- 1Faculty of Rehabilitation Medicine, University of Alberta, Edmonton, AB, Canada
- 2Department of Occupational Therapy, Faculty of Rehabilitation Medicine, University of Alberta, Edmonton, AB, Canada
There is a critical need to diversify health professionals to better serve the growing minority population in North America. Unfortunately, minority groups remain underrepresented in health professions. Despite recruitment efforts by government and academic institutions, fewer underrepresented minority (URM) students choose careers in healthcare. Identifying the key factors influencing URM students’ decisions to pursue health sciences programs could enhance diversity in these programs through targeted admissions strategies, ultimately leading to a more diverse future healthcare workforce. This scoping review was conducted in accordance with the Joanna Briggs Institute methodology for scoping reviews. Five electronic databases and gray literature were searched to identify North American papers published between 1942 and 2022. Identified studies focused on URM students’ perceptions of facilitators and barriers to matriculate into a health science degree. Twenty-one articles were analyzed. Following content analysis, the facilitators and barriers identified comprised personal, socio-cultural, institutional, and financial. The most frequent facilitators reported were scholarships, family support, and the presence of role models. Common barriers included high tuition fees, pre-admission criteria, lack of awareness about the health profession, availability of financial aid, and the admission process. The findings of this review will facilitate the development and implementation of customized, comprehensive strategies to recruit more URM students to health science programs in the future, thereby improving efforts toward creating a diverse healthcare workforce.
1 Introduction
Underrepresented minority (URM) groups in North America have historically included racialized visible minorities, Indigenous peoples, individuals with disabilities, those from socioeconomically disadvantaged backgrounds, and LGBTQ2+ individuals. In the United States, URM groups typically encompass African Americans/Blacks, Hispanics/Latinos, Native Americans/Alaska Natives, and Native Hawaiians/Pacific Islanders. In contrast, Canada defines URM groups more broadly under the category of visible minorities or people of color, which includes Blacks, Latinos, South Asians, Chinese, and Filipinos. It is predicted by 2036, that 14.4 million people, or one-third of the Canadian population, will be members of a minority group, whereas, by 2060, 56% of Americans are expected to identify as members of a minority group (U.S. Census Bureau, 2015; Statistics Canada, 2017). Despite health professionals’ critical and fundamental role in providing high-quality healthcare to the population, a recent study by Salsberg et al. (2021) reported that some URM groups are severely underrepresented in the U.S. healthcare workforce, particularly African Americans, Latinos and American Indians. Cohen et al. (2002) warns this stagnation in minority representation in the healthcare workforce will have negative consequences.
Diversifying healthcare professionals improves trust and communication between healthcare workers and patients, enhancing compliance with regular follow-up visits and expanding healthcare access to URM populations (Health and Services, 2006; Williams et al., 2008). The more varied the healthcare workforce, the better they can treat their patients with respect and knowledge. URM patients prefer to select healthcare professionals of similar minority backgrounds when they have the freedom to choose healthcare professionals. These patients risk not being understood or being unable to obtain the right care when they cannot find caregivers who share their values, culture, or other aspects of their lives. When healthcare professionals treat URM patients of similar ethnicity with proper communication, they better understand and adhere to their treatment (Spevick, 2003; Chen et al., 2005). Additionally, these URM patients demonstrated better quality of care and higher satisfaction when treated by healthcare professionals of similar minority backgrounds (Cooper-Patrick et al., 1999; Chen et al., 2005; Saha and Beach, 2020). Studies indicate that URM patients frequently express greater satisfaction and a more positive healthcare experience when attended to by URM physicians. For instance, African American patients exhibited a tendency to rate their physicians more favorably when they shared the same racial background, attributing this preference to a perceived increase in physician participation (Cooper et al., 2003; Saha et al., 2008).
Diversity in the classroom is the only way to attain diversity in the professional healthcare workforce (The American Association of Colleges of Pharmacy, 2000). Historically, underrepresented minority students have disproportionately low representation in health science academic programs, resulting in a less varied healthcare workforce to provide the best care for an increasingly diverse population. Previously, few studies have reported on the overall program experience of URM students’ beyond just their admission experience to a health science program (Bright et al., 1998; Gardner, 2005; Loftin et al., 2012; Morrison et al., 2019). Boekeloo et al. (2017) also suggested the importance of early identification of intent and creating awareness among high school URM students to venture into health sciences career paths. Despite the increasing efforts to create diversity among health science programs and institutions, there is still significant underrepresentation of minority students. Therefore, determining the reason and key factors involved in selecting a health sciences program by URM students will improve diversity in future health science programs, thereby improving diversity in the healthcare workforce. Given the ambiguity in the literature on self-perceived factors influencing a minority student in selecting a health sciences program, a scoping review was conducted to systematically map the existing literature in this area and highlight any existing gaps in knowledge. This review was guided by the research question: “What perceived factors may influence minority students when choosing a health science program?” The findings of this research would be of significance to educational leaders in developing or modifying URM student recruitment and retention strategies to diversify their health science programs. This study will also assist education policymakers in developing policies to alleviate identified barriers for future URM students aspiring to pursue a healthcare career.
2 Methods
The scoping review was based on Arksey and O’Malley’s methodological guideline (Arksey and O’Malley, 2005) and later amended by the Joanna Briggs Institute-JBI (Peters et al., 2020). The review follows the PCC framework, i.e., population: URM students; concept: program selection; and content: health science and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews—PRISMA-ScR (Tricco et al., 2018).
2.1 Eligibility criteria
Peer-reviewed articles and gray literature written in English and published between 1942 and 2022 were eligible for this review. The focus was on articles examining URM students’ self-perceptions of barriers and facilitators that influenced or might influence their decision to apply for health science programs. Articles included representations from various URM groups: Black, Indigenous, and people of color (BIPOC); Low-Income or Socioeconomically Disadvantaged Students (SES); students from Lesbian, Gay, Bisexual, Transgender, Queer, and Two-Spirit (LGBTQ2+) communities; Students with Disabilities (SwD); and First-generation students (first-gen).
