
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Educ. , 18 May 2023
Sec. Special Educational Needs
Volume 8 - 2023 | https://doi.org/10.3389/feduc.2023.1125929
This article is part of the Research Topic Educational Approaches for Promoting Neurodivergent Health, Well-Being, and Thriving Across the Life Course View all 9 articles
Introduction: Children and youth on the autism spectrum and their families use health and educational services to address their complex needs. They use primary health care services in the medical home, as endorsed by the American Academy of Pediatrics (AAP). They can also use educational services for their cognitive, social, and adaptive skill development, beginning in early intervention and through their transition to postsecondary or vocational roles. Medical and educational services are organized and delivered in separate systems, thereby placing the primary responsibility for coordinating these services on their families.
Methods: Pooled data from 2016 through 2019 National Survey of Children's Health were used to measure the association between current educational service use and six medical home primary care components, controlling for select sociodemographic and clinical factors in children and youth on the autism spectrum (n = 1,922).
Results: After controlling for select sociodemographic and clinical factors, difficulty getting referrals [aOR = 2.93, 95% CI (1.33, 6.41), P = 0.007] and no shared decision-making in the medical home [aOR = 2.93, 95% CI (1.21, 7.06), P = 0.016] resulted in higher likelihood of current educational service use. Older children had a lower likelihood of current educational service use [aOR = 0.91, 95% CI (0.85, 0.97), P = 0.003], whereas higher autism severity increased the likelihood of current educational service use [aOR = 1.80, 95% CI (1.10, 2.95), P = 0.019].
Conclusion: Children and youth on the autism spectrum, especially those with moderate or severe autism, had a higher likelihood of education service use, unless they were older, had difficulty getting referrals, and no shared decision-making. Results suggest that the way services are currently provided between health and educational systems separates medical and educational professionals, therefore increasing the demands on caregivers and educational systems to facilitate current educational service use. Further study is needed for improving the medical home referral or shared decision-making pathways and to identify caregiver strategies for navigating educational systems.
Children and youth on the autism spectrum use multiple service systems for their health, cognitive, social, and behavioral needs, beginning in early childhood. Medical home care, endorsed by the American Academy of Pediatrics (AAP), provides primary care to children and youth on the autism spectrum for their preventive, acute, and chronic care needs, and effective care management of secondary co-morbidities (American Academy of Pediatrics, 2002). They can also concurrently receive educational services for their cognitive, social, emotional, communication, and adaptive development, beginning in early intervention (EI) and extending through to their transition to postsecondary or vocational roles (Lipkin and Okamoto, 2015).
Collaboration between medical home care providers and educationally based service professionals (Shahidullah et al., 2018) is complex because of different federal laws for these systems, funding structures, and processes of care (e.g., frequency of contact with families and the time available during visits; Shahidullah et al., 2018). For example, EI providers serve infants, toddlers, and families in their natural environment (e.g., family home), and consequently, become familiar with familial interactions, and their strengths and challenges, but this type of service provision is not feasible for primary care providers (PCPs). Similarly, EI providers may see families weekly, while PCPs may see families at well-child visits (Sobotka et al., 2016). Finally, special education services for students aged 3–21 years vary by state and neighboring location (Shahidullah et al., 2018).
There are limited professional guidelines to support recommendations for how medical home providers coordinate with educational service systems (Sobotka et al., 2016). Prior studies have examined the adequacy of medical home care (American Academy of Pediatrics, 2002), which includes these components: (1) family centeredness (Toomey et al., 2010; Montes and Halterman, 2011), (2) care coordination (Ronis et al., 2015), (3) comprehensiveness (Raphael et al., 2009), (4) continuity (McManus et al., 2013), (5) compassion (Weedon et al., 2012), and (6) culturally effective care (Lipkin and Okamoto, 2015). Two studies have primarily assessed for quality of medical home care with respect to its family centeredness and effective care coordination (Long et al., 2013; Lipkin and Okamoto, 2015).
