- Department of Psychology, University of Nevada, Las Vegas, Las Vegas, NV, United States
Rates of mental disorder for youth have increased substantially over recent years and this trend, coupled with persistent barriers to community-based care, has led researchers and others toward a “where they are” approach that emphasizes preventative and health promotion practices within ecologically valid environments such as schools. A key mechanism of this approach involves multi-tiered systems of support (MTSS) models that allocate supports based on student need across multiple domains of functioning. MTSS models have been implemented with moderate success but students in rural districts may be underserved. This article introduces a blueprint for a sample MTSS approach in rural schools by initially presenting their challenges and advantages as well as implementation science frameworks, and particularly the School Implementation Strategies, Translating ERIC Resources (SISTER) project, geared toward educational settings. The blueprint incorporates SISTER pillars rated highest for importance and feasibility throughout linchpin strategies to set the basis for the MTSS model; readiness strategies to determine needs, structure, and feasibility; Tier 1 strategies to implement preventative practices and address emerging cases; Tier 2 strategies to provide early intervention services for acute cases; Tier 3 strategies to provide intensive intervention services for chronic and severe cases; and strategies to enhance sustainability (including fidelity) and expansion. The blueprint thus represents a blending of emerging implementation science ideas with real-world constraints often evident in rural schools to provide a practice perspective and one set of ideas to promote discussion and innovation for a key underserved student constituency.
1 Introduction
Rates of mental disorder for children and adolescents have increased substantially over recent decades and particularly in the post-pandemic era (World Health Organization, 2023). The prevalence of mental disorder has been estimated to be 12.7% among youths in high-income counties, 13.4% among youths worldwide, and likely higher among youths in low- and middle-income countries (Barican et al., 2022; Kieling et al., 2011; Polanczyk et al., 2015). Unfortunately, the combined treatment rate for any child or adolescent mental disorder is only 38% (Wang et al., 2023). This is partly due to substantial and persistent barriers to community-based care, especially for underserved youths, that include inaccessible and too few care providers, mistrust of care providers, dearth of specialized care options, cultural and language differences, lack of insurance, discontinuity of care, limited mental health literacy and knowledge of help-seeking processes, transportation vulnerability, competing family priorities and time poverty, excessive cost, stigma, and protracted wait times (Castro-Ramirez et al., 2021; Gage et al., 2025; Radez et al., 2022). In addition, many children and adolescents are placed in juvenile justice, child protective services, residential, or related supervisory agencies where mental health care options may be quite underdeveloped (Scott C. K. et al., 2019).
In response, advocates of mental health care for children and adolescents have gravitated toward a “where they are” approach that emphasizes preventative and health promotion practices within the context of ecologically valid environments such as schools (Weist et al., 2023). Indeed, mental health and other key services for youths worldwide often occur within the context of educational settings (Margaretha et al., 2023). In the United States, schools are sometimes referred to as a de facto mental health system (Burns et al., 1995) given that up to 80% of youths who receive such care do so to some extent in these settings (Lyon et al., 2019). Schools are the most common location for mental health service utilization for youths, and more so for those with elevated symptomatology or clinical diagnoses (Duong et al., 2021). This process has been driven partly by legislative and policy directions that emphasize school-based mental and behavioral health services, mental health awareness training, and crisis intervention and safety procedures as well as school-based reimbursement for mental health services or physical, speech, and occupational therapy (e.g., via Individuals with Disabilities Education Act funding or Medicaid) (Ali et al., 2019). In addition, a key advantage of utilizing schools in this regard is that they can serve as “soft entry” points for care via centralized access to multiple avenues of resources, partnerships with external support agencies, and greater family engagement due to less stigma and financial and transportation challenges (McGorry et al., 2022).
2 Multi-tiered systems of support
An emerging mechanism for service delivery within schools involves multi-tiered models or continua of supports based on student need across multiple domains of functioning (Benner et al., 2013). These models, embedded in various pieces of federal legislation, are designed to help school officials and other stakeholders move away from a “wait to fail” approach and instead more proactively identify and ameliorate student performance challenges (Splett et al., 2018; Zirkel, 2017). Main components of these models thus often include regular screening and progress monitoring; evidence-based assessment, intervention, and decision-making practices; implementation fidelity; and incorporation with existing school-based improvement plans and health services (Collins et al., 2019). Partnerships with external entities such as researchers, universities, professional development entities, or community practice or government agencies are common as well (Goldstein et al., 2019).
Multi-tiered models of school-based service delivery are typically trichotomous in nature and emphasize universal or primary prevention practices to promote adaptive behavior and address emerging problems (Tier 1); early, selective intervention or secondary prevention practices to address acute and less severe problems (Tier 2); and intensive intervention or tertiary prevention practices to address chronic and severe problems (Tier 3) (Stoiber and Gettinger, 2016). Tier 1 supports often represent school-wide practices to prevent a particular condition from emerging. Tier 2 supports often represent targeted initial interventions for emerging cases of a condition as well as a focus on at-risk youth who have yet to display serious symptomatology. Tier 3 supports often represent indicated interventions for youth with a particular condition in order to lessen or ameliorate the effects of the condition (McIntosh and Goodman, 2016). A particular student could receive one or more tiers of support (Morse, 2024).
Some multi-tiered models have been designed to address a particular domain of student performance such as academic (e.g., Response to Intervention; Fletcher and Vaughn, 2009) or behavioral (e.g., Positive Behavioral Interventions and Supports; Bradshaw et al., 2015) functioning. Other multi-tiered models have been designed to address multiple domains of functioning (e.g., Integrated Multi-Tiered Systems of Support; Thomas et al., 2023); to enhance other, existing multi-tiered models by improving social and emotional functioning (e.g., Social–Emotional Learning in a Multi-tiered System; Olson et al., 2022); and to merge with school mental health, community, and family partners toward a synergistic ecological approach for complex, multifaceted problems such as school climate/student discipline (e.g., Interconnected Systems Framework; Weist et al., 2023). These approaches are collectively referred to in this article as multi-tiered systems of support (MTSS) (Loftus-Rattan et al., 2023).
MTSS approaches have been used to address broad school as well as specific student issues. MTSS approaches have been used to enhance school safety and engagement, boost literacy and academic performance, reduce school violence, and ameliorate inequities in access to student services and supports on a districtwide scale (Bohnenkamp et al., 2023; Bradshaw et al., 2021). In addition, MTSS approaches have been adapted for specific student challenges such as aggression and defiance (Waschbusch et al., 2019), anxiety (Jones et al., 2019), attention-deficit/hyperactivity disorder (Fabiano and Pyle, 2019), autism (Leytham et al., 2021), depression (Arora et al., 2019), suicide prevention (Singer et al., 2019), trauma (Reinbergs and Fefer, 2018; Smith et al., 2025), and mental health needs among homeless youth (Sulkowski and Michael, 2014). Multidimensional MTSS approaches have also been designed for various domains relevant to heterogeneous problems such as school absenteeism (Kearney and Graczyk, 2020, 2022). Multi-tiered frameworks including MTSS approaches have been found to be moderately effective for cultivating the organizational health of schools and educational districts and for improving student outcomes, though evidence continues to emerge (Lee and Gage, 2020; Nitz et al., 2023).
At the same time, MTSS approaches carry significant logistical, instructional, structural, and financial challenges for many school districts (Durrance, 2023). In particular, a key predictor of better MTSS outcome is implementation with high fidelity, which can be especially difficult in educational settings with limited resources, considerable population, and large geographical size (Scott T. M. et al., 2019). In addition, MTSS approaches often must be tailored to the individual characteristics of a given school or educational level to enhance acceptability (Eagle et al., 2015), but such nuances in the literature remain sparse. MTSS approaches are also needed particularly for rural schools given that many youths worldwide are educated in rural districts (Echazarra and Radinger, 2019). In the United States, 28% of public schools are in rural areas and enroll 19% of all public-school students, and 53% of all school districts serve at least some rural students (National Center for Education Statistics, 2023).
MTSS approaches in rural schools are emerging, often in case study format (e.g., Shenoy et al., 2024; Vetter et al., 2024). Researchers and other stakeholders in this area have focused on key barriers to implementation in rural districts, including lack of data-based decision making, one-size-fits-all interventions, uncoordinated teams, low administrator support, and limited training (Olsen et al., 2023; Nygaard et al., 2025; Ormiston et al., 2025). Others, however, have posed new frameworks for developing MTSS approaches in rural schools with an eye toward further testing (Calvert et al., 2023; Turner et al., 2022). In addition, key mechanisms related to the success of MTSS approaches, such as collaborative and interdisciplinary leadership teams, are becoming better understood (Porter, 2022). At the same time, however, researchers and practitioners have called for greater integration of community school approaches and implementation guidelines vis-à-vis rural schools in particular (Knox et al., 2024; Santiago et al., 2025).
The primary purpose of this article is to offer a practice perspective for improving mental health care for underserved youths in rural schools via a multi-tiered systems of support mechanism supported by implementation guidelines. A practice perspective is emphasized for several reasons. First, as mentioned, empirical data on MTSS approaches continue to emerge in general, and less data are available with respect to rural educational settings. Second, many rural districts have very limited resources and no formalized school-based health or mental health centers, necessitating an almost no-added-cost approach (Graves et al., 2020). Indeed, multi-tiered approaches are often abandoned by school districts due to excessive expense, complexity, and burden (Kittelman et al., 2020). Third, the field of implementation science to advance multi-tiered systems of support mechanisms continues to evolve but can be overwhelming and confusing due to a plethora of frameworks and jargonistic and often murky terminology (Curran, 2020; Goldstein and Olswang, 2017). Implementation science has also been criticized for divestiture from real-world constraints and policy considerations, including the removal of harmful operations (Crable et al., 2022). A practice perspective for rural schools must therefore rely on appropriate implementation guidelines trimmed to the most valuable elements.
This article thus draws upon known challenges to rural schools and their communities, an implementation framework designed specifically for educational settings and evaluated for importance and feasibility, and a sample MTSS model based heavily on extant infrastructure to advance a practice perspective. A potential blueprint is provided for relying on existing yet high-value targets (available resources that are critical to achieve objectives) as well as an economical implementation framework to enhance sustainability. Although such a blueprint could be extended to care more broadly, such as to medical or developmental care, this article focuses on mental health care. About 85% of federally designated mental health professional shortage areas in the United States are in rural settings and about 60% of rural areas have been deemed underserved vis-à-vis mental health practice (Keeler et al., 2018). The article proceeds next with a discussion of challenges and advantages especially pertinent to rural schools and communities. The following sections then introduce implementation frameworks with an emphasis on one designed especially for educational settings. Subsequent sections detail a sample MTSS model for mental health care in rural schools within the context of key implementation pillars.
3 Challenges and advantages of rural schools and communities
Many rural schools and communities hold special challenges with respect to service care delivery compared to urban and suburban areas, and rural residents thus often experience significant disparities in mental health outcomes compared to metropolitan areas (Morales et al., 2020). A key challenge is extended physical distance between remote locations, meaning that rural communities often lack public transportation and broadband internet and require longer driving distances to services (Douthit et al., 2015). In related fashion, if urgent family or other services are needed at home, intervention delays can be substantial (Chung et al., 2016). Many rural communities experience a lack of qualified (e.g., Master’s/doctoral-level) mental health professionals, particularly with respect to demand for specialized services (Hoeft et al., 2018). Concerns about confidentiality and financial obligations due to greater poverty are especially pertinent in rural settings as well (Cheesmond et al., 2019). Others have noted that mental health challenges may be more stigmatizing in rural than urban communities (Polaha et al., 2015) and that such stigma may intersect with greater wariness of outside influences, psychological barriers to help-seeking, and cultural mismatches with providers who may lack familiarity with local customs (Hagen et al., 2022). These factors can contribute to less overall service utilization (Schultz et al., 2021).
Such challenges in rural schools and communities carry specific ramifications for MTSS approaches as well. Full-scale or formal implementation of a MTSS framework may be too costly, cumbersome, and labor-intensive for rural schools with limited resources (Yell, 2018). This applies particularly to training requirements and staff development as well as to specialized positions needed to support such a framework, such as program coordinators (Robinson et al., 2013). Rural schools also tend to have less class subject variability and specialized courses, which can limit curriculum-based MTSS intervention components, and greater challenges recruiting and training teachers (Wallender et al., 2020). Many parents in rural communities also have seasonal or other nonstandard work schedules (e.g., in agriculture, energy, mining) that require frequent relocation or time away from families, which can impact involvement in school-related activities (Katras et al., 2015). Economic pull factors also contribute to premature student departure from school prior to graduation (McDermott et al., 2018).
At the same time, rural schools and communities have unique advantages that could be leveraged to support MTSS approaches. More broadly, schools are often a central institutional and economic nexus point for rural communities (Frankland, 2021). Rural school settings are an important impetus for social cohesion and community identity, particularly via clubs, extracurricular activities, sports teams, and service initiatives (Hemming, 2018). Rural schools often serve multiple civic, business, and cultural functions in addition to their educational mandate (Schafft, 2016). In addition, children in rural communities often have greater access to extended family and kinship that frequently intersects with school officials at multigenerational levels (Vernon-Feagans and Swingler, 2020). All of these factors may help counterbalance barriers to, and increase engagement with, culturally responsive school-based mental health care in rural communities. In addition, frameworks to boost engagement in school-based mental health care in rural schools also emphasize the need to focus on cultural identity, insurance coverage, and community norms to develop interventions that best reduce mental health disparities (Morales et al., 2020).
