- 1Department of Neurointervention, Zhangzhou Affiliated Hospital of Fujian Medical University, Zhangzhou, China
- 2Department of Neurology, Heze Municipal Hospital, Heze, China
- 3Department of Neurology, Ganzhou People’s Hospital, Ganzhou, China
Background: Few studies have focused on factors associated with futile recanalization in patients with an acute basilar artery occlusion (BAO) that was treated with modern endovascular therapy (EVT). The aim of this study was to explore the factors associated with futile recanalization in patients with an acute BAO presented within 12 h.
Methods: This is a post-hoc analysis of the ATTENTION trial (The Trial of Endovascular Treatment of Acute Basilar-Artery Occlusion, ClinicalTrials.gov, number NCT 04751708). Demographics, clinical characteristics, acute stroke workflow interval times, and imaging characteristics were compared between the futile recanalization and favorable recanalization groups. The favorable outcome was defined as a modified Rankin scale (mRS) score of 0–3 at 90 days, successful reperfusion was defined as thrombolysis in cerebral infarction (TICI) 2b and 3 on the final angiogram, and futile recanalization was defined as failure to achieve a favorable outcome despite successful reperfusion. A multivariate analysis was performed to identify the predictors of futile recanalization.
Results: In total, 185 patients were included in the final analysis: 89 (48.1%) patients had futile recanalization and 96 (51.9%) patients had favorable recanalization. In the multivariable logistic regression analysis, older age (OR 1.04, 95% CI 1.01 to 1.08, p = 0.01) and diabetes mellitus (OR 3.35, 95% CI 1.40 to 8.01, p = 0.007) were independent predictors of futile recanalization.
Conclusion: Futile recanalization occurred in nearly half of patients with acute BAO following endovascular treatment. Old age and diabetes mellitus were identified as independent predictors of futile recanalization after endovascular therapy for acute BAO.
1 Introduction
Stroke caused by acute basilar artery occlusion (BAO) is associated with high morbidity and mortality (1, 2). Endovascular therapy (EVT) can quickly open the occluded artery and improve the prognosis of stroke patients with intracranial large artery occlusion (LVO) and is the standard treatment for LVO in the anterior circulation (3). Recently, two breakthrough trials showed the clinical benefit of EVT for BAO (4, 5). According to the results of the ATTENTION trial (the Trial of Endovascular Treatment of Acute Basilar-Artery Occlusion, ClinicalTrials. gov, number NCT 04751708) (4), the proportion of patients with successful reperfusion (modified thrombolysis in cerebral infarction (mTICI) ≥2b) was 93.0%. However, the rate of a favorable outcome (defined as a modified Rankin scale (mRS) score of 0–3) was only 46% (4), indicating that approximately 50% of patients failed to achieve a favorable outcome despite successful recanalization, and this phenomenon was defined as futile recanalization. The risk factors and incidence of futile recanalization in patients with ischemic stroke caused by BAO undergoing EVT have yet to be identified. Thus, in this study, we analyzed data from the ATTENTION trial to identify the incidence and predictive factors of futile recanalization.
2 Methods
The ATTENTION trial was an investigator-initiated, multicenter, prospective, randomized, open-label trial that investigated the outcomes of EVT in Chinese stroke patients with basilar artery occlusion (BAO). The study methods and patient eligibility criteria have been reported previously (4). Patients who were not followed up, did not undergo catheter angiography, or had failed recanalization (mTICI <2b) were excluded from this subgroup analysis. In order to minimize the impact of the premorbid state, patients with a premorbid mRS score of ≥1 were also excluded from this study.
The baseline information included age, sex, baseline National Institutes of Health Stroke Scale (NIHSS) score, history of hypertension, dyslipidemia, diabetes, smoking, atrial fibrillation, previous stroke/transient ischemic attack (TIA), and coronary artery disease. The cause of stroke included cardioembolic, large-artery atherosclerosis, undetermined causes, or other determined causes. The symptom onset to presentation time, reperfusion time, whether intravenous thrombolysis was performed, time of endovascular procedure initiation, and recanalization time were also recorded.