The review considered papers involving graduate and undergraduate URM students enrolled in health sciences programs or high school URM students aspiring to apply to health sciences programs in North America. Studies were excluded if they did not meet the inclusion criteria, specifically those focusing solely on gender discrimination, linguistic discrimination, academic success, degree completion, and retention. Additionally, studies were excluded if they involved students who were not from minority backgrounds in North America or were not enrolled in health sciences programs. However, studies with combined URM student populations from the health sciences and other disciplines were included.
2.2 Literature search and data extraction
A comprehensive literature search was performed in academic databases ranging from 1942 to 2022: Medline, Scopus, Embase, CINAHL, Web of science, including gray literature. The literature search results for each database were imported into Zotero Citation Manager and Covidence Systematic Review software. After performing title and abstract screening, all searched records were de-duplicated and saved. Later, seed papers were manually searched. Subsequently, a snowballing search approach was used with Research Rabbit, a tool for mapping the literature based on citations. Data extraction was performed using a pre-designed data-charting form developed by the authors that included the author’s name, year, purpose, participants, data collection method, health science discipline, facilitators and barriers.
Once the data was categorized into facilitators and barriers, an inductive analysis was conducted for each category, creating unique sub-category codes to further describe the contents of the initial categories (Elo and Kyngäs, 2008). The investigators reached total agreement on the identified sub-categories, which were also influenced by previous studies by De Freitas et al. (2021), Freeman et al. (2016), Fuse (2018), and Snyder and Bunkers (1994). Four sub-categories of barriers and facilitators were identified as:
1. Personal: This sub-category includes elements pertinent to the individual characteristics of URM students, such as motivation, drive, commitment, perceived self-efficacy, fear, exposure to a health-related incident/illness, learning difficulties, underachievement, insufficient academic preparation, self-awareness, or misinformation about the healthcare field.
2. Socio-cultural: These factors relate to familial, societal, and other variables influencing URM students. They involve family education/awareness, friends, religious/political/community/ethnic group leaders, healthcare professionals, or alumni of a health science program in the family or extended family.
3. Institutional: This sub-category encompasses academic institutions, faculty, and other related factors. It includes faculty/teachers, reputable institutions/programs, distance/location of the educational institution, duration of the program, prerequisites to enter a program, misinformation about the admission process, and discrimination in the admission process.
4. Financial: These factors pertain to economic considerations, such as family income, tuition fees, scholarships, student loans/bursaries, employment opportunities as a student, and future earnings.
3 Results
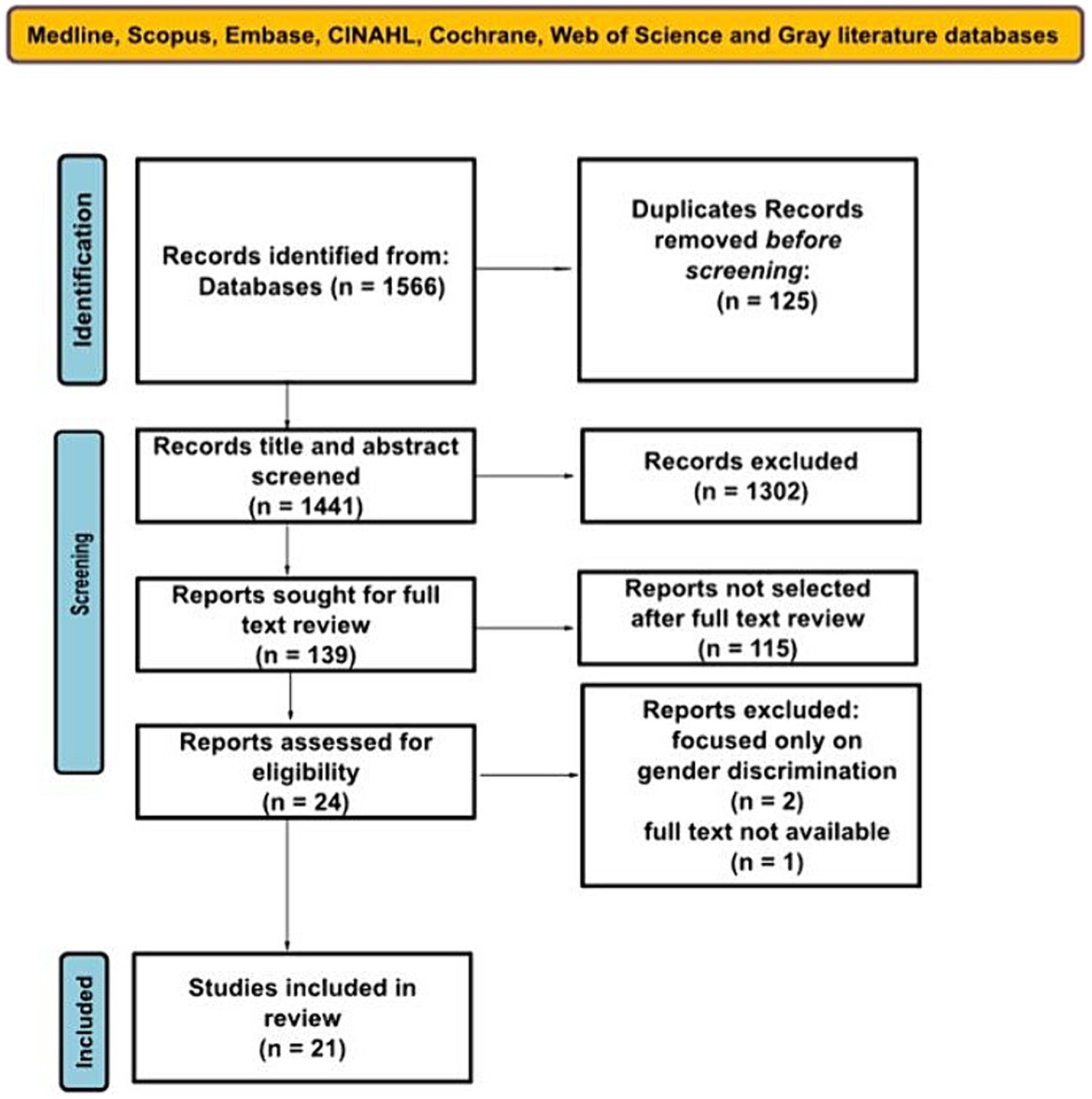
A total of 1,566 articles were retrieved; after removing duplicates, 1,441 articles remained. Subsequent screening of the title and abstract resulted in 1,302 exclusions, and 139 articles were retrieved for full-text review. Out of these, 115 were excluded as they did not fit the inclusion criteria, and 24 were assessed for eligibility. Three publications were removed for the following reasons: two articles focused only on gender discrimination, and one study was excluded as full text could not be retrieved. The remaining 21 studies were considered eligible for this scoping review. The summary of the literature search process is illustrated in Figure 1.
