
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Educ. , 03 August 2023
Sec. Digital Learning Innovations
Volume 8 - 2023 | https://doi.org/10.3389/feduc.2023.1200879
Background: There are various methods for teaching surgery to undergraduate students. Lecture-based learning (LBL) is a teacher-centered approach that comprehensively, accurately, and systematically conveys knowledge. Team-based, case-based, and problem-based learning methods are student-centered approaches that increase student enthusiasm and subject-related motivation. However, the COVID-19 pandemic disrupted conventional methods for teaching surgery to undergraduate students and its impact continues even today. This research investigates a variety of surgical teaching strategies and suggests optimal strategies for undergraduate students, especially within the context of the COVID-19 crisis.
Methods: Various teaching methods in undergraduate medical education that have emerged over the last 5 years are reviewed and analyzed, specifically those used for surgical training during the COVID-19 pandemic.
Results: Traditional in-person teaching methods have been replaced by novel approaches that increase efficiency, including social media adoption, simulation-based training, flipped-classroom concepts, and “Hand as Foot” teaching. However, traditional and novel approaches can be combined to teach students the fundamentals of science and basic surgical skills, which include incision, suturing and drainage, and chest tube insertion. Each method has its advantages and disadvantages under certain circumstances.
Conclusion: Several alternative teaching strategies and a combination of methods can complement traditional face-to-face learning, promoting the successful dissemination of academic knowledge and the improvement of clinical surgical skills in terms of objectivity, time-efficiency, and feasibility. The effects of the COVID-19 pandemic on the learning context can provide a reference for future teaching in response to unavoidable emergencies.
Medical student education is a vital responsibility entrusted to surgeons associated with medical schools (Emanuel, 2020). Undergraduate medical education (UME) programs should equip all graduating medical students with core knowledge and skills to become qualified general practitioners (Theodoulou et al., 2018). UME has changed in ways that reflect significant trends in education and healthcare. Some changes include new expectations of surgical teachers, education quality, and patient safety; staff shortages and time constraints in surgical teams; a shift to competency-based education; and the establishment of commissionable professional activities (Acton, 2015). Thus, surgical educators must modify their approaches to course curricula.
Undergraduate surgery is at a major crossroads; many departments face difficulties in delivering effective teaching (Baker et al., 2015), particularly during the COVID-19 pandemic (Imediegwu et al., 2022). Examples include the significant impact of the pandemic on the didactic and clinical components of undergraduate surgical training in South-Eastern Nigeria (Imediegwu et al., 2022), student self-confidence in Italy (Francesca et al., 2023), and the availability of personnel and time to produce teaching materials in Germany (Mielke et al., 2023) and Ireland (Curran et al., 2022). Furthermore, the field of surgery is developing rapidly; therefore, students must be proficient in basic surgical training (Sideris et al., 2017). One study found that only 8% of medical students pursued a career in surgery (Prideaux and Marshall, 1994). Thus, more efficient teaching methods are needed to encourage students to choose surgical specialties. Traditional teaching involves gaining basic surgical knowledge through books, lectures, and apprenticeships, and putting this knowledge to use in the operating theater (Dinsmore and North, 2000). However, challenges remain, including budgetary constraints, complex diseases, ethical restrictions, and concerns about patient safety when inexperienced residents and students perform procedures (Bauer et al., 2014). In response, novel methods and technological advancements demonstrating significant efficacy alone or in combination are continually emerging; for example, 3D printing, cadaver surgery, live surgery, and virtual simulation (Hu et al., 2018).
This review examines the advantages and disadvantages of undergraduate surgical education methods (Supplementary Table S1). It investigates (1) novel teaching methods for surgical learning that emerged in the past 5 years, and (2) how an effective combination of teaching methods can maximize student learning, providing tailored education to suit different students’ needs in various surgical specialties.
Lecture-based learning (LBL) is teacher-centered. The teacher imparts knowledge, which is passively received by students (Zhao et al., 2020). LBL relies on the availability of educational materials and the experience and skill of the lecturer (Chotiyarnwong et al., 2021). In one study, 106 students were randomly divided into an LBL-only group (control group) and one that integrated LBL with clinical problem-based learning (PBL); it demonstrated that the combination of the LBL and PBL approaches led to a deeper understanding and more effective use (p < 0.05) of burn-surgery knowledge, with students viewing it more favorably than in the case of LBL alone (Yao et al., 2020). Nevertheless, LBL relies heavily on teaching materials, skills, availability, and experience, with students receiving insufficient opportunities for analysis, practical application, and development of spatial and visual conversion abilities (Nawabi et al., 2021; Wang et al., 2022).
Case-based learning (CBL) emphasizes the discussion of patient cases (Muthukrishnan et al., 2019) based on the analysis of medical records. It is designed to represent real clinical settings and motivate students to recognize and expand new areas of learning. CBL facilitates self-learning through increased real-world relevance and understanding of concepts, problem-solving abilities, and the cultivation of students’ rigorous logical reasoning (Muthukrishnan et al., 2019; Zhao et al., 2020). Students apply fundamental biomedical knowledge to specific patient cases and overall clinical case management (Gartmeier et al., 2019). In a retrospective study, blending lectures and case workshops enhanced the learning climate (Sundbom et al., 2021). Moreover, students enjoy CBL courses, which teach a variety of problem-solving approaches while also stimulating a sense of active learning and competence (Nessler et al., 2021). In a 2023 study regarding online case-based surgical training series in Trauma & Orthopedics, over 90% of participants improved their skills and knowledge and expanded the scope of their surgical training (Brennan et al., 2023). However, in larger lecture environments, its utility may be limited (Pearson et al., 2018).
Effective learning environments should emphasize a culture where problem-solving skills, operative skills (Kronenfeld et al., 2022), critical thinking, and judgments are enhanced (White et al., 2004). PBL, a student-focused approach, prioritizes these. Trainees are assigned to groups of a maximum of eight students without the direct guidance of a tutor. This approach guides students to address issues via self-study, research, discussion, and collaboration within the group (Yao et al., 2020). In a prospective randomized trial including 175 medical students, PBL scored higher on the post-training multiple-choice examination than LBL for teaching theoretical surgery courses (p = 0.048) (Davari et al., 2021). PBL also promotes enjoyment and intrinsic motivation toward active learning, prompting students to adopt a deep learning approach (Dolmans et al., 2016). However, PBL is designed to be a hands-off approach—the teacher promotes group problem-solving and facilitates interaction through the use of non-directive questioning, but without lecturing or giving the answers (Dolmans et al., 2016; Yao et al., 2020).
Flipped learning (FL) inverts conventional classroom-centered learning. Students study the material before class, while face-to-face sessions focus on solving group problems and applying what they have learned (Tune et al., 2013). In a prospective non-randomized controlled trial, holistic FL teaching was viable in both medical and surgical education covering digestive disorders and otorhinolaryngology (Dombrowski et al., 2018). This approach improved student satisfaction, class attendance, academic outcomes (Hernandez-Guerra et al., 2021), and instructor time management compared to traditional learning (Barrett et al., 2022).
FL can assist students in gaining suture skills in various areas, particularly with their affective (β = 0.413, p < 0.001), psychomotor (β = 0.399, p < 0.001), and cognitive skills (β = 0.526, p < 0.001) (Wu et al., 2018). A randomized controlled trial focused on electrocardiogram (ECG) learning reported that flipped-classroom instruction resulted in the experimental group scoring higher in ECG interpretation compared with the control group (8.72 ± 1.01 vs. 8.03 ± 1.01, p < 0.001). The FL group invested more time learning before class than the control group did (42.33 ± 22.19 vs. 30.55 ± 10.15, t = 4.586, p < 0.001) (Rui et al., 2017).
