- Rocky Mountain Hospital for Children, Denver, CO, United States
Background and objective: The COVID-19 pandemic substantially impacted mental health globally, leading to increased levels of anxiety and fear. Although it is well known that socioeconomic factors and ethnicity play a role in mental health outcomes, the intersectional effects of these determinants during the pandemic are unclear, especially among adolescents. Thus, this study sought to explore the relationship between socioeconomic factors, ethnicity, and two mental health parameters—fear of COVID-19 (FCV) and generalized anxiety disorder (GAD)—among high school students in California, United States.
Methods: A cross-sectional analysis was performed with 990 high school-aged participants from the San Joaquin Valley and Santa Clara County, California, recruited via convenience/snowball sampling using an online questionnaire from 15 June to 14 August 2022. The Fear of Coronavirus Scale (FCV-19S) and Generalized Anxiety Disorder-7 (GAD-7) were used to measure fear and anxiety, respectively.
Results: The results reveal significant associations between ethnicity, socioeconomic status (i.e., family income), and FCV-19S and GAD-7 scores. Severe GAD and FCV were reported in 9.8% (n = 97) and 8.38% (n = 83) of participants. Black participants reported significantly higher levels of FCV (F = 6.867, p < 0.001) and generalized anxiety (F = 17.066, <0.001) than their counterparts Additionally, girls exhibited higher anxiety scores (t = 2.960, p = 0.003, CI = 0.23–1.15) and fear scores (t = 3.619, p = 0.001, CI = 0.40–1.37) than boys. Furthermore, fear and anxiety scores exhibited a strong positive correlation (r = 0.702, p < 0.001).
Conclusion: This study suggests that gender, ethnicity, and socioeconomic factors are significantly linked to higher levels of FCV and GAD in teenagers during the pandemic. These findings underscore the importance of considering social determinants of mental health when addressing the psychological impact of COVID-19 on teenagers, particularly for vulnerable populations.
Introduction
The coronavirus disease 2019 (COVID-19), caused by the virus SARS-CoV-2, was officially declared a pandemic by the World Health Organization (WHO) on 11 March 2019 (World Health Organization, 2020). According to the WHO, there were more than 70 million COVID-19 infections and more than 7 million deaths (WHO, 2024). Thus, the COVID-19 pandemic had a profound impact on societies, health systems, and economies worldwide, resulting in widespread economic, social, and mental health-related issues (Chakraborty and Maity, 2020; Naseer et al., 2023; Pfefferbaum and North Carol, 2020). Moreover, the pandemic resulted in a humanitarian crisis, including excess deaths beyond official COVID-19 figures, significant disruptions in health services, and increased mortality rates (Moynihan et al., 2021; Sawicka et al., 2022).
In addition to widespread socioeconomic effects and precipitous increases in morbidity and mortality, the COVID-19 pandemic has also greatly impacted mental health, with mental health conditions such as stress-related disorders rising dramatically across a wide range of populations, including the general public, COVID-19 patients and their loved ones, police, teachers, individuals with pre-existing mental health conditions, and healthcare workers (Bower et al., 2023; Khan et al., 2022; Kush et al., 2022; Majeed et al., 2021; Manchia et al., 2022; Robinson et al., 2023; Stogner et al., 2020). In particular, psychological stress and mental health issues—such as loneliness, depression, anxiety, and traumatic stress—were especially pronounced in children and adolescents resulting from health concerns, disruption in school education, social distancing measures, self-isolation/social disconnection, and lockdowns (Jost et al., 2023; Kupcova et al., 2023; Meherali et al., 2021; Panchal et al., 2023; Wolf and Schmitz, 2024). Furthermore, studies have shown that vulnerable populations were disproportionately affected by the pandemic, exacerbating existing inequalities based on income, age, ethnicity, sex, and geographic location (Choukou et al., 2022; Sawicka et al., 2022; Siegel and Mallow, 2021). However, the impacts of intersecting determinants of health on mental health outcomes during the COVID-19 pandemic remain poorly understood, especially among youth (Pujolar et al., 2022; Sawicka et al., 2022).
Social determinants of health (SDOH) [e.g., socioeconomic status (SES), ethnicity, access to healthcare, stigma, and trauma] have been shown to be associated with negative psychological impacts of COVID-19, such as anxiety, fear, stress, and depression (Siegel and Mallow, 2021; Thomeer et al., 2023). It has been shown that Black persons, Hispanic persons, and Asian persons experienced a more significant decline in mental health than white adults during the COVID-19 pandemic (Thomeer et al., 2023). Furthermore, limited access to mental health services in these marginalized groups resulted in higher levels of unmet mental healthcare needs throughout the pandemic (Thomeer et al., 2023). Additionally, a study that included a nationally representative sample of 2,709 adults residing in the United States, with a deliberate oversampling of minority populations, revealed that Latine individuals exhibited the highest prevalence of severe distress, followed by Asian and Black persons, while white individuals exhibited the lowest prevalence of stress (Wen et al., 2023). These mental health disparities were largely attributed to socioeconomic disadvantages in certain ethnic groups (Wen et al., 2023). Moreover, the COVID-19 pandemic and lockdown have been shown to exacerbate the already severe negative impacts of socioeconomic deprivation on mental health and wellbeing owing to increased social stresses, stigma, and trauma (Bonnini and Borghesi, 2022; Lee et al., 2022).
According to a study, the prevalence of depressive symptoms, anxiety symptoms, and a combination of both depressive and anxiety symptoms among Chinese high school students during the COVID-19 outbreak was found to be 43.7, 37.4, and 31.3%, respectively. A multivariable logistic regression analysis indicated that girls constituted a significant risk factor for the manifestation of depressive and anxiety symptoms (Zhou et al., 2020).
Children and adolescents faced numerous stressors during the pandemic, including the loss of access to mental healthcare, social services, income, food, and housing, as well as the loss of loved ones to COVID-19. These challenges resulted in persistent anxiety, worry, and distress among young people (Fortuna et al., 2023). In particular, factors such as sex, SES, and cultural conditions can influence the prevalence of anxiety disorders (Fortuna et al., 2023). Moreover, the pandemic has disproportionately affected ethnic minority youth, who have experienced higher rates of anxiety, depression, and other mental health issues owing to increased stressors and discrimination (Kauhanen et al., 2023; Samji et al., 2022).
While the psychological effects of COVID-19 in youth have been well characterized, few studies have explored the effects of ethnicity and socioeconomic factors on mental health in high school students during the COVID-19 pandemic, specifically in relation to fear of COVID-19 (FCV) and generalized anxiety disorder (GAD), specifically among American adolescents. This knowledge gap impedes the formulation of targeted interventions designed to address the distinct mental health needs of this vulnerable population, particularly those originating from marginalized communities.
The objective of the present study was to elucidate the effects of mental health, along with ethnic, sociodemographic, and social factors, on high school students during the COVID-19 pandemic. Using an intersectional lens, the study explores how socioeconomic and demographic factors influence GAD and fear of COVID-19 among teenagers in California, United States, highlighting inequalities related to ethnicity and SES.
Methods
Ethical considerations
The present study followed the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines for cross-sectional studies (von Elm et al., 2007). Ethical clearance for data collection and the study was obtained from the Ethics and Review Committee from Summit Tahoma via A Brush on Recovery (EC/2022/017A). To maintain confidentiality, this study used anonymous online surveys, encrypted data transmission, and secure data storage.
Study design and participants
This cross-sectional study included 990 high school-aged participants who were recruited through a convenience/snowball sampling method using an online questionnaire. This approach allowed for the efficient recruitment of a diverse group of adolescents during the COVID-19 pandemic. To maintain participant anonymity and minimize social desirability bias, the study implemented several strategies. Potential biases were identified and addressed through data weighting, validation, and strict confidentiality measures. By recruiting participants from various educational institutions and online platforms, we reduced selection bias and improved sample diversity, ensuring a more accurate representation of the target population despite the limitations associated with convenience sampling.
Survey forms were initially shared with Teenagers who attended A Brush on Recovery, a 501(c)(3) non-profit organization that promotes mental health awareness and opiate recovery, after which the students were asked to circulate the survey via WhatsApp. Inclusion criteria were as follows: enrollment in high school and residency in California at the time of the study. Those who were under psychiatric treatment were excluded. Moreover, students who (or their parents) did not sign the informed consent were also excluded from the study. Participants were assured anonymity, as no personal or identifiable information was collected or stored, and participants were offered the option to discontinue the survey or skip questions if they were uncomfortable.