All patients underwent head CT on admission; the baseline infarct range was assessed by posterior circulation using the Alberta Stroke Program Early CT Score (PC-ASPECTS) with non-contrast CT; and the location of the intracranial artery occlusion was identified on digital subtraction angiography (DSA), which included the vertebral artery V4, proximal basilar artery, middle basilar artery, and distal basilar artery. The mTICI score assessed on the final angiogram indicated successful reperfusion, which was graded as 2b or 3 (4). Perioperative complications, including symptomatic intracranial hemorrhage (sICH), thromboembolism, thrombosis or plaque shedding, arterial dissection and vessel perforation, and patency at 24–72 h on computed tomography angiography (CTA) or magnetic resonance angiography (MRA) were also recorded.
2.1 Ethics approval
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients/participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
2.2 Statistical analysis
Clinical and radiological outcomes were dichotomized into the favorable recanalization group (defined as a 90-day mRS score ≤ 3) and the futile recanalization group (defined as a 90-day mRS score > 3). The association between futile recanalization and baseline clinical variables, imaging characteristics, and acute stroke workflow interval times was examined in the univariate analysis. Continuous data were summarized as a median and interquartile range (IQR) or as means and standard deviation. Means and medians were compared using the t-test and Mann–Whitney U-test, respectively. Frequencies were compared using the χ2 test. Multivariate logistic regression was used to determine the relationship between confounders and futile recanalization. To maximize sensitivity, variables with a p-value of <0.05 were entered into the multivariate logistic regression with a backward likelihood ratio model. The confounders adjusted for included age, diabetes mellitus, baseline NIHSS score, and baseline GCS score. Data are presented as the adjusted odds ratio (OR) and its 95% confidence interval (95% CI). All analyses were performed using SPSS software, version 22.0 (SPSS, Chicago, IL, USA), with a significance level of a p-value of <0.05 (two-sided).
3 Results
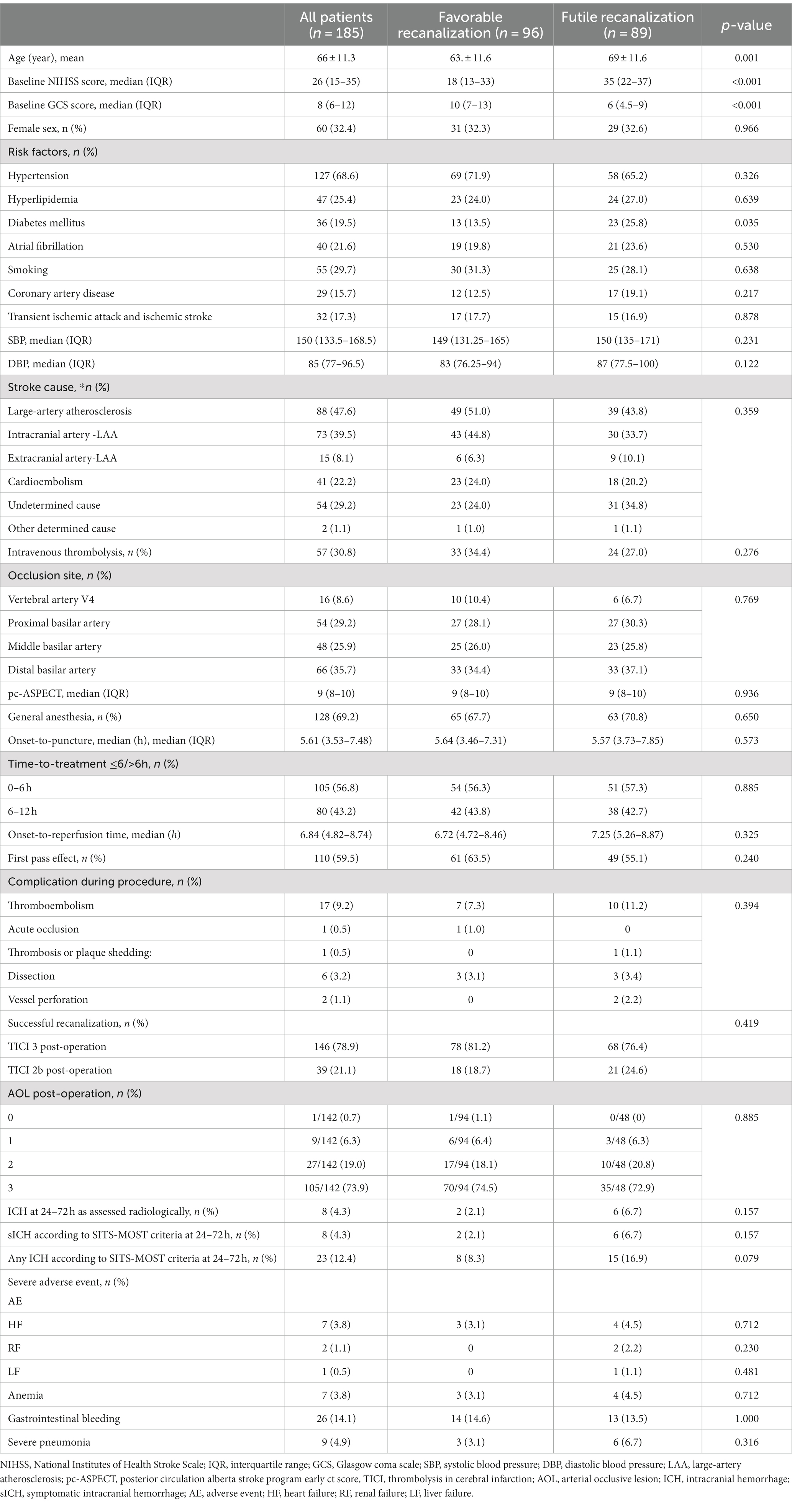
From 21 February 2021 to 3 January 2022, a total of 507 patients were assessed for eligibility for the ATTENTION trial; a total of 342 patients were enrolled in the trial (4). In total, 228 patients were allocated to the thrombectomy group and 114 were allocated to the best medical treatment. The legal representatives of two patients who had been assigned to the thrombectomy group withdrew their consent, so 226 patients in the thrombectomy group were included. Successful reperfusion was achieved in 208 (92.0%) patients. After excluding 23 patients with pre-mRS scores of 1 or 2, 185 patients were included in the analysis (Figure 1).