This model has advantages and disadvantages. One advantage is that it integrates the benefits of face-to-face in-classroom instruction (e.g., teacher and peer engagement, applied problem-solving, collaborative learning) and internet-driven instruction (including self-regulated learning and digital video together with online discussions) (He et al., 2019). In terms of viability, time efficiency, and objectivity, FL may be superior to direct observations of surgical skills and clinical performance (Bock et al., 2020). Ultimately, students who received combined traditional teaching and digital media education (namely, FL) were better prepared to implement procedural skills than those who received only traditional teaching (Kraut et al., 2019). However, for FL to be successful, faculty must invest time in the preparation of materials prior to class, resulting in higher labor and material costs for their employers (Kraut et al., 2019).
Team-based learning (TBL) utilizes teamwork and in-depth critical reasoning; it requires pre-class study and integrates collaborative and active learning (Anas et al., 2022). TBL combines aspects of PBL and FL by having a single instructor conduct multiple group discussions. Teams work together to develop concepts and apply them to problem-solving activities in a single classroom (Lafleur et al., 2021; Yaqoob et al., 2021). Ideally, instructors create diverse groups of five to seven students (Shiels et al., 2017). The main TBL components include individual preparation (before class), readiness assurance (in class), application of concepts (small-group peer learning to complete tasks and student-assisted learning—in class), and long-term retention of knowledge (Sakamoto et al., 2020; Burgess et al., 2022). The learning content, objectives, and relevant resources are provided to each student 1 week before the lesson (Shiels et al., 2017). TBL helps students fulfill course-learning objectives and determine ways to be part of a team; students interact in the classroom and develop a sense of personal responsibility and teamwork behavior (Daou et al., 2022). The scores of the TBL group were considerably higher compared to the traditional self-directed learning group in a quasi-experimental study on undergraduate surgical education (74.70 ± 6.81 vs. 63.77 ± 4.18, p < 0.01) (Sim et al., 2023). However, TBL asks students to stick to the study before the class (Anas et al., 2022).
In simulation-based training (SBT), surgeons commonly divide the study material into various classification schemes: animal/non-animal, partial task/procedure, or virtual/real (Acton, 2015). Basic technical-skill task simulators and animated laboratories have been incorporated into the educational curricula of surgical students to teach fundamental surgical skills and procedures. Two examples of these include an abdominal cavity simulator (Ferreira Filho et al., 2018) and a simulator for corneal rust ring removal (Mednick et al., 2017). A prospective, randomized, blinded trial reported SBT as more effective (p < 0.001) and a more straightforward, intuitive, and easily understood approach (p < 0.001) than textbook learning, resulting in superior learning (p < 0.001) (Plana et al., 2019). Virtual simulations have been incorporated into operative procedure training, including otorhinolaryngology (Hardcastle and Wood, 2018), cesarean sections (Acosta et al., 2020), urology (Williams et al., 2021), and ophthalmology (Deuchler et al., 2022). Nevertheless, several challenges remain, such as the inaccessibility of virtual simulation teaching resources, the lack of infrastructure, the “decoupling” of users from reality, and the necessity to enhance student engagement and motivation (Wu et al., 2022). One study indicated that virtual reality might not be suitable for students with low visuospatial ability, while physical models might enable better learning, irrespective of visuospatial ability (Pang et al., 2021). In a retrospective survey study of a new type of informed consent module in virtual undergraduate surgical clerkship, a virtual module utilizing standardized patient and faculty communication skills training enhanced beliefs about students’ self-efficacy in gaining informed consent (p < 0.01) (Pang et al., 2021).
A single-center cohort study of 1,178 undergraduate students revealed that simulation-based medical education considerably increased students’ theoretical or practical achievement (p < 0.001), doctor-patient communication (improvement rate of 56.3%), and humanistic care (improvement rate of 69.2%) compared with the control group. In simulation-based medical education groups, the students were inclined to assign more time to interact with others (Wang et al., 2021).
Simulations utilizing standardized patients [defined as “a layperson trained to portray a patient, family member, and others in realistic and repeatable ways to provide practice” (Kim and De Gagne, 2018)] are widely used in UME, mainly for teaching physical diagnostic skills that involve anogenital and pelvic examinations (Low et al., 2015).
Robotic surgery is uncommon among final-year medical students; however, exposure to simulated robotic surgery allows a better understanding of related challenges, including depth perception and economy of motion (Naik and Mandal, 2020). The robotic simulator delivers a wider range of property measurements than other technologies, which allows students to improve their learning curve. It also enables doctors to communicate with patients promptly and effectively, further inspiring the next generation of robotic surgeons (Naik and Mandal, 2020).
Limitations of SBT, nonetheless, include financial barriers and fidelity (Nataraja et al., 2020). Surgical simulation research is frequently underpowered, due to considerable heterogeneity, while effective utilization of simulation requires the adequacy of all major factors, namely, trained educators, training resources, as well as the institutionalization of the curriculum (Miller et al., 2019; Mandal and Ojha, 2020; Iqbal et al., 2021).
The COVID-19 pandemic led universities worldwide to switch to distance learning despite constrained resources and preparation (Schlegl et al., 2020). Accordingly, online virtual teaching (e-learning) is now extensively accepted and expected by medical students. These technologies are essential for otolaryngology–head and neck surgery (Fung, 2015), surgical anatomy (Abi-Rafeh et al., 2021), urology (Margolin et al., 2021), neurosurgery (Hoffman et al., 2022), and plastic surgery (Koljonen et al., 2022) curricula, offering enhanced learning (Imai et al., 2022). In a study comparing in-person vs. virtual courses, no variations were observed in the efficacy of teachers preparing their students for oral examinations (6.4 vs. 6.8, p = 0.58) or National Board of Medical Examiners evaluations (6.2 vs. 6.7, p = 0.46) in the context of the COVID-19 crisis (Kronenfeld et al., 2021); this confirms that e-education sufficiently prepares students for exams (Kronenfeld et al., 2021).
Augmented reality (AR) offers a live representation of real-world environments while incorporating extra computer-generated elements (Luck et al., 2021). Online surgical education courses applying AR have been successfully delivered during the particularly challenging COVID-19 pandemic (Luck et al., 2021; Grady et al., 2022). This demonstrates that, when access to operating rooms is restricted, computer-based virtual education can be an effective and realistic alternative to traditional textbooks and face-to-face teaching (Kumins et al., 2021; Schmitz et al., 2021).
However, when the task is less demanding, the usefulness of AR applications is limited; for example, to fit particular task requirements, which include physical stress on the participant (weight > 500 g) and tissue disruption across the case (Tagaytayan et al., 2018; Gsaxner et al., 2021; Luck et al., 2021; Plewan et al., 2021; Tanzer et al., 2022). Besides, video-guided learning methods are inadequate for teaching surgical skills compared with those that use expert or peer feedback (Tejos et al., 2021). The SSuRF (Scene, Surgery, Reflection, and Feedback) method can assist in peer-led surgical training (Gracie et al., 2021). It enables peers, particularly those without adequate formal educational training, to use a structured format to teach junior students, which is then documented in workplace-based evaluations (Kennedy, 2022). Peer-assisted learning can improve average scores in many areas (Pinter et al., 2021), such as those included in the World Health Organization (WHO) Surgical Safety Checklist (+3.94), scrubbing (+2.99), gowning/gloving (+3.34), knot tying (+5.53), interrupted sutures (+5.89), continuous sutures (+6.53), vertical mattress sutures (+6.46), and local anesthesia (+3.73) (Bennett et al., 2018). Additionally, the effectiveness of a new system of interactive education with an emphasis on urological procedures can motivate student interest in surgery, demonstrating efficient surgical education within the operating room (Nakayama et al., 2016).
