
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 05 March 2025
Sec. Healthcare Professions Education
Volume 12 - 2025 | https://doi.org/10.3389/fmed.2025.1554011
This article is part of the Research Topic Innovations in Teaching and Learning for Health Professions Educators View all 17 articles
Introduction: Faculty development programs in the health professions are essential in addressing the evolving and expanding roles of educators. These programs have become a cornerstone of organizational development and contribute significantly to improving student learning. However, the motivation of faculty to engage in such programs is often challenged by the significant demands of their clinical responsibilities and already busy schedules. This study aims to explore the motivation of teaching health professionals to voluntarily participate in the Digital Health Professions Education (d-HPE) program, a 200-h certification program at the Charité - Universitätsmedizin Berlin to train digital teaching skills and competencies.
Methods: In this qualitative study, we analyzed the motivation letters from faculty members who volunteered to participate in the d-HPE program. We used coding based on Self-Determination Theory (SDT) as a framework for analysis with three main themes: autonomy, competence and relatedness. Within autonomy, the sub-themes were intrinsic motivation and self-directed choices. Competence included the sub-themes of mastery of teaching practices and digital skill development. Relatedness included the sub-themes of interprofessional collaboration and mentorship.
Results: A total of 21 motivational letters were analyzed from two d-HPE cohorts, representing diverse health professional backgrounds and career stages. Analysis of the autonomy theme revealed an intrinsic motivation shaped by early teaching experiences and a self-directed decision to pursue advanced qualifications. The competence theme reflected the need to master evidence-based teaching practices and to develop advanced digital skills, with the COVID-19 pandemic as a driving factor. The relatedness theme demonstrated the importance of inter-professional collaboration and mentorship in promoting educational innovation across disciplines and institutions.
Discussion: The motivation of health professions educators to participate in faculty development programs goes beyond the traditional 'carrots and sticks' of external rewards or punishments constellation; it is rooted in their intrinsic motivation to improve teaching qualifications and fulfill their role in digital education. Despite the demands of a busy clinical and professional work schedule, active engagement in intensive faculty development programs is aligned with the need for interprofessional networking and the evolving demands of digital education.
The rapidly changing landscape of health professions education creates significant challenges for both students and educators, particularly with the increasing integration of digital technologies into education, research, and patient care (1–3). As these changes usually bring both opportunities and challenges, digital education has emerged as a key strategy to equip health professionals with the skills needed to navigate this transformation. Its growing adoption spans all levels of health professions education, from pre- and post-graduate university programs, as well as faculty development, lifelong learning and continuous professional development (2). Faculty participation in development programs to improve digital competencies often depends on intrinsic and extrinsic motivational factors, including the perceived relevance of training to their teaching practice, the opportunity for personal and professional growth, and institutional support (4). However, traditional management approaches commonly rely on the “carrots and sticks model of rewards and punishment that may fail to address the deeper motivational needs, potentially limiting faculty engagement and the long-term impact of such programs. Understanding these motivational factors may be essential for designing effective faculty development programs that promote long-term engagement and successful and sustainable implementation of digital teaching competencies. Therefore, this study seeks to move beyond the “carrots and sticks” framework by exploring intrinsic motivational factors, as outlined by self-determination theory, to better understand what motivates faculty to join and remain engaged in a digital health professions educator program.
Digital education is broad and evolving in nature and is used as an umbrella term for different educational approaches, methods and technologies and is defined as “teaching and learning using digital technologies, ranging from the simple conversion of content into a digital format (e.g., a book into a PDF or HTML format) to the complex use of digital technologies (e.g., mobile education, serious games, virtual patients and virtual reality)” (2). The benefits of digital education generally include flexible and widespread access to content, personalized learning experiences, increased engagement with content and deeper information processing. However, it is also likely to present challenges such as the digital divide (requiring IT infrastructure and digital literacy), higher development and deployment costs, and potential negative emotional effects such as anxiety and feelings of isolation among students and teachers (2).
Following the COVID-19 pandemic, which led to a rapid transition to digital teaching and learning in many educational institutions, there has been an increasing need for faculty development specifically aiming at preparing and supporting health professions educators to deliver effective digital instruction and assessment, maintain student engagement, and foster interprofessional collaboration in a virtual environment (5). Digitally competent faculty are generally better equipped to design and implement educational strategies that meet diverse needs of learners and to navigate the complexities of digital health education (6). As a result, faculty development programs that focus specifically on digital education have received increasing attention for their ability to address the specific learning needs of educators and equip them with skills to teach in a rapidly digitizing environment (4). However, given time pressures associated with clinical practice and service, understanding factors which motivate faculty to voluntarily engage in such faculty development programs is crucial for effective design and implementation in the future (3).
Teaching competencies in health professions education are evolving and expanding to encompass various roles, including the teacher as facilitator and mentor, curriculum developer and implementer, assessor and diagnostician, role model, manager and leader, scholar and researcher, and professional (7, 8). In addition, with recent advances in digital technology, there has been a growing emphasis on digital competence, defined as “the set of knowledge, skills, attitudes, abilities, strategies, and awareness required to use information and communication technology (ICT) and digital media” (9, 10). It includes self-rated competencies (e.g., digital literacy and eHealth literacy), psychological and emotional aspects of using digital technologies (e.g., attitudes and beliefs, confidence and awareness), use of digital technologies (e.g., for general and specific functions) and knowledge of digital technologies (11).
Digital competence is often interchangeably referred to as pedagogical digital competence (PDC), which refers to the ability to consistently apply knowledge, skills, attitudes, approaches to technology and learning theory to plan, deliver, evaluate and continually revise digital education (4). Several digital competency frameworks have been developed for health professions educators to inform the development of faculty training programs in this area (12). However, the digital competencies and support needed by educators vary widely, depending on factors such as pre-existing skills, local conditions and individual needs, which differ from region to region (13).