Data collection
Data were collected via an online survey administered through Google Forms and disseminated via WhatsApp over a 2-month period from 15 June to 14 August 2022. Participants were invited to complete the survey at their convenience, with instructions provided for accessing and submitting their responses electronically.
The survey used in the present study consisted of three parts. Part 1 of the survey instrument consisted of questions pertaining to demographic characteristics and SES (exposure variable). The demographic section included questions related to sex, age, and ethnicity, with a focus on the following groups: white persons, Black persons, Hispanic persons, Asian persons, and Others (encompassing people who identified as Arab, European, and other ethnicities). Part 2 and part 3 assessed the outcome variables, in which part 2 was comprised of The Fear of Coronavirus Scale (FSC-19S) (Ahorsu et al., 2022) and part 3 had questions from The Generalized Anxiety Disorder-7 (GAD-7) Scale (Spitzer et al., 2006).
Measures
Fear of Coronavirus Scale (FSC-19S)
The Fear of Coronavirus Scale (FSC-19S), a validated scale, with Cronbach’s α value of 0.82, was used to assess participants’ fear related to COVID-19 (Ahorsu et al., 2022). For the current data, the internal consistency was found to be 0.73, which is acceptable. This scale consists of seven items measured on a 5-point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). Total scores on the FSC-19S range from 7 to 35, where higher scores indicate greater fear of COVID-19. The main outcome was a score of ≥21 points, which was suggestive that individuals were experiencing psychological distress or facing challenges in their daily lives owing to the fear of COVID-19 (Midorikawa et al., 2022).
Generalized Anxiety Disorder-7 (GAD-7) Scale
The Generalized Anxiety Disorder-7 (GAD-7) scale, with Cronbach’s α value of 0.92 (Spitzer et al., 2006) was employed to measure the severity of participants’ anxiety. For the current data, the internal consistency was found to be 0.756, which is acceptable. This scale comprises seven items that assess symptoms of anxiety over the previous 2 weeks. Participants rate each item on a scale of 0 to 3, corresponding to “not at all,” “several days,” “more than half the days,” and “nearly every day,” respectively. The total score on the GAD-7 ranges from 0 to 21, with scores categorized as follows:
• 0–4: Minimal anxiety
• 5–9: Mild anxiety
• 10–14: Moderate anxiety
• 15–21: Severe anxiety
Sample size calculation
A finite population correction (FPC) was applied owing to the large population size (N = 1,000,000). We hypothesized a 50% prevalence (p) of the outcome factor with a desired margin of error of +/− 5% (d). To achieve a high degree of certainty (99% confidence level), a design effect (DEFF) of 1 (assuming no cluster sampling) was used in the sample size calculation. The formula employed was N = [DEFF*Np(1 − p)]/[(d2/Z2(1 − α/2)) + (p(1 − p))], where n is the sample size, Z is the Z-statistic for the confidence level (2.576 for 99%), and α is the significance level (α = 0.01). This resulted in a calculated sample size of 810 to ensure sufficient power to detect a statistically significant difference in the outcome factor between the study population and the hypothesized prevalence, while prioritizing a high level of confidence in the generalizability of the findings. The sample size calculations were performed using OpenEpi, version 3, an open-source online calculator.1
Data analyses
Statistical analyses were performed using the Statistical Package for Social Sciences (SPSS version 26; Armonk, New York, United States). Sociodemographic data were reported as frequencies and percentages. Independent-samples t-tests and one-way ANOVA were used to analyze differences in the FCV and anxiety scores and their correlation with sociodemographic variables, respectively. Moreover, post hoc analyses were performed to assess the differences in the GAD-7 and FCV-19S scores between the different categories (i.e., ethnicity, SES, and household size). Finally, Pearson’s correlation test was used to evaluate the correlation between the GAD-7 and FCV-19S scores.
Results
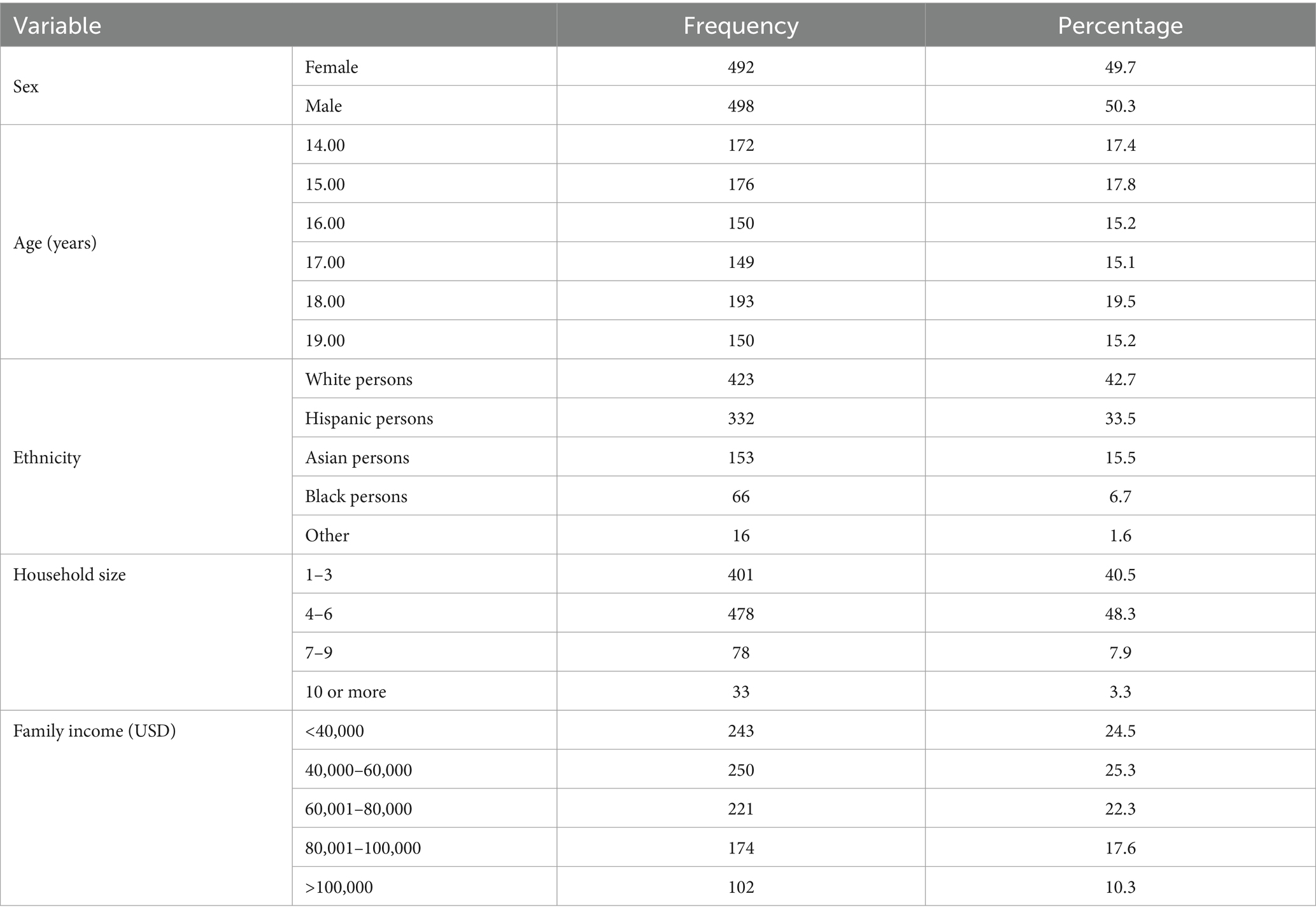
The demographic characteristics of the study participants are presented in Table 1. The study population consisted of 990 participants, of which 492 indicated that they were female (49.7%) and 498 indicated they were male (50.3%). The participants had an age range of 14–19 years, of which the majority were 18 years old (n = 193, 19.5%). The ethnic distribution was as follows: 423 (42.7%) white persons, 332 (33.5%) Hispanic persons, 153 (15.5%) Asian persons, 66 (6.7%) Black persons, and 16 (1.6%) Other. The majority of the participants, 478 (48.3%), lived in households with four to six people, and the family income was distributed across several different brackets, ranging from less than $40,000 (24.5%) to >$100,000 (10.3%) (Table 1).