The Essential Skills in the Management of the Surgical Case (ESMSC) masterclass is another effective and innovative three-day multi-disciplinary teaching format for the international undergraduate surgical masterclass; it effectively improves students’ objective behavior in basic surgical skills (Sideris et al., 2018). During the global financial crisis of the National Health Service of the UK, the ESMSC model provided free, high-quality surgical education and subsequently developed into the Integrated Generation 4 (iG4) model via a dynamic feedback mechanism (Sideris et al., 2018). The iG4 curricula were built largely on the distinctive characteristics of the ESMSC, inviting a wide range of students from various educational backgrounds and enhancing interaction and the exchange of knowledge among them. iG4 concepts set the stage for a standardized, replicable, and novel effort to generate an undergraduate surgical skillset (Sideris et al., 2020).
In one study, participants with musical experience outperformed non-musicians on the Mini-Profile of Music Perception Skills test (p = 0.015), particularly in the speed of laparoscopic staple transfer (p < 0.01), suture quality (p < 0.03), and dexterity of the dominant hand (p = 0.05) (Sun et al., 2021). Dexterity together with the Mini-Profile of Music Perception Skills score had a predictive effect on suture quality (p < 0.01). In a case–control study of the COVID-19 pandemic, students undergoing an online surgical skills learning course performed comparably to those receiving traditional face-to-face tutoring in surgical skills, with average scores between 4 and 5 for both (Co et al., 2021).
The “Hand as Foot” teaching innovation refers to anatomical relationships, where clinical knowledge can be intuitively grasped and explained using the simplest gestures with hands and feet (Cui et al., 2020). It integrates the changes in the limb skeleton with clinical teaching in orthopedic education, which strengthens simulation and metaphor in teaching (He et al., 2021). This approach has been applied to ulnar olecranon fracture and patellar fracture surgery (Sun and Liu, 2021), spinal surgery (Chang et al., 2021), lumbar puncture (Xin et al., 2021), transcavernous sinuscranial nerve surgery (Zhang et al., 2021), thyroid surgery (Han et al., 2022), nursing, and rehabilitation interventions, among others (Guo et al., 2021). A point-by-point and integrated curriculum is formed by comparing the associated knowledge points of the upper and lower limbs. This new teaching model stimulates students’ interest while also enhancing their ability to think proactively; furthermore, it improves teaching, learning efficiency, student self-esteem, and sense of medical responsibility (Zhang Y. et al., 2022).
Game-based training is increasingly practiced in various areas of healthcare because it provides students with experiential learning and can be adapted to individual ability and progress (Akbari et al., 2022). In one study, average theoretical test scores were considerably higher in the game training group (n = 27) than those in the lecture training group (n = 24) post-training (p = 0.040) (Akbari et al., 2022).
A randomized controlled trial reported video-assisted peer feedback as a feasible and cost-effective alternative to the qualified instructor feedback typically employed in medical education (Boecker et al., 2022). In another approach, students’ performance regarding objectively assessed surgical skills was enhanced and their confidence was boosted following a two-week multi-modal surgical boot camp (Bevilacqua et al., 2020). Finally, animation can facilitate facial transplant education; it improved performance scores (p = 0.029), confidence, and satisfaction (p < 0.001) compared with learning via text resources (Wolfe et al., 2021).
Online and offline learning approaches can be combined to create blended training modules that help undergraduate surgery students develop fundamental knowledge and basic surgical skills (Agarwal, 2020). Blended learning—also referred to as hybrid learning/inverted learning—can combine traditional face-to-face learning and synchronous Internet and digital media, catering to trainee-specific learning styles (Engel, 2014; Liu et al., 2016; Senkoylu et al., 2021). Relevant examples include PBL and CBL in thyroid surgery (Zhao et al., 2020), a classroom response system with FL and TBL (Malekigorji and Hatahet, 2020), virtual and AR in plastic surgery (Sayadi et al., 2019), a step-by-step method and CBL in otoendoscopy (Wei et al., 2021), and traditional approaches and PBL, algorithms, mind maps, and peer discussion (Ahmad and Asif, 2018) (Figure 1; Table 1).
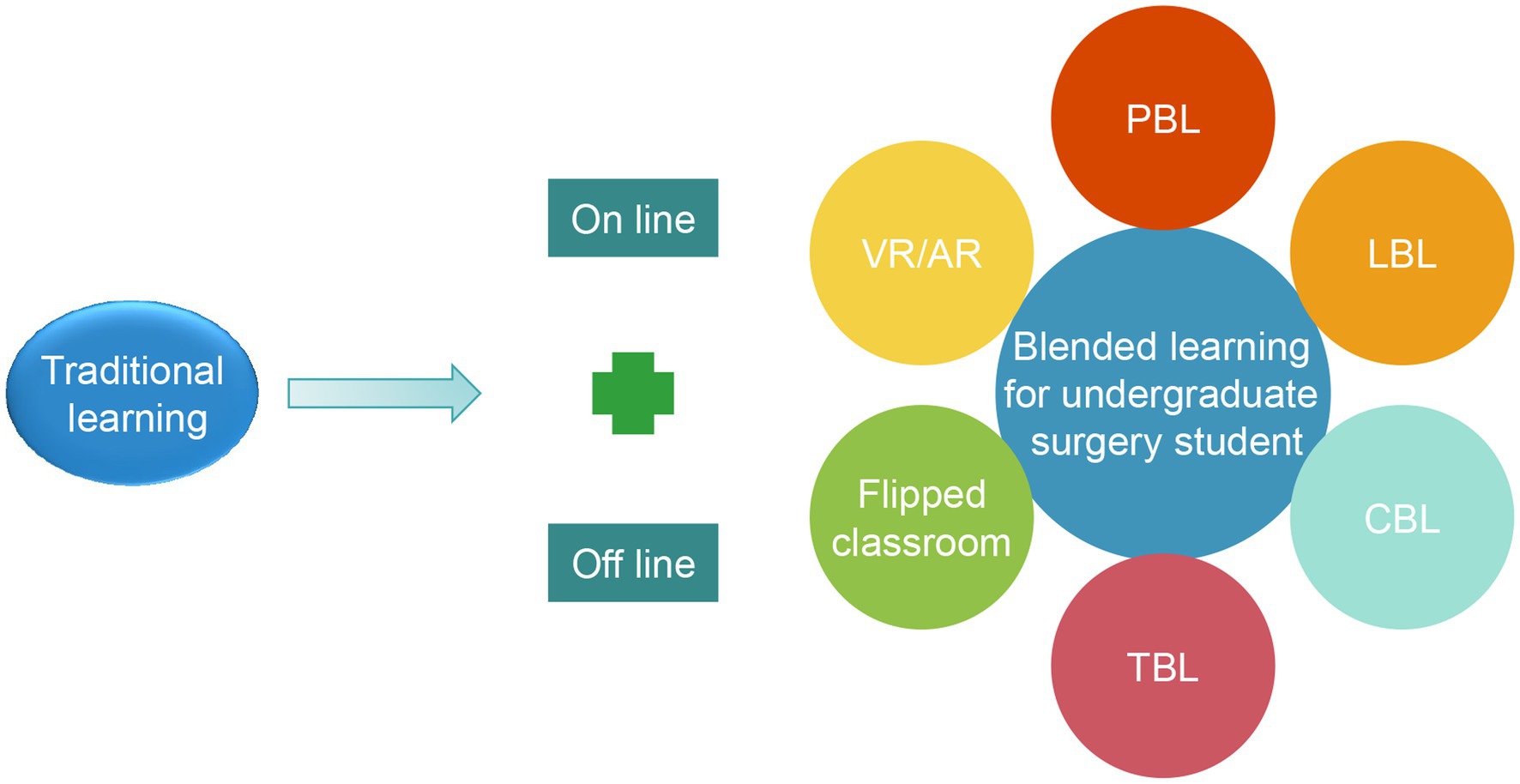
Figure 1. Online and offline blended methods can effectively supplement traditional courses for undergraduate surgical students. LBL, lecture-based learning; TBL, team-based learning; CBL, case-based learning; PBL, problem-based learning; AR, augmented reality; VR, virtual reality.