More specifically, rural educational settings often involve smaller school-based teams and networks, including within and between schools in a district as well as with parents and central administrators. Communications may be more efficient because team members often assume multiple roles, meaning less need for frequent data collection and fewer scheduled meetings, and can align MTSS approaches more readily across a smaller and more compact K-12 system (Bailey, 2014). Rural schools also tend to be less bureaucratic and potentially more receptive to external sources of support, assuming low cost and burden (Lakin et al., 2021). Smaller class sizes, more personalized approaches to student need, and less violence are also characteristic of rural schools, which can facilitate an increased focus on mental health care (Johnson et al., 2021). Rural schools often benefit from considerable community support and ethos as well, meaning potentially greater buy-in and enthusiasm for school-based services (Seelig and McCabe, 2021). This may be especially the case if such services are culturally and linguistically responsive to the surrounding community, including Indigenous, BIPOC, migrant, and undocumented communities (Hoover and Soltero-González, 2018; Jongen et al., 2023). Practical recommendations in this regard can include adoption of strengths-based perspectives, shared decision-making with youth and families, reliance on trusted community partners vis-à-vis minoritized populations, use of accessible family-school communication processes, and providing educator support with respect to professional development, accountability, and social and emotional capacities (Beason et al., 2024).
4 Implementation science frameworks
The field of implementation science involves the scientific study of methods to promote the systematic uptake of evidence-based practices into routine settings to improve the quality and effectiveness of health services (Eccles and Mittman, 2006). Implementation science often focuses on strategies to overcome barriers to, and enhance facilitators of, such uptake (Bauer and Kirchner, 2020). Some of these efforts are targeted toward specific settings to sustain improvements in health and related outcomes among the setting’s constituents as well as the setting’s organizational context (Lobb and Colditz, 2013). Frameworks to organize and define the main pillars and prescriptive steps associated with implementation science, the components of which are briefly described next, are designed to better facilitate the adoption of evidence-based procedures into routine general practice (Bauer et al., 2015). The field of implementation science is also evolving toward a greater understanding of the key mechanisms of how these strategies work to influence service care delivery (Lewis et al., 2018). Part of this latter approach involves evaluating different implementation strategies along key metrics related to importance and feasibility (Hull et al., 2019).
Implementation frameworks have been designed for many different clinical and health care contexts (see, in particular, Damschroder et al., 2022; Glasgow et al., 2019; Meyers et al., 2012; Moullin et al., 2019). Nilsen and Bernhardsson (2019) identified four key contextual dimensions across these frameworks. The micro level of health care dimension included individual characteristics of the target population that could affect implementation, including attitudes, knowledge, and specific needs, among others. The meso level of health care dimension included organizational characteristics such as climate, readiness for change, support, and available structures. The macro level of health care dimension included wider, exogeneous influences such as policies and legislative mandates. The multiple levels of health care dimension included important supportive aspects related to social relations, financial resources, leadership, time availability, feedback, and the physical environment. Nilsen (2020) further noted that the complexity of dimensions within the implementation science framework literature means that combining the merits of multiple approaches in this regard may be desirable, with an added dose of “common sense” to adapt theories to specific contexts and across ecological levels.
One implementation framework partly adapted for mental health care, the Expert Recommendations for Implementing Change (ERIC) project, involved a compilation of 73 consensus-based strategies across nine main categories (Powell et al., 2015). These categories included engage consumers (e.g., patients and family members); use evaluative and iterative strategies (e.g., feedback); change infrastructure (e.g., record systems); adapt and tailor to the context (e.g., use data experts); develop stakeholder interrelationships (e.g., academic partnerships); utilize financial strategies (e.g., alter incentive structures); support clinicians (e.g., create new teams); provide interactive assistance (e.g., local technical support); and train and educate stakeholders (e.g., provide ongoing consultation). A key advantage of this approach is that the strategies were also evaluated for importance and feasibility. As such, decision-makers were equipped with a prioritization method for planning implementation initiatives (Waltz et al., 2015).
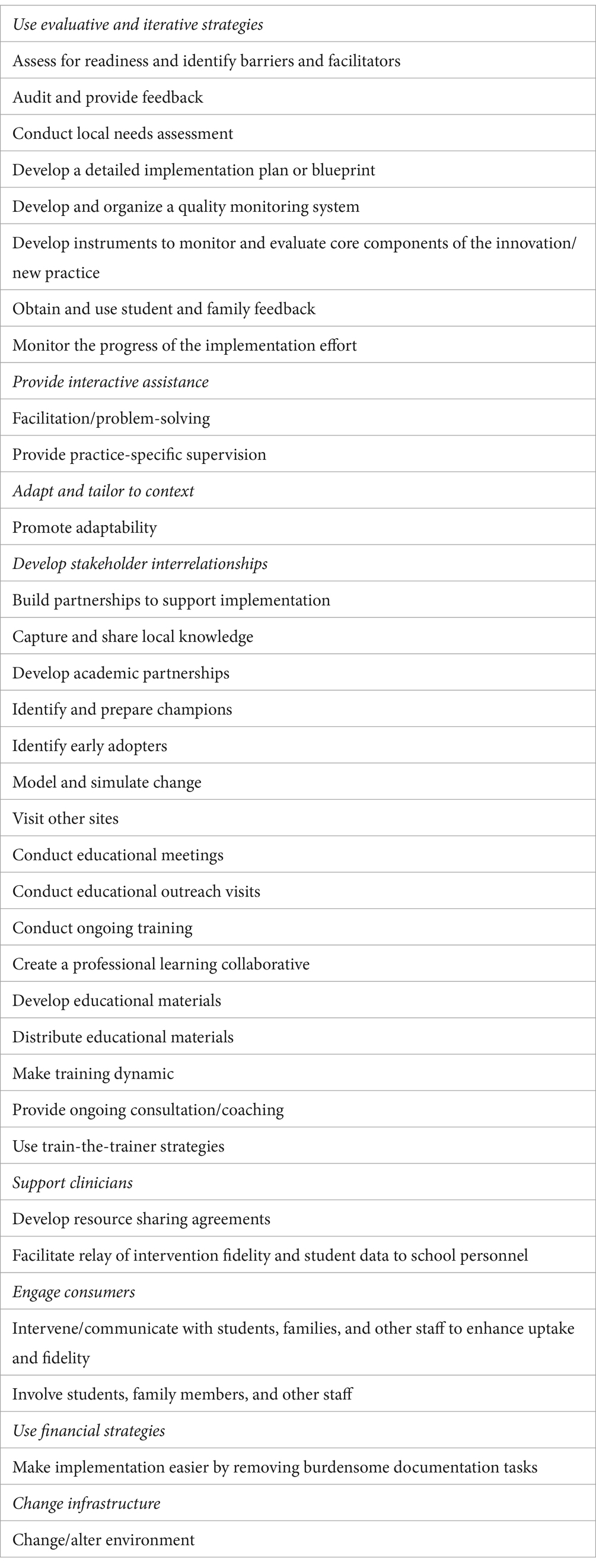
The ERIC implementation framework was further adapted to specific contexts and across ecological levels via the School Implementation Strategies, Translating ERIC Resources (SISTER) project that focused on the educational sector (Cook et al., 2019). This project resulted in 75 unique school-based implementation strategies that were arranged into the nine ERIC categories. Lyon et al. (2019) subsequently asked evaluators to rate each strategy for importance and feasibility (i.e., 1 = relatively unimportant/not at all feasible; 5 = extremely important/extremely feasible) and derived 33 that were deemed to be most valuable (Table 1). These 33 SISTER strategies form the basis and guide for the practice perspective guidelines presented in the next sections for the sample MTSS model for rural schools. Lyon and Bruns (2019) noted that these strategies for program implementation in school-based settings should be supplemented with a consideration of determinants (e.g., barriers, facilitators), mechanisms of action (e.g., skill development), and outcomes (e.g., student wellness). Larson and Cook (2023) further added recommendations for these strategies vis-à-vis feasible fidelity measurement (e.g., adherence to a data collection process), penetration (e.g., number of students who actually receive a service), and sustainability (e.g., ongoing efforts to provide services despite staff turnover).
5 Sample MTSS model for rural schools
The next sections outline key components of a sample, practice perspective-based MTSS model for mental health services for rural school youths. SISTER implementation strategies (Table 1) are included in each section to illustrate their incorporation into the sample MTSS model. These sections include: linchpin strategies to set the basis for the model; readiness strategies to determine needs, structure, and feasibility; Tier 1 strategies to implement preventative practices and address emerging cases; Tier 2 strategies to provide early intervention services for acute cases; Tier 3 strategies to provide intensive intervention services for chronic and severe cases; and strategies to enhance sustainability (including fidelity) and expansion for continuity purposes. These sections were chosen in accordance with stages common to implementation completion, which generally include pre-implementation (linchpin and readiness strategies), implementation (Tier 1, Tier 2, and Tier 3 strategies), and sustainability (continuation strategies) (Moore et al., 2017; Saldana, 2014). Note that linchpin and readiness strategies in rural districts typically involve a lengthy process, at least two years (Frankland, 2021; Webb and Michalopoulou, 2021). Linchpin and readiness strategies must be fully established and in place prior to any formal implementation.
5.1 Linchpin strategies
Several key SISTER strategies important for setting the basis for the sample MTSS model involve promoting adaptability and making implementation easier by removing burdensome documentation tasks. These involve to an extent easing the implementation process by utilizing procedures that already represent a best fit with a particular school context, that minimize or reject extra workload for existing staff, that maximize cost-effectiveness, that are relatively straightforward and realistic, that do not require added infrastructure, and that leverage extant or easily repurposed infrastructure. These strategies also focus on methods that best meet local needs, ease fidelity assessment, and remove procedures (e.g., data forms, rubrics, reports) that have little added or less significant value to making informed decisions (Lyon et al., 2019). In essence, these implementation strategies focus on existing systems that can be capitalized for maximum value within contexts with limited resources such as rural school districts. Three primary linchpin strategies undergird the sample MTSS model proposed here: partnerships, school attendance, and school-based teams. These strategies are discussed next.
5.1.1 Partnerships
A crucial SISTER implementation pillar is building partnerships to support implementation, or developing benevolent relationships with entities internal and external to a school setting (Lyon et al., 2019). Key internal partners include central administrators and district-wide personnel who can help coordinate implemented components across schools, provide developmental support for the components, draw chronic and severe cases into a central catchment mechanism (see later Tier 3 section), and interface with influential community partners about the implementation. Key external partners include state departments of education and higher education institutions (below), both of which are considered indispensable for new implementation in rural schools (Gagnon and Mattingly, 2015). State education agency partnerships are particularly vital for coaching, financial and technical assistance, policy alignment, professional development opportunities, stakeholder engagement, and workforce capacity (Greenwald et al., 2018). Other potential external partners include local businesses, preschools, and those mentioned throughout this article (e.g., faith settings, primary care centers).
A more specific SISTER strategy, developing academic partnerships, refers to accessing training and research skills for an implementation project (Lyon et al., 2019). Academic partnerships are instrumental for even more specific SISTER strategies involving modeling or simulating the change that is sought prior to formal implementation, developing resource sharing agreements to supply expertise, and conducting educational outreach visits and conducting educational meetings with specific stakeholders to educate school personnel and others about the new practices (Lyon et al., 2019). For the purposes of the sample MTSS model vis-à-vis these strategies, academic partnerships would be especially useful for conducting root cause analyses and developing decision-making algorithms for moving cases across tiers, constructing information dashboards, providing consultation for Tier 2 treatments, instituting culturally responsive practices, and establishing telemental health practices (e.g., Hoover et al., 2020; see later preparedness and tiers sections for greater detail). Other crucial aspects include developing a community asset map to coordinate adjunct, local systems of care (e.g., medical, legal, developmental) as well as shared alliances across key entities (e.g., a particular school and housing/public assistance agencies) to better track students separated from the educational process and address multilayered problems in more timely fashion (e.g., Fenelon et al., 2021). Academic partnerships are also important for supplying graduate, practicum, and internship students for professional development, consultation, therapy, and data collection and dissemination purposes (Capps et al., 2019).
5.1.2 School attendance
School attendance is a metric commonly used by districts to satisfy state and federal education accountability reporting mandates and to receive funding (Bauer et al., 2018). School attendance is a multifaceted construct but most educational agencies focus on simple presence or absence from a regular classroom or virtual learning/hybrid setting. School attendance data may be recorded manually by staff and/or electronically via software programs and mobile apps. School attendance data have several advantages, including availability, equitability, comparability and communicability across jurisdictions, and utility in detecting problems, though caveats apply with respect to quality (Kearney and Childs, 2023a; Moodley et al., 2020). Still, school attendance data are a feasible and valuable benchmark for schools with limited assessment resources. Other basic metrics also readily available to districts include course grades and office disciplinary referrals (ODRs); indeed, attendance, grades, and ODRs are often used in statistical models to predict later school dropout (Balfanz and Byrnes, 2019).
School attendance data are an important marker or early warning signal for instability and transition to unhealthy states across academic, social–emotional, family, school, and community domains of functioning (see Kearney et al., 2023 for review). School attendance and its problems are also closely associated with student mental health functioning. School attendance relates to improved wellbeing by connecting students to social and academic competence supports as well as to more specific mental health and other supports at school (Weare, 2017). School attendance problems, however, are closely associated with emotional, disruptive behavior, substance use, developmental, and traumatic disorders (Lawrence et al., 2019). Examples of key mechanisms that link these constructs include school-based stimuli (including victimization) that provoke emotional distress; psychological symptoms and risky behaviors that interfere with social and academic competence; and sleep problems and lower self-efficacy, self-esteem, and perceived self-competence that affect concentration, motivation, coping abilities, participation in school activities, expectations of negative evaluations, and disengagement (e.g., Askeland et al., 2020). As such, school attendance problems can be a cost-effective, simple, and readily available means to help initially screen for mental health functioning.
