- Department of Anesthesiology, Faculty of Medicine, Prince of Songkla University, Hat-Yai, Thailand
Introduction: The impact of medical student involvement in anesthetic procedures on operating room (OR) efficiency and patient outcomes remains understudied, despite its importance in medical education. This study aimed to quantify the effects of fifth-year medical students’ participation in anesthetic procedures on key time metrics, perceived difficulty, procedural success, and postoperative complications and to compare these effects with those of anesthetic residents and student nurse anesthetists.
Methods: This prospective observational study was conducted between April and July 2022 in the OR of a tertiary university hospital in southern Thailand. We analyzed 111 elective obstetric-gynecologic and general surgery procedures under subarachnoid block or general anesthesia, equally distributed among three groups: fifth-year medical students, anesthetic residents, and student nurse anesthetists. Key time intervals, perceived difficulty, number of attempts, success rates, and postoperative complications were recorded and compared across groups.
Results: Fifth-year medical students exhibited significantly prolonged anesthesia release time, anesthesia-controlled time, anesthetic preparation time, and anesthetic procedure time compared to anesthetic residents and student nurse anesthetists (p < 0.05). Medical students perceived case inductions as more challenging than the other groups did (p < 0.001), but procedural success rates were comparable across groups. Immediate postoperative airway complications were more frequent among medical students than anesthetic residents, but no significant differences were found in intraoperative or 24-h postoperative complications.
Discussion: While the involvement of medical students in anesthetic procedures extends specific time metrics, it does not significantly impact overall case duration or major patient outcomes. These findings support the continued integration of medical student training in the OR, with appropriate supervision to manage the slightly increased risk of immediate postoperative complications. Further research is needed to optimize the balance between educational opportunities and OR efficiency.
Clinical trial registration: https://www.thaiclinicaltrials.org/show/TCTR20220418006, identifier TCTR20220418006.
1 Introduction
Anesthesia is among the specialties included in the undergraduate medical curriculum, providing students with exposure to preoperative evaluation, intraoperative attendance, anesthetic procedures, and postoperative care during anesthesia rotation. Clinical attachment and simulations in the operating room (OR) play vital roles in the educational process. However, the OR is not only a learning environment but also a critical component of healthcare delivery systems, in which efficiency is paramount (Overdyk et al., 1998).
Fifth-year medical students typically have limited exposure to anesthetic procedures, typically during short rotations lasting one week. This brief period challenges acquiring the necessary procedural skills and confidence compared to anesthetic residents who undergo more immersive training. Balancing education with OR efficiency becomes even more important when considering the varying levels of experience among trainees.
Efforts to improve OR efficiency often raise questions regarding their impact on medical education. Concerns arise regarding the balance between providing adequate training for future clinicians and optimizing OR workflow to increase productivity and reduce costs (Udelsman, 2003). Experience in the OR influences students’ interest in pursuing careers in anesthesiology (Rukewe et al., 2017; Emmanouil et al., 2017), and the lessons learned during clinical rotations can influence patient care and surgical case timing (Udelsman, 2003).
While several previous studies have examined the impact of anesthetic residents on surgical case timing (Browne et al., 2011; Davis et al., 2006; Lynch et al., 2024; Hoffman et al., 2019), there is a knowledge gap in understanding the contribution of fifth-year medical students to OR efficiency. This study seeks to provide insights into the impact of fifth-year medical student training on key time metrics, OR efficiency, and patient outcomes, contributing to the ongoing dialogue about optimizing medical education in the perioperative setting.
2 Materials and methods
2.1 Study design
This prospective observational study was conducted to assess the impact of anesthesia clerkship training on surgical procedure time (SPT) between April and July 2022 in the operating theatre of Prince of Songkla University, a tertiary university hospital in Songkhla, southern Thailand. This study was approved by the Institutional Human Research Ethics Committee of the Faculty of Medicine, Prince of Songkla University (REC.65-156-8-1).
2.2 Outcomes
1. Primary outcomes were quantified to compare the impact of fifth-year medical students’ involvement in anesthetic procedures on key time metrics, including anesthesia release time (ART), anesthesia-controlled time (ACT), anesthetic preparation time (APpT), and anesthetic procedure time (APT), relative to procedures involving anesthetic residents and student nurse anesthetists.
2. Secondary outcomes were: (a) to assess the effect of medical student involvement on overall surgical case timing, specifically focusing on total case time (TCT) and surgical time (ST); (b) to evaluate and compare the perceived difficulty of case induction among fifth-year medical students, anesthetic residents, and student nurse anesthetists; (c) to analyze the number of attempts and success rates of anesthetic procedures across the three groups of trainees; and (d) to compare the incidence of immediate postoperative complications, with a focus on airway-related issues, among procedures performed by the three groups.
