- 1Department of Surgery, University Sapienza, Rome, Italy
- 2Department of Translational and Precision Medicine, University Sapienza, Rome, Italy
- 3Department of General Surgery and Surgical Specialties, University Sapienza, Rome, Italy
Multimorbidity is defined as the co-existence of two or more chronic diseases in a patient, and it is increasing in prevalence. This condition poses new problems for clinical reasoning. Few studies inquire regarding the construct of reasoning in multimorbidity and the teaching/learning methods. The objectives of this scoping review were searching for a definition of the construct of clinical reasoning in multimorbidity and the related learning methods, and special ways in which information technology can help. We searched PubMed, Scopus, ERIC and CORE databases. After an iterative process of selection and thematic analysis, we selected 30 articles, that were thematized in three classes: the multimorbid patient as a teacher (8 articles), defining a framework of competence (11 articles), representing multimorbidity and related clinical reasoning (11 articles). In this last theme were also grouped studies using technology to enhance learning. The construct of clinical reasoning in multimorbidity expands over three domains: clinical (including managing uncertainty, anticipating, and detecting evolutions and conflicting guidelines, and setting priorities); relational (concerning communicating uncertainty and developing a feasible, shared plan of care with the patient; organizational) (managing the wide system of resources needed to take care of a multimorbid patient). The preferred teaching methods are based on the encounter with real or expert patients, technology enhanced case-based learning and graphical representations of clinical cases. Perspectives of research should be addressed to permit the learner to experience a patient’s life-long experience by moving forward and back over time while exploring interactions among diseases and social determinants with respect to possibly conflicting treatments. Perspectives on rich, technology-enhanced simulations should be researched.
1. Introduction
Clinical reasoning describes the mental process doctors use to make a diagnosis based on a patient’s medical history, physical examination, and investigations (Eva, 2005). Besides diagnostic reasoning, management reasoning is the process involved in reasoning about patient management decisions (Cook et al., 2023). In past decades, studies in cognitive psychology led to a better understanding of this complex process (Eva, 2005; Croskerry, 2009). Dual process theory is currently still considered the model that best describes the process of clinical diagnostic reasoning. It takes place through two processes, distinct but in a circular relationship: hypothetical-deductive reasoning and intuition, the latter based on pattern recognition (Eva, 2005; Croskerry, 2009). Cognitive psychology and information theory maintain that intuitive recognition is possible because the storage of diagnoses as mental constructs takes place in the form of typical frameworks (illness scripts), that is, compact lists of characteristics (Charlin et al., 2007). Clinical reasoning is not a static concept, yet it is a complex, non-linear multidimensional construct that is best learned over time using multiple learning methods at different stages of learners’ intellectual development (Mamede et al., 2007).
A recent systematic review (Xu et al., 2021) upgraded the knowledge about specific methods to improve clinical reasoning of students in the clinical setting, highlighting the role of reflection in developing the ability of clinical reasoning. Schaye et al. (2023) noted in an editorial how crucial it is to approach the diagnostic process through the prism of situativity because the relationship between the human decision-maker and their surroundings (context) is inexorably intertwined. This is the most relevant new theoretical contribution to the field.
The most common result of clinical reasoning is a diagnosis, that is the act of classification of the patient’s condition within a nosology class. Usually, in educational activities and in clinical exercises, students deal with the diagnosis of a single disease, mostly an acute one or the onset of a new chronic condition (Hawkes, 2012; McCartney et al., 2016). However, the current epidemiology of many countries shows an increasing prevalence of old people with more than one healthcare issue. Multimorbidity is the co-existence of at least two chronic diseases, it is common, and its prevalence and incidence are increasing in many countries (Kudesia et al., 2021). The presence of multiple intersecting diseases, characterized by signs and symptoms from multiple illness scripts further increase complexity and cognitive load, ultimately affecting the clinical reasoning process (Soh et al., 2020). The change of a patient’s overall condition over time (Vetrano et al., 2020) and the mutual impacts between the contemporaneous health conditions (McMillan and Hubbard, 2012) appear to be two concepts that are missing from the existing paradigm of diagnostic reasoning. A preliminary review of the literature revealed little and inconsistent information in this area. A systematic review in 2015 (Bogetz et al., 2015) identified 22 articles on educational interventions on chronic care, but most of them were on a single chronic condition and the studies did not consider clinical reasoning but rather focused the knowledge of the health care delivery system, the development of management and inter-disciplinary teamwork skill, or attitudes of students and residents toward chronic care. According to the same situational approach as Schaye et al. (2023), a recent study (Hughes, 2022) investigated the general practitioners’ reasoning process when managing patients with multimorbidity, identifying internal, external, and relationship-based elements.
The underlying assumptions in the Introduction lead to the conclusion that medical educators need both new pedagogies to encourage the development of cognitive abilities necessary in the management of patients with complicated trajectories of multimorbidity and theoretical models to describe the non-linear complexity of multimorbidity (Shi and Nambudiri, 2018). A special problem arises when chronic illness narratives reflect the passage of time, a crucial element (Consorti et al., 2023).
In this situation, we thought that a scoping review was the right method to fill this gap of knowledge and to describe constructs and methods in the education of clinical reasoning in patients with multimorbidity, with a particular interest for information technology-based methods. The review was aimed to examine if research in this field described a single learning outcome or more than one, and the kinds of methods of teaching, learning and assessment. Finally, we considered the possible research perspectives.
Hence, the research questions were:
– What is the definition of the construct of clinical reasoning in patients with chronic multimorbidity?
– What are the considered learning outcomes?
– What are the teaching and learning methods?
– In which special way can information technology help in developing clinical reasoning in multimorbidity?
– What are the research perspectives?
This article is compliant with the PRISMA-ScR checklist for scoping reviews (Tricco et al., 2018).
