- 1Action Research Partnerships, Adelaide, SA, Australia
- 2Torrens University Australia, Public Health, Equity and Human Flourishing, Adelaide, SA, Australia
- 3Department of Psychiatry, Women’s and Children’s Health Network, SA, Australia
- 4Faculty of Health and Medical Sciences, University of Adelaide, SA, Australia
Background: Maternal mental illness is a major growing global concern which can affect parenting with serious negative implications for offspring. Group-based parenting programs for mothers which both enhance the parent-child relationship and address mental health symptoms in a supportive social setting may optimise better outcomes for mothers and children. The Acorn program in South Australia draws on attachment theory to integrate dance play, reflective diary keeping and therapeutic letters in a holistic program for a diversity of vulnerable mothers and children aged 1–36 months. The program seeks to nurture and enhance parental wellbeing and the quality of the parent-child relationship for mothers experiencing identified mental health illnesses that impinge upon their parenting. This study presents the evaluation of the program and its effectiveness.
Methods: Action research approach for continuous monitoring and program improvement engaging Acorn program staff in evaluation data collection and interpretation of pre and post self-completion measures and standardized observations. Additional data was collected through a telephone interview of attending mothers 6–8 months after program completion to address sustainable impacts on parenting and wellbeing.
Results: The program engaged 353 diverse vulnerable mothers with their children. Many had profound overlapping mental health issues including borderline personality disorder (BPD) and depression. The quality of the parent-child interaction, parental confidence, competence and enjoyment were enhanced; mothers' wellbeing, ability to cope and lasting social supports were augmented. This occurred for a number of “most vulnerable” subgroups including single mothers, mothers with BPD, mothers from non-English speaking households and those with lower levels of education or household income. Mothers reported sustained improvements in their wellbeing, parenting, social and family lives, and feeling closer to their child as a result of participating in the program.
Conclusions: Given the high prevalence of maternal mental health issues and substantial potential negative consequences for mothers and offspring, the Acorn parenting program offers an effective means of addressing this pressing public health issue potentially helping large numbers of vulnerable mothers and their children. This has additional gravitas in the shadow of COVID-19 due to expanded numbers of those experiencing greater parental stress, isolation and mental illness.
1. Introduction
Maternal mental illness and particularly maternal depression is common (1) and for many enduring. A recent overview of 80 countries estimated a global postpartum depression prevalence of around 17.2%; the highest rate of 39.96% was found in South Africa, with Australia being around 11.22% (2). The majority of people suffering from depression have at least one comorbid mental disorder (3), and an array of other specific mental health illnesses experienced during motherhood including psychosis, bipolar disorders and borderline personality disorder (BPD) contribute to an overall persistently high prevalence of maternal mental illness (4). While postpartum depression can be experienced by women up to twelve months after the birth of their child (5), experiencing depression is not limited to the postpartum period; an Australian study has found maternal depression to be more common when the child passes toddler age than in the first twelve months postpartum (6), and severe postnatal depression elevates mothers' risk of continuing to experiencing depression in the following decade (7).
Mothers with maternal mental illnesses may experience a range of issues including depressed mood and sadness, mood swings, difficulties coping, feelings of guilt, shame and worthlessness, extreme concerns about their baby, anxiety, a loss of interest in daily activities, a sense of overwhelming loneliness and feeling alone in their experiences, and a strong sense of stigma (8–14) Experiencing mental illness also increases the risk of family conflict and relationship breakdown (15) and maternal suicide (16, 17), a leading cause of maternal death in the peripartum period (18) with elevated risk for those experiencing BPD (19–21).
The compromised emotions many mothers with maternal mental illness experience can distort emotional communication with their children. Subsequently mothers' enjoyment of the parental role may be reduced affecting a delay in developing competency in parenting skills and potentially creating a detached, mechanistic caregiving experience (22). Given these difficulties, it is predictable that maternal mental illness is associated with low perceived parental self-efficacy (PPSE) (23, 24), and low maternal confidence (25). PPSE refers to the capabilities parents believe they have to successfully organise and execute situation specific parenting tasks (26), and this is positively associated with actual parenting competence (23). Low maternal confidence experienced in the early postpartum period by mothers with maternal mental illness has also been shown to persist for several years to pre-school age despite improvements in the mother's mental health, and may continue to have a negative effect on the mother-child relationship (25, 27). Postpartum depressive symptoms are also associated with higher parenting stress (28–30), and “Parental Distress” in particular has also been found to predict later depressive symptoms (31). However, despite these myriad issues there is qualitative evidence that women with severe mental illness may value motherhood more highly as a central positive influence in their lives (12).
The profoundly negative effects maternal mental health can have on offspring have been broadly documented (32–40). However, this causal pathway has been shown to be mediated by the quality of parenting behaviours (33, 41–43). There is a large body of research associating a broad range of maternal mental illnesses with negative parenting behaviours, disengaged parenting and poorer mother-infant interaction during infancy, with most of this work addressing maternal depression (41, 44–57). Stress in the parenting system has also been specifically shown to impinge on the quality of parenting behaviour (58), the quality of the developing relationship between mother and infant (35), and the meaning and satisfaction these mothers derive from caregiving (59). The quality of mother-child interaction has been shown to predict the child's later positive cognitive and socio-emotional development, and academic competence in middle childhood (60–64). Moreover, an important predictor of parenting behaviour is how parents were parented themselves (65, 66), highlighting the potential endurance of unchecked problems through generations.
There is accumulated evidence, that a variety of psychosocial and psychological programs including peer/social support, group treatment, and non-directive counselling where mothers are encouraged to explore their feelings and find their own solutions benefit mothers with postpartum depression (67–69). A major challenge here is that treating the mother's mental illness alone does not necessarily help enhance an impaired parent-child relationship and its negative consequences for the child (70–76). Notably, studies with mothers in remission have demonstrated that impairments in parenting developed during acute maternal depression can persist (77, 78). However, building parental confidence and PPSE, can have a positive influence on healthy parenting practices (79), and interventions that successfully enhance the mother-infant relationship and build parental confidence have been shown to provide a protective buffer for the effects of maternal mental illness and subsequent compromised child development (75, 79, 80).
Given the potential to modify parenting behaviour, there is a strong case for developing effective parenting interventions for mothers with maternal mental illness to mediate the effects of their illness on child outcomes (33). Interventions that utilised both maternal-child interaction guidance and psychotherapeutic group support can significantly improve the mother's mental health, parenting and child development outcomes (81). The evidence therefore suggests the need to combine strategies to address mental health symptom relief with strategies to enhance the quality of the parent-child relationship. In the latter case integrating activities that enhance mother-infant interaction, build parental confidence/perceived parental self-efficacy, and encourage sensitive parenting and maternal bonding may be of particular benefit (74, 82, 83). Holistic group-based parenting interventions may offer additional social support along with the potential for a mutual learning environment where skills and strategies can be practiced (84). This composite approach may optimise the likelihood of better outcomes for mothers, children, and families (73, 75, 85, 86). However, it is important to highlight that studies to date have tended to have relatively small samples of often homogeneous groups of women, focussing on a small number of outcomes (81). It is against this background of the need for an effective blended composite group-based approach implemented in the broader diverse community of mothers with maternal ill health that the Acorn program in South Australia and its concurrent evaluation emerged.
The effectiveness of a community-based program delivered to a relatively heterogeneous client base should include consideration of identified vulnerable subpopulations. Mothers who are single have been found to be particularly vulnerable to maternal mental illness (87), including chronic stress and depression (88–90). Migrant mothers to higher income countries are also at increased risk particularly where there are language difficulties (91, 92) with this applying to both clinical and non-clinical levels of postpartum depression (93, 94). In both cases these risk factors may be compounded by greater social isolation and loneliness, both of which are commonly associated with significant mental illness and poorer mental health (95–101). Income and education have been found to have significant negative associations with depression severity among mothers of young children (102), and socioeconomic factors have been found to moderate the relationship between maternal mental illness and negative parenting practices with the association tending to be stronger in lower socio-economic groups and where the mother has lower formal education (41, 54). A systematic review addressing maternal BPD has concluded that these mothers are more likely to engage in maladaptive interactions with their offspring (103) and qualitative research has identified the emotional intensity, social isolation and lack of positive parenting models for these mothers warrant parent-focussed support (104). Finally, postpartum depression has been found to be more prevalent in multiparous mothers of young children than their nulliparous counterparts, with this being attributed to the greater psychological demands of parenting more than one young child (102, 105, 106).
The evaluation of the Acorn program has therefore examined its effects for a diverse client base of mothers with mental illness including the specific subpopulations: single mothers, those who speak a language other than English at home, those whose main source of household income is Government benefit, and mothers whose education level has not progressed beyond Year 12 school level. Mothers who indicate BPD, and those with more than one young child of the ages targeted by the Acorn intervention were also considered as additional vulnerable subpopulations to consider in order to assess the value of the program.
2. Program overview
The Acorn parenting program is a face-to-face group-based holistic intervention of 15 weekly sessions of two hours duration provided in South Australian community venues (mostly child care centres) to help mothers of young children (0–3 years) who are experiencing chronic, and in many cases profound mental health challenges which impinge upon the quality of their parenting. Mother-child dyads are referred by a broad range of sources including Child and Family Health Services, Perinatal and Infant Mental Health Services, general hospitals, and private psychiatric and psychology consultants. This enables a diverse range of mothers to be directed to the program by their referrers with the only exclusion criteria being a current diagnosis of a psychotic disorder which might render group work with other mothers inappropriate. Acorn groups were conducted across fifteen geographically dispersed locations in metropolitan and outer metropolitan Adelaide suburbs with the program being delivered in “waves” twice a year to between 4 and 10 groups at a time.
The theoretical underpinnings of the Acorn program were informed by attachment research which reinforces how the quality of the parent child attachment has a significant role in the life trajectory of the child (107) and highlights the importance of addressing the origins of disorganization (108), encouraging parental sensitivity (109) and developing reflective functioning (110). This therapy allows the women to experience a relationship that is safe, curious and reflective, while assisting the processing and integration of her past parenting and mental health history (111).
Each Acorn session incorporates three evidence based “primary components”. “Dance Play”, “Reflective Journaling” and “Therapeutic Letters”. Dance Play activities are designed to encourage meaningful mutually enjoyable playful interactions between mothers and infants (112–115) and to nurture the child's agency to visibly emerge while developing the mothers’ abilities to recognize and respond to their child's cues, needs and behaviours as they build new repertoires of play and engagement (116). Dance play activities and songs engage all attending children including a “Hello” song at the beginning of the session in which each participating child's name is sung by the group, but Dance Workers also draw from compiled program activities and songs tailored to the developmental ages of the attending children drawing on Clark and Dawson's conceptual stages of “being, thinking and doing” (117). “Reflective Journaling” (118–120) seeks to encourage mothers' strength based reflection on their perspectives and lived experiences surrounding their parenting and mental health, including exploration of core relational conflicts (121). This component also provides a forum where mothers can share and explore their experiences with their peers, helping them to understand that they are not alone in their struggles and encouraging supportive friendships to develop. “Therapeutic letters” (122, 123) sent as e-mail correspondence between sessions act as a mode of extending reflections from the therapist to patient beyond formal sessions. Parents are supported in a “non-judgmental” safe environment to overcome blocks in their ability to read, interpret and respond to their infant's cues accurately and appropriately.
The groups are staffed by a dance and movement specialist (qualified dance practitioners with formal post graduate qualifications in this area) who facilitates Dance Play, a Mental Health Clinician (a psychologist, social worker, or mental health nurse, trained in maternal and infant mental health and attachment theory), who facilitates the compilation of Therapeutic Letters, and a Family Support Practitioner (qualified social worker) who leads the journaling and reflection components of the groups.
Following the Acorn group session, the staff team conducts a ninety-minute group supervision and debriefing session facilitated by the Mental Health Clinician in which reflections on each dyad are shared to inform the tailored Therapeutic Letter, and any staff concerns are discussed. The Mental Health Clinicians also provide individual supervisory support for the other team members, and are supported themselves by an external clinical supervisor. An Acorn Coordinator, a qualified social worker with knowledge of attachment theory, organizes group referral allocation and program promotion activities, with the whole program being overseen by a Program Manager.
Peer meetings of Acorn Dance Workers, Family Support Practitioners and Mental Health Clinicians are regularly conducted to enable shared reflections on practice and maintain program fidelity within their own discipline. Whole of program team meetings are conducted at the end of each program year in which evaluation findings are also presented and discussed.
Facilitator capacity is enhanced through internal training using developed program resources and induction including observations of existing Acorn groups followed by staff debriefing. Externally sourced training needs are reviewed periodically through a Critical Reference Group (124) comprised of program stakeholders and representatives of referring agencies, and this has included formal training in therapeutic letter writing, perinatal infant mental health, the Circle of Security (125), attachment theory, Marte Meo training (126), understanding personality disorders, strengths based practice, and developing cultural competence.
The Acorn program inclusively workshopped and designed a program logic stipulating a range of short, intermediate, and longer-term desired Acorn outcomes (Figure 1). The stated goal of the Acorn program is: “To holistically nurture and enhance parental wellbeing and the quality of the parent-child relationship for mothers experiencing identified mental health illnesses and their young children aged 0–36 months”. The four longer-term collectively agreed objectives of the program are: to enhance the quality of the parent-child interaction; to improve parenting confidence, competence and enjoyment for vulnerable mothers; to enhance mothers' wellbeing, coping skills, resilience and self-efficacy; to expand and strengthen Social/Community supports and build Social Connectedness. The program logic and full program details are included as part of the Acorn Manual available through the MeB4three website (116).
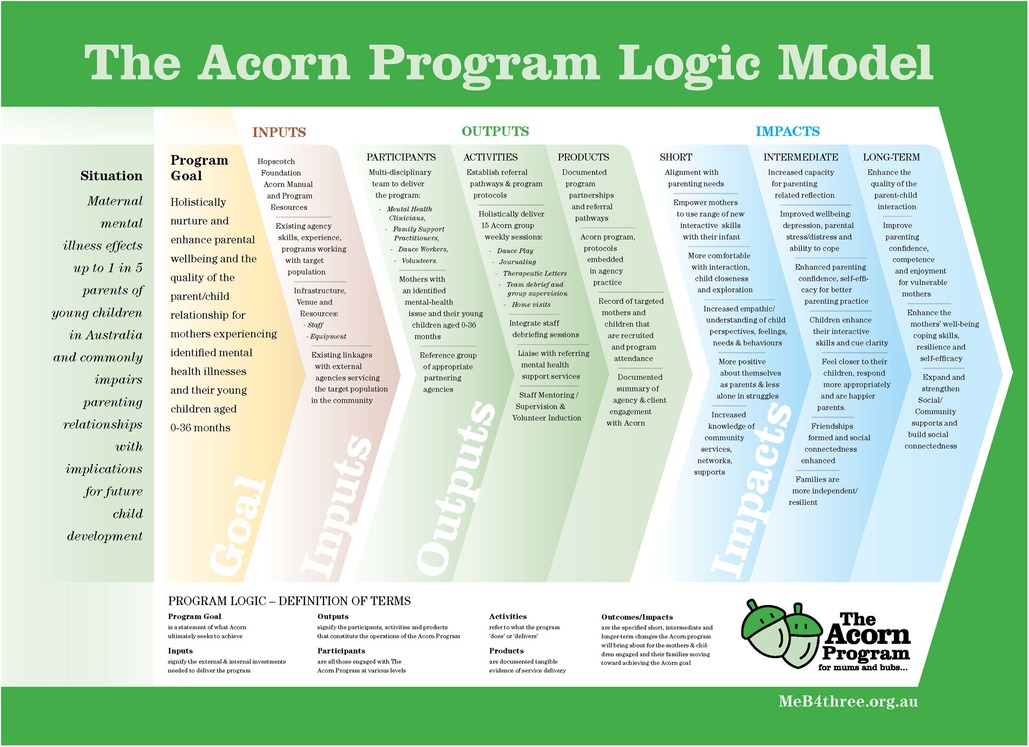
Figure 1. “The Acorn Program Logic Model”: source: Chance S. The Acorn Program: from small things big things grow. 2021. South Australia: The Hopscotch Foundation PTY. https://meb4three.org.au/acorn/.