According to the GAD-7 scoring criteria, minimal anxiety was reported in 63 participants (6.3%), mild anxiety in 360 (36.4%), moderate anxiety in 471 (47.6%), and severe anxiety in 97 participants (9.8%) (Figure 1). The mean GAD score was 10.26 (SD = 3.69); the medium GAD score was found to be 10. The minimum and maximum GAD scores were 1 and 21, respectively.
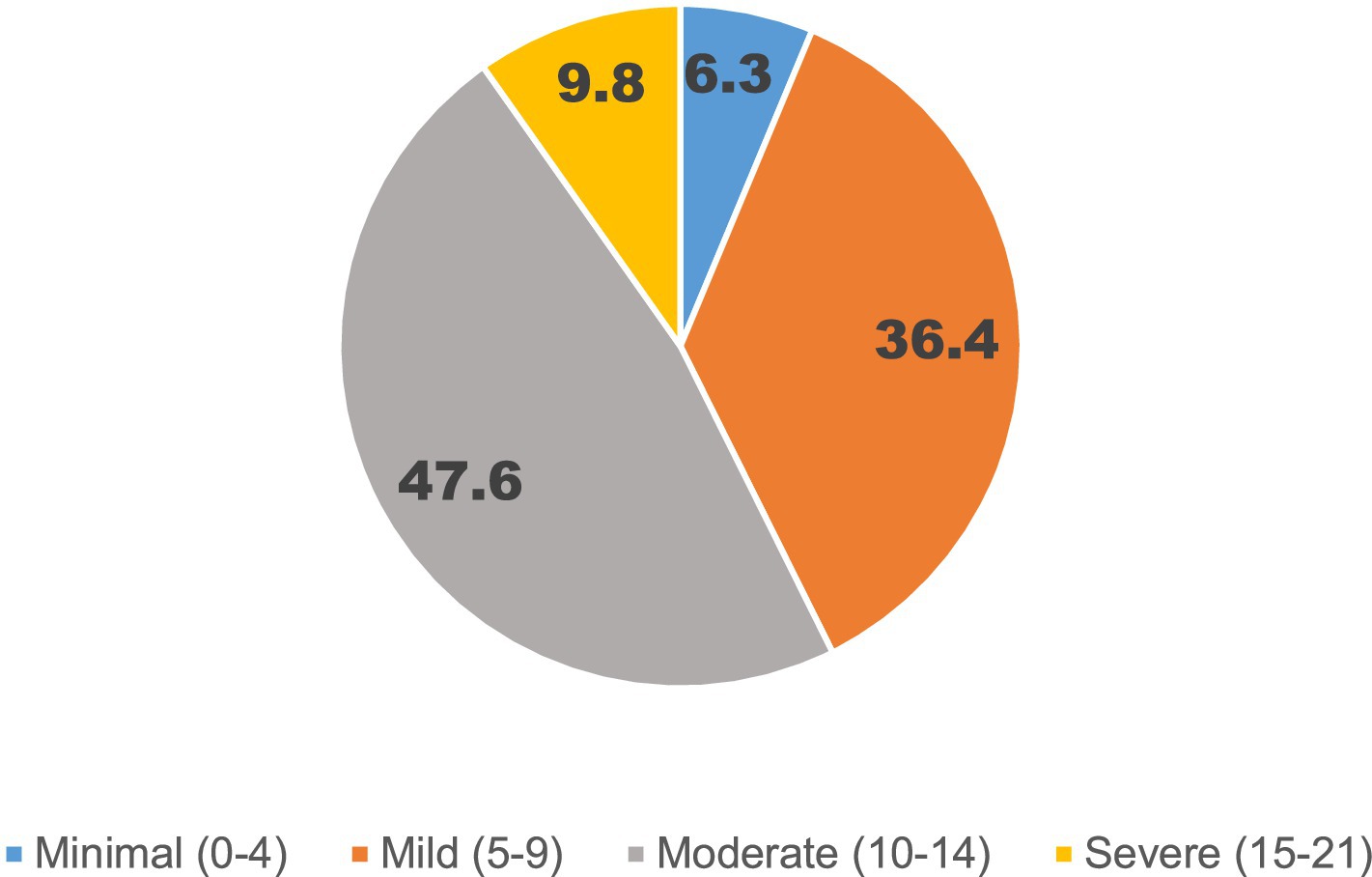
Figure 1. Percentage of population according to different levels of anxiety as measured by the Generalized Anxiety Disorder-7 Scale.
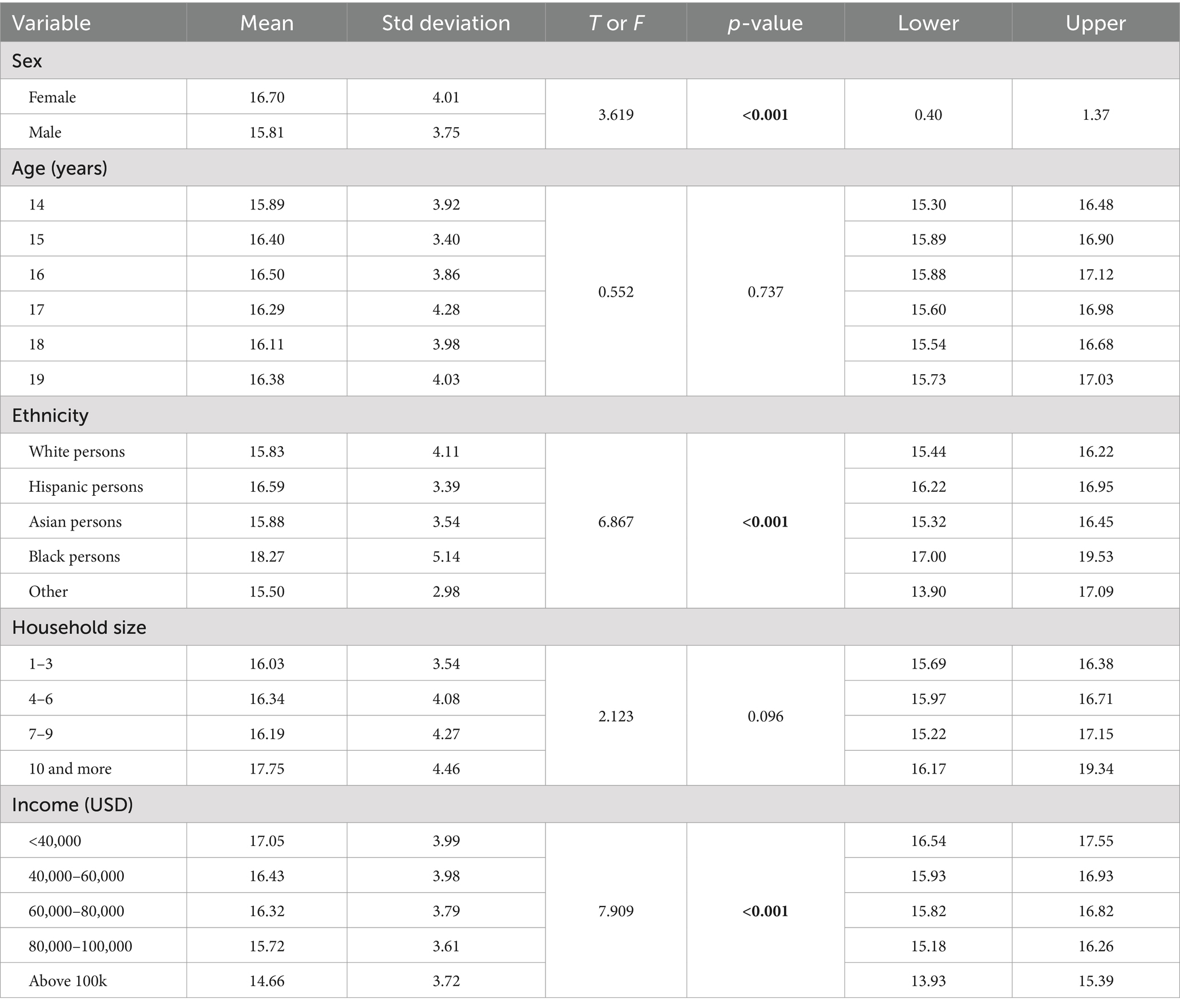
Additionally, we assessed the association between demographic factors and generalized anxiety (Table 2) as measured by the GAD-7. Female participants had a mean anxiety score of 10.61 (SD = 3.64), which was significantly higher than that of male participants (x̄ = 9.91; SD = 3.71; t = 2.96, p = 0.003, CI = 0.23–1.15). Anxiety scores varied by age, with means ranging from 9.83 (SD = 3.63) for 14-year-olds to 10.55 (SD = 3.71) for 15-year-olds. However, no significant differences were observed across age groups (F = 1.107, p = 0.355). Significant differences in anxiety scores were observed as a function of ethnic group (F = 17.066, p < 0.001), in which Black participants exhibited the highest mean anxiety score (x̄ = 12.09; SD = 4.49), followed by Hispanic participants (x̄ = 11.22; SD = 3.72). White participants exhibited the lowest mean score (x̄ = 9.53, SD = 3.51). Tukey’s post hoc test revealed that there is a significant difference between the level of score between white and Hispanic participants (p < 0.001) and white and Black participants (p < 0.001). Similarly, there were also significant differences between Asian and Hispanic participants, and between Asian and Black participants (p < 0.001). There was no statistically significant difference between the white and Asian participants and Hispanic and Black participants (p > 05). Participants in the Other category did not show any significant differences in GAD levels compared to other ethnicities. In addition, there was a significant association between family income and anxiety scores (F = 16.863, p < 0.001). Participants from families with incomes below $40,000 exhibited the highest mean anxiety score (x̄ = 11.39; SD = 3.72), whereas participants from families with incomes greater than $100,000 had the lowest mean score (x̄ = 8.08; SD = 3.18). Moreover, post hoc analysis revealed that the GAD levels were significantly higher in individuals with family income below 40,000 when compared with other income groups (p < 0.05). Participants with family income between $40,000 to 60,000, $60,001 to 80,000, and $80,001 to 100,000 showed significant differences compared to individuals with incomes above $100,000 (p < 0.001). Finally, there was no significant effect of household size on anxiety (F = 0.638, p = 0.591) (Table 2).