2.3 Participants
The participants in this study were categorized into three groups: (1) 5th-year medical students, (2) anesthetic residents, and (3) student nurse anesthetists. Time measurements were recorded for each group.
The participants were assigned to care for patients with an American Society of Anesthesiologists (ASA) physical status of I–II, who were scheduled for elective obstetric-gynecologic or general surgery under subarachnoid block (SAB) or general anesthesia (GA). However, participants assigned to care for patients with ASA class > II or those involved in emergency procedures were excluded from the study.
2.4 Study setting
The study was conducted in the ORs at Prince of Songkla University. The hospital features multiple standardized ORs equipped for a wide range of surgical procedures. Each participant managed patients admitted to the OR, where they were prepared for surgery by an assigned anesthesia team consisting of 5th-year medical students, anesthetic residents, or student nurse anesthetists.
Fifth-year medical students had limited exposure to anesthesia, with rotations lasting 1 week, whereas anesthetic residents and student nurse anesthetists had ongoing, immersive training in anesthesia.
All teaching faculty were board-certified anesthesiologists with a minimum of 1 year of clinical and teaching experience. While the level of commitment to teaching varied, all instructors were required to provide consistent, hands-on guidance during procedures to ensure that all trainee groups received high-quality education. Teaching methods before the start of each case were standardized across all trainee groups using a predefined curriculum covering intubation and spinal block techniques, ensuring that all trainees received equal instruction time and exposure to key procedural tasks.
Anesthetic techniques were standardized across all procedures, following a consistent protocol. All procedures were supervised by experienced anesthesiologists to ensure adherence to these standardized techniques.
2.5 Data collection
The study was conducted by M.S., S.C., T.K., and trained observer nurse anesthetists in each OR who observed and recorded the data on standardized forms. Eligible participants were carefully screened, and baseline data of patients under their care were collected. Specific time points during the perioperative period were meticulously recorded. Time measurements were recorded at the nearest 20-s interval using synchronized theatre clocks. To minimize bias, the OR staff were not informed of the nature of the project and were instructed to perform all duties as usual.
2.6 Time definition
Time definitions were based on the Association of Anesthesia Clinical Directors Procedural Times Glossary (Donham, 1998).
TCT refers to the period from patient entry into the anesthetic room to departure from the OR.
1. ART refers to the time at which a sufficient level of anesthesia is established, allowing for surgical preparation to begin. ART was used as a marker for the completion of this phase (e.g., endotracheal intubation and placement of the pulmonary artery catheter).
2. ACT refers to the period from when the patient enters the anesthetic room until they are ready for surgical skin preparation, in addition to the time from surgical dressing application to the time of departure from the OR and includes all time intervals during which the anesthetic team can affect the workflow.
3. APpT refers to the time from patient entry into the OR to the start of the anesthetic procedure.
4. APT refers to the period from the start of the anesthetic procedure to its completion (e.g., GA: time starts from pre-oxygenation until the endotracheal tube position is confirmed; SAB: time starts from when local anesthesia is injected into the patient’s skin until an adequate level of anesthesia is reached).
5. ST begins when the patient is ready for skin preparation and continues until the dressing is applied at the end of surgery.
6. SPT refers to the time from the end of ART to skin incision or the occurrence of a painful stimulus.
7. Therefore, ACT + ST = TCT. Clear identifiable events were selected to designate the time points to minimize the variation between observers. Time points were documented on a data collection form. Additionally, the component task times were recorded.
2.7 Statistical analysis
The sample-sized calculation was based on a previous study; the ACT was 37.1 ± 8.8 min for the group with medical students, compared to 31.9 ± 5.4 min for the group without medical students (Browne et al., 2011). The statistical power was 80% with a significance level (alpha) of 0.05. This calculation ensures that the study has sufficient power to detect a clinically significant difference between groups while controlling for the likelihood of Type-I errors. Assuming that 10% of the study participants would withdraw from the study, 37 patients per group were required.
Analyses were performed using R software, version 4.1.0. Continuous variables were expressed as median and interquartile range (IQR) because the data were not normally distributed. The Shapiro–Wilk test was used to assess the distribution along the Gaussian curve, and the skewed distribution justified the use of median and IQR instead of mean and standard deviation. Differences between groups were analyzed using the Kruskal-Wallis test for non-parametric data, followed by pairwise comparisons using the Wilcoxon rank-sum test with Holm correction. For categorical data, the Chi-square test or Fisher’s exact test was applied as appropriate. A p-value <0.05 was considered statistically significant.
