- 1Department of Food Science, Nutrition and Technology, University of Nairobi, Nairobi, Kenya
- 2Kenya Institute for Public Policy Research and Analysis, Nairobi, Kenya
- 3Feed the Future Innovation Lab for Animal Health, Washington State University, Pullman, WA, United States
- 4Center for Epidemiological Modelling and Analysis, University of Nairobi, Nairobi, Kenya
- 5Paul G. Allen School for Global Health, Washington State University, Pullman, WA, United States
- 6Department of Clinical Studies, Faculty of Veterinary Medicine, University of Nairobi, Nairobi, Kenya
- 7Institute of Immunology and Infection Research, School of Biological Sciences, University of Edinburgh, Edinburgh, United Kingdom
- 8Center for Public Health Research, Kenya Medical Research Institute, Nairobi, Kenya
Background: Inadequate food intake is the most common cause of malnutrition worldwide. There is paucity of knowledge on the influence of farming systems, a proxy for contextualizing community-based food networks, and sociocultural perspectives necessary for creating impactful nutritional programs and policies for young children from infancy to early childhood in Kenya and their mothers, especially in Kenya. This study sought to evaluate nutrient intakes of young children and their mothers from Pastoral, Agro-pastoral and Mixed farming system in Kenya.
Methods: Mothers and their children were recruited from households in Narok south as part of the Animal Health Innovation Study. One day multiple pass 24-h dietary recall was completed for a sample of infants 6–11 months, and toddlers aged 12–48 months (n = 161), and women of reproductive age (15–49 years) (n = 161) via face-to-face interviews with the primary caregiver. Nutrient intakes were estimated using CS Dietary Software and compared with the Adequate Intakes, Recommended Dietary Allowance and/or Estimated Average Requirement.
Results: The mean intake of key nutrients varied across farming systems. Children aged 6–11 months, met the Adequate Intake and Recommended Dietary Allowance levels for protein and Vitamin A. However, deficiencies were noted in thiamine, vitamin C, vitamin B6, selenium, and niacin across different farming systems, with insufficient Iron intake, particularly in pastoral and agro-pastoral systems (3 mg/d vs. 7 mg/d and 5 mg/d vs. 7 mg/d respectively. Folate intake was significantly lower in pastoral and mixed farming systems, with levels below the recommended 100 μg dfe/d. Calcium intake was sufficient across all farming systems, while phosphorus intake was consistently below the AI of 180 mg/d in children aged 12–48 months. In the mixed farming group, intake exceeded the Recommended Nutrient Intake for calcium, while phosphorus intake remained low across all age groups in agro-pastoral and mixed farming systems. Magnesium intake fell below AI levels in all groups (<65AI). Among women of reproductive age (15–49 years), the agro-pastoral group exhibited the highest carbohydrate intake, while the mixed farming group had the highest protein intake (51.07 ± 6.5). Women met vitamin A recommendations, with zinc, iron, and selenium intake felling below the Adequate Intake in all groups.
Conclusion: While certain nutrients such as protein and vitamin A intake were met in children and mothers, deficiencies were noted in crucial nutrients like iron and folate across various farming systems. These findings underscore the importance of considering local contextual factors when designing nutrition interventions. To address nutritional disparities and improve overall health outcomes and wellbeing for children and mothers in diverse agricultural settings in Kenya, it is important to prioritize an understanding sociocultural contexts and/or regional variations in designing and implementation of targeted interventions.
1 Introduction
Insufficient dietary intake among Women of Reproductive Age (WRA) and under five-year-old children is associated with undernutrition and child mortality. The 2021 Global Nutrition Report highlights the pervasive challenge of malnutrition worldwide, especially in low and middle-income countries (LMICs) and sub-Saharan Africa. Malnutrition, encompassing undernutrition, overweight, and obesity, contributes to over 12 million deaths annually from non-communicable diseases (NCDs), with 78% of NCD deaths in LMICs attributed to poor diets and malnutrition. Deficient dietary intake, particularly in low- and middle-income countries (LMIC), disproportionately affects poorer LMICs and is most prevalent in sub-Saharan Africa (WHO, 2020). Progress in reducing the global burden of malnutrition has been slow (Were et al., 2023). Adequate nutrition during infancy and early childhood is crucial for ensuring children’s optimal growth, health, and development. Proper feeding practices during this period play a significant role in stimulating psycho-social development, maintaining good nutritional status, promoting physical growth, reducing susceptibility to common childhood infections, and enhancing the ability to cope with them. This is also emphasized in UNICEF Nutrition Strategy 2020–2030 which aims at improving diets that support optimal nutrition, growth, and development in WRA and under 5-year-old children (UNICEF, 2020).
Optimal nutrition depends on the balance between nutritional requirements and dietary intake. In women of reproductive age (WRA) and children, a healthy and balanced diet is essential to prevent all forms of malnutrition, as stated in UNICEF (2023). The first 1,000 days of life are significant for children as it correlates with a child’s brain growth and development and constitutes the foundations for their lifelong health (Hayes, 2023). Malnutrition during this time can cause irreversible damage to a child’s growing brain, affecting their ability to learn and thrive, and can lead to chronic diseases later in life. WHO et al. (2020) reiterate that good nutrition is essential to break the inter-generational cycle of maternal and child malnutrition. Therefore, the nutritional adequacy of the diet is fundamental.
In rural areas of Kenya, diets are often monotonous and mainly cereal-based with low animal source foods and micronutrients (vitamin A, iron, zinc and calcium) rich foods (Ngala, 2015; Ronoh, et al., 2017). This was confirmed by the National survey by Kenya National Bureau of Statistics (KNBS) 2022 report, which showed that 51% of WRA and 63% of children 6–23 months did not meet the requirement for dietary diversity. The poor diet observed in these areas leads to an increase in maternal and child malnutrition, predominantly micronutrient deficiencies. This is evident in Narok County, a predominantly livestock-keeping community, which has relatively high levels of under-five malnutrition (underweight, wasting and stunting) at 11%, 2% and 22% respectively (Kenya National Bureau of Statistics (KNBS) 2022). Micronutrients (iron, zinc, calcium, Vitamin A) and iron deficiencies and anemia are also prevalent in this region (Ronoh, et al., 2017) and affect both children under 5 years of age and WRA (Kenya National Bureau of Statistics (KNBS) 2022). Different strategies such as vitamin A supplementation among children 6–59 months old, iron/folic acid in pregnant and lactating women, and food fortification have been implemented by the Ministry of Health (MoH) Kenya to prevent maternal and child malnutrition (Obonyo, 2018). Despite these efforts, it is worth noting that malnutrition remains a public health issue in rural livestock keeping communities in Kenya. In recent times, dietary diversity and nutrition education strategies are increasingly promoted to improve the quality of the diets (Ochola and Masibo, 2014; Margolies et al., 2022; Bechoff et al., 2023). Promoting Animal Source Food (ASF) consumption through nutrition-sensitive programs is also used as a new approach for optimizing the nutrients contents of diets consumed widely to address malnutrition, particularly the hidden hunger (Kim et al., 2019; Flax et al., 2021). ASF refer to food products derived from animals such as meat, eggs, fish, dairy, snails, and some worms/insects (Leroy and Alonso, 2024).