Despite a widespread need to support these teaching and digital competencies, specialized training programs remain scarce, highlighting a necessity to integrate these skills into faculty development programs to reach health professionals, especially those with heavy workloads and leadership roles (3, 6, 14). Evidence from the literature shows that digital education faculty development interventions have been designed and delivered to a diverse range of healthcare professionals, in a variety of settings, and with a range of different outcome measures (2, 4). The most common approaches used were formal workshops, group work, case studies, discussions and practical exercises or simulations, but relatively little attention was paid to informal and individualized approaches (e.g., peer coaching and collegial support) (8, 15). Evidence from the literature recommends the integration of multi-method strategies in authentic contexts such as experiential learning, role modeling, reflection, and applying evidence to teaching practice to improve digital competencies of teaching health professionals (8, 16, 17). It is also recommended to provide extended longitudinal programs, which could have the advantage of fostering a community of practice, aligning with institutional priorities, promoting educational leadership, and increasing scholarly productivity (8, 18, 19).
To further enhance the effectiveness of faculty development programs, it is essential to consider how learning processes align with key dimensions: cognitive (what to learn), affective or motivational (why to learn), and metacognitive regulation (how to learn) (20). Among these dimensions, motivation plays a critical role in faculty engagement hence focusing on stimulating faculty motivation can have a significant impact on the outcomes of faculty development (FD) programs. Several motivational theories have evolved over time, such as Murray's Need to Achieve Theory (1938), which suggests that motivation is a dynamic construct shaped by time and context rather than a fixed trait (21), Hull's Drive Theory (1943), which suggests that human behavior is driven by needs that must be met to maintain a steady state (22), and Maslow's Hierarchy of Needs (1943), which proposes that human motivation is organized in a hierarchy (23). Other motivational theories include Atkinson's Expectancy-Value Theory (1966), which argues that motivation is influenced by an individual's desire to succeed or avoid failure (24), and Bandura's Social Cognitive Theory (1977), which emphasizes the role of self-efficacy in motivation (25). The Self-Determination Theory (SDT), developed by Edward Deci and Richard Ryan, is one of the current major motivational theories in many fields, including education and health care, and its applications in medical education are gaining increasing interest (26). It was selected for this study because it is particularly well suited to exploring faculty motivation to voluntarily engage in development programs, such as the program that is subject of this study where participation is not externally mandated but driven by personal and professional factors. Given the voluntary nature of the program and the challenges posed by faculty's clinical responsibilities, SDT would allow for a nuanced understanding of internal drivers that influence their decision to participate in an intensive and time-consuming program. This theoretical framework enables the exploration of how intrinsic motivation, rather than external rewards or obligations, plays a key role in faculty engagement, making SDT an appropriate choice for examining the factors influencing participation in faculty development (27, 28).
In Germany, the digitalisation of healthcare has been established by law with the “Digital Healthcare Act” from 2020, and there is a growing need for further training in digital education (13). However, only a few German medical schools have integrated digital health skills into their curricula, often as an elective course that reaches a small number of students (29). There is a growing need to train faculty in digital skills in order to make future courses more accessible to a wider range of students (29). Existing research has predominantly focused on either assessing the digital competencies of health professions educators (11, 30–33) or evaluating the outcomes of faculty development programs designed to enhance digital competencies (15, 34, 35). These evaluations typically assess program effectiveness in terms of teaching effectiveness and successful integration of digital tools into teaching practice. However, there is a gap in the literature regarding the motivations that drive faculty to participate in these programs (36). Addressing this gap seems important for several reasons. First, as motivation directly influences the level of commitment of healthcare educators to their professional development, it is important to design and implement programmes that not only meet institutional goals but also resonate with the personal and professional aspirations of educators. This approach ensures greater commitment and sustained success by investing time and effort in learning new skills, experimenting with innovative teaching methods and overcoming technological challenges (37). A second reason is that faculty development programs require significant institutional investment in terms of resources, time and funding, so it is important for institutions to understand what motivates faculty to participate and remain engaged in these programs (38). Third, motivation research has shown that adult learners, such as educators, have distinct needs to see clear value and relevance to their practice, to have autonomy in their learning, and to feel competent in new skills (39, 40). Finally, sustaining behavioral change in teaching practices, particularly in the context of digital health education, requires more than initial skill development; it requires ongoing motivation to implement and refine new approaches (41, 42). Thus, understanding motivational factors is critical for designing faculty development programs that support the long-term integration of digital competencies into teaching practices.
The purpose of this study is to explore the motivations of teaching health professional at Charité - Universitätsmedizin Berlin (Charité) to voluntarily enroll in the Digital Health Professions Educator (d-HPE) program, a 200-h interprofessional faculty development program. This research focuses on understanding why educators choose to voluntarily participate in such an intensive program, despite their demanding professional responsibilities.
This study is underpinned by a constructivist epistemology which assumes that knowledge is created through social interaction and that motivation is a complex, contextual phenomenon shaped by personal beliefs, prior experiences and social interactions (43). In line with this paradigm, we adopted an exploratory qualitative research approach to understand the perspectives and motivations of health professions educators applying for the d-HPE program, designed for faculty interested in obtaining a formal qualification in digital education. A qualitative approach also allows for in-depth exploration of nuanced and multifaceted motivational aspects and is increasingly used in the context of motivational theories (44).
The study was conducted from May 2023 to July 2024 at the Charité Germany. The sampling frame consisted of educators in the health professions applying for the d-HPE program, a blended learning interprofessional faculty development program delivered over 1 year.
The d-HPE program was developed and implemented as a comprehensive faculty development initiative aimed at equipping healthcare educators from diverse professional backgrounds and career stages at the Charité with digital competencies needed to teach, assess, and mentor in digital education contexts. The program is structured into three progressive modules, comprising a total of 200 teaching units (45 min each), designed to build participants' basic knowledge and skills in addition to advanced application (Figure 1).