3 Results
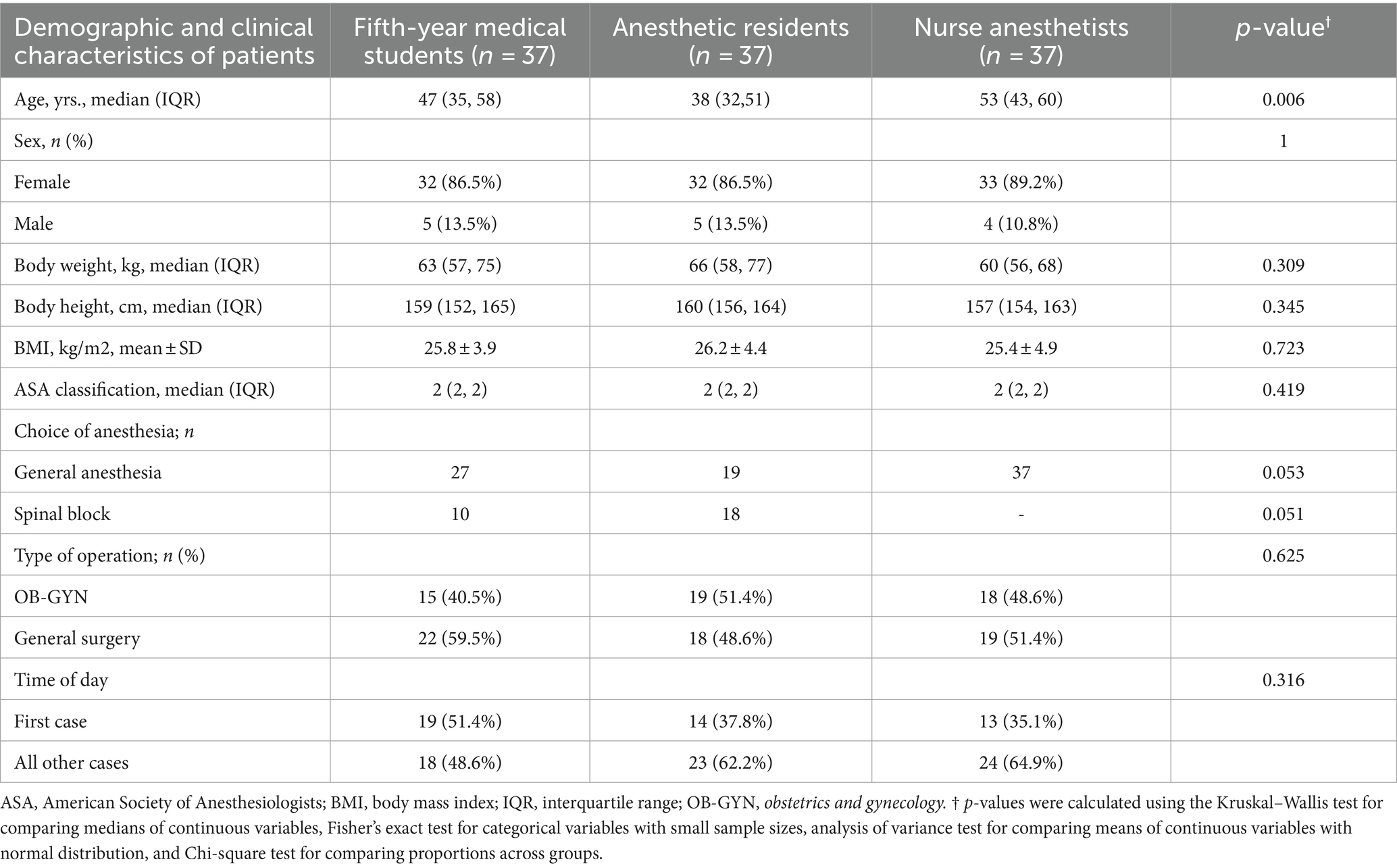
Complete datasets were collected from 111 eligible patients undergoing obstetric-gynecologic and general surgery procedures. These patients were evenly distributed among three groups of anesthesia providers: (1) fifth-year medical students, (2) anesthetic residents, and (3) student nurse anesthetists. Each group was responsible for taking care of 37 patients, ensuring an equal distribution across the study. Table 1 presents the groups’ baseline characteristics.