One study observed a negative relationship between medical home care and current educational service use in children and youth on the autism spectrum for a nationally representative sample of children and youth on the autism spectrum. Rizk et al. (2023) found lower overall maternal health was correlated with medical home care inadequacy and current educational service use, and similarly, another study found that children with autism who received medical home care were significantly associated with reportedly lower parental stress (Limbers et al., 2020). Receiving inadequate medical home care had significantly higher odds of current educational service use, as attenuated by child age, maternal health status, and other special needs factors (Rizk et al., 2023). While this negative association between inadequate medical home care and current educational service use was established for children and youth on the autism spectrum, it remains unclear which medical home care component(s) are significantly associated with their current educational service use (Shahidullah et al., 2018).
Using population-based data to examine medical home care components moves beyond simply identifying associations between medical home care, a complex construct captured in the NSCH, and current educational service use. Leveraging population-based data in this way advances our understanding of why observed service access disparities occur and key pathways or leverage points within a given system that provides more information on how these systems of care work and how sociodemographic characteristics work through these pathways to drive these associations. The purpose of this study was to build greater specificity about the relationship between medical home care adequacy and current educational service use for children and youth on the autism spectrum. Based on previous literature, we hypothesized that medical home care component inadequacy will be associated with a lower likelihood of current educational service use, and select child, youth, and family sociodemographic and clinical factors will further attenuate the likelihood of current educational service use in children and youth on the autism spectrum.
We used data from the pooled 2016–2019 National Survey (NSCH) to examine the association between individual medical home care components and current educational service use in children and youth on the autism spectrum. This cross-sectional survey collected information from parents or guardians (caregivers) of children and youth aged 0–17 years old in the United States and District of Columbia about their health, healthcare access, family characteristics, neighborhoods, school, and social conditions. Eligible households advanced to age-specific NSCH topical questionnaires, yielding data on all variables of this study (US Census Bureau, 2019).
We included children and youth aged 1–17 years old with positive and valid responses to, “Has a doctor or other health care provider EVER told you that this child has ASD or autism spectrum disorder (ASD)?” (n = 1,922).
We selected positive and valid caregiver responses to the current educational service use question as the primary dependent variable. This variable was ascertained first through an ever question: “...” and respondents indicating Yes received a follow-up question: “Is this child CURRENTLY receiving services under one of these plans?” We defined current educational service as children and youth on the autism spectrum reportedly receiving educational services currently use under one of these plans (US Census Bureau, 2019).
We measured the five individual NSCH medical home care components aligned with HRSA MCHB's medical home care measure as the independent variables (US Census Bureau, 2019). The 2016–2019 NSCH defined medical home care with an algorithm aggregating caregivers' responses to five items pertaining to medical home care: (1) personal doctor or nurse (one item), (2) usual source of sick care (two items), (3) family-centered care (five items), (4) difficulty getting referrals (one item), and (5) effective care coordination (six items) when needed. For this study, as part of the NSCH National Performance Measure 11 (NPM-11), 16 Medical Home Among CSHCN and Non-CSHCN, shared decision-making (four items), was included by applying parameters specified in the NSCH (US Census Bureau, 2019) Data on medical home care components were collected by first asking caregivers, “During the past 12 months, did this child see a doctor, nurse, or other health care provider for sick-child care, well-child check-ups, physical exams, hospitalizations, or any other kind of medical care?” Caregivers who responded affirmatively were then administered the subsequent 20 items across the six individual medical home care components.
This NSCH component solicited caregiver information on whether their child or youth had one or more persons that caregivers thought of as their child's doctor or nurse. Affirmative responses were coded as meeting criteria. Examples of a personal doctor or nurse included providers who know and are familiar with the child and their health history (US Census Bureau, 2019).
This NSCH medical home component was derived from a two-part item: (1) “Is there a place that this child USUALLY goes when he or she is sick or you or another caregiver needs advice about his or her health?” followed by, (2) “If yes, where does this child go?” During the 2018 NSCH, the first part of this item was modified to include, “…. you or another caregiver USUALLY take this child…” Usual source of sick care was operationalized as having a usual place to go when the child is sick, excluding the emergency department (ED; US Census Bureau, 2019).