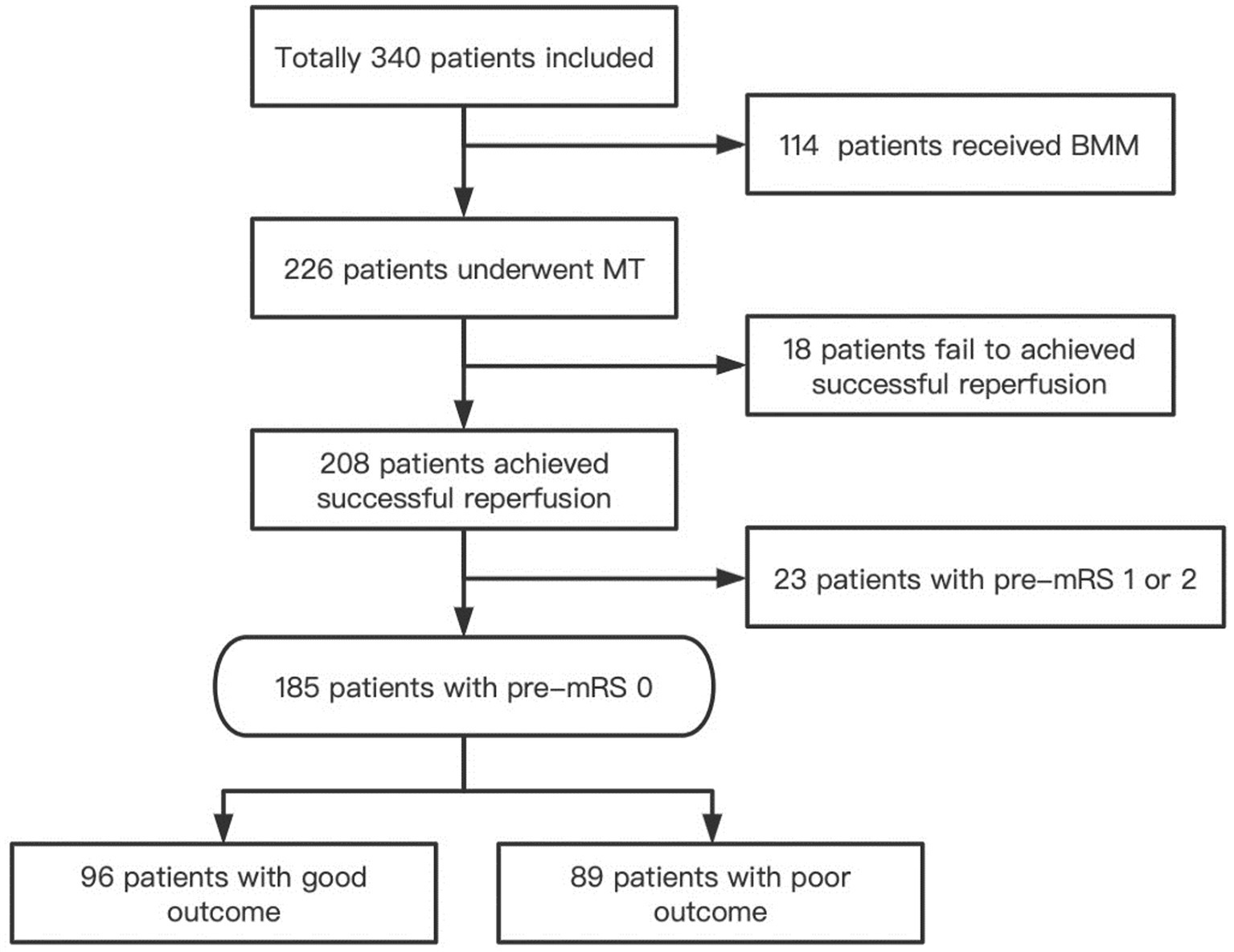
Figure 1. Flowchart. BMM, Indicate best medical management; MT, Mechanical thrombectomy; mRS, Modified rankin scale.
Futile recanalization was observed in 89 (48.1%) patients, favorable recanalization in 96 (51.9%) patients, and death in 57 (30.8%) patients. The baseline characteristics of the patients are listed in Table 1. Compared with the patients in the favorable recanalization group, the patients in the futile recanalization group were significantly older (mean 69 vs. 63 years, p = 0.001) and had significantly higher NIHSS scores (median 35 vs. 18, p < 0.001) on admission, lower admission baseline GCS scores (median 6 vs. 10, p < 0.001), and a higher prevalence of diabetes mellitus (25.8% vs. 13.5%, p = 0.035).
There were 36 patients with diabetes mellitus and 149 patients without diabetes mellitus. Patients with diabetes had a higher mortality rate (25.0% vs. 20.1%, p = 0.521), a higher prevalence of sICH (8.8% vs. 3.6%, p = 0.196), and less functional independence (36.1% vs. 55.7%, p = 0.035) than those without diabetes (Figure 2). Patients with TICI 3 reperfusion had a trend of a lower mortality rate (30.1% vs. 33.3%, p = 0.701) and a better prognosis (53.4% vs. 46.2%, p = 0.419) than patients with TICI 2b reperfusion.