3.1 Key time intervals
Fifth-year medical students exhibited prolonged times across multiple measured intervals, including ART, ACT, APpT, and APT, compared to anesthetic residents and student nurse anesthetists. These differences were statistically significant, indicating that the involvement of fifth-year medical students was associated with extended anesthetic management times (Tables 2, 3).
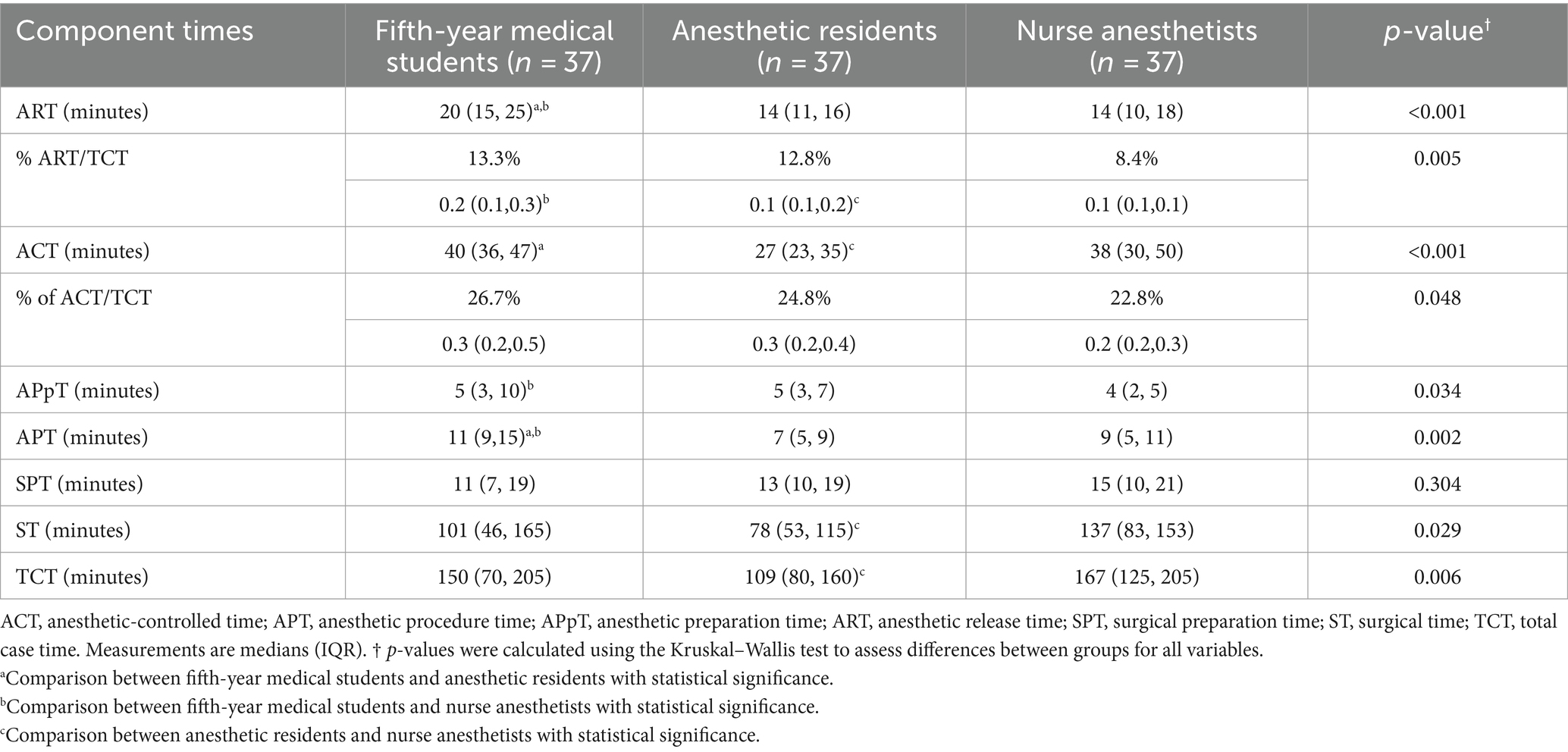
Table 2. Component times and their proportions of total case time among medical students, residents, and nurse anesthetists.