This NSCH medical home care component included five items assessing the frequency that healthcare providers: (1) spent enough time with the child, (2) listened carefully, (3) showed sensitivity to families' values and customs, (4) provided specific information, (5) and helped families feel like a partner in the child's care (US Census Bureau, 2019). Items were collapsed based on the sample and to delineate whether families ever experienced one or more family-centered care (always and usually/sometimes) or did not experience them (never; US Census Bureau, 2019).
This NSCH medical home care component included a two-part item related to if children and youth needing referrals to see any doctors or receive any services, and if so, how difficult it was to get referrals. Difficulty getting referrals was dichotomized (not difficult/no referral needed); difficult (somewhat, very, not possible; US Census Bureau, 2019).
This NSCH medical home care component was derived from the following four items: (1) need for health care decision-making (e.g., prescriptions, referrals, and procedures), (2) frequency that providers discussed options, (3) ease with raising caregivers' concerns or disagreeing with providers, and (4) working together to make the best decision for child's health care or treatment options. Caregivers who reported “Always” or “Usually” all shared decision-making items (i.e., frequency of discussing options, ease of raising concerns, and working together to make best decisions for children) met criteria for shared decision-making (US Census Bureau, 2019).
Children and youth on the autism spectrum, who reportedly had “No health care visit in the past 12 months,” “Did not need referrals,” “Did not see more than one health care provider,” “Did not need care coordination,” or “No decisions needed,” met criteria for receiving the individual medical home care component corresponding with these responses.
The NSCH medical home care measure is a multidimensional construct with several care components (US Census Bureau, 2019). Given the focus on examining specific medical home care components in this study, internal consistency estimates were generated for those three medical home variables with multiple items: (1) family-centered care (α = 0.91), (2) effective care coordination (α = 0.29), and (3) shared decision-making (α = 0.72). The NSCH family-centered care internal consistency estimates are comparable to existing family-centered measures, such as the Measure of Processes of Care (MPOC)-20 (α = 0.83 – 0.90; King et al., 2004). Due to low internal consistency estimation for effective care coordination, we retained: (1) doctor communication with early intervention, childcare providers, and special educational programs, and (2) caregiver satisfaction with communication among these providers, aligned with the dependent variable.
The Andersen Behavioral Model of Health Services Use (Andersen, 1995) was used to examine relevant factors expected to be associated with the likelihood of current educational service use. Predisposing factors included child sex, child age (continuous), child race/ethnicity (White, Non-Hispanic; Black, Non-Hispanic; Other), adult education level (≤ high school; > high school), maternal mental health (excellent or very good; < excellent or very good), and family structure (two parents, married; two parents, unmarried; single parent; other family type). Enabling factors included insurance type (public only/public and private; private only; unspecified/uninsured), family federal poverty level (FPL; 0–100% FPL; 101–200% FPL; ≥ 201% FPL), primary household language (English; Spanish and other), and number of ACEs (continuous; 0–9). Need included child age at autism diagnosis (continuous) and autism severity (mild; moderate/severe). We also measured the number of adverse child experiences (ACEs; 0–9 ACEs; Berg et al., 2016), such as their experiences living with a relative with mental health issues (Health Resources Administration Maternal and Child Health, 2020), and how caregiver health is relative to their children and youth's service use (Rizk et al., 2023).
Analyses were performed in Stata 17 to account for the NSCH complex survey design features (StataCorp, 2022). Prior to the main analyses, independent variables (six individual medical home care components) and covariates (predisposing, enabling, and need factors) were inspected for multicollinearity and resulted in no violations. Children were coded as “Missing” if they had missing responses to at least one item used to generate an individual medical home care component and were excluded from main analyses. Univariate (see Table 1) and bivariate analyses (see Appendix A) were performed using non-imputed data to describe the proportions of children and youth on the autism spectrum (n = 13,454) before multiple imputation (Eddings and Marchenko, 2012). Bivariate analyses assessed the associations between each of the six medical home care components, and predisposing, enabling, and need factors, related to current educational service use. Independent variables and covariates were selected for inclusion if statistically significant in bivariate analyses (p < 0.05) or established in prior health or educational service use literature involving children and youth on the autism spectrum (see Appendix A; Heeringa et al., 2017).