2. Methods
2.1. Population
After a brief search, we soon discovered that studies on a group of graduate students may also satisfy the research demand. Initially, we solely considered undergraduate medical students as the target demographic. As a result, we broadened our scope to incorporate both graduate and undergraduate students as well as practicing physicians. This choice was motivated by the first sample of retrieved publications, which adopted the same methodology and constructions for other professional groups. Because of this, we assumed that the issue of interest—also for its novelty—was common across all levels in medical education.
2.2. Concept
We searched for any kind of article or monograph dealing with education of clinical reasoning for patients with chronic multimorbidity. The supposed construct or competence is not clearly defined in literature, and this was one of the main reasons for this review. Nevertheless, we considered the ability of conceiving a complex clinical history over time, with multiple intersecting conditions, and the ability to foresee and manage the evolutions of the patient’s condition.
2.3. Context
As anticipated above, we searched for undergraduate, graduate, and continuing education, since we were interested in defining the construct of clinical reasoning in multimorbidity patients and related methods of education. To explore how information technology can support the development of clinical reasoning in multimorbidity patients, we also probed the technological domain of the application of methods and models of knowledge representation for temporal reasoning in medicine.
2.4. Eligibility criteria and source of information
Due to the exploratory nature of a scoping review, we searched any kind of publications, both from the bibliographic databases and the grey literature. A publication was selected if it reported about any kind of synthesis of research or an experimental study (observational, quasi-experimental, trial, qualitative research) or case study, commentaries, and editorials about the education of clinical reasoning in multimorbidity, including articles defining—as learning outcomes—the competencies for the clinical management of multimorbidity. Articles reporting the technological problems of representing the clinical knowledge used to manage a condition of multimorbidity were selected if they contained elements relevant to the research questions of this scoping review, especially when dealing with the representation of temporal relationships.
We excluded articles dealing with education to the management of a single chronic disease or pediatric conditions. We also excluded articles concerning only the competencies to manage organization and the system of resources to care for multimorbidity, or only communication skill, and articles only defining the concepts of multimorbidity and clinical complexity. Overall, if an article did not provide at least a perspective of education, it was excluded.
We accessed the following databases: Pubmed, Scopus, ERIC, and CORE for grey literature. The reference list of the retrieved reviews and other kinds of articles was also scanned.
Because scoping reviews are exploratory in nature and attempt to map all of the current literature that is accessible in a particular area of interest, we did not place time constraints on them (Maggio et al., 2021). An unbounded time restriction would also have allowed for the historical development of ideas and practices over time to be shown. The search was only conducted in English.
2.5. Selection and data charting
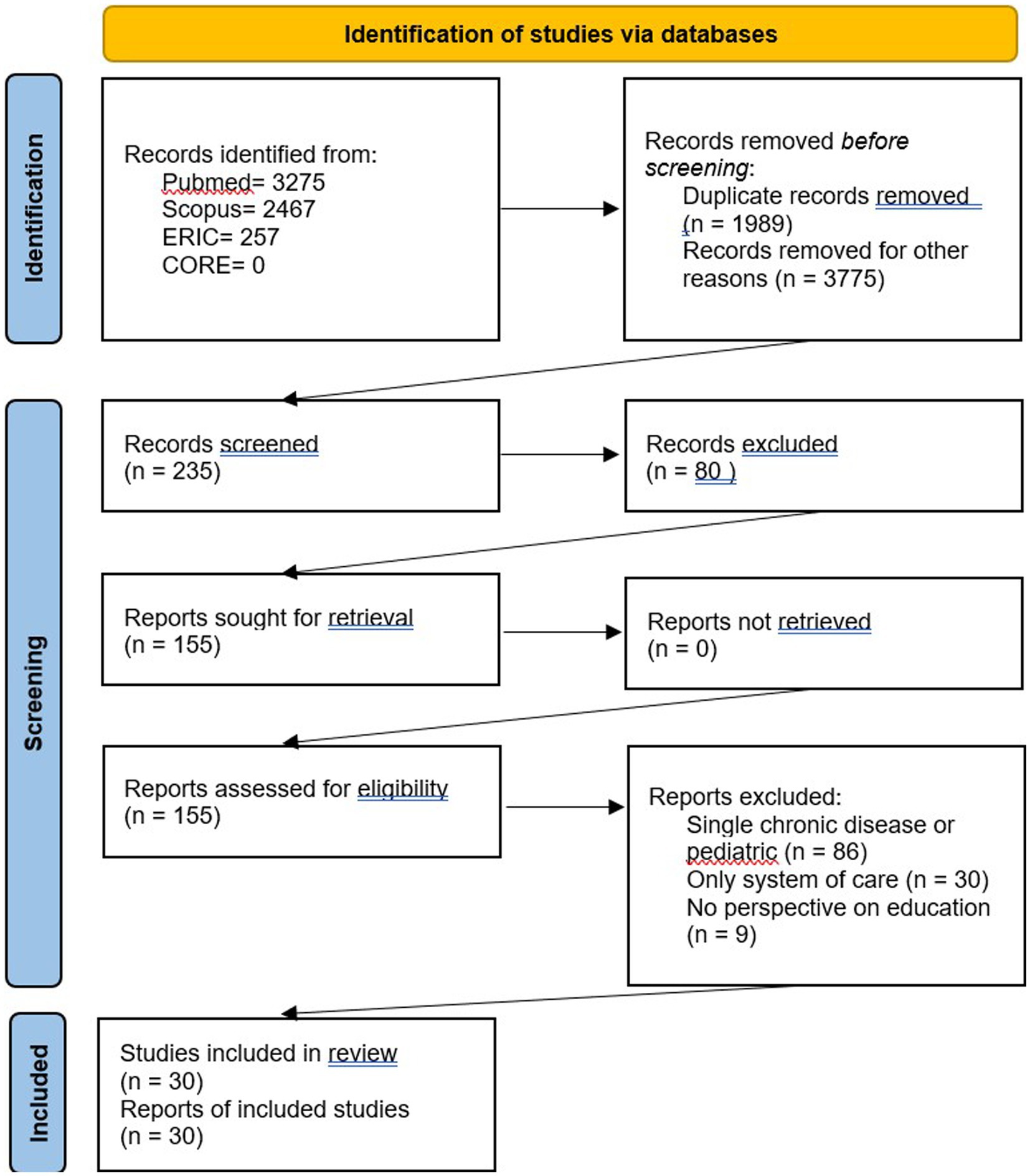
Together, FC and AL searched Pubmed, Scopus, ERIC, and CORE in the bibliographical databases. After importing all the retrieved articles into a bibliographic management application, duplicate articles were removed. The articles were divided into groups, and MB, AL, RM, CS, and LV (one group each) quickly reviewed their titles to eliminate any that were not pertinent. To assess the eligibility of the remaining articles, three groups of abstracts were produced, and two authors (LG joined the aforementioned authors in this phase) separately reviewed each group. The few cases of disagreement were handled under FC’s direction by discussion and agreement rather than by using a formal procedure. FC and LG periodically sought information from the other authors to identify uncertainty throughout the entire process.
