
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CONCEPTUAL ANALYSIS article
Front. Educ. , 14 January 2025
Sec. Higher Education
Volume 9 - 2024 | https://doi.org/10.3389/feduc.2024.1494445
Brazil faces significant challenges in the equitable distribution of health professionals across its vast territory, with remote and underdeveloped areas often lacking doctors. Initiatives like “Programa Mais Médicos” have expanded medical courses and residency programs nationwide. Recently, new Ministry of Education guidelines authorized courses and increased slots in response to judicial demands, highlighting the complexity of Brazil’s educational and health landscape. This initiative increased available slots, particularly in areas lacking healthcare professionals, and attracted private institutions to the medical sector. Despite advancements in expansion and geographical distribution, there are criticisms and challenges facing the current medical training process. Against this backdrop, this study offers a critical analysis of Brazil’s medical education, drawing from the experience of experts involved in the implementation of new medical schools in the Brazilian Northeast and Midwest regions. The study outlines the history, challenges, and outcomes of government policies, reflecting on future impacts and contributing to the debate on medical training quality and health service provision amidst the expansion and privatization of medical education in the country. We hope the lessons and insights can guide Brazil and other countries facing similar challenges, inspiring innovative and sustainable solutions to complex issues of doctor shortage and unequal distribution.
The recent expansion of undergraduate medical courses in Brazil has emerged as a pivotal strategy to mitigate inequalities in the availability of health professionals across the territory. A significant restructuring in the offering of new slots for both undergraduate and medical residency programs was propelled by the “Programa Mais Médicos” (PMM) (Brazil, 2013), a governmental initiative aimed at improving access and quality of services within the Brazilian Unified Health System (SUS), which accounts for the country’s public health system. Additionally, the Ministry of Education (MEC) established guidelines for the authorization of new medical courses and the increase in slots for existing courses, underscoring the complexity of the educational and health scenario in the country.
This initiative led to a notable increase in the availability of slots for medical courses, particularly in areas suffering from a shortage of health professionals, and fostered the entry of private higher education institutions into the market. The opening of these new slots was also accelerated by the repeal of the moratorium imposed by Ordinance No. 328/2018 (Brazil Ministry of Education, 2018), which had suspended the public calls for new medical courses for 5 years. During this suspension period, some institutions obtained judicial authorizations to begin their activities. With the repeal of this ordinance, there is an expectation of a significant increase in the number of slots, given the hundreds of processes requesting the opening of medical courses throughout the country.
Nonetheless, despite advancements in the expansion and geographical distribution of medical courses, the current medical training process (Figure 1) faces various criticisms and challenges. With the aim of addressing this issue, the present study is based on the experience of a select group of medical education experts, directly involved in the planning, implementation and management of medical schools in the Southeast, Northeast and Midwest regions of Brazil. The article provides a detailed analysis of the historical context, the challenges overcome, and the main outcomes, both positive and negative, of current government policies. Moreover, it projects reflections on the potential impacts of the current medical educational scenario in the future.
This study offers a critical and constructive analysis aimed at contributing to the debate on public policies that prioritize quality in medical training and healthcare services amid the expansion, internalization, and privatization of medical education in Brazil. The lessons learned and insights presented are intended to guide policymakers and support other countries facing similar challenges of doctor shortages and unequal distribution, inspiring innovative and sustainable solutions.
The research process involved gathering data from official government reports, legislation, and academic publications to identify key historical and contemporary trends. A systematic approach was taken to review the regulatory frameworks, such as the Law of Guidelines and Bases for National Education (“Lei de Diretrizes e Bases da Educação Nacional,” LDB) (Brazil, 1996), and the National Curriculum Guidelines (“Diretrizes Curriculares Nacionais,” DCNs) for the medical course, established by the National Council of Education (“Conselho Nacional de Educação,” CNE) (Brazil, 2014), along with international benchmarks. By comparing these legal frameworks with recent evidence-based studies, the analysis identified gaps and potential improvements in current educational policies. This approach enabled a comprehensive review of data on medical school distribution and the privatization of higher education in the health sector, supported by qualitative inputs from expert interviews and discussions.
Therefore, this study offers a critical and constructive analysis aimed at contributing to the debate on public policies that prioritize quality in medical training and healthcare services amid the expansion and privatization of medical education in Brazil. The lessons learned and insights presented are intended to guide policymakers and support other countries facing similar challenges of doctor shortages and unequal distribution, inspiring innovative and sustainable solutions.
Education constitutes one of the fundamental pillars for the social, economic, and human development of a nation. In a globalized world, where the economy and innovation advance at an accelerated pace, quality educational formation becomes a competitive differentiator for countries (Garcia, 2022). Despite the progress observed in recent decades, the Brazilian educational system still faces significant challenges, especially concerning regional inequalities in access to quality education (Albuquerque et al., 2017). These disparities have a significant impact on health promotion among the population, since, although Brazilian legislation guarantees health as a right secured by the State (Brazil Constitution of the Federative Republic of Brazil, 1988), a shortage of medical professionals persists across various regions of the country.
Therefore, the training of physicians plays a crucial role in ensuring universal access to health services, as the unequal distribution of these professionals directly impacts the quality and effectiveness of medical care provided to the population (Perim, 2020). In Brazil, although the ratio of 2.6 doctors per thousand inhabitants may seem reasonable, this average is obscured by a high concentration of professionals working in the economically more developed regions (Midwest, South, and Southeast) and in the capitals of the country, contrasting with a blatant scarcity in the neediest regions (North and Northeast), as well as in various municipalities in the interior. In concrete numbers, the ratios of doctors per thousand inhabitants in the Midwest (3.10), Southeast (3.39), and South (2.95) regions are considerably higher than in the North (1.45) and Northeast (1.93) regions (Figure 2). Similarly, the capitals present a ratio of doctors per thousand inhabitants 3.3 times greater than the average of the interior municipalities (Scheffer et al., 2023).