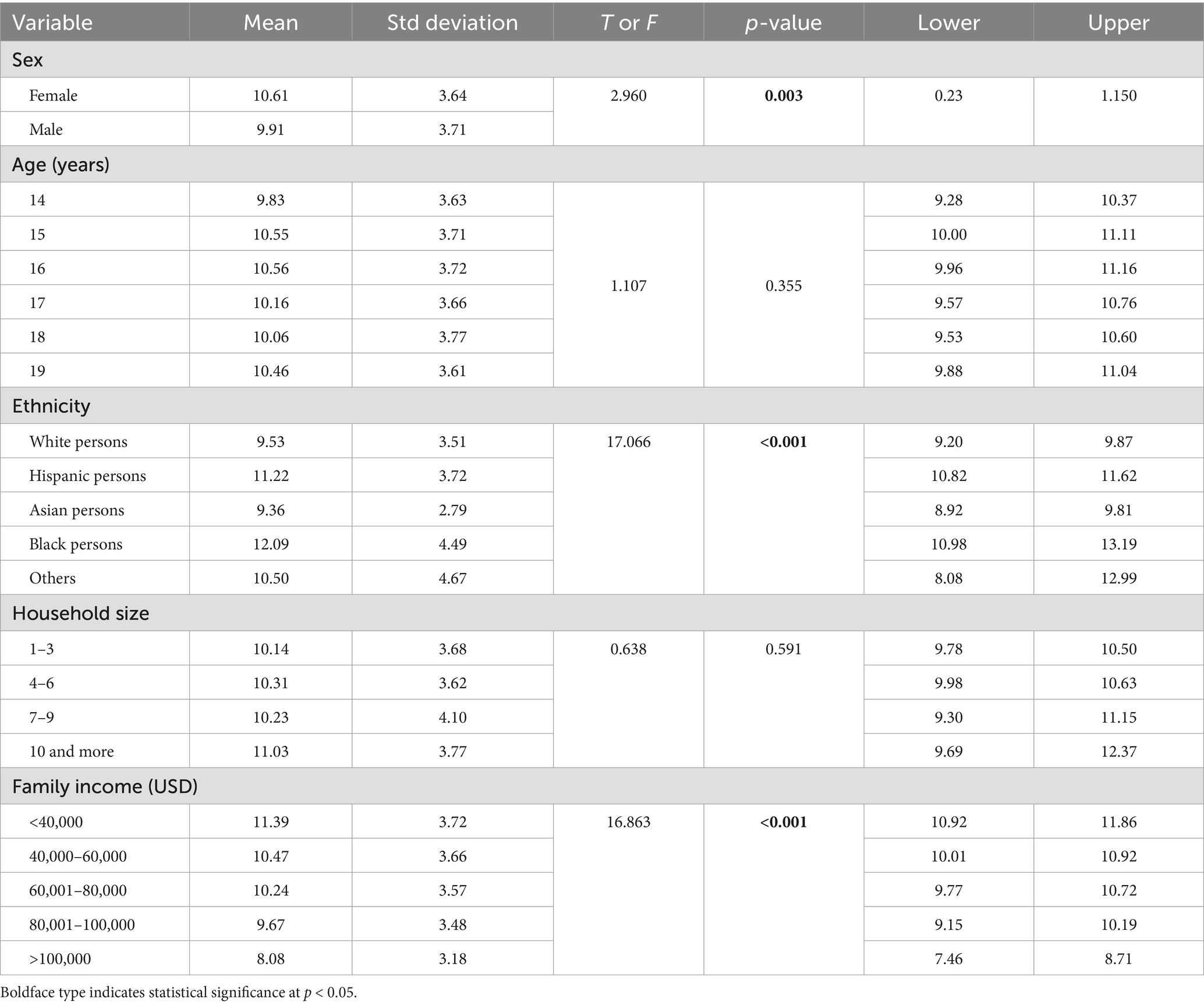
Table 2. Association between demographic factors and generalized anxiety as measured using the Generalized Anxiety Disorder-7 Scale.
The mean score for fear of COVID-19 as measured by FCV-19S was 16.26 (SD = 3.91). The median score was 17. The FCV-19S scores ranged from 7 to 33. Additionally, we observed that 91.6% (n = 907) of study participants exhibited an FCV-19S score below the cutoff score of ≥21, indicating that the majority of participants had low levels of psychological distress owing to COVID-19. Thus, 8.38% (n = 83) of study participants demonstrated considerable fear of COVID-19 (Figure 2).