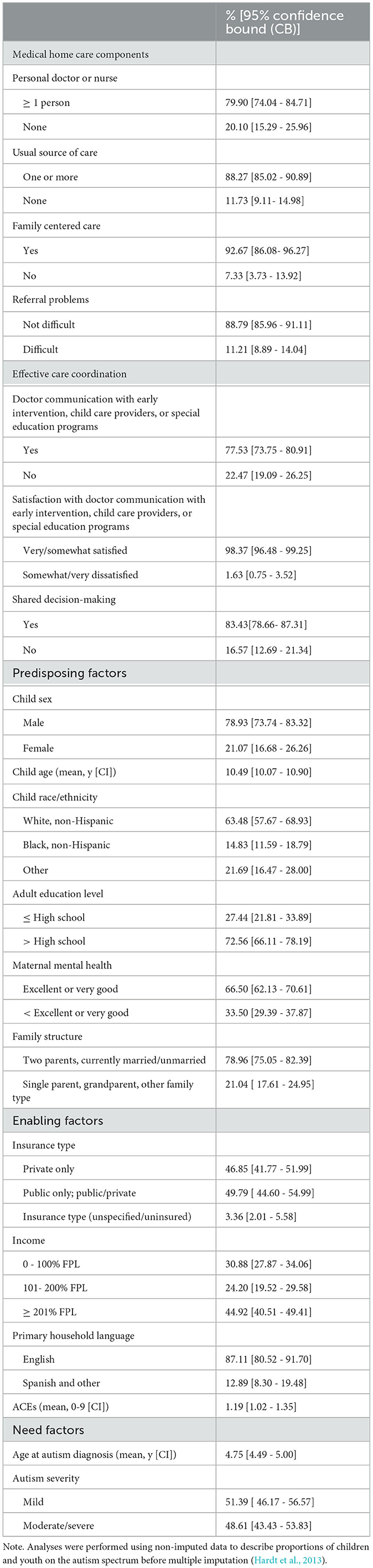
Table 1. Characteristics of children and youth on the autism spectrum, ages 1 to 17 years old (n = 13,454).
Multivariate analyses (see Figure 1 or Appendix B) included multiply imputed data (n = 1,922) that are more appropriate for inferential associations (Hardt et al., 2013) and reported using odds ratios (OR), 95% confidence interval (CI), and α < 0.05 to reduce type 1 error. Model 1 contained the six individual medical home care components. Model 2 added predisposing factors, Model 3 added enabling factors, and Model 4 added need factors (see Appendix B).