5.1.3 School-based teams
School-based teams are frequently utilized to implement and sustain new programs because their key focal areas include problem identification, progress-monitoring data, intervention recommendations, and teacher support (Brendle, 2015). More specifically, school-based teams are often already in place (or easily amenable to development) to generate accommodation and academic plans, counsel students about career paths, and conduct assessment and intervention practices, among many other tasks (Markle et al., 2014). In addition, school-based team members are prime candidates for identifying local champions to advocate for a particular implemented program (next section). School-based team members in rural settings typically collect from available in-house support personnel (e.g., school-based social worker, psychologist, nurse, counselor, speech and language pathologist, attendance officer), administrators (e.g., principal, vice principal, dean), school board members, general and special education teachers, and/or other staff employees (Nichols et al., 2017).
In rural districts, as mentioned, school-based teams tend to be small in size and its members often adopt multiple roles (Fitzgerald et al., 2014). Team members often must serve as generalists as opposed to specialists, cover various domains of student functioning simultaneously, be adept at addressing elevated rates of adverse child experiences and trauma, and be competent in cultural and poverty issues (Michael et al., 2023). Teams need to be more collaborative in nature, with an emphasis on shared data and expertise and fundamental progress-monitoring assessments. School-based team meetings and interventions in these settings typically must be highly efficient, often with a focus more on skill development rather than on targeted treatments. As such, only the most necessary and convenient MTSS components and data collection sources may be implementable, and perhaps only in specific locations or via online mechanisms (McDaniel et al., 2021; Pierce and Mueller, 2018). In related fashion, successful tiered approaches in rural settings are often better viewed by teams as a general education initiative or schoolwide vision for improvement rather than as a special implementation (Shepherd and Salembier, 2011). More specific duties of school-based teams for the sample MTSS model are described in greater detail in the later Tier 1, Tier 2, and Tier 3 sections.
5.2 Readiness strategies
Readiness strategies refer here to assessments of needs, structure, and feasibility to determine if a new program such as a MTSS framework, in this case for a rural school district, is indeed essential, supportable, and realistically workable. Aspects of the readiness process include preparedness, installation, and implementation plan, each of which relate to various SISTER strategies. These aspects are discussed next.
5.2.1 Preparedness
The first readiness aspect refers to preparedness, or an exploration of measurable needs, evidence that a new program produces highly valued outcomes related to the needs, practicality of the new program, and the program’s whole-school value (Sugai and Horner, 2020). Key SISTER strategies in this regard include conducting a local needs assessment to determine whether new practices are imperative and assessing for readiness and identifying barriers and facilitators. The advent of large data sets within educational settings and the development of machine learning and other sophisticated data analytic strategies mean that school districts can pinpoint causes and patterns of constructs such as school absenteeism in a particular community, school, student group, or classroom (Kearney and Childs, 2023b).
Partnerships with universities and researchers with expertise in algorithm- and model-based analyses are especially helpful with respect to measurable needs. A particularly valuable process involves root cause analysis of local conditions that act as barriers and facilitators of a new program. Root cause analysis with respect to school attendance, for example, can illuminate policy and practice changes that may be needed, such as improved transportation, reduced use of exclusionary discipline, school-based meals and mentoring, and increased use of emotional competency enhancement and trauma-informed classrooms (e.g., Shamblin et al., 2016). Such partnerships must also emphasize data literacy training, however, to ensure that school staff can more easily understand and utilize such information. Key components of data literacy training, and especially for learning analytic methods, include understanding data structure and sources, visualizing data, drawing insights and making decisions based on data, and engaging in real-world applications, among others (Mandinach and Abrams, 2022).
Evidence that a new program produces highly valued outcomes related to the needs can come in the form of examining functional impairment as a result of school absences. Functional impairment refers to how certain actions interfere with a child’s ability to operate adequately across multiple domains such as social and academic performance (Rapee et al., 2012). School absences carry different impacts for different students depending on available support systems, meaning that not all absences are necessarily problematic. Rural schools can leverage school attendance data monitoring to focus specifically on those absences that carry greater negative impact. This includes absences that occur early in an academic year, during critical evaluation periods, and/or in higher-impact grades (e.g., first semester of middle school); that interfere with academic competence (e.g., grades, homework completion); that trigger an administrative or disciplinary action that produces further absences; and that interfere with social competence and interpersonal relationships (e.g., loss of friendships) (Kearney, 2022). Over time and with academic data support, a rural school-based team can become adept at isolating instances of school absences that create functional impairment, that may be more predictive of mental health problems and thus additional screening, and that promote highly valued outcomes by more proactively and efficiently linking students to necessary support systems.
The practicality of a new program refers in part to the ease with which the established system can be administered. Readiness in this case means that any new system must leverage an extant practice toward greater utility. The creation of an information dashboard, for example, can involve entry of local and easily interpreted variables such as attendance, grades, and screening data in real time to serve as an early warning system and enhance efficient data-based decision making by a school-based team (Childs and Grooms, 2018). Such a dashboard should be pragmatic and constructive vis-à-vis effortless or autoscored data entry, production of straightforward reports, and amenability to disaggregation to isolate students and student groups in greatest need of resources (Leverson et al., 2016). Such a dashboard could also be linked with interagency data systems within government services agencies and state departments of education (shared alliances) to better track students and coordinate available services (Chang and Balfanz, 2016). Dashboards can also be utilized by researchers via sophisticated learning analytic techniques to develop practical risk classification algorithms (such as for root cause analyses) to support school-based teams (Sahin and Ifenthaler, 2021). A key example of this approach involves data-based individualization, or an iterative process of collecting and analyzing progress monitoring information to identify when a particular student should move from Tier 1 to Tier 2/3 or from Tier 2 to Tier 3 supports (Sussman et al., 2022).
Finally, whole-school value can refer to collective understanding and buy-in from multiple parties with respect to the rationale for the proposed program. Indeed, enthusiasm among teachers and coaches for a particular program, particularly in rural areas, is considered critical for successful implementation (Shepherd and Salembier, 2011). Readiness in this case can involve whole staff participation in at least one key element of the implementation plan. An example is training all school staff to monitor and report to a school-based team key early warning signs of attendance and social and academic problems, and thus possibly internalizing and other mental health problems. Such signs can include student difficulties attending specialized classes, entering the school building, eating lunch with others, or transitioning from class to class. Other signs may include frequent visits to a non-classroom space, persistent distress in the classroom or upon separation from caregivers, sudden declines in grades or quality of completed work, and abrupt emotional or behavioral changes, among others (Kearney, 2016). Collective action also serves to boost sustainability of an implemented program (Herlitz et al., 2020).
5.2.2 Installation
The second readiness aspect refers to installation by district and school leadership teams that identify clear outcomes and develop policies and structures to support the implemented program (Sugai and Horner, 2020). Often this means identifying leadership, competency, and organizational drivers that promote system-level changes and pinpoint infrastructure elements that support strong fidelity, effectiveness, and sustainability (Bertram et al., 2015). Leadership drivers include trailblazers that understand the overall context of a given setting and its challenges and that involve other agencies to resolve the challenges (Fixsen et al., 2018). One set of SISTER strategies in this regard refers to identifying and preparing champions and providing practice-specific supervision (Lyon et al., 2019). Champions refer to those who support, market, and drive an implementation process, including overcoming resistance that a new program can provoke among stakeholders. In rural school settings in particular, principals often have outsized influence and have been shown to be essential in implementation efforts (Klar et al., 2020). Principals in particular are well-positioned to provide practice-specific supervision, or authoritative support for those delivering new services, by organizing assessment protocols, designing leadership roles, mentoring teachers and others, securing materials, spearheading professional development efforts, and arranging technical assistance from government, academic, and other agencies (Shepherd and Salembier, 2011).
Competency drivers include elements that promote confidence among those providing and receiving services and that enhance sustainability (Fixsen et al., 2018). A key component of this process is staff selection, particularly with respect to staff with knowledge and aptitude regarding a target population (Bertram et al., 2015). In a rural setting, such selection is imperative and must emphasize utilizing school-based team members most familiar with the surrounding community, culture, and language to engender greater trust and understanding (Schultz et al., 2021). Researchers have also noted the importance of school-based teams that understand and address the culture of poverty affecting many students in rural schools, particularly less access to health resources and greater food insecurity (Michael et al., 2023). In addition, valuable school-based team members would be those active in local operations that most draw rural populations together, including faith settings, community and sporting events, primary care settings, business and social cooperatives, agricultural and county gatherings, and other insider mechanisms (Preston and Barnes, 2017).
Organization drivers refers to elements that reshape system culture and enhance a hospitable environment for intended services (Fixsen et al., 2018). This relates to the SISTER strategy of creating a professional learning collaborative or forming groups within or between schools to foster a joint learning environment to enhance implementation of new practices (Lyon et al., 2019). Key aspects in this regard include (a) adopting a proactive approach, (b) reviewing existing policies and procedures, (c) reducing caseload size, (d) making decisions to target limited resources to areas of greatest need, and (e) aligning federal, state, organization, and community systems (Bertram et al., 2015). The MTSS blueprint provided here relies on school-based teams to (a) eschew a “wait to fail” approach in favor of a more proactive screening and early intervention approach; (b) minimize exclusionary discipline and zero tolerance policies that deter future school attendance and linkage to school-based mental health supports; (c) reduce caseload size by developing a central catchment mechanism for chronic and severe cases (later Tier 3 section); (d) target resources by identifying student groups in most need of services; and (e) align various care systems via the community asset mapping and shared alliance process described earlier (Scott T. M. et al., 2019).
5.2.3 Implementation plan
The third readiness aspect refers to the development and initiation of the implementation plan, complete with identifying its primary components and developing assessments in support of the plan (Sugai and Horner, 2020). A key SISTER strategy in this regard, developing a detailed implementation plan or blueprint, refers to delineating the primary aim of the implementation, scope of the change, goals or outcomes to be achieved, timeframe and milestones, appropriate performance/progress measures, and specific strategies to attain the goals or outcomes (Lyon et al., 2019). The blueprint is designed to propose what is most feasible to enhance student outcomes along these facets.
The primary aim of the implementation plan proposed here is to establish an organized, school team-based process to proactively monitor and respond to school absences, screen for mental health and related difficulties, and link students to appropriate mental health support options. The scope of change of the implementation plan proposed here (who and what settings) focuses on students and their families and initially on a pilot process designed for later elementary school grades (e.g., 4–5) and the first semester of middle school (e.g., grade 6). A focus on only two schools initially is done to maximize limited resources toward educational time periods that involve substantial social and academic development, students with enhanced cognitive development, and the transition to middle school, which is a high-risk period for school maladjustment (Ryan et al., 2013). Lessons from the pilot process can then inform modifications and possible expansion to other grades and schools. Note that an alternative high-impact pilot would involve a pre-kindergarten-kindergarten-first grade focus.
The goals or outcomes of the implementation plan proposed here are to improve student mental health functioning/wellbeing via enhanced school attendance and mental health services utilization. The timeframe of the implementation plan proposed here involves the beginning to the end of the academic year (e.g., September to May), whereas milestones involve biweekly attendance data review, main grading periods, and end of semester points. Each of these represent typical extant meeting times for school-based teams. The appropriate performance/progress measures of the implementation plan proposed here include school attendance, functional impairment data (grades, ODRs, screening), and type and frequency of mental health services utilization (e.g., Tier 2 school-based intervention, telehealth, outpatient, inpatient, emergency department). The specific strategies to attain the goals or outcomes of the implementation plan proposed here are described in the following tier-based sections.
6 Tier 1
Recall that Tier 1 strategies include universal or school-wide practices to promote adaptive behavior and deter maladaptive behavior. The primary purpose of the proposed school-based team at Tier 1 is to engage consumers, review school attendance and impairment data, manage emerging cases, and implement preventative tactics. With respect to engaging consumers, key SISTER strategies include intervening and communicating with students, families, and other staff to enhance uptake and fidelity and involving students, family members, and other staff (Lyon et al., 2019). These strategies focus on attracting stakeholders who may not be directly involved in a new implemented program but who can help problem solve toward greater adoption and fidelity. In a rural setting, efforts to draw caregivers and extended family members into the MTSS approach must be prioritized at Tier 1. Such engagement would facilitate consultations to resolve school attendance problems and link students to appropriate mental health service options. Engagement examples include linking informal school events (e.g., performances, fairs, parties) that often attract family members to consultation opportunities, events scheduled at flexible and staggered times, caregiver recruitment efforts to assist school-based tasks, campus-based (and community satellite if feasible) resource rooms devoted specifically to caregiver assistance (including non-academic resources), transportation assistance, and use of social media and other communication platforms (Hamlin and Flessa, 2018). Family members can also be recruited to report early warning signs as noted earlier.