Module I (60 teaching units) focuses on the fundamental principles of digital health education, including topics such as constructive alignment, teaching and learning methods, instructional design, and the use of blended learning and online teaching tools. Participants are also introduced to media production techniques where they learn to create digital teaching materials such as screencasts and videos. This module emphasizes reflective practice and peer feedback as essential components of professional development. Module II (60 teaching units) provides more advanced training, enabling participants to engage in the practical application of tools and educational strategies specific to online environments, e.g., the development of virtual patient cases, online seminars and exams, with a particular focus on humanizing online learning environments. Module III (80 teaching units) requires participants to undertake a major digital teaching project, synthesizing and applying their knowledge to the design and implementation of a large-scale digital learning initiative. Throughout this module, participants receive individual mentoring and participate in workshops and journal clubs focused on digital health professions education.
The 12-month program offers a flexible, blended learning approach that includes both online self-study and face-to-face workshops. The final module culminates in the presentation and peer review of participants' digital teaching projects. The program has been co-designed by an interprofessional team of experts in medical education, faculty development, e-learning and interprofessional education at the Charité. A collaborative design process ensured that the program is tailored to the needs of a broader interprofessional range of participants from various areas and health professions. Based on adult learning principles, the program emphasizes collaborative inquiry, where participants learn through shared experiences, and reflective practice, which encourages critical self-assessment and continuous professional development (3).
For data collection we used letters of motivation of applicants to the d-HPE program in the two consecutive cohorts of 2023/2024 and 2024/2025. The motivational letters, with an average length of one page, were anonymized and translated into English by the author MS.
A deductive approach to qualitative data analysis was adopted for this study, which begins with an organizing framework derived from existing literature to provide a structured starting point for analysis, making it both structured and flexible and ensuring that the coding process was grounded in the existing literature (45, 46).
In contrast to conventional qualitative content analysis, used for example in grounded theory, where coding categories are derived directly and inductively from raw data, the current study adopted a directed content analysis approach with the aim of extending the conceptual framework or theory, in our case the Self-Determination Theory (46, 47). Analysis was conducted using Atlas.ti qualitative data analysis (QDA) software (a computerized indexing system, Berlin, Germany) (48). The coding framework was constructed around the three main themes of autonomy, competence, and relatedness (49). The main themes, subthemes, and their definitions are summarized in Table 1.
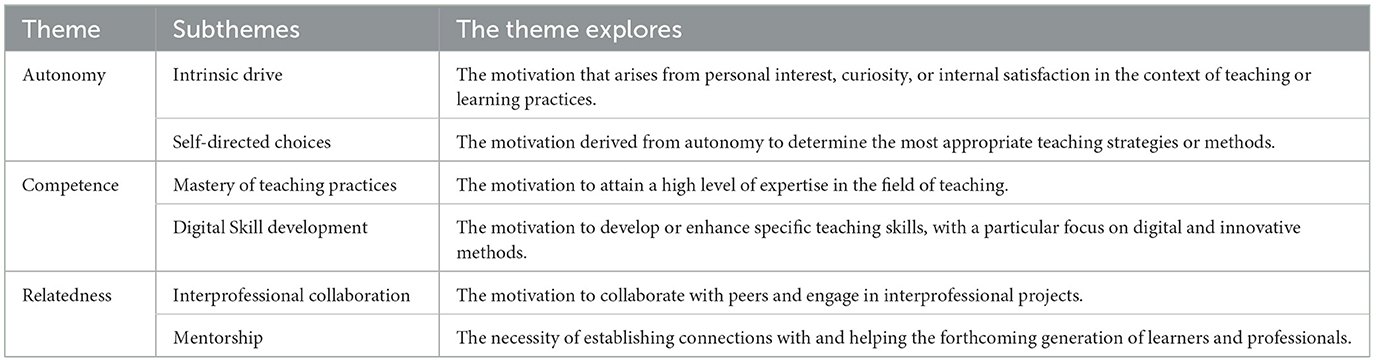
Table 1. Coding framework adapted from Ryan and Deci (49).
In a collaborative, iterative analysis process, author (MS) carried out the initial analysis based on the first cohort of motivation letters. The analysis was revised by authors (ML) and (HP) and a consensus-building process followed: disagreements in the collaborative analysis process were addressed through a structured and iterative approach. Any differences in analysis were resolved through in-depth discussion to ensure agreement on the coding process. Finally, the analysis of the remaining motivation letters was continued in an iterative process by MS, ML, and HP.
This study was conducted in compliance with the data protection regulations at the Charité and was approved by the Ethics Committee of the Charité. Anonymity was ensured; a consent form was signed by the participants, who were informed about the study purpose, the use of data collected, and their right to withdraw at any time without consequences for their success in the program.
The reflexivity was achieved through the maintenance of a research diary, which included notes and comments on the motivation letters as well as interaction between the researchers and the course participants (50). In this case, researchers act as insiders, taking on the role of course development, implementation, and evaluation, as well as being responsible for teaching all participants and providing ongoing support throughout the program. While this role facilitated a deeper understanding of contextual complexities, potential drawbacks emerged, primarily in terms of power dynamics between researchers and participants. Measures were taken to mitigate this, including anonymizing the motivational letters and ensuring that participants' performance was not influenced by their involvement in the study. We also recognize that the researchers' intense involvement in the program may have potentially influenced the data analysis process (51). To address this, we engaged in an iterative process of careful review of the analysis in which initial disagreements were discussed and resolved through collaborative discussions. This approach ensured that consensus was reached and the integrity of the research findings was maintained.
A total of 21 motivation letters were analyzed from two d-HPE program cohorts in academic years 2023/2024 and 2024/2025 including anaesthesiology (n = 3), pediatrics (n = 2), geriatrics (n = 2), internal medicine (n = 2), emergency medicine (n = 2), clinical nursing (n = 1), pediatric Surgery (n = 1), orthodontics (n = 1), radiation oncology (n = 1), nephrology (n = 1), pharmacology (n = 1), IT/scientific computing (n = 1), pathology (n = 1), medical physics (n = 1) and social medicine (n = 1).