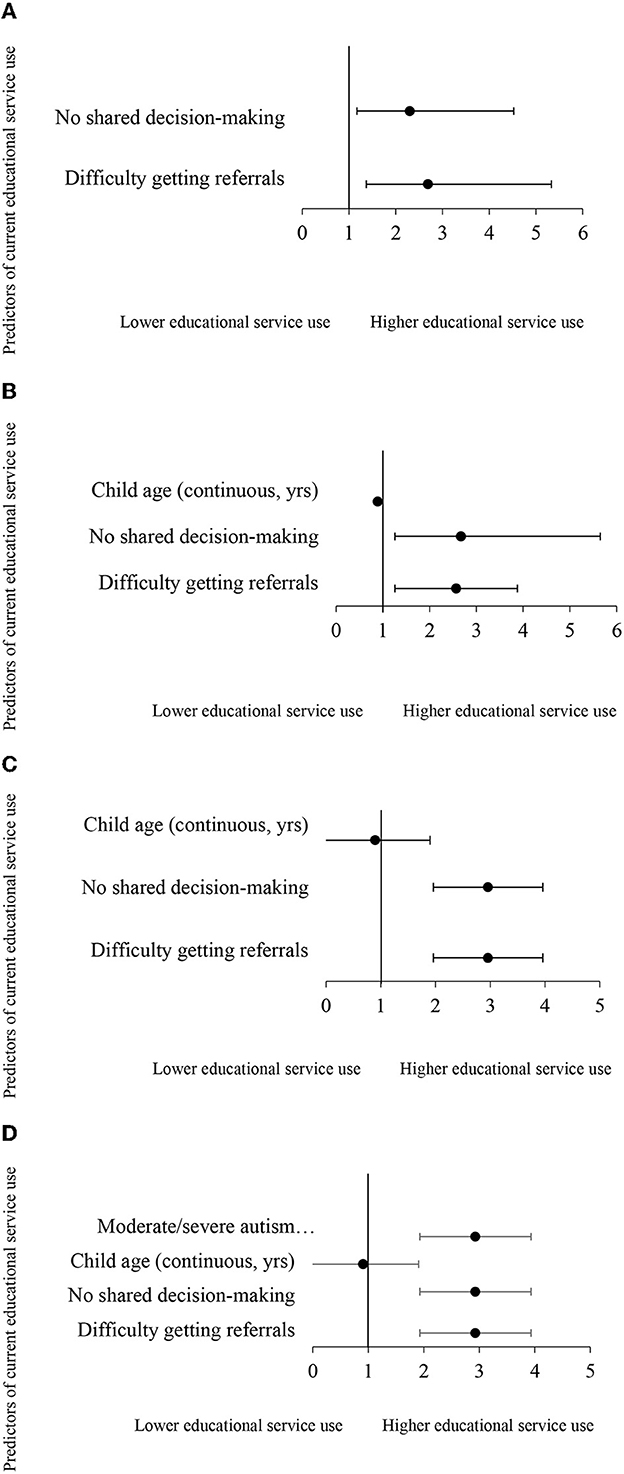
Figure 1. (A) Multivariate model predicting current educational service use from difficulty getting referrals and no shared decision-making, in children and youth on the autism spectrum, ages 1-17 (n = 1,922). Non-significant predictors: personal doctor or nurse, usual source of sicks care, family centered care, doctor communication with early intervention, child care providers, or special education programs, satisfaction with communication with early intervention, child care providers, and special education programs. (B) Multivariate model predicting current educational service use from difficulty getting referrals and no shared decision-making, controlling for predisposing factors, in children and youth on the autism spectrum, ages 1-17 (n = 1,922). Non-significant predictors: personal doctor or nurse, usual source of sicks care, family centered care, doctor communication with early intervention, child care providers, or special education programs, satisfaction with communication with early intervention, child care providers, and special education programs, child race/ethnicity, adult education level, maternal mental health, and family structure. (C) Multivariate model predicting current educational service use from medical home care components, controlling for predisposing and enabling factors, in children and youth on the autism spectrum, ages 1-17 (n = 1,922). Non-significant predictors: personal doctor or nurse, usual source of sicks care, family centered care, doctor communication with early intervention, child care providers, or special education programs, satisfaction with communication with early intervention, child care providers, and special education programs, child race/ethnicity, adult education level, maternal mental health, family structure, insurance type, income, and primary household language. (D) Multivariate model predicting current educational service use from medical home care components, controlling for predisposing, enabling, and need factors, in children and youth on the autism spectrum, ages 1-17 (n = 1,922). Non-significant predictors: personal doctor or nurse, usual source of sicks care, family centered care, doctor communication with early intervention, child care providers, or special education programs, satisfaction with communication with early intervention, child care providers, and special education programs, child race/ethnicity, adult education level, maternal mental health, family structure, insurance type, income, primary household language, number of ACEs (continuous, 0-9), and age at autism diagnosis (continuous, yrs).