Mixed reality, the fusion of the physical and digital worlds, can result in increased precision and efficiency along with better outcomes (Sayadi et al., 2019). Virtual reality entirely substitutes the real world with a digital setting, while AR superimposes computer-generated content (i.e., video or graphics) onto the physical landscape. Additionally, the effectiveness of contemporary face-to-face teaching compared with blended learning has been explored (Jawaid et al., 2021). The average objective structured clinical examination score for face-to-face learners was (78.01 ± 13.29) compared with (85.12 ± 13.77) for blended learners (p = 0.49); thus, the blended surgical learning approach was more effective than the single-face-to-face teaching method.
Scores from the Operative Performance Rating System revealed that a surgical boot camp, which prepares senior medical students for anatomy education with surgical simulation practice, improved students’ surgical skills, which included instrumentation, incision, peripheral tissue (vascular and nerve) handling, and general surgical smoothness (all p < 0.01) (Zhang J. et al., 2022). Furthermore, a combination of step-by-step and CBL methods improved professional knowledge and otoendoscopic skills (p < 0.05) more than the combination of LBL and CBL in otoendoscopic surgery (Wei et al., 2021). It bolstered interest in learning, competence in surgery, mobility in surgery, and satisfaction with the learning experience (p < 0.05).
A meta-analysis demonstrated that a clever integration of conventional and PBL methods may deliver the most effective training for undergraduate surgical clerks (Chang et al., 1995). A hybrid online and offline teaching approach may become the optimal pedagogy for the training of surgery students, especially in the post-pandemic era (Su, 2022).
In general, blended learning, which includes virtual teaching approaches, should be exploited along with conventional teaching environments to deliver real-time, face-to-face surgical skills training, and essential theoretical knowledge to students (Koljonen et al., 2022).
Surgical education is a crucial component of the UME curriculum. Traditional teaching methods, adopting social media platforms, SBT, the flipped-classroom concept, “Hand as Foot” teaching, and multi-modal systems can be useful in undergraduate surgical training. As the impacts of COVID-19 are more evident, virtual teaching has become normalized. It is recommended that various teaching methods should be combined and multimedia and networking technology should be applied based on their circumstantial suitability (Supplementary Table S2). Web-based distance training approaches can be consolidated to create undergraduate surgical training programs. For example, flipped classroom concepts and social media platforms should be created to supplement in-person lectures; including undergraduate surgical students participating in a telemedicine consultation as an alternative to a didactic clinic; and high-end surgical videos and multi-modal computer programs can be used to learn essential surgical skills. This blended teaching approach should emphasize students’ subjective motivation and cultivate their innovative spirit.
It is important to note that blended learning, “Hand as Foot” teaching, as well as other distance-learning models for mitigating the loss of face-to-face learning time should be considered as an adjunct, but not a substitute, for an authentic experience in the post COVID-19 pandemic era. Furthermore, 55.8% of the 181 medical students indicated they were exposed to substantially fewer general surgical cases [Field (Imediegwu et al., 2022)]. Consequently, the modalities and syllabus of surgical training for medical students should be flexibly recalibrated through remote online platforms to adapt to inevitable events, such as a pandemic.
Factors to be considered include the learner, learning goals, technology genre, and team-based module development. Innovative teaching approaches, namely, the SSuRF method, ESMSC model, and “Hand as Foot” teaching, have a high acceptance rate among teachers and students. Nevertheless, some of these are in the early stages of exploration. Medical education practitioners should continue to innovate, share, and implement valuable medical student education methods in the future (Guo et al., 2021).
QZ and YZ: conceptualization and writing—review and editing. LZ and YZ: methodology and software. LZ: investigation and writing—original draft preparation. YZ and QZ: supervision. All authors contributed to the article and approved the submitted version.
This study was supported by the National Natural Science Foundation (grant number: 82202989); the Regional Innovation Cooperation Project of the Sichuan Science and Technology Program (grant number: 2021YFQ0029); the China Postdoctoral Science Foundation (grant number: 2022M722279); the Sichuan Science and Technology Program (2023YFS0163); the Postdoctoral Research Project of West China Hospital, Sichuan University, Chengdu, China (grant number: 2021HXBH045); Fundamental Research Funds for the Central Universities (2022SCU12063, awarded to LZ); the Sichuan University Postdoctoral Interdisciplinary Innovation Fund (awarded to LZ).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/feduc.2023.1200879/full#supplementary-material
Abi-Rafeh, J., Safran, T., and Gilardino, M. S. (2021). Development and implementation of an online virtual teaching curriculum for the continuity of undergraduate medical education in surgical anatomy. Plast. Reconstr. Surg. 148, 528e–529e. doi: 10.1097/PRS.0000000000008290
Acaroglu, E., Assous, M., Bransford, R., Dal Oglio Da Rocha, L. G., Falavigna, A., France, J., et al. (2022). Evaluation of blended online learning in three spinal surgery educational courses. J. Eur. CME 11:2014042. doi: 10.1080/21614083.2021.2014042
Acosta, T., Sutton, J. M., and Dotters-Katz, S. (2020). Improving Learners' comfort with cesarean sections through the use of high-fidelity, low-cost simulation. MedEdPORTAL 16:10878. doi: 10.15766/mep_2374-8265.10878
Acton, R. D. (2015). The evolving role of simulation in teaching surgery in undergraduate medical education. Surg. Clin. North Am. 95, 739–750. doi: 10.1016/j.suc.2015.04.001
Agarwal, P. K. (2020). A combined approach in prolonged COVID-19 pandemic to teach undergraduate surgery students-future primary care physicians. J. Fam. Med. Prim Care 9, 5480–5483. doi: 10.4103/jfmpc.jfmpc_1129_20
Ahmad, H. N., and Asif, M. (2018). Medical student's learning habits: a mixed method study during clinical rotation in general surgery. J. Pak. Med. Assoc. 68, 600–605.
Akbari, F., Nasiri, M., Rashidi, N., Zonoori, S., Amirmohseni, L., Eslami, J., et al. (2022). Comparison of the effects of virtual training by serious game and lecture on operating room novices' knowledge and performance about surgical instruments setup: a multi-center, two-arm study. BMC Med. Educ. 22:268. doi: 10.1186/s12909-022-03351-5
Anas, S., Kyrou, I., Rand-Weaver, M., and Karteris, E. (2022). The effect of online and in-person team-based learning (TBL) on undergraduate endocrinology teaching during COVID-19 pandemic. BMC Med. Educ. 22:120. doi: 10.1186/s12909-022-03173-5
Baker, R. C., Spence, R. A., Boohan, M., Dorman, A., Stevenson, M., Kirk, S. J., et al. (2015). A novel approach to improve undergraduate surgical teaching. Ulster Med. J. 84, 30–36.