With respect to reviewing school attendance/impairment data and managing emerging cases, key SISTER strategies include developing and distributing educational materials that support the implemented program (Lyon et al., 2019). In the sample MTSS model proposed here, such materials would include in-print and online handbooks for caregivers with contact information and availability for school staff (especially team members), school policies regarding attendance, transportation options, and progress reports. In addition, information would be provided on the implemented program and a community asset map of resources (Werch and Runyons-Hiers, 2020). In related fashion, the school-based team would actively monitor school attendance data as an early warning signal. This should occur at least once every 2 weeks, and ideally weekly, to identify students who have missed at least 25% of school time (Kearney, 2016). Such identification would then be linked to further screening with respect to functional impairment (interference with social and/or academic competence; e.g., Brann et al., 2021), other readily available school-based metrics (e.g., ODRs), and no-cost but culturally responsive and equitable mental health symptom screening and targeted measures (e.g., National Center for School Mental Health; School Health and Performance Evaluation; Gonzálvez et al., 2021).
A Tier 1 school-based team would then efficiently determine, via the academic partnership algorithms described earlier, if school absences and any related impairment are temporary and nonproblematic or emerging and thus in need of early intervention. A key SISTER strategy in this regard, facilitation/problem-solving, involves interactive efforts to support students and their families with respect to the implemented program within the context of a non-evaluative interpersonal relationship (Lyon et al., 2019). In a rural setting in particular, this requires an emphasis on additional qualitative data and ecological decision-making to identify interventions best tailored to home and community circumstances (Hoover and Soltero-González, 2018). Examples include adjustments for students with hybrid or home-based learning formats, families with nontraditional work schedules, and very remote areas with particularly sparse community resources (Garbacz et al., 2022).
With respect to preventative tactics, key SISTER strategies include conducting ongoing training and facilitating relay of intervention fidelity and student data to school personnel (Lyon et al., 2019). These refer to engaging in the implemented practices in an ongoing fashion and providing real-time data about student outcomes using various channels of communication. In the Tier 1 phase proposed here, this can involve extensive use of teachers to engage in specific curriculum-based interventions, provide a welcoming and destigmatizing culture, and monitor school attendance in real time to support the school-based team. Essential aspects of a curriculum-based intervention shown to promote mental health and academic success could be emphasized, such as a cost-effective focus on classroom-based social and emotional learning or psychoeducation (Gueldner et al., 2020). Teachers can also focus on regular praise and encouragement to students who are in class and emphasize that their attendance is valued. In addition, the use of first period or homeroom teachers, or a primary teacher in elementary school, could involve immediate reporting of a school absence to the team, which could spur efforts to minimize the absences and their effects via texts, apps, or other contact methods with caregivers (Cook et al., 2017). Teacher, peer, and community mentoring and advocacy programs are also helpful in this regard as low-cost options (Hart et al., 2021).
7 Tier 2
Recall that Tier 2 interventions refer to early, selective intervention or secondary prevention practices to address acute problems. The role of the school-based team at Tier 2 is to address acute cases of school attendance and mental health problems identified via Tier 1 decision-making procedures. Key SISTER strategies in this regard include making training dynamic and providing ongoing consultation/coaching (Lyon et al., 2019). These refer broadly to varying delivery methods in an implemented program according to different student and professional development needs, with an emphasis on interactive and experiential practices. Although this refers in part to the initial training and development process, these strategies are also important for direct service delivery. In this context, the interventions to be implemented must focus on what is most feasible, valuable, and cost-effective while at the same time empirically supported. As such, the focus in this section is on methods to provide interventions in formats that reach a wider audience as well as the use of school-based treatments to provide maximum coverage. In addition, the providers of such interventions in rural schools may need to more intensely involve teachers given limited personnel and could involve training in the practices described next to promote task-sharing and help bridge staffing gaps (Hoeft et al., 2018).
Intervention formats to maximize exposure and reach a wider audience can include in-person as well as novel modes of service delivery. In-person formats, particularly in rural settings, generally involve small groups (i.e., 2–6 members) that meet 1–4 times per week for 20–25 min per session (Guy et al., 2016). Settings could involve the school building as well as association with local primary care centers and other proximal task-sharing sites (Hoeft et al., 2018). Novel modes of service delivery include computer-assisted programs, digital device applications, games, portals, text messaging, videoconferencing, virtual reality, and wearable devices, among others (Hollis et al., 2017). Such modes can also be leveraged to inform caregivers in real time regarding school absences and mental health and other functioning concerns, to upload academic work and other resources to minimize impairment, and to provide mentoring and other support (Smythe-Leistico and Page, 2018). Novel modes of service delivery can also be used to support direct interventions, such as via peer-to-peer communications, reminders, skills development, and social networking (Liverpool et al., 2020). Access to such technology cannot necessarily be assumed in low-resource rural schools, however, necessitating technology readiness analyses, creative onboarding of new hardware, workarounds for bandwidth deficits, and reliance on more available devices such as smartphones (Wargo et al., 2021).
Tier 2 school-based treatments in rural settings must maximize feasibility, value, and coverage while addressing the most pressing mental health issues in these areas: emotional and substance use disorders, including aspects of trauma, suicidal ideation, anxiety, and depression (Schultz et al., 2021). Examples of two primary approaches to meet these requirements are described here. The first approach involves school-based transdiagnostic treatments that target multiple problems or disorders that share common features. Examples of common features include avoidance, cognitive biases, emotional dysregulation, exposure to traumatic life events, low self-esteem and self-efficacy, and social skill deficits (Fusar-Poli et al., 2019). School-based transdiagnostic treatments thus focus on intervention techniques that address multiple common features. Examples of such techniques include acceptance, behavioral activation, cognitive reappraisal, mindfulness, psychoeducation, relaxation, and various aspects of coping, interpersonal, problem-solving, self-supporting, and social skills training (Berryhill et al., 2022). Mechanisms for delivery can include readings, individual or group exercises and discussion, social performances, support, videotaped role-playing and feedback, and homework (Fernández-Martínez et al., 2020). Although some school-based transdiagnostic treatment protocols contain a parent component, most focus on students, which is of particular benefit in rural settings where extensive caregiver contact can be challenging. School-based transdiagnostic treatments have been found effective for symptom and impairment reduction (e.g., Martinsen et al., 2019). Fewer such treatments have focused on substance use per se, though many of the transdiagnostic features relevant to emotional problems, such as regulation and social skill deficits, also apply (Shadur and Lejuez, 2015).
The second approach involves school-based trauma-informed practices that are geared toward students with adverse child experiences that often precipitate impairment in multiple domains (Thomas et al., 2019). The overarching goal of these practices is to support impacted students via trauma-sensitive classroom and school-wide strategies as well as via the transdiagnostic techniques mentioned above. At a broader level, such practices often involve educating school staff about childhood trauma and its effects and signs; providing rationales and transparency with respect to expected student behavior; developing collaborative and trust-based student-teacher interactions via active listening, empathy, multiple forms of communication, and positive affirmations; utilizing supportive feedback within predictable and consistent classroom routines; and enhancing a sense of safety. Other trauma-informed practices can be targeted toward specific students, including extended compliance times, calming strategies, and competency development (Minahan, 2019). School-based trauma-informed practices are effective in individual and group formats but classroom-based and school-wide applications tend to enhance integration, access to services, and sustainability (Herrenkohl et al., 2019).
Tier 2 interventions can also be maximized for efficiency via a multidimensional MTSS approach that addresses multiple domain clusters simultaneously and thus in more nuanced fashion (Kearney and Graczyk, 2020). This involves tailoring a MTSS approach to better fit students and schools of various developmental levels, performance challenges, or ecological domains, among other clusters. For example, the Tier 2 interventions described above could be tailored more specifically for students at elementary and middle school levels and for students with different combinations of challenges as well as substantial family (e.g., divorce) and other inner and outer contextual variables impacting their mental health. In addition, a multidimensional approach would potentially include variation with respect to formats for information and treatment provision, inclusion of other broad intervention frameworks (e.g., anti-bullying), and parent-focused interventions (Weingarten et al., 2020).
8 Tier 3
Recall that Tier 3 interventions refer to intensive practices to address chronic and severe problems. As mentioned earlier, the proposed school-based team at Tier 3 would be a central catchment mechanism for student problems that require extensive case management efforts due to frequent absenteeism, academic disengagement, intense symptomatology, comorbid conditions, and multiple contributing contextual factors. This could involve a district-wide panel, task force, or review board process that coordinates efforts for these cases, thus reducing caseload for the Tier 1/2 school-based teams described earlier (Battal et al., 2020). Members could include district officials or central administrators and representatives from law enforcement/probation and community health and mental health, social service, and youth agencies, among others (Oyen and Wollersheim-Shervey, 2019). This centralized mechanism would be responsible for reviewing complex cases, gathering the extensive historical and clinical knowledge and special circumstances relevant to a particular case, examining school and district policies applicable to the case, and developing a multifaceted intervention plan (Kearney, 2016). Policy review would also include reconfiguration or removal of practices that are biased toward certain student groups and that paradoxically aggravate school attendance and mental health problems (Conry and Richards, 2018; Wilson and Cariola, 2020).
Intervention plans at Tier 3 would likely involve a combination of academic support, wraparound care, and more formal mental health services. Academic support could include accommodation plans (e.g., IEP, 504) to leverage available alternative educational settings or pathways, part-time attendance schedules, modifications in class schedule and academic work, mentoring or increased supervision at school, tutoring and homework assistance, assessment of previously undiagnosed learning and other disorders, student visits to school-based team members, and daily feedback to caregivers (Chaparro et al., 2022). Family and mental health support as described below can also be key aspects of these plans. Wraparound care in rural settings often involves linking families with available community supports as established by the asset map and shared alliances described earlier. A full description is beyond the scope of this article but common supports surround crisis care and outreach, employment, foster care, housing, independent living, legal services, nutrition, physical health, recreation, residential and respite care, self-help, and transportation (Olson et al., 2021). Another internal mechanism for Tier 3 support in rural schools includes fostering partnerships with community organizations, nonprofit agencies, and local businesses to provide mentorship opportunities (Kraft and Falken, 2021).
With respect to mental health support, a key mechanism at Tier 3 can be university-supported telehealth practices, often via videoconferencing but also potentially via the novel strategies mentioned earlier, that link students directly to psychiatric and psychological therapies (telemental or telebehavioral health; Michael et al., 2025; Patel et al., 2020; Sylvan et al., 2025). University-supported telehealth practices and telehealth consultation models for rural schools remain in development but could be integrated into the central catchment mechanism mentioned above to relieve caseload surrounding chronic and severe mental health problems (Calleja et al., 2022). Telemental health practices in rural settings commonly involve individual or group therapy, medication management, symptom monitoring, and substance use counseling, though screening procedures can be included as well (Emmett et al., 2022). Acceptance and satisfaction with telemental health practices is typically good, and video-based communication may be as effective as face-to-face formats, at least in the short term, though data continue to emerge (Barnett et al., 2021). The practices are less amenable to students with severe auditory, visual, or cognitive impairments or conditions such as psychotic symptoms, active suicidality, and addictions that may require specialized, crisis, or long-term treatment (Schlief et al., 2022). Other barriers to telemental health practices must also be addressed and include service reimbursement, technology, and facilitating acceptance among school staff and students and families (Fox et al., 2022). In addition, telemental health practices must be developmentally appropriate; for example, treatment for substance use in adolescents may include advanced cognitive-behavioral and motivational interviewing techniques but such treatment in elementary school children may need to focus more on psychoeducation about substances, coping skills development, and promoting healthy behaviors (Liu et al., 2023).
Two key SISTER strategies for these Tier 3 practices include changing or altering the environment and developing and organizing a quality monitoring system. Specific space will need to be identified or repurposed to accommodate telemental health practices and to maximize privacy, confidentiality, and security. In addition, such spaces must be well integrated into existing school processes (Fox et al., 2022). Facilities for virtual and related communications must also be established for Tier 3 school-based team members, community partners, and caregivers. Quality monitoring systems vis-à-vis telemental health practices can include measures of student engagement and safety, symptom change, technical complexity, provider and student experiences and satisfaction, adverse events, economic impact, treatment adherence, equitable access, and student outcomes (Demaerschalk et al., 2023).
9 Sustainability and expansion
To be clear, sustainability and expansion of MTSS approaches must rely on steady funding sources that often include federal and state grants, possible Medicaid reimbursement, community entities, private foundations, and other streams (Gozali-Lee et al., 2021). Mechanisms to enhance rural schools’ ability to access such funding are imperative. In addition, the development of pipelines to augment the number of qualified school mental health providers remains necessary. Mechanisms to strengthen these pipelines can include loan forgiveness and other incentives, internships with high school and college and other students, and reducing costs to school districts (Michael et al., 2023).
Several SISTER strategies are also important in the MTSS model proposed here to enhance sustainability and expansion. With respect to sustainability, these include auditing and providing feedback, developing instruments to monitor and evaluate core components of the innovation/new practice, obtaining and using student and family feedback, and monitoring the progress of the implementation effort (Lyon et al., 2019). These strategies collectively and broadly refer to methods to regularly monitor implementation components to determine their acceptability and thus sustainability. Sustainability constructs within implementation science relate to inner and outer contexts and include continued delivery, behavior change, adaptation, and continued benefits (Hall et al., 2022). Specific sustainability constructs for MTSS models remain in development but typically surround assessment of implementation fidelity, formative assessment of student performance, program annual evaluation, teacher buy-in and adjustment of traditional roles, involvement of all school personnel, adequate meeting time for coordination, strong administrative support at building and district levels, and ongoing professional development (Bahr et al., 2023). Measures in this regard can include checklists, observations, and interviews but must minimize burden in rural settings (Hoover et al., 2020; Santiago et al., 2025).