Regarding the intrinsic drive, the analysis revealed a strong passion for teaching and an enthusiasm for creative and effective teaching methods, e.g., the inherent interest in digital tools combined with a personal passion for drawing and illustrating to enhance medical presentations for research and teaching (Table 2, quote 1). Intrinsic drive is also associated with an early commitment to teaching, either early in the medical career (Table 2, quote 2) or even during the participants' undergraduate years (Table 2, quotes 3 and 4). These examples illustrate how intrinsic motivation, often rooted in personal interests and early experiences, served as a foundational driver for engagement in an intensive faculty development program.
In addition to intrinsic motivation, participants made self-directed choices to improve their digital teaching skills and to pursue career advancement and leadership in education. A key motivation was the decision to acquire substantial additional qualifications, reflecting a commitment to continuous improvement in teaching methods (Table 2, quote 5). In addition, the program was seen as an essential investment in personal academic growth, with participants recognizing its potential to enrich their teaching while positioning them to lead the development and implementation of innovative teaching strategies (Table 2, quote 6). This highlights a deliberate and forward-thinking approach, with participants choosing the program to align with their long-term goals of becoming leaders in the evolving field of medical education.
In summary, the analysis of the autonomy theme reveals that faculty members' motivation to engage in the d-HPE program stems from both an intrinsic drive, rooted in a passion for teaching and early teaching experiences, and a self-directed decision to strategically pursue advanced qualifications to improve teaching practice and position themselves as leaders in educational innovation.
In terms of mastering teaching practice, participants expressed a need to expand expertise and refine evidence-based teaching methods. For some, this need stemmed from an early transition from learner to teacher, which highlighted a need to better understand teaching practices and pursue structured educational training in didactics in order to gain confidence and competence (Table 3, quote 1). Participants also emphasized the importance of continuously improving their pedagogical and instructional skills in order to increase their teaching effectiveness and adaptability (Table 3, quote 2). In addition, grounding teaching on sound evidence while remaining open to experimenting with innovative approaches was highlighted as a key strategy, reflecting a commitment to combining proven pedagogical methods with flexibility and creativity in practice (Table 3, quotes 3 and 4).
Regarding the development of digital skills, participants highlighted the challenges and opportunities presented by the COVID-19 pandemic, emphasizing the need to adopt innovative digital approaches to enhance knowledge transfer, such as creating digital learning content like videos and live online surveys, as essential tools for future educational success (Table 3, quote 5). In addition, there was a motivation to use the dHPE program to help develop and implement personalized media-based teaching concepts or interactive online courses tailored to specialized topics to support student engagement and provide real-time feedback (Table 3, quotes 6 and 7).
In summary, the theme of competence underscores participants' motivation to master teaching practice in general and to develop advanced digital skills in particular, acknowledging the role of the COVID pandemic in accelerating an adoption of innovative teaching strategies and reflecting a dual focus on evidence-based methods and innovative approaches.
Regarding interprofessional collaboration, motivation to engage in collaborative learning and interdisciplinary programs was particularly evident, with some participants emphasizing the collaborative nature of their fields, making interprofessional faculty development programs and collaborative learning opportunities essential to advancing interprofessional collaboration in therapy, research, and teaching (Table 4, quote 1). Others expressed a commitment to developing teaching methods and tools tailored to the needs of interprofessional health care teams, e.g., creating and implementing digital teaching and learning tools for interprofessional contexts as a key goal for applying to the program (Table 4, quote 2). Similarly, participants recognized the role of interprofessional networking in improving educational practice and promoting innovative, future-oriented teaching methods in an interprofessional skills lab (Table 4, quote 3). Other participants highlighted the potential of such collaboration to initiate interprofessional teaching projects and drive development of digital teaching approaches, emphasizing the critical role of interprofessional exchange (Table 4, quote 4).
Mentorship was highlighted as a central component of motivation, with participants aiming not only to support the development of students, but also to actively contribute to professional growth of their professional peers, ensuring that advances in education and digital instructional methods are widely shared and implemented. Passing on knowledge and skills to future generations of health professionals reflects a commitment to supporting peers and junior colleagues with digital tools in a rapidly evolving educational landscape (Table 4, quote 5). Application to the d-HPE program was also motivated by an intention to integrate digitization into university teaching by disseminating any knowledge gained to colleagues, further underscoring the cascading effect of mentorship in fostering innovation across disciplines (Table 4, quote 6). Other participants noted the value of sharing insights with colleagues in specialized fields while also contributing to broader digital teaching projects at universities (Table 4, quote 7).
In summary, the theme relatedness emphasizes the importance of interprofessional collaboration and mentorship to promote educational innovation, professional development and the dissemination of advanced teaching practices across disciplines and institutions.
The motivation of teaching health professionals to deliberately participate in an extensive faculty development program, despite the significant demands of their clinical roles, is a critical factor to the success and sustainability of such initiatives. This study explored motivations of health professions faculty to engage in a voluntary faculty development program, the d-HPE at the Charité Berlin. The theoretical framework of self-determination theory, with its three dimensions of autonomy, competence and relatedness, provided a deeper understanding of the personal and professional factors that drive participation in such a faculty development program. In the following sections, we will discuss our findings in the context of the literature, highlighting the importance of intrinsic motivation and the need for teachers to feel supported in their professional development. In addition, we will derive implications on how to motivate faculty to engage in similar faculty development programs based on the findings identified in our sample of motivation letters.