The Animal Health Innovation Lab (AHIL) project, implemented in Narok County, aims to evaluate the nutritional and dietary habits of children and mothers. Additionally, the project seeks to increase the consumption of animal-source foods among the participants to enhance their nutritional status. Thus, this study sought to assess the baseline dietary intakes of mother-child pairs (mothers aged 15–49 years and children aged 6–48 months) in Narok County, Kenya.
2 Methodology
2.1 Study setting
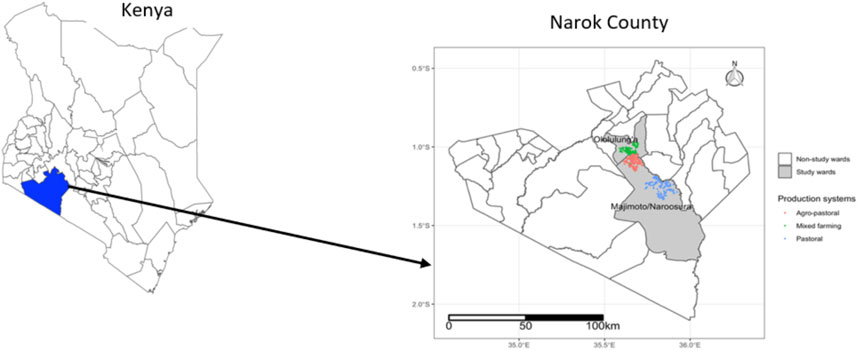
Narok County, one of the 47 counties in Kenya, is located at an average altitude of 1,800 m above sea level, and is divided into six sub-counties, namely, Narok North, Narok South, Narok East, Narok West, Transmara East, and Transmara West. The County is known for its fertile land and favourable climate, making it suitable for agriculture and livestock rearing. However, it is also characterized by a bimodal rainfall pattern, ranging from 500 mm in the southeast to 1,300 mm in the northwest (Bartzke et al., 2018) leading to variability in climate systems, and hence a dry-wet heterogeneity leading to the pastoral, agro-pastoral and mixed systems. It is a major producer of wheat, barley, maize, and beans, and also has a significant livestock population, including cattle, sheep, and goats (Kenya National Bureau of Statistics (KNBS) and ICF Macro, 2010). Narok South was purposively selected because due to the variability in farming systems and presence of high rates of undernutrition in children. Two wards, Ololulung’a and Naroosura Majimoto were further sub-selected from Narok South.
A cross-sectional study design was conducted on 20% of the sample selected for the larger Animal Health Innovation Lab (AHIL) project. Twelve villages were simple randomly selected from the study area: five in Narosura Majimoto Ward and seven in Ololulung’a Ward (Figure 1). A total of 165 households participated in the 24-h recall, with 62 households from Narosura Majimoto and 103 households from Ololulung’a, each having at least one child aged 6–48 months. In households with more than one child in the target age group, the youngest child (the index child) was selected. The primary respondent for the study was the mother or caretaker of the index child.
2.2 Data collection
Mothers with children 6–59 months of age who were willing to participate in this study were interviewed using a pretested questionnaire. Information collected included sociodemographic characteristics and child-feeding practices (breastfeeding and complementary feeding). In assessing dietary intake, multiple-pass 24-h dietary recall was used where a mother/caregiver was asked to recall foods and beverages fed to the child in the 24 h prior to the interview using a validated questionnaire by the Food and Agricultural Organization of the United Nations (FAO, 2018). A mother/caregiver was requested to show the local utensils used and the amount of food fed to the child to estimate the food portion/weight in grams. Measuring cylinders were used for liquid foods while rice was used for solid foods such as ugali (stiff porridge) and cooked rice. Other common household measures such as cups, plates, serving spoons were also used to estimate the portion sizes served. Further, the Kenya Medical Research Institute (KEMRI) photo booklet (unpublished) was used to estimate the food when the sample was not available. One picture per food item was used for most foods, but for some food items, there were three to five pictures for the different portion sizes. Each photo showed the Gram weight equivalent for the food portion shown, as well as a common household utensil such as a spoon, cup, or plate) to show scale. During data collection, the nature of each day was recorded, categorizing it as either a normal day, a celebration or ceremony occasion, and specifying the day of the week (Monday to Friday) or weekend. This categorization was crucial for the subsequent analysis, as it allowed for a nuanced understanding of the data. The CS dietary tool incorporated these distinctions in its analytical framework, accounting for the potential variability introduced by different types of days. This approach was instrumental in identifying and explaining any outliers, ensuring that the analysis accurately reflected the influence of daily variations on the data.
2.3 Implementing multiple-pass 24-h recall survey
Trained personnel were involved in multiple pass 24-h recall data collection. This allowed for one person to ask questions to the mother, one to record the responses, and another to carry out measurements and portion size estimation. Training for the 24-h recall lasted for 7 days, during which we covered recall interview techniques and all aspects of the multiple-pass 24-h recall form. Staff conducted training sessions where they practiced interview techniques and data entry through hypothetical scenarios and role-playing, culminating in a pilot interviewer collecting data from mothers in a neighbourhood not chosen for the study, under supervision to ensure interview quality, measurement accuracy, and data entry precision.
The interviewers asked the primary caregiver of the participating child to recall the child’s food intake, following the prompts and food description questions described previously. For quality control, 10% of interviews were randomly selected using a computerized selection process. The computerized selection process involved entering all interview form’s ID and random sampling algorithm using R programming to select 10% of the interviews to ensured that each interview form had an equal chance of being chosen, thereby minimizing human bias and enhancing the reliability of the quality control checks. Senior research staff also observed these visits to ensure that interviewers adhered to the recall protocol. Questionnaires were checked for completeness and securely stored for data entry and analysis.