This study included data on 1,922 children and youth aged 1–17 on the autism spectrum (M = 10.5 years), most of whom received all six medical home care components (see Table 1). Many children and youth were White, Non-Hispanic (63.5%), had public insurance alone or combined with private insurance (49.8%), earned > 201% above the FPL (44.9%), with moderate/severe autism (48.6%). Most caregivers who were sampled reported higher maternal mental health status, and most of the children and youth sampled experienced at least one ACE (M = 1.2).
Bivariate analyses revealed significantly higher rates of current educational service use with difficulty obtaining referrals (87.7%) and no shared decision-making (82%). Approximately 86% of children and youth on the autism spectrum, whose primary household language was English, were currently using educational services, compared with children and youth whose primary household language was Spanish or other (14%; see Appendix A).
Multivariate analyses began with Model 1 containing the six medical home care components. Children and youth on the autism spectrum whose caregivers had difficulty getting referrals had significantly higher odds of current educational service use [OR = 2.69; 95% confidence interval (CI), 1.36 – 5.33, P = 0.005] Additionally, children and youth on the autism spectrum with no shared decision-making had significantly higher odds of current educational service use (OR = 2.30; 95% CI, 1.17 – 4.52, P = 0.015; see Appendix B or Figure 1A).
In Model 2, the odds of current educational service use with difficulty getting referrals decreased but remained statistically significant, after controlling for predisposing factors (OR = 2.58; 95% CI, 1.26 – 5.27, P = 0.009). Children and youth whose caregivers reported no shared decision-making sustained a higher likelihood of current educational service use, after controlling for predisposing factors (OR = 2.67; 95% CI, 1.26 – 5.65, P = 0.010). Older children and youth had significantly lower odds of current educational service use (see Appendix B or Figure 1B).
In Model 3, the odds of current educational service use for those with difficulty getting referrals (OR = 2.96; 95% CI, 1.36 – 6.42, P = 0.006) and no shared decision-making (OR = 2.96; 95% CI, 1.24 – 7.05, P = 0.014) increased, after controlling for predisposing and enabling factors. Specific enabling factors did not affect the lower likelihood of current educational service use for older children and youth on the autism spectrum (see Appendix B or Figure 1C).
In Model 4, the odds of current educational service use were higher for those with difficulty getting referrals (OR = 2.93; 95% CI, 1.33 – 6.41, P = 0.006) and no shared decision-making (OR = 2.93; 95% CI, 1.22 – 7.06 P = 0.016) in the fully adjusted model. Predisposing factor of child age (i.e., older children and youth) was significantly associated with less likelihood of current educational services (OR= 0.91, 95% CI, 0.85, 0.97, P = 0.003) and autism severity (i.e., moderate/severe) was significantly associated with higher odds of current educational service use (OR= 1.80, 95% CI, 1.10, 2.95, P = 0.019; see Appendix B or Figure 1D).
This study further establishes a negative association between medical home care in relationship to educational service use for children and youth on the autism spectrum, accounting for predisposing, enabling, and need factors. Findings also extend prior evidence in two ways: (1) by specifying two of six medical home care components, referral difficulty, and no shared decision-making, as being associated with a higher likelihood of current educational service use, and (2) confirming that this inverse cross-sector relationship is attenuated by older child age and intensified by greater autism severity. In this study, children and youth on the autism spectrum, especially those with moderate or severe autism, had a higher likelihood of current educational service use, except if they were older, had difficulty getting referrals from medical home providers, and experienced no shared decision-making in their medical home care. These results indicate that children and youth on the autism spectrum in this study gain access to educational services considering unmet need for medical home referral and shared decision-making. Although the medical and educational systems have made advancements in providing care to children and youth on the autism spectrum, caregivers often assume the role of coordinator between these service systems and, consequently, experience increased caregiver stress, increased confusion, and inconsistent information between each system's providers (Carbone et al., 2010). In addition, it sustains the current “three components” service model, separating caregivers, medical, and educational professionals (Williams et al., 2012).