3. Design, materials and methods
This paper presents the summative quantitative process and outcome findings (pre-post measures and follow-up interviews) from the first eleven Waves of Acorn over a period of 5.5 years. Qualitative findings from the open-ended questions and focus groups exploring in-depth experiences of mothers on the program will be reported in a separate paper.
The evaluation adapted an action research approach (127, 128), providing evaluation training to Acorn service providers who administered the battery of evaluation tools pre and post each program wave to attending mothers. There were no incentive payments for participating in the evaluation and mothers were informed that while their participation may not benefit them directly, their answers may inform future program refinement. All mothers who had enrolled were eligible for the pre-measures and all mothers who had not formally withdrawn from the program were eligible for post-measures regardless of how many sessions they had attended. Client self-completion tools were answered individually and sealed in envelops to ensure and demonstrate confidentiality before being sent to the evaluator for data entry and analysis. The findings were analyzed between waves by the evaluator and presented to the Critical Reference Group. Evaluation was a standing agenda item here, informing a collective and democratic process of interpretation, reflection, and planned revisions to program delivery to be formulated progressively in order to refine and improve program implementation and evaluation in subsequent waves. Representatives from each of the discipline groups facilitating Acorn also provided their group reflections for discussion during these meetings to further inform improvement to future practice in a continuing cyclical learning process (127, 129).
Given the vulnerability of Acorn participants, and the concern to retain client engagement in Acorn, ensuring that the compounding burden of evaluation demands was acceptable and manageable was a primary concern, with this being monitored during client focus groups and regular feedback from Acorn staff interviews. The standardised psychometric tools were selected based on: the ability of the tool to provide reliable, valid, and relevant indications of objectives being met; the appropriateness of the tool for application with vulnerable Australian mothers of children aged between 0 and 36 months of mixed educational and cultural backgrounds; the ease of administration and completion for participating subjects in a community-based group setting. The Bellberry Human Research Ethics Committee scientifically and ethically reviewed all aspects of the evaluation.
The tools applied throughout the 11 waves of the program were:
The Parenting Stress Index Short Form [PSI-SF] (130) is a 36 item scale measuring “Total Parenting Stress” with the following 12 item subscales: “Parental Distress”, the distress parents experience in their role as a function of personal factors that are directly related to parenting; “Parent–Child Dysfunctional Interaction”, the degree to which the mother perceives their child as not meeting expectations, with scores in the 96th percentile suggesting potential for abuse; “Difficult Child”, the parent's perception of the behavioural characteristics of the infant that makes him/her either easy or difficult to manage. Scores are interpreted relative to percentiles from a normative sample for each subscale and the total provides indications of “Clinically Significant”, “High”, “Normal Range” or “Low” levels for each respondent. The scale has been translated into over 40 different languages and validated across a broad range of cultures and populations (ibid).
The Patient Health Questionnaire [PHQ-9] (131) provides a criteria-based indication of depressive disorders and measure of depression severity. The PHQ-9 is the nine-item depression module taken from the larger Patient Health Questionnaire (PHQ) which is a self-administered version of the Primary Care Evaluation of Mental Disorders (PRIME-MD) diagnostic instrument for common mental disorders. The PHQ-9 focusses exclusively on the 9 diagnostic criteria for DSM-IV depressive disorders, scoring each as “0” (not at all) to “3” (nearly every day). A total score of ≥10 has a demonstrated sensitivity of 88% and specificity of 88% for major depression, with scores of 5, 10, 15 and 20 validly demarcating the lower limits indicating “minimal symptoms”, “minor depression/major depression mild”, “major depression moderately severe”, and “major depression severe”. The tool includes a supplemental scale addressing the level of functional difficulty respondents may have in their work, home or social life as a result of any indicated symptoms with this ranging from “not difficult at all” to “extremely difficult”.
The Karitane Parenting Confidence Scale [KPCS] (132) is used to assess the unidimensional construct Perceived Parental Self-Efficacy (PPSE) in parents with infants aged 0–12 months. To ensure eligibility for this measure pre and post scores were analysed for children aged 8 months or less on commencing the program. This 15-item scale was developed using an Australian population of mothers including participants from culturally and educationally diverse backgrounds. Grounded in Bandura' self-efficacy theory (133), the items in the KPCS follow his recommendation to be of a “task specific” nature, which is considered to imbue a greater sensitivity and predictive validity for scales addressing “self-constructs” (134, 135). Higher scores indicate greater Perceived Parental Self-Efficacy with clinical cut-off scores: “severe clinical” range <31, “moderate clinical” range 31–35, “mild clinical” range 36–39, and “non-clinical” range ≥40. Cronbach's alpha for the KPCS has been calculated as .81 and test-retest reliability .88, with sensitivity and positive predictive power calculated at .86 and .88 respectively (134).
Client Self-Completion Questionnaires, semi-structured pre and post tools including demographics, process and impact Likert scales and open questions inviting further comments on the “closed” item responses. The pre-measure included Likert Scale items for mothers to indicate personal reasons for attending Acorn (e.g., I would like to be able to interact better with my child/children). The post-measure included a Likert scale operationalising indicators addressing each objective (e.g., I interact better with my child because of attending this group; The group has helped me to cope better as a parent; I made friends with other parents in the group); and a separate scale under the heading “For each area, please indicate the extent to which your current parenting abilities or experiences have improved (if at all) as a result of attending the group”, with this including items addressing parental understandings, feelings and reflections; all items appear in Table 5. Scales included negatively worded items (e.g., The group was not very helpful for me), to provide an indication of diligence in client response. Mothers were also asked to indicate the extent to which they would recommend the Acorn program to their peers. The questionnaires were piloted with a small group of mothers prior to the evaluation.
A six-eight month “Follow-Up” Telephone Interview was applied with mothers from Waves 1–9 who had consented to be contacted for the purpose at the beginning of the program. This was conducted by a trained female independent interviewer who had professional experience in social work and maternal mental health. The interview schedule included Likert scale items from the post Client Self-Completion Questionnaire which were read verbatim to participants to enable direct comparisons with responses provided on completion of the program. The interviews lasted between 25 and 60 min.
Two additional tools were introduced as the program developed:
The McLean Screening Instrument for Borderline Personality Disorder [MSI-BPD] (136), applied in wave 4, is a 10 item self-report measure addressing BPD based on DSM-IV BPD criteria. Each endorsed item scores 1 point with a score of 7 or more indicating likely BPD. The tool has demonstrated good sensitivity (.81) and specificity (.85). For young adults between the ages of 18–25 years diagnostic efficiency of the tool was higher; sensitivity .90 and specificity .93. The tool has good internal consistency with a Cronbach's alfa of .74. The MSI-BPD was applied as a pre-measure only to provide indications of borderline personality disorder (BPD).
The Nursing Child Assessment Satellite Training [NCAST] Parent-Child Interaction Teaching Scale [NCAT] (137), introduced in Wave 6 is a 73 item observational tool used to measure the quality of the parent-child interaction with children up to 36 months. This is comprised of a number of subscales with the most reliable measures over time being the composite scales of “Caregiver-Infant Total” (the overall quality of the interaction), “Caregiver Total” (assessing the quality of the mother's contribution to the interaction, including a subscale of items addressing the mother's “sensitivity to cues”), and “Child Total” (assessing the child's contribution, including a subscale of items addressing “clarity of cues”). The NCAT is theoretically grounded in the Barnard model (138, 139) conceptualising the caregiver-child interaction as a reciprocal dialogue in which quality is defined and created by the contributions of both participants (140). The NCAT has acceptable internal consistency for the composite scales with Cronbach's alphas of .87 for “Caregiver Total”, .81 for “Child Total”, and .88 for “Caregiver/Infant Total” (141). A normative database has been established for the NCAT using a large US sample of 1,887 dyads from a range of ethnic, educational, and familial backgrounds and this has been found to be appropriate for other culturally diverse Western populations (137). Applied from Wave 6–10 the NCAT was administered in mother's homes, using video of dyad interactions addressing child age-specific tasks. Pre and post assessments were balanced using different annually certified Mental Health Clinicians all of whom were accredited through a three-day structured training program to apply the tool for clinical and research purposes having achieved inter-observer reliability score of >90% (142).
4. Analyses
Data were analysed using IBM SPSS Statistics Version 25. Paired samples t tests were employed to assess change from pre to post measures for the standardized tools with a two-tailed statistic used as more conservative test, and effect sizes are presented using Cohen's d (143). More vulnerable subgroups of mothers identified from the literature were considered individually, and where samples were relatively small (20 cases or less), a robust bootstrapping technique was employed and the bias corrected and accelerated 95% confidence interval (BCa 95% CI) estimated (144, 145). Where available, scores are compared with normative data for interpretive purposes. A “reliable change index score” (146) was applied for the KPCS to determine clinically meaningful changes in PPSE. A clinically significant improvement in depression from a clinical to non-clinical score for the PHQ-9 was also calculated by obtaining a post-treatment score of ≤9 combined with an improvement of 50% or more (131).
While some mothers went on to repeat the program (including twelve who had originally withdrawn from it), the findings presented are for the first attendance of the Acorn program to provide clear indications of its worth as a single intervention for the targeted population. Where completing mothers had two children attending Acorn, unless otherwise stated the figures refer to their youngest child for clarity.
5. Results
5.1. Client participation & profile
The total number of enrolled mothers (Ne) to the program was 493 (Mean age 30.8 years, SD 5.6) with 520 children (mean age 9.1 months, SD 7.1). The number of individual mothers completing the program (N) was 388 (78.7%), with 353 (71.6%) providing both pre and post measures of the client self-completion questionnaire (n). Of the 27 mothers who enrolled with two children, 19 completed the program. Mothers who completed the program are referred to as “Acorn mothers” in this paper. 105 (21.3%) mothers withdrew from the program. Reasons obtained for withdrawal from Acorn were largely innocuous and unrelated to the program although twenty-six mothers indicated a health reason for withdrawing. There does not appear to be a systematic reason for client withdrawal: the demographic and psychological profile of “withdrawing” mothers (depression, PPSE, Parenting Stress, BPD) was very similar to that of retained Acorn mothers, and the proportion of withdrawing dyads performing poorly in the pre-measure of the NCAT mirrored that of retained dyads. Withdrawal was not related to the geographical location of the group attended. Client personal objectives for attending Acorn were also very similar for withdrawing and retained mothers. Client withdrawal has declined over the duration of the program from 42.5% in Waves 1–4, to 23.0% in Waves 8–11.
The follow-up telephone survey of completing mothers yielded a response rate of 37.8% (135 mothers) - (62.8% of consenting mothers who could be contacted). The profile of interviewed mothers was very similar to that of the broader group of mothers although they were slightly older (M 31.7 years, SD 5.38) and more likely to have more than one child (44.0% vs. 34.8%, respectively).
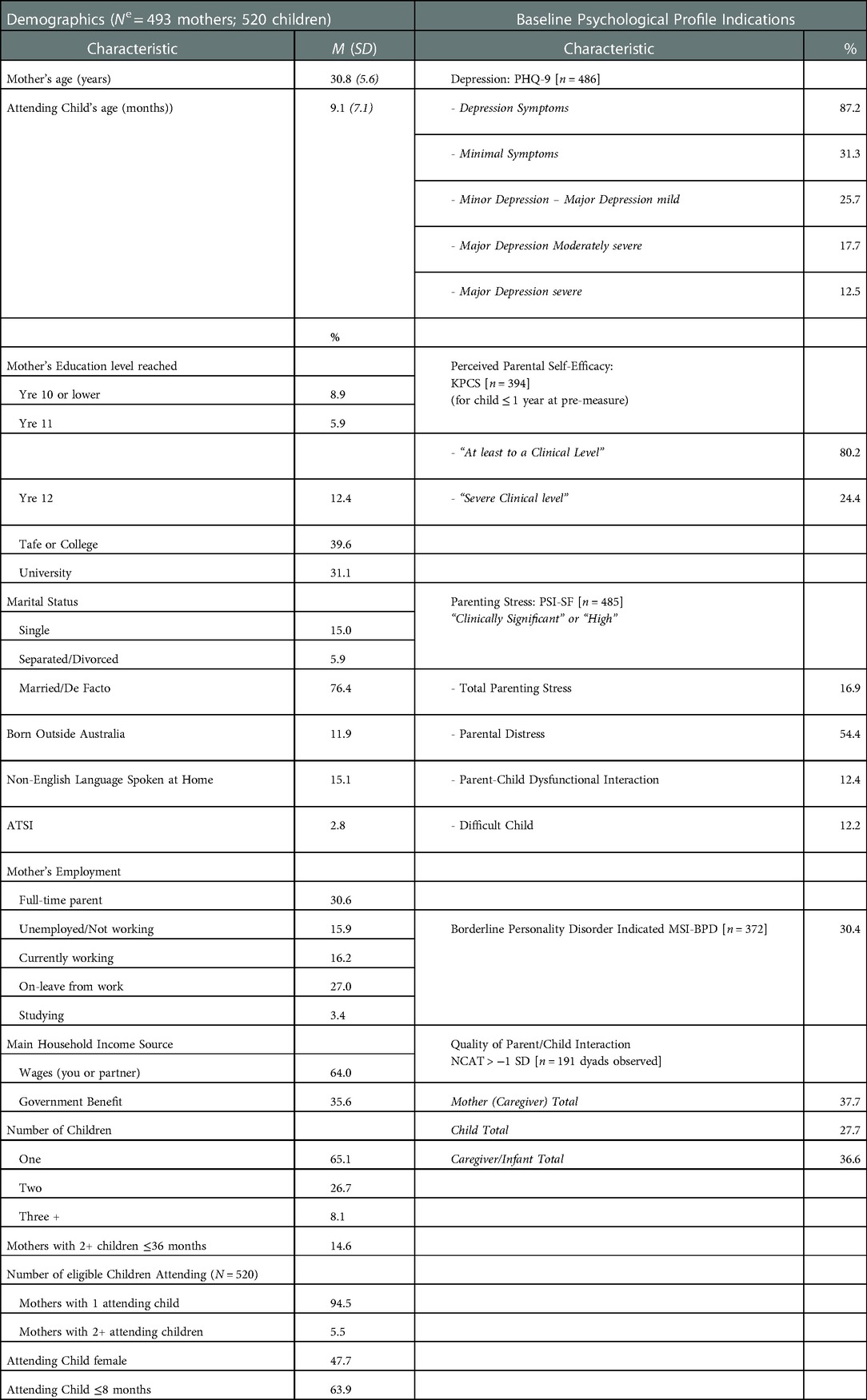
Acorn recruits a wide variety of participants from a broad spread of socio-economic, cultural, familial, and educational backgrounds, and has enrolled a profile of mothers where depression, poor perceived parental self-efficacy (PPSE), and high parental stress are overlapping causes of concern and which for many indicate the need for clinical intervention (Table 1). Nearly nine in ten mothers had symptoms of depression and 30.2% indicated moderate-severe major depression, of whom 84.5% (123 mothers) also indicated “clinically significant” or “high” levels of “Parental Distress”. One hundred and thirteen (30.4%) mothers indicated BPD on commencing the program from Wave 4, with 81 (71.6%) of these completing the program. Just under half of the 113 mothers who indicated BPD (49.6%) also indicated moderate-severe major depression. Acorn dyads scored relatively low in the NCAT observational scale addressing the quality of the parent-child interaction where 36.6% scored >−1 SD from the normative mean in their “Caregiver-Infant Total”.