Assessment of implementation fidelity for the MTSS model proposed here could involve real-world measures such as adherence to regular school attendance/impairment data review, frequency of Tier 1 screening and problem-solving activities, latency of responding to absences and linking students to necessary supports, and student participation in Tier 2/3 mental health supports, among other constructs (Gage et al., 2022). Formative assessment of student performance could involve ongoing evaluations of academic, behavioral, social, and mental health functioning for youths receiving Tier 2 and 3 services. Program annual evaluation could involve a district-wide report of rates of school absenteeism and student functioning for pilot and non-pilot schools, as well as surveys of students and families regarding acceptability and reach of the interventions (Sanetti and Collier-Meek, 2019).
Teacher buy-in and adjustment of traditional roles could involve participation in the school-based team, student absenteeism reporting, curriculum delivery, and mentoring roles. Involvement of all school personnel could be evaluated by participation in reporting early warning signs to the school-based team. Adequate meeting time for coordination can be examined via documented schedules. Strong administrative support for the implemented program could be measured via resources, community intersection efforts, policy review and revision, and development of a Tier 3 team. Finally, ongoing professional development could involve online and university-based trainings to boost sustainability via problem-solving. A primary goal of these processes would be to derive organic, nuts-and-bolts data in real time about what works and what may be burdensome, extraneous, and subject to simplification or removal (Forman et al., 2017).
With respect to expansion, successful elements of the implemented program may be eventually pursued to other grade levels and schools in a rural district. The key SISTER strategies in this regard, capturing and sharing local knowledge, identifying early adopters, visiting other sites, and using train-the-trainer strategies, refer broadly and collectively to methods to disseminate information on effective aspects of the new program that could be implemented in different settings (e.g., student group, grade, school). Potential expansion would require a detailed assessment of available resources and particularly those at provider and organizational levels (Williams and Beidas, 2019). Examples include provider competence and perceptions/motivation surrounding the implemented program as well as strong leadership and available school-based teams in the new settings. Readers should note, however, that longitudinal studies examining the expansion of MTSS approaches in rural schools remain needed (Johnson et al., 2021).
Initial expansion would involve distribution strategies (e.g., interpersonal connections, websites) to promote the spread of effective implementations and new innovations. Subsequent stages of expansion include integration strategies, such as gradual forays into a new grade; capacity-building strategies, such as having a member of the original school-based team provide coaching; and scale-up strategies, such as infrastructure development and policy advocacy (Leeman et al., 2017). Such dissemination could be more active, utilizing continued engagement of academic partnerships, or more passive by diffusing naturally throughout a system (Rapport et al., 2018). In a rural setting, a strong connection of implementation agents with the local environment is especially important for expansion efforts, meaning that any generalizability must not necessarily assume whole system implementation but rather tenability at more specific levels (Braithwaite et al., 2018). Expansion could, for example, focus more on preschool and early grade efforts to address school attendance and academic and social–emotional skills that often set the stage for improved mental health functioning in later grades (e.g., Huber et al., 2019).
10 Conclusion
Rural schools and communities present significant challenges with respect to service delivery for mental health problems in children and adolescents, yet at the same time contain unique advantages that may be especially amenable to an implemented MTSS approach. More broadly, rural schools are fertile ground for examining overarching, futuristic trends in youth mental health care, including “where they are” interventions, innovative service delivery methods, cultural responsiveness, policy review, barrier removal, shared alliances, and ecological systemic (whole child) approaches, all within the context of an implementation science framework. These areas of focus can also help advance other key research areas such as how a newly implemented program affects long-term student performance metrics, the overall climate of a given school or district, and degree of community engagement. Such areas of focus also have ramifications for training new mental health professionals, particularly with respect to competencies in sophisticated data analysis, consultation, ethics, networking, interdisciplinary and multicultural practices, creative interventions, technology, telehealth provision, and program evaluation, among others. Indeed, rural schools are excellent laboratories for clarifying implementation guidelines and for developing practical, real-world solutions. The blueprint provided in this article is designed not as the final word but rather one set of ideas to promote discussion and innovation in this regard and help address an often overlooked and underserved set of youth.
Author contributions
CK: Conceptualization, Supervision, Visualization, Writing – original draft, Writing – review & editing. MF: Writing – original draft, Writing – review & editing. RD: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Article costs were supported by a UNLV-UNR Cooperative Extension grant.
Acknowledgments
The authors express gratitude to the University of Nevada, Las Vegas.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ali, M. M., West, K., Teich, J. L., Lynch, S., Mutter, R., and Dubenitz, J. (2019). Utilization of mental health services in educational setting by adolescents in the United States. J. Sch. Health 89, 393–401. doi: 10.1111/josh.12753
Arora, P. G., Collins, T. A., Dart, E. H., Hernández, S., Fetterman, H., and Doll, B. (2019). Multi-tiered systems of support for school-based mental health: a systematic review of depression interventions. Sch. Ment. Heal. 11, 240–264. doi: 10.1007/s12310-019-09314-4
Askeland, K. G., Bøe, T., Lundervold, A. J., Stormark, K. M., and Hysing, M. (2020). The association between symptoms of depression and school absence in a population-based study of late adolescents. Front. Psychol. 11:1268. doi: 10.3389/fpsyg.2020.01268
Bahr, M. W., Edwin, M., and Long, K. A. (2023). Development of a brief measure for multi-tiered systems of support sustainability. Assess. Eff. Interv. 48, 90–99. doi: 10.1177/15345084221119418
Bailey, T. R. (2014). An initial exploratory analysis of RTI implementation in rural schools. Researcher 26, 34–39.
Balfanz, R., and Byrnes, V. (2019). “Early warning indicators and early intervention systems: state of the field” in Handbook of student engagement interventions: Working with disengaged students. eds. J. A. Fredricks, A. L. Reschly, and S. L. Christenson (New York, NY: Elsevier), 45–56.
Barican, J. L., Yung, D., Schwartz, C., Zheng, Y., Georgiades, K., and Waddell, C. (2022). Prevalence of childhood mental disorders in high-income countries: a systematic review and meta-analysis to inform policymaking. BMJ Mental Health 25, 36–44. doi: 10.1136/ebmental-2021-300277
Barnett, P., Goulding, L., Casetta, C., Jordan, H., Sheridan-Rains, L., Steare, T., et al. (2021). Implementation of telemental health services before COVID-19: rapid umbrella review of systematic reviews. J. Med. Internet Res. 23:e26492. doi: 10.2196/26492
Battal, J., Pearrow, M. M., and Kaye, A. J. (2020). Implementing a comprehensive behavioral health model for social, emotional, and behavioral development in an urban district: an applied study. Psychol. Sch. 57, 1475–1491. doi: 10.1002/pits.22420
Bauer, L., Liu, P., Schanzenbach, D. W., and Shambaugh, J. (2018). Reducing chronic absenteeism under the every student succeeds act. Washington, DC: Brookings.
Bauer, M. S., Damschroder, L., Hagedorn, H., Smith, J., and Kilbourne, A. M. (2015). An introduction to implementation science for the non-specialist. BMC Psychology 3, 32–12. doi: 10.1186/s40359-015-0089-9
Bauer, M. S., and Kirchner, J. (2020). Implementation science: what is it and why should I care? Psychiatry Res. 283:112376. doi: 10.1016/j.psychres.2019.04.025
Beason, T., Knox, J., Lever, N., Hoover, S., Dubin, M., and Gorden-Achebe, K. (2024). Using a culturally responsive, antiracist, and equitable approach to school mental health. Child Adolescent Psychiatr. Clinics. 33, 541–556. doi: 10.1016/j.chc.2024.04.001
Benner, G. J., Kutash, K., Nelson, J. R., and Fisher, M. B. (2013). Closing the achievement gap of youth with emotional and behavioral disorders through multi-tiered systems of support. Educ. Treat. Child. 36, 15–29.
Berryhill, B., Carlson, C., Hopson, L., Culmer, N., and Williams, N. (2022). Adolescent depression and anxiety treatment in rural schools: a systematic review. J. Rural Ment. Health 46, 13–27. doi: 10.1037/rmh0000183
Bertram, R. M., Blase, K. A., and Fixsen, D. L. (2015). Improving programs and outcomes: Implementation frameworks and organization change. Res. Soc. Work Pract. 25, 477–487. doi: 10.1177/1049731514537687
Bohnenkamp, J. H., Hartley, S. N., Splett, J. W., Halliday, C., Collins, D., Hoover, S., et al. (2023). Promoting school safety through multi-tiered systems of support for student mental health. Prev. Sch. Fail. Altern. Educ. Child. Youth 67, 9–17. doi: 10.1080/1045988X.2022.2124221
Bradshaw, C. P., Cohen, J., Espelage, D. L., and Nation, M. (2021). Addressing school safety through comprehensive school climate approaches. Sch. Psychol. Rev. 50, 221–236. doi: 10.1080/2372966X.2021.1926321
Bradshaw, C. P., Pas, E. T., Debnam, K. J., and Lindstrom Johnson, S. (2015). A focus on implementation of positive behavioral interventions and supports (PBIS) in high schools: associations with bullying and other indicators of school disorder. Sch. Psychol. Rev. 44, 480–498. doi: 10.17105/spr-15-0105.1
Braithwaite, J., Churruca, K., Long, J. C., Ellis, L. A., and Herkes, J. (2018). When complexity science meets implementation science: a theoretical and empirical analysis of systems change. BMC Med. 16:63. doi: 10.1186/s12916-018-1057-z
Brann, K. L., Naser, S. C., Splett, J. W., and DiOrio, C. A. (2021). A mixed-method analysis of the implementation process of universal screening in a tiered mental health system. Psychol. Sch. 58, 2089–2113. doi: 10.1002/pits.22579
Brendle, J. (2015). A survey of response to intervention team members' effective practices in rural elementary schools. Rural Special Educ. Q. 34, 3–8. doi: 10.1177/875687051503400202
Burns, B. J., Costello, E. J., Angold, A., Tweed, D., Stangl, D., Farmer, E. M., et al. (1995). Children's mental health service use across service sectors. Health Aff. 14, 147–159. doi: 10.1377/hlthaff.14.3.147
Calleja, P., Wilkes, S., Spencer, M., and Woodbridge, S. (2022). Telehealth use in rural and remote health practitioner education: an integrative review. Rural Remote Health 22, 1–13. doi: 10.22605/RRH6467
Calvert, H. G., McQuilkin, M., Havlicak, A., Lewis, T., and Turner, L. (2023). Acceptability, appropriateness, and feasibility of rural school support strategies for behavioral interventions: a mixed methods evaluation over two years of a hybrid type 3 implementation-effectiveness trial. Implem. Sci. Commun. 4:92. doi: 10.1186/s43058-023-00478-4
Capps, R. E., Michael, K. D., Jameson, J. P., and Sulovski, K. (2019). “Providing school-based mental health services in rural and remote settings” in Handbook of rural, remote, and very remote mental health. eds. T. Carey and J. Gullifer (Singapore: Springer), 1–19.
Castro-Ramirez, F., Al-Suwaidi, M., Garcia, P., Rankin, O., Ricard, J. R., and Nock, M. K. (2021). Racism and poverty are barriers to the treatment of youth mental health concerns. J. Clin. Child Adolesc. Psychol. 50, 534–546. doi: 10.1080/15374416.2021.1941058
Chang, H., and Balfanz, R. (2016). Preventing missed opportunity: Taking collective action to confront chronic absence. San Francisco, CA: Everyone Graduates Center/Attendance Works.
Chaparro, E. A., Kittelman, A., McDaniel, S. C., Peshak George, H., VanLone, J., and So, S. (2022). Examining rural school implementation of positive behavioral supports across tiers. Rural Special Educ. Q. 41, 116–128. doi: 10.1177/87568705221097114
Cheesmond, N. E., Davies, K., and Inder, K. J. (2019). Exploring the role of rurality and rural identity in mental health help-seeking behavior: a systematic qualitative review. J. Rural Ment. Health 43, 45–59. doi: 10.1037/rmh0000109
Childs, J., and Grooms, A. A. (2018). Improving school attendance through collaboration: a catalyst for community involvement and change. J. Educ. Stud. Placed Risk 23, 122–138. doi: 10.1080/10824669.2018.1439751
Chung, E. K., Siegel, B. S., Garg, A., Conroy, K., Gross, R. S., Long, D. A., et al. (2016). Screening for social determinants of health among children and families living in poverty: a guide for clinicians. Curr. Probl. Pediatr. Adolesc. Health Care 46, 135–153. doi: 10.1016/j.cppeds.2016.02.004
Collins, T. A., Dart, E. H., and Arora, P. G. (2019). Addressing the internalizing behavior of students in schools: Applications of the MTSS model. Sch. Ment. Health. 11, 191–193. doi: 10.1007/s12310-018-09307-9
Conry, J. M., and Richards, M. P. (2018). The severity of state truancy policies and chronic absenteeism. J. Educ. Stud. Placed Risk 23, 187–203. doi: 10.1080/10824669.2018.1439752
Cook, C. R., Lyon, A. R., Locke, J., Waltz, T., and Powell, B. J. (2019). Adapting a compilation of implementation strategies to advance school-based implementation research and practice. Prev. Sci. 20, 914–935. doi: 10.1007/s11121-019-01017-1
Cook, P. J., Dodge, K. A., Gifford, E. J., and Schulting, A. B. (2017). A new program to prevent primary school absenteeism: results of a pilot study in five schools. Child Youth Serv. Rev. 82, 262–270. doi: 10.1016/j.childyouth.2017.09.017
Crable, E. L., Lengnick-Hall, R., Stadnick, N. A., Moullin, J. C., and Aarons, G. A. (2022). Where is “policy” in dissemination and implementation science? Recommendations to advance theories, models, and frameworks: EPIS as a case example. Implement. Sci. 17:80. doi: 10.1186/s13012-022-01256-x
Curran, G. M. (2020). Implementation science made too simple: a teaching tool. Implement. Sci. Commun. 1, 1–3. doi: 10.1186/s43058-020-00001-z
Damschroder, L. J., Reardon, C. M., Widerquist, M. A. O., and Lowery, J. (2022). The updated consolidated framework for implementation research based on user feedback. Implement. Sci. 17:75. doi: 10.1186/s13012-022-01245-0
Demaerschalk, B. M., Hollander, J. E., Krupinski, E., Scott, J., Albert, D., Bobokalonova, Z., et al. (2023). Quality frameworks for virtual care: expert panel recommendations. Mayo Clinic Proc. Innov. Quality Outcomes 7, 31–44. doi: 10.1016/j.mayocpiqo.2022.12.001
Douthit, N., Kiv, S., Dwolatzky, T., and Biswas, S. (2015). Exposing some important barriers to health care access in the rural USA. Public Health 129, 611–620. doi: 10.1016/j.puhe.2015.04.001
Duong, M. T., Bruns, E. J., Lee, K., Cox, S., Coifman, J., Mayworm, A., et al. (2021). Rates of mental health service utilization by children and adolescents in schools and other common service settings: a systematic review and meta-analysis. Adm. Policy Ment. Health Ment. Health Serv. Res. 48, 420–439. doi: 10.1007/s10488-020-01080-9
Durrance, S. (2023). Implementing MTSS in secondary schools: Challenges and strategies. Greensboro, NC: SERVE Center at UNC Greensboro.