Barrett, G., Seniors, R., Okoli, J., Chase, A., Henry, B., Mubasher, M., et al. (2022). Validation of use of flipped classroom for surgery Core clerkships. J. Surg. Educ. 79, 668–675. doi: 10.1016/j.jsurg.2021.12.005
Bauer, F., Rommel, N., Kreutzer, K., Weitz, J., Wagenpfeil, S., Gulati, A., et al. (2014). A novel approach to teaching surgical skills to medical students using an ex vivo animal training model. J. Surg. Educ. 71, 459–465. doi: 10.1016/j.jsurg.2014.01.017
Bennett, S. R., Morris, S. R., and Mirza, S. (2018). Medical students teaching medical students surgical skills: the benefits of peer-assisted learning. J. Surg. Educ. 75, 1471–1474. Epub 2018/04/15. doi: 10.1016/j.jsurg.2018.03.011
Bevilacqua, L. A., Simon, J., Rutigliano, D., Sorrento, J., Wackett, A., Chandran, L., et al. (2020). Surgical boot camp for fourth-year medical students: impact on objective skills and subjective confidence. Surgery 167, 298–301. doi: 10.1016/j.surg.2019.06.041
Bock, A., Heitzer, M., Lemos, M., Peters, F., Elvers, D., Kniha, K., et al. (2020). "flipped OR": a modified didactical concept for a surgical clerkship in Oral and maxillofacial surgery. Br. J. Oral Maxillofac. Surg. 58, 1245–1250. doi: 10.1016/j.bjoms.2020.03.008
Boecker, A. H., Bank, C., Kim, B. S., Aman, M., Pears, K. H., Klasen, M., et al. (2022). Video-assisted peer teaching for surgical skills training - innovative potential for the medical curriculum and beyond: a randomized controlled trial. J. Surg. Educ. 79, 441–451. doi: 10.1016/j.jsurg.2021.10.008
Brennan, J. N., Hall, A. J., and Baird, E. J. (2023). Online case-based educational meetings can increase knowledge, skills, and widen access to surgical training:the nationwideVirtualTrauma & Orthopaedic Meetingseries. Surgeon. doi: 10.1016/j.surge.2023.02.005
Burgess, A. W., Luscombe, G. M., and Ramsey-Stewart, G. (2022). An intensive anatomy by whole-body dissection elective: a longitudinal study. Clin. Anat. 35, 550–559. doi: 10.1002/ca.23861
Chang, G., Cook, D., Maguire, T., Skakun, E., Yakimets, W. W., and Warnock, G. L. (1995). Problem-based learning: its role in undergraduate surgical education. Can. J. Surg. 38, 13–21.
Chang, Q., Liu, R., Zhao, J., and Wang, H. (2021). Application of "hand as foot" teaching method in spinal surgery teaching. Asian J. Surg. 44, 587–589. doi: 10.1016/j.asjsur.2020.12.030
Chotiyarnwong, P., Boonnasa, W., Chotiyarnwong, C., and Unnanuntana, A. (2021). Video-based learning versus traditional lecture-based learning for osteoporosis education: a randomized controlled trial. Aging Clin. Exp. Res. 33, 125–131. doi: 10.1007/s40520-020-01514-2
Co, M., Chung, P. H., and Chu, K. M. (2021). Online teaching of basic surgical skills to medical students during the COVID-19 pandemic: a case-control study. Surg. Today 51, 1404–1409. doi: 10.1007/s00595-021-02229-1
Cui, X., Liu, R., Zhao, J., Li, Y., and Nian, L. (2020). "hand as foot" teaching method in brachial plexus anatomy: an orthopedics teaching experience. Asian J. Surg. 43, 1113–1114. doi: 10.1016/j.asjsur.2020.08.004
Curran, S., O'Brien, D., and Kerin, M. (2022). A lecture series - neurosurgery in an Irish medical school without an associated neurosurgical Centre. Br. J. Neurosurg. 36, 372–376. doi: 10.1080/02688697.2021.2024505
Daou, D., Chakhtoura, M., El-Yazbi, A., Mukherji, D., Sbaity, E., Refaat, M. M., et al. (2022). Teaching critical appraisal to large classes of undergraduate medical students using team-based learning versus group discussions: a randomized controlled trial. BMC Med. Educ. 22:77. doi: 10.1186/s12909-022-03145-9
Davari, F. V., Teymouri, F., Amoli, H. A., Mojtabavi, H., Sharifi, A., Alaeddini, F., et al. (2021). Problem-based learning as an effective method for teaching theoretical surgery courses to medical students. J. Educ. Health Promot. 10:477. doi: 10.4103/jehp.jehp_266_21
Deuchler, S., Scholtz, J., Ackermann, H., Seitz, B., and Koch, F. (2022). Implementation of microsurgery simulation in an ophthalmology clerkship in Germany: a prospective, exploratory study. BMC Med. Educ. 22:599. doi: 10.1186/s12909-022-03634-x
Dinsmore, R. C., and North, J. H. (2000). Basic skin flaps for the general surgeon: a teaching method. South. Med. J. 93, 783–786. doi: 10.1097/00007611-200093080-00008
Dolmans, D., Loyens, S. M. M., Marcq, H., and Gijbels, D. (2016). Deep and surface learning in problem-based learning: a review of the literature. Adv. Health Sci. Educ. Theory Pract. 21, 1087–1112. doi: 10.1007/s10459-015-9645-6
Dombrowski, T., Wrobel, C., Dazert, S., and Volkenstein, S. (2018). Flipped classroom frameworks improve efficacy in undergraduate practical courses - a quasi-randomized pilot study in otorhinolaryngology. BMC Med. Educ. 18:294. doi: 10.1186/s12909-018-1398-5
Emanuel, E. J. (2020). The inevitable reimagining of medical education. JAMA 323, 1127–1128. doi: 10.1001/jama.2020.1227
Engel, A. (2014). Hybrid learning: to blend, flip, and interact. Color. Dis. 16, 325–326. doi: 10.1111/codi.12621
Ferreira Filho, F., Moura Junior, L. G., Rocha, H. A. L., Rocha, S., Ferreira, L. F. P., and Ferreira, A. F. P. (2018). Abdominal cavity simulator for skill progression in videolaparoscopic sutures in Brazil. Acta Cir. Bras. 33, 75–85. doi: 10.1590/s0102-865020180010000008
Francesca, Z., Luca, R., Andrea, P., Davide, P., and Nicoletta, Z. (2023). Clinical activities suspended: how the COVID-19 affected the self-confidence of Italian dental students. Eur. J. Dent. Educ. doi: 10.1111/eje.12894
Fung, K. (2015). Otolaryngology--head and neck surgery in undergraduate medical education: advances and innovations. Laryngoscope 125, S1–S14. doi: 10.1002/lary.24875
Gartmeier, M., Pfurtscheller, T., Hapfelmeier, A., Grunewald, M., Hausler, J., Seidel, T., et al. (2019). Teacher questions and student responses in case-based learning: outcomes of a video study in medical education. BMC Med. Educ. 19:455. doi: 10.1186/s12909-019-1895-1
Gracie, D. J., Winter, G., and Clarke, M. C. C. (2021). Improving undergraduate education in surgical paediatrics using near-peer assisted learning tutorials. Scott. Med. J. 66, 84–88. doi: 10.1177/0036933021994256
Grady, Z. J., Gallo, L. K., Lin, H. K., Magod, B. L., Coulthard, S. L., Flink, B. J., et al. (2022). From the operating room to online: medical student surgery education in the time of COVID-19. J. Surg. Res. 270, 145–150. doi: 10.1016/j.jss.2021.08.020
Gsaxner, C., Pepe, A., Li, J., Ibrahimpasic, U., Wallner, J., Schmalstieg, D., et al. (2021). Augmented reality for head and neck carcinoma imaging: description and feasibility of an instant calibration, Markerless Approach. Comput. Methods Prog. Biomed. 200:105854. doi: 10.1016/j.cmpb.2020.105854