Overall, the results indicate that intrinsic motivation plays an important role in attracting faculty to participate in faculty development initiatives, moving beyond the “carrots and sticks” of extrinsic motivations commonly highlighted in the literature, such as scholarships, awards, promotions, incentives, or coercion by department heads (36). While intrinsically motivated faculty may be more likely to use best teaching practices, extrinsically motivated faculty may choose less effective strategies as their goal is the shortest path to outcome completion (28). Autonomy and self-direction were associated with increased motivation, so rather than focusing solely on institutional and functional needs, addressing faculty members' perceived needs for autonomy in planning their own professional development path led to higher levels of curiosity to learn and try new things, resulting in increased sustainability and success of faculty development initiatives (52–55). Conversely, the limited autonomy experienced by some educators appeared to inhibit the long-lasting impact of continuing professional development projects, despite the voluntary nature of attendance (56, 57). Autonomous motivation was also found to predict greater incorporation of effective teaching strategies and instructional clarity, as well as collaborative learning, by healthcare professions educators (28). It is therefore recommended that teachers' engagement in professional development activities should be driven by their own determination, alignment with their personal aspirations or values, confidence in their ability to acquire new skills, and autonomy in shaping their own professional development trajectories, rather than by extrinsic sources of motivation.
Early teaching experiences serve as important sources of motivation for engaging in faculty development, which is consistent with the literature suggesting that early teaching experiences can play a critical role in shaping educators' long term commitment to teaching (58, 59). This is particularly important in shaping the identity as a health professions educator, as prior to teaching, students do not make an explicit connection between teaching and being a physician (or maybe better) “health professional” (58). Thus, our findings underscore an importance of promoting early teaching experiences as it can significantly increase motivation to participate in faculty development programs and promote an identity as a teacher (54).
Regarding the competence theme, our results show that motivation to master evidence-based teaching practices and develop advanced digital skills encourages health professionals to engage in faculty development activities, which is consistent with previous research (36). In this context, digital competence, characterized by a desire to learn and develop professionally, is crucial for institutions to develop digital competence policies and initiatives, plan professional development and integrate technology into teaching practice (60, 61). However, research has shown that motivation to learn and teach digital competence is not always directly related to training received; it is also influenced by other factors such as “working climate” and institutional support (62). A key implication, therefore, is that faculty development and competence are mutually reinforcing. The participation in faculty development activities enhances teachers' digital competence, while the desire to improve one's own competence serves as a key motivator for engaging in such initiatives (61).
Regarding the relatedness theme, participants showed a strong appreciation of interprofessional collaboration, recognizing its value in networking, developing collaborative skills and fostering a better understanding of different professional roles. These findings are consistent with recent literature advocating a growing need for interprofessional faculty development programs and describing relatedness as the “enjoyment” of working with and learning from others (63, 64). This reinforces the notion that faculty development should foster a sense of community and support, and that digital interprofessional education is needed across the continuum of undergraduate, postgraduate and faculty development (65, 66). In addition, the integration of digital tools into interprofessional teaching contexts addresses the frequent lack of advanced digital skills among health professional educators, particularly in collaborative and interdisciplinary settings (67). Participants in our study emphasized the importance of creating and implementing digital teaching tools tailored to interprofessional health care teams, reflecting a commitment to bridging this digital skills gap.
Mentorship emerged as another key theme, with participants in our study expressing a strong desire to support the professional development of colleagues and students through mentoring initiatives. This focus on mentorship reflects a commitment to long-term professional development, with teachers acting as catalysts for innovation by passing on knowledge and skills to both students and colleagues. Just as formal faculty development programs—such as workshops—provide structured opportunities for professional growth, mentoring serves as an important, often informal, approach to fostering long-term development (68). This highlights the critical role of mentorship in promoting sustainable professional development and reinforces the idea that faculty development is not only about individual growth and promotion, but also about creating communities of practice and cultivating a culture of continuous learning and excellence in healthcare education.
In summary, faculty are intrinsically motivated to engage in intensive programs in addition to their clinically demanding lifestyles and daily responsibilities when the faculty development initiatives combine formal and informal learning elements to provide a flexible, longitudinal learning experience in an interprofessional setting. The motivation for faculty to participate in such intensive programs goes beyond carrots and sticks, i.e., external rewards and punishments, and is driven by their personal commitment to professional development, the desire to acquire new skills, and the opportunity to collaborate with colleagues across disciplines, all of which contribute to their long-term satisfaction and development as educators. The carrots and sticks metaphor is consistent with the findings of the current study, where faculty participation is driven by internal factors (autonomy, competence and relatedness) rather than external rewards or punishments. It is also consistent with the theoretical framework of Self-Determination Theory (SDT) used in the study, which emphasizes intrinsic motivation over external rewards and punishments. The use of the metaphor also aims to effectively challenge traditional management approaches that rely heavily on rewards and punishments and reflects the modern understanding of professional motivation in education. The integration of structured workshops with peer coaching and collaborative networking to promote personal and professional growth helps to increase motivation. By fostering interprofessional collaboration and sustained engagement, the faculty development program not only improves individual teaching practice, but also supports the development of a culture of continuous learning, ultimately bridging the digital skills gap and advancing healthcare education.
While this study provides valuable insights into motivations of health professions educators to engage in a digital health professions education program, some limitations need to be acknowledged. First, the study relies on a small sample size of 21 motivational letters from two d-HPE cohorts, which may limit the generalisability of the findings to a broader population of health professions educators. In addition, all participants were from a single institution, Charité Berlin, where the 21 teachers are known within the institution for their participation in the programme. To protect their confidentiality and adhere to ethical research standards, we anonymised detailed demographic data such as place of work and specialty. However, this limits the level of contextual detail in the findings and their wider applicability to different educational settings with different institutional cultures and resources. In addition, the analysis is based on self-reported data, which introduces the potential for social desirability bias. Participants may have framed their motivations in ways that they perceived to be more socially acceptable or in line with the goals of the programme. While collaborative discussions during the analysis helped to ensure rigor and consensus, the inclusion of additional methods, such as interviews or focus groups, in future research could provide richer and more triangulated data. The lack of a comparison group of faculty who did not participate in the d-HPE program is another limitation, as this would have allowed for a deeper exploration of the unique factors driving participation relative to broader faculty development needs. Future research should aim to address these limitations by including a larger and more diverse sample from multiple institutions, incorporating a mixed methods approach, and including a comparison group to provide a more comprehensive and generalizable understanding of faculty motivations in similar programs.
