- 1Department of Biomedical Sciences and Pathobiology, Virginia Tech, Blacksburg, VA, United States
- 2Center for Engineered Health, Virginia Tech, Blacksburg, VA, United States
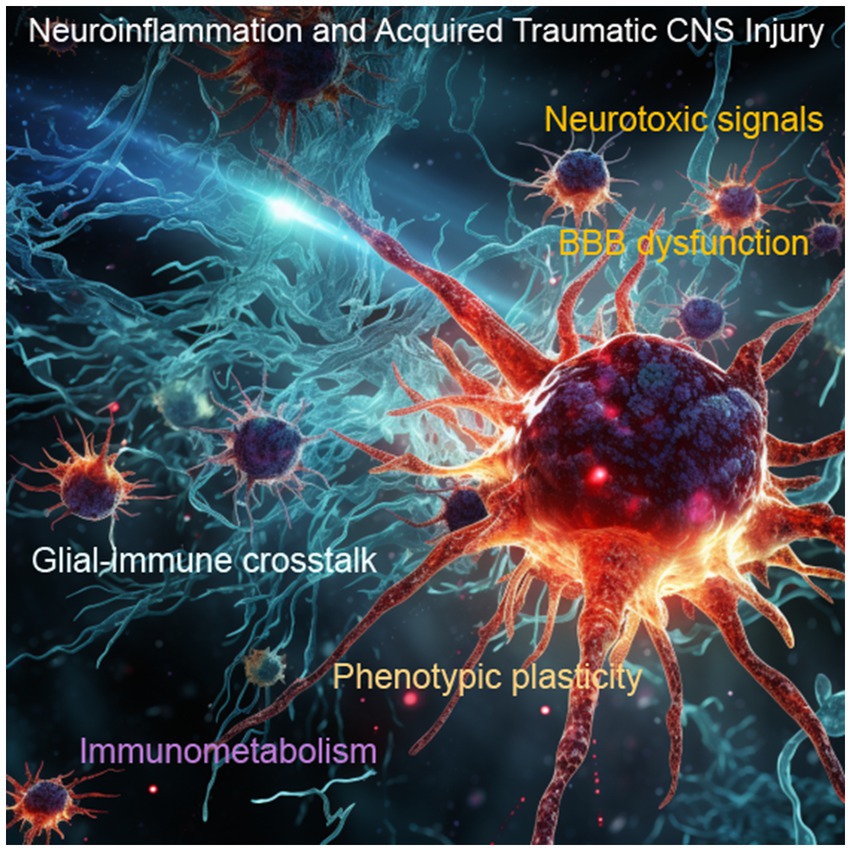
Acquired traumatic central nervous system (CNS) injuries, including traumatic brain injury (TBI) and spinal cord injury (SCI), are devastating conditions with limited treatment options. Neuroinflammation plays a pivotal role in secondary damage, making it a prime target for therapeutic intervention. Emerging therapeutic strategies are designed to modulate the inflammatory response, ultimately promoting neuroprotection and neuroregeneration. The use of anti-inflammatory agents has yielded limited support in improving outcomes in patients, creating a critical need to re-envision novel approaches to both quell deleterious inflammatory processes and upend the progressive cycle of neurotoxic inflammation. This demands a comprehensive exploration of individual, age, and sex differences, including the use of advanced imaging techniques, multi-omic profiling, and the expansion of translational studies from rodents to humans. Moreover, a holistic approach that combines pharmacological intervention with multidisciplinary neurorehabilitation is crucial and must include both acute and long-term care for the physical, cognitive, and emotional aspects of recovery. Ongoing research into neuroinflammatory biomarkers could revolutionize our ability to predict, diagnose, and monitor the inflammatory response in real time, allowing for timely adjustments in treatment regimens and facilitating a more precise evaluation of therapeutic efficacy. The management of neuroinflammation in acquired traumatic CNS injuries necessitates a paradigm shift in our approach that includes combining multiple therapeutic modalities and fostering a more comprehensive understanding of the intricate neuroinflammatory processes at play.