Eagle, J. W., Dowd-Eagle, S. E., Snyder, A., and Holtzman, E. G. (2015). Implementing a multi-tiered system of support (MTSS): collaboration between school psychologists and administrators to promote systems-level change. J. Educ. Psychol. Consult. 25, 160–177. doi: 10.1080/10474412.2014.929960
Eccles, M. P., and Mittman, B. S. (2006). Welcome to implementation science. Implement. Sci. 1:1. doi: 10.1186/1748-5908-1-1
Echazarra, A., and Radinger, T. (2019). Learning in rural schools: Insights from PISA, TALIS, and the literature. Paris: Organisation for Economic Co-operation and Development.
Emmett, S. D., Platt, A., Turner, E. L., Gallo, J. J., Labrique, A. B., Inglis, S. M., et al. (2022). Mobile health school screening and telemedicine referral to improve access to specialty care in rural Alaska: a cluster-randomised controlled trial. Lancet Glob. Health 110, 1308–1314.
Fabiano, G. A., and Pyle, K. (2019). Best practices in school mental health for attention-deficit/ hyperactivity disorder: a framework for intervention. Sch. Ment. Heal. 11, 72–91. doi: 10.1007/s12310-018-9267-2
Fenelon, A., Boudreaux, M., Slopen, N., and Newman, S. J. (2021). The benefits of rental assistance for children's health and school attendance in the United States. Demography 58, 1171–1195. doi: 10.1215/00703370-9305166
Fernández-Martínez, I., Orgilés, M., Morales, A., Espada, J. P., and Essau, C. A. (2020). One-year follow-up effects of a cognitive behavior therapy-based transdiagnostic program for emotional problems in young children: a school-based cluster-randomized controlled trial. J. Affect. Disord. 262, 258–266. doi: 10.1016/j.jad.2019.11.002
Fitzgerald, C. B., Geraci, L. M., and Swanson, M. (2014). Scaling up in rural schools using positive behavioral interventions and supports. Rural Special Educ. Q. 33, 18–22. doi: 10.1177/875687051403300
Fixsen, D. L., Ward, C., Blase, K., Naoom, S., Metz, A., and Louison, L. (2018). Assessing drivers best practices. Chapel Hill, NC: Active Implementation Research Network.
Fletcher, J. M., and Vaughn, S. (2009). Response to intervention: preventing and remediating academic difficulties. Child Dev. Perspect. 3, 30–37. doi: 10.1111/j.1750-8606.2008.00072.x
Forman, S. G., Ward, C. S., and Fixsen, D. L. (2017). Comprehensive behavioral health and school psychology: an implementation agenda. J. Appl. Sch. Psychol. 33, 233–244. doi: 10.1080/15377903.2017.1317153
Fox, K., Burgess, A., Williamson, M. E., Massey, J., Shaler, G., Pearson, K., et al. (2022). Implementation of telehealth services in rural schools: a qualitative assessment. J. Sch. Health 92, 71–78. doi: 10.1111/josh.13104
Frankland, M. (2021). Meeting students where they are: trauma-informed approaches in rural schools. Rural Educ. 42, 51–71. doi: 10.35608/ruraled.v42i2.1243
Fusar-Poli, P., Solmi, M., Brondino, N., Davies, C., Chae, C., Politi, P., et al. (2019). Transdiagnostic psychiatry: a systematic review. World Psychiatry 18, 192–207. doi: 10.1002/wps.20631
Gage, N. A., Baker, C. N., Splett, J. W., and Halliday, C. A. (2025). Mental health literacy of multi-tiered systems of support team members. Am. J. Health Educ. 56, 36–45. doi: 10.1080/19325037.2024.2422077
Gage, N. A., Kern, L., Peshak George, H., Elfner, K., and Robbie, K. (2022). Exploring SWPBIS implementation outcomes in rural and urban schools in Florida. Rural Special Educ. Q. 41, 129–139. doi: 10.1177/87568705221094560
Gagnon, D. J., and Mattingly, M. J. (2015). State policy responses to ensuring excellent educators in rural schools. J. Res. Rural. Educ. 30, 1–14.
Garbacz, S. A., Santiago, R. T., and Gulbrandson, K. (2022). Examining implementation of positive behavioral interventions and supports in rural schools. Rural Spec. Educ. Q. 41, 95–107. doi: 10.1177/87568705221097117
Glasgow, R. E., Harden, S. M., Gaglio, B., Rabin, B., Smith, M. L., Porter, G. C., et al. (2019). RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-year review. Front. Public Health 7:64. doi: 10.3389/fpubh.2019.00064
Goldstein, H., McKenna, M., Barker, R. M., and Brown, T. H. (2019). Research–practice partnership: application to implementation of multitiered system of supports in early childhood education. Persp. ASHA Special Interest Groups 4, 38–50. doi: 10.1044/2018_PERS-ST-2018-0005
Goldstein, H., and Olswang, L. (2017). Is there a science to facilitate implementation of evidence-based practices and programs? Evid. Based Commun. Assess. Interv. 11, 55–60. doi: 10.1080/17489539.2017.1416768
Gonzálvez, C., Kearney, C. A., Vicent, M., and Sanmartín, R. (2021). Assessing school attendance problems: A critical systematic review of questionnaires. Int. J. Educ. Res. 105:101702. doi: 10.1016/j.ijer.2020.101702
Gozali-Lee, E., Petersen, A., Lee, D., and Hall, T. (2021). Funding for multi-tiered system of supports implementation: Summary of interview findings with Minnesota schools. St. Paul, MN: Wilder Research.
Graves, J. M., Abshire, D. A., Mackelprang, J. L., Amiri, S., and Beck, A. (2020). Association of rurality with availability of youth mental health facilities with suicide prevention services in the US. JAMA Netw. Open 3:e2021471. doi: 10.1001/jamanetworkopen.2020.21471
Greenwald, A., Fleetwood, K., Wagner, B., and Reid, A. (2018). MTSS implementation in Nevada. Carson City, NV: Nevada Department of Education.
Gueldner, B. A., Feuerborn, L. L., and Merrell, K. W. (2020). Social and emotional learning in the classroom: Promoting mental health and academic success. New York, NY: Guilford.
Guy, R., Fields, A., and Edwards, L. (2016). “Implementing response to intervention in a rural setting” in Handbook of response to intervention: The science and practice of multi-tiered systems of support. eds. S. R. Jimerson, M. K. Burns, and A. M. VanDerHeyden (New York: Springer), 693–701.
Hagen, B. N., Sawatzky, A., Harper, S. L., O’Sullivan, T. L., and Jones-Bitton, A. (2022). “Farmers aren’t into the emotions and things, right?”: a qualitative exploration of motivations and barriers for mental health help-seeking among Canadian farmers. J. Agromedicine 27, 113–123. doi: 10.1080/1059924X.2021.1893884
Hall, A., Shoesmith, A., Doherty, E., McEvoy, B., Mettert, K., Lewis, C. C., et al. (2022). Evaluation of measures of sustainability and sustainability determinants for use in community, public health, and clinical settings: a systematic review. Implement. Sci. 17, 1–28. doi: 10.1186/s13012-022-01252-1
Hamlin, D., and Flessa, J. (2018). Parental involvement initiatives: an analysis. Educ. Policy 32, 697–727. doi: 10.1177/0895904816673739
Hart, M. J., Flitner, A. M., Kornbluh, M. E., Thompson, D. C., Davis, A. L., Lanza-Gregory, J., et al. (2021). Combining MTSS and community-based mentoring programs. Sch. Psychol. Rev. 53, 185–199. doi: 10.1080/2372966X.2021.1922937
Hemming, P. J. (2018). Faith schools, community engagement and social cohesion: a rural perspective. Sociol. Rural. 58, 805–824. doi: 10.1111/soru.12210
Herlitz, L., MacIntyre, H., Osborn, T., and Bonell, C. (2020). The sustainability of public health interventions in schools: a systematic review. Implement. Sci. 15, 1–28. doi: 10.1186/s13012-019-0961-8
Herrenkohl, T. I., Hong, S., and Verbrugge, B. (2019). Trauma-informed programs based in schools: linking concepts to practices and assessing the evidence. Am. J. Community Psychol. 64, 373–388. doi: 10.1002/ajcp.12362
Hoeft, T. J., Fortney, J. C., Patel, V., and Unützer, J. (2018). Task-sharing approaches to improve mental health care in rural and other low-resource settings: a systematic review. J. Rural. Health 34, 48–62. doi: 10.1111/jrh.12229
Hollis, C., Falconer, C. J., Martin, J. L., Whittington, C., Stockton, S., Glazebrook, C., et al. (2017). Annual research review: Digital health interventions for children and young people with mental health problems -a systematic and meta‐review. J. Child Psychol. Psychiatry 58, 474–503. doi: 10.1111/jcpp.12663
Hoover, J. J., and Soltero-González, L. (2018). Educator preparation for developing culturally and linguistically responsive MTSS in rural community elementary schools. Teach. Educ. Spec. Educ. 41, 188–202. doi: 10.1177/0888406417753689
Hoover, J. J., Soltero-González, L., Wang, C., and Herron, S. (2020). Sustaining a multitiered system of supports for English learners in rural community elementary schools. Rural Special Educ. Q. 39, 4–16. doi: 10.1177/8756870519847466
Huber, L., Plötner, M., and Schmitz, J. (2019). Social competence and psychopathology in early childhood: a systematic review. Eur. Child Adolesc. Psychiatry 28, 443–459. doi: 10.1007/s00787-018-1152-x
Hull, L., Goulding, L., Khadjesari, Z., Davis, R., Healey, A., Bakolis, I., et al. (2019). Designing high-quality implementation research: development, application, feasibility and preliminary evaluation of the implementation science research development (ImpRes) tool and guide. Implement. Sci. 14, 1–20. doi: 10.1186/s13012-019-0897-z
Johnson, A., Kuhfield, M., and Soland, J. (2021). The forgotten 20%: achievement and growth in rural schools across the nation. AERA Open 7:1105. doi: 10.1177/2332858421105
Jones, A. M., West, K. B., and Suveg, C. (2019). Anxiety in the school setting: a framework for evidence-based practice. Sch. Ment. Heal. 11, 4–14. doi: 10.1007/s12310-017-9235-2
Jongen, C., Campbell, S., Saunders, V., Askew, D., Spurling, G., Gueorguiev, E., et al. (2023). Wellbeing and mental health interventions for indigenous children and youth: a systematic scoping review. Child Youth Serv. Rev. 145:106790. doi: 10.1016/j.childyouth.2022.106790
Katras, M. J., Sharp, E. H., Dolan, E. M., and Baron, L. A. (2015). Non-standard work and rural low-income mothers: making it work. J. Fam. Econ. Iss. 36, 84–96. doi: 10.1007/s10834-014-9410-7
Kearney, C. A. (2016). Managing school absenteeism at multiple tiers: An evidence-based and practical guide for professionals. New York, NY: Oxford University Press.
