Psychol. (2010) 6:109–38. doi: 10.1146/annurev.clinpsy.121208.131413
56. Frankfurt S, Frazier P, Syed M, Jung KR. Using group-based trajectory and growth mixture modeling to identify classes of change trajectories. Counsel Psychol. (2016) 44:622–60. doi: 10.1177/0011000016658097
57. Nelson G, Patterson M, Kirst M, Macnaughton E, Isaak CA, Nolin D, et al. Life changes among homeless persons with mental illness: a longitudinal study of housing first and usual treatment. Psychiatr Serv. (2015) 66:592–7. doi: 10.1176/appi.ps.201400201
58. Patterson ML, Rezansoff S, Currie L, Somers JM. Trajectories of recovery among homeless adults with mental illness who participated in a randomised controlled trial of Housing First: a longitudinal, narrative analysis. BMJ Open. (2013) 3:e003442. doi: 10.1136/bmjopen-2013-003442
59. Stergiopoulos V, Gozdzik A, O'Campo P, Holtby AR, Jeyaratnam J, Tsemberis S. Housing First: exploring participants' early support needs. BMC Health Serv Res. (2014) 14:167. doi: 10.1186/1472-6963-14-167
60. Jones AD. Food insecurity and mental health status: a global analysis of 149 countries. Am J Prevent Med. (2017) 53:264–73. doi: 10.1016/j.amepre.2017.04.008
Keywords: psychopathology, substance use disorder, housing trajectories, food security, homeless adults
Citation: Lachaud J, Mejia-Lancheros C, Liu M, Wang R, Nisenbaum R, Stergiopoulos V, Hwang SW and O'Campo P (2021) Severe Psychopathology and Substance Use Disorder Modify the Association Between Housing Trajectories and Food Security Among Homeless Adults. Front. Nutr. 8:608811. doi: 10.3389/fnut.2021.608811
Received: 21 September 2020; Accepted: 15 March 2021;
Published: 12 May 2021.
Edited by:
Leila Itani, Beirut Arab University, LebanonReviewed by:
Jimmy Bourque, Royal College of Physicians and Surgeons of Canada, CanadaCarla Dandreamatteo, Red River College, Canada
Copyright © 2021 Lachaud, Mejia-Lancheros, Liu, Wang, Nisenbaum, Stergiopoulos, Hwang and O'Campo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: James Lachaud, amFtZXMubGFjaGF1ZEB1bml0eWhlYWx0aC50bw==
 James Lachaud
James Lachaud Cilia Mejia-Lancheros
Cilia Mejia-Lancheros Michael Liu
Michael Liu Ri Wang1
Ri Wang1 Vicky Stergiopoulos
Vicky Stergiopoulos