When autism spectrum concerns are raised during the provision of medical home care, the PCP should make two important referrals: (1) for diagnostic evaluation by an autism specialist, and (2) educational evaluation to determine eligibility for EI or special education (Carbone et al., 2010). Our findings specific to difficulty getting these referrals can be explained in three ways. First, caregivers of children referred to an EI program commonly express attitudinal and communication problems getting these referrals (Carbone et al., 2010). Information about the EI referral process and the services provided are not always conveyed to parents (Sobotka et al., 2016), and fewer parents reported making referrals to autism spectrum specialists. Consequently, these findings may explain why caregivers are pursuing their option to self-refer their child or managed through friends, other families, and/or the media vs. waiting for a physician referral. Second, workload issues such as increased referral volumes and demands, and reimbursement for non-billable time expended on care coordination hinder referral processes (Williams et al., 2012). Third, workforce capacity needs persist, such as limited availability of fellowship-trained developmental and behavioral providers; medical home providers can lack understanding of special education services for counseling families in how to obtain special education services (Shahidullah et al., 2018) that vary from state to state (Williams et al., 2012; Barger et al., 2021). For example, only 51% of physicians reportedly felt comfortable providing information to caregivers in IEP development, and 38% of caregivers reported physicians' difficulty answering educationally related questions (Rizk et al., 2023). Many physicians have reported never attending widely available continuing medical education or other autism training, other upstream approaches to support physicians' need for autism training have included embedding autism content in medical school curricula and or residency programs serving children and youth on the autism spectrum (i.e., schools or psychiatry placements) (34).
Similarly, no shared decision-making via medical home care was significantly associated with a higher likelihood of current educational service use. Shared decision-making involves medical home care providers collaborating with caregivers to establish evidence-based medical care plans that are responsive to caregivers' goals and priorities (Edwards et al., 2018). As eligibility determination for educational services and service plan design are required to be conducted with family involvement, caregivers may experience shared decision-making for educational service use as indicated by receipt of an IFSP or IEP. Alternatively, caregivers have experience making decisions on how to manage their child or youth's conditions (e.g., prescription medications, scope of available skilled, therapeutic, and complementary alternative medicine (CAM) service options; Ellerbeck et al., 2015). In one study, EI providers had significantly higher ratings than PCS on the MPOC-20 for enabling and partnership domain (i.e., “…explain treatment choices to you” and “…provide opportunities for you to make decisions about treatment”; Aloisio and Huron, 2020). In another study, most pediatricians were reportedly willing to engage with families who approached them for support in treatment decisions (Carbone et al., 2010). This increases caregivers' propensity to initiate and bridge the gap between health and educational systems by demonstrating their expertise in making decisions on how to manage their child's conditions and receipt of services. These caregivers with acquired expertise in decision-making (Williams et al., 2012) may challenge providers and information they receive concerning their child's diagnosis and/or service plan. We also found that shared decision-making demonstrated good internal consistency. Shared decision-making included the NPM-11 may be worth further unpacking to understand specific qualities of shared decision-making that drive this association (Data Resource Center for Child Adolescent Health, 2021).
Older children and youth had significantly lower odds of current educational service use. Educational transitions (e.g., EI to special education, high school to postsecondary, or vocational roles) may place children and youth on the autism spectrum and their families in particularly vulnerable positions related to decreased service intensity from EI to early childhood special education (Aloisio and Huron, 2020) and getting referrals and shared decisions about scope and intensity of service options and vocational roles. One study of children and youth aged 2–17 found that older child age was associated with a greater likelihood of poorer care coordination perceptions (Sobotka et al., 2016). Our study's sample may not yet have experienced the waning of services and supports commonly associated with transition to adulthood.
Autism spectrum severity was linked to higher likelihood of current educational service use. Based on the extent that cognitive, physical, communication, social, emotional, or adaptive skills are affected, greater autism condition severity may facilitate referral for comprehensive evaluations to determine educational service eligibility and environment (e.g., regular classroom environment or other least restrict environment; Christiansen et al., 2021).