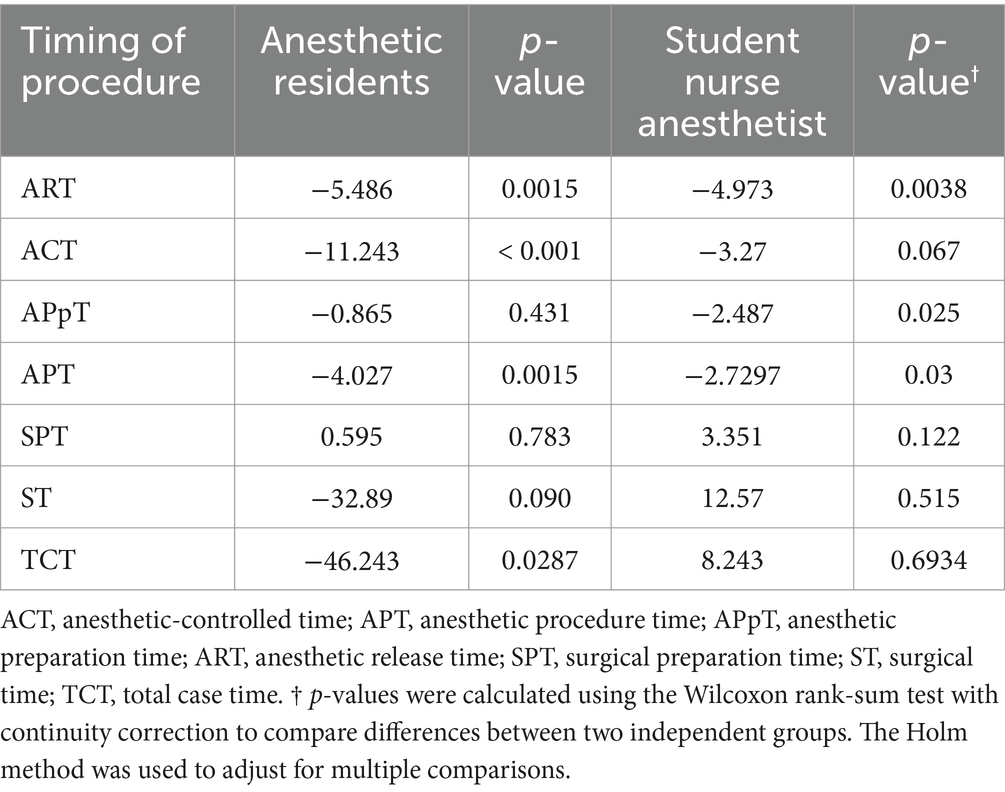
Table 3. Linear regression analysis of procedure timing differences compared to fifth-year medical students.
3.2 ART
Fifth-year medical students had significantly prolonged ART compared with both anesthetic residents and student nurse anesthetists.
3.3 ACT
A significant increase in ACT was observed for fifth-year medical students compared to anesthetic residents, while no significant difference was found compared to student nurse anesthetists.
3.4 APT and APpT
Similar trends were noted, with fifth-year medical students showing significantly longer APT and APpT than the other groups, highlighting the impact of medical student involvement on these specific time intervals.
3.5 ART/TCT and ACT/TCT
Fifth-year medical students had higher ART/TCT ratios than student nurse anesthetists, with no significant difference observed when compared to anesthetic residents. ACT/TCT ratios were slightly elevated in the medical student group but did not differ significantly across the groups.
3.6 ST and TCT
No significant differences were observed in ST and TCT between fifth-year medical students and the other groups, although student nurse anesthetists had extended ST and TCT compared to anesthetic residents, suggesting a variability in surgical timing based on the type of trainee (Table 2).
3.7 Difficulty of case induction and success rates
Fifth-year medical students rated case induction as significantly more difficult than the other groups, reflecting their relative lack of experience. However, the number of attempts and success rates of procedures did not differ significantly across the groups, indicating that while perceived difficulty was higher, performance was comparable (Table 4).