Introduction
Neurotrauma research has undergone a remarkable transformation in recent years. One of the most pressing and intriguing areas of study is the intricate nexus between neuroinflammation and traumatic injuries to the central nervous system (CNS). Traumatic brain injury (TBI) and spinal cord injury (SCI), pose significant challenges to both patients and healthcare providers. These injuries result from a wide range of traumatic events, including accidents, falls, sports-related incidents, and acts of violence, making them a global public health concern (1, 2). Understanding the etiology of TBI and SCI is essential to appreciate the complexity of these conditions and the hurdles they present to effective treatment. Mechanisms of injury include the primary initial impact and the direct damage it inflicts on neural tissue, as well as secondary injury, which evolves over hours to days due to complex pathological processes (3, 4). Secondary injury mechanisms include neuroinflammation, oxidative stress, and excitotoxicity, all of which exacerbate tissue damage and hinder recovery (5, 6). The severity of TBI can range from mild, often characterized by temporary cognitive impairment, to severe, causing profound and lasting neurological deficits (7, 8). The heterogeneity of TBI’s etiology and outcomes underscores the need for individualized treatment approaches. Moreover, recent emphasis has been placed on mechanistic endophenotypes of TBI, which includes neuroinflammation, that may aid in biomarker-based improvements in diagnostic and prognostic trajectories (9). Likewise, the location and severity of SCI are key determinants of the functional deficits experienced by patients. Currently, no curative treatment exists for SCI, making it a life-altering condition with limited therapeutic options.
The role of neuroinflammation in the pathophysiology of traumatic CNS injury is a subject of increasing importance. Neuroinflammation plays a pivotal role in both the acute and chronic phases of these injuries, with the potential to either exacerbate damage or contribute to recovery (10). Neuroinflammation is a dynamic and complex response involving the activation of glial cells, infiltration of immune cells, and the release of various inflammatory mediators within the injured CNS (11). This response is triggered as a protective mechanism to clear debris, fight infection, and facilitate tissue repair. In the acute phase of CNS injury, neuroinflammation can exacerbate tissue damage by contributing to excitotoxicity, oxidative stress, blood–brain barrier dysfunction, and neuronal cell death. Paradoxically, it also participates in reparative processes, such as scar formation, neurogenesis, and synaptic plasticity, which can influence long-term outcomes (12). The intricate balance between neuroinflammation’s detrimental and reparative aspects remains a major challenge in the field. Elucidating the specific factors that tip the scale toward either neuroprotection or neurodegeneration is a crucial objective. Key factors such as timing, location, and duration of neuroinflammatory responses influencing acute and chronic outcomes require comprehensive investigation.
Current research seeks to decipher the intricate signaling pathways and identify potential targets for intervention, aiming to exploit the benefits of neuroinflammation while minimizing its detrimental effects. Addressing these challenges is essential for improving the prognosis and quality of life for individuals affected by traumatic CNS injuries.
Understanding the fundamentals of neuroinflammation
Neuroinflammation is a fundamental process in the CNS characterized by the activation of immune responses within the brain and spinal cord. This complex cascade of events involves glial cells, particularly microglia and astrocytes, as well as immune cells that infiltrate the CNS (13). Neuroinflammation can have both protective and detrimental effects, serving as a double-edged sword. In its protective role, neuroinflammation helps clear debris, fight infections, and promote tissue repair (14, 15). However, when dysregulated, it can lead to prolonged inflammation, contributing to secondary damage, excitotoxicity, oxidative stress, blood–brain barrier disruption, and neuronal cell death (16).
Microglia and astrocytes play vital roles in regulating neuroinflammation, and their interactions involve complex pathways. Promoting the transition of pro-inflammatory microglia to an anti-inflammatory state, reducing the release of pro-inflammatory cytokines, and enhancing the removal of neurotoxic debris through phagocytosis is a critical component of combinatory therapy for CNS trauma (17, 18). Activated astrocytes can impact the BBB by releasing pro-inflammatory cytokines, producing reactive oxygen species (ROS), releasing matrix metalloproteinases (MMPs), upregulating glial fibrillary acidic protein (GFAP) expression, and promoting the expression of chemokines and adhesion molecules, leading to increased permeability, oxidative stress, damage to endothelial cells, and immune cell infiltration into the central nervous system (19, 20).
Microglia and astrocytes can exchange information via the release of signaling molecules such as cytokines, chemokines, and neurotrophic factors (21). For instance, microglia can release interleukin-1β (IL-1β) or tumor necrosis factor-alpha (TNF-α) in response to an inflammatory stimulus, which can then trigger astrocytes to produce chemokines like CCL2 (chemokine ligand 2), attracting immune cells to the site of injury or inflammation. Additionally, both cell types can interact through direct physical contact, such as gap junctions, which allow the exchange of ions, metabolites, and signaling molecules (22). This coordinated communication between microglia and astrocytes is essential for the regulation of neuroinflammatory responses.