Motivation of teaching health profession faculty to participate voluntarily in an intensive faculty development program is primarily driven by intrinsic motivational factors, particularly the desire for professional development and mastery of digital teaching skills. Rather than being swayed by the traditional “carrots and sticks” of external rewards or pressures, faculty are motivated by the opportunity to improve their teaching practice and contribute to educational innovation in digital health, despite the challenges posed by their busy clinical workloads. The findings also highlight the importance of interprofessional collaboration and mentorship in fostering a sense of belonging and supporting continuous professional development. Effective faculty development programs should prioritize autonomy, competence and relatedness to enhance engagement and align with the evolving demands of digital education. In addition, there is a need for faculty development initiatives that not only respond to external pressures, but also cultivate intrinsic motivations to ensure sustained faculty engagement and to facilitate professional growth.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Ethics Committee of the Charité University of Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
MS: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. ML: Data curation, Formal analysis, Writing – review & editing. HP: Formal analysis, Resources, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Stiftung Innovation in der Hochschullehre. The funders had no role in the study design, analyses, interpretation of data, writing the manuscript, approval, or decision to publish the results. No author was paid to write this article by any agency.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that Gen AI was used in the creation of this manuscript. The author(s) acknowledge the use of generative AI tools for language editing and rephrasing during the preparation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Cintra KA, Borges MC, Panúncio-Pinto MP, de Almeida Troncon LE, Bollela VR. The impact and the challenges of implementing a faculty development program on health professions education in a Brazilian Medical School: a case study with mixed methods. BMC Med Educ. (2023) 23:784. doi: 10.1186/s12909-023-04754-8
2. Car J, Carlstedt-Duke J, Tudor Car L, Posadzki P, Whiting P, Zary N, et al. Digital education in health professions: the need for overarching evidence synthesis. J Med Internet Res. (2019) 21:e12913. doi: 10.2196/12913
3. Foadi N, Varghese J. Digital competence–a key competence for todays and future physicians. J Eur CME. (2022) 11:2015200. doi: 10.1080/21614083.2021.2015200
4. Shon S, Shin H, Rim D, Jeon H. Nursing faculty development program for digital teaching competence. BMC Med Educ. (2024) 24:511. doi: 10.1186/s12909-024-05453-8
5. Almarzooq ZI, Lopes M, Kochar A. Virtual Learning During the COVID-19 Pandemic: A Disruptive Technology in Graduate Medical Education. Washington DC: American College of Cardiology Foundation (2020). p. 2635–8.
6. Car LT, Poon S, Kyaw BM, Cook DA, Ward V, Atun R, et al. Digital education for health professionals: an evidence map, conceptual framework, and research agenda. J Med Internet Res. (2022) 24:e31977. doi: 10.2196/31977
7. Harden RM, Lilley P. The Eight Roles of the Medical Teacher: The Purpose and Function of a Teacher in the Healthcare Professions. Edinburgh: Elsevier Health Sciences (2018).
8. Kohan M, Changiz T, Yamani N. A systematic review of faculty development programs based on the Harden teacher's role framework model. BMC Med Educ. (2023) 23:910. doi: 10.1186/s12909-023-04863-4
9. Janssen J, Stoyanov S, Ferrari A, Punie Y, Pannekeet K, Sloep P. Experts' views on digital competence: Commonalities and differences. Comput Educ. (2013) 68:473–81. doi: 10.1016/j.compedu.2013.06.008
10. Ferrari A, Punie Y, Redecker C, editors. Understanding digital competence in the 21st century: an analysis of current frameworks. In: Proceedings of the 21st Century Learning for 21st Century Skills: 7th European Conference of Technology Enhanced Learning, EC-TEL 2012, Saarbrücken, Germany, September 18-21, 2012. Berlin: Springer (2012).
11. Longhini J, Rossettini G, Palese A. Digital health competencies among health care professionals: systematic review. J Med Internet Res. (2022) 24:e36414. doi: 10.2196/36414
12. Nazeha N, Pavagadhi D, Kyaw BM, Car J, Jimenez G, Tudor Car L. A digitally competent health workforce: scoping review of educational frameworks. J Med Internet Res. (2020) 22:e22706. doi: 10.2196/22706
13. Jobst S, Lindwedel U, Marx H, Pazouki R, Ziegler S, König P, et al. Competencies and needs of nurse educators and clinical mentors for teaching in the digital age–a multi-institutional, cross-sectional study. BMC Nurs. (2022) 21:240. doi: 10.1186/s12912-022-01018-6
14. Laakkonen N, Jarva E, Hammarén M, Kanste O, Kääriäinen M, Oikarinen A, et al. Digital competence among healthcare leaders: a mixed-methods systematic review. J Nurs Manage. (2024) 2024:8435248. doi: 10.1155/2024/8435248
15. Kulju E, Jarva E, Oikarinen A, Hammarén M, Kanste O, Mikkonen K. Educational Interventions and their effects on healthcare professionals' digital competence development: a systematic review. Int J Med Inform. (2024) 185:105396. doi: 10.1016/j.ijmedinf.2024.105396
16. King SM, Richards J, Murray A-M, Ryan VJ, Seymour-Walsh A, Campbell N, et al. Informal faculty development in health professions education: identifying opportunities in everyday practice. Med Teach. (2021) 43:874–8. doi: 10.1080/0142159X.2021.1931080
17. Steinert Y, Mann K, Centeno A, Dolmans D, Spencer J, Gelula M, et al. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med Teach. (2006) 28:497–526. doi: 10.1080/01421590600902976
18. Wenger E. Communities of Practice: Learning, Meaning, and Identity. Cambridge: Cambridge University Press (1999).
19. Gruppen LD. Intensive Longitudinal Faculty Development Programs. Faculty Development in the Health Professions: A Focus on Research and Practice. Berlin: Springer (2013). p. 197–216.