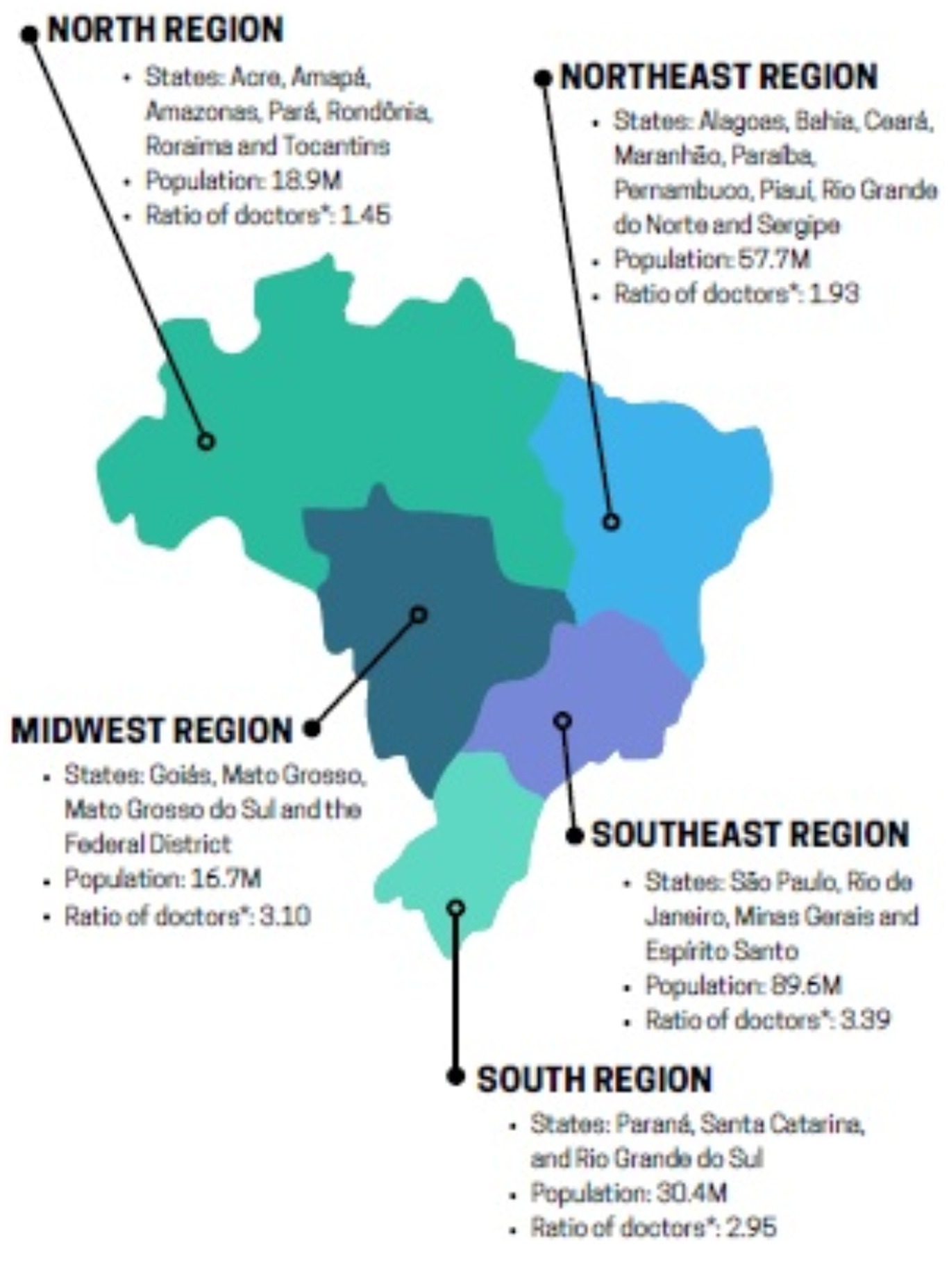
Figure 2. Ratio of doctors per Brazilian regions, in 2022. *Ration of doctors per 1,000 inhabitants.
Given the challenges mentioned above, there is a clear need to foster the strategic training and allocation of doctors in priority areas, aiming to meet the health demands of the most vulnerable communities and promote equitable access to healthcare services across the country.
To address this increasing demand, over the years, Brazilian medical education has been shaped by various legal frameworks and programs designed to expand and enhance professional medical training in Brazil. Key among these are the LDB (Brazil, 1996), enacted in 1996, and the DCNs for medical courses (Brazil, 2014). While these frameworks provide a broad foundation, they have not fully resolved issues such as the unequal distribution of doctors or the quality concerns arising from the rapid expansion of private medical schools. Our research contributes to this ongoing debate by offering insights into the strengths and weaknesses of current policies and by identifying areas where recent scientific evidence suggests a need for policy reform.
The LDB (Brazil, 1996) sets the foundation of education in Brazil and defines the principles guiding the education of health professionals, including doctors. It emphasizes the need for a generalist, humanist, and ethical training that addresses the entirety of healthcare attention and the promotion of the population’s well-being. In turn, the DCNs for medical courses (Brazil, 2014) further direct institutions in shaping their curricula, focusing on developing competencies such as critical thinking, teamwork, and responsiveness to public health needs.
Beyond these legal frameworks, the PMM (Brazil, 2013), launched in 2013, significantly impacted medical education and healthcare in Brazil. The program aimed to improve access to health services, particularly in underserved and hard-to-reach areas, by recruiting foreign doctors and prioritizing regions with doctor shortages. Despite controversies and criticisms, the PMM reduced regional inequalities and strengthened primary care.