Neither maternal mental health nor a number of child ACEs were significantly associated with current educational service use. These findings depart from existing literature suggesting current educational service use disparities for those with mothers with lower overall maternal health (Berg et al., 2016), higher ACEs, delayed autism spectrum identification, and accessing intervention (Hoover and Kaufman, 2018). This study measured maternal mental health only and a number of ACEs that may provide insufficient inferential information with measuring number of ACEs on a continuous scale.
Localized health records may help to further assess this type of service disparity, as health visits or encounters are documented by electronic data capture systems (e.g., point of care, demographic data, and referral information) related to referral processes or engaging families within the medical home sector. Localized health data affords for systematized use of coding systems (e.g., International Classification of Diseases (ICF) for diagnostic data, the Current Procedural Terminology (CPT) codes for clinical services rendered), that when integrated with sociodemographic data, can support reliable interpretation of electronic health information (Dankwa-Mullan et al., 2021).
This study has limitations. The NSCH uses caregiver-reported data, which may produce biased estimates of autism diagnoses, receipt of certain medical home care components, and current educational service use. NSCH data solicit medical home care experiences retrospectively (e.g., “During the past 12 months”) and may be subject to recall bias. Our study uses a cross-sectional design that does not permit causal inferences between explanatory and outcome variables.
Findings revealed difficulties getting referrals and no shared decision-making are medical home care components that are significantly correlated with current educational service use among children and youth on the autism spectrum. New inquiries may potentially show differences in educational service use by comparing the temporal data elements of educational service use captured by the NSCH (i.e., “ever” vs. “current” educational service use). Future studies should also examine how the medical home referral and shared decision-making pathways operate and assess how these pathways work and how specific sociodemographic characteristics drive their higher likelihood of current educational service use.
Publicly available datasets were analyzed in this study. This data can be found at: https://mchb.hrsa.gov/national-survey-childrens-health-questionnaires-datasets-supporting-documents.
The studies involving human participants were reviewed and approved by University of Illinois Chicago. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
SR, KB, and MK contributed to conception and design of the study. CS organized the database. SR, TB, and CS performed the statistical analyses. SR wrote the first draft of the manuscript. TB, CS, KB, and MK wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
This study was supported by the University of Illinois Chicago Bridge to Faculty Postdoctoral Scholars Program in Occupational Therapy and the Children's Participation in Environment Research Lab.
MK declares an affiliation as an Associate Editor for Frontiers in Pediatrics, Frontiers in Public Health, and Frontiers in Rehabilitation Sciences.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/feduc.2023.1125929/full#supplementary-material
Aloisio, D., and Huron, R. F. (2020). Autism as representative of disability. Pediatr. Clin. North Am. 67, 341–355. doi: 10.1016/j.pcl.2019.12.008
American Academy of Pediatrics (2002). American of pediatrics medical home initiatives for children with special needs project advisory committee the medical home. Pediatrics 110, 184–186. doi: 10.1542/peds.110.1.184
Andersen, R. M. (1995). Revisiting the behavioral model and access to medical care: Does it matter? JHSB 36, 1–10. doi: 10.2307/2137284
Barger, B. D., Rice, C. E., and Roach, A. T. (2021). Developmental screening and monitoring are associated with increased preschool special education receipt. J. Child Fam. Stud. 30, 1342–1352. doi: 10.1007/s10826-021-01940-4
Berg, K. L., Shiu, C., Acharya, K., Stolbach, B. C., and Msall, M. E. (2016). Disparities in adversity among children with autism spectrum disorder: A population-based study. Dev. Med. Child Neurol. 58, 1124–1131. doi: 10.1111/dmcn.13161
Carbone, P., Behl, D., Azor, V., and Murphy, N. A. (2010). The medical home for children with autism spectrum disorders: Parent and pediatrician perspectives. J. Autism Dev. Disord. 40, 317–324. doi: 10.1007/s10803-009-0874-5
Christiansen, J., White, S. W., McPartland, J., Volkmar, F., