- 1Department of Neurology and Interventional Neuroradiology, Hartford Hospital, Hartford, CT, United States
- 2Department of Neurology, NYU Langone Medical Center, New York, NY, United States
- 3Department of Neurology, University of Connecticut, Farmington, CT, United States
- 4Department of Neurosurgery, Radiology and Neurology, University of Minnesota, Minneapolis, MN, United States
Background and Purpose: Aneurysmal subarachnoid hemorrhage (SAH) is associated with high mortality. Prophylactic treatment of the unruptured intracranial aneurysm (UIA) is considered in a select group of patients thought to be at high for aneurysmal rupture. Hospital readmission rates can serve as a surrogate marker for the safety and cost-effectiveness of treatment options for UIAs; we present an analysis of the 30-day rehospitalization rates and predictors of readmission following UIA treatment with surgical and endovascular approaches.
Methods: We retrospectively analyzed data from the National Readmission Database (NRD) derived from the Healthcare Cost and Utilization Project for the year 2014. The cohort included patients with a primary discharge diagnosis of a treated unruptured aneurysm. The primary outcome variable was the 30-day readmission rate in open surgical vs. endovascularly treated groups. The secondary outcomes included predictors of readmissions, and causes of 30-day readmissions in these two groups.
Results: The 30-day readmission rate for the surgical group was 8.37% compared to 4.87% for the endovascular group. The index hospitalization duration was longer in the surgical group. A larger proportion of the patients readmitted following surgical treatment were hypertensive (76.35, vs. 63.43%), but the prevalence of other medical comorbidities was comparable in the two treatment groups.
Conclusions: There is a higher likelihood for 30-day readmission, longer duration of initial hospitalization and a lower likelihood of discharge home following surgical treatment of UIAs when compared to endovascular treatment. These findings, however, do not demonstrate long-term superiority of one specific treatment modality.
Introduction
The prevalence of intracranial aneurysms (IAs) in the general population is estimated to be 3.6–6.0% (1). However, the incidence of SAH from the rupture of IAs is much lower at 5–20 per 100,000 (2). The mortality rate following aneurysmal SAH approaches 25–50%, with most deaths resulting from the initial hemorrhage or its immediate complications (3). Therefore, prophylactic treatment of unruptured intracranial aneurysms (UIA) is considered for selected patients considered to be at high risk for aneurysm rupture. It is important that these prophylactic treatment modalities are safe and cost-effective.
In this context, hospital readmission rates can serve as one surrogate for the safety and cost-effectiveness of preventive treatment options for UIAs. Treatment options for UIAs can be broadly categorized as endovascular (coil embolization, stent-assisted coiling, balloon-assisted coiling, flow diversion, and liquid embolics) and surgical (clipping, vessel sacrifice with or without bypass, wrapping and taping) options. Herein, we have analyzed the 30-day readmission rates and the predictors for readmission following UIA treatment with either modality.
Materials and Methods
This retrospective study analyzed data from the National Readmission Database (NRD) derived from the Healthcare Cost and Utilization Project (HCUP) for the year 2014- this year was chosen with the consideration that the NRD database starts from 2013, and 2015 onward it contains ICD-10 codes, which we thought could have more coding variations given its more recent implementation. Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants was not required to participate in this study in accordance with the national legislation and the institutional requirements. The index admissions were identified by using International Classification of Diseases, Ninth Revision, and Clinical Modification (ICD-9 CM) code for unruptured aneurysm 437.3; treated with coiling 39.75, 39.76; stenting 00.65, 39.90; or surgical clipping 39.51. The treatments were subdivided into endovascular (consisting of coil embolization, stent-assisted coil embolization, and stent-placement only sub-groups) and open surgical groups.
We used the “NRD visit link (NVL)” to identify index visits and to track readmissions following the index admissions. For our purposes, “readmission” was defined as admission to particular state hospitals for any cause within 30 days of discharge following the index hospitalization. We used the sampling weights provided in the NRD database to generate the national readmission rate. Sampling discharge weights for national appraisals are produced utilizing the objective collection of community hospitals (excluding rehabilitation and long-term acute care hospitals) in the United States.
The study cohort consisted of patients admitted between January 1, 2014, and November 30, 2014, with a primary discharge diagnosis of a treated unruptured aneurysm. The patients admitted during the month of December were excluded as 30-day follow-up data to identify readmissions for these index admissions were not available in the 2014 NRD dataset. Additionally, cases with a missing or zero length of stay (LOS), and age <18 years were excluded. NRD is de-identified publicly available data exempt from institutional review boards. All the authors analyzing the database signed the HCUP data use agreement.
The following data were collected from the NRD (4): patient demographics; hospital characteristics such as bed size and teaching status; socioeconomic factors including median household income category for patient's zip code and primary payer; comorbidities, LOS, admission day, and discharge disposition. The co-morbidities were identified by ICD 9 diagnostic codes listed in secondary diagnoses fields during the index admission. The modified Charlson-Deyo Comorbidity Index (CCI) is an established measure to quantify the burden of comorbid conditions; the scores range from 0 to 33 with a higher score indicating a greater burden of concomitant diseases (5).
The primary outcome variable chosen for the study was comparison of the 30-day readmission rate (DRR) in open surgical vs. endovascularly treated groups. The secondary outcomes included predictors of readmissions, and causes of 30-DRR in these two groups. We used SAS 9.4 (SAS Institute Inc, Cary, North Carolina) for data analysis. Categorical variables and continuous variables were assessed by the Rao Scott Chi-square test and the Student's t-test, respectively. The predictors of readmissions were identified using multivariable logistic regression after adjusting for the stratified cluster design of NRD and co-variables including patient demographics, hospital-specific factors, socioeconomic variables, discharge disposition, and the most prevalent comorbidities to identify factors associated with readmission. The power of the model and association of predicted probabilities are determined by “concordance” statistic C which is significantly higher (>0.7) for multivariate analysis. The variables with missing or invalid values were excluded from the final analysis.
Results
The baseline characteristics of the two comparison groups with respect to patient demograph1ics, medical comorbidities, median household income, insurance, hospital type and discharge disposition are depicted in Table 1.
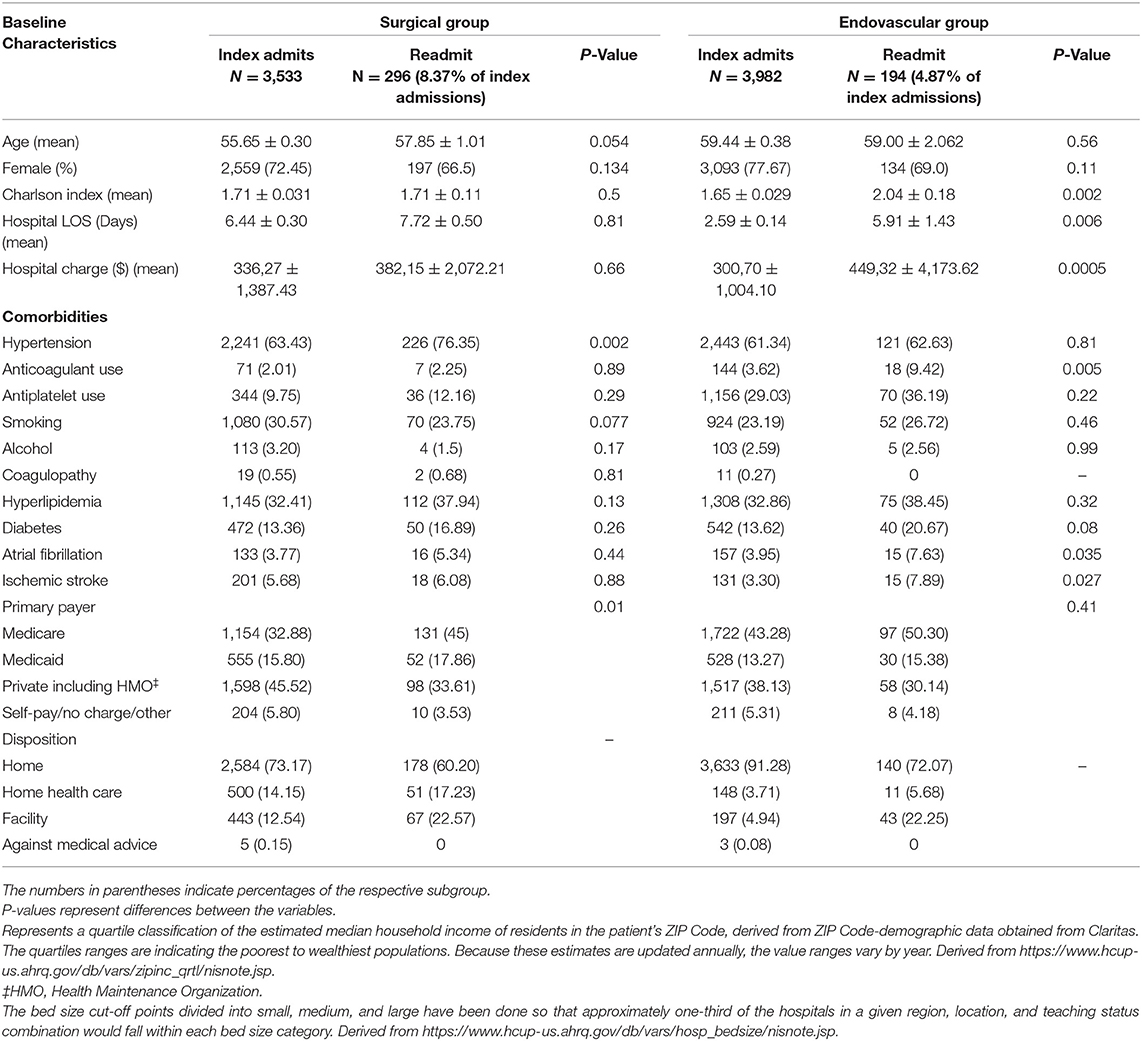
Table 1. Baseline characteristics of study patients with UIAs who underwent surgical or endovascular intervention.
The 30-day readmission rate for the surgical group was 8.37% (296 of 3,533) compared to 4.87% (194 of 3,982) for the endovascular group. The index hospitalization duration was longer in the surgical group when compared to the endovascular group (6.44 ± 0.30 days vs. 2.59 ± 0.14). A larger proportion of the patients readmitted following surgical treatment were hypertensive (76.35, vs. 63.43% of index surgical admissions), but the prevalence of other medical comorbidities was comparable in the two treatment groups. Over 90% of the endovascularly treated patients were discharged home following index admission, vs. just under three-fourths in the surgical group (Chi-square statistic 429.0,536, p < 0.00001).
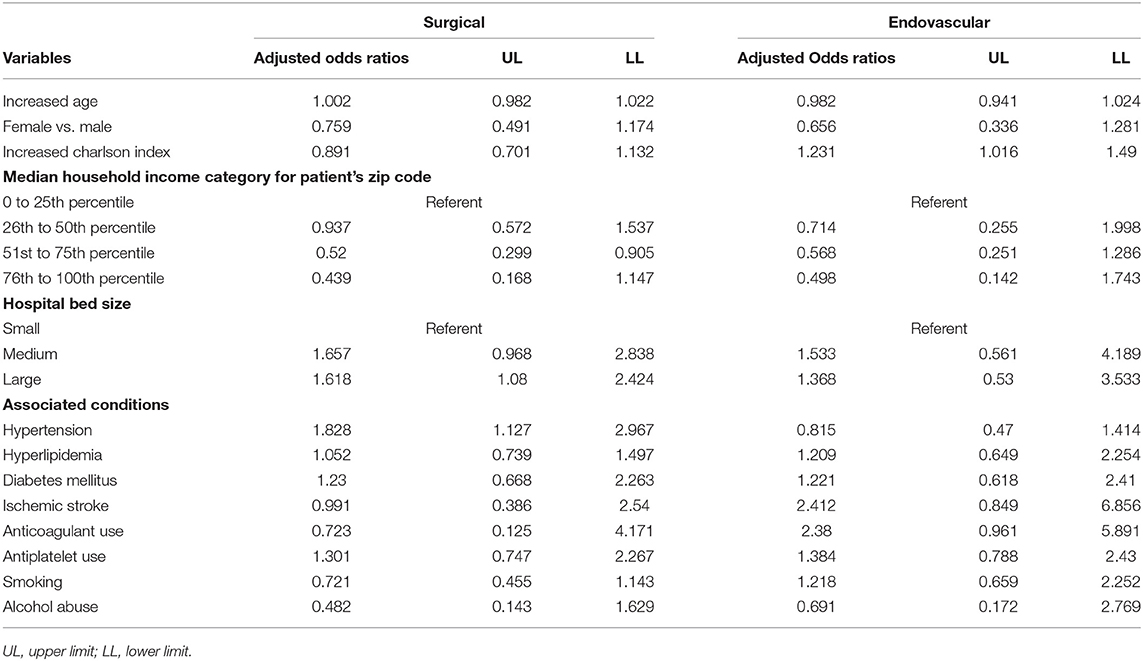
Table 2 shows logistic regression models for outcomes of readmission in separate surgical and endovascular populations.
Figure 1 shows the timing of readmission following discharge from index hospitalization for both surgical and endovascular groups.
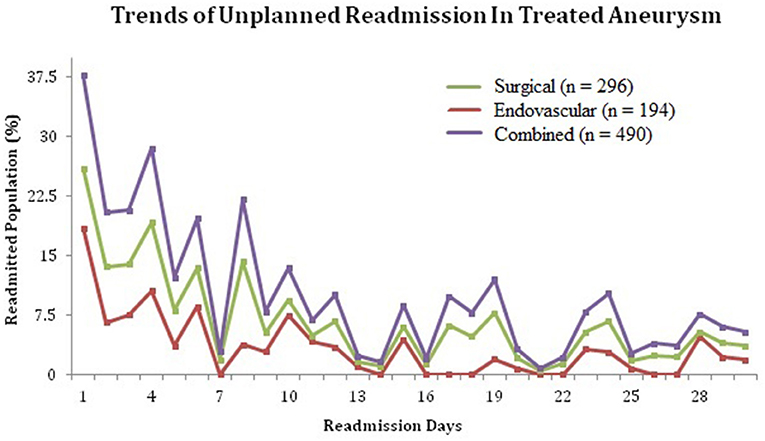
Figure 1. Trends of unplanned readmissions in patients treated for unruptured intracranial aneurysms.
Patients readmitted following surgical treatment had a significantly higher prevalence of hypertension [Odds Ratio 1.828 (95% CI 1.127–2.967, p = 0.149)] although this was not the case for other medical comorbidities. The CCI, a predictor of 10-year survival in patients with multiple medical comorbidities, was significantly higher in patients readmitted following endovascular therapy [Odds Ratio 1.231 (95% CI 1.016–1.49, p = 0.0338)] vs. those who were not.
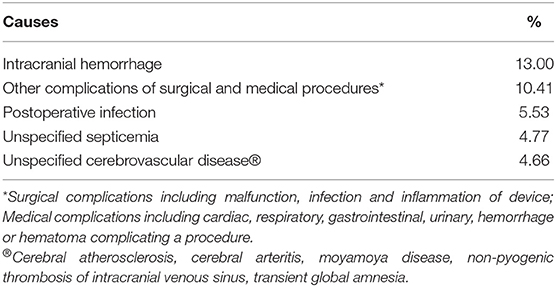
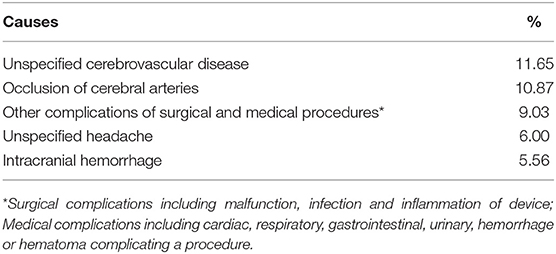
Table 3 shows the combined Odds Ratios for readmission based on various patient characteristics while Tables 4A,B show the common readmission diagnoses in the two groups. As indicated in Table 3, the Odds Ratio for readmission following surgical treatment of UIAs was 1.89 times that of endovascular treatment. For both Surgical and Endovascular groups, ischemic and/or hemorrhagic complications of UIA treatment were the most common causes of readmission.