The full text of the selected articles was read individually and then discussed in some joint meetings, to agree a final evaluation. In this phase no formal methods of agreement were used. Due to the exploratory intent of a scoping review, no quality assessment was done, but we extracted data from every selected article.
We used a form, shared in a virtual drive, to extract and store data. Each author was assigned a set of articles for data extraction, FC supervised the whole process. The items of the form are the columns of Table 1.
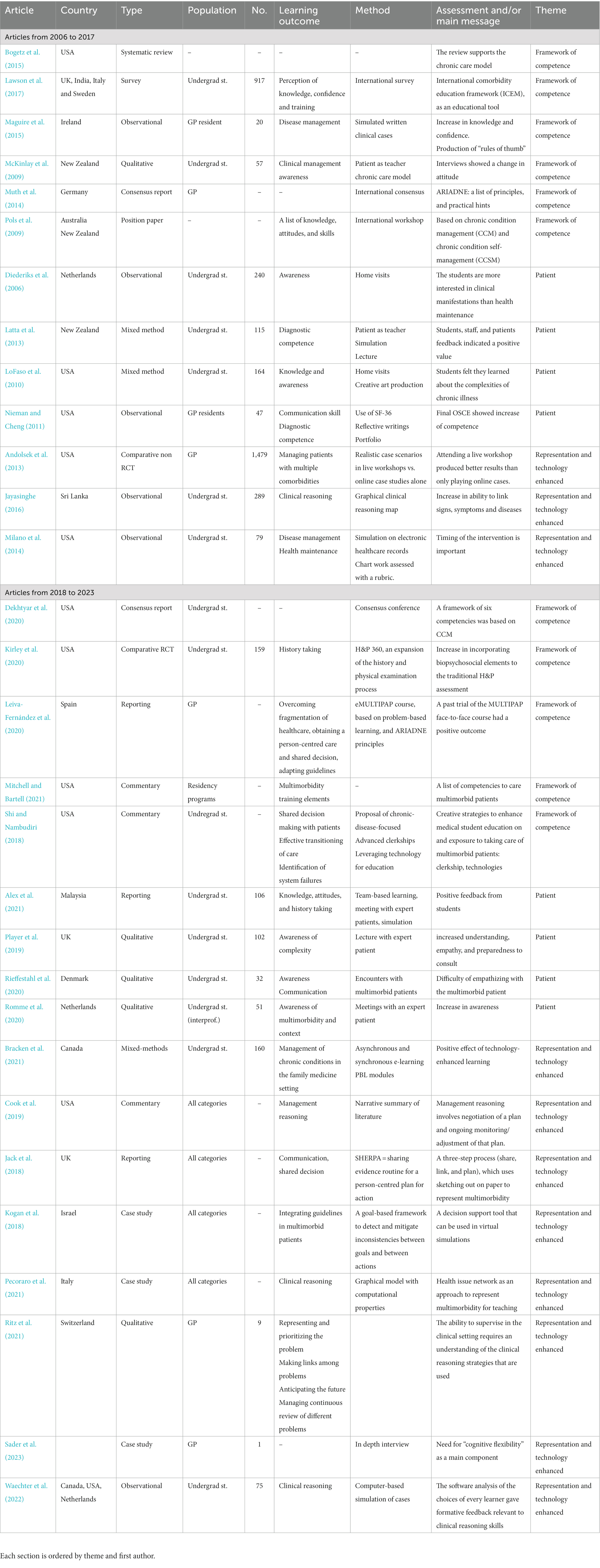
Table 1. The list of selected articles and their characteristics, divided in two sections (articles older than 5 years, articles of the last 5 years).
2.6. Data synthesis
In a series of meetings, we applied the same principles as in thematic analysis (Braun and Clarke, 2019) to abstract in an inductive way the themes from the itemized data. The themes and sub-themes were used to answer the research questions.
3. Results
The selection process is depicted in Figure 1. It resulted in 30 articles (see Table 1), that were thematized into three classes: the multimorbid patient as a teacher (8 articles), defining a framework of competence (11 articles), representing multimorbidity and related clinical reasoning (11 articles). In this last theme were also grouped studies using technology to enhance learning, with various ways to focus on the representation of the process of reasoning. Although we retrieved studies about temporal reasoning in medicine, no one was explicitly addressed to multimorbidity. Finally, we could not find any article in the grey literature.
3.1. Descriptive summary of the selected articles
Thirteen of the 30 selected articles (43.3%) were published before 2018, the remaining 17 (56.7%) between 2018 and 2023. The area of origin of the first author was Europe (13; 43.3%), USA (10; 33.3%), Australia-New Zealand (3; 10%), Asia (2; 6.7%), and Canada (2; 6.7%). Three of these articles were produced by an international collaboration.