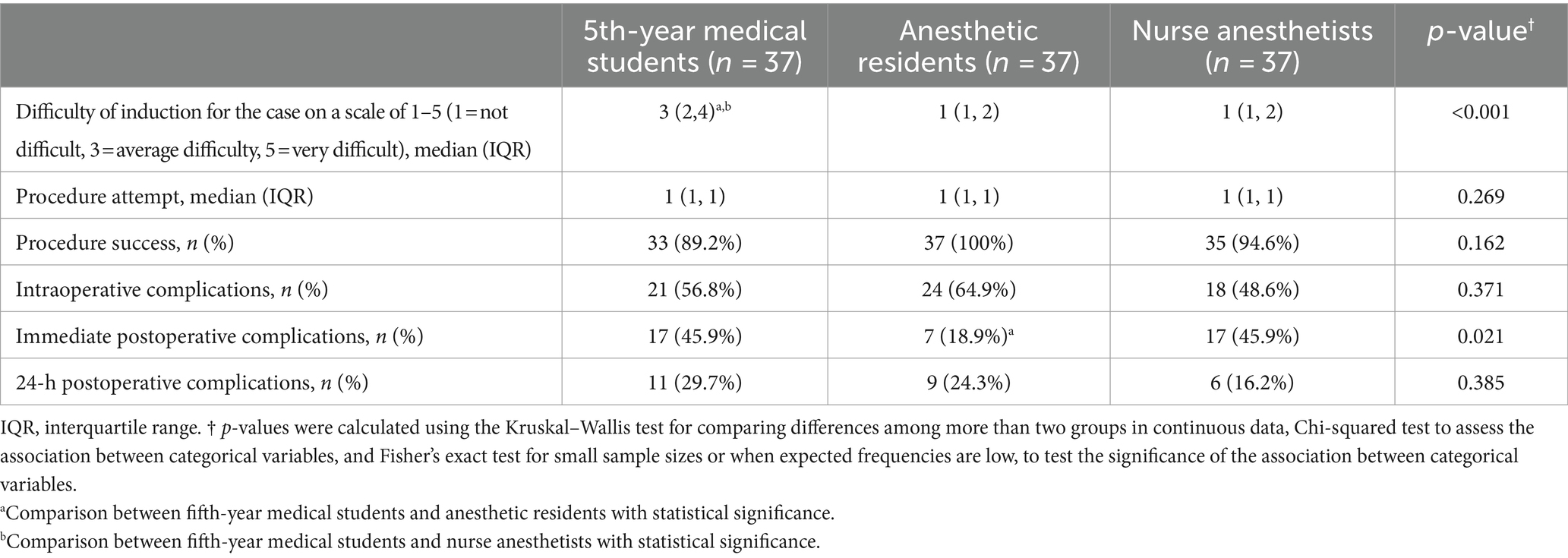
Table 4. Assessment of case difficulty, procedural attempts, success rates, and complications by medical students, residents, and nurse anesthetists.
3.8 Complications
Immediate postoperative complications, particularly airway-related issues, were more common among fifth-year medical students than anesthetic residents. However, these complications did not differ significantly between fifth-year medical students and student nurse anesthetists. Intraoperative and 24-h postoperative complications were similar across all groups, suggesting that the increased procedural times did not adversely affect overall patient outcomes (Table 4).
4 Discussion
This study found that fifth-year medical students’ involvement in anesthetic procedures significantly increased several key time metrics, including ART, ACT, APpT, and APT, when compared to anesthetic residents and student nurse anesthetists. This may be attributed to the students’ lack of hands-on experience and clinical skills as well as the brief duration of their rotation in anesthesiology (only 1 week). By contrast, anesthetic residents and student nurse anesthetists, with more advanced skills and experience, showed shorter procedure times.
These results align with and extend previous research on the effects of trainee involvement in anesthetic procedures. Eappen et al. (2004) reported similar findings, where teaching anesthesia residents was associated with a statistically significant increase in the time required for induction and emergence from anesthesia. Our study corroborates these findings and further demonstrates that this effect is even more pronounced with medical students, likely because of their more limited experience compared to anesthetic residents. Browne et al. (2011) found that the inclusion of anesthetic trainees increased ACT during Cesarean sections by approximately 5.2 min. Our results show a similar trend, with medical students’ involvement leading to extended ACT compared to both anesthetic residents and nurse anesthetists. This consistency across studies suggests a generalizable effect of trainee involvement on procedural times, regardless of the specific surgical context.
Interestingly, our study showed a higher proportion of ACT across all groups, ranging from 22.6 to 26.7% of TCT, compared to the previous literature. Davis et al. (2006) reported that teaching anesthesia residents increased time to incision by a mean of 4.5 ± 3.2 min and this increase was insignificant compared with the time required to complete the surgical procedure. Dexter et al. (1995) found ACT in obstetric-gynecologic and general surgery in approximately 15% of TCT cases. Meanwhile, Irani et al. (2010) showed ART to be approximately 8.4 to 13.3% of the TCT. The difference between these studies and ours may reflect changes in anesthetic practices over time or variations in institutional protocols, highlighting the need for ongoing research in this area.
4.1 Impact on operating room efficiency and training balance
Enhancing OR efficiency often presents a challenge in academic teaching hospitals, as it may compromise the training of medical students and residents. As most surgical cases involve trained clinicians, medical students’ involvement in anesthetic procedures may affect both OR learning opportunities and patient care, including procedural timing.
The concept of “time on task” refers to the correlation between learning and time spent engaging with the subject material (Spijkerman et al., 2024). However, equal time investment does not result in the same benefit across different tasks, and such factors as the nature and quality of activities and student engagement influence learning (Godwin et al., 2021).