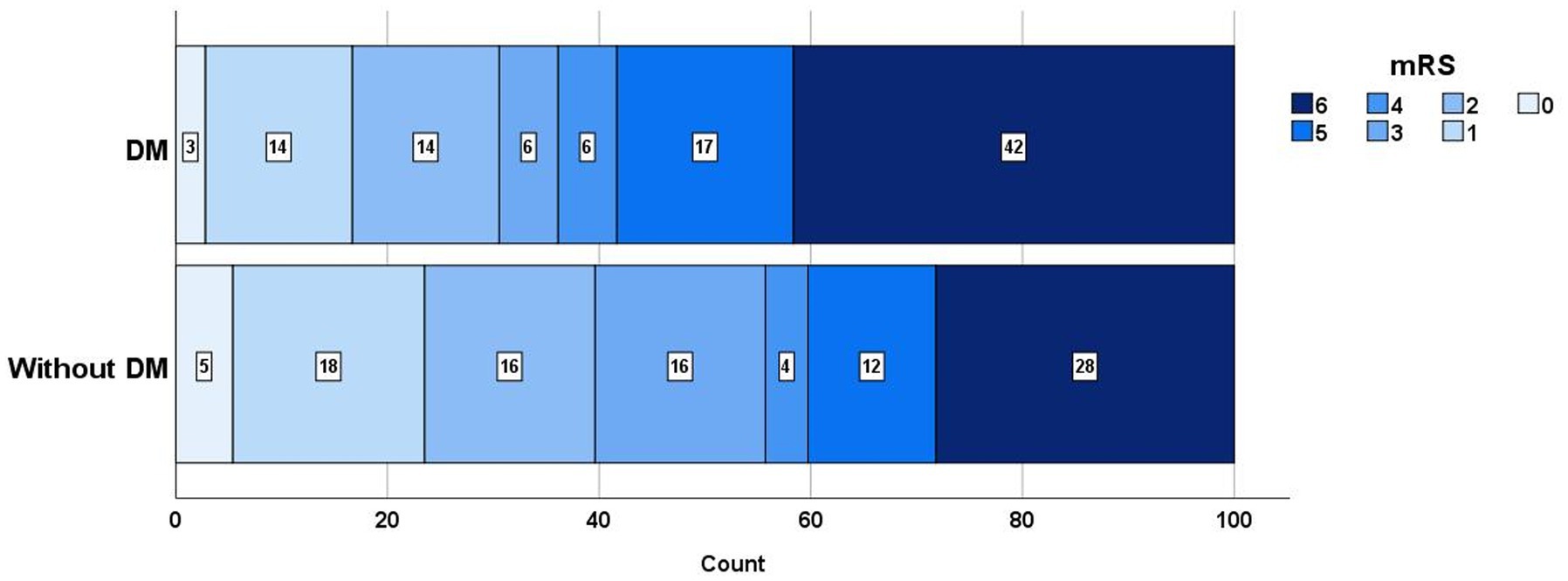
Figure 2. mRS distribution in patients with DM and without DM. mRS, Indicate modified Rankin scale; DM, Diabetes mellitus.
In the multivariable logistic regression analysis (Table 2), the following factors were associated with futile recanalization: older age (OR 1.04, 95% CI 1.01–1.08, p = 0.01) and diabetes mellitus (OR 3.35, 95% CI 1.40–8.01, p = 0.0107).
4 Discussion
Due to the development of EVT techniques and adjustment of patient selection (i.e., NIHSS>6), trials have shown that patients with acute ischemic stroke caused by basilar artery occlusion can benefit from EVT (4, 5). However, despite successful recanalization, some patients suffer a poor prognosis, a condition referred to as futile recanalization. In the current study, a subgroup analysis from the ATTENTION research revealed that the rate of futile recanalization was 48.1%, which is similar to the 45.1% (6) and 46.9% (7) reported previously but lower than the 62.8% (8). The highest rate was reported in the study by Yang et al. (8), and the main reason may be the different onset-to-reperfusion times, in which presentation within 24 h was included in Yang et al.’s study, and only presentation within 12 h was included in our study and 8 h in Pop et al.’s study.
Our post-hoc analysis demonstrated that old age and diabetes mellitus were associated with a higher risk of futile recanalization. Consistent with a previous study, older age was associated with futile recanalization (6, 9)in acute BAO patients, which is similar to the results observed in acute anterior circulation LVO (10). Age is a common factor that is associated with clinical outcomes in patients with LVO who underwent EVT. The HERMES meta-analysis showed that in patients over 80 years old who received EVT, the good prognosis rate decreased to 29.8% (10), and the functional independence rate decreased with increasing age in patients with low ASPECTS (11). The possible reasons are listed as follows: a. Elderly patients often have a poor arterial collateral network (9), which is associated with a good prognosis; b. Elderly patients are more likely to have cardiovascular risk factors, such as hypertension, diabetes mellitus, and smoking, which can impair endothelial function and stiffen the vessels’ myogenic tone, affecting the self-regulating ability of arteries (12); c. Leukoaraiosis is more common in elderly patients and is an imaging marker of poor prognosis in patients who receive EVT (13); d. Elderly patients often have more comorbidities that limit their complete rehabilitation.