Six articles were observational (20.0%), six case studies or reporting of single experience (20.0%), six position papers, consensus and commentary (20.0%), five qualitative research articles (16.7%), three mixed method and one survey that reported both quantitative and qualitative data (13.3%), and one systematic review (3.3%), that was included because it concluded with an endorsement of the chronic care model (CCM) (Wagner et al., 2001) as a preferred theoretical method to teach caring of multimorbid patients. We found only two comparative studies (6.7%).
Sixteen articles (53.3%) were about undergraduate students, five on general practitioners (16.7%), and four on residents or in general referred to all kinds of medical learners (13.3% each). Two articles (7.2%) were not clearly addressed to a category of learners.
3.2. The patient as a teacher
The most used educational methods to develop the clinical competencies needed to manage multimorbid patients was the live experience of the student meeting face to face real multimorbid patients—specially in their home environment—or simulated patients. More encounters or lectures with the expert patient were highly valued (Latta et al., 2013; Player et al., 2019; Romme et al., 2020; Alex et al., 2021). Expert patients are real chronic patient who attended a special training to become more aware of their condition and skilled to transform the knowledge of their illness into a positive input for medical students and young doctors in training. Home visits were also a useful context for understanding multimorbidity (Diederiks et al., 2006; LoFaso et al., 2010; Rieffestahl et al., 2020). The only study on residents (Nieman and Cheng, 2011) used a mix of reflective writings after patient’s encounters and a structured portfolio of activities, including the training to use SF-36, a multidimensional questionnaire to assess quality of life.
According to the chronological trend, the expert patient has just recently begun to gain popularity as a tool for improving communication skill, attitudes, and comprehension of the complexity of multimorbid conditions.
3.3. Frameworks of competence
This was the largest class of selected articles, grouping articles from 2009 to 2021 reporting a proposal of theoretical framework or a list of clinical competencies supporting healthcare for multimorbidity. Four (McKinlay et al., 2009; Pols et al., 2009; Bogetz et al., 2015; Dekhtyar et al., 2020) out of the 11 articles quoted the chronic care model (CCM) as the reference model for multimorbidity, to develop effective educational interventions. Other proposals were the International Comorbidity Education Framework (Lawson et al., 2017), and ARIADNE, a list of principles and practical hints (Muth et al., 2014; Leiva-Fernández et al., 2020). Finally, the remaining three articles reported a more limited set of learning outcomes (Maguire et al., 2015; Kirley et al., 2020; Mitchell and Bartell, 2021). One commentary, written by an undergraduate student (Shi and Nambudiri, 2018) recalled the core entrustable professional activities defined by the Association of American Medical Colleges.
The creation of a framework of competence for chronic care was the subject of more than half of the papers from 2006 to 2017 (7/13; 53.8%), mostly as a consequence of an international survey or consensus meeting. However, this subject was still covered in five of the seventeen (39.5%) publications that were published in the last 5 years.
3.4. Knowledge representation and technology-enhanced learning
The articles in this class were of relevance, because they reported some attempts to represent the process of clinical reasoning in multimorbidity and coherent methods to develop it. This is the reason why apparently different methods like hand drawings of diagrams and the use of technology are grouped together. Four articles reported of technology-based, case-based learning (Andolsek et al., 2013; Milano et al., 2014; Bracken et al., 2021; Waechter et al., 2022) as an effective way to simulate the process of reasoning and management of complex cases of multimorbidity. Interestingly, Milano et al. (2014) built their system on a simulated electronic medical record. Both this and Waechter’s systems were able to provide the learners an automated feedback, based on the data they used and the choices they did.
A quite different approach was adopted by Jack et al. (2018) with the SHERPA method (Sharing Evidence Routine for a Person-Centred Plan for Action), who designed and tested a three-step process (share, link, and plan), to sketch out on paper the representation of the situation of a multimorbid patient and the related plan of management. The same idea of graphical representation of a complex clinical situation underlay the proposal of Jayasinghe (2016) and Pecoraro et al. (2021). While the former is a developed kind of concept map, the latter is a formal approach with computational properties, based on Petri nets. The system was designed to represent the evolution of the patient’s condition over time and also includes a computer-assisted design environment to draw time-oriented diagrams. Kogan et al. (2018) tackled the problem of the conflict of guidelines for different diseases, which often occur in multimorbidity. Their system was designed to facilitate the integration of guidelines in multimorbid patients and can be used in virtual simulations.
Three last articles were included (Cook et al., 2019; Ritz et al., 2021; Sader et al., 2023), because they were the only retrieved articles that explicitly explored the way a general practitioner reasons when dealing with a multimorbid patient. Cook et al. (2019) proposed the concept of management reasoning, as the ability of “negotiation of a plan and ongoing monitoring/adjustment of that plan,” while Ritz et al. (2021) and Sader et al. (2023), from the same research group, reported the result of a qualitative study and an in-depth interview, highlighting the need for “cognitive flexibility” as a main component of clinical reasoning in multimorbidity, which has been described as composed by the abilities of representing and prioritizing the problem, making links among problems, anticipating the future, managing continuous review of different problems.
The number of articles discussing the use of technology-enhanced learning techniques has definitely increased over time, going from 3/13 (23.0%) of the oldest articles to 8/17 (47.0%) of the articles in the previous 5 years, showing a potential development trend.
4. Discussion
The results of this scoping review offer an answer to the research questions we posed, pointing out also the wide gaps of knowledge and practices in the domain of medical education to clinical reasoning in multimorbidity and suggesting direction for further research.
4.1. Construct and learning outcomes
This part of the Discussion aims to answer to the first two research questions.