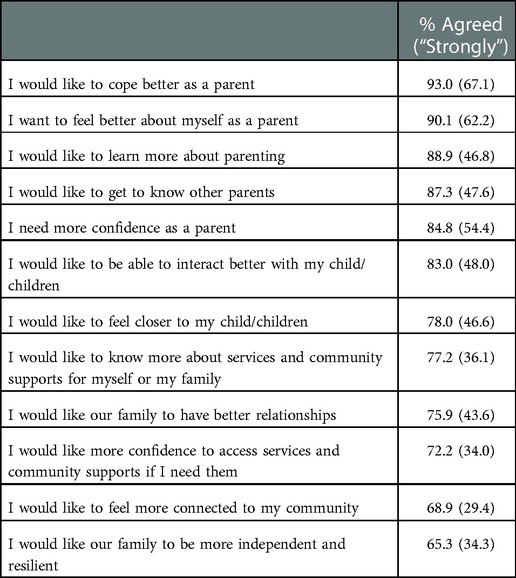
There is a clear alignment of intended program outcomes with the needs of its referred clients; most mothers endorsed a range of Likert statements relating to the Acorn program objectives as their own “personal objectives” for attending the program (Table 2).
5.2. Process evaluation
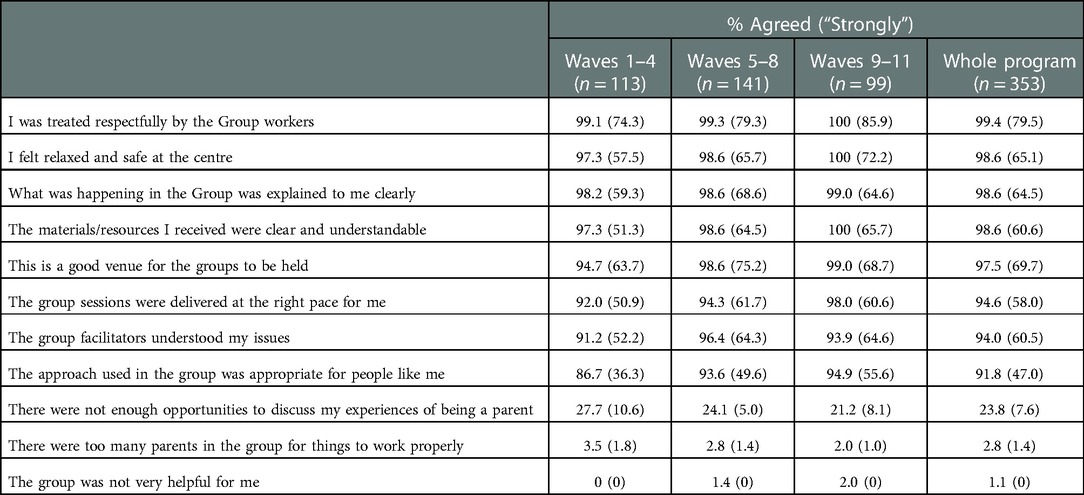
The median number of Acorn sessions attended was 11 (mode of 12). Attending families have engaged well with the program (Table 3). Over nine in ten Acorn mothers agreed that they felt relaxed and safe in the program and that the approach used was respectful and appropriate for them, with clear explanations provided by understanding facilitators using clear comprehendible resources at a suitable pace and venue. This included mothers indicating BPD where 96.3% (78 mothers) agreed they felt relaxed and safe (63.0% “strongly”).
While positive endorsement of the program was consistently high throughout the program, this improved as the program matured from Wave 5 and this was particularly notable in the increased proportions of mothers “strongly” agreeing with process items between the earlier Waves 1–4 and the later waves 9–11 in Table 3, with The approach used in the group was appropriate for people like me improving 19.3 percentage points between Waves 1–4 and Waves 9–11. Eighty-four mothers (23.8%) indicated they would have liked more opportunities to discuss their parenting experiences with this declining as the program matured and refinements where gradually implemented in the reflective journaling component; by Wave 11 three mothers agreed with this item (6.7%) and only one “strongly”.
Over eight in ten completing mothers considered all three principal components of Acorn to be either a “huge help” (for just over half of the attending mothers) or “quite a lot of help”, with 88.6% (312 mothers) indicating this for Dance Play, 86.4% for the Therapeutic Letters and 82.1% for the Reflective Journaling. Talking with other mothers was also considered “a huge help” or “quite a lot of help” by 82.7%. Despite the high rates of approval for the Acorn strategies throughout the program, the perceived helpfulness of strategies has improved as the program has matured and its delivery refined. Comparing Waves 1–4 with Waves 9–11, those indicating that Dance Play was “a huge help” increased from 48.2% to 58.6% and for the Therapeutic Letters from 49.6% to 61.6%. Those asserting that talking with other mothers was a “Huge help” improved from 38.1% to 56.6%. The perceived helpfulness of Reflective Journaling remained consistent throughout the program (54.0% and 54.5% respectively indicating this had been a “huge help”).
All but a single participating mother in the Acorn program indicated that they would recommend the program for other parents like them, with 265 (77.3%) indicating “Yes, with no changes”.
5.3. Outcome evaluation
5.3.1. Objective 1: to enhance the quality of the parent-child interaction
Significant improvement was evident across the NCAT dimensions addressing the quality of the mother-child interaction for the 145 dyads observed pre and post Acorn: “Caregiver-Infant Total” with a small-medium effect size (Mdiff = 2.67, t(144) = 4.39, p < 0.000, d = 0.37); “Caregiver Total” (Mdiff = 1.46, t(144) = 3.04, p < .01, d .29), and “Child Total” (Mdiff = 0.95, t(144) = 2.63, p = 0.01, d .25). Significant improvements in the “Caregiver-Infant Total” were also evident across the majority of “most” vulnerable subgroups considered including those where the mother indicated BPD on the MSI-BPD, (Table 4).
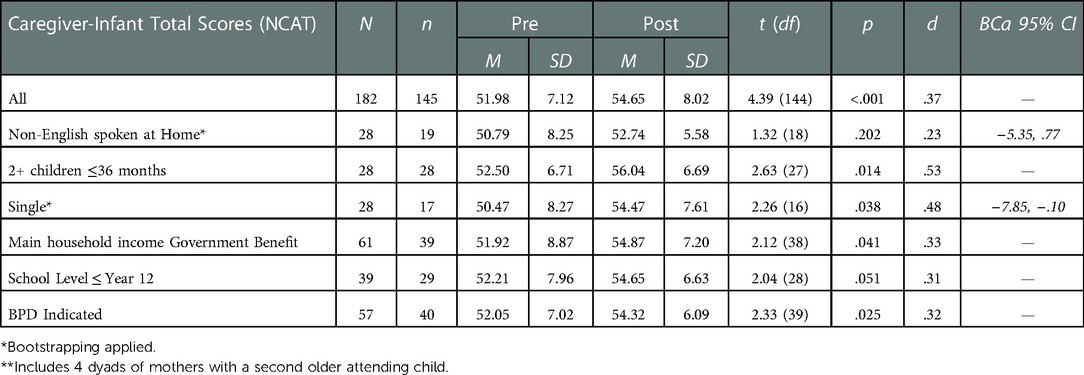
Table 4. Quality of parent–child interaction outcomes for acorn mothers and vulnerable subgroups (dyads)** waves 6–10.
For mothers there were also significant improvements with small effect sizes in: “sensitivity to cues” (Mdiff = 0.34, t(144) = 2.24, p < .03, d .24), and for children there was also significant improvement in “clarity of cues” which approached a medium effect size (Mdiff = 0.67, t(144) = 4.45, p < 0.00, d .41).
These improvements were reflected in reductions in scores >−1SD below the normative mean. Taking those dyads for whom pre and post measures were observed: for the “Caregiver-Infant Total”, 34.4% scored >−1SD below the NCAST population mean in the pre-measure and 24.8% in the post measure; “Caregiver Total” reduced from 35.2% to 31.1%; and “Child Total” from 27.6% to 17.2% respectively.
Improvements in the Child Total NCAT scores were reflected in the almost universal agreement (98.9%) that my child has benefitted from my attending the group, with nearly seven in ten mothers “strongly” agreeing with this item (Table 5). The strength of this response has improved over the duration of the program; those indicating “strongly agree” increased steadily from 65.4% in Waves 1–4 to 72.7% in Waves 9–11.
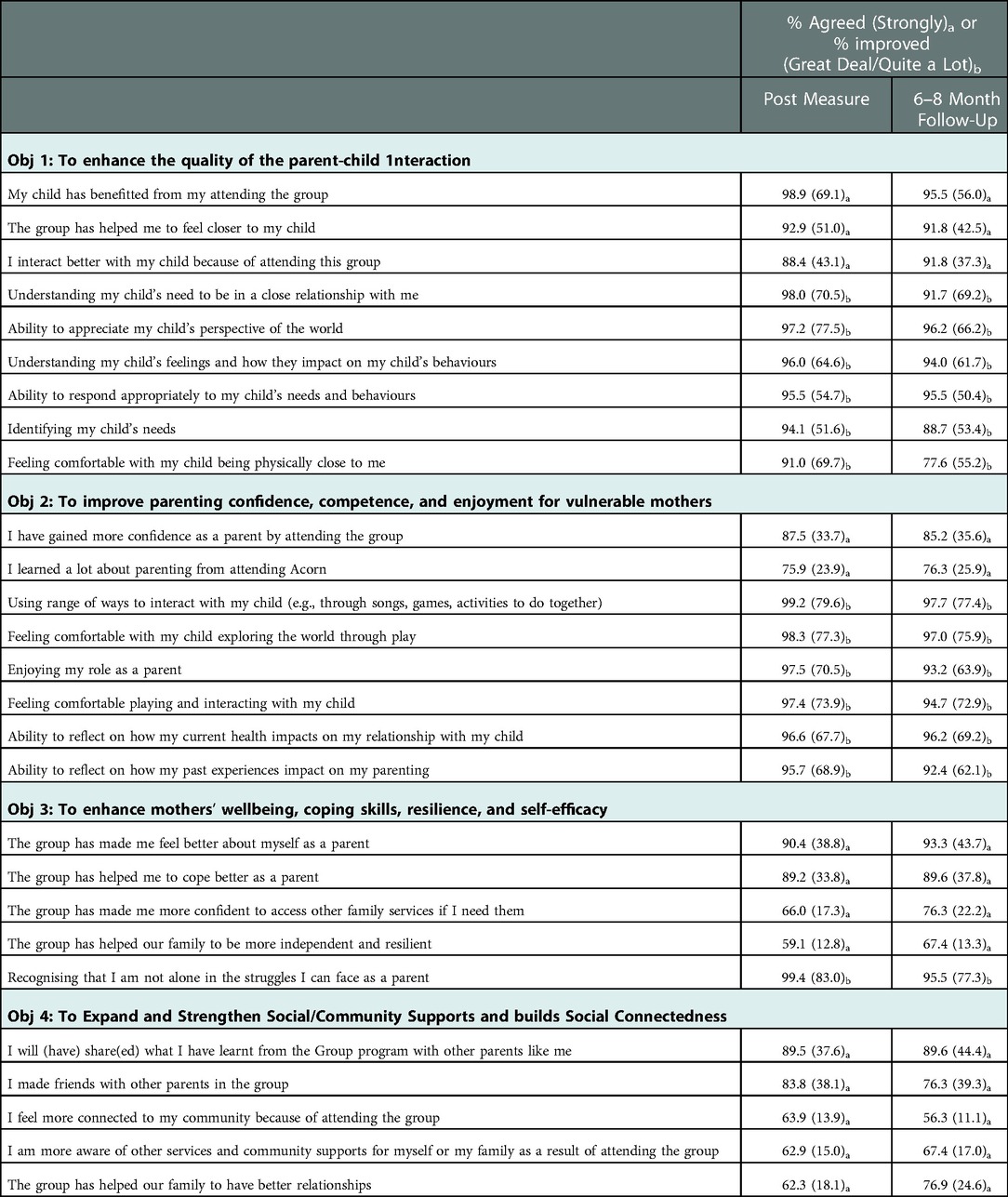
Table 5. Scaled responses: Acorn mothers self completion questionnaire post-measures (n = 353) & six-eight month follow-up interview (n = 135).
Over nine in ten completing mothers indicated that because of participating in Acorn they had improved across all items related to the quality of the parent-child interaction addressed in the Client Self-Completion Questionnaire (Table 5).
A culmination of improvements in these parenting areas may have resulted in 312 mothers (88.4%) agreeing (including 152 “strongly”) that I interact better with my child because of attending this group. The proportions of mothers strongly agreeing with this item improved as the program matured, from 37.2% in Waves 1–4 to 50.3% in Waves 9–11. Moreover, most mothers (328, 92.9%) indicated that the group has helped me to feel closer to my child (with 180 mothers strongly agreeing). Just over nine in ten mothers also agreed that they felt more comfortable with their child being physically close to them, with just under seven in ten indicting this had improved “a great deal” or “quite a lot.” The above improvements were also consistently reported by mothers six-eight months after completing the program providing indications of sustained program impact in these areas.
These findings were also similar in relation to those 19 completing mothers who brought a second older child to Acorn, with 78.9% agreeing that I interact better with my child because of attending this group (7 “strongly”), and 84.2% indicating that the group has helped me to feel closer to my child (8 “strongly”).