20. Kusurkar RA, Croiset G, Mann KV, Custers E, Ten Cate O. Have motivation theories guided the development and reform of medical education curricula? A review of the literature. Acad Med. (2012) 87:735–43. doi: 10.1097/ACM.0b013e318253cc0e
21. Costa Jr PT, McCrae RR. From catalog to classification: Murray's needs and the five-factor model. J Pers Soc Psychol. (1988) 55:258. doi: 10.1037//0022-3514.55.2.258
22. Hull CL. Goal attraction and directing ideas conceived as habit phenomena. Psychol Rev. (1931) 38:487. doi: 10.1037/h0071442
23. Trivedi AJ, Mehta A. Maslow's hierarchy of needs-theory of human motivation. Int J Res Subj Multi Lang. (2019) 7:38–41.
24. Wigfield A, Eccles JS. Expectancy–value theory of achievement motivation. Contemp Educ Psychol. (2000) 25:68–81. doi: 10.1006/ceps.1999.1015
25. Bandura A. Social cognitive theory: an agentic perspective. Ann Rev Psychol. (2001) 52:1–26. doi: 10.1146/annurev.psych.52.1.1
26. Ten Cate OTJ, Kusurkar RA, Williams GC. How self-determination theory can assist our understanding of the teaching and learning processes in medical education. AMEE guide No. 59. Med Teach. (2011) 33:961–73. doi: 10.3109/0142159X.2011.595435
27. Nonaillada J. Applying Self-Determination Theory (SDT) to faculty engagement for curriculum development. J Faculty Dev. (2019) 33:103–8.
28. Stupnisky RH, BrckaLorenz A, Yuhas B, Guay F. Faculty members' motivation for teaching and best practices: testing a model based on self-determination theory across institution types. Contemp Educ Psychol. (2018) 53:15–26. doi: 10.1016/j.cedpsych.2018.01.004
29. Aulenkamp J, Mikuteit M, Löffler T, Schmidt J. Overview of digital health teaching courses in medical education in Germany in 2020. GMS journal for medical education. (2021) 38.
30. Ersoy H, Baskici C, Aytar A, Strods R, Ratinika NJ, Fernandes AML, et al. Digital competence of faculty members in health sciences measured via self-reflection: current status and contextual aspects. PeerJ. (2024) 12:e18456. doi: 10.7717/peerj.18456
31. Urrejola G, Lillo AH. Competencias digitales docentes:: reporte de autopercepción en ciencias de la salud. Horizonte médico. (2023) 23:8. doi: 10.24265/horizmed.2023.v23n4.07
32. Litina S, Svētina K. In: Daniela L, editor. Digital Competence of Medical College Teachers According to Digcompedu Framework. Riga: University of Latvia Press (2023). p. 985. doi: 10.22364/atee.2022
33. Ryhtä I, Elonen I, Hiekko M, Katajisto J, Saaranen T, Sormunen M, et al. Enhancing social and health care educators' competence in digital pedagogy: A pilot study of educational intervention. Finnish J eHealth eWelfare. (2021) 13:302–14. doi: 10.23996/fjhw.107466
34. Haas M, Triemstra J, Tam M, Neuendorf K, Reckelhoff K, Gottlieb-Smith R, et al. A decade of faculty development for health professions educators: lessons learned from the Macy Faculty Scholars Program. BMC Med Educ. (2023) 23:185. doi: 10.1186/s12909-023-04155-x
35. Alexandraki I, Rosasco RE, Mooradian AD. An evaluation of faculty development programs for clinician–educators: a scoping review. Acad Med. (2021) 96:599–606. doi: 10.1097/ACM.0000000000003813
36. Lowenthal PR, Wray ML, Bates B, Switzer T, Stevens E. Examining faculty motivation to participate in faculty development. Int J Univ Teach Fac Dev. (2013) 3:149–64.
37. Love LM, Haggar FL, McBrien SB, Buzalko RJ, Hartman TL, Shope RJ, et al. Supporting the professional identity of medical science educators: understanding faculty motivations for quality improvement in teaching. Med Sci Educ. (2018) 28:655–65. doi: 10.1007/s40670-018-0609-3
38. Kamel AM. Role of faculty development programs in improving teaching and learning. Saudi J Oral Sci. (2016) 3:61–8. doi: 10.4103/1658-6816.188073
39. Olivares SLO, Lopez M, Martinez R, Alvarez JPN, Valdez-García JE. Faculty readiness for a digital education model: a self-assessment from health sciences educators. Aust J Educ Technol. (2021) 37:116–27. doi: 10.14742/ajet.7105
40. Mirmohamadkhani MM, Rezaie M, Kohsarian P, Eskandari F, Nazemi F. Motivational Factors affecting the educational performance of faculty members. Iran J Med Educ. (2017) 17:392–9. Available at: http://ijme.mui.ac.ir/article-1-4330-en.html
41. Ong CCP, Foo YY, Chiu FY, Nestel D. ‘It's going to change the way we train': Qualitative evaluation of a transformative faculty development workshop. Perspect Med Educ. (2021) 11:86–92. doi: 10.1007/S40037-021-00687-4
42. Broadbent J, Bearman M, Boud D, Dawson P. Academics' intention to sustain new teaching practices after the COVID-19 pandemic: examined through the theory of planned behaviour. High Educ. (2024) 1–16. doi: 10.1007/s10734-024-01326-7
43. DiCicco-Bloom B, Crabtree BF. The qualitative research interview. Med Educ. (2006) 40:314–21. doi: 10.1111/j.1365-2929.2006.02418.x
44. Dwivedula R, Singh P. A qualitative approach to understand generation Z work motivation. Eur J Behav Sci. (2021) 4:1–17. doi: 10.33422/ejbs.v4i2.542
45. Azungah T. Qualitative research: deductive and inductive approaches to data analysis. Qual Res J. (2018) 18:383–400. doi: 10.1108/QRJ-D-18-00035
46. Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. (2005) 15:1277–88. doi: 10.1177/1049732305276687
47. Zhang Y, Wildemuth BM. Qualitative analysis of content. In: Applications of Social Research Methods to Questions in Information and Library Science, vol. 308. Bedford Square: Bloomsbury Publishing (2009). p. 1–12.