3.1 Descriptive characteristics of selected studies
All 21 selected studies were empirical studies comprising 11 (52%) qualitative and 10 (48%) quantitative. The majority were from the United States, 19 (90.5%) and the remaining were from Canada 2 (9.5%). All 21 of the studies reported barriers (100%), of which 5 (24%) stated only barriers whereas 16 (76%) studies conveyed both facilitators and barriers. The total sample population comprised 3,693 underrepresented students from diverse minority ethnicities including African American, American Indian, Latina, Hispanic, Indigenous groups, and students from low socioeconomic status pursuing different health science programs, which included medicine, dentistry, dental hygiene, nursing, pharmacy, speech pathology, physical therapy, and kinesiology. The majority of the studies had graduate students, 14 (67%), whereas some of them had undergraduates 5 (24%) and high school students 2 (9%). A descriptive summary of study characteristics is provided in Table 1.
In 12 out of 21studies, socio-cultural factors were reported as key facilitators, representing 57% of the total. Personal factors were facilitators in 10 studies (48%), while institutional factors were noted in nine studies (43%). The primary facilitators for URM students included mentorship from role models, support from family and friends, personal self-efficacy and social compassion, access to counseling programs, and availability of scholarships and financial aid.
Financial factors were the predominant barriers, identified in 17 of the studies (81%). Socio-cultural factors were the next most influential, mentioned in 16 of the studies (76%). Personal and institutional factors were less frequently noted, with 15 (71%) and 13 studies (62%), respectively. Major barriers cited by URM students were the high cost of education, lack of financial aid awareness, misconceptions about the health profession, insufficient mentorship, and inadequate academic preparation along with challenging admission criteria.
Figure 2 illustrates distribution of studies on facilitators and barriers for URM students entering health science programs and Figure 3 shows key barriers and facilitators influencing URM students’ matriculation into health science programs.
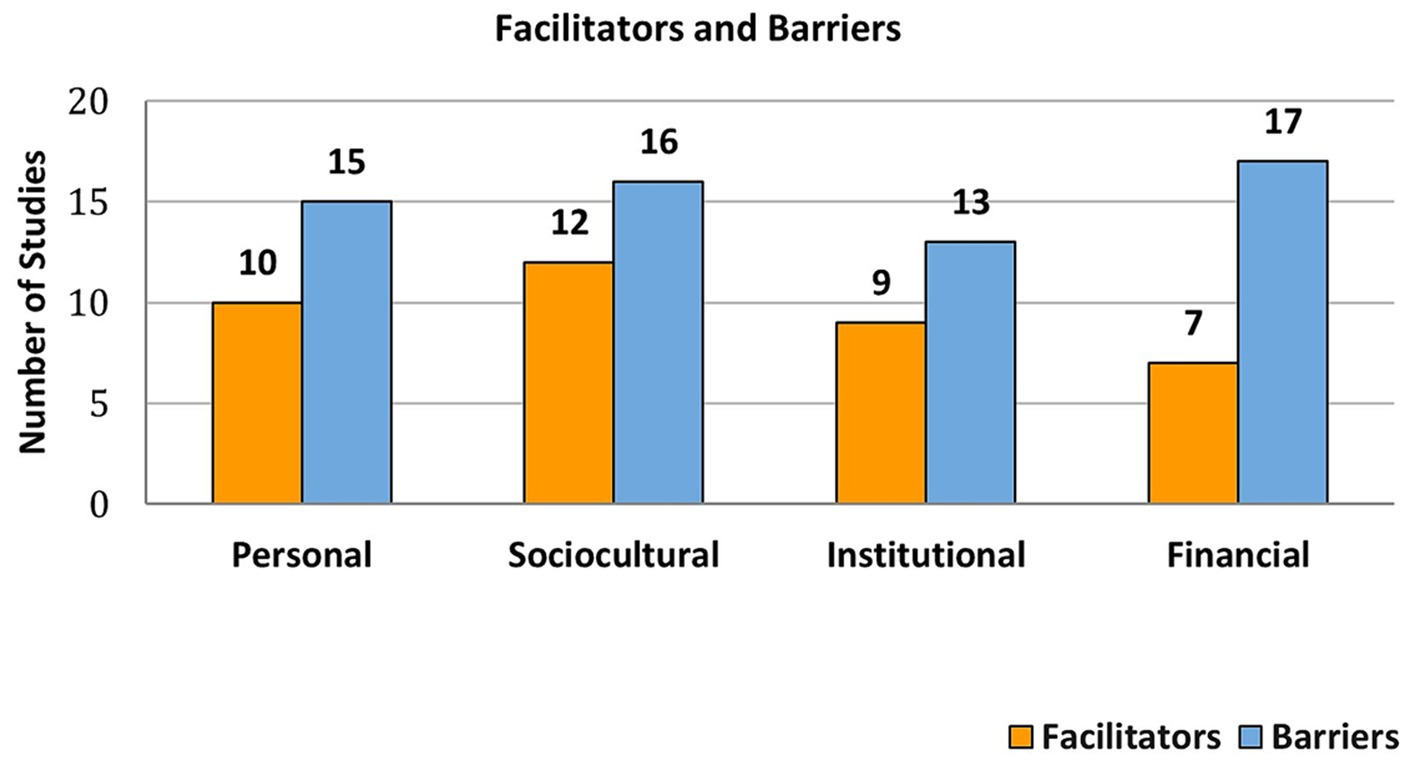
Figure 2. Distribution of studies on facilitators and barriers for URM students entering health science programs.