A first contribution to explore the mental construct of clinical reasoning in multimorbidity came from Ritz et al. (2021) and Sader et al. (2023), and their contribution came from a series of interviews, not yet leading to a clear theoretical framework. In depth interviews have been the main method through which we built our present understanding of clinical reasoning, as described in short in the Introduction of this review (Eva, 2005; Croskerry, 2009). Unfortunately, that model of reasoning seems not to be adequate in multimorbidity, especially because it is addressed to reach a diagnosis, while in multimorbidity the diagnoses are often already known, and the clinical problem is managing the evolutions. A cross-sectional study on the epidemiology of multimorbidity (Barnett et al., 2012) concluded that “our findings challenge the single-disease framework by which most health care, medical research, and medical education is configured.” To a similar conclusion came Hughes (2022), who argued that there are three groups of factors involved in clinical reasoning and decision making in multimorbidity: internal factors of the individual, external factors (environment, context of the encounter) and relationship-based factors, linked to the process of collaborative planning with the patient. A second proposal of definition of the mental process at play when a clinician reasons of a case of multimorbidity is the concept of “management reasoning” (Cook et al., 2019) and the related construct of “management scripts” (Cook et al., 2023). Analogous to the illness scripts, already defined in the Introduction, a management script is a list of characteristics that, after the recognition of a pattern, is triggered and drives the process of thinking of the clinician. Hence, for Cook and his research group, the problem of multimorbidity is mainly a problem of management.
Even if an agreed definition of the construct of clinical reasoning in multimorbidity has not yet been reached, several proposals of framework of competencies for healthcare provision in multimorbidity has been designed. Overall, based on what we summarized in the previous paragraph, the competencies can be divided in three domains (Table 2): from a strictly clinical point of view, the ability of managing uncertainty, anticipating and detecting evolutions and conflicting guidelines, and setting priorities; from a relational point of view, the ability of communicating uncertainty and developing a feasible, shared plan of care with the patient; from an organizational point of view, the ability of managing the wide system of resources needed to take care of a multimorbid patient. This simple subdivision offers an important orientation to the choice of the teaching-learning methods and to the support technology can offer.

Table 2. Domains of competencies related to clinical reasoning in multimorbidity and aligned teaching/learning methods.
4.2. Methods of teaching and learning
If we consider the third research question and the three domains of competencies summarized in Table 2, Bigg’s principle of constructive alignment (Biggs, 1993) should drive the selection of the best method for every domain and sub-domain. In this theoretical perspective, every type of learning outcome should be “aligned” with the assessment method and, consequently, with the suitable teaching or learning method. Both the encounter with a real and an expert patient proved to be particularly effective in developing communication skills and awareness of the dimensions of multimorbidity. When real encounters were supplemented with reflective writings, this produced an increase in the learner’s awareness of what multimorbidity is. Case-based learning is the preferred method to increase competencies in the clinical domain, and technology can provide a multiplier effect. Finally, a combination of activities based on theoretical models of multimorbidity such as the CCM or ARIADNE and case-based learning, possibly played in inter-professional groups, are the aligned methods for the competencies in the management domain.
4.3. Technology-enhanced learning and perspectives of research
The last research question related to the role of information technology in developing clinical reasoning in multimobidity. The efficacy of computer-based simulation of clinical cases has been proven (Consorti et al., 2012), and some articles selected for this review confirmed this finding also for cases of multimorbidity (Andolsek et al., 2013; Milano et al., 2014; Bracken et al., 2021; Waechter et al., 2022), even if reaching conclusive evidence needs more comparative studies. What seems to be missing is the “sense of time lapse.” One of the key features of multimorbidity is that the overall condition of patients evolves over time (Vetrano et al., 2020). For a simulation of multimorbidity to be more effective, the learner must perceive the passage of time and the time-based interactions among the trajectories of the illnesses and their treatment.
Among the selected articles, traces of the concept of evolution over time are found in Diederiks et al. (2006) and LoFaso et al. (2010), who both quoted the “awareness” developed by their students after home visits. Nevertheless, awareness is an elusive construct that is difficult to define and assess, especially from an operational point of view. It could be awareness of the living condition of an old, multimorbid patient, of organizational issues and the availability of resources in the local healthcare system, or of the sequencing and time management of activities. A more robust proposal comes from Pecoraro et al. (2021). Their research group developed a syntax of evolutions of the health-related problems over time of the health issues of a patient (Ricci et al., 2022), such as “worsening,” “improving,” “complication,” “recurrence,” “examining in-depth” (i.e., moving from the occurrence of symptoms and signs to a diagnosis), “persistence,” and “cycle” (i.e., an alternance of acute and sub-acute or asymptomatic phases of a disease). They also modeled the coexistence and mutual influence among different health issues. As described in Section 3.4, the diagrams representing the story of a chronic patient are ordered over time. This model is still under development, and a recent article discusses its philosophical tenets (Consorti et al., 2023).
Adaptive e-learning is a broad term indicating methods and tools used in technology-assisted learning to support the different learning needs and styles of students (Gupta et al., 2020; Yakin and Linden, 2021). The main applications are in the field of formative assessment, and we found an example of adaptive learning in Waechter et al. (2022), in which the software analysis of the choices of every learner gave personalized formative feedback relevant to clinical reasoning skills.
In their review of ten years of international workshops on knowledge representation (KR) for health care (KR4HC), Riaño et al. (2019) summarized the main topics. Two of these topics are very interesting for the goal of this scoping review: temporal knowledge and reasoning and guideline integration for multimorbid patients. We suggest that these topics are relevant to designing and implementing a technology-assisted simulation environment in which a learner can experience a patient’s life-long time lapse, move forward and back over time, explore the interactions among diseases and social determinants, and possibly conflicting treatments to be prescribed according to the guidelines of the different diseases. Examples of the value of temporal reasoning in such an advanced simulation for clinical training are the work of van der Heijden and Lucas (2013), who, through Allen’s algebra, formally defined the seven basic relations that can hold between two-time intervals when describing a clinical case (before, meets, overlaps, starts, during, finishes, equals). Another example is the work of Kamišalić et al. (2018), who analyzed time constraints in a set of fifty real clinical procedures to detect possible conflicts with the constraints imposed by the clinical guidelines.