Guo, J., Liu, R., Cui, X., Zhang, Y., Zou, D., Nian, L., et al. (2021). Application of "hand as foot teaching method" in rehabilitation medicine of venous thrombosis after orthopedic surgery. Asian J. Surg. 44, 572–573. doi: 10.1016/j.asjsur.2020.12.035
Han, Y., Bi, Y., Zhao, C., and Xu, S. (2022). The "hand as foot" teaching method in thyroid surgery. Asian J. Surg. 45, 1279–1280. doi: 10.1016/j.asjsur.2022.01.122
Hardcastle, T., and Wood, A. (2018). The utility of virtual reality surgical simulation in the undergraduate otorhinolaryngology curriculum. J. Laryngol. Otol. 132, 1072–1076. doi: 10.1017/S0022215118002025
He, B., Li, Q., Zhao, J., Liu, R., Li, Y., and Xu, Y. (2021). The innovation and practice of "hand as foot teaching method" in the teaching of motion system injury course. BMC Med. Educ. 21:553. doi: 10.1186/s12909-021-02944-w
He, Y., Lu, J., Huang, H., He, S., Ma, N., Sha, Z., et al. (2019). The effects of flipped classrooms on undergraduate pharmaceutical marketing learning: a clustered randomized controlled study. PLoS One 14:e0214624. doi: 10.1371/journal.pone.0214624
Hernandez-Guerra, M., Quintero, E., Morales-Arraez, D. E., Carrillo-Pallares, A., Nicolas-Perez, D., Carrillo-Palau, M., et al. (2021). Comparison of flipped learning and traditional lecture method for teaching digestive system diseases in undergraduate medicine: a prospective non-randomized controlled trial. Med. Teach. 43, 463–471. doi: 10.1080/0142159X.2020.1867312
Hickmann, A. K., Ferrari, A., Bozinov, O., Stienen, M. N., and Ostendorp, C. (2022). Neurosurgery resident training using blended learning concepts: course development and participant evaluation. Neurosurg. Focus. 53:E13. doi: 10.3171/2022.5.FOCUS22193
Hoffman, S. E., Vega, R. A., and Stippler, M. (2022). Teaching through the screen: a toolbox for creating a virtual neurosurgical subinternship program. Neurosurg. Focus. 53:E7. doi: 10.3171/2022.5.FOCUS22171
Hu, M., Wattchow, D., and de Fontgalland, D. (2018). From ancient to avant-Garde: a review of traditional and modern multimodal approaches to surgical anatomy education. ANZ J. Surg. 88, 146–151. Epub 2017/09/19. doi: 10.1111/ans.14189
Imai, T., Tanaka, Y., Hatanaka, Y., Suetsugu, T., Sato, Y., Matsuhashi, N., et al. (2022). Incorporation of virtual reality in the clinical training of medical students studying esophageal and mediastinal anatomy and surgery. Surg. Today 52, 1212–1217. doi: 10.1007/s00595-022-02457-z
Imediegwu, K. U., Onwuka, P. C., Uwaezuoke, A. C., Abor, J. C., and Oladiran, A. (2022). Effects of Covid-19 pandemic on the surgical training of final year medical students in south-eastern Nigeria. J. West Afr. Coll. Surg. 12, 64–70. doi: 10.4103/jwas.jwas_129_22
Iqbal, M. H., Khan, O., and Aydin, A. (2021). Editorial commentary: simulation-based training in Orthopaedic surgery: current evidence and limitations. Arthroscopy 37, 1008–1010. doi: 10.1016/j.arthro.2020.12.003
Jawaid, M., Baig, L., and Aly, S. M. (2021). Comparison of OSCE scores of surgical clinical education after face-to-face vs. blended learning methods among undergraduate medical students. J. Pak. Med. Assoc. 71, 1535–1539. doi: 10.47391/JPMA.571
Jeganathan, S., and Fleming, P. S. (2020). Blended learning as an adjunct to tutor-led seminars in undergraduate orthodontics: a randomised controlled trial. Br. Dent. J. 228, 371–375. doi: 10.1038/s41415-020-1332-1
Kennedy, L. (2022). Peer training in surgery: the SSuRF model approach. Surgeon 20, e187–e194. doi: 10.1016/j.surge.2021.06.004
Kim, S. S., and De Gagne, J. C. (2018). Instructor-led vs. peer-led debriefing in preoperative care simulation using standardized patients. Nurse Educ. Today 71, 34–39. doi: 10.1016/j.nedt.2018.09.001
Koljonen, V., Puolakkainen, P., and Helenius, I. (2022). Lessons learned from COVID-19 pandemic in undergraduate surgical education. Scand. J. Surg. 111:14574969221083138. doi: 10.1177/14574969221083138
Kraut, A. S., Omron, R., Caretta-Weyer, H., Jordan, J., Manthey, D., Wolf, S. J., et al. (2019). The flipped classroom: a critical appraisal. West. J. Emerg. Med. 20, 527–536. doi: 10.5811/westjem.2019.2.40979
Kronenfeld, J. P., Ryon, E. L., Kronenfeld, D. S., Hui, V. W., Rodgers, S. E., Thorson, C. M., et al. (2021). Medical student education during COVID-19: electronic education does not decrease examination scores. Am. Surg. 87, 1946–1952. doi: 10.1177/0003134820983194
Kronenfeld, J. P., Saberi, R. A., Cioci, A. C., Urrechaga, E. M., Ryon, E. L., Thorson, C. M., et al. (2022). Implementation of a surgical problem-based learning curriculum: a one-year single-center experience. Am. Surg. 89:31348211068014, 1807–1813. doi: 10.1177/00031348211068014
Kumins, N. H., Qin, V. L., Driscoll, E. C., Morrow, K. L., Kashyap, V. S., Ning, A. Y., et al. (2021). Computer-based video training is effective in teaching basic surgical skills to novices without faculty involvement using a self-directed, sequential and incremental program. Am. J. Surg. 221, 780–787. doi: 10.1016/j.amjsurg.2020.08.011
Lafleur, A., Rousseau-Gagnon, M., Cote-Maheux, M., Tremblay-Laroche, D., Rene De Cotret, P., and Caumartin, Y. (2021). Three weeks of team-based leaning do not overload undergraduate students. Med. Sci. Educ. 31, 1369–1378. doi: 10.1007/s40670-021-01314-x
Liu, Q., Peng, W., Zhang, F., Hu, R., Li, Y., and Yan, W. (2016). The effectiveness of blended learning in health professions: systematic review and Meta-analysis. J. Med. Internet Res. 18:e2. doi: 10.2196/jmir.4807
Low, E., Tessler, R., Hauer, K. E., Leavitt, A. D., Miller, B., and Maa, J. (2015). The surgical clerkship and medical student performance in a standardized patient case of acute cholecystitis. J. Surg. Educ. 72, 1045–1051. doi: 10.1016/j.jsurg.2015.04.019
Luck, J., Gosling, N., and Saour, S. (2021). Undergraduate surgical education during COVID-19: could augmented reality provide a solution? Br. J. Surg. 108, e129–e130. doi: 10.1093/bjs/znaa159
Malekigorji, M., and Hatahet, T. (2020). Classroom response system in a super-blended learning and teaching model: individual or team-based learning? Pharmacy (Basel) 8:197. doi: 10.3390/pharmacy8040197
Mandal, I., and Ojha, U. (2020). Training in interventional radiology: a simulation-based approach. J. Med. Educ. Curric. Dev. 7:2382120520912744. doi: 10.1177/2382120520912744