The program also accelerated the expansion of medical schools and increased undergraduate slots, particularly in regions with fewer medical professionals. However, persistent challenges remain, including infrastructure deficits, unequal doctor distribution, and difficulties retaining professionals in economically vulnerable areas. These challenges highlight the complexity of Brazil’s healthcare and education systems and underscore the need for integrated policies that ensure both high-quality training and equitable doctor distribution, especially in underserved regions.
Furthermore, the PMM also reorganized and propelled the expansion of medical schools and the increase in the number of slots in the undergraduate medical course. These new schools and slots prioritized regions with a lower ratio of slots and doctors per inhabitant (Brazil Ministry of Education, 2024b). However, despite the undertaken efforts, challenges such as the lack of adequate infrastructure in some educational institutions, the unequal distribution of medical professionals across the national territory, and the lack of attractiveness for the retention of professionals in some economically more vulnerable regions persist. These historical challenges highlight the complexity of the educational and health system in Brazil, underscoring the importance of integrated policies that promote both the quality of medical training and the equitable distribution and retention of these professionals throughout the country, especially in areas with a shortage of healthcare services.
According to a recent publication of demography of physicians in Brazil (Scheffer et al., 2023), in 2022, the country had 389 medical schools offering 41,805 undergraduate slots, of which 23,287 (55.7%) were created after 2014, when the PMM came into effect. Further analysis of this document reveals that this period was marked by the continuation of the privatization process of medical education in Brazil. From 2013 to 2022, approximately 87% of the new medical slots were offered by private educational institutions, contrasting with the 53.4% recorded in the previous period. In absolute numbers, over two decades, the annual slots at public educational institutions increased from 5,917 to 9,725 (+64%), while at private medical schools, this number jumped from 7,001 to 32,080 (+358%).
Faced with this scenario, the rapid growth in the number of slots, the deterioration of public institutions due to poor management and budget cuts, in addition to the concurrent privatization of schools, have raised legitimate concerns regarding the quality of education. It is suggested that these factors, collectively, may contribute to a decline in the quality of training. We might consider, for instance, that the reduction of entry requirements for medical courses due to the significant expansion in the number of slots could be associated with the risk of increased dropout rates and lower qualification of students. However, to date, the actions of evaluation and monitoring of the quality of institutions carried out by the MEC and their graduates through the National Student Performance Exam (ENADE) do not clearly demonstrate this scenario.
A recent study analyzed the panorama of medical training in Brazil and sought to infer the results of institutional evaluations performed by regulatory bodies regarding the performance of the country’s undergraduate medical courses. It was shown that the majority of Brazil’s medical training courses are classified with an average Preliminary Course Concept (CPC) score, situated in the range of 3, on a scale of up to 5 (Brito et al., 2024; Santos Júnior et al., 2021). This study is in line with recent work carried out by our group that demonstrates an average of 2.7 in the ENADE score, also on a scale of up to 5, with a significant reduction of schools with low grades (grades 1 and 2; Figure 3). These data, despite not being encouraging, suggest that the quality of training has not significantly diminished with the expansion of schools in recent years. Nevertheless, it is noted that there is substantial room for improvement.
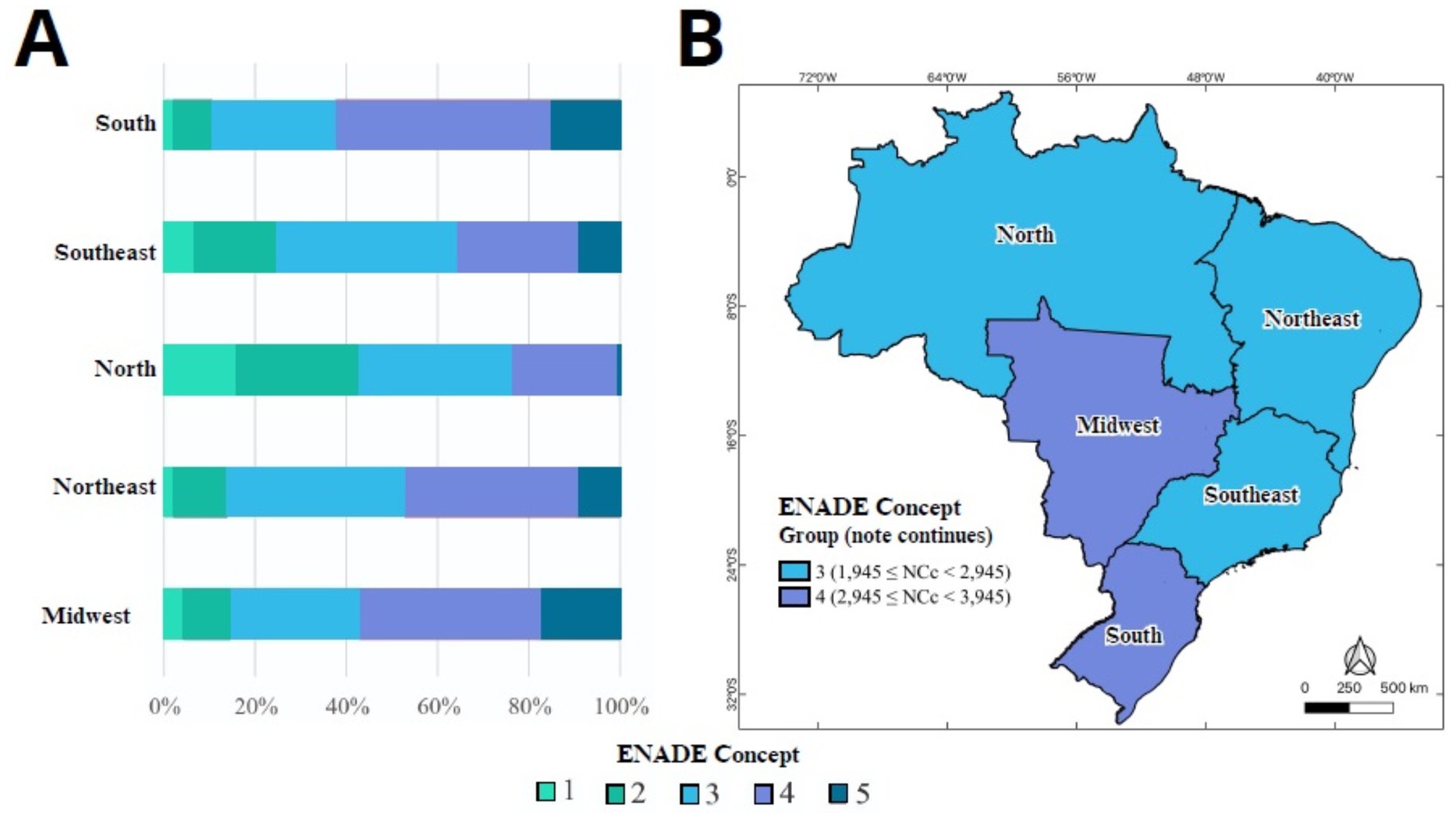
Figure 3. Regional distribution of Enade scores obtained by medical schools in Brazil. (A) Proportion of medical schools by Enade score considering all exams (2007, 2010, 2013, 2016 and 2019). (B) Map representing the majority band of each Brazilian geographic region. nNCc: the graduates’ Enade score; Enade: Brazilian Student Performance Exam.