Navigating the complex interplay between the neuroimmune response
The interaction between the nervous and immune systems is a central theme in neurotrauma research with profound consequences on neurological outcomes. Microglia can adopt different activation states, ranging from a pro-inflammatory phenotype that releases cytokines and reactive oxygen species, to an anti-inflammatory phenotype that promotes tissue repair and resolution of inflammation (23). The balance between these activation states is critical in determining the trajectory of neuroinflammation and, subsequently, the extent of secondary damage and recovery. Crosstalk between neuroimmune players extends beyond microglia and infiltrating immune cells. Neurons and astrocytes actively communicate with immune cells, influencing their activation and response to injury (24–26). This includes releasing neurotransmitters and neuropeptides that can modulate the activity of microglia and peripheral immune cells.
Microglia and astrocytes also recruit neutrophils to the CNS through a coordinated release of signaling molecules, including chemokines like IL-8, CXCL1 and MIP-2, pro-inflammatory cytokines like IL-1β and TNF-α, and the upregulation of adhesion molecules like ICAM-1 and VCAM-1 on the blood vessel walls (27, 28). These mechanisms create a chemotactic and adhesive environment that guides neutrophils from the bloodstream into the CNS in response to inflammatory or injury-related cues (29). Recent efforts have begun to dissect the role of neutrophil extracellular traps (NETs), web-like structures released by neutrophils to combat infections, in adverse effects on neuronal health following trauma (30). The pro-inflammatory components within NETs trigger local inflammation, and BBB disruption, contributing to neuronal damage. Components of NETs, such as histones and proteases, can directly injure neurons, disrupt synaptic function, and induce cell death, which may lead to cognitive and motor deficits (31–33). Thus, understanding and targeting the detrimental effects of NETs in the CNS is an active area of research with the potential to offer new therapeutic avenues.
Unraveling metabolic regulation of neuroinflammation in neurotrauma
Neuroinflammation is not a one-size-fits-all phenomenon. Its consequences can vary depending on factors such as age, sex, metabolic conditions, and epigenetic stressors (34–36). The dynamic changes in epigenetics and the reprogramming of immunometabolism influence modifications in how cells respond to internal and external signals and subsequent cell fate decisions. Metabolic regulation is a fundamental aspect of how different neuroimmune cells function within the central nervous system (CNS). Immune cells, such as microglia and infiltrating monocytes, as well as glial cells like astrocytes, adapt their metabolic profiles in response to various challenges and signaling pathways which allows for plastic use of energy substrates (37). Single-cell sequencing and omics analysis have provided valuable insights into the metabolic diversity among these cells (38, 39). Microglia, for instance, exhibit a high degree of plasticity, switching between glycolytic and oxidative phosphorylation pathways depending on their activation state. In their pro-inflammatory state, microglia tend to favor glycolysis, which generates energy quickly but is less efficient, while an anti-inflammatory state often corresponds to increased oxidative phosphorylation, which produces more ATP (37). Single-cell sequencing has unveiled the complexity of these metabolic shifts, highlighting the intricate balance required to maintain immune responses and CNS homeostasis.
Astrocytes, on the other hand, primarily rely on glycolysis for energy production (40). This metabolic profile supports their critical functions in neurotransmitter recycling and maintaining the blood–brain barrier. Importantly, astrocytes can release lactate, which serves as an energy source for neurons, emphasizing their role in the metabolic regulation of the CNS. Single-cell sequencing has revealed heterogeneity among astrocytes, suggesting that specific subpopulations may have distinct metabolic profiles and functions (41). Understanding these metabolic differences among neuroimmune and glial cells at the single-cell level is essential for developing targeted interventions that can modulate their metabolic responses, potentially optimizing neuroinflammatory processes and promoting neuroprotection in various neurological disorders.