This review has the usual limitations of a scoping review. Despite the wide strategy of search, some relevant articles could have been missed, especially from the grey literature. As a scoping review, we did not assess the quality of the selected articles, because we were interested in detecting what topics and issues were present in this field of research. Hence, some of the reported articles could be of low value as evidence of effectiveness; they only testify that a researcher felt that a topic deserved attention. Our synthesis arose from a thematic analysis, and, as in all qualitative methods, a different perspective could have been adopted. Nevertheless, we think we provided enough interpretations and quotes to let the readers develop their own vision of the problems in the field of medical education and clinical reasoning in multimorbidity.
5. Conclusion
The increasing prevalence of multimorbidity in many countries is a challenge both from a healthcare and educational point of view. This review contributed by providing a better understanding of the current positions on the nature of clinical reasoning in multimorbidity and a synthesis of the knowledge about the methods of development of this construct. Suggested perspectives for research are toward a deeper understanding of the process of clinical reasoning from the point of view of cognitive psychology and education sciences. The need to simulate chronicity and the passage of time highlights the importance of developing methods and technologies to support a lively representation of the life-long experience of patients, embedded in a powerful environment of simulation equipped with temporal logics, natural language processing, and the ability to manage a graphical synthetic representation of the network of health-related problems and of their interactions, integrated with the flow of clinical activities and the relevant clinical guidelines. This kind of environment could also have gaming capabilities to provide a more engaging learning experience for the learners.
Author contributions
FC designed the review, defined the search strategy, supervised the process of selection, analysis and synthesis, and drafted the manuscript. LG cooperated to supervise the process of selection, analysis and synthesis, and edited the draft manuscript. MB, AL, RM, CS and LV did and refined the search and filled the forms for data extraction. All authors contributed to the article and approved the submitted version.
Funding
Funded under Erasmus+ KA220-HED—Cooperation partnership in higher education. ELPIS project 2021-1-IT02-KA220-000023205.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alex, D., Kumari, Y., and Kadirvelu, A. (2021). An experiential aged care module for first-year undergraduate medical students. Educ. Sci. 11:565. doi: 10.3390/educsci11100565
Andolsek, K., Rosenberg, M. T., Abdolrasulnia, M., Stowell, S. A., and Gardner, A. J. (2013). Complex cases in primary care: report of a CME-certified series addressing patients with multiple comorbidities. Int. J. Clin. Pract. 67, 911–917. doi: 10.1111/ijcp.12175
Barnett, K., Mercer, S. W., Norbury, M., Watt, G., Wyke, S., and Guthrie, B. (2012). Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 380, 37–43. doi: 10.1016/S0140-6736(12)60240-2
Biggs, J. B. (1993). From theory to practice: a cognitive systems approach. High. Educ. Res. Dev. 12, 73–85. doi: 10.1080/0729436930120107
Bogetz, J. F., Rassbach, C. E., Bereknyei, S., Mendoza, F. S., Sanders, L. M., and Braddock, C. H. (2015). Training health care professionals for 21st-century practice: a systematic review of educational interventions on chronic care. Acad. Med. 90, 1561–1572. doi: 10.1097/ACM.0000000000000773
Bracken, K., Levinson, A. J., Mahmud, M., Allice, I., Vanstone, M., and Grierson, L. (2021). Spiralling pre-clerkship concepts into the clinical phase: augmenting knowledge transfer using innovative technology-enhanced curriculum activities. Med. Sci. Educ. 31, 1607–1620. doi: 10.1007/s40670-021-01348-1
Braun, V., and Clarke, V. (2019). Reflecting on reflexive thematic analysis. Qual. Res. Sport Exerc. Health 11, 589–597. doi: 10.1080/2159676X.2019.1628806
Charlin, B., Boshuizen, H. P., Custers, E. J., and Feltovich, P. J. (2007). Scripts and clinical reasoning. Med. Educ. 41, 1178–1184. doi: 10.1111/j.1365-2923.2007.02924.x
Consorti, F., Mancuso, R., Nocioni, M., and Piccolo, A. (2012). Efficacy of virtual patients in medical education. A meta-analysis of randomized studies. Comput. Educ. 59, 1001–1008. doi: 10.1016/j.compedu.2012.04.017
Consorti, F., Torre, D., Luzi, D., Pecoraro, F., Ricci, F., and Tamburis, O. (2023). The challenge of clinical reasoning in chronic multimorbidity: time and interactions in the health issues network model. Diagnosis. doi: 10.1515/dx-2023-0041. [Epub ahead of print].