Another notable point in the current scenario of Brazilian medical education is the expanded presence of medical schools in inland cities from the interior of Brazil. This movement was intended to address the unequal distribution of doctors across the national territory, which was concentrated in urban and more developed areas. This goal has been, at least in part, achieved. There is evidence of improved access to health services in remote areas, resulting from the implementation of policies to encourage the training and retention of newly graduated doctors in these regions. In this context, the implementation of medical residency programs in Family and Community Medicine marks a significant advance in the medical educational field. Furthermore, the integration of innovative pedagogical methodologies favors the immersion of the medical student in different social strata, especially in rural areas and urban peripheries (Separavich and Couto, 2021).
Additionally, it is noteworthy that in the last survey, the majority of undergraduate medical slots in the country were located in municipalities in the interior of the states, particularly in the southern and southeastern regions. This phenomenon, coupled with the expansion of courses and slots, thus confirms a partial success in the quest for better geographical distribution of medicine in the country (Figueiredo et al., 2019). The creation of new slots in previously underserved regions allowed more students, especially those from rural areas and with lower income, to access medical training. In this context, some legal provisions stand out, such as the obligation to provide a scholarship plan for undergraduate medical students based on socioeconomic criteria.
Corroborating this trend, it is noted that all regions showed an increase in slot density, with emphasis on the North and Northeast regions, the most underserved in the country. Despite questions about the retention of these graduates outside of the capitals and metropolitan regions due to multifactorial contexts, notably socioeconomic aspects, healthcare infrastructure, and the (lack of) professional development programs in some regions (Oliveira et al., 2015), it is estimated that more than 22,000 new professionals are trained annually in these localities. Aspects such as the mandatory payment of medical residency scholarships in family and community medicine programs and the requirement for a financial counterpart corresponding to 10% of the annual gross revenue in the local health system have been important strategies in the training and retention of medical professionals in these regions, providing an increase in the ratio of doctors and health establishments per inhabitant (Figueiredo et al., 2019).
However, despite efforts towards a more equitable geographical distribution of slots, there still exists a scenario of inequality in the distribution of doctors, with remote and vulnerable areas showing significant deficits. Some studies question whether the results obtained so far have been adequate and whether they have corresponded to what was planned with the expansion actions. For this reason, there has been a movement to pause and broadly evaluate the results obtained with the expansion policy.
Despite the potential direct and indirect benefits of the expansion of medical education in Brazil (Figueiredo et al., 2019), there is an urgent need to reflect on possible questionable consequences of this process. Understanding how to expand training sites without compromising the quality of education; how to increase the number of graduates to work in rural and underprivileged regions; and how to sustainably develop private sector education are among the main concerns among experts worldwide (Couper and Worley, 2010).
It is known that in Brazil, medical course tuition fees are notoriously high. It is estimated that an average medical course fee is about seven times higher than the minimum wage practiced in Brazil and six times higher than the average income per resident in Brazilian homes (Globo, 2024). This scenario moves, directly and indirectly, billions of dollars and, obviously, generates great interest from large business groups. Thus, the influence of private interests over the initial premises of democratizing access to health, the initial goal of the expansion of medical education in Brazil, is undeniable.
Another point for reflection lies precisely in the economic aspects related to the privatization process of medical schools. Although there are some legal provisions for offering scholarships and governmental student financing programs such as the University for All Program (PROUNI) (Brazil Ministry of Education, 2024c) and the Higher Education Student Financing Fund (FIES) (Brazil Ministry of Education, 2024a), which allow for greater diversity in the profile of medical students and contribute to a health workforce more representative of the Brazilian population, the high cost of tuition fees in private medical courses imposes a considerable financial burden. This reality clearly limits access to medical education to a portion of the economically privileged population.