Diverse research approaches and developing innovative therapeutic strategies to retool the neuroimmune response
The intricacies of neurotrauma-induced neuroinflammation demand a collaborative endeavor encompassing various research methods, both in basic science and translational applications. This multidisciplinary approach fosters advances that underscore the importance of inclusivity in the research process. Current approaches to date, include the use of immunomodulatory therapies, and monoclonal antibodies that block pro-inflammatory cytokines like tumor necrosis factor-alpha (TNF) or interleukin-1β (IL-1β) that can dampen the neuroinflammatory response (42). The use of cell-based therapies, such as chimeric antigen receptor (CAR) T-cell therapy, and dendritic or myeloid-derived suppressor cell (MDSC) or mesenchymal stem cells (MSCs) therapies have been investigated (43, 44). Engineered cells may offer a controlled release of anti-inflammatory factors aimed at creating an immunosuppressive environment. Furthermore, nanotechnology-based strategies are being explored to enable targeted drug delivery to specific cell populations such as phagocytic cells (45).
Artificial intelligence (AI) and machine learning have become invaluable tools in the study of neuroinflammation due to their ability to analyze complex and vast datasets, recognize patterns, and make predictions based on data-driven insights. These technologies play a pivotal role in identifying novel biomarkers for neuroinflammatory conditions, which can aid in early diagnosis and disease monitoring (46). AI and machine learning can integrate multi-omics data, including genomics, transcriptomics, proteomics, and metabolomics, to uncover intricate molecular mechanisms underlying neuroinflammation (47). By identifying gene expression patterns, epigenetic modifications, and metabolic signatures associated with neuroinflammation, a deeper understanding of new and novel pathways may be revealed. As such, AI-powered predictive models can help assess treatment responses and prognosis, and support the categorization of neuroinflammatory endophenotypes in brain trauma (48–50). Further, neuromodulation techniques or non-invasive approaches including focused ultrasound, are being explored to directly influence the activity of neuroimmune cells within the CNS (51). These non-invasive approaches have the potential to modulate neuroinflammatory responses, by facilitating the delivery of immunotherapeutic agents into the brain and exerting direct immune-related effects (52, 53). As these technologies continue to advance, they hold the promise of revolutionizing our understanding of neuroinflammation and improving diagnostic and treatment strategies.
Conclusion
Neuroinflammation in the context of acquired traumatic CNS injury underscores the complexity and multifaceted nature of the neuroimmune response. Recent advances in understanding the metabolic and phenotypic regulation of neuroimmune cells, the complex interplay between different cell types, and the development of innovative therapeutic strategies have shed new light on potential interventions for mitigating neuroinflammatory processes. Diverse research approaches, from single-cell omics analysis to AI integration, offer promising avenues for unraveling the intricate pathophysiological dimensions of neuroinflammation.
Author contributions
MT: Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health, R01NS112541 (MT), NS121103 (MT), NS119540 (MT).
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
TBI, Traumatic brain injury; SCI, Spinal cord injury; CNS, Central nervous system; ROS, Reactive oxygen species; MMPs, Matrix metalloproteinases; GFAP, Glial fibrillary acidic protein.
References
1. Badhiwala, JH, Wilson, JR, and Fehlings, MG. Global burden of traumatic brain and spinal cord injury. Lancet Neurol. (2019) 18:24–5. doi: 10.1016/S1474-4422(18)30444-7