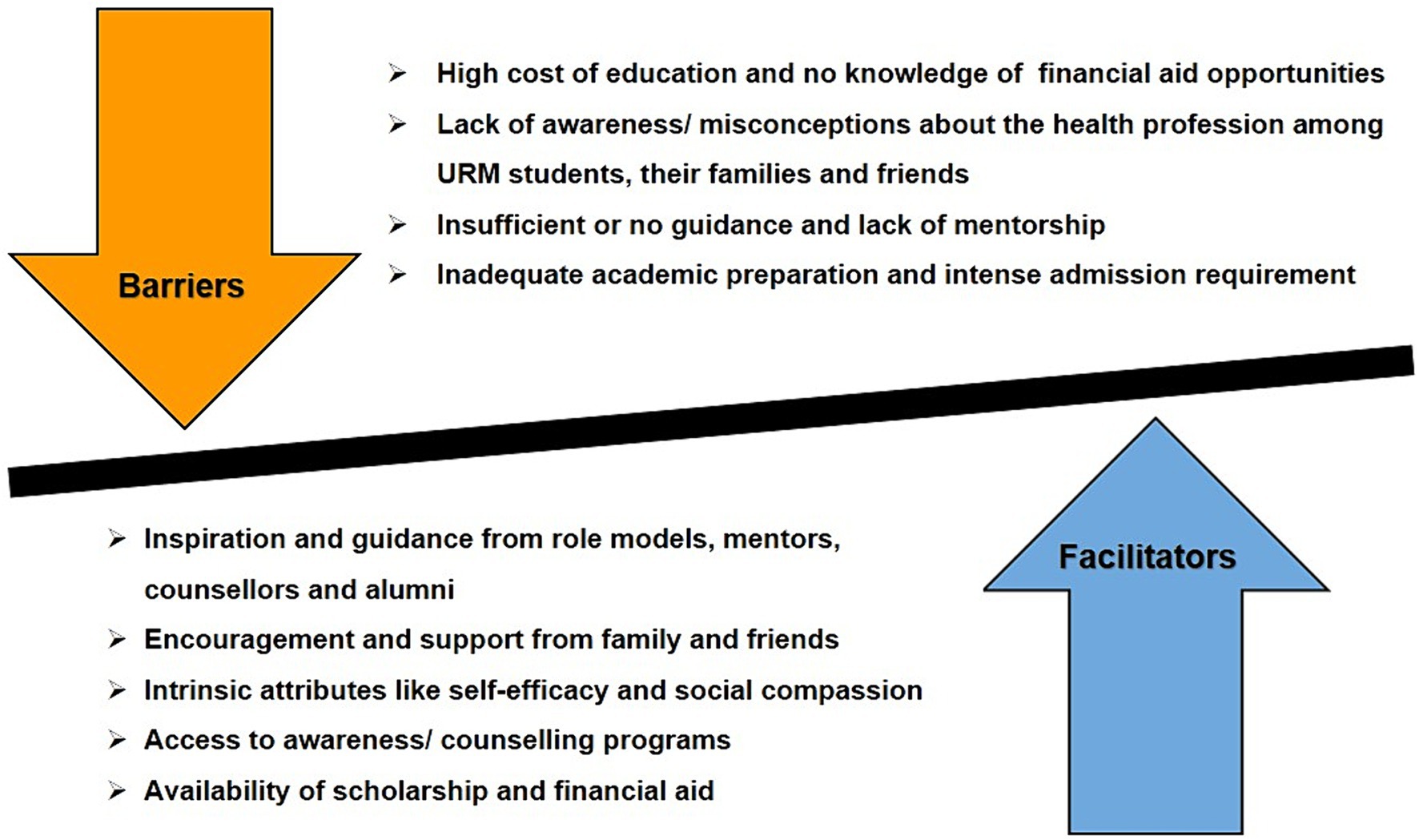
Figure 3. Key barriers and facilitators influencing URM students’ matriculation into health science programs.
3.2 Facilitators and barriers for selecting a health science program
3.2.1 Personal
Participants perceived that the health science program requires passion, inner drive, and motivation to persevere even when the path appears difficult (Hadinger, 2016). Self-confidence, attitude, strategy, seeking and sorting information and motivation were skills participants identified as facilitators. These facilitators helped participants to generate compelling reasons to seek a career in the health profession, persevere when faced with hurdles, and devise proactive plans to gain admission to these programs (Snyder and Bunkers, 1994; Henry, 2006; Barfield et al., 2012; De Freitas et al., 2021).
However, health science academic programs can be overwhelming, highly competitive and require considerable time commitment (Joseph et al., 2021). URM students perceive the admission process requiring lengthy commitment and personal conviction (Hadinger, 2016). Limited knowledge, self-doubt, fear of isolation from family and friends, fear of low chance of acceptance and religious beliefs are the key factors which prohibit URM students from applying to a health sciences program (Freeman et al., 2016; Alonzo et al., 2019; Burns et al., 2021; De Freitas et al., 2021; Joseph et al., 2021).
3.2.2 Socio-cultural
Despite misperceptions about the health profession, URM students received encouragement and support from loved ones (Woods-Giscombe et al., 2020). Racial and cultural communities provided representation, encouragement, and role modeling. Parents’ education, familial support, exposure to the healthcare field through family, and association with peers and friends who could guide them through the admission process were stated as major facilitators (Wilcox et al., 2005; Hollow et al., 2006; Wadenya and Lopez, 2008; Sandino and Rowe, 2014; Hadinger, 2016; Fuse, 2018; Woods-Giscombe et al., 2020; De Freitas et al., 2021).
However, several socio-cultural barriers discouraged URM students from selecting healthcare programs. Lack of role models, absence of mentoring/guidance, family education, parental misconception about the healthcare discipline, discouragement from family/friends, societal pressure to choose different careers, spiritual/cultural beliefs and practices and fear of discrimination hindered URM students in selecting healthcare programs (Henry, 2006; Hollow et al., 2006; Freeman et al., 2016; Woods-Giscombe et al., 2020; Abdulrazzak et al., 2021; Burns et al., 2021; Joseph et al., 2021) Furthermore, Joy-Correll et al. (2022) reported racism, othering, and tokenism as barriers.
3.2.3 Institutional
Underrepresented minority students’ program selection was influenced by institutional reputation, institutional support, faculty reputation and distance from home (Snyder and Bunkers, 1994; Wilcox et al., 2005; De Freitas et al., 2021). Professional exposure programs, academic counseling, increasing awareness of career opportunities, and meeting minority alumni emerged as key facilitators (Hollow et al., 2006; Burns et al., 2021).