5.3.2. Objective 2: to improve parenting confidence, competence, and enjoyment for vulnerable mothers
The desire to improve parenting confidence was specifically indicated by 84.8% of attending mothers with over half feeling this strongly prior to attending the program. On completing Acorn, 309 mothers (87.5%) indicated that I have gained more confidence as a parent by attending the group (one third “strongly” agreeing) with this applying equally to parents of older and younger eligible children completing Acorn. Strength of agreement improved as the program matured, from 23.9% “strongly” agreeing in Waves 1–4, to 43.4% in Waves 9–11. Reported improvements in parental confidence was sustained six-eight months after completing the program with a slight shift toward strongly agreeing that this was the case.
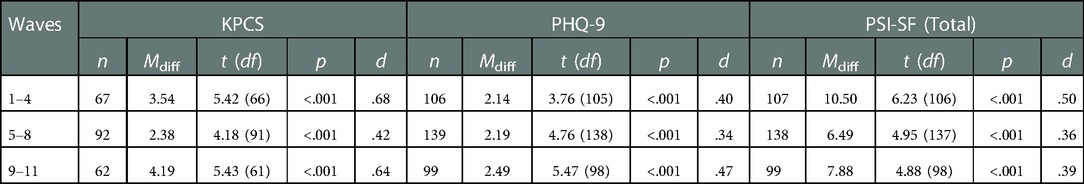
This improvement was mirrored in findings from the KPCS for those 221 mothers with children who were aged one year or less on completing the program. Perceived parental self-efficacy (PPSE) has significantly and substantially increased for mothers attending Acorn with a medium effect size (Mdiff = 3.24, t(220) = 8.55, p < .0001, d .56). Taking those for whom pre and post measures were available, the proportion of mothers in the “non-clinical” range more than doubled in the post-measure (from 17.6% to 35.7%) and the proportions of mothers in “severe clinical range” more than halved (from 24.9% to 9.5%). Sixty (27.1%) mothers improved their scores by six or more points on the scale in the post measure signifying a “clinically reliable improvement” (146) in PPSE. Significant improvements in PPSE were found for the diversity of more vulnerable Acorn mothers (Table 6) and particularly for those who also had additional children aged 3 years or less, where the effect size for their youngest child was large (d .75). Significant improvements in PPSE occurred consistently with medium effect sizes at different time groupings across the 5.5 years duration of the program (Table 7).
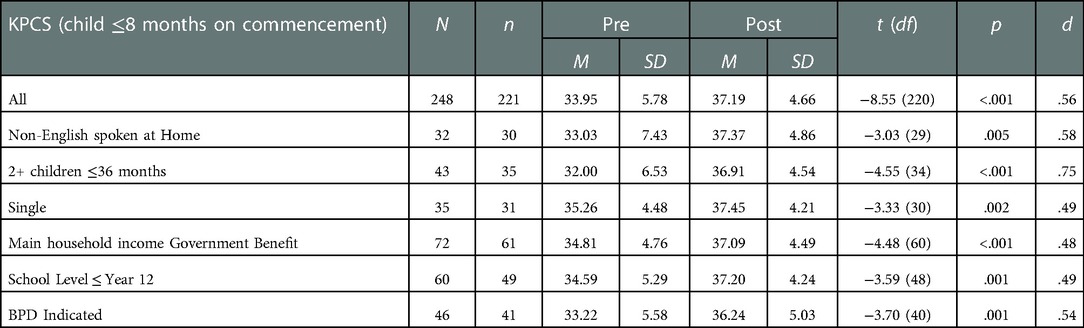
Table 6. Perceived parental self-efficacy (PPSE) outcomes for acorn mothers and vulnerable subgroups.
268 Acorn mothers (75.9%) indicated they had learned a lot about parenting from attending Acorn, with 103 (76.3%) reaffirming this in the follow-up measure. Nearly all Acorn mothers (99.3%) indicated improvement in Using a range of ways to interact with my child (e.g., through songs, games, activities to do together) because of attending Acorn with 281 (79.6%) indicating “a great deal” or “quite a lot” of improvement. This was more pronounced for the second older attending child with 89.5% (17 mothers) indicating “a great deal” or “quite a lot” of improvement in this area. Over 9 in 10 Acorn mothers indicated they had improved across all of the remaining items addressing Objective 2 as a result of attending the program, with this being sustained 6–8 months later (Table 5).
Taking the 108 Acorn mothers who completed a post-measure and had older children (of any age) who had not attended Acorn, when asked has Acorn helped with your parenting for any other children who did not attend, 95 (87.9%) indicated in the affirmative with 40 (37.0%) indicating “a great deal”. Of the 47 mothers with older non-attending children who completed the follow-up interview, 33 (70.2%) indicated the program had helped in this area with 14 (29.8%) indicating “a great deal”.
Over 9 in 10 Acorn mothers reported improvements in both their Ability to reflect on how my past experiences impact on my parenting (with 242, indicating this improved “a great deal” or “quite a lot” because of attending Acorn), and their Ability to reflect on how my current health impacts on my relationship with my child (with 239, 67.7% indicating “a great deal” or “quite a lot” of improvement). These positive reported outcomes were consistently indicated six-eight months after completing the program (Table 5).
5.3.3. Objective 3: to enhance mothers' wellbeing, coping skills, resilience, and self-efficacy
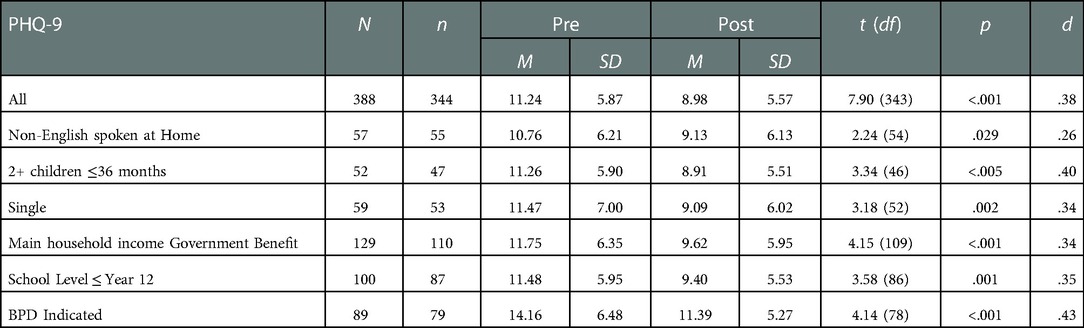
There are strong indications that the Acorn approach has provided holistic wellbeing benefits for engaged mothers. The PHQ-9 has demonstrated significant improvement in depression scores pre and post Acorn with a small-medium effect size (Mdiff = 2.27, t(343) = 8.90, p < .0001, d .37). All of the vulnerable subgroups considered improved their PHQ-9 scores significantly with small to medium effect sizes (Table 8). While mothers with BPD scored highest in both pre and post measures of depression, this reduced significantly with the largest effect size d.43. Improvements were significant at different time points throughout the program (Table 7). Clinically significant improvement (from a “clinical” to “non-clinical score”) were calculated for the 190 mothers scoring in the clinical range in the PHQ-9 pre-measure for whom post-measures were obtained; 50 of these mothers (26.3%) met these criteria for “clinically significant” improvement.
Taking those mothers who provided both pre- and post-measures, the number of Acorn mothers with “Minimal” or “No” depressive symptoms improved to a majority in the post-measure from 154 (44.8%) to 212 (61.7%); the number of mothers with no symptoms doubled to just over one in four. Reductions in “Major Depression moderately severe to severe” were also evident, from 97 (28.2%) indicating this in the pre-measure to 60 mothers (17.4%) in the post-measure. Those finding coping with their depressive symptoms “very” or “extremely” difficult also reduced by more than half, from 101 (29.4%) to 43 (12.5%).
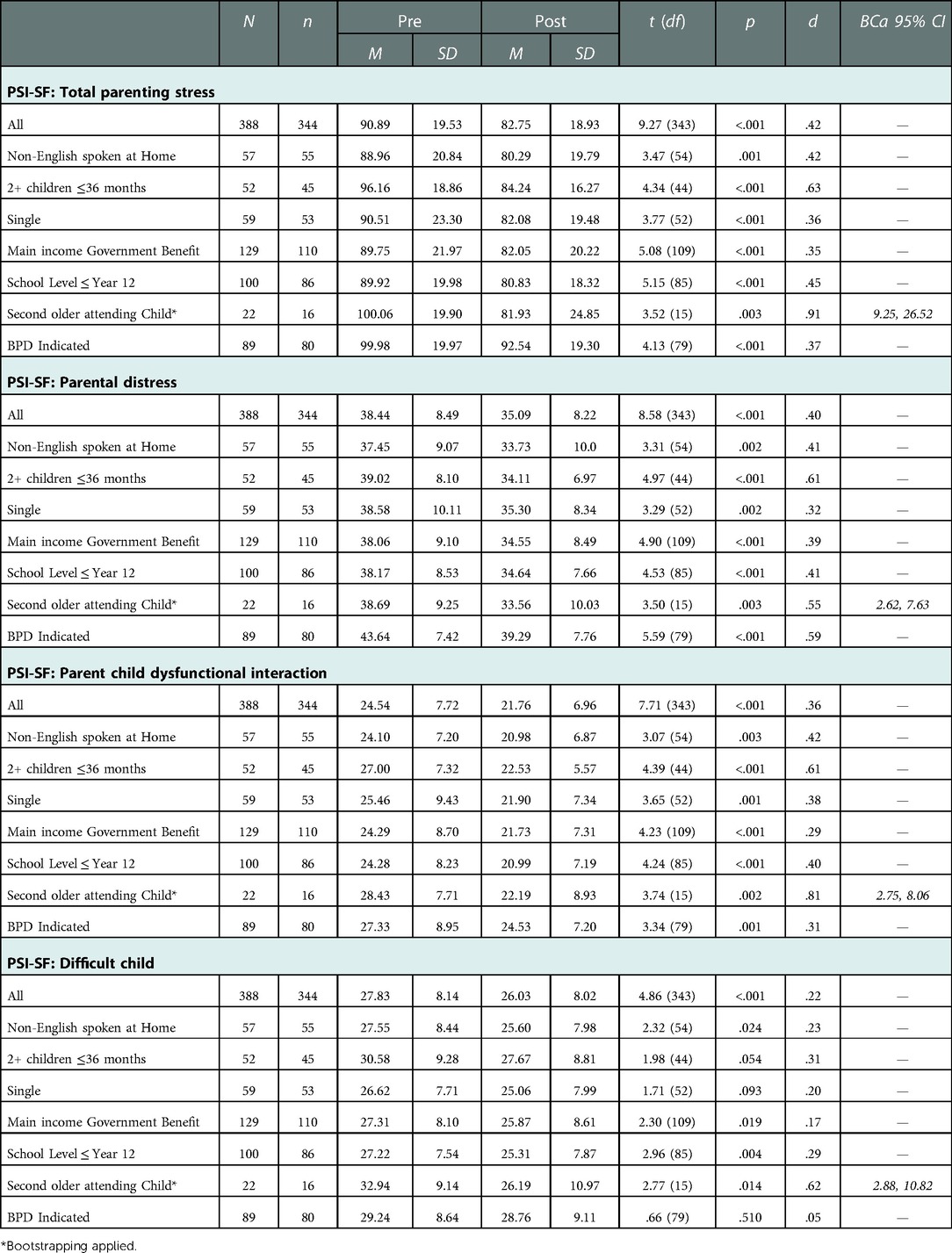
There has also been a clear significant improvement for Acorn mothers in “Total Parenting Stress” and in each of the PSI-SF domains (Table 9). Taking those for whom pre and post measures were obtained, the numbers indicating “clinically significant” or “high” for “Total Parenting Stress” halved from 60 (17.4%) to 30 (8.7%), and for “Parental Distress” (the most prevalent stress related issue for participating mothers), the numbers in these levels moved from 190 (55.2%) to 144 (41.9%). These significant improvements with effect sizes ranging from medium to large were evident for a range of “most vulnerable” subgroups of Acorn mothers including those whose household income was mainly Government benefit and those with lower educational levels. Sixteen Acorn mothers scored in the 96th percentile or higher in the pre-measure of the “Parent-Child Dysfunctional Interaction” scale with this reducing to 4 in the post-measure.
Mothers who brought two children to the program appear to have benefitted most across the domains addressed by the PSI-SF with higher effect sizes evident in relation to both their younger and older attending children. “Total Parenting Stress” was noticeably higher in relation to the second older attending child on commencing Acorn but this improved substantially. Applying the bootstrapping technique, there was on average a decrease in this score from pre (M = 100.06, SE = 4.98) to post (M = 81.93, SE = 6.21), and this difference of 18.13, BCa 95% CI [9.25, 26.52] was significant t(15) = 3.52, p = .003, representing a large effect size d = .91.
Nearly nine in ten mothers indicated that the program has helped me to cope better as a parent, with 119 (33.8%) indicating “strongly agree” with this item. This included mothers indicating BPD with 72 (88.9%) agreeing that Acorn had helped them in this regard (30.9% “strongly” agreeing). The proportions of completing mothers “strongly” agreeing with this item improved as the program matured from 23.4% in Waves 1–4 to 40.4% in Waves 9–11. 319 (90.4%) mothers indicated that the group has made me feel better about myself as a parent (38.8% “strongly”) including 71 mothers indicating BPD (87.7%) with 29 (35.8%) of these mothers “strongly” agreeing.
While 233 (66.0%) endorsed the item, Acorn mothers were less likely to agree that the group has made me more confident to access other family services if I need them, with this lower level of agreement being partly explained by some mothers expressing existing confidence in this area prior to Acorn; this may be related to the fact that all mothers were referred to Acorn by existing services with which they had some degree of engagement. However, enhanced confidence to access suitable family services appeared to improve after completing Acorn and was accompanied by the almost universal recognition among Acorn mothers that I am not alone in the struggles I can face as a parent; 293 (83.0%) mothers indicated this had improved “a great deal” or “quite a lot” by the end of the program and 77.3% indicated this level of improvement six-eight months later.
While around one third of mothers did not indicate a desire to improve family independence and resilience prior to beginning the program, most mothers in the post-measure (208, 59.1%) indicated that the group had helped in this area and this appears to have improved months after completing the program (67.4%). There were sixty mothers indicating BPD who expressed the wish for their family to be more independent and resilient at the beginning of Acorn and thirty-eight of these (63.3%) agreed that the group had helped them in this regard in the post-measure.
5.3.4. Objective 4: to expand and strengthen social/community supports and build social connectedness
Over eight in ten (295 mothers) agreed I made friends with other parents in the group, with 134 (38.1%) strongly agreeing this was the case. Strength of agreement improved as the program matured (from 33.9% “strongly” agreeing in Waves 1–4 to 44.4% in Waves 9–11) and was sustained 6–8 months later (Table 5). For mothers indicating BPD, 77.8% agreed they had made friends, and 39.5% strongly agreed this had occurred. Of the 53 single mothers who completed Acorn, 79.2% (42 mothers) agreed they had made friends at the end of the program, 34.0% “strongly”. Of the 56 completing mothers who spoke a language other than English at home, 78.6% (44 mothers) agreed they had made friends at the end of the program, 35.7% “strongly”.