2. Guan, B, Anderson, DB, Chen, L, Feng, S, and Zhou, H. Global, regional and national burden of traumatic brain injury and spinal cord injury, 1990-2019: a systematic analysis for the global burden of disease study 2019. BMJ Open. (2023) 13:e075049. doi: 10.1136/bmjopen-2023-075049
3. Alizadeh, A, Dyck, SM, and Karimi-Abdolrezaee, S. Traumatic spinal cord injury: an overview of pathophysiology, models and acute injury mechanisms. Front Neurol. (2019) 10:282. doi: 10.3389/fneur.2019.00282
4. Anjum, A, Yazid, MD, Fauzi Daud, M, Idris, J, Ng, AMH, Selvi Naicker, A, et al. Spinal cord injury: pathophysiology, multimolecular interactions, and underlying recovery mechanisms. Int J Mol Sci. (2020) 21, 1–35. doi: 10.3390/ijms21207533
5. Schimmel, SJ, Acosta, S, and Lozano, D. Neuroinflammation in traumatic brain injury: a chronic response to an acute injury. Brain Circ. (2017) 3:135–42. doi: 10.4103/bc.bc_18_17
6. Jarrahi, A, Braun, M, Ahluwalia, M, Gupta, RV, Wilson, M, Munie, S, et al. Revisiting traumatic brain injury: from molecular mechanisms to therapeutic interventions. Biomedicines. (2020) 8, 1–42. doi: 10.3390/biomedicines8100389
7. Brenner, LA, Vanderploeg, RD, and Terrio, H. Assessment and diagnosis of mild traumatic brain injury, posttraumatic stress disorder, and other polytrauma conditions: burden of adversity hypothesis. Rehabil Psychol. (2009) 54:239–46. doi: 10.1037/a0016908
8. Ganti, L, Daneshvar, Y, Bodhit, A, Ayala, S, Patel, PS, Lottenberg, LL, et al. TBI ADAPTER: traumatic brain injury assessment diagnosis advocacy prevention and treatment from the emergency room--a prospective observational study. Mil Med. (2015) 180:380–6. doi: 10.7205/MILMED-D-14-00316
9. Wilde, EA, Wanner, IB, Kenney, K, Gill, J, Stone, JR, Disner, S, et al. A framework to advance biomarker development in the diagnosis, outcome prediction, and treatment of traumatic brain injury. J Neurotrauma. (2022) 39:436–57. doi: 10.1089/neu.2021.0099
10. Gorji, A. Neuroinflammation: the pathogenic mechanism of neurological disorders. Int J Mol Sci. (2022) 23, 1–5. doi: 10.3390/ijms23105744
11. Yang, QQ, and Zhou, JW. Neuroinflammation in the central nervous system: symphony of glial cells. Glia. (2019) 67:1017–35. doi: 10.1002/glia.23571
12. DiSabato, DJ, Quan, N, and Godbout, JP. Neuroinflammation: the devil is in the details. J Neurochem. (2016) 139:136–53. doi: 10.1111/jnc.13607
13. Ransohoff, RM, Schafer, D, Vincent, A, Blachere, NE, and Bar-Or, A. Neuroinflammation: ways in which the immune system affects the brain. Neurotherapeutics. (2015) 12:896–909. doi: 10.1007/s13311-015-0385-3
14. Banjara, M, and Ghosh, C. Sterile Neuroinflammation and strategies for therapeutic intervention. Int J Inflam. (2017) 2017:8385961–20. doi: 10.1155/2017/8385961
15. Cherry, JD, Olschowka, JA, and O'Banion, MK. Neuroinflammation and M2 microglia: the good, the bad, and the inflamed. J Neuroinflammation. (2014) 11:98. doi: 10.1186/1742-2094-11-98
16. Simon, DW, McGeachy, MJ, Bayir, H, Clark, RSB, Loane, DJ, and Kochanek, PM. The far-reaching scope of neuroinflammation after traumatic brain injury. Nat Rev Neurol. (2017) 13:572. doi: 10.1038/nrneurol.2017.116
17. Shao, F, Wang, X, Wu, H, Wu, Q, and Zhang, J. Microglia and Neuroinflammation: crucial pathological mechanisms in traumatic brain injury-induced neurodegeneration. Front Aging Neurosci. (2022) 14:825086. doi: 10.3389/fnagi.2022.825086
18. Mills, J, Ladner, L, Soliman, E, Leonard, J, Morton, PD, and Theus, MH. Cross-talk and subset control of microglia and associated myeloid cells in neurological disorders. Cell. (2022) 11, 1–22. doi: 10.3390/cells11213364
19. Mira, RG, Lira, M, and Cerpa, W. Traumatic brain injury: mechanisms of glial response. Front Physiol. (2021) 12:740939. doi: 10.3389/fphys.2021.740939