Despite these facilitators, URM students claim that their low high school performance, competitive admission exam score, lack of URM faculty, prerequisite requirements, complex admission process and lack of assistance prevented them from enrolling in the health science program (Sandino and Rowe, 2014; Hadinger, 2016; Alonzo et al., 2019; Kovacs, 2022).
3.2.4 Financial
Funding was the predominant facilitator among URM students, and they rely on several different financial facilitators, including financial assistance from family, student loans, scholarships, admission test fee assistance, and tuition reimbursement programs (Snyder and Bunkers, 1994; Sandino and Rowe, 2014; De Freitas et al., 2021).
However, a notable barrier exists in the form of URM students’ general lack of awareness regarding the availability of financial aid (Veal et al., 2004; Joseph et al., 2021). A study by Freeman et al. (2016) also revealed that URM students’ families lacked information on the medical or dental career costs and the procedures and pathways to becoming a doctor or dentist. Many studies reported that URM students were concerned about the expenses, not only tuition fees but also regarding costs involving application fees, preparation of standardized tests and travel for admission interviews (Lopez et al., 2003; Henry, 2006; Wadenya and Lopez, 2008; Freeman et al., 2016; Hadinger, 2016; Fuse, 2018; Alonzo et al., 2019; Abdulrazzak et al., 2021; Burns et al., 2021; De Freitas et al., 2021; Joseph et al., 2021; Kovacs, 2022).
4 Discussion
There is an urgent need for diverse healthcare professionals to render high quality healthcare services to the growing minority population in North America. Unfortunately, there is continued shortage of health professionals, especially from minority groups. This is because fewer minority students choose a healthcare profession despite efforts made by the government and academic institutions. To increase underrepresented minority students’ admission to a health science program, it is crucial to understand their perceptions and factors influencing their decision to pursue and apply to a health science program. Therefore, this scoping review was conducted to explore URM students’ perceptions of facilitators and barriers that will or have influenced their decision to pursue or select healthcare as a career.
Five electronic databases were used to retrieve 21 papers from North America, where several significant self-perceived facilitators and barriers among URM students were discovered. Overall, the review identifies financial factors to be the most influential among URM students followed by socio-cultural factors. According to the results of this review, 17 out of 21 studies indicated that the financial barrier was the most commonly encountered challenge among URM students. Results showed that high admission and tuition fees were among the most often cited perceived barriers. Most of the URM students were from low socioeconomic backgrounds and often relied on loans to finance their education; hence were worried about consequent debt repayment and future job opportunities (Snyder and Bunkers, 1994; Veal et al., 2004; Wilcox et al., 2005; Alonzo et al., 2019; Woods-Giscombe et al., 2020; De Freitas et al., 2021).
Health science programs can be overwhelming; therefore, emotional, and social support may contribute positively to the selection, successful retention and completion of the program. In a research conducted in 1975, Crawford et al. (1975) first reported that the two most influential factors in a student’s decision to pursue a career in healthcare are parental support and participation in health career orientation programs. Since then, many studies have reported that family support is one of the most significant influencing factors when choosing a career among URM and non-URM students. Surprisingly, this review identified family support as a facilitator and barrier. The identified barriers included family misconceptions about the health profession, family obligations/responsibilities/issues, fear of living away from family, family pressure/discouragement and gender stereotyping of the healthcare profession (Hollow et al., 2006; Freeman et al., 2016; Woods-Giscombe et al., 2020; Joseph et al., 2021). Parental knowledge about the health profession significantly influences URM students’ education. Furthermore, Woods-Giscombe et al. (2020) reported that URM students revealed that their family and friends’ misperceptions of the healthcare profession were passed to them. Due to these misconceptions, their family discouraged them from pursuing a health career.
The interpretation of this review is consistent with the findings of Hagedorn and Fogel (2002) and Varner et al. (2018) that URM students and their parents lacked awareness about the health profession, availability of financial aid, and the admission process. This review indicates that it is highly recommended to conduct consistent early follow-up-based outreach awareness/mentorship programs for both URM students and their parents, as they unveil the misperceptions of health science programs and provide an opportunity for early exposure to healthcare careers (Lopez et al., 2003; Veal et al., 2004; Wilcox et al., 2005; Wadenya and Lopez, 2008; Barfield et al., 2012; Freeman et al., 2016; Hadinger, 2016; Woods-Giscombe et al., 2020; De Freitas et al., 2021; Joseph et al., 2021; Kovacs, 2022). Furthermore, a study by Valentine et al. (2016) confirmed that summer enrichment programs have also been effective in raising the awareness of health careers among URM students. In addition, organizing conferences and symposiums to inform high school URM students and their parents about healthcare profession options not only raises awareness but also offers a platform to enhance their academic skills (Figueroa, 2014). However, to enhance recruitment efforts to increase URM students, it is suggested to actively involve members of professional health associations and healthcare regulatory agencies in these awareness campaigns. The findings of our review also demonstrate the need to involve financial grant experts from government scholarship agencies and educational institutions to provide thorough explanations of grants (including grant writing), loans, scholarships, and other forms of financial aid that could help minority students and their families to overcome the financial obstacles that keep them from enrolling in a health science program.
Our interpretation of the literature is consistent with Toretsky et al.’s (2018) conclusion that many URM students face obstacles in meeting admission prerequisite criteria due to inadequate academic preparation and guidance. Furthermore, this review corroborates Agrawal et al.’s (2005) findings that low GPAs and standardized admission test scores pose significant challenges for URM students. To address these issues, a more holistic admission procedure is suggested (Mandulak, 2022) that incorporate non-cognitive variables (Sedlacek and Kalsbeek, 2017) and de-emphasize strict GPA and standardized test score requirements when reviewing URM student applications.
