
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Educ., 30 June 2023
Sec. Higher Education
Volume 8 - 2023 | https://doi.org/10.3389/feduc.2023.1170247
This article is part of the Research TopicResearch and Discussions in Critical Discourses and Remedies in Global Health EducationView all 20 articles
 J. Andrew Dykens1,2,3,4*
J. Andrew Dykens1,2,3,4* Keith Martin4
Keith Martin4 Elsie Kiguli-Malwadde4,5
Elsie Kiguli-Malwadde4,5 Linda Kupfer6
Linda Kupfer6 Zhuo (Adam) Chen4,7
Zhuo (Adam) Chen4,7 Nancy R. Reynolds4,8,9,10,11
Nancy R. Reynolds4,8,9,10,11 Aniruddh Behere4,12
Aniruddh Behere4,12 Suraj Bhattarai4,13,14
Suraj Bhattarai4,13,14 Caryn E. Peterson2,3,4,15
Caryn E. Peterson2,3,4,15 Stevan Merill Weine2,16
Stevan Merill Weine2,16The critical human resources deficit in the healthcare sector in low-resource settings (LRS) has an overwhelming impact on health outcomes and disparities in growth and development of the global healthcare workforce. There is a lack of qualified trainers and mentors and this makes it challenging to connect existing capacity gaps with existing expertise and established programs. Through global health partnerships, training programs, and mentorship, individuals and institutions from around the globe can connect to share training resources and strengthen clinical and research capacity in LRSs. Global health partnerships focused on capacity building face many challenges including; unequal access to information about potential partners and training opportunities, a lack of transparency regarding each institutions training priorities, and inequity and absent reciprocity within global health partnerships that have disproportionate power division between high-resource and LRSs. This initiative, the Consortium of Universities for Global Health Capacity Strengthening Platform (CUGH-CPS) (CUGHCapacityBuilding.org), aims to empower institutions and individuals in LRSs to address these challenges and drive partnership engagement through avenues that are beneficial to the LRS agent needs and context by leading the prioritization of training capacity development across clinical and research domains. The CUGH-CPS helps to identify and create a platform for the dissemination of training and mentorship needs from LRS institutions and share this information with the global community. This manuscript describes this new initiative officially launched to a global audience at the April 2023 CUGH meeting.
An adequate and fairly distributed healthcare workforce is essential to achieving equitable access to healthcare services at the primary, secondary, and tertiary levels, ensuring Universal Health Coverage (UHC), and responding to the Sustainable Development Goals (SDG) (World Health Organization [WHO], 2016a,b, 2017a). Currently, the critical human resources deficit in the healthcare sector of low-resource settings (LRS) has an overwhelming impact on health outcomes globally (Dreesch et al., 2005; World Health Organization [WHO], 2016a). The 2016 Global Strategy on Human Resources for Health: Workforce 2030 projected a global shortage of 18 million health workers by 2030 (World Health Organization [WHO], 2016a). Recent findings, aided by the availability of improved data, illustrate a reduction in this global shortage estimate from 15.4 million in 2020 to 10.2 million in 2030 (Boniol et al., 2022). However, while there is improvement, the human resources for health crisis remains a pressing concern. In addition to shortages, there are considerable disparities in growth and development of the healthcare workforce globally. Contrary to other global regions, the World Health Organization (WHO) African and Eastern Mediterranean regions did not show improvements between 2013 and 2020, and projections remain stagnant into 2030 (Boniol et al., 2022). The WHO African Region has the highest shortage of healthcare workers. Thirty-six of the fifty seven WHO Member States globally facing a critical shortage of doctors, nurses, and midwives were from the African Region (World Health Organization [WHO], 2021). While the SDGs require 4.5 health workers per 1,000, the African Region has an estimated average of only 1.55 per 1,000 population (World Health Organization [WHO], 2022a,b). The WHO African Region workforce shortage is estimated to reach 6.1 million by 2030 (World Health Organization [WHO], 2017b). In addition, there is an uneven distribution of workforce by country within Africa, ranging from 0.25 health workers per 1,000 people (Niger) to 9.15 per 1,000 (Seychelles) (World Health Organization [WHO], 2022b).