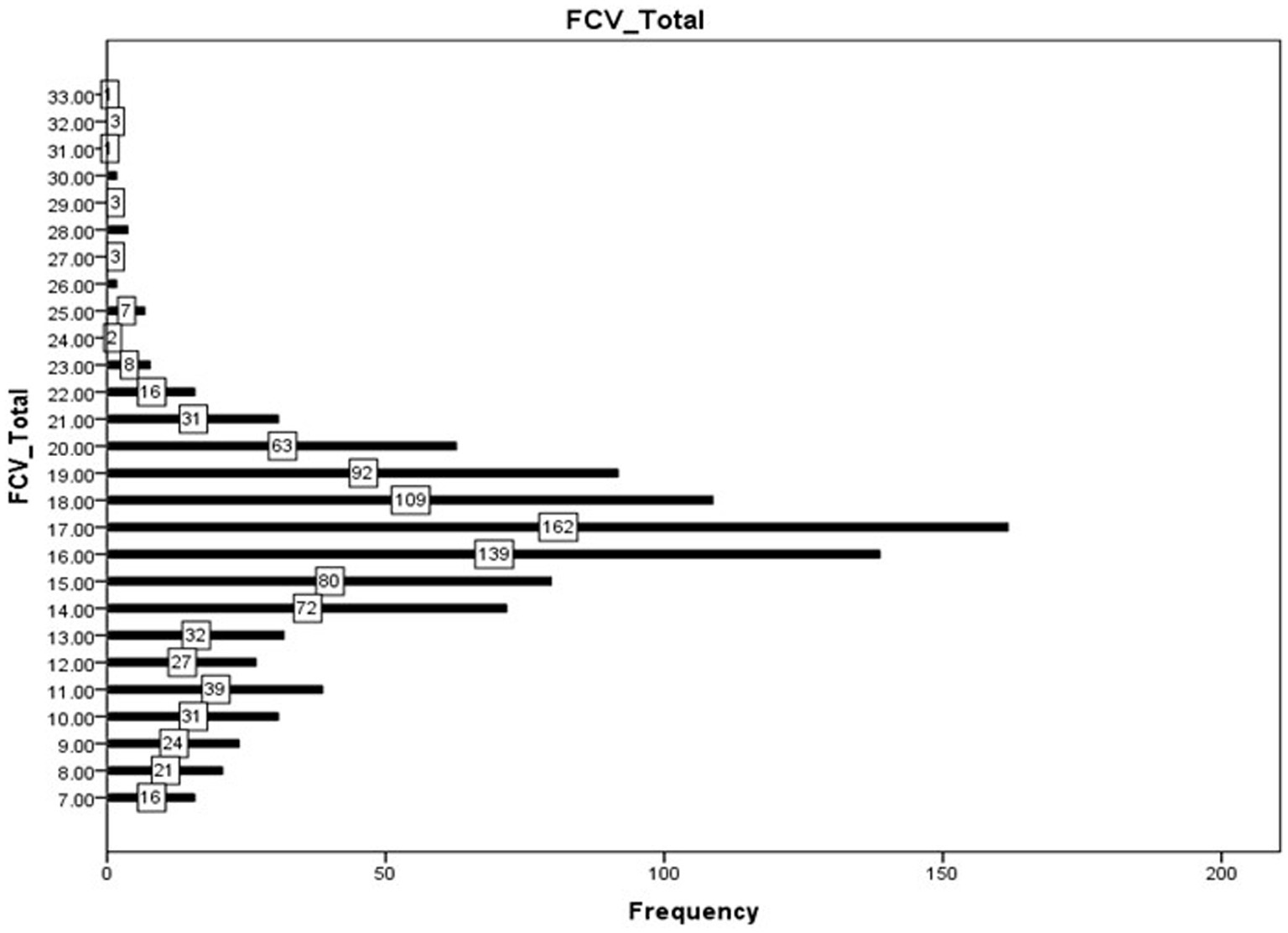
Figure 2. Frequency of FCV-19S scores as measured by the Fear of COVID-19 scale in 990 high school students from California, United States. The numbers in each bar indicate the sample size for each score.
Furthermore, we analyzed the association between demographic factors and FCV-19S scores (Table 3). Female participants exhibited significantly higher fear of COVID-19 scores (x̄ = 16.71, SD = 4.01) than male participants (x̄ = 15.81, SD = 3.75; t = 3.619, p < 0.001, CI = 0.40–1.37). Additionally, we observed significant differences in fear scores among ethnic groups (F = 6.867, p < 0.001). Black participants exhibited the highest mean fear of COVID-19 score (x̄ = 18.27, SD = 5.14), followed by Hispanic participants (x̄ = 16.59, SD = 3.39). White participants exhibited a mean score of 15.84 (SD = 4.11), Asian participants exhibited a mean of 15.89 (SD = 3.54), and participants categorized as “Other” exhibited a mean score of 15.50 (SD = 2.98). Tukey’s post hoc test revealed that there was a significant difference between the FCV-19S score between white and Hispanic participants (p < 0.001) and white and Black participants (p < 0.001). Similarly, there was a significant difference between Asian and Black participants (p < 0.001) and Hispanic and Black participants (p = 0.011). There was no statistically significant difference between the Hispanic participants and ethnicities, white participants, Asian participants and Others (p > 05). Moreover, participants in the Other category did not show any significant differences in the FCV-19S scores compared to other ethnicities.
Family income was also significantly associated with fear of COVID-19 scores (F = 7.909, p < 0.001, Table 3). Participants from families earning below $40,000 exhibited the highest mean fear score (x̄ = 17.05, SD = 3.99), whereas those from families earning above $100,000 exhibited the lowest mean score (x̄ = 14.67, SD = 3.72). Moreover, the post hoc analysis revealed that the FCV-19S scores were significantly higher in individuals with family income below $40,000 when compared to $80,000 to $100,000 and above $100,000 income groups (p < 0.01). Participants with family income between $40,000 to 60,000 and $60,000 to 80,000 showed significant differences with individuals having income above $100,000 (p < 0.01). Individuals with family income above $80,000–100,000 reported significantly lower FCV-19S scores when compared to those having a family income below $40,000 (p > 0.05). The fear of COVID-19 scores across different age groups and household sizes did not show significant differences (p > 0.05) (Table 3).
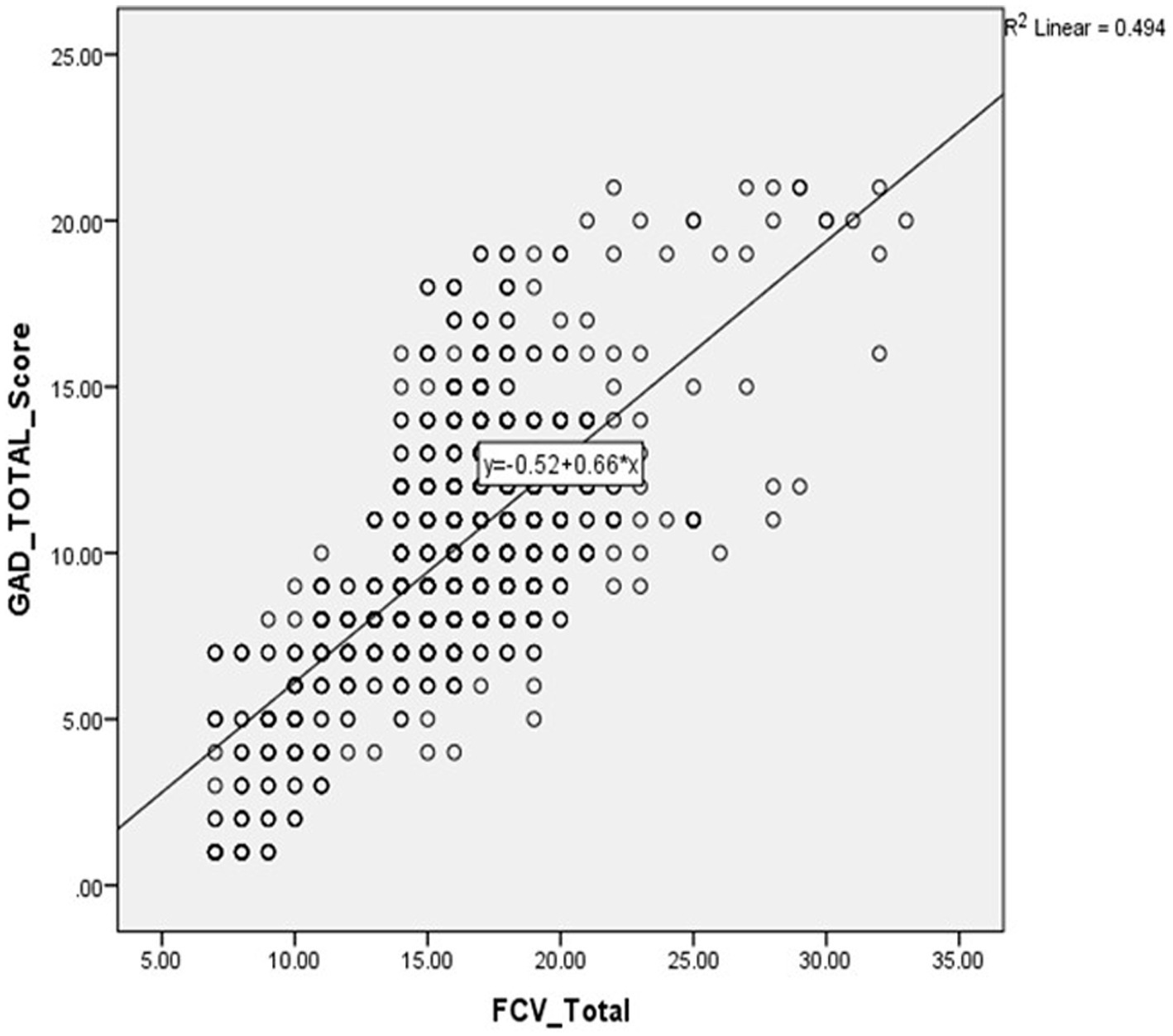
Importantly, a correlation analysis between the total FCV-19S score and the total score of the GAD-7 total revealed a significantly positive relationship between fear of COVID-19 and anxiety (r = 0.702, p < 0.001) (Figure 3).