2.4 Data analysis
Mean daily nutrient intake (energy, protein, fat, carbohydrate, vitamin A, calcium, iron and zinc) was estimated using CS Dietary (v2.11), developed by Harvestplus and SerPro S.A., August 2019), which was then integrated with the food composition table, recipes database and conversion factors database to yield nutrient intake from each food. The mean intake values of energy, protein, fat, carbohydrate, vitamin A, calcium, iron, and zinc were expressed as amount per day and compared by recommended daily intake (RDI/RDA) (IOM, 2006). It is reasonable to presume that a population group whose mean nutrient intake is at or above the AI has diets that are sufficiently nourishing and that the occurrence of deficient intakes is low.
The estimated energy requirements (EER) are used to express the energy requirements. The total energy intake expected to maintain energy balance for a given age plus an additional allowance for energy deposition to account for growth is known as the energy expenditure ratio, or EER.
3 Results
3.1 Sociodemographic characteristics of children, mothers, and households
The sociodemographic characteristics of children, mothers, and households in Pastoral, Agro-pastoral, and Mixed farming are shown in Table 1. Half of the children (50.3%) fell within the 24–48 months age group across all farming systems, with a slightly higher percentage of males (51.2%) compared to females (48.8%). In mothers, those with no education (50.9%) had the highest proportion across all systems with those with primary education accounting for nearly a third (29.2%) of the mothers. Livestock herding was the predominant (77.6%) occupation among mothers in all farming systems. The mean age of mothers was 30 (±5.0) years. Food insecurity was notably high, with 80.7% of households experiencing food insecurity in the three systems of farming.
3.2 Nutrient intake among children 6–11 months
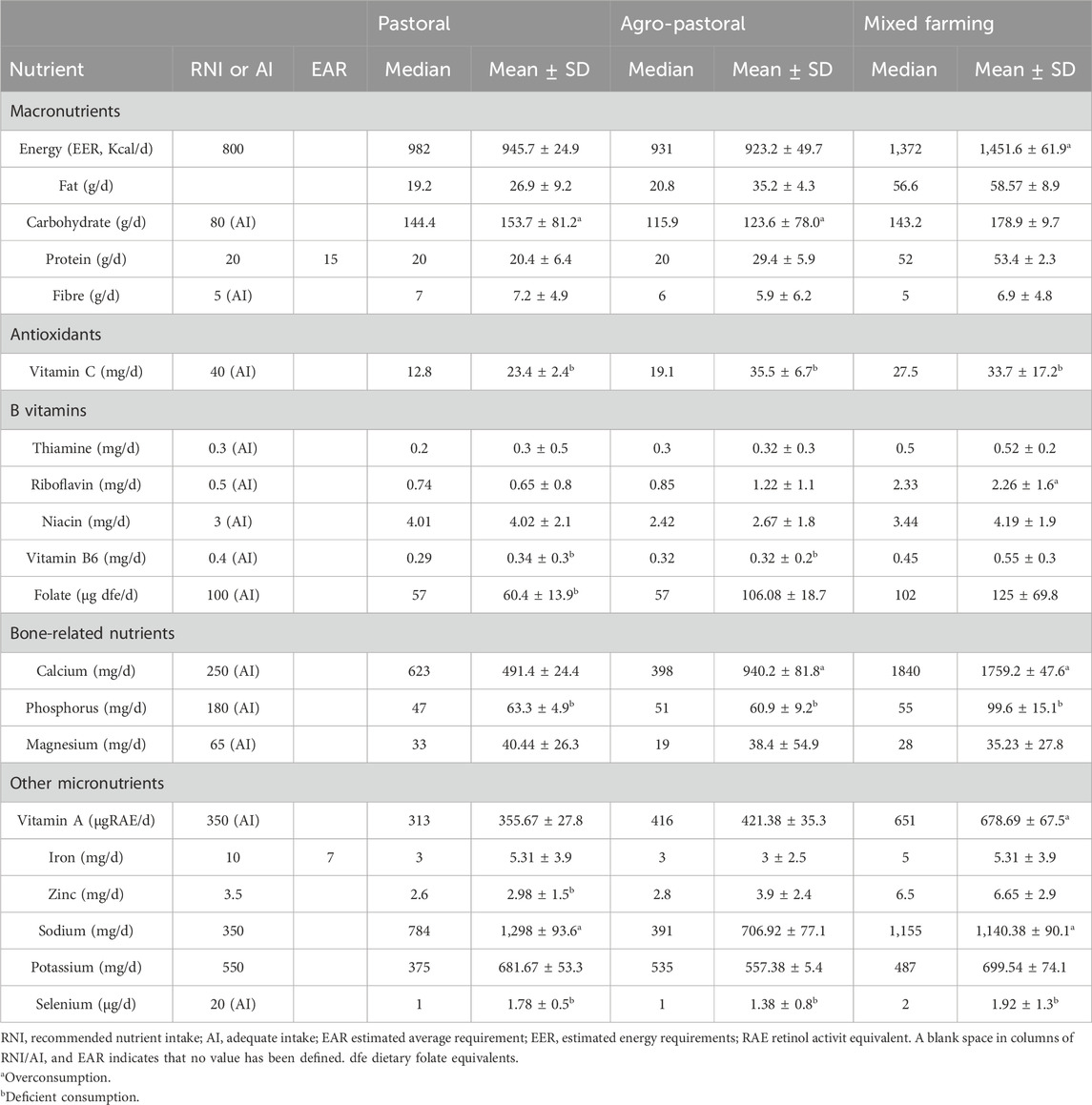
The mean nutrient intake among infants aged 6–11 months in three distinct farming systems in Kenya are displayed in Table 2. Mean energy intake was met in the three-farming systems with slightly higher mean intake (1,451.6 ± 61.9 Kcal/d vs. 800 Kcal/d) reported in Mixed farming systems. Both the mean and median intakes of fat as a percentage of total energy were lower in all the farming systems.
Mean intake of thiamine, vitamin c, vitamin B6 and selenium were notably deficient, falling below the Adequate Intake (AI) levels in all the farming systems. Children 6–11 months in the agro-pastoral system exhibit niacin intake below the recommended AI of 3 mg/d at 2.42 mg/d. Folate intake is significantly deficient in the pastoral and mixed farming systems, with values of 57 μg dfe/d and 60.4 ± 13.9 μg dfe/d, respectively, failing to meet the AI of 100 μg dfe/d. Calcium intake is sufficient in all farming systems. Phosphorus intake was lower than the AI (180 mg/d) in all the farming systems.