Our study revealed that diabetes mellitus is another factor that is associated with futile recanalization. A meta-analysis has demonstrated that diabetes mellitus is linked to unfavorable functional outcomes, increased mortality, and poor postprocedural safety outcomes, including symptomatic intracranial hemorrhage (sICH) and hypertension (HT) (14). Genceviciute also discovered that diabetes mellitus, especially admission hyperglycemia, was associated with less frequently successful reperfusion, worse 3-month functional outcomes, and in-hospital symptomatic intracranial hemorrhage in acute anterior circulation stroke patients who underwent EVT (15, 16). The possible reason for these findings may be that hyperglycemia is associated with an increased risk of infarct growth as it may potentially increase the vulnerability of the penumbra (15), and hyperglycemia is associated with unsuccessful recanalization. An animal study showed increased MMP-9, the receptor for advanced glycation end products, and vascular endothelial growth factor in diabetic mice, which were associated with increased blood–brain barrier leakage (17), which can explain why hemorrhage transformation was more commonly observed in acute stroke patients with diabetes mellitus who received reperfusion therapy than in patients without diabetes mellitus. Consistent with a previous study, our study showed that sICH was more common in patients with diabetes mellitus although without statistical significance probably due to the small sample size.
Compared with incomplete reperfusion, complete reperfusion (18), especially the first pass to achieve complete reperfusion, which is called the first pass effect (19–21), is related to better outcomes. De Havenon et al.’s study also showed that the benefit of recanalization in BAO patients was significantly decreased when recanalization was achieved after more than three attempts (22). However, in our study, we did not observe a correlation between the first-pass effect and clinical outcome, and this phenomenon was also observed in another study (6, 8). Interestingly, Yang’s study found that stent retriever passes were associated with futile recanalization in patients with late time windows (defined as 6–24 h), but the association was not observed in the early time window group (8). The discrepancy between the two groups may be attributed to the following reasons: the scope of the ischemic penumbra was larger in the early time window than in the late time window, which may minimize the influence of mechanical thrombectomy passes, and this can also explain the results of our study for the median onset-to-puncture’s time was 5.61 h, which was obviously shorter than that in Yang et al.’s study (8.88 h) (8).
Our study did not find any specific futile recanalization predictive factors that were not reported in previous studies. However, there were some strengths of our study: first, the dataset was acquired through a nationwide multicentric randomized controlled trial of consecutive thrombectomy procedures, and second, a systematic independent 90-day follow-up with adjudication of clinical outcomes was performed. All these factors make the data more reliable than that in the registry study. Nevertheless, there are certain limitations of our study. First, although data were prospectively registered, all data of this subgroup analysis were retrospectively assessed. Second, patients with a prestroke mRS score of ≥1 were excluded to reduce the influence of a previous stroke history on the clinical outcome. Third, the sample size is not large enough to explore more variables that are associated with futile recanalization. Fourth, blood glucose was not recorded on admission, which is a better indicator of futile recanalization. Fifth, the term futile recanalization suggests that patients might as well not have undergone mechanical thrombectomy; however, our study did not compare the therapeutic effect of mechanical thrombectomy with the best medical management, so we cannot know what the outcome of these patients would have been without endovascular treatment.
5 Conclusion
In our post-hoc analysis, we observed that futile recanalization is common in patients with BAO following endovascular treatment. Old age and diabetes mellitus were independent predictors of futile recanalization after endovascular therapy for acute BAO.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
TY: Writing – original draft, Writing – review & editing, Conceptualization, Formal analysis, Funding acquisition. KL: Conceptualization, Data curation. X-hL: Data curation, Methodology. D-lL: Data curation, Formal analysis. Y-MW: Data curation, Methodology. Z-nP: Data curation, Methodology. X-fZ: Data curation, Methodology. R-cC: Data curation, Methodology. GZ: Data curation, Methodology. W-hC: Conceptualization, Methodology, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study was funded by the National Health Commission Capacity Building and Continuing Education Center (Grant No. GWJJ2021100203) and the Research on Appropriate Intervention Technique for High-risk Crowds of Stroke (Grant No. BHPA2021IN002).