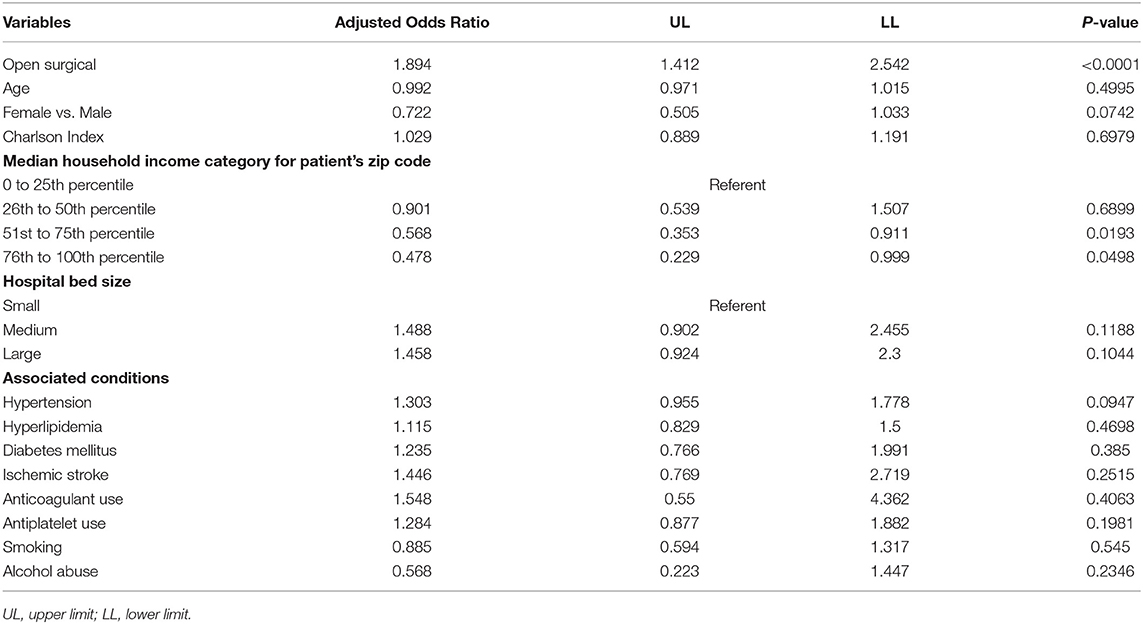
Table 3. All patients (surgical and endovascular) readmission model and potential contributory factors.
Discussion
Treatment paradigms for UIAs have shifted over the past two decades with a majority of patients now being treated with endovascular techniques. Currently, multiple patient and aneurysm characteristics are taken into consideration, first when choosing patients with UIAs for treatment, and subsequently for determining the best treatment approach, whether endovascular or open surgical. For the first step, various scoring systems including the PHASES score (6), have been employed to identify at-risk UIAs. However, for the next step, there is no widely adopted process for patient selection for a specific treatment.
A standardized process for determining the modality of treatment for UIAs could be very useful since both clipping and coiling can be associated with serious periprocedural complications, including arterial dissection, infarction, intracranial hemorrhage and seizures. Comprehensive knowledge of the outcomes with each type of procedure will be helpful in the development of such standardized criteria for patient selection. The outcomes of UIA clipping and coiling have been studied before with respect to aneurysm location (7), periprocedural complications (8–10), short- and long-term morbidity and mortality (11–13), expenditure (14), patient age (15), and aneurysm recurrence (16). In our study, we have focused on the readmission rates following UIA treatments with endovascular or open surgical techniques. These readmission rates can serve as a metric for the relative safety, cost and efficacy of these procedures.
Our study shows that the 30-day readmission rate following treatment of UIAs is higher with open surgical treatment than with endovascular treatment. It also shows that there is an increase in the likelihood of readmission for patients undergoing surgical treatment when there is an accompanying history of hypertension. Additionally, our study shows that the patients in the surgical group had a longer average duration of index hospitalization, and a lower likelihood for discharge to home, compared to the endovascular group. In part, at least, these findings may reflect the higher post-procedure complication rates associated with surgical clipping, which have been reported previously. We also found that there is an increased incidence of readmission due to intracranial hemorrhage after surgical treatment of UIAs. This finding could reflect the observation of development of chronic extra-axial hematomas/hygromas following clipping for UIAs, with higher rates in elderly patients (17–19). While intracranial hemorrhage was one of the top causes for readmission in both groups, certain other conditions were more specific to the type of intervention, as detailed in Tables 4A,B. Infections were a major reason for readmission in the open surgical group, while ischemic stroke seemed to be responsible for a sizeable number of readmissions in the endovascular group. These findings may reflect the complications specific to either procedure and post-procedure duration of hospitalization among other factors.