Conversely, instances of overconsumption are evident in various nutrients. Mean fat intake surpassed the Recommended Nutrient Intake (RNI) or AI in all three farming systems, with values of 26.9 ± 9.2 g/d, 35.2 ± 4.3 g/d, and 58.57 ± 8.9 g/d in the pastoral, agro-pastoral, and mixed farming systems, respectively. Carbohydrate intake exceeds the AI (80 g/d) in the mixed farming system, with a mean intake of 178.9 ± 9.7 g/d. Protein intake was met in all three farming systems, particularly in the mixed farming system, with a value of 53.4 ± 2.3 g/d. Vitamin C intake is consistently above the AI (40 mg/d) in all farming systems. In the mixed farming system, the mean riboflavin intake surpassed the AI at 2.26 ± 1.6 mg/d. Calcium intake exceeds the AI in the mixed farming system, with a mean intake of 1759.2 ± 47.6 mg/d.
Vitamin A intake was met in pastoral (mean 355.67 ± 27.8 vs. 350μgRAE/d) and 421.38 ± 35.3 vs. 350 μgRAE/d) in Agro pastoral and slightly higher than AI in mixed farming systems (678.69 ± 367.52 vs. 350 μg RAE/d). The mean iron intake was below the EAR in Pastoral and Agro-pastoral farming systems (3 mg/d vs.7 mg/d), with mixed farming systems 5 mg/d vs. 7 mg/d being very close to the EAR indicating that possibly some infants were at risk for inadequate iron intake. Mean intakes of other nutrients generally met or exceeded the recommendations.
3.3 Nutrient intake in children 12–23 and 24–48 months in different farming systems
Table 3 presents the mean nutrient intake in children 12–23 months and 24–48 months across different farming systems in Narok County, Kenya. Energy intake for all groups exceeded the Recommended Energy Requirements (EER). The Mixed Farming group exhibited the highest median and mean values, with a median of 1,544 kcal and a mean of 1,680.52 ± 769.23 kcal, indicating a potential overconsumption of calories.
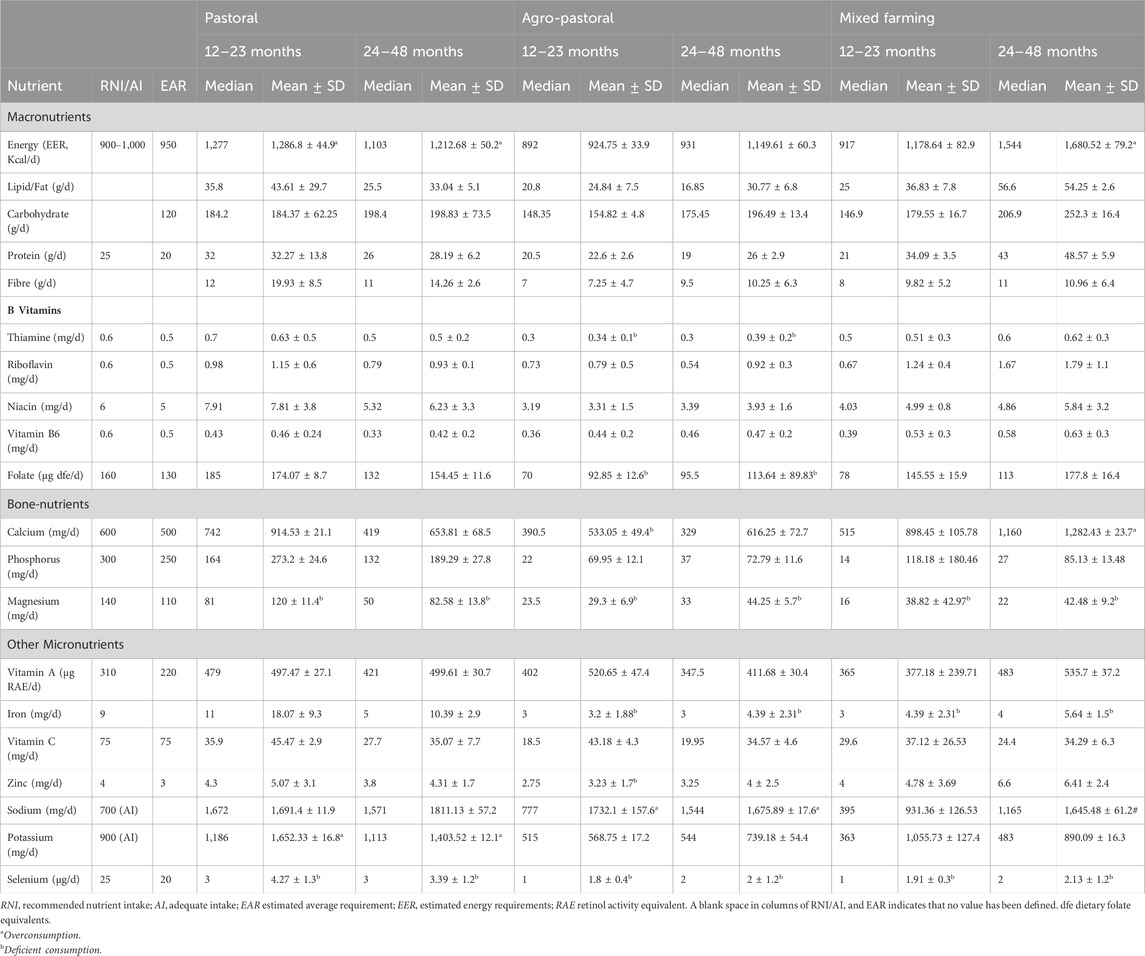
Table 3. Nutrient intakes from food and beverage of toddlers aged 12–48 months in Narok County, Kenya (n = 46).
Carbohydrate intake in the Mixed Farming group among the 24–48 months children exceeded the upper limit (252.3 ± 116.48 g/d vs. 120 g/day), while all other groups remained within the recommended range. Protein intake was generally adequate in pastoral (28.19 ± 6.2 g/d) and Agro-pastoral farming (26 ± 2.9 g/d), with children 24–48 months from Mixed farming system surpassing the RNI (48.57 ± 5.9 g/d vs. 20 g/d).
The intakes of Thiamine, Riboflavin, Niacin, Vitamin B6, and Folate generally met or exceeded the recommended values. For instance, the mean intake of Riboflavin in the Mixed Farming group was 1.79 ± 1.15 mg/d, surpassing the RNI of 0.6 mg/d.