Acknowledgments
The authors thank the team of American Journal Experts for editing the English text of a draft of this manuscript (https://secure.aje.com).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Schonewille, WJ , Wijman, CAC , Michel, P , Rueckert, C , Weimar, C , Mattle, H, et al. Treatment and outcomes of acute basilar artery occlusion in the basilar artery international cooperation study (BASICS): a prospective registry study. Lancet Neurol. (2009) 8:724–30. doi: 10.1016/S1474-4422(09)70173-5
2. Liu, X , Dai, Q , Ye, R , Zi, W , Liu, Y , Wang, H, et al. Endovascular treatment versus standard medical treatment for vertebrobasilar artery occlusion (BEST): an open-label, randomised controlled trial. Lancet Neurol. (2020) 19:115–22. doi: 10.1016/S1474-4422(19)30395-3
3. Powers, WJ , Rabinstein, AA , Ackerson, T , Adeoye, OM , Bambakidis, NC , Becker, K, et al. Guidelines for the early Management of Patients with Acute Ischemic Stroke: 2019 update to the 2018 guidelines for the early Management of Acute Ischemic Stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2019) 50:e344–418. doi: 10.1161/STR.0000000000000211
4. Tao, C , Nogueira, RG , Zhu, Y , Sun, J , Han, H , Yuan, G, et al. ATTENTION investigators. Trial of endovascular treatment of acute basilar-artery occlusion. N Engl J Med. (2022) 387:1361–72. doi: 10.1056/NEJMoa2206317
5. Jovin, TG , Li, C , Wu, L , Wu, C , Chen, J , Jiang, C, et al. Trial of Thrombectomy 6 to 24 hours after stroke due to basilar-artery occlusion. N Engl J Med. (2022) 387:1373–84. doi: 10.1056/NEJMoa2207576
6. Pop, R , Finitsis, SN , Arquizan, C , Elhorany, M , Naggara, O , Darcourt, J, et al. Poor clinical outcome despite successful basilar occlusion recanalization in the early time window: incidence and predictors. J Neurointerv Surg. (2023) 15:415–21. doi: 10.1136/neurintsurg-2022-018769
7. Meinel, TR , Kaesmacher, J , Chaloulos-Iakovidis, P , Panos, L , Mordasini, P , Mosimann, PJ, et al. Mechanical thrombectomy for basilar artery occlusion: efficacy, outcomes, and futile recanalization in comparison with the anterior circulation. J Neurointerv Surg. (2019) 11:1174–80. doi: 10.1136/neurintsurg-2018-014516
8. Yang, J , Jin, Z , Song, J , Guo, C , Xie, D , Yue, C, et al. Futile recanalization after endovascular treatment in patients with acute basilar artery occlusion. Neurosurgery. (2023) 92:1006–12. doi: 10.1227/neu.0000000000002313
9. Hu, J , Liu, X , Liu, S , Sang, H , Huang, J , Luo, W, et al. Outcomes of endovascular therapy in young patients with acute basilar artery occlusion: a substudy of BASILAR registry study. Neurol Ther. (2022) 11:1519–32. doi: 10.1007/s40120-022-00372-6
10. Zhou, T , Yi, T , Li, T , Zhu, L , Li, Y , Li, Z, et al. Predictors of futile recanalization in patients undergoing endovascular treatment in the DIRECT-MT trial. J Neurointerv Surg. (2022) 14:752–5. doi: 10.1136/neurintsurg-2021-017765
11. Zaidat, OO , Liebeskind, DS , Jadhav, AP , Ortega-Gutierrez, S , Nguyen, TN , Haussen, DC, et al. Impact of age and Alberta stroke program early computed tomography score 0 to 5 on mechanical Thrombectomy outcomes: analysis from the STRATIS registry. Stroke. (2021) 52:2220–8. doi: 10.1161/STROKEAHA.120.032430