Lastly, URM students bond well with faculty if they are from the same racial and ethnic background. A good role model of the same ethnicity can be a significant facilitator for URM students, while its absence acts as a barrier (Coleman, 2002). The data in this study showed that employing URM faculty is positively correlated to significant URM student recruitment and also serves as role models to mentor and guide them (Veal et al., 2004; Wilcox et al., 2005; Wadenya and Lopez, 2008). Similar findings were also reported by Agrawal et al. (2005), Allen et al. (1988), Kern (2000), Haskins and Rose-St Prix (1994), Sevier (1993), and Trevino (1994) in their studies. Additionally, Boekeloo et al. (2017) and DiBaise et al. (2015) recommended promoting faculty diversity by incorporating clinically practicing URM healthcare professionals who can serve as role models and mentors to new URM students. They further identified a correlation between the participation of URM faculty members on admissions committees and the enrolment of URM students. In addition, the insufficient number of URM faculty can pose challenges in recruiting URM students as well as new URM faculty members. Unfortunately, the representation of URM faculty (particularly those with a doctorate) remains consistently low in academic health sciences, leading to a vicious cycle (Matthews et al., 2020). Similarly, URM students who aspire to or are currently in a Ph.D. doctoral program are rare, making it crucial to study the facilitators and barriers they encounter. A substantial gap noted in this review of literature is that no study investigated the perspective of URM applicants who were not admitted or did not matriculate to an academic health program highlighting the need for future research. Additionally, it is essential to use an intersectional approach to investigate the challenges that URM students with disabilities or from other marginalized backgrounds face when seeking admission into a health science program.
Taken together, these results suggest that there is a need to update the existing pipeline enrichment programs, minority student recruitment policies and institutional strategies for URM students in North America according to the current needs of the diverse minority students and requirements for the future healthcare workforce. In order to design effective policies and strategies to enhance the enrolment of URM students, it is crucial to understand both the perceptions of URM students and the observations of admissions experts. It is hoped that these findings will facilitate the development and implementation of customized, comprehensive strategies to recruit more URM students to health science programs in the future, thereby improving efforts toward creating a diverse healthcare workforce.
This review is both essential and timely, given the recent significant backlash against diversity, equity, and inclusion (DEI) initiatives based on race-based college admissions policies in the US education sector (NACE, 2023). To achieve diversity without explicitly using race as a factor in admissions, our research findings suggest that educational institutions should employ same-ethnicity role models and implement consistent early follow-up outreach and mentorship programs to identify, guide, and mentor URM students and their families. Additionally, recruiting URM students to health science programs should involve a holistic admissions process that places greater emphasis on non-academic strengths and non-cognitive skills, providing a more comprehensive understanding of an applicant’s experiences, challenges, and strengths.
5 Limitations
This review had a few limitations. Firstly, even though a systematic process was used to find qualifying studies, it is still possible that pertinent studies were unintentionally missed. Secondly, the search was limited to North America and English language only, which restricts the generalizability. It is important to keep in mind that identified minority groups in North America might not be a minority in another geographical area. Lastly, the scope of the review was to identify and explore the perceived facilitators and barriers. The review did not concentrate on URM students’ perceptions of progress or retention in a health science program and the recruitment strategies used to admit URM students.
6 Conclusion
High priority is required to address these barriers and make modifications to improve equal opportunity and increase URM diversity in healthcare professionals. The review offers some important insights into unique barriers for URM students to enter a health science program that could inform education policymakers and admission committees to accommodate special admission policies and awareness workshops to motivate URM students to select a healthcare career.
Author contributions
SM: Investigation, Methodology, Writing – original draft, Writing – review & editing, Validation. MR: Supervision, Writing – review & editing, Methodology, Validation.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abdulrazzak, A., Chandler, A., Lu, R., Mobarakai, O., Lebron, B., Ingram, N., et al. (2021). Mini-medical school programs decrease perceived barriers to pursuing medical careers among underrepresented minority high school students. J. Osteopath. Med. 121, 883–890. doi: 10.1515/jom-2021-0125
Agrawal, J. R., Vlaicu, S., and Carrasquillo, O. (2005). Progress and pitfalls in underrepresented minority recruitment: perspectives from the medical schools. J. Natl. Med. Assoc. 97:1226.
Allen, M. E., Nunley, J. C., and Scott-Warner, M. (1988). Recruitment and retention of black students in baccalaureate nursing programs. J. Nurs. Educ. 27, 107–116. doi: 10.3928/0148-4834-19880301-05
Alonzo, N., Bains, A., Rhee, G., Htwe, K., Russell, J., Vore, D., et al. (2019). Trends in and barriers to enrollment of underrepresented minority students in a pharmacy school. Am. J. Pharm. Educ. 83:6925. doi: 10.5688/ajpe6925
Arksey, H., and O’Malley, L. (2005). Scoping studies: towards a methodological framework. Int. J. Soc. Res. Methodol. 8, 19–32. doi: 10.1080/1364557032000119616
Barfield, J. P., Cobler, D. C., Lam, E. T., Zhang, J., and Chitiyo, G. (2012). Differences between African-American and Caucasian students on enrollment influences and barriers in kinesiology-based allied Health education programs. Adv. Physiol. Educ. 36, 164–169. doi: 10.1152/advan.00129.2011
Boekeloo, B. O., Todaro Brooks, A., and Wang, Q. M. (2017). Exposures associated with minority high schoolers’ predisposition for health science. Am. J. Health Behav. 41, 104–113. doi: 10.5993/AJHB.41.2.1
Bright, C. M., Duefield, C. A., and Stone, V. E. (1998). Perceived barriers and biases in the medical education experience by gender and race. J. Natl. Med. Assoc. 90, 681–688.
Burns, L. E., Pezzullo, C., Amable, R., Mayorga, L., and Mejia, E. A. (2021). Assessing the pipeline: perceived barriers to applying to dental school among pipeline program alumni. J. Dent. Educ. 85, 157–165. doi: 10.1002/jdd.12406
Chen, F. M., Fryer, G. E., Phillips, R. L., Wilson, E., and Pathman, D. E. (2005). Patients beliefs about racism, preferences for physician race, and satisfaction with care. Ann. Fam. Med. 3, 138–143. doi: 10.1370/afm.282
Cohen, J. J., Gabriel, B. A., and Terrell, C. (2002). The case for diversity in the Health care workforce. Health Aff. 21, 90–102. doi: 10.1377/hlthaff.21.5.90
Coleman, P. M. (2002). The pre-entry guidance experiences of students undertaking an access to Health and professions allied to medicine (PAMs) Programme. Res. Post-Compuls. Educ. 7, 307–324. doi: 10.1080/13596740200200133
Cooper, L. A., Roter, D. L., Johnson, R. L., Ford, D. E., Steinwachs, D. M., Powe, N. R., et al. (2003). Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann. Intern. Med. 139:907. doi: 10.7326/0003-4819-139-11-200312020-0000
Cooper-Patrick, L., Gallo, J. J., Gonzales, J. J., Vu, H. T., Powe, N. R., Nelson, C., et al. (1999). Race, gender, and Partnership in the Patient-Physician Relationship. JAMA 282, 583–589.