The quality of clinical training stands as a cornerstone of medical education, critically shaping the competence and preparedness of future physicians to address the complex health needs of populations. This issue is particularly acute in regions such as Brazil, where the increasing number of medical students poses significant challenges to clinical training capacity. Nevertheless, meaningful clinical learning opportunities extend beyond traditional academic settings (Hays et al., 2019). Primary care facilities, smaller community hospitals, and non-acute healthcare services provide diverse and valuable training experiences, encompassing chronic disease management, comprehensive patient pathways, and community-based care. These alternative settings not only enrich clinical exposure but also cultivate interest in underserved areas, thereby contributing to workforce redistribution and addressing systemic inequities. By strategically reallocating resources, fostering intersectoral partnerships, and aligning institutional missions with educational objectives, it is possible to mitigate the risks associated with clinical capacity constraints. Moreover, through innovation and a steadfast commitment to quality, medical education can continue to produce highly competent and empathetic professionals capable of meeting the evolving needs of diverse and underserved populations. However, sustained oversight and rigorous monitoring remain essential to ensure the effectiveness and equity of these efforts.
The expansion and privatization of medical education in Brazil represent significant steps towards increasing access to health services across the national territory (Oliveira et al., 2019). However, it is imperative that such efforts are accompanied by effective policies for teaching quality and equal access to ensure adequate medical training and to meet the health needs of the Brazilian population. The lessons learned point to the need for a continued commitment to improving and adapting medical education strategies in the country, with special attention to ethics and the quality of training in contrast to unregulated economic interests.
As previously presented, the strategies for the expansion of medical courses in Brazil were partially successful (Kemper et al., 2016). Among the strengths, we highlight the increased access to medical education, the expansion of health services in inland cities from the interior of Brazil, and the diversification of the medical profile in the country. On the other hand, some weaknesses persist, such as the still present inequality in geographical distribution, questionable teaching quality, and ethical and economic issues, including the fact that a few educational groups control most of the slots in the country. This expansionist policy has raised a series of questions about the quality of professional training and has led entities such as the Federal Council of Medicine (CFM) and the Brazilian Medical Association (AMB) to position themselves against the scenario of indiscriminate expansion of medical schools in the country at the cost of such high fees and at the mercy of a disproportionate monitoring policy. In line with these criticisms, in 2018, the MEC suspended the opening of new medical courses in the country, arguing the need to curb the indiscriminate increase in medical schools without adequate quality and to discuss criteria for the authorization of slots. However, in practice, thousands of slots were created during the 5 years of moratorium through judicial actions. Currently, there are still hundreds of processes in the MEC requesting the opening of new medical courses in Brazil, in addition to schools already validated but without approval to start activities (Exam Magazine, 2023; Brazil Ministry of Education, 2023; Social Communication Advisory of the Brazilian Ministry of Education, 2023; São Paulo Medical Association, 2024).
In December 2023, the MEC published Ordinance No. 531/202324 in the Official Gazette of the Union (Brazil Ministry of Education, Secretariat for Regulation and Supervision of Higher Education, 2023). This regulation established new guidelines for processing requests for authorization of new medical courses and for increasing slots in already established courses initiated by judicial decision. The main goal of the publication was to consolidate the decision-making standard for processing requests implemented by judicial decision and to allow the inclusion of specific modifications.
Therefore, the pre-selection process adopts criteria that consider the relevance and social need of the municipalities, as well as the existence of appropriate public facilities for the development of new courses in the health care network within the scope of the SUS. As established by the Ordinance, the social need is configured by the judicialized requests that count on health regions already pre-selected in the authorization announcement for new medical courses. In addition, municipalities where the concentration of doctors per inhabitant is lower than the average of the member countries of the Organization for Economic Cooperation and Development (OECD) are also part of the pre-selection.
As defined by the recent 2023 announcement for the authorization of new medical courses in private institutions, judicialized requests can have a maximum of 60 slots. In the case of requests for increasing slots, the limit is up to 30% of those already authorized, and cannot occur in courses that have more than 240 slots. To comply with the guidelines of PMM (Brazil, 2013), institutions must present a term of adherence containing the signature of the local SUS manager, who will commit to providing the necessary structure for the operation of the course, through a financial counterpart that must correspond to 10% of the annual gross revenue pre-established for the course or increased slots. Moreover, it is established as a quality criterion of the Ordinance that the graduation achieves a Course Concept (CC) equal to or higher than 4 (on a scale of 5 possible) in the in loco evaluation.
According to information from the Ministry of Health, for the processes of opening new medical courses and increasing slots in those already existing, some specific criteria must be met, such as:
• Minimum availability of five SUS beds for the practice field per requested slot;
• Presence of multi-professional primary health care teams;
• Existence of urgent and emergency beds or emergency room;
• Commitment of SUS beds for academic use;
• Existence of a teaching hospital or hospital unit with more than 80 beds, with potential to receive teaching hospital certification in the health region, as established by current legislation.
Nevertheless, in addition to the requirements mentioned, requests for increasing slots must also be conditioned on the existence of a maximum of three Family Health students per team and the existence of at least three Medical Residency Programs implemented in priority specialties, with a total occupancy rate of the slots exceeding 50%.
The Brazilian example highlights the need for robust oversight and regulatory mechanisms to ensure the quality of medical education. Rigorous accreditation and periodic evaluations of institutions are crucial in this context. Additionally, with the market competitiveness stemming from expansion and privatization, investment in infrastructure and, most importantly, in faculty training are crucial for organic and quality growth (Quintanilha et al., 2020). This last point, perhaps, represents one of the main challenges, since, in Brazil, in general, educational activity is significantly less remunerated compared to clinical activities in the context of Medicine (Quintanilha et al., 2023).
Another important aspect in this juncture is public policies that provide equity in access to medical courses, such as student financing programs. These mechanisms are especially important to ensure diversity and inclusion in medical education. Finally, implementing leveling programs for incoming students and support for recent graduates in their transitions to underserved areas can be useful in the quality of training and retention of these professionals in needier regions (Figure 4).