The Mixed Farming group exceeded the RNI for Calcium, indicating potential overconsumption (mean: 1,282.43 ± 923.74 mg/d vs. 500 mg/d). Phosphorus intake was generally low across all groups, especially in 12–23 months and 24–48 months old children in the Agro-pastoral and Mixed Farming groups (69.95 ± 82.16 mg/d vs. 300 and 85.13 ± 133.48 mg/d vs. 300 mg/d) respectively. Magnesium intake was below the AI in all groups, indicating a potential deficiency.
Vitamin A intake was generally within or slightly above the recommended range for all groups. Iron intake varied, with the Pastoral and Agro-pastoral groups surpassing the RNI, while the Mixed Farming group deficient in its intake. Sodium intake was notably high in the Agro-pastoral and Mixed Farming groups (mean 1,675.89 ± 1,317.06 mg/d and 1,645.48 ± 161.02 vs. 700 mg/d) respectfully, suggesting a potential overconsumption, while Potassium intake was generally within the recommended range. Selenium intake was below the AI in all groups, indicating a potential deficiency.
3.4 Dietary intake for Women of reproductive age (15–49 years)
Table 4 presents dietary intake for Women of reproductive age (15–49 years) in three distinct farming systems in Kenya (n = 161). The macronutrient analysis reveals variations across the pastoral, agro-pastoral, and mixed farming groups. Notably, energy intake (EER) was highest in the pastoral group (2,365.11 ± 807.3 Kcal/d), while the mixed farming group exhibited the highest lipid/fat intake (52.99 ± 27.46 g/d). Carbohydrate and protein intake varied among the groups, with the agro-pastoral group showing the highest carbohydrate intake (437.74 ± 145.43 g/d) and the mixed farming group having the highest protein intake (51.07 ± 26.5 g/d). Antioxidant and B-vitamin analyses indicated mixed findings, with Vitamin C intake exceeding the recommended levels in all groups, while variations were observed in B-vitamin levels. Calcium, phosphorus, and magnesium exhibited differences among the farming systems with mixed framing (937.96 ± 686.23) having the highest mean calcium intake and the least mean intake in pastoral farming system (491.16 ± 306.91). Micronutrient analysis revealed diverse patterns, with vitamin A meeting recommendations, while zinc, iron and selenium intake felling below the Adequate Intake (AI) in all groups.
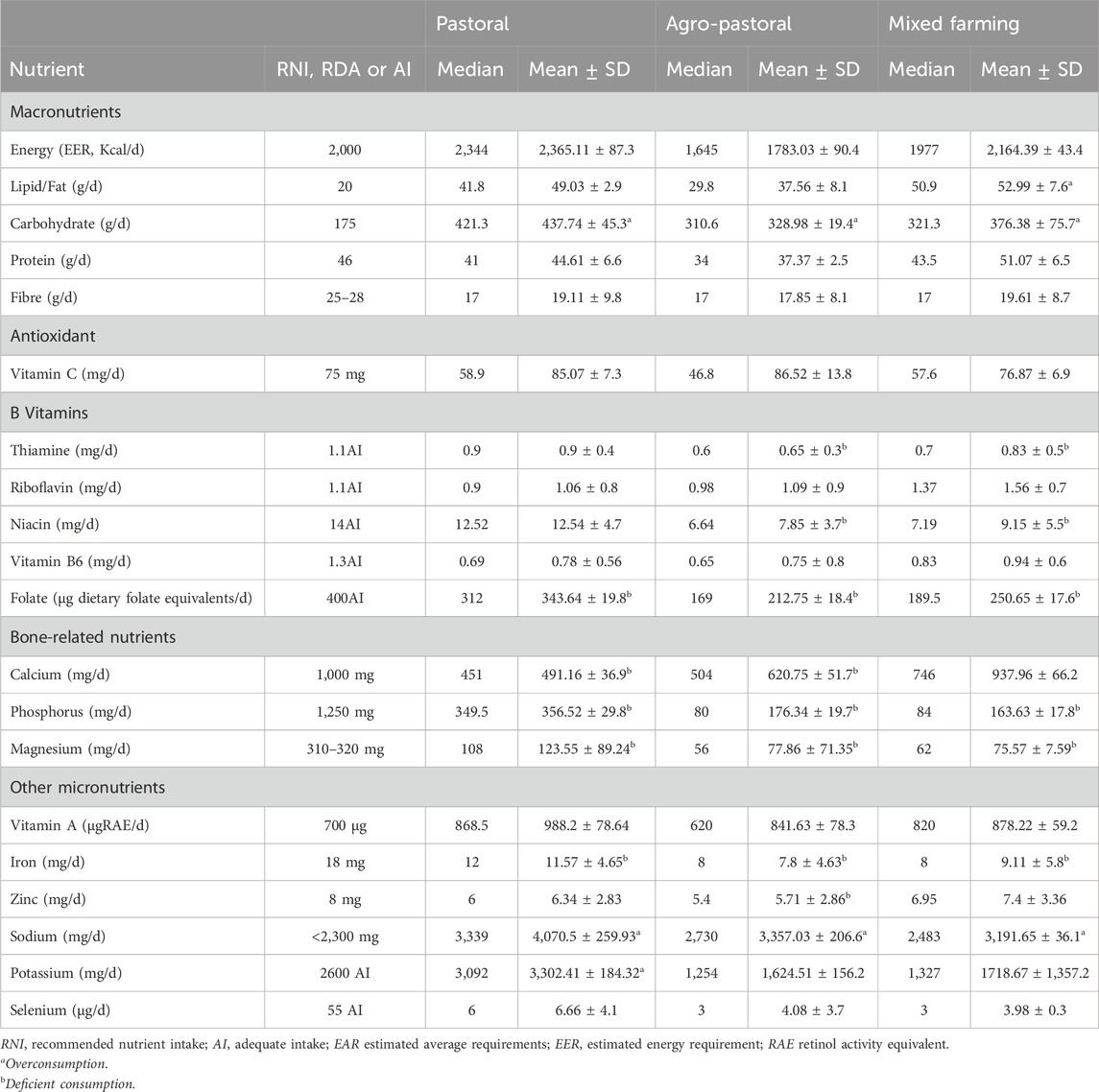
Table 4. Nutrient intakes of Women of reproductive age (15–49 years) in three farming systems in Kenya (n = 161).
4 Discussion
The mean nutrient intakes of children 6–48 months as well as mothers 15–49 years from pastoral, agro-pastoral and mixed farming systems of Kenya has been presented. To our knowledge, this is the first study of kind and the first to evaluate mean nutrient intakes from food and beverages and dietary supplement among children and mothers in pastoral, agro-pastoral and mixed farming systems in Kenya.