Crawford, C. O., Fleming, P. L., and Harrison, I. E. (1975). Effects of a Health careers program and family support for a Health career on eighth graders career interest. Public Health Rep. 90, 168–172.
De Freitas, C., Buckley, R., Klimo, R., Daniel, J. M., Mountjoy, M., and Vanstone, M. (2021). Admissions experiences of aspiring physicians from low-income backgrounds. Med. Educ. 55, 840–849. doi: 10.1111/medu.14462
DiBaise, M., Salisbury, H., Hertelendy, A., and Muma, R. D. (2015). Strategies and perceived barriers to recruitment of underrepresented minority students in physician assistant programs. J. Phys. Assist. Educ. 26, 19–27. doi: 10.1097/jpa.0000000000000005
Elo, S., and Kyngäs, H. (2008). The qualitative content analysis process. J. Adv. Nurs. 62, 107–115. doi: 10.1111/j.1365-2648.2007.04569.x
Figueroa, O. (2014). The significance of recruiting underrepresented minorities in medicine: an examination of the need for effective approaches used in admissions by higher education institutions. Med. Educ. Online 19:24891. doi: 10.3402/meo.v19.24891
Freeman, B. K., Landry, A., Trevino, R., Grande, D., and Shea, J. A. (2016). Understanding the leaky pipeline: perceived barriers to pursuing a career in medicine or dentistry among underrepresented-in-medicine undergraduate students. Acad. Med. 91, 987–993. doi: 10.1097/acm.0000000000001020
Fuse, A. (2018). Needs of students seeking careers in communication sciences and disorders and barriers to their success. J. Commun. Disord. 72, 40–53. doi: 10.1016/j.jcomdis.2018.02.003
Gardner, J. (2005). Barriers influencing the success of racial and ethnic minority students in nursing programs. J. Transcult. Nurs. 16, 155–162. doi: 10.1177/1043659604273546
Hadinger, M. A. (2016). Underrepresented minorities in medical school admissions: a qualitative study. Teach. Learn. Med. 29, 31–41. doi: 10.1080/10401334.2016.1220861
Hagedorn, L. S., and Fogel, S. F. (2002). “Making school to college programs work: academics, goals, and aspirations” in Extending Their Reach: Strategies for Increasing Access to College. eds. W. G. Tierney and L. S. Hagedorn (Albany: State University of New York Press).
Haskins, A. R., and Rose-St Prix, C. (1994). Minority student recruitment and retention strategies in physical therapy education. J. Phys. Therap. Educ. 8, 3–10. doi: 10.1097/00001416-199401000-00002
Health and Services (2006). The rationale for diversity in the health professions: A review of the evidence.
Henry, P. (2006). Educational and career barriers to the medical profession: perceptions of underrepresented minority students. Coll. Stud. J. 40, 429–442.
Hollow, W. B., Patterson, D. G., Olsen, P. M., and Baldwin, L. M. (2006). American Indians and Alaska natives: how do they find their path to medical school? Acad. Med. 81, S65–S69. doi: 10.1097/01.ACM.0000237698.72582.c1
Joseph, J., Dao, D., Hwang, S. M., Dotzler, S. M., Chesak, S. S., Weiskittel, T. M., et al. (2021). Perceptions of barriers and facilitators to becoming a medical professional among underrepresented undergraduate and postbaccalaureate learners. Mayo Clin. Proc. Innov. Qual. Outcomes 5, 347–358. doi: 10.1016/j.mayocpiqo.2021.01.003
Joy-Correll, K., Nevill, E., Bird-Matheson, H., McLennan, H., Quinn, A., Mayer, Y., et al. (2022). Barriers and facilitators for indigenous students and staff in Health and human services educational programs. Adv. Health Sci. Educ. 27, 501–520. doi: 10.1007/s10459-022-10099-6
Kern, C. W. K. (2000). College choice influences: urban high school students respond. Community Coll. J. Res. Pract. 24, 487–494. doi: 10.1080/10668920050137255
Kovacs, T. (2022). Assessing barriers to graduate school admission for applicants from underrepresented populations in a Master’s level speech-language pathology program. Am. J. Speech Lang. Pathol. 31, 819–837. doi: 10.1044/2021_ajslp-21-00124
Loftin, C., Newman, S. D., Dumas, B. P., Gilden, G., and Bond, M. L. (2012). Perceived barriers to success for minority nursing students: an integrative review. ISRN Nurs. 2012, 1–9. doi: 10.5402/2012/806543
Lopez, N., Wadenya, R., and Berthold, P. (2003). Effective recruitment and retention strategies for underrepresented minority students: perspectives from dental students. J. Dent. Educ. 67, 1107–1112. doi: 10.1002/j.0022-0337.2003.67.10.tb03703.x
Mandulak, K. C. (2022). The case for holistic review in communication sciences and disorders admissions. Perspect. ASHA Special Interest Groups 7, 476–481. doi: 10.1044/2020_persp-20-00137
Matthews, A. K., Allen-Meares, P., Watson, K., Crooks, N., Smith, A., Hart, A., et al. (2020). The use of strategies from the social sciences to inform pipeline development programs for under-represented minority faculty and students in the health sciences. J. Clin. Transl. Sci. 5:e73. doi: 10.1017/cts.2020.566
Morrison, N., Machado, M., and Blackburn, C. (2019). Student perspectives on barriers to performance for black and minority ethnic graduate-entry medical students: a qualitative study in a west midlands medical school. BMJ Open 9:e032493. doi: 10.1136/bmjopen-2019-032493
NACE (2023). U.S. Supreme Court Strikes Down Affirmative Action in College Admissions: How the Decision Impacts Institutions of Higher Education. Available at: https://naceweb.org/public-policy-and-legal/legal-issues/us-supreme-court-strikes-down-affirmative-action-in-college-admissions-how-the-decision-impacts-institutions-of-higher-education/
Peters, M. D. J., Marnie, C., Tricco, A. C., Pollock, D., Munn, Z., Alexander, L., et al. (2020). Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 18, 2119–2126. doi: 10.11124/jbies-20-00167
Saha, S., and Beach, M. C. (2020). Impact of physician race on patient decision-making and ratings of physicians: a randomized experiment using video vignettes. J. Gen. Intern. Med. 35, 1084–1091. doi: 10.1007/s11606-020-05646-z
Saha, S., Guiton, G., Wimmers, P. F., and Wilkerson, L. (2008). Student body racial and ethnic composition and diversity-related outcomes in US medical schools. JAMA 300, 1135–1145. doi: 10.1001/jama.300.10.1135
Salsberg, E., Richwine, C., Westergaard, S., Portela Martinez, M., Oyeyemi, T., Vichare, A., et al. (2021). Estimation and comparison of current and future racial/ethnic representation in the U. S. Health care workforce. JAMA Netw. Open 4:e213789. doi: 10.1001/jamanetworkopen.2021.3789
Sandino, A. H., and Rowe, D. J. (2014). Students from underrepresented racial and ethnic groups entering the dental hygiene profession. J. Dent. Educ. 78, 465–472. doi: 10.1002/j.0022-0337.2014.78.3.tb05696.x
Sedlacek, W. E., and Kalsbeek, D. (2017). Measuring noncognitive variables: Improving admissions, success and retention for underrepresented students. New York: Routledge.