This study underscores the need for a balanced approach between OR efficiency and the educational needs of medical trainees. The significant differences in ART, ACT, APpT, and APT among the groups did not translate into substantial clinical or economic impacts. The slightly extended procedural times associated with fifth-year medical students highlight the critical role of giving students hands-on experience, a key component of their training in anesthesiology. Educators should aim to provide adequate supervision to mitigate risks while maintaining educational value. This result aligns with the findings by Irani et al. (2010), who reported that 9.8% of TCT is spent on educational activities, including developing clinical and communication skills, which are vital for trainees’ development. Moreover, previous literature, such as Mazzei (1994) and Dexter et al. (1995), highlighted that even though ACT may be increased, the overall effect on OR efficiency and costs is minimal, because the time saved is often not enough to schedule additional cases during a standard workday. Thus, the financial impact of ACT secondary to teaching is minimal.
Although extended procedural times may raise concerns about OR efficiency, this study found the overall impact to be modest. These findings suggest that integrating medical education within the OR does not significantly compromise the efficiency of surgical procedures or patient outcomes. This result supports the education model in teaching hospitals, where the presence of trainees is essential for a robust learning environment and effective clinical training.
4.2 Complications and safety considerations
Regarding patient safety, our study found a higher rate of immediate airway complications among procedures involving fifth-year medical students, although this difference did not persist in intraoperative or 24-h postoperative outcomes. This discrepancy in complications may be attributed to the varying levels of clinical experience and expertise among the groups. The advanced training and clinical exposure that anesthetic residents undergo likely contribute to their proficiency in managing airways and perioperative challenges, resulting in fewer complications compared to less experienced trainees, such as medical students and nurse anesthetists. This nuanced finding adds to the literature on trainee involvement and patient outcomes, such as Lynch et al. (2024), who found no significant difference in patient outcomes between cases with and without anesthetic resident involvement.
These findings collectively suggest that while the involvement of fifth-year medical students in anesthetic procedures increases certain time metrics, it does not significantly impact the overall case duration or patient safety. These results support the continued integration of medical education within the OR, aligning with border literature on the importance of experiential learning in medical training (Wijnen-Meijer et al., 2022).
5 Strengths, limitations, and future directions
This study’s prospective design and the blinding of OR staff to the research objectives are notable strengths that help reduce potential biases. However, other limitations should be acknowledged, including the single-center design and relatively small sample size, which may limit the generalizability of the findings. Additionally, the variability in teaching methods among instructors could influence the time metrics observed, suggesting that more standardized training protocols could benefit future research. Moreover, we recognize that the shorter anesthesia rotation (one week) for fifth-year medical students compared to the immersive training received by anesthetic residents and nurse anesthetists likely influenced the procedural times and perceived difficulty. This variation in exposure could have introduced biases, which were not fully controlled in this study.
Future studies should aim to explore this research topic in larger and more diverse cohorts, possibly extending the evaluation to include the broader benefits of perioperative care and management skills acquired by medical students. Understanding the full scope of educational value within the OR beyond just procedural timing would help refine training programs and optimize the balance between education and efficiency in teaching hospitals.
6 Conclusion
These findings indicate that fifth-year medical students’ involvement in anesthetic procedures leads to some increases in specific time metrics. However, their involvement does not significantly compromise overall OR efficiency or patient safety. This supports the continued integration of hands-on training for medical students in the OR, with appropriate supervision to manage the slightly increased risk of immediate postoperative complications. Further research is needed to optimize the balance between educational opportunities and OR efficiency, particularly focusing on strategies to reduce the incidence of immediate postoperative complications associated with medical student involvement.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Institutional Human Research Ethics Committee of the Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand (REC.65-156-8-1). The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement for written informed consent due to the study being observational.