4.1 Nutrient intake of infants 6–11 months
Nutrient intake among children aged 6–11 months in the three farming systems in Kenya provide insights into both deficiencies and excesses, shedding light on the nutritional status of children 6–11 months in these farming systems. The observed deficiencies in thiamine, vitamin C, vitamin B6, selenium, niacin, and folate are consistent with studies conducted in other developing countries (Keats et al., 2021; Awoke et al., 2022; Shinde et al., 2022), highlighting common challenges in meeting micronutrient requirements among infants. Wakoli et al. (2023) in their micronutrient deficiency through dietary intake in Kenya observed that overreliance on starchy staples that are low in nutrition quality is to blame for increasing micronutrient deficiencies in children and women of reproductive age. In our findings, children 6–11 months surpassed the RDA for energy and carbohydrate in all the farming systems. This is an indication that the main source of nutrient was starchy staples which might have contributed to the low micronutrient levels in their intake.
The overconsumption of carbohydrates in children 6–11 months in this study mirrors trends observed in various developing countries undergoing a transition in nutrition. Dietary factors contributing to poor diet in children include the excessive consumption of energy-dense and micronutrient-poor foods, especially starchy staples (Jebeile et al., 2022; Li, Martin & Fernie, 2024). It is known that common foods consumed in the study area are cereal based which are naturally high in energy and carbohydrate. Elsewhere, Palandri et al. (2024) posits that overconsumption of carbohydrate is as a result of poor eating habits coupled with unsustainable production of diverse diets.
In the current study, while protein intake for children 6–11 met recommendations across all farming systems, variations existed in the adequacy of iron intake, with some infants being at risk of inadequate intake, especially in pastoral and Agro-pastoral farming systems. This highlights the importance of emphasising animal-source food consumption in addressing iron deficiency, timely initiation of complementary feeding, and promotion of dietary diversity practices (D’Auria et al., 2020; WHO, 2020). Moreover, the differences in vitamin A intake among farming systems suggest varying access to sources of this micronutrient, with implications for vision health and immune function (Nantel and Gingras, 2023). Animal source foods are rich sources of high-quality protein, essential fatty acids, and highly bioavailable micronutrients including iron, calcium, vitamin A, and B12 which contribute substantially to reducing childhood undernutrition and optimal development as well as reducing the double burden of malnutrition (Dasi et al., 2019).
4.2 Nutrient intake among children 12–48 months
The energy intake of children across all farming systems surpassed the EER. Children from the mixed farming system had the highest energy intake levels, potentially indicating an inclination towards overconsumption of calories. This finding aligns with previous research in Kenya, where studies have reported high energy intake among children in agricultural communities (Hotz et al., 2015; Kishino et al., 2024). However, it contrasts with findings from other developing countries where energy intake deficits are often observed among children in rural areas (Mengistu et al., 2017). Similarly, carbohydrate intake, particularly among children aged 24–48 months in the mixed farming system, exceeded the upper limit, suggesting a risk of overconsumption. This finding is consistent with studies conducted in Kenya (Waswa et al., 2021; Ronoh, 2017) in similar agricultural settings, where carbohydrate-rich diets are common due to the reliance on staple cereals. Thus, these findings underscore the importance of advocating for dietary diversity to ensure quality nutrient intake.
Protein intake was generally adequate across all farming systems, with children in the mixed farming group surpassing the Recommended Nutrient Intake (RNI). This finding coincides with study in similar settings (Danso-Abbeam et al., 2021) demonstrating the importance of animal-source foods in addressing protein intake among children in different agricultural systems (Musyoka et al., 2023). The micronutrient intake on the other hand revealed mixed outcome in the diets of children. While the intake of Thiamine, Riboflavin, Niacin, Vitamin B6, and Folate met the recommended levels of intake, concerns of overconsumption especially in calcium and sodium, and deficiencies in phosphorus and magnesium intake were noted. Iron intake varied across farming systems, with some groups surpassing the RNI while others remained within the recommended range. Overconsumption of a given nutrient has a negative health impact on the vulnerable population (Mosquera et al., 2024) and measures should be taken to overcome this challenge.
4.3 Nutrient intake among women 15–49 years
The macronutrient analysis among women 15–49 years revealed variations across the pastoral, agro-pastoral, and mixed farming groups. Energy intake (EER) was found to be highest in the pastoral group, indicating potentially overconsumption among mothers in the pastoral farming system. On the other hand, mothers in the mixed farming group exhibited the highest lipid/fat intake, which may reflect dietary habits influenced by available resources and food preferences within this community. These findings are consistent with the findings in similar study (Masibo et al., 2013; Seifu, 2021) where women of reproductive age were found to exhibit higher energy intake in their diets. This is however contrary to the findings by Tugjamba et al. (2023) who noted that women in small settlements and the nomadic community display patterns of long-term chronic energy deficiency that obscure short-term reproduction-related energy costs.
Women in farming systems also differed in terms of the amount of protein and carbohydrates they consumed; whereas women from the mixed farming system had the highest protein intake, those from the agro pastoral exhibited highest carbohydrate intake. These variations in the intake of macronutrients in this study may be explained by dietary habits that are impacted by unique cultural, environmental, and economic activities inherent in each farming system in the study areas. Furthermore, antioxidant and B-vitamin analyses showed that Vitamin C intake exceeded recommended levels in all groups. This suggests potential differences in dietary diversity and consumption of fruits and vegetables rich in antioxidants among the farming communities. Moreover, disparities in micronutrient intake were evident, with vitamin A and zinc intakes meeting or exceeding recommendations, while selenium intake fell below the Adequate Intake (AI) in all groups. These findings confirm the earlier finding among women of reproductive age where micronutrient malnutrition was found to be high due to overliance on poor diets (Harika et al., 2017; Wakoli et al., 2023).