At the heart of the problem is a lack of qualified trainers and mentors as well as the challenge of connecting existing expertise and established training programs to areas and individuals with identified training capacity gaps (The Academy of Medical Sciences, 2017; Consortium of Universities for Global Health, 2020; The Sustaining Technical and Analytic Resources (Star) project, 2020; Sustaining Technical and Analytic Resources (Star), 2020a). Global health partnerships, training programs, and mentorship are common ways through which individuals and institutions can connect and share training resources in order to strengthen clinical and research capacity in LRSs (The Academy of Medical Sciences, 2017). In 2019, the Consortium of Universities for Global Health (CUGH) led an initiative which included a structured review (including profiling and researching potential partners) and analysis of capacity needs for academic partnership in global health, followed by development of a capacity assessment process for enhanced knowledge sharing (The Academy of Medical Sciences, 2017; Consortium of Universities for Global Health, 2020;Sustaining Technical and Analytic Resources (Star), 2020a,b). In the same year, CUGH piloted a web-based platform aimed at connecting institutions for capacity strengthening partnerships. During the pilot phase there were 152 unique registrations from 34 different countries. The US had the most partnership opportunity listings (36.8%) followed by Nigeria (9.2%), South Africa (8.6%), Uganda (5.3%), Ethiopia (4.6%), and Pakistan (4.6%). Low- and lower-middle-income countries represented 82.4% of all countries. The countries represented spanned across all World Health Organization regions. Of the 98 listings that specified a technical domain: medicine accounted for 53.1% and nursing had 21.4%. We were unable to track partner matches on the platform, creating challenges in understanding the full impact of the database. Registered users of this pilot initiative were surveyed and the end-user feedback and impact of the pilot initiative is reported in a separate article (Jose et al., under review).1 This pilot initiative has informed the further development of this platform.
This manuscript describes a new initiative officially launched to a global audience at the April 2023 CUGH meeting, the CUGH Capacity Strengthening Platform (CUGH-CSP), which aims to empower institutions and individuals in any setting to address many of these challenges and drive partnership engagement in ways that are most beneficial to their own needs and context by specifying priorities for training capacity development across clinical and research domains. The CUGH-CSP2 identifies and aggregates institutional training training and individual mentorship needs from any setting and shares this information with the global community. Institutions can post training capacity resources, expertise, and available mentors. Global health stakeholders from any setting can use the platform to approach institutions and individuals with complementary priorities to explore partnership development, training program participation, and mentorship opportunities aimed at strengthening training capacity.
Global health partnerships focused on capacity building and education face several challenges: (1) unequal access to potential partners and training opportunities, (2) lack of transparency regarding institutional training capacity priorities, (3) lack of clarity regarding the context of training capacity gaps, (4) inequity, lack of reciprocity, and absence of bidirectionality within global health partnerships with disproportionate power division between high-resource and LRS, (5) training initiatives are often driven by the priorities of grant mechanisms, external funders, or external entities, (6) high resource setting institutions often benefit inordinately from associated indirect funding, faculty development, and trainee educational opportunities, (7) geographic distance between partnering institutions often leads to inefficient logistical challenges, and (8) short-term partnerships create challenges through steep learning curves, a lack of depth and breadth in mutual understanding, and limited collaborative experience. The CUGH-CPS aims to address these pervasive challenges.
Individuals at academic institutions, non-governmental organizations, health facilities, governmental agencies, international organizations, and private agencies are able to register on the CUGH-CPS. Individuals may then create and search postings relevant to three potential matching categories: (1) Institutional Partnership, (2) Training Programs, and (3) Mentorship. Individuals seeking an Institutional Partnership are able to submit two types of postings: (a) training capacity gaps or (b) training capacity expertise and resources at their own institution. Through the Training Programs focus, registrants may post open enrollment training programs that are offered through their institutions. These are variable duration training programs open to individuals external to the institution that do not require the development of an institutional partnership. Mentorship postings allow registrants the opportunity to offer expertise or seek guidance to another individual through a mentoring relationship. Partnership, Training Program, and Mentorship postings may be categorized according to clinical or research focus, clinical and non-clinical domain, diagnostic category, and training level, if relevant. For Partnership and Training Program postings one may also specify additional relevant details such as preferred training or timing, duration, scope, preferred language, partner engagement arrangement, format, setting, enrollment modality, cost, and relevant certification or degree.
The platform currently has two main areas of capacity focus. The General Database is broad, covering clinical and research domains across a wide range of professions that may have relevance to global health, including medicine, public health, economics, social sciences, and law. The Implementation Science Database is a secondary access point with a specific focus. Individuals, institutions, and programs with the goal of strengthening capacity in implementation research are able to directly engage through this focused area of the database. Future iterations of this platform will have additional areas of focus. In order to match with other institutions or individuals, registrants can search the site to identify potential collaborators, securely communicate directly through the platform to connect, and develop global health partnerships that meet their own needs.