Margolin, E. J., Gordon, R. J., Anderson, C. B., and Badalato, G. M. (2021). Reimagining the away rotation: a 4-week virtual subinternship in urology. J. Surg. Educ. 78, 1563–1573. doi: 10.1016/j.jsurg.2021.01.008
Mednick, Z., Tabanfar, R., Alexander, A., Simpson, S., and Baxter, S. (2017). Creation and validation of a simulator for corneal rust ring removal. Can. J. Ophthalmol. 52, 447–452. doi: 10.1016/j.jcjo.2017.02.024
Mielke, A. M., Ghanem, M., Back, D. A., Frohlich, S., Herbstreit, S., and Seemann, R. J. (2023). Medical studies in times of a pandemic - concepts of digital teaching for Orthopaedics and trauma at german universities. BMC Med. Educ. 23:257. doi: 10.1186/s12909-023-04213-4
Miller, Z. A., Amin, A., Tu, J., Echenique, A., and Winokur, R. S. (2019). Simulation-based training for interventional radiology and opportunities for improving the educational paradigm. Tech. Vasc. Interv. Radiol. 22, 35–40. doi: 10.1053/j.tvir.2018.10.008
Muthukrishnan, S. P., Chandran, D. S., Afreen, N., Bir, M., Dastidar, S. G., Jayappa, H., et al. (2019). Planning, implementation, and evaluation of multicomponent, case-based learning for first-year Indian medical undergraduates. Adv. Physiol. Educ. 43, 504–511. doi: 10.1152/advan.00080.2019
Naik, R., and Mandal, I. (2020). Robotic simulation experience in undergraduate medical education: a perspective. J. Robot. Surg. 14, 793–794. doi: 10.1007/s11701-020-01059-6
Nakayama, T., Numao, N., Yoshida, S., Ishioka, J., Matsuoka, Y., Saito, K., et al. (2016). A novel interactive educational system in the operating room--the IE system. BMC Med. Educ. 16:44. doi: 10.1186/s12909-016-0561-0
Nataraja, R. M., Oo, Y. M., Ljuhar, D., Webb, N. R., Pacilli, M., Win, N. N., et al. (2020). Overview of a novel paediatric surgical simulation-based medical education programme in Myanmar. ANZ J. Surg. 90, 1925–1932. doi: 10.1111/ans.16200
Nawabi, S., Bilal, R., and Javed, M. Q. (2021). Team-based learning versus traditional lecture-based learning: an investigation of students' perceptions and academic achievements. Pak. J. Med. Sci. 37, 1080–1085. doi: 10.12669/pjms.37.4.4000
Nessler, J., Schaper, E., and Tipold, A. (2021). Proof of concept: game-based Mobile learning-the first experience with the app Actionbound as case-based geocaching in education of veterinary neurology. Front. Vet. Sci. 8:753903. doi: 10.3389/fvets.2021.753903
Pang, J. H., Finlay, E., Fortner, S., Pickett, B., and Wang, M. L. (2021). Teaching effective informed consent communication skills in the virtual surgical clerkship. J. Am. Coll. Surg. 233, 64–72e2. doi: 10.1016/j.jamcollsurg.2021.04.026
Pearson, S. C., Eddlemon, T., Kirkwood, M., and Pate, A. (2018). Are fishbowl activities effective for teaching pharmacotherapy and developing postformal thought in pharmacy students? A pilot study. Curr. Pharm. Teach. Learn. 10, 1070–1075. doi: 10.1016/j.cptl.2018.05.009
Pinter, Z., Kardos, D., Varga, P., Kopjar, E., Kovacs, A., Than, P., et al. (2021). Effectivity of near-peer teaching in training of basic surgical skills - a randomized controlled trial. BMC Med. Educ. 21:156. doi: 10.1186/s12909-021-02590-2
Plana, N. M., Rifkin, W. J., Kantar, R. S., David, J. A., Maliha, S. G., Farber, S. J., et al. (2019). A prospective, randomized, blinded trial comparing digital simulation to textbook for cleft surgery education. Plast. Reconstr. Surg. 143, 202–209. doi: 10.1097/PRS.0000000000005093
Plewan, T., Mattig, B., Kretschmer, V., and Rinkenauer, G. (2021). Exploring the benefits and limitations of augmented reality for palletization. Appl. Ergon. 90:103250. doi: 10.1016/j.apergo.2020.103250
Prideaux, D. J., and Marshall, V. R.. A "common" surgery curriculum: health care delivery and undergraduate surgical education in Australian teaching hospitals. World J. Surg. (1994) 18:657–661; discussion 6. doi: 10.1007/BF00298892
Rui, Z., Lian-Rui, X., Rong-Zheng, Y., Jing, Z., Xue-Hong, W., and Chuan, Z. (2017). Friend or foe? Flipped classroom for undergraduate electrocardiogram learning: a randomized controlled study. BMC Med. Educ. 17:53. doi: 10.1186/s12909-017-0881-8
Sakamoto, S. R., Dell'Acqua, M. C. Q., Abbade, L. P. F., Caldeira, S. M., Fusco, S. F. B., and Avila, M. A. G. (2020). Team-based learning: a randomized clinical trial in undergraduate nursing. Rev. Bras. Enferm. 73:e20180621. doi: 10.1590/0034-7167-2018-0621
Sayadi, L. R., Naides, A., Eng, M., Fijany, A., Chopan, M., Sayadi, J. J., et al. (2019). The new frontier: a review of augmented reality and virtual reality in plastic surgery. Aesthet. Surg. J. 39, 1007–1016. doi: 10.1093/asj/sjz043
Schlegl, A. T., Pinter, Z., Kovacs, A., Kopjar, E., Varga, P., Kardos, D., et al. (2020). Teaching basic surgical skills using homemade tools in response to COVID-19. Acad. Med. 95:e7. doi: 10.1097/ACM.0000000000003586
Schmitz, S. M., Schipper, S., Lemos, M., Alizai, P. H., Kokott, E., Brozat, J. F., et al. (2021). Development of a tailor-made surgical online learning platform, ensuring surgical education in times of the COVID19 pandemic. BMC Surg. 21:196. doi: 10.1186/s12893-021-01203-5
Senkoylu, A., Senkoylu, B., Budakoglu, I., Coskun, O., and Acaroglu, E. (2021). Blended learning is a feasible and effective tool for basic pediatric spinal deformity training. Global Spine J. 11, 219–223. doi: 10.1177/2192568220916502
Shiels, L., Majmundar, P., Zywot, A., Sobotka, J., and Lau, C. S. M., Jalonen TO (2017). Medical student attitudes and educational interventions to prevent neurophobia: a longitudinal study. BMC Med. Educ. 17:225. doi: 10.1186/s12909-017-1055-4
Sideris, M., Hanrahan, J., Tsoulfas, G., Theodoulou, I., Dhaif, F., Papalois, V., et al. (2018). Developing a novel international undergraduate surgical masterclass during a financial crisis: our 4-year experience. Postgrad. Med. J. 94, 263–269. doi: 10.1136/postgradmedj-2017-135479
Sideris, M., Papalois, V., Athanasiou, T., Papagrigoriadis, S., Pierides, M., Velmahos, G., et al. (2020). A novel multi-faceted course blueprint to support outcome-based holistic surgical education: the integrated generation 4 model (iG4). In Vivo 34, 503–509. doi: 10.21873/invivo.11801
Sideris, M., Papalois, A., Theodoraki, K., Dimitropoulos, I., Johnson, E. O., Georgopoulou, E. M., et al. (2017). Promoting undergraduate surgical education: current evidence and Students' views on ESMSC international wet lab course. J. Investig. Surg. 30, 71–77. doi: 10.1080/08941939.2016.1220652
Sim, S. K., Myo, N., and Sohail, M. (2023). Team-based self-directed learning enhanced students' learning experience in undergraduate surgical teaching. Med J Malaysia 78, 61–67.