Finally, considering a society that is undergoing profound transformations, in addition to the aforementioned aspects, there is an urgent need to focus on training physicians that transcend technical skills and include cultural and socio-emotional skills. In this context, it is worth highlighting the recent proposal to update the curricular guidelines prepared by the Brazilian Association of Medical Education. This document, first published in November 2024, seeks to contemplate comprehensive training, the development of skills, as well as aspects related to inclusion, equity, and diversity. In addition to contemporary issues such as the epidemiological transition, climate change, and the inclusion of technology in health practice, it highlights the concern for population groups in situations of greater vulnerability (e.g., people living in poverty, LGBTQIA+ people, people with disabilities). The discussion of these issues in the context of medical education reflects the demands of a plural society, such as Brazil.
As illustrated, Brazil is undergoing significant expansions in the realm of medical education in recent years, reflecting a global trend of change in the landscape of health professional training (O’Sullivan and Chater, 2019; Table 1). Similarly, countries like India and China have also been undergoing substantial transformations in the context of medical education, highlighting the need to assess and share experiences to address common challenges and promote advancements in the quality and accessibility of health services on an international scale.
Like Brazil, other countries face similar problems regarding the distribution of physicians and seek public policies to mitigate the negative impacts on health care in their territories (O’Sullivan and Chater, 2019). Canada, for example, deals with challenges in the provision of equitable health services in rural and remote communities. Canadian medical schools have employed strategies to increase the likelihood of physicians entering rural practice, including admissions policies, curricula focused on rural health demands, rural practice experiences, and recruitment of rural students (O’Sullivan and Chater, 2019; Grierson and Vanstone, 2021). In Brazil, the opening of residency positions in priority specialties in regions with a shortage of physicians, as well as attention to local and regional health demands, have been a constant agenda.
The scenario of expansion and privatization in the field of medical education is also observed in India, where the number of courses and slots has been growing rapidly, with a strong presence of the private sector. However, unlike Brazil, the private sector’s presence was significantly less in the economically more vulnerable provinces (Oliveira et al., 2019). This disparity underscores the importance of policies like Brazil’s PMM (Brazil, 2013), which encourages private participation in municipalities further from the large urban centers with the requirement of offering scholarships based on socioeconomic criteria and the provision of allocating 10% of gross revenue to investments in the local health network.
Another member of the BRICS, China, which has the largest medical education system in the world, presents a distinct scenario. Despite also experiencing robust growth in the number of students (annual growth rate of 7.3%) and graduates (annual growth rate of 8.2%) between 2002 and 2018, public health schools are dominant in the Asian country with significant government involvement (Hou et al., 2014). The robustness of the accreditation program for quality is an important factor in China. According to studies, in 2020, China’s Medical Education Accreditation Working Committee was recognized as an accreditation body by the World Federation for Medical Education, defining Chinese clinical medicine’s professional accreditation as equivalent to international accreditation, endorsing and globalizing its medical training strategy (Wang, 2021).
In the context of healthcare provision outside large urban centers and population representation, we can draw parallels between the Brazilian model and other countries. In Australia, for example, despite the difference in the magnitude of the process, several aspects, such as government funding, expansion of medical education, creation of rural clinical schools and changes in curricular guidelines have shaped the country’s medical landscape in recent decades (Brooks et al., 2001). There is, for example, a commitment to involving students in rural practice (Roberts et al., 2012) and increasing the number of indigenous students and knowledge of the specificities of their health and culture (Roberts et al., 2012; Biggs and Wells, 2011). Similarly, new Brazilian medical schools legally need to consider the context of life and the biological, psychological, socioeconomic elements of the Afro-Indigenous-Brazilian matrix. Furthermore, there is an effort to increase the representativeness of the Brazilian people in Medicine through scholarship programs and student financing.
It is also important to mention that the increasing globalization of healthcare has facilitated the mobility of medical professionals (Monrouxe et al., 2022). Currently, an increasing number of Brazilian medical students and physicians desire or seek career opportunities abroad. This trend reflects the broader dynamics of global medicine, where advanced clinical and research training, better working conditions, and financial incentives attract professionals to countries with better healthcare infrastructure. In Brazil, despite the mentioned advances, systemic issues such as limited resources, inadequate infrastructure, and low financial compensation still challenge the retention of physicians in some areas of the country. As a result, international destinations are gaining popularity among Brazilian physicians, highlighting the intersection of global professional aspirations and local structural challenges (Garcia-Rosa et al., 2024). This phenomenon underscores the need for robust policies that not only address the root causes of physician emigration but also increase the attractiveness of local medical careers in a globally competitive context.
These data demonstrate that, despite cultural, political, and socioeconomic differences, many countries, given the need for healthcare assistance for their citizens, undergo or will undergo a process of reformulation and expansion of medical education. In this regard, benchmarking this process by observing successful practices internationally is recommended, and thus identifying and presenting historical and legal aspects, challenges, and potentialities of the Brazilian model are relevant for the enhancement of medical training at a global level.
Given the complexity of the educational and health scenario in Brazil, it is clear that the expansion, internalization, and privatization of medical education represent significant advances, but also considerable challenges. Increasing access to medical training is crucial to meet the health needs of the population, especially in underserved regions, yet the quality of education and equity in access must be non-negotiable priorities. In this context, a continuous commitment to effective policies that promote educational excellence, equitable distribution of health professionals, and ensure that economic interests do not override the ethical and humanitarian principles of medical practice is indispensable.
Furthermore, the conclusions highlight the need for robust strategies to address the persistent inequalities in the geographical distribution of doctors and the quality of medical education. These strategies must focus on balancing the rapid expansion of medical schools with mechanisms that ensure academic rigor, infrastructure development, and the retention of qualified professionals in rural and underserved areas. In addition, comprehensive training programs should emphasize the development of skills that meet the demands of contemporary healthcare, including fostering inclusion, equity, and diversity within the medical profession.