All contact information registered through this platform remains private and is not posted publicly. Registrants are able to connect to each other through the internal messaging platform to seek additional information and explore opportunities for partnering. These messages are not accessible outside of the platform. Each registrant has full control of when and how their own contact information is shared with other individuals. The activities of the CUGH-CPS are constrained to cataloging needs and capacity and sharing these needs online. The CUGH will not engage in the direct creation or maintenance of any partnerships.
This platform is an initiative of the CUGH Workforce Capacity Building Subcommittee of the Education Committee and has been developed in close collaboration with various strategic partners well-positioned to inform the responsiveness of the platform to end-user needs. This includes key advisors from academic centers and consortia focused on capacity building in the Global South, experts in implementation science, and representatives at academic centers in the Global North. The key advisory group met bi-weekly from February through June 2022 with a focused Beta Launch from July through September 2022 followed by revisions. A soft launch took place in January 2023 with continued refinements to the platform. In April 2023 at the initiation of the CUGH annual conference, the platform was formally launched and disseminated to a wide audience. Dissemination modalities include newsletters, webinars, conference presentations, journal articles, blog posts, and social media posts. In addition, CUGH will be engaging additional partners for support in dissemination efforts to a wider audience. We will fully evaluate the platform and disseminate quarterly reports that describe metrics related to (a) dissemination: modalities, number of communications; reach, (b) engagement: registrations, countries, institutions, messages, connections, number of website visits, time spent on website, pages per visit, conversion rate, user feedback, user satisfaction; (c) content: postings by region, country, type, and focus; and (d) impact: connections made by type, region, and country, established partnerships, projects, grants, and articles, number of resulting trainings and personnel trained, cost-effectiveness.
Global health partnerships are an essential strategy to facilitate the resource sharing requisite to addressing existing global health capacity gaps. Best practices within a global health partnership create an environment that is supportive of and beneficial to all partners while optimizing impact. Striving for these best practices are critical to avoiding colonial ideologies, elevating the priorities of under-resourced institutions, and fostering efficient, effective, and equitable collaborative relationships (Table 1).
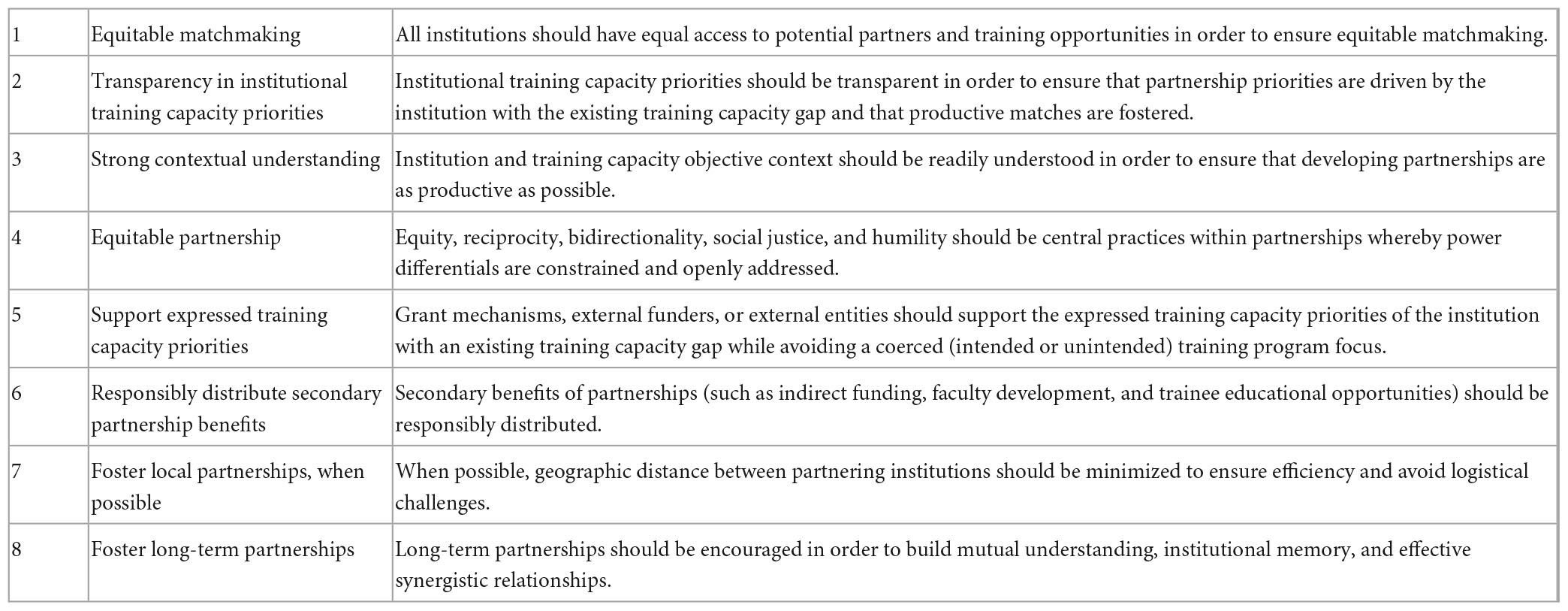
Table 1. Global health partnerships focused on capacity strengthening and education should ideally reflect the following eight strategies or approaches.