Sevier, R. A. (1993). Recruiting African-American undergraduates. A National Survey of the factors that affect institutional Choice. Coll. Univ. 68, 48–52.
Snyder, D. J., and Bunkers, S. J. (1994). Facilitators and barriers for minority students in master s nursing programs. J. Prof. Nurs. 10, 140–146. doi: 10.1016/8755-7223(94)90007-8
Soliman, Y. S., Rzepecki, A. K., Guzman, A. K., Williams, R. F., Cohen, S. R., Ciocon, D., et al. (2019). Understanding perceived barriers of minority medical students pursuing a career in dermatology. JAMA Dermatol. 155, 252–254. doi: 10.1001/jamadermatol.2018.4813
Spevick, J. (2003). The case for racial concordance between patients and physicians. AMA J. Ethics 5, 215–218.
Statistics Canada (2017). “Population Projections for Canada and Its Regions, 2011 to 2036.” Available at: https://www150.statcan.gc.ca/n1/pub/91-551-x/91-551-x2017001-eng.htm
The American Association of Colleges of Pharmacy (2000). “Ad hoc committee on affirmative action and diversity.” The American Association of Colleges of Pharmacy. Available at: https://www.aacp.org/sites/default/files/affirmativeactiondiversitycmte102000.pdf
Toretsky, C., Mutha, S., and Coffman, J. (2018). Breaking barriers for underrepresented minorities in the Health professions. Healthforce Center, University of California San Francisco.
Trevino, F. M. (1994). The representation of hispanics in the health professions. J. Allied Health 23, 65–77.
Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., et al. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 169, 467–473. doi: 10.7326/m18-0850
U.S. Census Bureau (2015). Census Bureau report. March 3). U. S. population projections. Available at: https://www.census.gov/newsroom/archives/2015-pr/cb15-tps16.html
Valentine, P., Wynn, J., and McLean, D. (2016). Improving diversity in the Health professions. N. C. Med. J. 77, 137–140. doi: 10.18043/ncm.77.2.137
Varner, K., Mey, L., Mentzel, T., Glazer, G., Tobias, B., and Seiple, T. (2018). Pulse check: underrepresented minority Health-care student recruitment and retention at the University of Cincinnati. J. Coll. Stud. Retent. Res. Theory Pract. 20, 388–405. doi: 10.1177/1521025116675179
Veal, K., Perry, M., Stavisky, J., and Herbert, K. D. (2004). The pathway to dentistry for minority students: from their perspective. J. Dent. Educ. 68, 938–946. doi: 10.1002/j.0022-0337.2004.68.9.tb03842.x
Wadenya, R. O., and Lopez, N. (2008). Parental involvement in recruitment of underrepresented minority students. J. Dent. Educ. 72, 680–687. doi: 10.1002/j.0022-0337.2008.72.6.tb04533.x
Wilcox, K. C., Weber, M., and Andrew, D. L. (2005). Factors influencing minority students’ Choice of physical therapist education programs. J. Phys. Therap. Educ. 19, 8–14. doi: 10.1097/00001416-200507000-00002
Williams, D. R., Costa, M. V., Odunlami, A. O., and Mohammed, S. A. (2008). Moving upstream: how interventions that address the social determinants of Health can improve Health and reduce disparities. J. Public Health Manag. Pract. 14, S8–S17. doi: 10.1097/01.PHH.0000338382.36695.42
Woods-Giscombe, C. L., Rowsey, J., Kneipp, P., Lackey, S. C., and Bravo, L. (2020). Student perspectives on recruiting underrepresented ethnic minority students to nursing: enhancing outreach, engaging family, and correcting misconceptions. J. Prof. Nurs. 36, 43–49. doi: 10.1016/j.profnurs.2019.08.006
Keywords: underrepresented minority students, URM, facilitators, barriers, health sciences, health professions, recruitment, diversity
Citation: Mohammed SAS and Roduta Roberts M (2024) Identifying factors influencing program selection in health sciences by underrepresented minority students—a scoping review. Front. Educ. 9:1369230. doi: 10.3389/feduc.2024.1369230
Edited by:
Renee J. Chosed, University of South Carolina, United StatesReviewed by:
William Burton, Albert Einstein College of Medicine, United StatesRam Krishna Mazumder, University of Kansas, United States
Candice M. Etson, Wesleyan University, United States
Copyright © 2024 Mohammed and Roduta Roberts. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mary Roduta Roberts, bXJvYmVydHNAdWFsYmVydGEuY2E=
 Sami Al Sufi Mohammed
Sami Al Sufi Mohammed Mary Roduta Roberts
Mary Roduta Roberts