The findings also suggest future lines of research, particularly in assessing the long-term impact of privatization on educational outcomes and healthcare access. Further studies should investigate how these trends affect the professional profiles of medical graduates and the dynamics of labor markets, as well as the broader implications for public health and social equity. By addressing these critical dimensions, future research can contribute to refining policies that will better align educational objectives with the healthcare needs of the Brazilian population.
KA: Conceptualization, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. LQ: Conceptualization, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. RL: Conceptualization, Formal Analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. BA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Intramural Research Program of the Oswaldo Cruz Foundation (Fiocruz). BA is a senior scientist from the Brazilian National Council for Scientific and Technological Development (CNPq 1D). KA is a postdoctoral researcher at Gonçalo Moniz Institute, Oswaldo Cruz Foundation. The funding source played no role in the study design; the data.
The authors thank Elze Leite for administrative support and Quécia Brito for her support in the development of Figure 3.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Albuquerque, M. V., Viana, A. L. A., Lima, L. D., Ferreira, M. P., Fusaro, E. R., and Iozzi, F. L. (2017). Regional health inequalities: changes observed in Brazil from 2000-2016. Ciênc. Saúde Colet. 22, 1055–1064. doi: 10.1590/1413-81232017224.26862016
Biggs, J. S. G., and Wells, R. W. (2011). The social mission of Australian medical schools in a time of expansion. Aust. Health Rev. 35:424. doi: 10.1071/AH10970
Brazil. (1996). Law no. 9, 394 of December 20, 1996: Establishes the guidelines and bases for national education. Official diary of the union. Brasília, DF: Presidency of the republic of Brazil. 9 p.
Brazil. (2013). Law no. 12,871, of October 22, 2013: Establishes the “Programa Mais Médicos”, amends Laws no. 8,745, of December 9, 1993, and no. 6, 932, of July 7, 1981, and provides other measures. Official diary of the union. Brasília, DF: Presidency of the republic of Brazil
Brazil, (2014). National curriculum guidelines for the undergraduate medicine course. Brasília, DF: National Education Council, 5 p.
Brazil Constitution of the Federative Republic of Brazil, (1988). Official diary of the union. Brasília, DF: Presidency of the Republic of Brazil, 496 p.
Brazil Ministry of Education. (2018) Provides for the suspension of the protocol for requests to increase vacancies and new public notices for authorization of undergraduate courses in Medicine and establishes the Working Group to analyze and propose the reo. Available at: https://www.in.gov.br/materia/-/asset_publisher/Kujrw0TZC2Mb/content/id/9362390/do1-2018-04-06-portaria-n-328-de-5-de-abril-de-2018-9362386 (Accessed March 18, 2024).
Brazil Ministry of Education. (2023). Ministry of Education publishes new rules for medical courses under judicialization [internet]. Available from: https://www.gov.br/mec/pt-br/assuntos/noticias/2023/dezembro/mec-divulga-novas-regras-para-cursos-de-medicina-em-judicializacao (Accessed March 18, 2024).
Brazil Ministry of Education. (2024a). Higher education student financing fund (FIES) [internet]. Available at: https://acessounico.mec.gov.br/fies (Accessed March 27, 2024).
Brazil Ministry of Education. (2024b). “Programa Mais Médicos”. Available at: http://portal.mec.gov.br/secretaria-de-regulacao-e-supervisao-da-educacao-superior-seres/30000-uncategorised/59441-programa-mais-medicos (Accessed March 15, 2024).
Brazil Ministry of Education. (2024c). University for all Program (PROUNI) [internet]. Available at: https://acessounico.mec.gov.br/prouni (Accessed March 27, 2024).
Brazil Ministry of Education, Secretariat for Regulation and Supervision of Higher Education. (2023). Ordinance no. 531, December 20, 2023: provides for the decision-making standard for processing requests for authorization of new medicine courses and for increasing places in existing medicine courses, established by virtue of a court decision, under t. Brasília, DF
Brito, Q. H. F., Silva, F. G. M., Menezes, R. C., Avena, K. M., Andrade, B. B., and Quintanilha, L. F. (2024). Shaping Tomorrow’s doctors: the impact of socioeconomic and institutional factors on medical education quality in Brazil. Res Sq. [preprint]. doi: 10.21203/rs.3.rs-5478550/v1
Brooks, P. M., Doherty, R. L., and Donald, K. J. (2001). Expansion and diversification of medical education in Australia 1951-2000. Med. J. Aust. 174, 25–28. doi: 10.5694/j.1326-5377.2001.tb143141.x
Couper, I. D., and Worley, P. S. (2010). Meeting the challenges of training more medical students: Lessons from Flinders University’s distributed medical education program. Med. J. Aust. 193, 34–36. doi: 10.5694/j.1326-5377.2010.tb03738.x
Exam Magazine. (2023). Veto on new medicine courses in the country comes to an end; there are 225 lawsuits in court to open vacancies [internet]. Available at https://exame.com/brasil/chega-ao-fim-veto-a-novos-cursos-de-medicina-no-pais-ha-225-acoes-na-justica-para-abertura-de-vagas/ (Accessed March 18, 2024).
Figueiredo, A. M., McKinley, D. W., Lima, K. C., and Azevedo, G. D. (2019). Medical school expansion policies: educational access and physician distribution. Med. Educ. 53, 1121–1131. doi: 10.1111/medu.13941
Garcia, J. C. (2022). “Analysis of medical education in Latin America” in Medical education in Latin America Eds. Mendes AB, Oliveira CD, (Salvador, BA: EDUFBA), 59–70.