The manner in which partnerships are developed is a critical aspect of ensuring responsible collaboration. Current opportunities and processes for creating connections between institutions are often ad hoc. The initiation of relationships regularly comes through introductions by colleagues, chance meetings at conferences, or, frequently, the whim of one institution to work in a particular geographic area. Relationships that develop from these auspicious beginnings are often imbalanced, significantly favoring the high resource institution. Similarly, global partnerships that originate around the development of research projects may be grant-driven (with defined parameters of technical domain, scope, and financing), creating power differentials between high resource institutions with access to agenda-focused funding opportunities and the LRSs where these projects ultimately take place (Ollila, 2005; Eichbaum et al., 2020). Individuals working for LRS institutions are limited in their ability to access timely information about opportunities, grow their network by attending international professional conferences in person, travel for collaborative exchange, and exercise choice in partnering relationships (López-Vergès et al., 2021). Institutions in LRSs may, therefore, be compelled to accept offers of project opportunities even when the focus runs counter to their existing priorities given the attraction of funding (López-Vergès et al., 2021). This situation may further stagnate or set-back progress toward strengthening their own capacity by draining personnel time and opportunities for trainee engagement in ways that respond to short- or long-term goals.
Ideally, global health partnerships and mentorship are equitable, reciprocal, and bidirectional (Melby et al., 2016; Eichbaum et al., 2020; Monette et al., 2021). In addition, a social justice focus and humility of partners are central practices (Plamondon et al., 2021). Global health partnerships may strengthen domain-specific workforce capacity within one or all of the engaged institutions as a core objective. These relationships also create additional opportunities such as the availability of unattached (indirect) funding for the institution, professional development for clinicians or researchers, and educational opportunities for trainees. Within a truly collaborative relationship, these benefits (primary and secondary) should be responsibly distributed, with equal opportunities for each institution to offer advantage and accept shared resources, as appropriate and ethical (Melby et al., 2016; Eichbaum et al., 2020; Monette et al., 2021).
Greater equity within the matching process could also facilitate the flow of resources and expertise in a bidirectional manner. In the current construct, knowledge innovation tends to be researched and recorded in high resource settings with subsequent unidirectional flow of evidence into LRSs where context is inherently different. In contrast, the concept of global innovation, whereby there is an innate recognition that disruptive and transformative technologies are developed in all settings, is highly valued. In turn, research, theory, commentary, and debate pass in a bidirectional manner to provide an evidence base to promote, support, and mainstream this type of knowledge flow that can solve problems of global implications (Harris et al., 2020; Crump et al., 2021).
Unfortunately, it is often challenging for institutions who are seeking partnerships to fully understand the needs and context of potential partners. The CUGH-CPS directly addresses these pervasive challenges by empowering institutions with training capacity gaps in several ways. Institutions in need of training capacity resources are now able to proactively catalog their high priority areas of need. These documented needs are, then, easily identifiable by high resource setting institutions who are seeking partnerships. This transparency raises awareness within the partnering process and encourages institutions with complementary training capacity to engage in ways that are the most meaningful. This priority sharing is, therefore, empowering and circumvents the influence of disproportionate power division in determining project focus (Boum et al., 2018). Institutions with matching goals are more able to connect with ease in a timely manner, which may result in a greater number of more efficient and equitable global health partnerships. The platform also directly empowers low-resource institutions in their ability to initiate engagement with high resource institutions in ways not previously possible.