Su, B. (2022). Enhancement of online education to the teaching paradigm: taking academic medical postgraduate cultivation as an example. Front. Med. (Lausanne) 9:807469. doi: 10.3389/fmed.2022.807469
Sun, M., Chu, F., Gao, C., and Yuan, F. (2022). Application of the combination of three-dimensional visualization with a problem-based learning mode of teaching to spinal surgery teaching. BMC Med. Educ. 22:840. doi: 10.1186/s12909-022-03931-5
Sun, K., and Liu, R. (2021). The "hand and foot teaching" in clinical teaching of olecranon fracture and patellar fracture of ulna. Asian J. Surg. 44, 481–484. doi: 10.1016/j.asjsur.2020.11.005
Sun, R. R., Wang, Y., Fast, A., Dutka, C., Cadogan, K., Burton, L., et al. (2021). Influence of musical background on surgical skills acquisition. Surgery 170, 75–80. doi: 10.1016/j.surg.2021.01.013
Sundbom, M., Hellstrom, P., and Graf, W. (2021). A new hybrid concept, combining lectures and case-seminars, resulted in superior ratings from both undergraduate medical students and teachers. Adv. Med. Educ. Pract. 12, 597–605. doi: 10.2147/AMEP.S309344
Tagaytayan, R., Kelemen, A., and Sik-Lanyi, C. (2018). Augmented reality in neurosurgery. Arch. Med. Sci. 14, 572–578. doi: 10.5114/aoms.2016.58690
Tanzer, M., Laverdiere, C., Barimani, B., and Hart, A. (2022). Augmented reality in arthroplasty: an overview of clinical applications, benefits, and limitations. J. Am. Acad. Orthop. Surg. 30, e760–e768. doi: 10.5435/JAAOS-D-21-00964
Tejos, R., Crovari, F., Achurra, P., Avila, R., Inzunza, M., Jarry, C., et al. (2021). Video-based guided simulation without peer or expert feedback is not enough: a randomized controlled trial of simulation-based training for medical students. World J. Surg. 45, 57–65. doi: 10.1007/s00268-020-05766-x
Theodoulou, I., Nicolaides, M., Athanasiou, T., Papalois, A., and Sideris, M. (2018). Simulation-based learning strategies to teach undergraduate students basic surgical skills: a systematic review. J. Surg. Educ. 75, 1374–1388. doi: 10.1016/j.jsurg.2018.01.013
Tune, J. D., Sturek, M., and Basile, D. P. (2013). Flipped classroom model improves graduate student performance in cardiovascular, respiratory, and renal physiology. Adv. Physiol. Educ. 37, 316–320. doi: 10.1152/advan.00091.2013
Wang, Q., Li, Z., Huang, X., Fu, X., Li, Q., and Li, H. (2022). Step-by-step method combined with simulation-enhanced learner outcomes in minimally invasive breast surgery education. Adv. Med. Educ. Pract. 13, 1051–1060. doi: 10.2147/AMEP.S367304
Wang, S., Ren, X., Ye, J., Wang, W., Huang, H., and Qin, C. (2021). Exploration of simulation-based medical education for undergraduate students. Medicine (Baltimore) 100:e25982. doi: 10.1097/MD.0000000000025982
Wei, F., Sun, Q., Qin, Z., Zhuang, H., Jiang, G., and Wu, X. (2021). Application and practice of a step-by-step method combined with case-based learning in Chinese otoendoscopy education. BMC Med. Educ. 21:89. doi: 10.1186/s12909-021-02513-1
White, M., Michaud, G., Pachev, G., Lirenman, D., Kolenc, A., and FitzGerald, J. M. (2004). Randomized trial of problem-based versus didactic seminars for disseminating evidence-based guidelines on asthma management to primary care physicians. J. Contin. Educ. Heal. Prof. 24, 237–243. doi: 10.1002/chp.1340240407
Williams, C., Familusi, O. O., Ziemba, J., Lee, D., Mittal, S., Mucksavage, P., et al. (2021). Adapting to the educational challenges of a pandemic: development of a novel virtual urology subinternship during the time of COVID-19. Urology 148, 70–76. doi: 10.1016/j.urology.2020.08.071
Wolfe, E. M., Alfonso, A. R., Diep, G. K., Berman, Z. P., Mills, E. C., Park, J. J., et al. (2021). Is digital animation superior to text resources for facial transplantation education? A randomized controlled trial. Plast. Reconstr. Surg. 148, 419–426. doi: 10.1097/PRS.0000000000008166
Wu, J. C., Chi, S. C., Wu, C. C., and Kang, Y. N. (2018). Helps from flipped classroom in learning suturing skill: the medical students' perspective. PLoS One 13:e0204698. doi: 10.1371/journal.pone.0204698
Wu, Q., Wang, Y., Lu, L., Chen, Y., Long, H., and Wang, J. (2022). Virtual simulation in undergraduate medical education: a scoping review of recent practice. Front. Med. (Lausanne) 9:855403. doi: 10.3389/fmed.2022.855403
Xin, C., Mei, H., Liu, R., and Wang, G. (2021). "hand as foot" teaching method in clinical practice teaching of lumbar puncture. Asian J. Surg. 44, 698–699. doi: 10.1016/j.asjsur.2021.01.037
Yao, P., OuYang, J., Liu, C., Wang, S., Wang, X., and Sun, S. (2020). Improving burn surgery education for medical students in China. Burns 46, 647–651. doi: 10.1016/j.burns.2019.09.012
Yaqoob, M. F., Khalid, Z., Azim, M. E., Ahsan, S., Hassan, M. F., and Naeem, A. (2021). Perceptions regarding team-based learning among undergraduate physical therapy students. J. Pak. Med. Assoc. 71, 1–10. doi: 10.47391/JPMA.1172
Zhang, Y., Han, X., Song, H., and Li, Y. (2022). The "hand as foot" teaching method in clinical practice of periodontal and peri-implant surgery. Asian J. Surg. 45, 2934–2935. doi: 10.1016/j.asjsur.2022.06.110
Zhang, J., Yu, J., Lin, Y., and Liu, R. (2021). The "hand as foot" teaching method in the clinical practice of transcavernous sinuscranial nerve. Asian J. Surg. 44, 1457–1458. doi: 10.1016/j.asjsur.2021.07.065
Zhang, J., Zilundu, P. L. M., Zhang, W., Yu, G., Li, S., Zhou, L., et al. (2022). The use of a surgical boot camp combining anatomical education and surgical simulation for internship preparedness among senior medical students. BMC Med. Educ. 22:459. doi: 10.1186/s12909-022-03536-y
Keywords: surgical education, undergraduate students, blended learning, teaching method, COVID-19
Citation: Zhu L, Zhang Q and Zhang Y (2023) Multiple teaching methods in undergraduate surgical training: a blended style may be the optimal choice!. Front. Educ. 8:1200879. doi: 10.3389/feduc.2023.1200879
Received: 19 April 2023; Accepted: 10 July 2023;
Published: 03 August 2023.
Edited by:
Rhythm Bains, King George's Medical University, IndiaReviewed by:
Rameshwari Singhal, King George’s Medical University, IndiaCopyright © 2023 Zhu, Zhang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qin Zhang, NzY2OTA4MzBAcXEuY29t; Yang Zhang, eWFuZ3poYW5nODI2MjAyMkAxNjMuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.