Acorn has been more successful in fostering relationships and connections between attending mothers than in enhancing feelings of connectedness to their communities. However, 224 mothers, (63.6%) indicated I feel more connected to my community because of attending the group, with this proportion being similar for mothers indicating BPD (66.7%). Most mothers continued to endorse this change and attribute this to Acorn six-eight months after the program (Table 5).
It was also the case that 314 mothers (89.7%) indicated they “will share” their learnings from the Acorn program with their peers, and confirmation that this intention was enacted was indicated in the follow-up measure with 121 (89.6%) agreeing I have shared what I have learnt from the group program with other parents like me, (with just under half of these strongly agreeing this item). The intention to share learnings from Acorn were also signified by 82.1% of mothers from households that spoke a non-English language at home (41.1% “strongly” agreeing), and by single mothers (90.6%, and 30.2% respectively). Confirmation from these groups that this had occurred 6–8 months later was provided by 81.1% of non-English speaking household mothers and 77.8% of single mothers.
Most Acorn mothers (220, 62.3%) indicated that participation in the program has helped our family to have better relationships, and this appears to have improved over time; taking those 122 mothers for whom both post, and follow-up measures are available, 58.2% of these mothers indicated Acorn had helped to improved family relationships in the post measure with this increasing to 76.9% in the follow-up measure.
5.4. Program effects and attendance
The extent to which program attendance effected outcomes was explored by considering the 21 mothers who completed Acorn and provided pre and post Client self-completion questionnaires but attended 7 sessions or less (just under half the program). The profile of these mothers was very similar demographically to the larger group of mothers. Applying paired sample t tests for all psychometric scales where pre and post scores were available for these mothers, significant improvements were found for all the PSI-SF measures: “Total Parenting Stress” (Mdiff = 15.37, t(18) = 3.50, p < .005, d .76); “Parental Distress” (Mdiff = 6.00, t(18) = 4.00, p < .001, d .63); “Parent-Child Dysfunctional Interaction” (Mdiff = 3.16, t(18) = 2.51, p < .05, d .45); “Difficult Child” (Mdiff = 4.58, t(18) = 2.17, p < .05, d .49). However, improvement in depression scores was not significant for these mothers, and for the 16 mothers whose children were aged 1 year or less Perceived Parental Self-Efficacy (KPCS) did not improve significantly. Only two of the mothers who had attended 7 times or less completed pre NCAT observations. Mothers who completed the program but attended less than half of the Acorn sessions reported improvements across all the indicators addressing each objective listed in Table 5 which largely mirrored the answers supplied by the broader group.
6. Discussion
It has been documented that group-based interventions addressing maternal mental health can record poor attendances with high drop-out rates (69). However, despite the requirement to commute to the program at set times each week with their child(ren), Acorn has successfully encouraged engagement for the majority of even the most vulnerable of its targeted population many of whom living with profound comorbid mental illness. The program is meeting the needs of its client base with its objectives clearly aligned with mothers' personal objectives for attending, and Acorn mothers broadly acknowledged and appreciated the helpfulness and delivery of the program's three principal components. From the Acorn mothers' perspective, the program has provided an environment that felt safe, appropriate, and respectful, with clear resources and explanations, using facilitators who were almost universally perceived as understanding of client issues, and presenting opportunities for group-based peer support. Many of these program delivery elements harmonise with previously identified service provision wishes of mothers experiencing postpartum mental illness (147). Subsequently, Acorn mothers almost universally indicated they would recommend the program to their peers after completing Acorn, and most indicated they had shared learnings with peers six-eight months later. The importance of client preference in choosing appropriate mental health therapies in order to optimise their engagement has been highlighted (148), and the willingness of Acorn mothers to discuss their experiences of this valued program with peers may have broader benefits in terms of extending its reach to those who may otherwise be more difficult to engage, including those from linguistically diverse backgrounds (149).
The program has blended evidence-based strategies that have successfully enhanced the quality of the mother-child interaction. NCAT observations applied to mother, child, and their interaction, found significant improvement evident in all three measures and these were triangulated with mother's self-reports which indicated related beneficial and lasting improvement. It is also noteworthy that the NCAT “Caregiver Total” has strong predictive validity with measures of “maternal support”, and measures of “maternal reflective functioning” (63, 137, 140, 141), and the latter is consistent with Acorn mothers' self-reports of improved ability to reflect on the impacts of their past experiences and current mental health on their relationship with their child and their parenting. “Caregiver-Infant Total” scores have been found to predict security of attachment (150) and improvements in this measure of the quality of the dyad interaction were significant across a range of “most” vulnerable subgroups taken from what can be considered an already vulnerable target population of mothers and children. Meta-analysis has also established the NCAT as a reliable outcome measure for interventions addressing parent sensitivity (151); a central parenting concept in attachment theory and a key determinant to promote parent-child attachment (37, 152). There were significant improvements in the subscale “sensitivity to cues”, and while this should be interpreted with some caution, this is consistent with the three more reliable composite scales and self-reported improvements in identifying their child's needs and responding appropriately. While the above improvements are encouraging across NCAT measures, many of the dyads began the program at a low baseline level and around one quarter of the dyads remained >−1 SD below the normative mean in the “Caregiver-Infant Total” post-measure. However, it was noteworthy that improvements in the child interactive behaviours with their mother were substantial and resulted in similar proportions scoring >−1SD in the “Child Total” post-observations to that of the normative population. This was largely influenced by significant improvements in the child's “clarity of cues” during the interaction which may be attributed to their engagement in Acorn dance play activities.
However, improvements in the quality of the dyad interaction were not found to be significant for those who spoke a language other than English at home. Interpretation of why the “non-English speaking household” dyads did not improve significantly is problematic; this finding contrasts with the significant improvements found for this subgroup in PPSE, and their self-reported improvements in parenting interaction. For example, 89.3% of mothers from non-English speaking homes agreed that they interacted better with their child because of Acorn in the post measure (39.3% “strongly”), and 100% that the group had helped them to feel closer to their child (50% “strongly”). However, this small NCAT group of 19 observed dyads were culturally heterogeneous (speaking 7 different languages at home), and while the NCAT has been successfully applied with some ethnic communities it is possible that cultural barriers to be being observed and videoed with their children may have influenced behaviour for some of these dyads.
The large majority of mothers indicated that they interacted better with their children because of the program, that their child had benefitted, and that the program had helped them feel closer to their child, and these positive indications endured six-eight months after completion. These benefits were also evident regarding the second older attending child to the program, and mothers almost universally indicated that the program has helped in their parenting of other non-attending children. The majority of Acorn mothers reported improving substantially across a range of parenting qualities including understanding their child's needs, feelings, and perspectives of the world and enhancing their ability to respond to their child appropriately, with these being reaffirmed six-eight months after leaving Acorn. Given the difficulties maternal mental illness can impose on mother-child interaction the above self-reported improvements are notable. These were accompanied by widespread reporting of improved (and sustained) parental confidence along with significant improvements in perceived parental self-efficacy (PPSE) with medium effect sizes for Acorn mothers across all the vulnerable subgroupings considered, including those for whom Government benefits were the main source of household income and those with low formal education (known moderators of the effects of maternal mental illness on parenting behaviour). Given the importance of PPSE for successful parenting and its relationship to actual parenting competence this is very encouraging and supports the substantial reported improvements in parental competence indicated by over 9 in 10 Acorn mothers both on completing the program and six-eight months later. These included employing a range of new ways to interact with their child, and feeling more comfortable with interactive playing and child exploration.
The standardized tools applied in this evaluation provide clear evidence that the well-being of most mothers attending Acorn has improved in the dimensions addressed. Additional self-reported indications provided after program completion and six-eight months later corroborate this improvement with mothers attributing this to their participation in the program. Many reported that they felt better about themselves as parents and were better able to cope as a parent (with substantial numbers also indicating that they were more able to cope with their depressive symptoms on the PHQ-9). While many participating mothers experienced clinically significant improvements in depression and PPSE, we support the view that in promoting the wellbeing of mothers with mental illnesses, reducing sub-clinical symptoms for mothers with mental health difficulties is also important (153) and this was broadly evident. In reference to the mental health movement conceptualisation of mental health “recovery” as a personal process above and beyond symptom relief, and involving the restoration of functioning (154), the burden of evidence here attests to the value of the Acorn program. Moreover, given the known protective buffering effects of improved parent-child relationships and parental confidence, it is likely that for those mothers experiencing on-going maternal mental health issues, there are still benefits acquired from the program in terms of well-being improvement and reducing possible detrimental impacts of their mental health problems on their children.
There were also significant improvements in “Total Parental Stress”, and in the “Parental Distress”, “Parent-Child Dysfunctional Interaction” and “Difficult Child” dimensions addressed by the PSI-SF, with those mothers who brought a second older eligible child to the program appearing to acquire greater benefit from the program in relation to this older child. Improvement in these dimensions of parental stress were identified across the vulnerable subgroupings considered. However, for the “Difficult Child” subscale, single mothers and those with two children aged 36 months or less did not reach statistically significant levels of improvement for their youngest child, although this was marginal (p = .093 and p = .054 respectively). In the latter case, there were 29 completing “Acorn mothers” with an older eligible child who did not attend Acorn. Given that the largest effect size for “Difficult Child” improvement was in relation to mothers with a second older attending child, further measures to encourage mothers to bring all their eligible children to the program could prove beneficial in this dimension. “Difficult Child” addresses the mother's perception of the child's temperament, defiance, noncompliance and demandingness, but this can be influenced by “external” factors (155), and it is possible that latent influences on the perceptions of some single mothers has dampened program impacts for this measure. More notably however, there was no significant improvement in the “Difficult Child” measure for mothers indicting BPD following participation in Acorn. Mothers with BPD have been found to be more likely to perceive their parental stress as being related to their child (156), and as many of the Acorn mothers indicting BPD were not previously diagnosed, it is possible that they had low knowledge of their illness and little insight into its possible influence on these perceptions making improvement in this area for these mothers more challenging. However, 80.0% of those Acorn mothers indicating BPD, scored within “normal” limits in the post-measure for the “Difficult Child” scale. It is also noteworthy that 12 of the 16 Acorn mothers who scored above the 96th percentile in the “Parent-Child Dysfunctional Interaction” scale pre-measure improved their score to move away from this indication of potential child abuse in the post-measure (130). This unexpected outcome highlights the importance of significant improvements evident in this dimension for Acorn mothers as a whole and for all of the vulnerable subgroups considered.
Improvements in family relationships, independence and resilience were also noted by most mothers with indications that these continued to improve months after the program was completed. This suggests that for some mothers, these improvements may have taken time to come to fruition after the program, but that where this was the case, these mothers nonetheless still identified and acknowledged the role of Acorn in helping this to happen. There is evidence that mental health programs that include partners benefit families (46) and future program adaptations in this regard could be considered. However, taken with the indications that Acorn had helped mothers in their parenting of non-attending children, participation in the program already appears to have precipitated improvements in family life for substantial numbers of engaged women.
Social connectivity has been enhanced and sustained for Acorn mothers including for those subgroups who may experience greater levels of social isolation, and improved recognition that participants were not alone in their parental struggles was broadly indicated following Acorn. This finding addresses an identified need for interventions that nurture social connectedness for migrant mothers of young children revealed in recent qualitative work (157). Assembling mothers with shared parenting and mental health issues and engaging them in collective interactive group activities has encouraged friendships to develop for over 8 in 10 participants including single mothers, mothers indicating BPD, and those speaking a language other than English at home. This has met a personal objective for attending Acorn for most participants and most considered being able to talk to other mothers in the group to be a “huge help”. Many of these friendships have continued; similar proportions of mothers indicated this in the follow-up interviews and around 4 in 10 “strongly” agreed this was the case. These outcomes are pertinent given evidence that improving social connectedness benefits mental health generally (158, 159) and depression specifically (160–163). There is also qualitative evidence that access to peer support promotes emotional wellbeing for mothers experiencing perinatal mental illness by helping to alleviate isolation, guilt and stigma (165). Given that there are known associations of social isolation and disconnect with maternal mental ill health, the program has clearly provided benefits in this regard.
Finally, Acorn mothers attending less than half of the Acorn sessions appear to still benefit from the program, notably in reducing dimensions of parental stress, and across the range of self-reported measures but not in significantly in PPSE or their depression measure. While small numbers render interpretations tentative, clearly mothers who for whatever reason cannot attend the whole program are still experiencing positive outcomes. While these mothers attended less sessions, their attendance was however spread over the duration of the program, allowing time to enact strategies at home at their own pace between attended sessions. It is also the case that providing the current program over the three months may be particularly important as most Acorn mothers were unable to attend all 15 sessions.
7. Study limitations and strengths
The identification of an appropriate instrument to observe the quality of the parent-child interaction was problematic, and we were particularly concerned to avoid a potential disincentive to participation for targeted mothers known to be difficult to engage. Once selected, the need for training and accreditation for Mental Health Clinicians to apply the NCAT in the homes of participants further delayed its application and its adoption also required substantial additional resources and time. Following a change of management and staffing at the host agency, the NCAT was not applied in Wave 11. However, the demographic and psychological profile of the 145 dyads completing these observations was very similar to that of all attending mothers, and this tended to be consistent across all Acorn waves (a consequence of maintaining consistent referral pathways over the duration of the program).
We were mindful of overburdening or alienating vulnerable women in the community setting with the demands of evaluation and focused specifically on tools that addressed the objectives of Acorn. The program did not screen for substance use disorder, and while the clinical diagnosis of psychotic disorder was an exclusion criterion, the program relied on referrers to identify this condition. We did not screen for bipolar disorder, the presence of which may interfere with the score for the MSI-BPD (136). We did not measure post-traumatic stress disorder or anxiety, and while we asked Acorn mothers about resilience in their family, we did not apply a quantitative measure of client resilience which we explored qualitatively as part of a supplemental study (165). We decided to screen for BPD in Wave 4 following revelations in the Critical Reference Group that some referred mothers leaving hospital had been diagnosed with this condition. It has been estimated that up to 23% of those who use outpatient psychiatric services have BPD (166) and given our findings that 30.4% of enrolled mothers indicated BPD, the prevalence of this condition among mothers with maternal mental ill health may be higher. There are of course a range of alternative tools and dimensions which could have been included to measure “wellbeing” and these could be usefully explored in the future.
Comparisons between post-measures and follow-up interviews employed different methods to obtain responses from Acorn mothers. It is possible that respondents may have been more inclined to provide positive answers in the follow-up because of these being elicited in an interview as opposed to the demonstrable anonymity of a self-completion questionnaire. However, given that the interviewer for the follow-up was independent, and that all mothers were clearly informed their responses and names would remain strictly confidential, participants had little motivation to provide misinformation about positive outcomes in their personal lives attributed to participating in a program they had completed months earlier. Moreover, it may have been expected that the perceived impact of a program would wane over time or possibly a contrast effect might occur whereby current impacts would be judged inferior in comparison to the largely positive impressions experienced immediately after the program. However, arguably the most striking finding has been the consistency of responses between the two measures taken six to eight months apart, and we are confident that this consistency coupled with the above considerations have yielded authentic responses from mothers.