Cook, D. A., Durning, S. J., Sherbino, J., and Gruppen, L. D. (2019). Management reasoning: implications for health professions educators and a research agenda. Acad. Med. 94, 1310–1316. doi: 10.1097/ACM.0000000000002768
Cook, D. A., Stephenson, C. R., Gruppen, L. D., and Durning, S. J. (2023). Management reasoning: empirical determination of key features and a conceptual model. Acad. Med. 98, 80–87. doi: 10.1097/ACM.0000000000004810
Croskerry, P. (2009). A universal model of diagnostic reasoning. Acad. Med. 84, 1022–1028. doi: 10.1097/ACM.0b013e3181ace703
Dekhtyar, M., Colford, C., Whisenant, E., Huber, J., Johnson, E., Thomas, P., et al. (2020). Development of learning objectives to guide enhancement of chronic disease prevention and management curricula in undergraduate medical education. Teach. Learn. Med. 32, 241–249. doi: 10.1080/10401334.2020.1724791
Diederiks, J. P., Bosma, H., van Eijk, J. T., van Santen, M., Scherpbier, A., and van der Vleuten, C. (2006). Chronic patients in undergraduate education: didactic value as perceived by students. Med. Educ. 40, 787–791. doi: 10.1111/j.1365-2929.2006.02527.x
Eva, K. W. (2005). What every teacher needs to know about clinical reasoning. Med. Educ. 39, 98–106. doi: 10.1111/j.1365-2929.2004.01972.x
Gupta, S., Ojeh, N., Sa, B., Majumder, M. A. A., Singh, K., and Adams, O. P. (2020). Use of an adaptive e-learning platform as a formative assessment tool in the cardiovascular system course component of an MBBS programme. Adv. Med. Educ. Pract. 11, 989–996. doi: 10.2147/AMEP.S267834
Hawkes, N. (2012). Better training is needed to deal with increasing multimorbidity. BMJ 344:e3336. doi: 10.1136/bmj.e3336
Hughes, L. D. (2022). Understanding the processes behind the decisions—GPs and complex multimorbidity decision making. BMC Prim. Care 23:162. doi: 10.1186/s12875-022-01781-0
Jack, E., Maskrey, N., and Byng, R. (2018). SHERPA: a new model for clinical decision making in patients with multimorbidity. Lancet 392, 1397–1399. doi: 10.1016/S0140-6736(18)31371-0
Jayasinghe, S. (2016). Describing complex clinical scenarios at the bed-side: is a systems science approach useful? Exploring a novel diagrammatic approach to facilitate clinical reasoning. BMC Med. Educ. 16, 1–6. doi: 10.1186/s12909-016-0787-x
Kamišalić, A., Riaño, D., and Welzer, T. (2018). Formalization and acquisition of temporal knowledge for decision support in medical processes. Comput. Methods Prog. Biomed. 158, 207–228. doi: 10.1016/j.cmpb.2018.02.012
Kirley, K., Hayer, R., Khan, T., Johnson, E., Sanchez, E. S., Kosowicz, L., et al. (2020). Expanding the traditional history and physical examination to address chronic diseases and social needs: a multisite randomized control trial of 4 medical schools. Acad. Med. 95, S44–S50. doi: 10.1097/ACM.0000000000003640
Kogan, A., Tu, S. W., and Peleg, M. (2018). Goal-driven management of interacting clinical guidelines for multimorbidity patients. 2018 AMIA Annual Symposium Proceedings. AMIA Symposium, 690–699
Kudesia, P., Salimarouny, B., Stanley, M., Fortin, M., Stewart, M., Terry, A., et al. (2021). The incidence of multimorbidity and patterns in accumulation of chronic conditions: a systematic review. J Multimorb. Comorb. 11:26335565211032880. doi: 10.1177/26335565211032880
Latta, L., Tordoff, D., Manning, P., and Dent, J. (2013). Enhancing clinical skill development through an ambulatory medicine teaching programme: an evaluation study. Med. Teach. 35, 648–654. doi: 10.3109/0142159x.2013.801553
Lawson, C., Pati, S., Green, J., Messina, G., Strömberg, A., Nante, N., et al. (2017). Development of an international comorbidity education framework. Nurse Educ. Today 55, 82–89. doi: 10.1016/j.nedt.2017.05.011
Leiva-Fernández, F., Prados-Torres, J. D., Prados-Torres, A., Del-Cura-González, I., Castillo-Jimena, M., López-Rodríguez, J. A., et al. (2020). Training primary care professionals in multimorbidity management: educational assessment of the eMULTIPAP course. Mech. Ageing Dev. 192:111354. doi: 10.1016/j.mad.2020.111354
LoFaso, V. M., Breckman, R., Capello, C. F., Demopoulos, B., and Adelman, R. D. (2010). Combining the creative arts and the house call to teach medical students about chronic illness care. J. Am. Geriatr. Soc. 58, 346–351. doi: 10.1111/j.1532-5415.2009.02686.x
Maggio, L. A., Larsen, K., Thomas, A., Costello, J. A., and Artino, A. R. (2021). Scoping reviews in medical education: a scoping review. Med. Educ. 55, 689–700. doi: 10.1111/medu.14431
Maguire, S., Hanley, K., Quinn, K., Sheeran, J., and Stewart, P. (2015). Teaching multimorbidity management to GP trainees: a pilot workshop. Educ. Prim. Care 26, 410–415. doi: 10.1080/14739879.2015.1101848
Mamede, S., Schmidt, H. G., and Rikers, R. (2007). Diagnostic errors and reflective practice in medicine. J. Eval. Clin. Pract. 13, 138–145. doi: 10.1111/j.1365-2753.2006.00638.x
McCartney, M., Treadwell, J., Maskrey, N., and Lehman, R. (2016). Making evidence-based medicine work for individual patients. BMJ 353:i2452. doi: 10.1136/bmj.i2452
McKinlay, E., McBain, L., and Gray, B. (2009). Teaching and learning about chronic conditions management for undergraduate medical students: utilizing the patient-as-teacher approach. Chronic Illn. 5, 209–218. doi: 10.1177/1742395309343812
McMillan, G. J., and Hubbard, R. E. (2012). Frailty in older inpatients: what physicians need to know. QJM 105, 1059–1065. doi: 10.1093/qjmed/hcs125
Milano, C. E., Hardman, J. A., Plesiu, A., Rdesinski, R. E., and Biagioli, F. E. (2014). Simulated electronic health record (Sim-EHR) curriculum: teaching EHR skills and use of the EHR for disease management and prevention. Acad. Med. 89, 399–403. doi: 10.1097/ACM.0000000000000149