12. Zeiher, AM , Drexler, H , Saurbier, B , and Just, H . Endothelium-mediated coronary blood flow modulation in humans. Effects of age, atherosclerosis, hypercholesterolemia, and hypertension. J Clin Invest. (1993) 92:652–62. doi: 10.1172/JCI116634
13. Yi, T , Zhang, Y , Chen, WH , Wu, YM , Lin, DL , Lin, XH, et al. Impact of leukoaraiosis in patients with acute ischemic stroke treated with thrombectomy: a post hoc analysis of the DIRECT-MT trial. J Neurointerv Surg. (2023) 15:139–45. doi: 10.1136/neurintsurg-2021-018293
14. Bradley, SA , Smokovski, I , and Bhaskar, SMM . Impact of diabetes on clinical and safety outcomes in acute ischemic stroke patients receiving reperfusion therapy: a meta-analysis. Adv Clin Exp Med. (2022) 31:583–96. doi: 10.17219/acem/146273
15. Maida, CD , Daidone, M , Pacinella, G , Norrito, RL , Pinto, A , and Tuttolomondo, A . Diabetes and ischemic stroke: an old and new relationship an overview of the close interaction between these diseases. Int J Mol Sci. (2022) 23:2397. doi: 10.3390/ijms23042397
16. Hao, Z , Yang, C , Xiang, L , Wu, B , and Liu, M . Risk factors for intracranial hemorrhage after mechanical thrombectomy: a systematic review and meta-analysis. Expert Rev Neurother. (2019) 19:927–35. doi: 10.1080/14737175.2019.1632191
17. Zhang, ZG , Zhang, L , Jiang, Q , Zhang, R , Davies, K , Powers, C, et al. VEGF enhances angiogenesis and promotes blood-brain barrier leakage in the ischemic brain. J Clin Invest. (2000) 106:829–38. doi: 10.1172/JCI9369
18. Lecouffe, NE , Kappelhof, M , Treurniet, KM , Lingsma, HF , Zhang, G , Van Den Wijngaard, IR, et al. 2B, 2C, or 3: what should be the angiographic target for endovascular treatment in ischemic stroke? Stroke. (2020) 51:1790–6. doi: 10.1161/STROKEAHA.119.028891
19. Zaidat, OO , Castonguay, AC , Linfante, I , Gupta, R , Martin, CO , Holloway, WE, et al. First pass effect: a new measure for stroke thrombectomy devices. Stroke. (2018) 49:660–6. doi: 10.1161/STROKEAHA.117.020315
20. Tonetti, DA , Desai, SM , Perez, J , Casillo, S , Gross, BA , and Jadhav, AP . Predictors of first pass effect and effect on outcomes in mechanical thrombectomy for basilar artery occlusion. J Clin Neurosci. (2022) 102:49–53. doi: 10.1016/j.jocn.2022.06.005
21. Farouki, Y , Bonnet, T , Mine, B , Hulscher, F , Wang, M , Elens, S, et al. First-pass effect predicts clinical outcome and infarct growth after Thrombectomy for distal medium vessel occlusions. Neurosurgery. (2022) 91:913–9. doi: 10.1227/neu.0000000000002129
Keywords: basilar artery occlusion, endovascular treatment, futile recanalization, prognosis, diabetes mellitus
Citation: Yi T, Li K, Lin X-h, Lin D-l, Wu Y-M, Pan Z-n, Zheng X-f, Chen R-c, Zeng G and Chen W-h (2023) Predictors of futile recanalization in basilar artery occlusion patients undergoing endovascular treatment: a post hoc analysis of the ATTENTION trial. Front. Neurol. 14:1308036. doi: 10.3389/fneur.2023.1308036
Edited by:
Nico Sollmann, University of California, San Francisco, United StatesReviewed by:
Thanh N. Nguyen, Boston University, United StatesHongfei Sang, Xinqiao Hospital, China
Copyright © 2023 Yi, Li, Lin, Lin, Wu, Pan, Zheng, Chen, Zeng and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wen-huo Chen, doctorwwenhuo@126.com
†These authors have contributed equally to this work
 Tingyu Yi
Tingyu Yi