Kearney, C. A. (2022). Functional impairment guidelines for school attendance problems in youth: recommendations for caseness in the modern era. Prof. Psychol. Res. Pract. 53, 295–303. doi: 10.1037/pro0000453
Kearney, C. A., and Childs, J. (2023a). Improving school attendance data and defining problematic and chronic school absenteeism: the next stage for educational policies and health-based practices. Prev. Sch. Fail. Altern. Educ. Child. Youth 67, 265–275. doi: 10.1080/1045988X.2022.2124222
Kearney, C. A., and Childs, J. (2023b). Translating sophisticated data analytic strategies regarding school attendance and absenteeism into targeted educational policy. Improv. Sch. 26, 5–22. doi: 10.1177/13654802231174986
Kearney, C. A., Dupont, R., Fensken, M., and Gonzálvez, C. (2023). School attendance problems and absenteeism as early warning signals: review and implications for health-based protocols and school-based practices. Front. Educ. 8:1253595. doi: 10.3389/feduc.2023.1253595
Kearney, C. A., and Graczyk, P. A. (2020). A multidimensional, multi-tiered system of supports model to promote school attendance and address school absenteeism. Clin. Child. Fam. Psychol. Rev. 23, 316–337. doi: 10.1007/s10567-020-00317-1
Kearney, C. A., and Graczyk, P. A. (2022). Multi-tiered systems of support for school attendance and its problems: an unlearning perspective for areas of high chronic absenteeism. Front. Educ. 7:1020150. doi: 10.3389/feduc.2022.1020150
Keeler, H., Sjuts, T., Niitsu, K., Watanabe-Galloway, S., Mackie, P. F. E., and Liu, H. (2018). Virtual mentorship network to address the rural shortage of mental health providers. Am. J. Prev. Med. 54, S290–S295. doi: 10.1016/j.amepre.2018.02.001
Kieling, C., Baker-Henningham, H., Belfer, M., Conti, G., Ertem, I., Omigbodun, O., et al. (2011). Child and adolescent mental health worldwide: evidence for action. Lancet 378, 1515–1525. doi: 10.1016/S0140-6736(11)60827-1
Kittelman, A., Strickland-Cohen, M. K., Pinkelman, S. E., and McIntosh, K. (2020). Variables contributing to abandonment and readoption of SWPBIS. J. Posit. Behav. Interv. 22, 67–77. doi: 10.1177/1098300719888748
Klar, H. W., Moyi, P., Ylimaki, R. M., Hardie, S., Andreoli, P. M., Dou, J., et al. (2020). Getting off the list: leadership, learning, and context in two rural, high-needs schools. J. School Leadership 30, 62–83. doi: 10.1177/1052684619867
Knox, P. N., Garnett, B., DeCarolis, J., and Haensch, J. (2024). Community school implementation in rural Vermont. Educ. Policy 39, 572–606. doi: 10.1177/08959048241239893
Kraft, M. A., and Falken, G. T. (2021). A blueprint for scaling tutoring and mentoring across public schools. AERA Open 7:23328584211042858. doi: 10.1177/23328584211042858
Lakin, J. M., Stambaugh, T., Ihrig, L. M., Mahatmya, D., and Assouline, S. G. (2021). Nurturing STEM talent in rural settings. Kappan 103, 24–30. doi: 10.1177/00317217211065823
Larson, M., and Cook, C. R. (2023). “Supporting implementation of evidence-based practices in schools: a focus on linking implementation strategies, determinants, and outcomes” in Handbook of school mental health. eds. S. W. Evans, J. S. Owens, C. P. Bradshaw, and M. D. Weist (Cham: Springer), 419–438.
Lawrence, D., Dawson, V., Houghton, S., Goodsell, B., and Sawyer, M. G. (2019). Impact of mental disorders on attendance at school. Aust. J. Educ. 63, 5–21. doi: 10.1177/0004944118823576
Lee, A., and Gage, N. A. (2020). Updating and expanding systematic reviews and meta-analyses on the effects of school-wide positive behavior interventions and supports. Psychol. Sch. 57, 783–804. doi: 10.1002/pits.22336
Leeman, J., Birken, S. A., Powell, B. J., Rohweder, C., and Shea, C. M. (2017). Beyond “implementation strategies”: classifying the full range of strategies used in implementation science and practice. Implement. Sci. 12:125. doi: 10.1186/s13012-017-0657-x
Leverson, M., Smith, K., McIntosh, K., Rose, J., and Pinkelman, S. (2016). PBIS cultural responsiveness field guide: Resources for trainers and coaches. Washington, DC: OSEP Technical Assistance Center.
Lewis, C. C., Klasnja, P., Powell, B. J., Lyon, A. R., Tuzzio, L., Jones, S., et al. (2018). From classification to causality: advancing understanding of mechanisms of change in implementation science. Front. Public Health 6:136. doi: 10.3389/fpubh.2018.00136
Leytham, P. A., Nguyen, N., and Rago, D. (2021). Curriculum programming in the general education setting for students with autism spectrum disorder. Teach. Except. Child. 53, 404–413. doi: 10.1177/0040059920968885
Liu, X. Q., Guo, Y. X., and Wang, X. (2023). Delivering substance use prevention interventions for adolescents in educational settings: a scoping review. World J. Psychiatr. 13, 409–422. doi: 10.5498/wjp.v13.i7.409
Liverpool, S., Mota, C. P., Sales, C. M., Čuš, A., Carletto, S., Hancheva, C., et al. (2020). Engaging children and young people in digital mental health interventions: systematic review of modes of delivery, facilitators, and barriers. J. Med. Internet Res. 22:e16317. doi: 10.2196/16317
Lobb, R., and Colditz, G. A. (2013). Implementation science and its application to population health. Annu. Rev. Public Health 34, 235–251. doi: 10.1146/annurev-publhealth-031912-114444
Loftus-Rattan, S. M., Wrightington, M., Furey, J., and Case, J. (2023). Multi-tiered system of supports: an ecological approach to school psychology service delivery. Teach. Psychol. 50, 77–85. doi: 10.1177/00986283211024262
Lyon, A. R., and Bruns, E. J. (2019). From evidence to impact: joining our best school mental health practices with our best implementation strategies. Sch. Ment. Heal. 11, 106–114. doi: 10.1007/s12310-018-09306-w
Lyon, A. R., Cook, C. R., Locke, J., Davis, C., Powell, B. J., and Waltz, T. J. (2019). Importance and feasibility of an adapted set of implementation strategies in schools. J. Sch. Psychol. 76, 66–77. doi: 10.1016/j.jsp.2019.07.014
Mandinach, E. B., and Abrams, L. M. (2022). “Data literacy and learning analytics” in The handbook of learning analytics. eds. C. Lang, G. Siemens, A. F. Wise, D. Gašević, and A. Merceron. 2nd ed (Beaumont, AB: Society for Learning Analytics Research), 196–204.
Margaretha, M., Azzopardi, P. S., Fisher, J., and Sawyer, S. M. (2023). School-based mental health promotion: a global policy review. Front. Psych. 14:1126767. doi: 10.3389/fpsyt.2023.1126767
Markle, R. S., Splett, J. W., Maras, M. A., and Weston, K. J. (2014). “Effective school teams: benefits, barriers, and best practices” in Handbook of school mental health: Research, training, practice, and policy. eds. M. Weist, N. Lever, C. Bradshaw, and J. Owens. 2nd ed (Boston, MA: Springer), 59–73.
Martinsen, K. D., Rasmussen, L. M. P., Wentzel-Larsen, T., Holen, S., Sund, A. M., Løvaas, M. E. S., et al. (2019). Prevention of anxiety and depression in school children: effectiveness of the transdiagnostic EMOTION program. J. Consult. Clin. Psychol. 87, 212–219. doi: 10.1037/ccp0000360
McDaniel, S. C., Bloomfield, B. S., Guyotte, K. W., Shannon, T. M., and Byrd, D. H. (2021). Telecoaching to support school wide positive behavior interventions and supports in rural schools. J. Educ. Stud. Placed Risk 26, 236–252. doi: 10.1080/10824669.2020.1834395
McDermott, E. R., Anderson, S., and Zaff, J. F. (2018). Dropout typologies: relating profiles of risk and support to later educational re-engagement. Appl. Dev. Sci. 22, 217–232. doi: 10.1080/10888691.2016.1270764
McGorry, P. D., Mei, C., Chanen, A., Hodges, C., Alvarez-Jimenez, M., and Killackey, E. (2022). Designing and scaling up integrated youth mental health care. World Psychiatry 21, 61–76. doi: 10.1002/wps.20938
McIntosh, K., and Goodman, S. (2016). Integrated multi-tiered systems of support: Blending RTI and PBIS. New York, NY: Guilford.
Meyers, D. C., Durlak, J. A., and Wandersman, A. (2012). The quality implementation framework: a synthesis of critical steps in the implementation process. Am. J. Community Psychol. 50, 462–480. doi: 10.1007/s10464-012-9522-x
Michael, K., Fischer, A. J., and Olsen, T. (2025). Addressing mental health needs in rural and indigenous communities: serving people on their terms. Focus 23, 19–24. doi: 10.1176/appi.focus.20240035
Michael, K., Yaros, A., Counts, J., and Hersh, J. (2023). “Preparing school mental health providers for practice in rural communities” in Handbook of school mental health: Innovations in science and practice. eds. S. W. Evans, J. S. Owens, C. P. Bradshaw, and M. D. Weist (Cham: Springer), 313–327.
Moodley, R., Chiclana, F., Carter, J., and Caraffini, F. (2020). Using data mining in educational administration: a case study on improving school attendance. Appl. Sci. 10:3116. doi: 10.3390/app10093116
Moore, J. E., Mascarenhas, A., Bain, J., and Straus, S. E. (2017). Developing a comprehensive definition of sustainability. Implement. Sci. 12, 110–118. doi: 10.1186/s13012-017-0637-1
Morales, D. A., Barksdale, C. L., and Beckel-Mitchener, A. C. (2020). A call to action to address rural mental health disparities. J. Clin. Transl. Sci. 4, 463–467. doi: 10.1017/cts.2020.42
Morse, T. E. (2024). Revisiting the multi-tiered system of supports framework: an important mechanism for realizing equitable education in urban schools. Educ. Urban Soc. 56, 1051–1064. doi: 10.1177/00131245241262013
Moullin, J. C., Dickson, K. S., Stadnick, N. A., Rabin, B., and Aarons, G. A. (2019). Systematic review of the exploration, preparation, implementation, sustainment (EPIS) framework. Implement. Sci. 14, 1–16. doi: 10.1186/s13012-018-0842-6
National Center for Education Statistics (2023). Enrollment and school choice in rural areas. Washington, DC: US Department of Education.
Nichols, L. M., Goforth, A. N., Sacra, M., and Ahlers, K. (2017). Collaboration to support rural student social-emotional needs. Rural. Educ. 38, 38–48.
Nilsen, P. (2020). “Making sense of implementation theories, models, and frameworks” in Implementation science 3.0. eds. B. Albers, A. Shlonsky, and R. Mildon (Geneva: Springer), 53–79.
Nilsen, P., and Bernhardsson, S. (2019). Context matters in implementation science: a scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv. Res. 19:189. doi: 10.1186/s12913-019-4015-3
Nitz, J., Brack, F., Hertel, S., Krull, J., Stephan, H., Hennemann, T., et al. (2023). Multi-tiered systems of support with focus on behavioral modification in elementary schools: a systematic review. Heliyon 9:e17506. doi: 10.1016/j.heliyon.2023.e17506
Nygaard, M. A., Ormiston, H. E., and Husmann, P. R. (2025). Barriers that interfere with the delivery of intensive school mental health services. J. Rural Ment. Health. doi: 10.1037/rmh0000289
Olsen, J., Edirmanasinghe, N., Donohue, P., and Betters-Bubon, J. (2023). “Addressing barriers to culturally responsive and sustaining MTSS implementation and school counseling program alignment: practical strategies for school counselors” in The school counselor’s guide to multi-tiered systems of support. eds. E. Goodman-Scott, J. Betters-Bubon, P. Donohue, and J. Olsen. 2nd ed (New York, NY: Routledge), 351–370.
Olson, J. R., Benjamin, P. H., Azman, A. A., Kellogg, M. A., Pullmann, M. D., Suter, J. C., et al. (2021). Systematic review and meta-analysis: effectiveness of wraparound care coordination for children and adolescents. J. Am. Acad. Child Adolesc. Psychiatry 60, 1353–1366. doi: 10.1016/j.jaac.2021.02.022
Olson, S., Lindsey, B. C., and Tan, K. (2022). “Social-emotional learning in a multitiered system” in The art of becoming indispensable. eds. T. Cox, T. Fitzgerald, and M. E. Alvarez (New York, NY: Oxford), 126–132.
Ormiston, H. E., Nygaard, M. A., and Husmann, P. (2025). School-based mental health practices within a multi-tiered system of support: a mixed methods investigation of targeted and intensive services. Psychol. Sch. 62, 1087–1099. doi: 10.1002/pits.23380
Oyen, K. A., and Wollersheim-Shervey, S. (2019). An examination of critical features of positive frameworks: impact in rural environments for school-based practitioners. Contemp. Sch. Psychol. 23, 388–400. doi: 10.1007/s40688-018-0198-6
Patel, S. Y., Huskamp, H. A., Busch, A. B., and Mehrotra, A. (2020). Telemental health and US rural–urban differences in specialty mental health use, 2010–2017. Am. J. Public Health 110, 1308–1314. doi: 10.2105/AJPH.2020.305657
Pierce, C. D., and Mueller, T. G. (2018). Easy as ABC: data-based guidelines for implementing a multitiered system of supports into rural schools. Rural Special Educ. Q. 37, 183–191. doi: 10.1177/8756870518777850
Polaha, J., Williams, S. L., Heflinger, C. A., and Studts, C. R. (2015). The perceived stigma of mental health services among rural parents of children with psychosocial concerns. J. Pediatr. Psychol. 40, 1095–1104. doi: 10.1093/jpepsy/jsv054
Polanczyk, G. V., Salum, G. A., Sugaya, L. S., Caye, A., and Rohde, L. A. (2015). Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J. Child Psychol. Psychiatry 56, 345–365. doi: 10.1111/jcpp.12381
Porter, S. G. (2022). “It takes a well-organized village: implementing RTI/MTSS models in secondary schools” in Research anthology on inclusive practices for educators and administrators in special education. ed. M. Khosrow-Pour (Hershey, PA: IGI Global), 339–368.