48. Hwang S. Utilizing qualitative data analysis software: a review of Atlas. Soc Sci Comput Rev. (2008) 26:519–27. doi: 10.1177/0894439307312485
49. Ryan RM, Deci EL. Self-determination theory. Encyclopedia of quality of life and well-being research. Berlin: Springer (2024). p. 6229–35.
50. Kuper A, Lingard L, Levinson W. Critically appraising qualitative research. BMJ. (2008) 337:a1035. doi: 10.1136/bmj.a1035
51. Schwandt T. Qualitative Inquiry: A Dictionary of Term, vol. 62. Thousand Oaks: Sage Publications (1997). p. 1118.
52. Dee JR, Daly CJ. Innovative models for organizing faculty development programs: Pedagogical reflexivity, student learning empathy, and faculty agency. Human Archit J Sociol Self-Knowl. (2009) 7:1. Available at: http://scholarworks.umb.edu/humanarchitecture/vol7/iss1/2
53. Rarasati N, Pramana RP. Giving Schools and Teachers Autonomy in Teacher Professional Development Under a Medium-Capability Education System. RISE Insight Series (2023).
54. Bergmark U. Rethinking researcher–teacher roles and relationships in educational action research through the use of Nel Noddings' ethics of care. Educ Action Res. (2020) 28:331–44. doi: 10.1080/09650792.2019.1567367
55. Daly CJ. Faculty learning communities: addressing the professional development needs of faculty and the learning needs of students. Curr Teach Learn. (2011) 4.
56. Hargreaves E, Berry R, Lai YC, Leung P, Scott D, Stobart G. Teachers' experiences of autonomy in continuing professional development: teacher learning communities in London and Hong Kong. Teach Dev. (2013) 17:19–34. doi: 10.1080/13664530.2012.748686
57. Basri F. Factors influencing learner autonomy and autonomy support in a faculty of education. Teach High Educ. (2023) 28:270–85. doi: 10.1080/13562517.2020.1798921
58. Amorosa JMH, Mellman LA, Graham MJ. Medical students as teachers: how preclinical teaching opportunities can create an early awareness of the role of physician as teacher. Med Teach. (2011) 33:137–44. doi: 10.3109/0142159X.2010.531154
59. Henry B, Haworth J, Hering P. Perceptions of medical school graduates and students regarding their academic preparation to teach. Postgrad Med J. (2006) 82:607–12. doi: 10.1136/pgmj.2006.045393
60. O'Sullivan PS, Irby DM. What motivates occasional faculty developers to lead faculty development workshops? A qualitative study. Acad Med. (2015) 90:1536–40. doi: 10.1097/ACM.0000000000000767
61. Amare EM, Zegeye RT, Wondie AG, Andargie BA. Surveying the Digital Competencies of Health Profession Educators at Ethiopian Higher Education Institutions. Ethiop J Health Sci. (2024) 34:281–9. doi: 10.4314/ejhs.v34i4.4
62. Navarro-Martínez O, Igual-García J, Traver-Salcedo V. Bridging the educational gap in terms of digital competences between healthcare institutions' demands and professionals' needs. BMC Nurs. (2023) 22:144. doi: 10.1186/s12912-023-01284-y
63. Chen HC, McNamara M, Teherani A, Cate Ot, O'Sullivan P. Developing entrustable professional activities for entry into clerkship. Acad Med. (2016) 91:247–55. doi: 10.1097/ACM.0000000000000988
64. Babin C, Salem Y, Quiben M, Davis B. Interprofessional Education (IPE) Faculty Development—a Scoping Review. Health Interprof Pract Educ. (2023) 5:1–26. doi: 10.61406/hipe.269
65. Virant-Young D, Forrest K, McCaskey S, Smith C, Saadeh C, Gudakunst J, et al. Faculty development in interprofessional education: designing and implementing a successful program. Med Sci Educ. (2014) 24:401–7. doi: 10.1007/s40670-014-0071-9
66. Cresswell NR, Walker ST, Harrison C, Kent F. Teaching digital interprofessional collaboration. Clin Teach. (2024) 21:e13651. doi: 10.1111/tct.13651
67. Tegegne MD, Tilahun B, Mamuye A, Kerie H, Nurhussien F, Zemen E, et al. Digital literacy level and associated factors among health professionals in a referral and teaching hospital: an implication for future digital health systems implementation. Front Public Health. (2023) 11:1130894. doi: 10.3389/fpubh.2023.1130894
Keywords: faculty development, qualitative study, digital health professions education, self-determination theory, intrinsic motivation
Citation: Schumann M, Lehmann M and Peters H (2025) Beyond carrots and sticks. Exploring faculty motivation to join a digital health professions educator program. Front. Med. 12:1554011. doi: 10.3389/fmed.2025.1554011
Received: 31 December 2024; Accepted: 17 February 2025;
Published: 05 March 2025.
Edited by:
Ardi Findyartini, University of Indonesia, IndonesiaReviewed by:
Rebecca S. Koszalinski, University of Central Florida, United StatesCopyright © 2025 Schumann, Lehmann and Peters. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marwa Schumann, bWFyd2Euc2NodW1hbm5AY2hhcml0ZS5kZQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.