Garcia-Rosa, B. S., Urmenyi, L. G., Santana, G. C., Marques, J. V. M., Miguez-Pinto, J. P., Ramalho, C., et al. (2024). Understanding the USMLE journey of Brazilian medical students and graduates: a narrative review. Front. Med. 11, 1–5. doi: 10.3389/fmed.2024.1484772
Globo, (2024) Brazilian Institute of Geography and Statistics publishes the average income of Brazilian families [internet]. Available at: https://g1.globo.com/jornal-nacional/noticia/2024/02/28/ibge-divulga-a-renda-dos-brasileiros-e-afirma-que-ainda-ha-muita-desigualdade-entre-os-estados.ghtml (Accessed March, 15, 2024)
Grierson, L., and Vanstone, M. (2021). The allocation of medical school spaces in Canada by province and territory: the need for evidence-based health workforce policy attribution des places dans les facultés de médecine au Canada selon la province ou le territoire: pour Une politique de la. Healthc Policy 16, 106–118. doi: 10.12927/hcpol.2021.26429
Hays, R. B., McKinley, R. K., and Sen Gupta, T. K. (2019). Twelve tips for expanding undergraduate clinical teaching capacity. Med. Teach. 41, 271–274. doi: 10.1080/0142159X.2018.1429587
Hou, J., Michaud, C., Li, Z., Dong, Z., Sun, B., Zhang, J., et al. (2014). Transformation of the education of health professionals in China: progress and challenges. Lancet 384, 819–827. doi: 10.1016/S0140-6736(14)61307-6
Kemper, E. S., Mendonça, A. V. M., and Sousa, M. F. (2016). The “Mais Médicos” (more doctors) program: panorama of the scientific output. Ciênc. Saúde Colet. 21, 2785–2796. doi: 10.1590/1413-81232015219.17842016
Monrouxe, L. V., Chandratilake, M., Chen, J., Chhabra, S., Zheng, L., Costa, P. S., et al. (2022). Medical students’ and trainees’ country-by-gender profiles: Hofstede’s cultural dimensions across sixteen diverse countries. Front. Med. 8, 1–13. doi: 10.3389/fmed.2021.746288
O’Sullivan, B. G., and Chater, B. (2019). Medical school expansion to areas of need improves physician distribution. Med. Educ. 53, 1072–1073. doi: 10.1111/medu.13957
Oliveira, B. L. C. A., Lima, S. F., Pereira, M. U. L., and Pereira Júnior, G. A. (2019). Evolution, distribution and expansion of medicine courses in Brazil (1808-2018). Trab Educ Saúde. 17:e0018317.
Oliveira, J. G. S., Paula, G. O., and Araujo, T. S. (2015). The training, work and retention of medical graduates in the Western Amazon. Rev Int Humanidades Médicas. 4, 101–114. doi: 10.1590/1981-7746-sol00183
Perim, G. L. (2020). “Medical education in Brazil” in Assessment of higher education: An experience in medical education. Eds. Oliveira AE, Santos LM, (Londrina, PR: iNESCO), 61–76.
Quintanilha, L. F., Farias, C. S. S., and Andrade, B. B. (2020). Training and pedagogical involvement among higher education professors in health: an analysis of medical courses. Rev Int Educ Super. 7:e021026.
Quintanilha, L. F., Pereira, M. A., Andrade, B. B., and Portilho, E. M. L. (2023). Teacher training and engagement in Brazilian health higher education: fragilities and strengths. Rev Bras Estud Pedagógicos 14:e5293. doi: 10.24109/2176-6681.rbep.104.5293
Roberts, C., Daly, M., Kumar, K., Perkins, D., Richards, D., and Garne, D. (2012). A longitudinal integrated placement and medical students’ intentions to practise rurally. Med. Educ. 46, 179–191. doi: 10.1111/j.1365-2923.2011.04102.x
Santos Júnior, C. J., Misael, J. R., Trindade Filho, E. M., Wyszomirska, R. M. A. F., Santos, A. A., and Costa, P. J. M. S. (2021). Expansion of vacancies and quality of medical courses in Brazil: “where do we stand?”. Rev. Bras. Educ. Med. 45:e058. doi: 10.1590/1981-5271v45.2-20200523
São Paulo Medical Association. (2024). New rules for medicine courses in Judicialization are released by the Brazilian Ministry of Education
Scheffer, M., Guilloux, A. G. A., Miotto, B. A., Almeida, C. J., Guerra, A., Cassenote, A., et al. (2023). Medical demography in Brazil 2023. São Paulo, SP: FMUSP, AMB, 344 p.
Separavich, M. A., and Couto, M. T. (2021). More doctors program: a critical review of the implementation from the perspective of access and the universalization of health care. Ciênc. Saúde Colet. 26, 3435–3446. doi: 10.1590/1413-81232021269.2.04572020
Social Communication Advisory of the Brazilian Ministry of Education. (2023). Brazilian Ministry of Education publishes new rules for medical courses under judicialization [internet]. Available at: https://www.gov.br/mec/pt-br/assuntos/noticias/2023/dezembro/mec-divulga-novas-regras-para-cursos-de-medicina-em-judicializacao (Accessed March 15, 2024).
Keywords: medical education, medical schools, undergraduate medical education, privatization and access to higher education, Brazil, more physicians program
Citation: Avena KM, Quintanilha LF, Luzardo Filho RL and Andrade BB (2025) Lessons learned from the expansion of medical schools in Brazil: a review of challenges and opportunities. Front. Educ. 9:1494445. doi: 10.3389/feduc.2024.1494445
Received: 10 September 2024; Accepted: 20 December 2024;
Published: 14 January 2025.
Edited by:
Freddy Marín-González, Costa University Corporation, ColombiaReviewed by:
Raul Aragão Martins, São Paulo State University, BrazilCopyright © 2025 Avena, Quintanilha, Luzardo Filho and Andrade. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bruno B. Andrade, YnJ1bm8uYW5kcmFkZUBmaW9jcnV6LmJy
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.