Powell, B. J., Waltz, T. J., Chinman, M. J., Damschroder, L. J., Smith, J. L., Matthieu, M. M., et al. (2015). A refined compilation of implementation strategies: results from the expert recommendations for implementing change (ERIC) project. Implement. Sci. 10:21. doi: 10.1186/s13012-015-0209-1
Preston, J., and Barnes, K. E. (2017). Successful leadership in rural schools: cultivating collaboration. Rural Educ. 38, 6–15. doi: 10.35608/ruraled.v38i1.231
Radez, J., Reardon, T., Creswell, C., Orchard, F., and Waite, P. (2022). Adolescents’ perceived barriers and facilitators to seeking and accessing professional help for anxiety and depressive disorders: a qualitative interview study. Eur. Child Adolesc. Psychiatry 31, 891–907. doi: 10.1007/s00787-020-01707-0
Rapee, R. M., Bőgels, S. M., Van Der Sluis, C. M., Craske, M. G., and Ollendick, T. (2012). Annual research review: Conceptualising functional impairment in children and adolescents. J. Child Psychol. Psychiatry 53, 454–468. doi: 10.1111/j.1469-7610.2011.02479.x
Rapport, F., Clay-Williams, R., Churruca, K., Shih, P., Hogden, A., and Braithwaite, J. (2018). The struggle of translating science into action: foundational concepts of implementation science. J. Eval. Clin. Pract. 24, 117–126. doi: 10.1111/jep.12741
Reinbergs, E. J., and Fefer, S. A. (2018). Addressing trauma in schools: multitiered service delivery options for practitioners. Psychol. Sch. 55, 250–263. doi: 10.1002/pits.22105
Robinson, G. G., Bursuck, W. D., and Sinclair, K. D. (2013). Implementing RTI in two rural elementary schools: encouraging beginnings and challenges for the future. Rural. Educ. 34, 1–9.
Ryan, A. M., Shim, S. S., and Makara, K. A. (2013). Changes in academic adjustment and relational self-worth across the transition to middle school. J. Youth Adolesc. 42, 1372–1384. doi: 10.1007/s10964-013-9984-7
Sahin, M., and Ifenthaler, D. (2021). Visualizations and dashboards for learning analytics. Cham: Springer.
Saldana, L. (2014). The stages of implementation completion for evidence-based practice: protocol for a mixed methods study. Implement. Sci. 9, 1–11. doi: 10.1186/1748-5908-9-43
Sanetti, L. M., and Collier-Meek, M. A. (2019). Increasing implementation science literacy to address the research-to-practice gap in school psychology. J. Sch. Psychol. 76, 33–47. doi: 10.1016/j.jsp.2019.07.008
Santiago, R. T., Hall, G. J., Garbacz, S. A., Gulbrandson, K., and Albers, C. A. (2025). Examining an integrated factor structure of schoolwide MTSS implementation measures. J. Posit. Behav. Interv. 27, 39–49. doi: 10.1177/10983007241249524
Schafft, K. A. (2016). Rural education as rural development: understanding the rural school–community well-being linkage in a 21st-century policy context. Peabody J. Educ. 91, 137–154. doi: 10.1080/0161956X.2016.1151734
Schlief, M., Saunders, K. R., Appleton, R., Barnett, P., San Juan, N. V., Foye, U., et al. (2022). Synthesis of the evidence on what works for whom in telemental health: rapid realist review. Int. J. Med. Res. 11:e38239. doi: 10.2196/38239
Schultz, K., Farmer, S., Harrell, S., and Hostetter, C. (2021). Closing the gap: increasing community mental health services in rural Indiana. Community Ment. Health J. 57, 684–700. doi: 10.1007/s10597-020-00737-x
Scott, C. K., Dennis, M. L., Grella, C. E., Funk, R. R., and Lurigio, A. J. (2019). Juvenile justice systems of care: results of a national survey of community supervision agencies and behavioral health providers on services provision and cross-system interactions. Health Justice 7:11. doi: 10.1186/s40352-019-0093-x
Scott, T. M., Gage, N. A., Hirn, R. G., Lingo, A. S., and Burt, J. (2019). An examination of the association between MTSS implementation fidelity measures and student outcomes. Prev. Sch. Fail. Altern. Educ. Child. Youth 63, 308–316. doi: 10.1080/1045988X.2019.1605971
Seelig, J. L., and McCabe, K. M. (2021). Why teachers stay: shaping a new narrative on rural teacher retention. J. Res. Rural. Educ. 37, 1–16. doi: 10.26209/jrre3708
Shadur, J. M., and Lejuez, C. W. (2015). Adolescent substance use and comorbid psychopathology: Emotion regulation deficits as a transdiagnostic risk factor. Curr. Addict. Rep. 2, 354–363. doi: 10.1007/s40429-015-0070-y
Shamblin, S., Graham, D., and Bianco, J. A. (2016). Creating trauma-informed schools for rural Appalachia: the partnerships program for enhancing resiliency, confidence and workforce development in early childhood education. Sch. Ment. Heal. 8, 189–200. doi: 10.1007/s12310-016-9181-4
Shenoy, S., Johnson, C., and Nannemann, A. (2024). School collaboration in a rural setting: improving student reading outcomes by implementing a tiered model of instruction. Sch. Community J. 34, 311–334.
Shepherd, K., and Salembier, G. (2011). Improving schools through a response to intervention approach: a cross-case analysis of three rural schools. Rural Special Educ. Q. 30, 3–15. doi: 10.1177/875687051103000302
Singer, J. B., Erbacher, T. A., and Rosen, P. (2019). School-based suicide prevention: A framework for evidence-based practice. Sch. Ment. Health. 11, 54–71. doi: 10.1007/s12310-018-9245-8
Smith, M., Roberts, A., Elahi, S., Eihentale, L., O’Rourke, M., Meldrum, M., et al. (2025). Efforts to improve and expand implementation of trauma-responsive schools: findings from a randomized pilot of the trauma education to advance community healing (TEACH) program. Sch. Ment. Heal. 6, 1–19. doi: 10.1007/s12310-024-09739-6
Smythe-Leistico, K., and Page, L. C. (2018). Connect-text: Leveraging text-message communication to mitigate chronic absenteeism and improve parental engagement in the earliest years of schooling. J. Educ. Stud. Placed Risk. 23, 139–152. doi: 10.1080/10824669.2018.1434658
Splett, J. W., Trainor, K. M., Raborn, A., Halliday-Boykins, C. A., Garzona, M. E., Dongo, M. D., et al. (2018). Comparison of universal mental health screening to students already receiving intervention in a multitiered system of support. Behav. Disord. 43, 344–356. doi: 10.1177/0198742918761339
Stoiber, K. C., and Gettinger, M. (2016). “Multi-tiered systems of support and evidence-based practices” in The handbook of response to intervention: The science and practice of multi-tiered systems of support. eds. K. Jimerson, A. M. Burns, and A. M. VanDerHeyden. 2nd ed (New York, NY: Springer), 124–141.
Sugai, G., and Horner, R. H. (2020). Sustaining and scaling positive behavioral interventions and supports: implementation drivers, outcomes, and considerations. Except. Child. 86, 120–136. doi: 10.1177/0014402919855331
Sulkowski, M. L., and Michael, K. (2014). Meeting the mental health needs of homeless students in schools: a multi-tiered system of support framework. Child Youth Serv. Rev. 44, 145–151. doi: 10.1016/j.childyouth.2014.06.014
Sussman, K., Burns, M. K., and Lembke, E. S. (2022). Effects of ECHO MTSS teleconsultation model on self-efficacy of data-based individualization of academic interventions. J. Educ. Psychol. Consult. 32, 395–415. doi: 10.1080/10474412.2021.1996243
Sylvan, L., Gouck, M., and Kwak, M. (2025). Teletherapy and multi-tiered system of support: synergies and challenges for school-based speech-language pathologists. Lang. Speech Hear. Serv. Sch. 11, 1–21. doi: 10.1044/2024_LSHSS-24-00088
Thomas, E. R., Lembke, E. S., and Gandhi, A. G. (2023). Universal design for learning within an integrated multitiered system of support. Learn. Disabil. Res. Pract. 38, 57–69. doi: 10.1111/ldrp.12302
Thomas, M. S., Crosby, S., and Vanderhaar, J. (2019). Trauma-informed practices in schools across two decades: an interdisciplinary review of research. Rev. Res. Educ. 43, 422–452. doi: 10.3102/0091732X18821123
Turner, L., Calvert, H. G., Fleming, C. M., Lewis, T., Siebert, C., Anderson, N., et al. (2022). Study protocol for a cluster-randomized trial of a bundle of implementation support strategies to improve the fidelity of implementation of schoolwide positive behavioral interventions and supports in rural schools. Contemp. Clin. Trials Commun. 28:100949. doi: 10.1016/j.conctc.2022.100949
Vernon-Feagans, L., and Swingler, M. M. (2020). “Early development and family life in rural America” in Rural families and communities in the United States: Facing challenges and leveraging opportunities. eds. J. E. Glick, S. M. McHale, and V. King (New York, NY: Springer), 201–235.
Vetter, J. B., Fuxman, S., and Dong, Y. E. (2024). A statewide multi-tiered system of support (MTSS) approach to social and emotional learning (SEL) and mental health. Soc. Emot. Learning Res. Prac. Policy 3:100046. doi: 10.1016/j.sel.2024.100046
Wallender, J. L., Hiebel, A. L., PeQueen, C. V., and Kain, M. A. (2020). Effects of an explicit curriculum on social-emotional competency in elementary and middle school students. Delta Kappa Gamma Bulletin 86, 32–43.
Waltz, T. J., Powell, B. J., Matthieu, M. M., Damschroder, L. J., Chinman, M. J., Smith, J. L., et al. (2015). Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the expert recommendations for implementing change (ERIC) study. Implement. Sci. 10:109. doi: 10.1186/s13012-015-0295-0
Wang, S., Li, Q., Lu, J., Ran, H., Che, Y., Fang, D., et al. (2023). Treatment rates for mental disorders among children and adolescents: a systematic review and meta-analysis. JAMA Netw. Open 6:e2338174. doi: 10.1001/jamanetworkopen.2023.38174
Wargo, E., Carr Chellman, D., Budge, K., and Canfield Davis, K. (2021). On the digital frontier: stakeholders in rural areas take on educational technology and schooling. J. Res. Technol. Educ. 53, 140–158. doi: 10.1080/15391523.2020.1760753
Waschbusch, D. A., Breaux, R. P., and Babinski, D. E. (2019). School-based interventions for aggression and defiance in youth: a framework for evidence-based practice. Sch. Ment. Heal. 11, 92–105. doi: 10.1007/s12310-018-9269-0
Weare, K. (2017). “Promoting social and emotional wellbeing and responding to mental health problems in schools” in Global mental health: Prevention and promotion. eds. S. Bährer-Kohler and F. Carod-Artal (Cham: Springer), 113–125.
Webb, A. F., and Michalopoulou, L. E. (2021). School psychologists as agents of change: implementing MTSS in a rural school district. Psychol. Sch. 58, 1642–1654. doi: 10.1002/pits.22521
Weingarten, Z., Zumeta Edmonds, R., and Arden, S. (2020). Better together: using MTSS as a structure for building school–family partnerships. Teach. Except. Child. 53, 122–130. doi: 10.1177/0040059920937733
Weist, M. D., Hoover, S. A., Daly, B. P., Short, K. H., and Bruns, E. J. (2023). Propelling the global advancement of school mental health. Clin. Child. Fam. Psychol. Rev. 26, 851–864. doi: 10.1007/s10567-023-00434-7
Werch, B. L., and Runyons-Hiers, J. (2020). Making MTSS system-level change in a rural district. Communique 49, 14–15.
Williams, N. J., and Beidas, R. S. (2019). Annual research review: the state of implementation science in child psychology and psychiatry: a review and suggestions to advance the field. J. Child Psychol. Psychiatry 60, 430–450. doi: 10.1111/jcpp.12960
Wilson, C., and Cariola, L. A. (2020). LGBTQI+ youth and mental health: a systematic review of qualitative research. Adolesc. Res. Rev. 5, 187–211. doi: 10.1007/s40894-019-00118-w
Yell, M. L. (2018). “Response to intervention, multi-tiered systems of support, and federal law: analysis and commentary” in Handbook of response to intervention and multi-tiered systems of support. eds. P. C. Pullen and M. J. Kennedy (New York, NY: Routledge).
Keywords: rural schools, multi-tiered systems of support, implementation science, School Implementation Strategies, Translating Eric Resources, school-based teams, school mental health
Citation: Kearney CA, Fensken M and Dupont R (2025) Implementing multi-tiered systems of support in rural schools: a practice perspective for improving mental health care for underserved youths. Front. Educ. 10:1553528. doi: 10.3389/feduc.2025.1553528
Edited by:
Angeliki Kallitsoglou, University of Exeter, United KingdomReviewed by:
Simon Benham-Clarke, University of Exeter, United KingdomNancy Lever, University of Maryland, United States
Jacob Olsen, California State University, Long Beach, United States
Copyright © 2025 Kearney, Fensken and Dupont. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christopher A. Kearney, Y2hyaXMua2Vhcm5leUB1bmx2LmVkdQ==
 Christopher A. Kearney
Christopher A. Kearney Michael Fensken
Michael Fensken