Discussion
Few studies have examined the role of intersecting SDOH on generalized anxiety and FCV in American youth during the COVID-19 pandemic (Jost et al., 2023; Prowse et al., 2021). The present study underscores the significant role that ethnic, financial, and other demographic factors played in fear of COVID-19 and generalized anxiety among teenagers in California during the COVID-19 pandemic. According to the findings of our study, sex, Black persons, and income less than $40,000 were correlated with higher levels of generalized anxiety and fear of COVID-19.
The GAD-7 and FCV-19 are two scales indicating the mental health condition of participants, with studies demonstrating that the higher GAD-7 scores predict higher FCV-19S scores (Green et al., 2022; Perz et al., 2022). The present study demonstrates that the mental health outcomes of GAD and FCV were significantly correlated and varied significantly by ethnicity, sex, and income. A significant correlation between GAD and FCV in US populations has been previously demonstrated in the literature (Perz et al., 2022). Furthermore, in agreement with previous studies conducted during COVID-19, the present study observed differences in GAD-7 and FCV-19 scores between sexes and ethnicities, with females and minorities—particularly Hispanic and Black populations—experiencing higher levels of anxiety and fear (Dryhurst et al., 2022; Green et al., 2022; Majeed et al., 2022). The association between lower income and higher GAD and FCV levels in both the current and previous studies (Hall et al., 2022; Kikuchi et al., 2021) highlights the negative mental health impacts of this social determinant of health and potential intersectional disparities experienced by people of lower SES during COVID-19 (Hall et al., 2022; Kikuchi et al., 2021).
The global prevalence of anxiety and depression rose by more than 25% in the first year of the COVID-19 pandemic (Nochaiwong et al., 2021), disproportionately impacting young people and women (Racine et al., 2021). Similarly, our findings on the distribution of anxiety during the COVID-19 pandemic among the teenage population were consistent with previous studies on a global scale (Madigan et al., 2023; Racine et al., 2021; Sabbagh et al., 2022; Zvolensky et al., 2024). A systematic review of 82 countries found that anxiety prevalence among adolescents ranged from 7 to 12% globally (Sabbagh et al., 2022). Nearly 60% of students in the present study reported moderate to extreme anxiety, while 8.3% exhibited fear of COVID-19, possibly in part because the study period coincided with a surge of cases in California (WHO, 2022; Worldometers, 2024). In particular, girls in the present study exhibited significantly higher levels of both GAD and FCV, in agreement with similar studies on university students using the Hamilton Anxiety Rating Scale, in which female students exhibited increased anxiety compared to male students owing to their complicated thoughts and sensitivity (Amerio et al., 2022).
Approximately 42.2% of Americans identified with an ethnic group other than white (Roman, 2022). Minoritized individuals were disproportionately affected by COVID-19 morbidity and mortality and ensuing mental health outcomes such as depression and anxiety during the COVID-19 pandemic (Nguyen et al., 2022; Tai et al., 2022). Furthermore, Black individuals reported various forms of discrimination and bore the brunt of heightened social and economic disparities amid the COVID-19 pandemic (Chae et al., 2021; Cokley et al., 2022). Other studies have reported the highest rates of COVID-19 infection, disease severity, hospitalization, and mortality, leading to mental health disparities such as anxiety and stress faced by ethnic minorities, which make up approximately 40% of the population in the United States, especially Hispanic and Black populations owing to systemic disinvestment and structural inequality in education, diagnosis, treatment, prevention rates, and access to healthcare (Nguyen et al., 2022). Our findings that Black and Hispanic persons exhibited both higher levels of generalized anxiety and FCV are also in agreement with previous studies on mental health outcomes in ethnically marginalized individuals (Xu et al., 2024). A previous study found that Black individuals were 1.16 times more likely than white Americans to screen positive for depression (Dunlop et al., 2003). Similarly, among university students in Brazil, the prevalence of GAD was significantly higher among Black individuals (da Silva Júnior et al., 2022).
In the present study, Asian teenagers reported the lowest level of GAD, followed by white individuals. Some studies report that during the initial phase of the COVID-19 pandemic, reports of racially discriminatory behaviors toward Asians surged in the United States (Lee and Singh, 2022; Lee and Waters, 2021).
The present study found a significant difference between income and mental health outcomes during COVID-19. Although the COVID-19 pandemic significantly influenced the mental health of whole populations, marginalized populations, who are burdened by a vast number of daily stressors such as financial challenges and income inequality, housing instability, and access to healthcare, exhibited worse outcomes (Dubey et al., 2020). Furthermore, increased food insecurity was reported as a major cause of depression in early pandemic screening, with a high prevalence of depression, anxiety, and high levels of stress (33, 39, and 39%, respectively) among low-income adults (Wolfson et al., 2021). According to the data, during the COVID-19 pandemic, individuals with lower socioeconomic status (SES) as determined by income, have faced greater levels of anxiety and other mental health problems than those with higher SES (Silva et al., 2021).
The findings of this study have significant implications for policies and practices related to adolescent mental health. They highlight the imperative for targeted interventions designed to address disparities in access to care, particularly within underserved communities. Policymakers should prioritize funding for culturally sensitive, school-based, and family-centered interventions, as well as the expansion of telehealth services, to promote resilience and ensure equitable access to mental healthcare.
This study has several limitations. First, the convenience sampling method used may not accurately represent the entire teenage population in California. Second, relying on self-reported data introduces the possibility of bias and inaccuracies (Rosenman et al., 2011). Third, the cross-sectional design cannot definitively establish cause-and-effect relationships. Fourth, by focusing primarily on specific anxiety and fear scales, we may have overlooked other mental health concerns. Finally, the study did not collect information that could influence anxiety and fear levels, such as participants’ prior COVID-19 infection, vaccination status, or whether they had family members who contracted or died from COVID-19.
Conclusion
The findings of the present study highlight several SDOH that are associated with worse mental health outcomes in American teenagers during the COVID-19 pandemic. To address these disparities, it is important to implement targeted interventions and educational campaigns as well as promote social support systems. Mental health practitioners should prioritize early identification and intervention while also addressing socioeconomic factors and cultural influences.
Additionally, it is crucial to conduct further research on the SDOH and intersectionality among teenagers during pandemics to develop effective strategies that promote wellbeing. To better address mental health disparities, future research should focus on interventions that specifically target vulnerable populations such as ethnic minorities and lower socioeconomic groups. Implementing educational campaigns to provide accurate information about COVID-19 and initiating social support system initiatives in schools and communities could improve resilience, and ultimately mental health outcomes, in these vulnerable populations.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by A Brush on Recovery with Summit Dental High School. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
EK: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. AP: Data curation, Funding acquisition, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
Ahorsu, D. K., Lin, C.-Y., Imani, V., Saffari, M., Griffiths, M. D., and Pakpour, A. H. (2022). The fear of COVID-19 scale: development and initial validation. Int. J. Ment. Heal. Addict. 20, 1537–1545. doi: 10.1007/s11469-020-00270-8
Amerio, A., Bertuccio, P., Santi, F., Bianchi, D., Brambilla, A., Morganti, A., et al. (2022). Gender differences in COVID-19 lockdown impact on mental health of undergraduate students. Front. Psych. 12:813130. doi: 10.3389/fpsyt.2021.813130
Bonnini, S., and Borghesi, M. (2022). Relationship between mental health and socio-economic, demographic and environmental factors in the COVID-19 lockdown period—a multivariate regression analysis. Mathematics 10:3237. doi: 10.3390/math10183237
Bower, M., Smout, S., Donohoe-Bales, A., O’Dean, S., Teesson, L., Boyle, J., et al. (2023). A hidden pandemic? An umbrella review of global evidence on mental health in the time of COVID-19. Front. Psych. 14:1107560. doi: 10.3389/fpsyt.2023.1107560
Chae, D. H., Yip, T., Martz, C. D., Chung, K., Richeson, J. A., Hajat, A., et al. (2021). Vicarious racism and vigilance during the COVID-19 pandemic: mental health implications among Asian and black Americans. Public Health Rep. 136, 508–517. doi: 10.1177/00333549211018675
Chakraborty, I., and Maity, P. (2020). COVID-19 outbreak: migration, effects on society, global environment and prevention. Sci. Total Environ. 728:138882. doi: 10.1016/j.scitotenv.2020.138882
Choukou, M.-A., Sanchez-Ramirez, D. C., Pol, M., Uddin, M., Monnin, C., and Syed-Abdul, S. (2022). COVID-19 infodemic and digital health literacy in vulnerable populations: a scoping review. Digital Health 8:205520762210769. doi: 10.1177/20552076221076927
Cokley, K., Krueger, N., Cunningham, S. R., Burlew, K., Hall, S., Harris, K., et al. (2022). The COVID-19/racial injustice syndemic and mental health among black Americans: the roles of general and race-related COVID worry, cultural mistrust, and perceived discrimination. J. Community Psychol. 50, 2542–2561. doi: 10.1002/jcop.22747
da Silva Júnior, A. E., de Lima Macena, M., de Oliveira, A. D. S., Praxedes, D. R. S., de Oliveira Maranhão Pureza, I. R., and Bueno, N. B. (2022). Racial differences in generalized anxiety disorder during the COVID-19 pandemic among Brazilian university students: a national survey. J. Racial Ethn. Health Disparities 9, 1680–1688. doi: 10.1007/s40615-021-01107-3
Dryhurst, S., Schneider, C. R., Kerr, J., Freeman, A. L., Recchia, G., Van Der Bles, A. M., et al. (2022). “Risk perceptions of COVID-19 around the world” in COVID-19. Ed. J. M. Ryan. (Routledge), 162–174.