Mitchell, K. B., and Bartell, S. (2021). Multimorbidity and resident education. Fam. Med. 53, 531–534. doi: 10.22454/FamMed.2021.106319
Muth, C., van den Akker, M., Blom, J. W., Mallen, C. D., Rochon, J., Schellevis, F. G., et al. (2014). The ARIADNE principles: how to handle multimorbidity in primary care consultations. BMC Med. 12:223. doi: 10.1186/s12916-014-0223-1
Nieman, L. Z., and Cheng, L. (2011). Chronic illness needs educated doctors: an innovative primary care training program for chronic illness education. Med. Teach. 33, e340–e348. doi: 10.3109/0142159X.2011.558532
Pecoraro, F., Ricci, F. L., Consorti, F., Luzi, D., and Tamburis, O. (2021). The friendly health issue network to support computer-assisted education for clinical reasoning in multimorbidity patients. Electronics 10:2075. doi: 10.3390/electronics10172075
Player, E., Gure-Klinke, H., North, S., Hanson, S., Lane, D., Culyer, G., et al. (2019). Humanising medicine: teaching on tri-morbidity using expert patient narratives in medical education. Educ. Prim. Care 30, 368–374. doi: 10.1080/14739879.2019.1670097
Pols, R. G., Battersby, M. W., Regan-Smith, M., Markwick, M. J., Lawrence, J., Auret, K., et al. (2009). Chronic condition self-management support: proposed competencies for medical students. Chronic Illn. 5, 7–14. doi: 10.1177/1742395308098888
Riaño, D., Peleg, M., and Ten Teije, A. (2019). Ten years of knowledge representation for health care (2009-2018): topics, trends, and challenges. Artif. Intell. Med. 100:101713. doi: 10.1016/j.artmed.2019.101713
Ricci, F. L., Consorti, F., Pecoraro, F., Luzi, D., and Tamburis, O. (2022). A petri-net-based approach for enhancing clinical reasoning in medical education. IEEE Trans. Learn. Technol. 15, 167–178. doi: 10.1109/TLT.2022.3157391
Rieffestahl, A. M., Risør, T., Mogensen, H. O., Reventlow, S., and Morcke, A. M. (2020). Ignitions of empathy. Medical students feel touched and shakened by interacting with patients with chronic conditions in communication skills training. Patient Educ. Couns. 104, 1668–1673. doi: 10.1016/j.pec.2020.12.015
Ritz, C., Sader, J., Cairo Notari, S., Lanier, C., Caire Fon, N., Nendaz, M., et al. (2021). Multimorbidity and clinical reasoning through the eyes of GPs: a qualitative study. Fam. Med. Community Health 9:e000798. doi: 10.1136/fmch-2020-000798
Romme, S., Bosveld, M. H., Van Bokhoven, M. A., De Nooijer, J., Van den Besselaar, H., and Van Dongen, J. J. J. (2020). Patient involvement in interprofessional education: a qualitative study yielding recommendations on incorporating the patient’s perspective. Health Expect. 23, 943–957. doi: 10.1111/hex.13073
Sader, J., Diana, A., Coen, M., Nendaz, M., and Audétat, M. C. (2023). A GP’s clinical reasoning in the context of multimorbidity: beyond the perception of an intuitive approach. Fam. Pract. 40, 113–118. doi: 10.1093/fampra/cmac076
Schaye, V., Parsons, A. S., Graber, M. L., and Olson, A. P. J. (2023). The future of diagnosis—where are we going? Diagnosis 10, 1–3. doi: 10.1515/dx-2023-0003
Shi, C. R., and Nambudiri, V. E. (2018). Time for an acute focus on chronic care in undergraduate medical education. Acad. Med. 93, 835–838. doi: 10.1097/ACM.0000000000002177
Soh, M., Konopasky, A., Durning, S. J., Ramani, D., McBee, E., Ratcliffe, T., et al. (2020). Sequence matters: patterns in task-based clinical reasoning. Diagnosis 7, 281–289. doi: 10.1515/dx-2019-0095
Tricco, A. C., Lillie, E., Zarin, W., O'Brien, K. K., Colquhoun, H., Levac, D., et al. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 169, 467–473. doi: 10.7326/M18-0850
van der Heijden, M., and Lucas, P. J. (2013). Describing disease processes using a probabilistic logic of qualitative time. Artif. Intell. Med. 59, 143–155. doi: 10.1016/j.artmed.2013.09.003
Vetrano, D. L., Roso-Llorach, A., Fernández, S., Guisado-Clavero, M., Violán, C., Onder, G., et al. (2020). Twelve-year clinical trajectories of multimorbidity in a population of older adults. Nat. Commun. 11:3223. doi: 10.1038/s41467-020-16780-x
Waechter, J., Allen, J., Lee, C. H., and Zwaan, L. (2022). Development and pilot testing of a data-rich clinical reasoning training and assessment tool. Acad. Med. 97, 1484–1488. doi: 10.1097/ACM.0000000000004758
Wagner, E. H., Austin, B. T., Davis, C., Hindmarsh, M., Schaefer, J., and Bonomi, A. (2001). Improving chronic illness care: translating evidence into action. Health Aff. 20, 64–78. doi: 10.1377/hlthaff.20.6.64
Xu, H., Ang, B. W. G., Soh, J. Y., and Ponnamperuma, G. G. (2021). Methods to improve diagnostic reasoning in undergraduate medical education in the clinical setting: a systematic review. J. Gen. Intern. Med. 36, 2745–2754. doi: 10.1007/s11606-021-06916-0
Keywords: clinical reasoning, multimorbidity, temporal reasoning, simulation, scoping review
Citation: Consorti F, Borcea MC, Laca A, Melcarne R, Scorziello C, Ventrone L and Giacomelli L (2023) Education of clinical reasoning in patients with multimorbidity: a scoping review and perspectives for technology-enhanced learning. Front. Educ. 8:1202360. doi: 10.3389/feduc.2023.1202360
Edited by:
Clifford A. Shaffer, Virginia Tech, United StatesReviewed by:
Keerti Singh, The University of the West Indies, Cave Hill, BarbadosCarol Nash, University of Toronto, Canada
Copyright © 2023 Consorti, Borcea, Laca, Melcarne, Scorziello, Ventrone and Giacomelli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fabrizio Consorti, ZmFicml6aW8uY29uc29ydGlAdW5pcm9tYTEuaXQ=
 Fabrizio Consorti
Fabrizio Consorti Maria Carola Borcea1
Maria Carola Borcea1 Rossella Melcarne
Rossella Melcarne Laura Giacomelli
Laura Giacomelli