Author contributions
SC: Conceptualization, Data curation, Funding acquisition, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing. MS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. TK: Conceptualization, Data curation, Methodology, Project administration, Validation, Visualization, Writing – review & editing. DY: Investigation, Software, Writing – review & editing. KS: Investigation, Software, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors thank Editage (www.editage.com) for English language editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Browne, W., Siu, L. W., and Monagle, J. P. (2011). The impact of anaesthetic trainees on elective caesarean section procedural times: a prospective observational study. Anaesth. Intensive Care 39, 936–940. doi: 10.1177/0310057X1103900521
Davis, E. A., Escobar, A., Ehrenwerth, J., Watrous, G. A., Fisch, G. S., Kain, Z. N., et al. (2006). Resident teaching versus the operating room schedule: an independent observer-based study of 1558 cases. Anesth. Analg. 103, 932–937. doi: 10.1213/01.ane.0000232444.52274.7a
Dexter, F., Coffin, S., and Tinker, J. H. (1995). Decreases in anesthesia-controlled time cannot permit one additional surgical operation to be reliably scheduled during the workday. Anesth. Analg. 81, 1263–1268
Donham, R. T. (1998). Defining measurable OR-PR scheduling, efficiency, and utilization data elements: the Association of Anesthesia Clinical Directors procedural times glossary. Int. Anesthesiol. Clin. 36, 15–30. doi: 10.1097/00004311-199803610-00005
Eappen, S., Flanagan, H., and Bhattacharyya, N. (2004). Introduction of anesthesia resident trainees to the operating room does not lead to changes in anesthesia-controlled times for efficiency measures. Anesthesiology 101, 1210–1214. doi: 10.1097/00000542-200411000-00022
Emmanouil, B., Goldacre, M. J., and Lambert, T. W. (2017). Aspirations to become an anaesthetist: longitudinal study of historical trends and trajectories of UK-qualified doctors' early career choices and of factors that have influenced their choices. BMC Anesthesiol. 17:100. doi: 10.1186/s12871-017-0392-5
Godwin, K. E., Seltman, H., Almeda, M., Davis Skerbetz, M., Kai, S., Baker, R. S., et al. (2021). The elusive relationship between time on-task and learning: not simply an issue of measurement. Educ. Psychol. 41, 502–519. doi: 10.1080/01443410.2021.1894324
Hoffman, C. R., Horrow, J., Ranganna, S., and Green, M. S. (2019). Operating room first case start times: a metric to assess systems-based practice milestones? BMC Med. Educ. 19:446. doi: 10.1186/s12909-019-1886-2
Irani, J. L., Greenberg, J. A., Blanco, M. A., Greenberg, C. C., Ashley, S., Lipsitz, S. R., et al. (2010). Educational value of the operating room experience during a core surgical clerkship. Am. J. Surg. 200, 167–172. doi: 10.1016/j.amjsurg.2009.06.023
Lynch, D., Mongan, P. D., and Hoefnagel, A. L. (2024). The impact of an anesthesia residency teaching service on anesthesia-controlled time and postsurgical patient outcomes: a retrospective observational study on 15,084 surgical cases. Patient Saf. Surg. 18:12. doi: 10.1186/s13037-024-00394-z
Mazzei, W. J. (1994). Operating room start times and turnover times in a university hospital. J. Clin. Anesth. 6, 405–408. doi: 10.1016/S0952-8180(05)80011-X
Overdyk, F. J., Harvey, S. C., Fishman, R. L., and Shippey, F. (1998). Successful strategies for improving operating room efficiency at academic institutions. Anesth. Analg. 86, 896–906. doi: 10.1097/00000539-199804000-00039
Rukewe, A., Abebe, W. A., Fatiregun, A. A., and Kgantshang, M. (2017). Specialty preferences among medical students in Botswana. BMC. Res. Notes 10:195. doi: 10.1186/s13104-017-2523-y
Spijkerman, S., Manning, D. M., and Green-Thompson, L. P. (2024). Undergraduate anesthesia skills for a global surgery agenda: students’ self-reported competence. Anesth. Analg. 138, 616–625. doi: 10.1213/ANE.0000000000006375
Udelsman, R. (2003). The operating room: war results in casualties. Anesth. Analg. 97, 936–937. doi: 10.1213/01.ANE.0000085295.04697.CC
Keywords: anesthesia, education, intraoperative period, medical, operating rooms
Citation: Chatmongkolchart S, Saetang M, Kunapaisal T, Yongsata D and Saelim K (2024) The impact of anesthesia clerkship training on procedural timing: a focus on medical students in anesthesiology. Front. Educ. 9:1446914. doi: 10.3389/feduc.2024.1446914
Edited by:
Habib Md Reazaul Karim, All India Institute of Medical Sciences, IndiaReviewed by:
Abhijit Nair, Ministry of Health, OmanKewithinwangbo Newme, All India Institute of Medical Sciences, India
Imran Ahmed Khan, Baba Raghav Das Medical College, India
Copyright © 2024 Chatmongkolchart, Saetang, Kunapaisal, Yongsata and Saelim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mantana Saetang, c3RtYW50YW5hQGdtYWlsLmNvbQ==
 Sunisa Chatmongkolchart
Sunisa Chatmongkolchart Mantana Saetang
Mantana Saetang Thitikan Kunapaisal
Thitikan Kunapaisal