Dubey, S., Biswas, P., Ghosh, R., Chatterjee, S., Dubey, M. J., Chatterjee, S., et al. (2020). Psychosocial impact of COVID-19. Diabetes Metab. Syndr. Clin. Res. Rev. 14, 779–788. doi: 10.1016/j.dsx.2020.05.035
Dunlop, D. D., Song, J., Lyons, J. S., Manheim, L. M., and Chang, R. W. (2003). Racial/ethnic differences in rates of depression among preretirement adults. Am. J. Public Health 93, 1945–1952. doi: 10.2105/AJPH.93.11.1945
Fortuna, L. R., Brown, I. C., Woods, G. G. L., and Porche, M. V. (2023). The impact of COVID-19 on anxiety disorders in youth: coping with stress, worry, and recovering from a pandemic. Child Adolesc Psychiatr. Clin. 32, 531–542. doi: 10.1016/j.chc.2023.02.002
Green, Z. A., Noor, U., Ahmed, F., and Himayat, L. (2022). Validation of the fear of COVID-19 scale in a sample of Pakistan’s university students and future directions. Psychol. Rep. 125, 2709–2732. doi: 10.1177/00332941211016754
Hall, L. R., Sanchez, K., da Graca, B., Bennett, M. M., Powers, M., and Warren, A. M. (2022). Income differences and COVID-19: impact on daily life and mental health. Popul. Health Manag. 25, 384–391. doi: 10.1089/pop.2021.0214
Jost, G. M., Hang, S., Shaikh, U., and Hostinar, C. E. (2023). Understanding adolescent stress during the COVID-19 pandemic. Curr. Opin. Psychol. 52:101646. doi: 10.1016/j.copsyc.2023.101646
Kauhanen, L., Mohd Yunus, W. M. A. W., Lempinen, L., Peltonen, K., Gyllenberg, D., Mishina, K., et al. (2023). A systematic review of the mental health changes of children and young people before and during the COVID-19 pandemic. Eur. Child Adolesc. Psychiatry 32, 995–1013. doi: 10.1007/s00787-022-02060-0
Khan, K. S., Mamun, M. A., Griffiths, M. D., and Ullah, I. (2022). The mental health impact of the COVID-19 pandemic across different cohorts. Int. J. Ment. Heal. Addict. 20, 380–386. doi: 10.1007/s11469-020-00367-0
Kikuchi, H., Machida, M., Nakamura, I., Saito, R., Odagiri, Y., Kojima, T., et al. (2021). Development of severe psychological distress among low-income individuals during the COVID-19 pandemic: longitudinal study. BJPsych Open 7:e50. doi: 10.1192/bjo.2021.5
Kupcova, I., Danisovic, L., Klein, M., and Harsanyi, S. (2023). Effects of the COVID-19 pandemic on mental health, anxiety, and depression. BMC Psychol. 11:108. doi: 10.1186/s40359-023-01130-5
Kush, J. M., Badillo-Goicoechea, E., Musci, R. J., and Stuart, E. A. (2022). Teachers’ mental health during the COVID-19 pandemic. Educ. Res. 51, 593–597. doi: 10.3102/0013189X221134281
Lee, S. Y., Lee, J. J., and Lee, H. (2022). Socio-economic factors associated with mental health outcomes during the COVID-19 pandemic in South Korea. Front. Public Health 10:1024751. doi: 10.3389/fpubh.2022.1024751
Lee, H., and Singh, G. K. (2022). Racial and ethnic disparities in the mental health impact of the COVID-19 pandemic in the United States: analysis of 3 million Americans from the National Health Interview Survey and household pulse survey. Int. J. Trans. Med. Res. Public Health 6:417. doi: 10.21106/ijtmrph.417
Lee, S., and Waters, S. F. (2021). Asians and Asian Americans’ experiences of racial discrimination during the COVID-19 pandemic: impacts on health outcomes and the buffering role of social support. Stigma Health 6, 70–78. doi: 10.1037/sah0000275
Madigan, S., Racine, N., Vaillancourt, T., Korczak, D. J., Hewitt, J. M. A., Pador, P., et al. (2023). Changes in depression and anxiety among children and adolescents from before to during the COVID-19 pandemic: a systematic review and Meta-analysis. JAMA Pediatr. 177, 567–581. doi: 10.1001/jamapediatrics.2023.0846
Majeed, M. M., Anwar, M., Uzair, M., Bashir, M. B., Syeda, N. I., and Tanoli, N. A. (2022). Fear of COVID-19 in dentistry students: an evaluation of their knowledge and practices. Pak. J. Public Health 12, 122–126. doi: 10.32413/pjph.v12i3.865
Majeed, M. M., Salim, Z., Shaikh, A. H., Ramzan, Z., Bhatia, M. R., and Rafique, S. (2021). A comparative study to evaluate COVID-19 related anxiety and fear among medical doctors and dental surgeons. Ethiop. Med. J. 59, 91–99.