In addition, partnerships that are able to engage frequently and longitudinally have the greatest opportunity for impact, given the depth of mutual understanding that develops over time (Dykens et al., 2014). Geographic proximity between partnering institutions can facilitate this longitudinal relationship and optimize the use of resources. The CUGH-CPS could foster more local connections between institutions in LRSs, offering opportunities for them to leverage their relative strengths within the exchange and sharing of resources (Evert et al., 2014; Herrick and Reades, 2016). The improved sharing of local resources and expertise to address training capacity gaps among institutions in the Majority World (Alam, 2008; Khan et al., 2022) could, therefore, facilitate more efficient capacity strengthening.
Addressing the overwhelming global healthcare workforce crisis requires accessible, high-quality, and reliable training capacity within institutions in LRSs, globally. As a global society, we will need to institute a wide range of creative solutions in order to change the existing trajectory. By strengthening and creatively leveraging a global network of training institutions through the use of this novel platform, global health partners can more rapidly realize equitable, efficient, and effective relationships through the matching of training capacity priorities. The potential resulting clinical and research capacity will have profound implications for individual and population health outcomes globally in the decades to come.
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
JD, KM, EK-M, LK, and ZC contributed to the conception and design of the project. JD, KM, and EK-M drafted the manuscript. LK, ZC, NR, AB, SB, CP, and SW revised the manuscript critically for content. All authors contributed to the acquisition, analysis, interpretation of data, and read and approved the final manuscript.
Research reported in this publication was supported by the Fogarty International Center through U.S. Civilian Research and Development Foundation Grant Number R-202110-68191.
The authors declare that this study received funding from the National Institutes of Health Fogarty International Center. The funder had the following involvement with the study: LK was a member of the advisory board during development of the platform.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. National Institutes of Health or Department of Health and Human Services.
Alam, S. (2008). Majority world: Challenging the west’s rhetoric of democracy. Am. J. 34, 88–98. doi: 10.17953/amer.34.1.l3176027k4q614v5
Boniol, M., Kunjumen, T., Nair, T., Siyam, A., Campbell, J., and Diallo, K. (2022). The global health workforce stock and distribution in 2020 and 2030: A threat to equity and “universal” health coverage? BMJ Glob. Health 7:e009316. doi: 10.1136/bmjgh-2022-009316
Boum, Y., Burns, B., Siedner, M., Mburu, Y., Bukusi, E., and Haberer, J. (2018). Advancing equitable global health research partnerships in Africa. BMJ Glob. Health. 3:e000868. doi: 10.1136/bmjgh-2018-000868
Consortium of Universities for Global Health (2020). Sustaining technical and analytic resources (star) project’s capacity landscape analysis. Washington, DC: Consortium of Universities for Global Health.
Crump, L., Maidane, Y., Mauti, S., Tschopp, R., Ali, S., Abtidon, R., et al. (2021). From reverse innovation to global innovation in animal health: A review. Heliyon 7:e08044. doi: 10.1016/j.heliyon.2021.e08044
Dreesch, N., Dolea, C., Dal Poz, M., Goubarev, A., Adams, O., Aregawi, M., et al. (2005). An approach to estimating human resource requirements to achieve the millennium development goals. Health Policy Plan 20, 267–276. doi: 10.1093/heapol/czi036
Dykens, A., Hedrick, C., Ndiaye, Y., and Linn, A. (2014). Peace corps partnered health services implementation research in global health: Opportunity for impact. Glob. Adv. Health Med. 3, 8–15. doi: 10.7453/gahmj.2014.031
Eichbaum, Q., Adams, L., Evert, J., Ho, M., Semali, I., and van Schalkwyk, S. (2020). Decolonizing global health education: Rethinking institutional partnerships and approaches. Acad. Med. 96, 329–335. doi: 10.1097/ACM.0000000000003473
Evert, J., Drain, P., and Hall, T. (2014). Developing global health programming: A guidebook for medical and professional schools, 2nd Edn. San Francisco: Global Health Education Collaborations Press.