5 Conclusion
This study explored the dietary habits of children and women across different agricultural systems, revealing critical nutritional disparities. Children in pastoral, agropastoral, and mixed farming systems generally had sufficient Vitamin A and protein intake. However, there was a notable deficiency in essential micronutrients such as iron, zinc, folate, and riboflavin across all systems, indicating a risk of micronutrient malnutrition that threatens the growth and development of children aged 6–48 months. Addressing these deficits is crucial to prevent long-term health issues and socioeconomic setbacks. Among women aged 15–49, dietary intake varied significantly by farming system. Women from pastoral setting had the highest energy intake, possibly indicating overconsumption, while women from mixed farming had the highest fat intake, likely influenced by local resources and preferences. Despite adequate Vitamin A intake, zinc, iron, and selenium levels were below the Adequate Intake (AI) across all groups, underscoring a critical need for tailored nutritional interventions. Enhancing awareness and promoting balanced dietary practices are essential steps toward improving health outcomes for women and children in these communities. Continued research is necessary to understand these dietary patterns better and develop strategies to address nutritional deficiencies in vulnerable populations.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Scientific and Ethics Review Unit (SERU) of Kenya Medical Research Institute (KEMRI) (Protocol No. SERU 4432). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
HW: Conceptualization, Investigation, Methodology, Validation, Writing–original draft, Writing–review and editing. GA: Validation, Writing–original draft, Writing–review and editing. CM: Validation, Writing–original draft, Writing–review and editing. JM: Validation, Writing–original draft, Writing–review and editing. NM: Data curation, Methodology, Validation, Writing–original draft, Writing–review and editing. GO: Data curation, Software, Writing–original draft, Writing–review and editing. ST: Validation, Writing–original draft, Writing–review and editing. ZB: Conceptualization, Methodology, Validation, Writing–original draft, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was funded in whole or part by the United States Agency for International Development (USAID) Bureau for Resilience and Food Security under Agreement # 7200AA20CA00022 as part of Feed the Future Innovation Lab for Animal Health. Any opinions, findings, conclusions, or recommendations expressed here are those of the authors alone.
Acknowledgments
The authors would like to express their gratitude to the Animal Health Innovation Lab (AHIL)-Kenya, The Department of Food Science, Nutrition and Technology University of Nairobi, Centre for Public Health Research (CPHR-KEMRI), The Centre for Epidemiological Modelling and Analysis (CEMA) at the University of Nairobi, WSU Global Health-Kenya, Narok County Administration, research assistants, participants, community leadership in the study area for their invaluable role throughout the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Awoke, M., Menber, Y., Desyibelew, H. D., Dagne, S., Tadesse, T., and Wassihun, Y. (2022). Micronutrient intake inadequacy and its associated factors among lactating women in Bahir Dar city, Northwest Ethiopia, 2021. Plos one 17 (7), e0271984. doi:10.1371/journal.pone.0271984
Bartzke, G. S., Ogutu, J. O., Mukhopadhyay, S., Mtui, D., Dublin, H. T., and Piepho, H. P. (2018). Rainfall trends and variation in the Maasai Mara ecosystem and their implications for animal population and biodiversity dynamics. PloS one 13 (9), e02028144e.
Bechoff, A., De Bruyn, J., Alpha, A., Wieringa, F., and Greffeuille, V. (2023). Exploring the complementarity of fortification and dietary diversification to combat micronutrient deficiencies: a scoping review. Curr. Dev. Nutr. 7, 100033. doi:10.1016/j.cdnut.2023.100033
Danso-Abbeam, G., Dagunga, G., Ehiakpor, D. S., Ogundeji, A. A., Setsoafia, E. D., and Awuni, J. A. (2021). Crop–livestock diversification in the mixed farming systems: implication on food security in Northern Ghana. Agric. Food Secur. 10, 35–14. doi:10.1186/s40066-021-00319-4
Dasi, T., Selvaraj, K., Pullakhandam, R., and Kulkarni, B. (2019). Animal source foods for the alleviation of double burden of malnutrition in countries undergoing nutrition transition. Anim. Front. 9 (4), 32–38. doi:10.1093/af/vfz031
D’Auria, E., Borsani, B., Pendezza, E., Bosetti, A., Paradiso, L., Zuccotti, G. V., et al. (2020). Complementary feeding: pitfalls for health outcomes. Int. J. Environ. Res. public health 17 (21), 7931. doi:10.3390/ijerph17217931
FAO (2018). Dietary Assessment: a resource guide to method selection and application in low resource settings. Rome.
Flax, V. L., Ouma, E., Izerimana, L., Schreiner, M. A., Brower, A. O., Niyonzima, E., et al. (2021). Animal source food social and behavior change communication intervention among girinka livestock transfer beneficiaries in Rwanda: a cluster randomized evaluation. Glob. Health Sci. Pract. 9 (3), 640–653. doi:10.9745/GHSP-D-21-00082
Harika, R., Faber, M., Samuel, F., Kimiywe, J., Mulugeta, A., and Eilander, A. (2017). Micronutrient status and dietary intake of iron, vitamin A, iodine, folate and zinc in women of reproductive age and pregnant women in Ethiopia, Kenya, Nigeria and South Africa: a systematic review of data from 2005 to 2015. Nutrients 9 (10), 1096. doi:10.3390/nu9101096
Hotz, C., Pelto, G., Armar-Klemesu, M., Ferguson, E. F., Chege, P., and Musinguzi, E. (2015). Constraints and opportunities for implementing nutrition-specific, agricultural and market-based approaches to improve nutrient intake adequacy among infants and young children in two regions of rural Kenya. Maternal Child Nutr. 11, 39–54. doi:10.1111/mcn.12245
Jebeile, H., Kelly, A. S., O'Malley, G., and Baur, L. A. (2022). Obesity in children and adolescents: epidemiology, causes, assessment, and management. lancet Diabetes and Endocrinol. 10 (5), 351–365. doi:10.1016/S2213-8587(22)00047-X
Keats, E. C., Oh, C., Chau, T., Khalifa, D. S., Imdad, A., and Bhutta, Z. A. (2021). Effects of vitamin and mineral supplementation during pregnancy on maternal, birth, child health and development outcomes in low-and middle-income countries: a systematic review. Campbell Syst. Rev. 17 (2), e1127. doi:10.1002/cl2.1127
Kenya National Bureau of Statistics (KNBS) (2022). Demographic and Health Survey 2022. Nairobi: KNBS.
Kenya National Bureau of Statistics (KNBS) and ICF Macro (2010). Kenya Demographic and Health Survey 2008-09. Calverton, Maryland: KNBS and ICF Macro.
Kim, S. S., Nguyen, P. H., Tran, L. M., Abebe, Y., Asrat, Y., Tharaney, M., et al. (2019). Maternal behavioural determinants and livestock ownership are associated with animal source food consumption among young children during fasting in rural Ethiopia. Maternal child Nutr. 15 (2), e12695. doi:10.1111/mcn.12695
Kishino, M., Hida, A., Ishikawa-Takata, K., Tada, Y., Kariuki, L., Maundu, P., et al. (2024). Relationship of dietary intake between children aged 12–59 months and their mothers in rural Kenya: a cross-sectional study in two seasons. J. Hum. Nutr. Dietetics 37 (2), 491–502. doi:10.1111/jhn.13271
Leroy, J. L., and Alonso, S. (2024). Animal-source foods: their role in sustainable healthy diets. IFPRI book chapters, 62–70.