Manchia, M., Gathier, A. W., Yapici-Eser, H., Schmidt, M. V., de Quervain, D., van Amelsvoort, T., et al. (2022). The impact of the prolonged COVID-19 pandemic on stress resilience and mental health: a critical review across waves. Eur. Neuropsychopharmacol. 55, 22–83. doi: 10.1016/j.euroneuro.2021.10.864
Meherali, S., Punjani, N., Louie-Poon, S., Abdul Rahim, K., Das, J. K., Salam, R. A., et al. (2021). Mental health of children and adolescents amidst COVID-19 and past pandemics: a rapid systematic review. Int. J. Environ. Res. Public Health 18:3432. doi: 10.3390/ijerph18073432
Midorikawa, H., Tachikawa, H., Aiba, M., Shiratori, Y., Sugawara, D., Kawakami, N., et al. (2022). Proposed cut-off score for the Japanese version of the fear of coronavirus disease 2019 scale (FCV-19S): evidence from a large-scale national survey in Japan. Int. J. Environ. Res. Public Health 20:429. doi: 10.3390/ijerph20010429
Moynihan, R., Sanders, S., Michaleff, Z. A., Scott, A. M., Clark, J., Kitchener, E., et al. (2021). Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open 11:e045343. doi: 10.1136/bmjopen-2020-045343
Naseer, S., Khalid, S., Parveen, S., Abbass, K., Song, H., and Achim, M. V. (2023). COVID-19 outbreak: impact on global economy. Front. Public Health 10:1009393. doi: 10.3389/fpubh.2022.1009393
Nguyen, L. H., Anyane-Yeboa, A., Klaser, K., Merino, J., Drew, D. A., Ma, W., et al. (2022). The mental health burden of racial and ethnic minorities during the COVID-19 pandemic. PLoS One 17:e0271661. doi: 10.1371/journal.pone.0271661
Nochaiwong, S., Ruengorn, C., Thavorn, K., Hutton, B., Awiphan, R., Phosuya, C., et al. (2021). Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis. Sci. Rep. 11:10173. doi: 10.1038/s41598-021-89700-8
Panchal, U., Salazar de Pablo, G., Franco, M., Moreno, C., Parellada, M., Arango, C., et al. (2023). The impact of COVID-19 lockdown on child and adolescent mental health: systematic review. Eur. Child Adolesc. Psychiatry 32, 1151–1177. doi: 10.1007/s00787-021-01856-w
Perz, C. A., Lang, B. A., and Harrington, R. (2022). Validation of the fear of COVID-19 scale in a US college sample. Int. J. Ment. Heal. Addict. 20, 273–283. doi: 10.1007/s11469-020-00356-3
Pfefferbaum, B., and North Carol, S. (2020). Mental health and the COVID-19 pandemic. N. Engl. J. Med. 383, 510–512. doi: 10.1056/NEJMp2008017
Prowse, R., Sherratt, F., Abizaid, A., Gabrys, R. L., Hellemans, K. G., Patterson, Z. R., et al. (2021). Coping with the COVID-19 pandemic: examining gender differences in stress and mental health among university students. Front. Psych. 12:650759. doi: 10.3389/fpsyt.2021.650759
Pujolar, G., Oliver-Anglès, A., Vargas, I., and Vázquez, M.-L. (2022). Changes in access to health services during the COVID-19 pandemic: a scoping review. Int. J. Environ. Res. Public Health 19:1749. doi: 10.3390/ijerph19031749
Racine, N., McArthur, B. A., Cooke, J. E., Eirich, R., Zhu, J., and Madigan, S. (2021). Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 175, 1142–1150. doi: 10.1001/jamapediatrics.2021.2482
Robinson, L. E., Valido, A., Drescher, A., Woolweaver, A. B., Espelage, D. L., Lomurray, S., et al. (2023). Teachers, stress, and the COVID-19 pandemic: a qualitative analysis. Sch. Ment. Heal. 15, 78–89. doi: 10.1007/s12310-022-09533-2
Roman, Y. (2022). The United States 2020 census data: implications for precision medicine and the research landscape. Pers. Med. 19, 5–8. doi: 10.2217/pme-2021-0129
Rosenman, R., Tennekoon, V., and Hill, L. G. (2011). Measuring bias in self-reported data. Int. J. Behav. Healthcare Res. 2, 320–332. doi: 10.1504/IJBHR.2011.043414
Sabbagh, H. J., Abdelaziz, W., Alghamdi, W., Quritum, M., AlKhateeb, N. A., Abourdan, J., et al. (2022). Anxiety among adolescents and young adults during COVID-19 pandemic: a multi-country survey. Int. J. Environ. Res. Public Health 19:10538. doi: 10.3390/ijerph191710538
Samji, H., Wu, J., Ladak, A., Vossen, C., Stewart, E., Dove, N., et al. (2022). Mental health impacts of the COVID-19 pandemic on children and youth–a systematic review. Child Adolesc. Mental Health 27, 173–189. doi: 10.1111/camh.12501
Sawicka, B., Aslan, I., Della Corte, V., Periasamy, A., Krishnamurthy, S. K., Mohammed, A., et al. (2022). “Chapter 14 - The coronavirus global pandemic and its impacts on society” in Coronavirus drug discovery. Ed. C. Egbuna. (Elsevier), 267–311.
Siegel, R. M., and Mallow, P. J. (2021). The impact of COVID-19 on vulnerable populations and implications for children and health care policy. Clin. Pediatr. 60, 93–98. doi: 10.1177/0009922820973018
Silva, A. N. D., Guedes, C. R., Santos-Pinto, C. D. B., Miranda, E. S., Ferreira, L. M., and Vettore, M. V. (2021). Demographics, socioeconomic status, social distancing, psychosocial factors and psychological well-being among undergraduate students during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 18:7215. doi: 10.3390/ijerph18147215
Spitzer, R. L., Kroenke, K., Williams, J. B., and Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166, 1092–1097. doi: 10.1001/archinte.166.10.1092
Stogner, J., Miller, B. L., and McLean, K. (2020). Police stress, mental health, and resiliency during the COVID-19 pandemic. Am. J. Crim. Justice 45, 718–730. doi: 10.1007/s12103-020-09548-y
Tai, D. B. G., Sia, I. G., Doubeni, C. A., and Wieland, M. L. (2022). Disproportionate impact of COVID-19 on racial and ethnic minority groups in the United States: a 2021 update. J. Racial Ethn. Health Disparities 9, 2334–2339. doi: 10.1007/s40615-021-01170-w
Thomeer, M. B., Moody, M. D., and Yahirun, J. (2023). Racial and ethnic disparities in mental health and mental health care during the COVID-19 pandemic. J. Racial Ethn. Health Disparities 10, 961–976. doi: 10.1007/s40615-022-01284-9
von Elm, E., Altman, D. G., Egger, M., Pocock, S. J., Gøtzsche, P. C., Vandenbroucke, J. P., et al. (2007). The Strengthening the reporting of Observational studies in epidemiology (STROBE) statement: guidelines for reporting Observational studies. Epidemiology 335, 806–808. doi: 10.1136/bmj.39335.541782.AD
Wen, M., Shi, L., Zhang, D., Li, Y., Chen, Z., Chen, B., et al. (2023). Racial-ethnic disparities in psychological distress during the COVID-19 pandemic in the United States: the role of experienced discrimination and perceived racial bias. BMC Public Health 23:957. doi: 10.1186/s12889-023-15912-4
WHO. (2022). COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide. Available at: https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide (Accessed July 17, 2024).
WHO. (2024). WHO COVID-19 dashboard. Available at: https://data.who.int/dashboards/covid19/cases?n=c (Accessed July 17, 2024).
Wolf, K., and Schmitz, J. (2024). Scoping review: longitudinal effects of the COVID-19 pandemic on child and adolescent mental health. Eur. Child Adolesc. Psychiatry 33, 1257–1312. doi: 10.1007/s00787-023-02206-8
Wolfson, J. A., Garcia, T., and Leung, C. W. (2021). Food insecurity is associated with depression, anxiety, and stress: evidence from the early days of the COVID-19 pandemic in the United States. Health Equity 5, 64–71. doi: 10.1089/heq.2020.0059
World Health Organization. (2020). WHO director-general’s opening remarks at the mission briefing on COVID-19-12 march 2020. Geneva, Switzerland: World Health Organization. Available at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-mission-briefing-on-covid-19---12-march-2020 (Accessed December 24, 2024).
Worldometers. (2024). California coronavirus cases. Available at: https://www.worldometers.info/coronavirus/usa/california/
Xu, L., Lu, W., Smith, A. W., Wu, Q., Chan, V., and Hou, A. (2024). Gender, ethnicity differences in mental health status and COVID-19 vaccine intention among US college students during COVID-19 pandemic. J. Am. Coll. Heal. 72, 1166–1175. doi: 10.1080/07448481.2022.2070024
Zhou, S. J., Zhang, L. G., Wang, L. L., Guo, Z. C., Wang, J. Q., Chen, J. C., et al. (2020). Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 29, 749–758. doi: 10.1007/s00787-020-01541-4
Keywords: anxiety, COVID-19, race, fear, students, socioeconomic status, social determinants
Citation: Kumra E and Patange A (2025) Ethnic, socioeconomic, and demographic determinants of generalized anxiety disorder and fear of COVID-19 among teenagers in California, United States: a cross-sectional analysis. Front. Educ. 9:1496137. doi: 10.3389/feduc.2024.1496137
Edited by:
Faiza Manzoor, Zhejiang University, ChinaReviewed by:
Vincent James Hooper, SPJ GLOBAL, United Arab EmiratesSiti Kholifah, University of Brawijaya, Indonesia
Muhammad Ali Hussain, Zhejiang University, China
Copyright © 2025 Kumra and Patange. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elina Kumra, MjAyNWVwa0BnbWFpbC5jb20=
 Elina Kumra
Elina Kumra Amit Patange
Amit Patange