With regards to cost-effectiveness, the increased readmission rates, as well as the higher rates of initial discharge to nursing facilities shown here, are likely responsible for the increased costs associated with clipping in the initial 30-day postoperative period. Similar findings have recently been reported in a large meta-analysis comparing cost-effectiveness of the two treatment modalities (20). However, this finding of increased initial costs with surgical clipping must be interpreted with caution, given the much lower rates for aneurysm recurrences and retreatments associated with surgical clipping for UIAs, when compared to endovascular treatments. On the lines of another recently published study (21), we found lower initial complication rates with endovascular treatments, but this may also be offset by the additional morbidity and mortality risks from re-treatment procedures. In this context, the impact of potentially longer-lasting endovascular treatments such as flow diversion on long term cost reduction also needs to be studied.
Our findings must be viewed in the context of the limitations associated with the methodology of this study. The NRD does not track out of state readmissions. Similarly, NRD does not provide specific information regarding additional factors that can potentially affect the readmission rates such as aneurysm characteristics and procedural details. Additionally, the ICD-9-CM codes used in our study may have been affected by coding practices and errors. The retrospective design, implemented here using a large database not designed explicitly for this study, can only show associations. The cause of readmission is not always attributed to the procedure which is difficult to confirm in the NRD database. Different proportions of patients with UIAs with index surgical or endovascular treatment subsequently require repeat hospitalization for intervention, and this treatment complication could not be assessed using the NRD. Finally, the results could be subject to random variations as only the data from the year 2014 were included. Despite these limitations, our study included a large number of patients from a national database and is broadly representative of national estimates and predictors of 30-RR in treated UIA population.
Summary
In the studied population, patients undergoing endovascular treatment for UIA were less likely to be readmitted within the first 30 days following treatment, and were more likely to be discharged home compared to patients undergoing open surgery. It also shows that a history of hypertension in the open surgical group appears to increase the likelihood of readmission for patients. These findings, however do not demonstrate the long term superiority of one specific treatment modality over the other. Optimal perioperative management of medical and surgical complications and careful patient selection for either intervention may help prevent avoidable readmissions following UIA treatment.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants to participate in this study was not required in accordance with the national legislation and the institutional requirements.
Author Contributions
TM, RT, and BJ were involved in the conceptualization of the study. ND, SM, AK, and AG participated in manuscript writing. TM, SM, AK, and AG were involved in collection of data. TM and SP performed the statistical analysis. TM, ND, RT, and BJ reviewed and critiqued the manuscript before presenting it in its final form. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
2. de Rooij N, Linn F, van der Plas J, Algra A, Rinkel G. Incidence of subarachnoid haemorrhage: a systematic review with emphasis on region, age, gender and time trends. J Neurol Neurosurg Psychiatry. (2007). 78:1365–72. doi: 10.1136/jnnp.2007.117655
3. Hop J, Rinkel G, Algra A, van Gijn J. Case-fatality rates and functional outcome after subarachnoid hemorrhage: a systematic review. Stroke. (1997) 28:660–4. doi: 10.1161/01.STR.28.3.660
4. NRD Database Documentation. Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research Quality (2018).
5. Roffman C, Buchanan J, Allison G. Charlson comorbidities Index. J Physiother. (2016) 62:171. doi: 10.1016/j.jphys.2016.05.008
6. Backes D, Vergouwen MD, Tiel Groenestege AT, Bor AS, Velthuis BK, Greving JP, et al. PHASES score for prediction of intracranial aneurysm growth. Stroke. (2015) 46:1221–6.
7. Regli L, Dehdashti AR, Uske A, de Tribolet N. Endovascular coiling compared with surgical clipping for the treatment of unruptured middle cerebral artery aneurysms: an update. Acta Neurochir Suppl. (2002) 41–6. doi: 10.1007/978-3-7091-6736-6_8
8. Johnston SC, Wilson CB, Halbach VV, Higashida RT, Dowd CF, McDermott MW, et al. Endovascular and surgical treatment of unruptured cerebral aneurysms: comparison of risks. Ann Neurol. (2000) 11–9. doi: 10.1002/1531-824948:1<11::AID–ANA4>3.0.CO;2-V
9. Alshekhlee A, Mehta S, Edgell RC, Vora N, Feen E, Mohammadi A, et al. Hospital mortality and complications of electively clipped or coiled unruptured intracranial aneurysm. Stroke. (2010) 41:1471–6.