Li, J., Martin, C., and Fernie, A. (2024). Biofortification’s contribution to mitigating micronutrient deficiencies. Nat. Food 5, 19–27. doi:10.1038/s43016-023-00905-8
Margolies, A., Kemp, C. G., Choo, E. M., Levin, C., Olney, D., Kumar, N., et al. (2022). Nutrition-sensitive agriculture programs increase dietary diversity in children under 5 years: a review and meta-analysis. J. Glob. health 12, 08001. doi:10.7189/jogh.12.08001
Masibo, P. K., Buluku, E., Menya, D., and Malit, V. C. (2013). Prevalence and determinants of under-and over-nutrition among adult Kenyan women; evidence from the Kenya Demographic and Health survey 2008-09.
Mengistu, G., Moges, T., Samuel, A., and Baye, K. (2017). Energy and nutrient intake of infants and young children in pastoralist communities of Ethiopia. Nutrition 41, 1–6. doi:10.1016/j.nut.2017.02.012
Mosquera, E. M. B., Tonon, K. M., Augusto, R. A., de Carvalho, T. M., and Morais, M. B. D. (2024). Improving the nutritional status of socially vulnerable children in manaus, Brazilian amazon, through a food supplementation programme. Nutrients 16 (7), 1051. doi:10.3390/nu16071051
Musyoka, M. M., Bukachi, S. A., Muga, G. O., Otiang, E., Kwoba, E. N., and Thumbi, S. M. (2023). Addressing child and maternal nutrition: a qualitative study on food prescriptions and proscriptions determining animal source food consumption in rural Kenya. Food Secur. 15 (4), 901–917. doi:10.1007/s12571-023-01368-2
Nantel, A., and Gingras, V. (2023). Are complementary feeding practices aligned with current recommendations? A narrative review. Children 10 (5), 794. doi:10.3390/children10050794
Ngala, S. A. (2015). Evaluation of dietary diversity scores to assess nutrient adequacy among rural Kenyan women. Wageningen University and Research.
Ochola, S., and Masibo, P. K. (2014). Dietary intake of schoolchildren and adolescents in developing countries. Ann. Nutr. Metabolism 64 (Suppl. 2), 24–40. doi:10.1159/000365125
Palandri, L., Rocca, L., Scasserra, M. R., Vigezzi, G. P., Odone, A., Iughetti, L., et al. (2024) “Investigating eating habits of children aged between 6 Months and 3 Years in the provinces of modena and reggio emilia: is our kids’ diet sustainable for their and the planet’s health?,” in Healthcare. MDPI, 453.
Ronoh, A. K., Were, G. M., Wakhu-Wamunga, F., and Wamunga, J. B. (2017). Food consumption patterns among pre-school children 3-5 years old in Mateka, Western Kenya. Food Nutr. Sci. 8 (08), 801–811. doi:10.4236/fns.2017.88057
Seifu, W. (2021). Nutritional status of woman reproductive age (15-49) and proximate analysis of selected traditional foods of asayita town, Afar region, Ethiopia. Doctoral dissertation, Haramaya university.
Shinde, S., Wang, D., Yussuf, M. H., Mwanyika-Sando, M., Aboud, S., and Fawzi, W. W. (2022). Micronutrient supplementation for pregnant and lactating women to improve maternal and infant nutritional status in low-and middle-income countries: protocol for a systematic review and meta-analysis. JMIR Res. Protoc. 11 (8), e40134. doi:10.2196/40134
Tugjamba, N., Walkerden, G., and Miller, F. (2023). Adapting nomadic pastoralism to climate change. Clim. Change 176 (4), 28. doi:10.1007/s10584-023-03509-0
United Nations Children’s Fund. (UNICEF) (2020). Nutrition, for every child: UNICEF nutrition Strategy 2020–2030. New York: UNICEF.
United Nations Children’s Fund (UNICEF) (2023) “Early childhood development,” in UNICEF vision for every child. New York: UNICEF. Available at: https://www.unicef.org/media/145336/file/Early_Childhood_Development_-_UNICEF_Vision_for_Every_Child.pdf.
Wakoli, K. S., Muthoni, N. E., Mwaka, M. P., and Tunje, K. T. (2023). Assessment of micronutrient deficiency through dietary intake, food consumption practices and nutritional status amongst women of reproductive age in kongowea, mombasa county. Eur. J. Med. Health Res. 1 (2), 122–129. doi:10.59324/ejmhr.2023.1(2).17
Waswa, L. M., Jordan, I., Krawinkel, M. B., and Keding, G. B. (2021). Seasonal variations in dietary diversity and nutrient intakes of women and their children (6–23 months) in Western Kenya. Front. nutr. 8, 636872.
Were, J. M., Stranges, S., Wilk, P., Ali, S., Sharma, I., Vargas-Gonzalez, J. C., et al. (2023). The double burden of malnutrition among women of reproductive age and preschool children in low-and middle-income countries: a scoping review and thematic analysis of literature. Nutrition 111, 112053. doi:10.1016/j.nut.2023.112053
Keywords: agro-pastoral, child, mother, mixed farming, nutrient intakes, pastoral farming
Citation: Wakhungu HK, Abong’ G, Muthike C, Muema J, Mutono N, Omondi GP, Thumbi SM and Bukania Z (2024) Assessment of dietary intake in children (6–48 months) and mothers (15–49 years) in different farming systems in Kenya using multiple pass 24-h recall. Front. Food. Sci. Technol. 4:1430391. doi: 10.3389/frfst.2024.1430391
Received: 09 May 2024; Accepted: 11 July 2024;
Published: 15 August 2024.
Edited by:
José S. Câmara, Universidade da Madeira, PortugalReviewed by:
Waseem Khalid, Government College University, Faisalabad, PakistanNaohisa Shobako, Kyoto University, Japan
Copyright © 2024 Wakhungu, Abong’, Muthike, Muema, Mutono, Omondi, Thumbi and Bukania. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: H. K. Wakhungu, aGlsd2FrODhAZ21haWwuY29t
 H. K. Wakhungu
H. K. Wakhungu G. Abong’
G. Abong’ C. Muthike
C. Muthike J. Muema
J. Muema N. Mutono
N. Mutono G. P. Omondi
G. P. Omondi S. M. Thumbi
S. M. Thumbi Z. Bukania3,8
Z. Bukania3,8