We employed an action research design for this evaluation which precluded using a comparison/control group. Given the heterogeneity of the client base, the range of impacts sought reflected in the objectives, and the combination of different program strategies to achieve them, the importance of utilizing the evaluation formatively was recognised in anticipation that program processes and outcomes would need to be monitored closely to inform potential program revision. There were ethical concerns raised by stakeholders about withholding the intervention from some vulnerable mothers and their young children for the purpose of establishing a comparison group. There was no “waiting list” available as the program expanded to accommodate all referrals. Causal attribution was premised on triangulating mixed methods addressing a range of dimensions germane to parental wellbeing and the quality of the parenting relationship articulated in Acorn's program logic. Participant own judgements of causality were obtained through the Client Self-Completion Questionnaires and through follow-up interviews in which former clients could personally reflect on how the program had (or had not) achieved its objectives in relation to their own lives. A range of deeply personal positive improvements were broadly attributed to the program, and often strongly indicated. Given the profound challenges experienced by Acorn mothers in the most intimate of their human relationships, providing this evidence supports the effectiveness of the Acorn program. While future studies may be able to include a waiting list control or randomised control design to establish efficacy, the case that the Acorn program has achieved its stated goal and objectives is strongly supported by this evaluation.
There are several strengths to this study. The action research design of the evaluation enabled on-going monitoring, timely feedback, reflection and refinements to be integrated into this community program over a long period of time between “Waves” of delivery. The evaluation design also enabled the service providers to be enlisted in the efficient collection of data across the geographically dispersed groups of this multi-site program. While the three principal components remained constant throughout, supplemental adjustments to the program, its delivery and its evaluation were flexibly facilitated resulting in a matured program model detailed in its completed Manual (116). Participant indications of process improvements resulting from this endeavour over the duration of the program are evident, and particularly improved client engagement and retention as the program matured. This was accompanied by consistently highly significant improvements across the three applied standardized self-completion measures throughout the duration of the program (Table 7). It is notable that the effect size for each of the these measures tended to be lower around the middle of the program during Waves 5–8, a period when three Mental Health Clinicians left the program and were replaced with new workers who required a period of induction. However, the strength of self-reported positive endorsement clearly improved in terms of perceived child benefits, improved parent-child interaction, improved parental confidence and coping, and establishing friendships. We therefore conclude that these process and outcome improvements are related and were nurtured by the formative use of action research in the evaluation.
The application of mixed methods in this study has provided comprehensive, consistent and triangulated evidence of the suitability of the program and its array of lasting beneficial impacts. The inclusion of direct standardized observations of the quality of the parenting interaction also answers the call to implement measures of parenting quality which are not wholly reliant on mothers' self reports (85) and for studies that treat depressed mothers to include measures that address benefits for children (76). A major strength of this study is the exploration of a range of program impacts for a heterogeneous community with sub-analyses addressing known at risk groups.
8. Conclusion
The evaluation findings lend support to growing evidence of the benefits of psychotherapy approaches to enhancing mental health wellbeing in community settings (69, 167–169). Moreover, this evaluation demonstrates that by integrating specific evidence-based strategies within a holistic group-based community program that addresses both maternal mental health wellbeing and the mother-infant relationship, substantial benefits to both can be acquired for a diverse population of mothers and a range of specific “at risk” groups of vulnerable mothers experiencing mental health issues, their children and families. To our knowledge this is the first study that examines the effectiveness of a single program for the range of subgroups of mothers with maternal mental health issues we have identified. Many mothers in this study had mental health difficulties which could be considered to be at the severe end of the spectrum, and while some dyads may require further support, the Acorn program has succeeded in its goal of holistically nurturing and enhancing the wellbeing of those most vulnerable of mothers experiencing maternal mental illness and promoting a sustained quality of their relationship with their children. All Acorn mothers were referred by existing mental health services, but the program has enhanced and added value to their mental wellbeing, parenting and parenting enjoyment including for mothers from ethnically diverse communities who often experience additional barriers to engagement with maternal mental health services (170).
Given the global prevalence of maternal mental ill health and the alarming expansion in numbers of those experiencing greater parental stress, isolation and mental illness in the shadow of COVID-19 (171, 172), the increasing numbers of previously undiagnosed cases of maternal depression emerging through the implementation and expansion of routine screening procedures (173, 174), and the profound inter-generational consequences of poor quality parenting, this refined, highly appreciated and effective Acorn program model offers the potential to strengthen the mental health system's response for a diversity of families. However, it is still the case that many families living in rural and remote areas may be restricted from participating in a program that congregates mothers and children at the same geographical venue. These mothers may be at elevated risk of maternal mental illness (106, 175). As a future development, alternative “distance” modes of delivery for Acorn could be developed and evaluated to assess the engagement and effectiveness of this program for these relatively isolated families.
Data availability statement
The datasets presented in this article are not readily available because of Ethics Committee requirements. Requests to access the datasets should be directed tocGF1bC5heWx3YXJkQHRvcnJlbnMuZWR1LmF1.
Ethics statement
The studies involving human participants were reviewed and approved by Bellberry Human Research Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author contributions
All authors contributed to the article and approved the submitted version.
Acknowledgments
We thank the following for their contributions to the program and its evaluation: Mandy Seyfang and Neil Underwood of the Women and Children's Health Network (WCHN) the originators of the Acorn program. Amanda Reinschmidt, Louise Byrne and Janelle Hutt in their management roles for the program while at AnglicareSA, the principal Dance Worker Sally Chance, and the many staff who delivered the program over its duration.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Cox EQ, Sowa NA, Meltzer-Brody SE, Gaynes BN. The perinatal depression treatment cascade baby steps toward improving outcomes. J Clin Psychiatry. (2016) 77:1189–200. doi: 10.4088/JCP.15r10174
2. Wang Z, Liu J, Shuai H, Cai Z, Fu X, Liu Y, et al. Mapping global prevalence of depression among postpartum women. Transl Psychiatry. (2021) 11:543. doi: 10.1038/s41398-021-01663-6
3. Steffen A, Nübel J, Jacobi F, Bätzing J, Holstiege J. Mental and somatic comorbidity of depression: a comprehensive cross-sectional analysis of 202 diagnosis groups using German nationwide ambulatory claims data. BMC Psychiatry. (2020) 20:142. doi: 10.1186/s12888-020-02546-8
4. Yelland C, Girke T, Tottman C, Williams AS. Clinical characteristics and mental health outcomes for women admitted to an Australian mother–baby unit: a focus on borderline personality disorder and emotional dysregulation? Australas Psychiatry. (2015) 23:683–7. doi: 10.1177/1039856215590251
5. Kroh S, Lim G. Perinatal depression. Int Anesthesiol Clin. (2021) 59:45–51. doi: 10.1097/AIA.0000000000000325
6. Woolhouse H, Gartland D, Mensah F, Brown SJ. Maternal depression from early pregnancy to 4 years postpartum in a prospective pregnancy cohort study: implications for primary health care. BJOG Int J Obstet Gynaecol. (2015) 122(3):312–21. doi: 10.1111/1471-0528.12837
7. Netsi E, Pearson RM, Murray L, Cooper P, Craske MG, Stein A. Association of persistent and severe postnatal depression with child outcomes. JAMA Psychiatry. (2018) 75:247. doi: 10.1001/jamapsychiatry.2017.4363
8. Norhayati MN, Hazlina NH, Asrenee AR, Emilin WM. Magnitude and risk factors for postpartum symptoms: a literature review. J Affect Disord. (2015) 175:34–52. doi: 10.1016/j.jad.2014.12.041
9. Dunford E, Granger C. Maternal guilt and shame: relationship to postnatal depression and attitudes towards help-seeking. J Child Fam Stud. (2017) 26:1692–701. doi: 10.1007/s10826-017-0690-z
10. Caldwell J, Meredith P, Whittingham K, Ziviani J. Shame and guilt in the postnatal period: a systematic review. J Reprod Infant Psychol. (2021) 39:67–85. doi: 10.1080/02646838.2020.1754372
11. Beck CT. The lived experience of postpartum depression:a phenomenological study. Nurs Res. (1992) 41:166–70. doi: 10.1097/00006199-199205000-00008
12. Dolman C, Jones I, Howard LM. Pre-conception to parenting: a systematic review and meta-synthesis of the qualitative literature on motherhood for women with severe mental illness. Arch Womens Ment Health. (2013) 16:173–96. doi: 10.1007/S00737-013-0336-0
13. McLoughlin J. Stigma associated with postnatal depression: a literature review. Br J Midwifery. (2013) 21:784–91. doi: 10.12968/bjom.2013.21.11.784
14. Bilszta J, Ericksen J, Buist A, Milgrom J. Women's experience of postnatal depression - beliefs and attitudes as barriers to care. Aust J Adv Nurs. (2010) 27:44–54.
15. Hanington L, Heron J, Stein A, Ramchandani P. Parental depression and child outcomes—is marital conflict the missing link? Child Care Health Dev. (2012) 38:520–9. doi: 10.1111/j.1365-2214.2011.01270.x
16. Sit D, Rothschild AJ, Wisner KL. A review of postpartum psychosis. J Womens Health. (2006) 15:352–68. doi: 10.1089/jwh.2006.15.352
17. Knight M. MBRRACE-UK update: key messages from the UK and Ireland confidential enquiries into maternal death and morbidity 2020. Obstet Gynecol. (2021) 23:161–3. doi: 10.1111/tog.12731
18. Meurk C, Wittenhagen L, Lucke J, Barker R, Roberts S, Moss K, et al. Suicidal behaviours in the peripartum period: a systematic scoping review of data linkage studies. Arch Womens Ment Health. (2021) 24:579–93. doi: 10.1007/s00737-021-01102-x
19. Doyle M, While D, Mok PLH, Windfuhr K, Ashcroft DM, Kontopantelis E, et al. Suicide risk in primary care patients diagnosed with a personality disorder: a nested case control study. BMC Fam Pract. (2016) 17. doi: 10.1186/s12875-016-0479-y
20. Schneider B, Schnabel A, Wetterling T, Bartusch B, Weber B, Georgi K. How do personality disorders modify suicide risk? J Pers Disord. (2008) 22:233–45. doi: 10.1521/pedi.2008.22.3.233
21. Black D, Blum N, Pfohl B, Hale N. Suicidal behavior in borderline personality disorder: prevalence, risk factors, prediction, and prevention. J Pers Disord. (2004) 18:226–39. doi: 10.1521/pedi.18.3.226.35445
22. Barr JA. Postpartum depression, delayed maternal adaptation, and mechanical infant caring: a phenomenological hermeneutic study. Int J Nurs Stud. (2008) 45:362–9. doi: 10.1016/j.ijnurstu.2006.10.002
23. Teti D, Gelfand D. Behavioral competence among mothers of infantsin the first year: the mediational role of self-efficacy. Child Dev. (1991) 62:918–29. doi: 10.2307/1131143
24. Reece S. The parent expectation survey. Clin Nurs Res. (1992) 1:336–46. doi: 10.1177/105477389200100404
25. Arante FO, Tabb KM, Wang Y, Faisal-Cury A. The relationship between postpartum depression and lower maternal confidence in mothers with a history of depression during pregnancy. Psychiatr Q. (2020) 91:21–30. doi: 10.1007/s11126-019-09673-w
26. Bloomfield L, Kendall S, Applin L, Vicky Attarzadeh RR, Dearnley K, Edwards L, et al. A qualitative study exploring the experiences and views of mothers, health visitors and family support centre workers on the challenges and difficulties of parenting. Health Soc Care Community. (2005) 13:46–55. doi: 10.1111/j.1365-2524.2005.00527.x
27. Zietlow AL, Schlüter MK, Nonnenmacher N, Müller M, Reck C. Maternal self-confidence postpartum and at Pre-school age: the role of depression, anxiety disorders, maternal attachment insecurity. Matern Child Health J. (2014) 18:1873–80. doi: 10.1007/s10995-014-1431-1
28. Cornish AM, McMahon CA, Ungerer JA, Barnett B, Kowalenko N, Tennant C. Maternal depression and the experience of parenting in the second postnatal year. J Reprod Infant Psychol. (2006) 24:121–32. doi: 10.1080/02646830600644021
29. Gerdes AC, Hoza B, Arnold LE, Pelham WE, James M, Swanson Wigal T, et al. Maternal depressive symptomatology and parenting behavior: exploration of possible mediators. J Abnorm Child Psychol. (2007) 35:705–14. doi: 10.1007/s10802-007-9134-3
30. Sidor A, Kunz E, Schweyer D, Eickhorst A, Cierpka M. Links between maternal postpartum depressive symptoms, maternal distress, infant gender and sensitivity in a high-risk population. Child Adolesc Psychiatry Ment Health. (2011) 5:7. doi: 10.1186/1753-2000-5-7
31. Thomason E, Volling BL, Flynn HA, McDonough SC, Marcus SM, Lopez JF, et al. Parenting stress and depressive symptoms in postpartum mothers: bidirectional or unidirectional effects? Infant Behav Dev. (2014) 37:406–15. doi: 10.1016/j.infbeh.2014.05.009
32. Hoffman C, Dunn DM, Njoroge WFM. Impact of postpartum mental illness upon infant development. Curr Psychiatry Rep. (2017) 19:100. doi: 10.1007/s11920-017-0857-8
33. Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. (2014) 384:1800–19. doi: 10.1016/S0140-6736(14)61277-0
34. Rayce SB, Rasmussen IS, Væver MS, Pontoppidan M. Effects of parenting interventions for mothers with depressive symptoms and an infant: systematic review and meta-analysis. BJPsych Open. (2020) 6:E9. doi: 10.1192/bjo.2019.89
35. Tharner A, Luijk MPCM, IJzendoorn MHv, Bakermans-Kranenburg MJ, Jaddoe VWV, Hofman A, et al. Infant attachment, parenting stress, and child emotional and behavioral problems at age 3 years. Parenting. (2012) 12:261–81. doi: 10.1080/15295192.2012.709150
36. Abidin RR. Parenting stress Index. 4th ed. Florida: PAR Psychological Assessment Resources, Inc. (2012).
37. Ainsworth MDS, Blehar MC, Waters E, Wall S. Patterns of attachment: A psychological study of the strange situation. Hillsdale: NJ: Erlbaum (1978).
38. Izett E, Rooney R, Prescott SL, De Palma M, McDevitt M. Prevention of mental health difficulties for children aged 0-3 years: a review. Front Psychol. (2020) 11. doi: 10.3389/fpsyg.2020.500361
39. O'Connor TG, Monk C, Burke AS. Maternal affective illness in the perinatal period and child development: findings on developmental timing, mechanisms, and intervention. Curr Psychiatry Rep. (2016) 18. doi: 10.1007/s11920-016-0660-y
40. Weiss SJ, Quides C. Disorders specific to infants and young children. In: Yearwood L,Pearson GS, editors. Child and adolescent behavioral Health. West Sussex, UK: John Wiley & Sons, Ltd. (2013). p. 333–54.