10. Ruan C, Long H, Sun H, He M, Yang K, Zhang H, et al. Endovascular coiling vs. surgical clipping for unruptured intracranial aneurysm: a meta-analysis. Br J Neurosurg. (2015) 29:485–92. doi: 10.3109/02688697.2015.1023771
11. Higashida R, Lahue B, Torbey M, Hopkins L, Leip E, Hanley D. Treatment of unruptured intracranial aneurysms: a nationwide assessment of effectiveness. Am J Neuroradiol. (2007) 28:146–51.
12. Brinjikji W, Rabinstein AA, Lanzino G, Kallmes DF, Cloft HJ. Effect of age on outcomes of treatment of unruptured cerebral aneurysms: a study of the National Inpatient Sample 2001-2008. Stroke. (2011) 42:1320–4.
13. Darsaut TE, Findlay JM, Magro E, Kotowski M, Roy D, Weill A, et al. Surgical clipping or endovascular coiling for unruptured intracranial aneurysms: a pragmatic randomised trial. J Neurol Neurosurg Psychiatry. (2017) 88:663–8. doi: 10.1136/jnnp-2016-315433
14. Hoh BL, Chi YY, Lawson MF, Mocco J, Barker FG II. Length of stay and total hospital charges of clipping versus coiling for ruptured and unruptured adult cerebral aneurysms in the Nationwide Inpatient Sample database 2002 to 2006. Stroke. (2010). 41:337–42. doi: 10.1161/STROKEAHA.109.569269
15. Lawson MF, Neal DW, Mocco J, Hoh BL. Rationale for treating unruptured intracranial aneurysms: actuarial analysis of natural history risk versus treatment risk for coiling or clipping based on 14,050 patients in the Nationwide Inpatient Sample database. World Neurosurg. Mar-Apr. (2013) 79:472–8. doi: 10.1016/j.wneu.2012.01.038
16. Bernat AL, Clarençon F, André A, Nouet A, Clémenceau S, Sourour NA, et al. Risk factors for angiographic recurrence after treatment of unruptured intracranial aneurysms: Outcomes from a series of 178 unruptured aneurysms treated by regular coiling or surgery. J Neuroradiol. (2017) 44:298–307. doi: 10.1016/j.neurad.2017.05.003
17. Inamasu J, Watabe T, Ganaha T, Yamada Y, Nakae S, Ohmi T, et al. Clinical characteristics and risk factors of chronic subdural haematoma associated with clipping of unruptured cerebral aneurysms. J Clin Neurosci. (2013) 20:1095–8. doi: 10.1016/j.jocn.2012.09.024
18. Ohno T, Iihara K, Takahashi JC, Nakajima N, Satow T, Hishikawa T, et al. Incidence and risk factors of chronic subdural hematoma after aneurysmal clipping. World Neurosurg. (2013) 80:534–7. doi: 10.1016/j.wneu.2012.09.025
19. Park J, Cho JH, Goh DH, Kang DH, Shin IH, Hamm IS. Postoperative subdural hygroma and chronic subdural hematoma after unruptured aneurysm surgery: age, sex, and aneurysm location as independent risk factors. J Neurosurg. (2016) 124:310–7. doi: 10.3171/2015.1.JNS14309
20. Zhang X, Tang H, Huang Q, Hong B, Xu Y, Liu J. Total hospital costs and length of stay of endovascular coiling versus neurosurgical clipping for unruptured intracranial aneurysms: systematic review and meta-analysis. World Neurosurg. (2018) 115:393–9. doi: 10.1016/j.wneu.2018.04.028
Keywords: unruptured, intracrainal, aneurysm, endovascular, clipping
Citation: Mehta T, Desai N, Patel S, Male S, Khan A, Grande AW, Tummala RP and Jagadeesan BD (2021) Readmission Trends Related to Unruptured Intracranial Aneurysm Treatment. Front. Neurol. 12:590751. doi: 10.3389/fneur.2021.590751
Received: 02 August 2020; Accepted: 14 April 2021;
Published: 20 May 2021.
Edited by:
Serge Marbacher, Aarau Cantonal Hospital, SwitzerlandReviewed by:
Mouhammad A. Jumaa, University of Toledo, United StatesBasil Erwin Grüter, Aarau Cantonal Hospital, Switzerland
Copyright © 2021 Mehta, Desai, Patel, Male, Khan, Grande, Tummala and Jagadeesan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ninad Desai, ninaddd@gmail.com
 Tapan Mehta
Tapan Mehta