20. Michinaga, S, and Koyama, Y. Pathophysiological responses and roles of astrocytes in traumatic brain injury. Int J Mol Sci. (2021) 22:1–17. doi: 10.3390/ijms22126418
21. Matejuk, A, and Ransohoff, RM. Crosstalk between astrocytes and microglia: an overview. Front Immunol. (2020) 11:1416. doi: 10.3389/fimmu.2020.01416
22. Liu, LR, Liu, JC, Bao, JS, Bai, QQ, and Wang, GQ. Interaction of microglia and astrocytes in the neurovascular unit. Front Immunol. (2020) 11:1024. doi: 10.3389/fimmu.2020.01024
23. Butovsky, O, and Weiner, HL. Microglial signatures and their role in health and disease. Nat Rev Neurosci. (2018) 19:622–35. doi: 10.1038/s41583-018-0057-5
24. Han, RT, Kim, RD, Molofsky, AV, and Liddelow, SA. Astrocyte-immune cell interactions in physiology and pathology. Immunity. (2021) 54:211–24. doi: 10.1016/j.immuni.2021.01.013
25. Xie, L, and Yang, SH. Interaction of astrocytes and T cells in physiological and pathological conditions. Brain Res. (2015) 1623:63–73. doi: 10.1016/j.brainres.2015.03.026
26. Dantzer, R. Neuroimmune interactions: from the brain to the immune system and vice versa. Physiol Rev. (2018) 98:477–504. doi: 10.1152/physrev.00039.2016
27. Liu, P, Wang, X, Yang, Q, Yan, X, Fan, Y, Zhang, S, et al. Collaborative action of microglia and astrocytes mediates neutrophil recruitment to the CNS to defend against Escherichia coli K1 infection. Int J Mol Sci. (2022) 23, 1–18. doi: 10.3390/ijms23126540
28. Drummond, RA, Swamydas, M, Oikonomou, V, Zhai, B, Dambuza, IM, Schaefer, BC, et al. CARD9(+) microglia promote antifungal immunity via IL-1beta- and CXCL1-mediated neutrophil recruitment. Nat Immunol. (2019) 20:559–70. doi: 10.1038/s41590-019-0377-2
29. Metzemaekers, M, Gouwy, M, and Proost, P. Neutrophil chemoattractant receptors in health and disease: double-edged swords. Cell Mol Immunol. (2020) 17:433–50. doi: 10.1038/s41423-020-0412-0
30. Papayannopoulos, V. Neutrophil extracellular traps in immunity and disease. Nat Rev Immunol. (2018) 18:134–47. doi: 10.1038/nri.2017.105
31. Shi, G, Liu, L, Cao, Y, Ma, G, Zhu, Y, Xu, J, et al. Inhibition of neutrophil extracellular trap formation ameliorates neuroinflammation and neuronal apoptosis via STING-dependent IRE1alpha/ASK1/JNK signaling pathway in mice with traumatic brain injury. J Neuroinflammation. (2023) 20:222. doi: 10.1186/s12974-023-02903-w
32. Vaibhav, K, Braun, M, Alverson, K, Khodadadi, H, Kutiyanawalla, A, Ward, A, et al. Neutrophil extracellular traps exacerbate neurological deficits after traumatic brain injury. Sci Adv. (2020) 6:eaax8847. doi: 10.1126/sciadv.aax8847
33. Feng, Z, Min, L, Liang, L, Chen, B, Chen, H, Zhou, Y, et al. Neutrophil extracellular traps exacerbate secondary injury via promoting Neuroinflammation and blood-spinal cord barrier disruption in spinal cord injury. Front Immunol. (2021) 12:698249. doi: 10.3389/fimmu.2021.698249
34. Bekhbat, M, and Neigh, GN. Sex differences in the neuro-immune consequences of stress: focus on depression and anxiety. Brain Behav Immun. (2018) 67:1–12. doi: 10.1016/j.bbi.2017.02.006
35. Brickler, TR, Hazy, A, Guilhaume Correa, F, Dai, R, Kowalski, EJA, Dickerson, R, et al. Angiopoietin/Tie2 Axis regulates the age-at-injury cerebrovascular response to traumatic brain injury. J Neurosci. (2018) 38:9618–34. doi: 10.1523/JNEUROSCI.0914-18.2018
36. Zhu, X, Chen, Z, Shen, W, Huang, G, Sedivy, JM, Wang, H, et al. Inflammation, epigenetics, and metabolism converge to cell senescence and ageing: the regulation and intervention. Signal Transduct Target Ther. (2021) 6:245. doi: 10.1038/s41392-021-00646-9
37. Lauro, C, and Limatola, C. Metabolic reprograming of microglia in the regulation of the innate inflammatory response. Front Immunol. (2020) 11:493. doi: 10.3389/fimmu.2020.00493