41. Stein A, Malmberg LE, Sylva K, Barnes J, Leach P, the FCCC team**. The influence of maternal depression, caregiving, and socioeconomic status in the post-natal year on children’s language development. Child Care Health Dev. (2008) 34:603–12. doi: 10.1111/j.1365-2214.2008.00837.x
42. Pelham WE, West SG, Lemery-Chalfant K, Goodman SH, Wilson MN, Dishion TJ, et al. Depression in mothers and the externalizing and internalizing behavior of children: an attempt to go beyond association. J Abnorm Psychol. (2021) 130:60–77. doi: 10.1037/abn0000640
43. Goodman SH, Simon HFM, Shamblaw AL, Kim CY. Parenting as a mediator of associations between depression in mothers and children's functioning: a systematic review and meta-analysis. Clin Child Fam Psychol Rev. (2020) 23:427–60. doi: 10.1007/s10567-020-00322-4
44. Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. (1999) 106:458–90. doi: 10.1037/0033-295x.106.3.458
45. Field T, Hernandez-Reif M, Diego M. Intrusive and withdrawn depressed mothers and their infants. Dev Rev. (2006) 26:15–30. doi: 10.1016/j.dr.2005.04.001
46. Letourneau NL, Dennis CL, Benzies K, Duffett-Leger L, Stewart M, Tryphonopoulos PD, et al. Postpartum depression is a family affair: addressing the impact on mothers, fathers, and children. Issues Ment Health Nurs. (2012) 33:445–57. doi: 10.3109/01612840.2012.673054
47. Reck C, Hunt A, Fuchs T, Weiss R, Noon A, Moehler E, et al. Interactive regulation of affect in postpartum depressed mothers and their infants: an overview. Psychopathology. (2004) 37:272–80. doi: 10.1159/000081983
48. Field T, Hernandez-Reif M, Diego M, Feijo L, Vera Y, Gil K, et al. Still-face and separation effects on depressed mother-infant interactions. Infant Ment Health J. (2007) 28:314–23. doi: 10.1002/imhj.20138
49. Field T. Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant Behav Dev. (2010) 33:1–6. doi: 10.1016/j.infbeh.2009.10.005
50. Ramsauer B, Achtergarde S. Mothers with acute and chronic postpartum psychoses and impact on the mother-infant interaction. Schizophr Res. (2018) 197:45–58. doi: 10.1016/j.schres.2018.02.032
51. Dennis CL, Falah-Hassani K, Shiri R. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatry. (2017) 210:315–23. doi: 10.1192/bjp.bp.116.187179
52. Petfield L, Startup H, Droscher H, Cartwright-Hatton S. A systematic review of the parenting and outcomes experienced by offspring of mothers with borderline personality pathology: potential mechanisms and clinical implications. Clin Psychol Rev. (2016) 47:85–105. doi: 10.1016/j.cpr.2016.04.002
53. Bartsch DR, Roberts RM, Davies M, Proeve M. Borderline personality disorder and parenting: clinician perspectives. Adv Ment Health. (2015) 13:113–26. doi: 10.1080/18387357.2015.1065554
54. Lovejoy MC, Graczyk PA, O'Hare E, Neuman G. Maternal depression and parenting behavior: a meta-analytic review. Clin Psychol Rev. (2000) 20:561–92. doi: 10.1016/S0272-7358(98)00100-7
55. Murray L, Cooper PJ. The impact of postpartum depression on child development. Int Rev Psychiatry. (1996) 8:55–63. doi: 10.3109/09540269609037817
56. Tronick E, Reck C. Infants of depressed mothers. Harv Rev Psychiatry. (2009) 17:147–56. doi: 10.1080/10673220902899714
57. Field T. Postnatal anxiety prevalence, predictors and effects on development: a narrative review. Infant Behav Dev. (2018) 51:24–32. doi: 10.1016/j.infbeh.2018.02.005
58. Mulsow M, Caldera YM, Pursley M, Reifman A, Huston AC. Multilevel factors influencing maternal stress during the first three years. J Marriage Fam. (2002) 64:944–56. doi: 10.1111/j.1741-3737.2002.00944.x
59. Rholes WS, Simpson JA, Friedman M. Avoidant attachment and the experience of parenting. Pers Soc Psychol Bull. (2006) 32:275–85. doi: 10.1177/0146167205280910
60. NICHD Early Child Care Research Network. The relation of child care to cognitive and language development. Child Dev. (2000) 71:960–80. doi: 10.1111/1467-8624.00202
61. Stright AD, Gallagher KC, Kelley K. Infant temperament moderates relations between maternal parenting in early childhood and children’s adjustment in first grade. Child Dev. (2008) 79:186–200. doi: 10.1111/j.1467-8624.2007.01119.x
62. Evans CA, Porter CL. The emergence of mother–infant co-regulation during the first year: links to infants’ developmental status and attachment. Infant behavior and development. Infant Behav Dev. (2009) 32:147–58. doi: 10.1016/j.infbeh.2008.12.005
63. Oxford ML, Findlay DM. NCAST Caregiver/parent–child interaction teaching manual. 2nd ed. Washington, Seattle: University of Washington, School of Nursing: NCAST Publication (2013).
64. Kochanska G, Aksan N, Carlson JJ. Temperament, relationships, and young children’s receptive cooperation with their parents. Dev Psychol. (2005) 41:648–60. doi: 10.1037/0012-1649.41.4.648
65. Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood. Eur Arch Psychiatry Clin Neurosci. (2006) 256:174–86. doi: 10.1007/s00406-005-0624-4
66. Conger RD, Belsky J, Capaldi DM. The intergenerational transmission of parenting: closing comments for the special section. Dev Psychol. (2009) 45:1276–83. doi: 10.1037/a0016911
67. Dennis CL, Hodnett ED. Psychosocial and psychological interventions for treating postpartum depression. Cochrane Database Syst Rev. (2007) (4):CD006116. doi: 10.1002/14651858.CD006116.pub2.17943888
68. Lumley J, Austin MP, Mitchell C. Intervening to reduce depression after birth: a systematic review of the randomized trials. Int J Technol Assess Health Care. (2004) 20:128–44. doi: 10.1017/s0266462304000911
69. Goodman JH, Santangelo G. Group treatment for postpartum depression: a systematic review. Arch Womens Ment Health. (2011) 14:277–93. doi: 10.1007/s00737-011-0225-3
70. Cicchetti D, Toth SL, Rogosch FA. The efficacy of toddler-parent psychotherapy to increase attachment security in offspring of depressed mothers. Attach Hum Dev. (1999) 1:34–66. doi: 10.1080/14616739900134021
71. Murray L, Cooper P, Wilson A, Romaniuk H. Controlled trial of the short-and long-term effect of psychological treatment of post-partum depression. Br J Psychiatry. (2002) 182:412–9. doi: 10.1192/bjp.182.5.412
72. McMahon CA, Barnett B, Kowalenko NM, Tennant CC. Maternal attachment state of mind moderates the impact of postnatal depression on infant attachment. J Child Psychol Psychiatry. (2006) 47:660–9. doi: 10.1111/j.1469-7610.2005.01547.x
73. Forman D, O'Hara MW, Stuart S, Gorman LL, Larsen KE, Coy KC. Effective treatment for postpartum depression is not sufficient to improve the developing mother-child relationship. Dev Psychopathol. (2007) 19:585–602. doi: 10.1017/S0954579407070289
74. Ericksen J, Loughlin E, Holt C, Rose N, Hartley E, Buultjens M, et al. A therapeutic playgroup for depressed mothers and their infants: feasibility study and pilot randomized trial of community hugs. Infant Ment Health J. (2018) 39:396–409. doi: 10.1002/imhj.21723
75. Nylen KJ, Moran TE, Franklin CL, O'Hara MW. Maternal depression: a review of relevant treatment approaches for mothers and infants. Infant Ment Health J. (2006) 27:327–43. doi: 10.1002/imhj.20095
76. Poobalan AS, Aucott LS, Ross L, Smith WC, Helms PJ, Williams JH. Effects of treating postnatal depression on mother-infant interaction and child development: systematic review. Br J Psychiatry. (2007) 191:378–86. doi: 10.1192/bjp.bp.106.032789
77. Dittrich K, Fuchs A, Bermpohl F, Meyer J, Führer D, Reichl C, et al. Effects of maternal history of depression and early life maltreatment on children's health-related quality of life. J Affect Disord. (2018) 225:280–8. doi: 10.1016/j.jad.2017.08.053
78. Kluczniok D, Boedeker K, Fuchs A, Hindi Attar C, Fydrich T, Fuehrer D, et al. Emotional availability in mother-child interaction: the effects of maternal depression in remission and additional history of childhood abuse. Depress Anxiety. (2016) 33:648–57. doi: 10.1002/da.22462
79. Jones TL, Prinz RJ. Potential roles of parental self-efficacy in parent and child adjustment: a review. Clin Psychol Rev. (2005) 25:341–63. doi: 10.1016/j.cpr.2004.12.004
80. Coleman PK, Karraker KH. Self-efficacy and parenting quality: findings and future applications. Dev Rev. (1997) 18:47–85. doi: 10.1006/drev.1997.0448
81. Letourneau NL, Dennis CL, Cosic N, Linder J. The effect of perinatal depression treatment for mothers on parenting and child development: a systematic review. Depress Anxiety. (2017) 34:928–66. doi: 10.1002/da.22687
82. Lieberman A, Zeanah C. Contributions of attachment theory to infant–parent psychotherapy and other interventions with young children. In: Cassidy J, Shaver PR, editors. Handbook of attachment. New York: Guilford Press (1999). p. 555–75.
83. Knitzer J, Theberge S, Johnson K. Reducing maternal depression and its impact on young children: toward a responsive early childhood policy framework, project thrive issue brief 2. City of New York: National Center for Children in Poverty, Columbia University, Mailman School of Public Health (2008).
84. Frisch U, Hofecker-fallahpour M, Stieglitz RD, Riecher-rössler A. Group treatment for depression in mothers of young children compared to standard individual therapy. Psychopathology. (2013) 46:94–101. doi: 10.1159/000338633
85. Muzik M, Rosenblum KL, Alfafara EA, Schuster MM, Miller NM, Waddell RM, et al. Mom power: preliminary outcomes of a group intervention to improve mental health and parenting among high-risk mothers. Arch Womens Ment Health. (2015) 18:507–21. doi: 10.1007/s00737-014-0490-z
86. Reck C, Zietlow AL, Müller M, Dubber S. Perceived parenting stress in the course of postpartum depression: the buffering effect of maternal bonding. Arch Womens Ment Health. (2016) 19:473–82. doi: 10.1007/s00737-015-0590-4
87. Ifcher J, Zarghamee H. The happiness of single mothers: evidence from the general social survey. J Happiness Stud. (2014) 15:1219–38. doi: 10.1007/s10902-013-9472-5
88. Jackson AP, Brooks-Gunn J, Huang C, Glassman M. Single mothers in low-wage jobs: financial strain, parenting, and preschoolers’ outcomes. Child Dev. (2000) 7:1409–23. doi: 10.1111/1467-8624.00236
89. Cairney J, Boyle M, Offord DR, Racine Y. Stress, social support and depression in single and married mothers. Soc Psychiatry Psychiatr Epidemiol. (2003) 38:442–9. doi: 10.1007/s00127-003-0661-0
90. Baranowska-Rataj A, Matysiak A, Mynarska M. Does lone motherhood decrease women’s happiness? Evidence from qualitative and quantitative research. J Happiness Stud. (2014) 15:1457–77. doi: 10.1007/s10902-013-9486-z
91. Nilaweera I, Doran F, Fisher J. Prevalence, nature and determinants of postpartum mental health problems among women who have migrated from south Asian to high-income countries: a systematic review of the evidence. J Affect Disord. (2014) 166:213–26. doi: 10.1016/j.jad.2014.05.021
92. Wittkowski A, Patel S, Fox JR. The experience of postnatal depression in immigrant mothers living in western countries: a meta-synthesis. Clin Psychol Psychother. (2017) 24:411–27. doi: 10.1002/cpp.2010
93. Falah-Hassani K, Shiri R, Vigod S, Dennis CL. Prevalence of postpartum depression among immigrant women: a systematic review and meta-analysis. J Psychiatr Res. (2015) 70:67–82. doi: 10.1016/j.jpsychires.2015.08.010
94. Davey HL, Tough SC, Adair CE, Benzies KM. Risk factors for sub-clinical and Major postpartum depression among a community cohort of Canadian women. Matern Child Health J. (2011) 15:866–75. doi: 10.1007/s10995-008-0314-8
95. Teo AR, Lerrigo R, Rogers MA. The role of social isolation in social anxiety disorder: a systematic review and meta-analysis. J Anxiety Disord. (2013) 27:353–64. doi: 10.1016/j.janxdis.2013.03.010
96. da Rocha M, Rhodes S, Vasilopoulou E, Hutton P. Loneliness in psychosis: a meta-analytical review. Schizophr Bull. (2018) 13:114–25. doi: 10.1093/schbul/sbx036
97. Pucker HE, Temes CM, Zanarini MC. Description and prediction of social isolation in borderline patients over 20 years of prospective follow-up. Pers Disord Theory Res Treat. (2019) 10:383–8. doi: 10.1037/per0000337
98. Cruwys T, Haslam SA, Dingle GA. Depression and social identity: an integrative review. Pers Soc Psychol Rev. (2014) 18:215–38. doi: 10.1177/1088868314523839
99. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: dSM-5. 5th ed. Washington, DC: APA (2013).
100. Beck CT. Predictors of postpartum depression. Nurs Res. (2001) 50:275–85. doi: 10.1097/00006199-200109000-00004
101. Eastwood J, Jalaludin B, Kemp L, Phung H, Barnett B, Tobin J. Social exclusion, infant behavior, social isolation, andmaternal expectations independently predict maternaldepressive symptoms. Brain Behavior. (2013) 3:14–23. doi: 10.1002/brb3.107
102. Mayberry LJ, Horowitz JA, Declercq E. Depression symptom prevalence and demographic risk factors among U.S. Women during the first 2 years postpartum. J Obstet Gynecol Neonatal Nurs. (2007) 36:542–9. doi: 10.1111/j.1552-6909.2007.00191.x
103. Eyden J, Winsper C, Wolke D, Broome M, MacCallum F. A systematic review of the parenting and outcomes experienced by offspring of mothers with borderline personality pathology: Potential mechanisms and clinical implications. Clin Psychol Rev. (2016) 47:85–105. doi: 10.1016/j.cpr.2016.04.002
104. Dunn A, Cartwright-Hatton S, Startup H, Papamichail A. The parenting experience of those with borderline personality disorder traits: practitioner and parent perspectives. Front Psychol. (2020) 11. doi: 10.3389/fpsyg.2020.01913
105. Mathisen SE, Glavin K, Lien L, Lagerløv P. Prevalence and risk factors for postpartum depressive symptoms in Argentina: a cross-sectional study. Int J Womens Health. (2013) 5:787–93. doi: 10.2147/IJWH.S51436
106. Villegas L, McKay K, Dennis CL, Ross LE. Postpartum depression among rural women from developed and developing countries: a systematic review. J Rural Health. (2011) 27:278–88. doi: 10.1111/j.1748-0361.2010.00339.x
107. Schore A. Effects of secure attachment relationship on right brain development, affect regulation and infant mental health. Infant Ment Health J. (2001) 22:7–66. doi: 10.1002/1097-0355(200101/04)22:1%3C7::AID-IMHJ2%3E3.0.CO;2-N
108. Bakermans-Kranenburg MJ, Van IJzendoorn MH, Juffer F. Disorganized infant attachment and preventive interventions: a review and meta-analysis. Infant Ment Health J. (2005) 26:191–216. doi: 10.1002/imhj.20046
109. De Wolff MS, Van IJzendoorn MH. Sensitivity and attachment: a meta-analysis on parental antecedents of infant attachment. Child Dev. (1997) 68:571–91. doi: 10.2307/1132107
110. Berlin L, Zeanah CH, Lieberman AF. Prevention and intervention programmes for supporting early attachment security. In: Cassidy J, Shaver PR, editors. Handbook of attachment: theory, research, and clinical applications. New York: The Guilford Press (2008). p. 745–61.