Harris, M., Dadwal, V., and Syed, S. (2020). Review of the reverse innovation series in globalization and health - where are we and what else is needed? Glob. Health 16:26. doi: 10.1186/s12992-020-00555-6
Herrick, C., and Reades, J. (2016). Mapping university global health partnerships. Lancet Glob. Health 4:e694. doi: 10.1016/S2214-109X(16)30213-3
Khan, T., Abimbola, S., Kyobutungi, C., and Pai, M. (2022). How we classify countries and people—and why it matters. BMJ Glob. Health 7:e009704. doi: 10.1136/bmjgh-2022-009704
López-Vergès, S., Urbani, B., Fernández Rivas, D., Kaur-Ghumaan, S., Coussens, A., Moronta-Barrios, F., et al. (2021). Mitigating losses: How scientific organisations can help address the impact of the COVID-19 pandemic on early-career researchers. Hum. Soc. Sci. Commun. 8:284. doi: 10.1057/s41599-021-00944-1
Melby, M., Loh, L., Evert, J., Prater, C., Lin, H., and Khan, O. (2016). Beyond medical “missions” to impact-driven short-term experiences in global health (STEGHs): Ethical principles to optimize community benefit and learner experience. Acad. Med. 91, 633–638. doi: 10.1097/ACM.0000000000001009
Monette, E., McHugh, D., Smith, M., Canas, E., Jabo, N., Henley, P., et al. (2021). Informing “good” global health research partnerships: A scoping review of guiding principles. Glob. Health Action 14:1892308. doi: 10.1080/16549716.2021.1892308
Ollila, E. (2005). Global health priorities - priorities of the wealthy? Glob. Health 1:6. doi: 10.1186/1744-8603-1-6
Plamondon, K., Brisbois, B., Dubent, L., and Larson, C. (2021). Assessing how global health partnerships function: An equity-informed critical interpretive synthesis. Glob. Health 17:73. doi: 10.1186/s12992-021-00726-z
Sustaining Technical and Analytic Resources (Star) (2020a). Capacity assessment toolkit for enhanced knowledge sharing. Washington, DC: Consortium of Universities for Global Health.
Sustaining Technical and Analytic Resources (Star) (2020b). Partnership assessment toolkit companion document. Washington, DC: Consortium of Universities for Global Health.
The Academy of Medical Sciences (2017). “Strengthening clinical research capacity in low- and middle-income countries,” in Workshop report, (London: The Academy of Medical Sciences).
The Sustaining Technical and Analytic Resources (Star) project (2020). Comprehensive review of academic partnerships. Washington, DC: Consortium of Universities for Global Health.
World Health Organization [WHO] (2016a). Global strategy on human resources for health: Workforce 2030. Geneva: World Health Organization.
World Health Organization [WHO] (2016b). Working for health and growth: Investing in the health workforce. Report of the high-level commission on health employment and economic growth. Geneva: World Health Organization.
World Health Organization [WHO] (2017a). National health workforce accounts: A handbook [Internet]. Geneva: World Health Organization.
World Health Organization [WHO] (2017b). What needs to be done to solve the shortage of health workers in the African Region. Geneva: World Health Organization.
World Health Organization [WHO] (2021). The state of the health workforce in the WHO African Region, 2021 [Internet]. Geneva: World Health Organization.
World Health Organization [WHO] (2022a). African region WHO AFRO health workforce observatory database african health observatory. Available online at: https://aho.afro.who.int/hrh/af (accessed August 30, 2022).
World Health Organization [WHO] (2022b). Chronic staff shortfalls stifle Africa’s health systems: WHO study. Available online at: https://www.afro.who.int/news/chronic-staff-shortfalls-stifle-africas-health-systems-who-study (accessed August 30, 2022).
Keywords: global health partnership, healthcare workforce, capacity building, institutional capacity, low-resource settings, CUGH
Citation: Dykens JA, Martin K, Kiguli-Malwadde E, Kupfer L, Chen ZA, Reynolds NR, Behere A, Bhattarai S, Peterson CE and Weine SM (2023) A global matchmaking web platform facilitating equitable institutional partnerships and mentorship to strengthen health workforce training capacity. Front. Educ. 8:1170247. doi: 10.3389/feduc.2023.1170247
Received: 20 February 2023; Accepted: 30 May 2023;
Published: 30 June 2023.
Edited by:
Tomlin Paul, University of Global Health Equity, RwandaReviewed by:
Phuoc Le, University of California, San Francisco, United StatesCopyright © 2023 Dykens, Martin, Kiguli-Malwadde, Kupfer, Chen, Reynolds, Behere, Bhattarai, Peterson and Weine. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: J. Andrew Dykens, amR5a2Vuc0B1aWMuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.