38. Gustafsson, J, Anton, M, Roshanzamir, F, Jornsten, R, Kerkhoven, EJ, Robinson, JL, et al. Generation and analysis of context-specific genome-scale metabolic models derived from single-cell RNA-Seq data. Proc Natl Acad Sci USA. (2023) 120:e2217868120. doi: 10.1073/pnas.2217868120
39. Ahl, PJ, Hopkins, RA, Xiang, WW, Au, B, Kaliaperumal, N, Fairhurst, AM, et al. Met-flow, a strategy for single-cell metabolic analysis highlights dynamic changes in immune subpopulations. Commun Biol. (2020) 3:305. doi: 10.1038/s42003-020-1027-9
40. Turner, DA, and Adamson, DC. Neuronal-astrocyte metabolic interactions: understanding the transition into abnormal astrocytoma metabolism. J Neuropathol Exp Neurol. (2011) 70:167–76. doi: 10.1097/NEN.0b013e31820e1152
41. Batiuk, MY, Martirosyan, A, Wahis, J, de Vin, F, Marneffe, C, Kusserow, C, et al. Identification of region-specific astrocyte subtypes at single cell resolution. Nat Commun. (2020) 11:1220. doi: 10.1038/s41467-019-14198-8
42. Strzelec, M, Detka, J, Mieszczak, P, Sobocinska, MK, and Majka, M. Immunomodulation-a general review of the current state-of-the-art and new therapeutic strategies for targeting the immune system. Front Immunol. (2023) 14:1127704. doi: 10.3389/fimmu.2023.1127704
43. Bonilla, C, and Zurita, M. Cell-based therapies for traumatic brain injury: therapeutic treatments and clinical trials. Biomedicines. (2021) 9, 1–32. doi: 10.3390/biomedicines9060669
44. von Baumgarten, L, Stauss, HJ, and Lunemann, JD. Synthetic cell-based immunotherapies for neurologic diseases. Neurol Neuroimmunol Neuroinflamm. (2023) 10, 1–3. doi: 10.1212/NXI.0000000000200139
45. Cerqueira, SR, Ayad, NG, and Lee, JK. Neuroinflammation treatment via targeted delivery of nanoparticles. Front Cell Neurosci. (2020) 14:576037. doi: 10.3389/fncel.2020.576037
46. Vatansever, S, Schlessinger, A, Wacker, D, Kaniskan, HU, Jin, J, Zhou, MM, et al. Artificial intelligence and machine learning-aided drug discovery in central nervous system diseases: state-of-the-arts and future directions. Med Res Rev. (2021) 41:1427–73. doi: 10.1002/med.21764
47. Gaetani, L, Bellomo, G, Parnetti, L, Blennow, K, Zetterberg, H, and Di Filippo, M. Neuroinflammation and Alzheimer's disease: a machine learning approach to CSF proteomics. Cell. (2021) 10, 1–12. doi: 10.3390/cells10081930
48. Abu Hamdeh, S, Tenovuo, O, Peul, W, and Marklund, N. "omics" in traumatic brain injury: novel approaches to a complex disease. Acta Neurochir. (2021) 163:2581–94. doi: 10.1007/s00701-021-04928-7 1–12.
49. Vaughan, LE, Ranganathan, PR, Kumar, RG, Wagner, AK, and Rubin, JE. A mathematical model of neuroinflammation in severe clinical traumatic brain injury. J Neuroinflammation. (2018) 15:345. doi: 10.1186/s12974-018-1384-1
50. Galbusera, F, Casaroli, G, and Bassani, T. Artificial intelligence and machine learning in spine research. JOR Spine. (2019) 2:e1044. doi: 10.1002/jsp2.1044
51. Curley, CT, Sheybani, ND, Bullock, TN, and Price, RJ. Focused ultrasound immunotherapy for central nervous system pathologies: challenges and opportunities. Theranostics. (2017) 7:3608–23. doi: 10.7150/thno.21225
52. Huang, L, Kang, J, Chen, G, Ye, W, Meng, X, Du, Q, et al. Low-intensity focused ultrasound attenuates early traumatic brain injury by OX-A/NF-kappaB/NLRP3 signaling pathway. Aging (Albany NY). (2022) 14:7455–69. doi: 10.18632/aging.204290
Keywords: inflammation, immunometabolism, glia, traumatic brain injury, spinal cord injury, Neurotoxic injury, phenotypic plasticity, peripheral immune cells
Citation: Theus MH (2024) Neuroinflammation and acquired traumatic CNS injury: a mini review. Front. Neurol. 15:1334847. doi: 10.3389/fneur.2024.1334847
Edited by:
Lingxiao Deng, Indiana University, United StatesReviewed by:
Stuart Iain Jenkins, Keele University, United KingdomCopyright © 2024 Theus. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michelle H. Theus, bXRoZXVzQHZ0LmVkdQ==
 Michelle H. Theus
Michelle H. Theus