111. Lieberman AF. Child-parent psychotherapy: a relationship-based approach to the treatment of mental health disorders in infancy and early childhood. In: Sameroff AJ, McDonough SC, Rosenblum KL, editors. Treating parent-infant relationship problems: strategies for intervention. New York, NY: Guilford Press (2004). p. 97–122.
112. Sroufe LA. Emotional development: the organization of emotional life in the early years. New York, NY: Cambridge University Press (1997).
113. De L’Etoile S. Infant behavioural responses to infant directed singing and other maternal interactions. Infant Behav Dev. (2006) 29:456–70. doi: 10.1016/j.infbeh.2006.03.002
114. Malloch S, Shoemark H, Črnčec R, Newnham C, Paul C, Prior M, et al. Music therapy with hospitalized infants—the art and science of communicative musicality. Infant Ment Health J. (2012) 33:386–99. doi: 10.1002/imhj.21346
115. Van Puyvelde M, Rodrigues H, Loots G, De Coster L, Du ville K, Matthijs L, et al. Shall we dance? Music as a port of entrance to maternal–infant intersubjectivity in a context of postnatal depression. Infant Ment Health J. (2014) 35:220–32. doi: 10.1002/imhj.21431
116. Chance S. The acorn program: from small things big things grow. South Australia: The Hopscotch Foundation PTY (2021). Available at: https://meb4three.org.au/acorn/
118. Fonagy P, Target M. Attachment and reflective function: their role in self organization. Dev Psychopathol. (1997) 9:679–700. doi: 10.1017/S0954579497001399
119. Miller W. Interactive journaling as a clinical tool. J Ment Health Couns. (2014) 36:31–42. doi: 10.17744/mehc.36.1.0k5v52l12540w218
120. Slade A. Parental reflective functioning: an introduction. Attach Hum Dev. (2005) 7:269–81. doi: 10.1080/14616730500245906
122. Kindsvatter A, Desmond K, Yanikoski A, Stahl S. The use of therapeutic letters in addressing parent-child attachment problems. Fam J. (2013) 21:74–9. doi: 10.1177/1066480712456824
123. Moules NJ. The past and future of therapeutic letters: family suffering and healing words. J Fam Nurs. (2009) 15:102–11. doi: 10.1177/1074840709332238
124. Wadsworth Y. What is participatory action research?: Action Research International, Paper 2. (1998).
125. Hoffman KT, Marvin RS, Cooper G, Powell B. Changing toddlers’ and preschoolers’ attachment classifications: the circle of security intervention. J Consult Clin Psychol. (2006) 74:1017–26. doi: 10.1037/0022-006X.74.6.1017
128. Fernie S, Smith K. Action research. In: Fernie S, Smith K, editors. Practical research and evaluation: a start-to-finish guide for practitioners. London: SAGE Publications Ltd (2010). p.95–110.
129. Kemmis K, McTaggart R. Participatory action research. In: Denzin N, Lincoln Y, editors. Handbook of qualitative research. Thousand Oaks, CA: Sage (2000). p.559–603.
130. Abidin RR. Parenting stress Index (PSI) manual. 3rd ed. Charlottesville, VA: Pediatric Psychology Press (1995).
131. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
132. Crncec R, Barnett B, Matthey S. Karitane parenting confidence scale: manual. Sydney, Australia: karitane: Sydney South West Area Health Service (2008a).
134. Crncec R, Barnett B, Matthey S. Review of scales of parenting confidence. J Nurs Meas. (2010) 18:210–40. doi: 10.1891/1061-3749.18.3.210
135. Coleman PK, Karraker KH. Maternal self efficacy beliefs, competence in parenting, and toddlers’ behaviour and developmental status. Infant Ment Health J. (2003) 24:126–48. doi: 10.1002/imhj.10048
136. Zanarini MC, Vujanovic AA, Parachini EA, Boulanger JL, Frankenburg FR, Hennen J. A screening measure for BPD: the mclean screening instrument for borderline personality disorder (MSIBPD). J Pers Disord. (2003) 17:568–73. doi: 10.1521/pedi.17.6.568.25355
137. Sumner G, Spitz A. NCAST Caregiver/parent-child interaction teaching manual. Seattle, WA: NCAST Publications, University of Washington School of Nursing (1994).
138. Barnard KE, Hammond MA, Booth CL, Mitchell SK, Spieker SJ. Measurement and meaning of parent–child interaction. In: Morrison CLF, Keating D, editors. Applied developmental psychology. 3rd ed. New York, NY: Academic Press (1989). p. 39–80.
139. Barnard K, Martell L. Mothering. In: Bornstein M, editors. Handbook of parenting. 3rd ed. Hillsdale, NJ: Lawrence Erlbaum (1995). p. 3–26.
140. Byrne M, Keefe M. Comparison of two measures of parent-child interaction. Nurs Res. (2003) 52:34–41. doi: 10.1097/00006199-200301000-00005
141. Letourneau NL, Tryphonopoulos PD, Novick J, Hart JM, Giesbrecht G, Oxford ML. Nursing child assessment satellite training parent-child interaction scales: comparing American and Canadian normative and high-risk samples. J Pediatr Nurs. (2018) 40:47–57. doi: 10.1016/j.pedn.2018.02.016
142. Nakamura WM, Stewart KB, Tatarka ME. Assessing father–infant interactions using the NCAST teaching scale: a pilot study. Am J Occup Ther. (2000) 54:44–51. doi: 10.5014/ajot.54.1.44
143. Cohen J. Statistical power analysis for the behavioural sciences. 2nd ed. Hillsdale NJ: Erlbaum (1988).
146. Jacobson NS, Truax P. Clinical significance: a statistical approach to determining meaningful change in psychotherapy research. J Consult Clin Psychol. (1991) 59:12–9. doi: 10.1037/0022-006X.59.1.12
147. Muzik M MA, Bonham C, Lisa Rosenblum K, Broderick A, Kirk R. Perspectives on trauma-informed care from mothers with a history of childhood maltreatment: a qualitative study. Child Abuse Negl. (2013) 37:1215–24. doi: 10.1016/j.chiabu.2013.07.014
148. Naber D, Bullinger M. Should antidepressants be used in minor depression? Dialogues Clin Neurosci. (2018) 20:223–8. doi: 10.31887/DCNS.2018.20.3/dnaber
149. Minas H, Kakuma R, Too LS, Vayani H, Orapeleng S, Prasad-Ildes R, et al. Mental health research and evaluation in multicultural Australia: developing a culture of inclusion. Int J Ment Health Syst. (2013) 7(23). doi: 10.1186/1752-4458-7-23
150. Zaslow M, Bronte-Tinkew J, Capps R, Horowitz A, Moore KA, Weinstein D. Food security during infancy: implications for attachment and mental proficiency in toddlerhood. Matern Child Health Care J. (2009) 13:66–80. doi: 10.1007/s10995-008-0329-1
151. Bakermans-Kranenburg MJ, Van IJzendoorn MH, Juffer F. Less is more: meta-analytic arguments for the use of sensitivity-focused interventions. In: Juffer F, Bakermans-Kranenburg MJ, Van IJzendoorn MH, editors. Promoting positive parenting: an attachment-based intervention. New York, NY: Taylor & Francis Group/Lawrence Erlbaum Associates (2008). p. 59–74.
152. Bakermans-Kranenburg MJ, van Ijzendoorn MH, Juffer F. Less is more: meta-analyses of sensitivity and attachment interventions in early childhood. Psychol Bull. (2003) 129:195–215. doi: 10.1037/0033-2909.129.2.195
153. Davenport MH, Meyer S, Meah VL, Strynadka MC, Khurana R. Moms are not OK: cOVID-19 and maternal mental health. Front Glob Women's Health. (2020) 1. doi: 10.3389/fgwh.2020.00001
154. Davidson L. The recovery movement: implications for mental health care and enabling people to participate fully in life. Health Aff. (2016) 35:1091–7. doi: 10.1377/hlthaff.2016.0153
155. Reitman D, Currier RO, Stickle TR. A critical evaluation of the parenting stress Index-short form (PSI-SF) in a head start population. J Clin Child Adolesc Psychol. (2002) 31:384–92. doi: 10.1207/s15374424jccp3103_10
156. Ramsauer B, Mühlhan C, Mueller J, Schulte-Markwort M. Parenting stress and postpartum depression/anxiety in mothers with personality disorders: indications for differential intervention priorities. Eur Child Adolesc Psychiatry. (2016) 25:589–600. doi: 10.1007/s00787-015-0775-4
157. Lim M, Van Hulst A, Pisanu S, Merry L. Social isolation, loneliness and health: a descriptive study of the experiences of migrant mothers with young children (0–5 years old) at la maison bleue. Front Glob Women's Health. (2022) 3. doi: 10.3389/fgwh.2022.823632
158. Kawachi I, Berkman LF. Social ties and mental health. J Urban Health. (2001) 78:458–67. doi: 10.1093/jurban/78.3.458
159. Perkins JM, Subramanian SV, Christakis NA. Social networks and health: a systematic review of sociocentric network studies in lowand middle-income countries. Soc Sci Med. (2015) 125:60–78. doi: 10.1016/j.socscimed.2014.08.019
160. Cruwys T, Dingle GA, Haslam C. Social group memberships protect against future depression, alleviate depression symptoms and prevent depression relapse. Soc Sci Med. (2013) 98:179–86. doi: 10.1016/j.socscimed.2013.09.013
161. Cruwys T, Haslam SA, Dingle GA. Feeling connected again: interventions that increase social identification reduce depression symptoms in community and clinical settings. J Affect Disord. (2014) 159:139–46. doi: 10.1016/j.jad.2014.02.019
162. Haslam C, Cruwys T, Haslam SA. Groups 4 health: evidence that a social-identity intervention that builds and strengthens social group membership improves mental health. J Affect Disord. (2016) 194:188–95. doi: 10.1016/j.jad.2016.01.010
163. Saeri AK, Cruwys T, Barlow FK, Stronge S, Sibley CG. Social connectedness improves public mental health: investigating bidirectional relationships in the New Zealand attitudes and values survey. Aust N Z J Psychiatry. (2018) 52:365–74. doi: 10.1177/0004867417723990
164. Jones CC, Jomeen J, Hayter M. The impact of peer support in the context of perinatal mental illness: a meta-ethnography. Midwifery. (2014) 30:491–8. doi: 10.1016/j.midw.2013.08.003
165. Aylward P. Evaluation of the acorn parenting program. South Australia: Action Research Partnerships & The Hopscotch Foundation PTY (2022). Available at: https://meb4three.org.au/acorn/
166. Government of South Australia. Borderline Personality Disorder Implementation Plan (2017). Available at: https://www.sahealth.sa.gov.au/wps/wcm/connect/fd259a8042ad4f2f9d5ebf80c298878e/borderline+personality+disorder+(bpd)+service+implementation+plan.pdf?mod=ajperes (Accessed January 10, 2018).
167. Stephens S, Ford E, Paudyal P, Smith H. Effectiveness of psychological interventions for postnatal depression in primary care: a meta-analysis. Ann Fam Med. (2016) 14:463–72. doi: 10.1370/afm.1967
168. Cuijpers P, Quero S, Noma H, Ciharova M, Miguel C, Karyotaki E, et al. Psychotherapies for depression: a network meta-analysis covering efficacy, acceptability and long-term outcomes of all main treatment types. World Psychiatry. (2021) 20:283–93. doi: 10.1002/wps.20860
169. Cuijpers P, Brännmark JG, van Straten A. Psychological treatment of postpartum depression: a meta-analysis. J Clin Psychol. (2008) 64:103–18. doi: 10.1002/JCLP.20432
170. Iturralde E, Hsiao CA, Nkemere L, Kubo A, Sterling SA, Flanagan T, et al. Engagement in perinatal depression treatment: a qualitative study of barriers across and within racial/ethnic groups. BMC Pregnancy Childbirth. (2021) 21:512. doi: 10.1186/s12884-021-03969-1
171. COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12. doi: 10.1016/S0140-6736(21)02143-7
172. Adams EL, Smith D, Caccavale LJ, Bean MK. Parents are stressed! patterns of parent stress across COVID-19. Front Psychiatry. (2021) 12. doi: 10.3389/fpsyt.2021.626456
173. Austin M-P, Highet N, The Expert Working Group. Mental health care in the perinatal period: australian clinical practice guideline. Melbourne: Centre of Perinatal Excellence (2017).
174. Waqas A, Koukab A, Meraj H, Dua T, Chowdhary N, Fatima B, et al. Screening programs for common maternal mental health disorders among perinatal women: report of the systematic review of evidence. BMC Psychiatry. (2022) 22:54. doi: 10.1186/s12888-022-03694-9
Keywords: maternal mental health, parenting, holistic, depression, borderline personality disorder, well-being, action research, attachment theory
Citation: Aylward P and Sved Williams A (2023) Holistic community-based group parenting programs for mothers with maternal mental health issues help address a growing public health need for a diversity of vulnerable mothers, children and families: Findings from an action research study. Front. Glob. Womens Health 3:1039527. doi: 10.3389/fgwh.2022.1039527
Received: 8 September 2022; Accepted: 20 December 2022;
Published: 17 January 2023.
Edited by:
Caroline Gurvich, Monash University, AustraliaReviewed by:
Huynh-Nhu Le, George Washington University, United StatesNusrat Husain, The University of Manchester, United Kingdom
© 2023 Aylward and Sved Williams. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Paul Aylward cGF1bC5heWx3YXJkQHRvcnJlbnMuZWR1LmF1; UGF1bEBhY3Rpb25ycC5jbw==
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Women's Mental Health, a section of the journal Frontiers in Global Women's Health
 Paul Aylward
Paul Aylward Anne Sved Williams3,4,†
Anne Sved Williams3,4,†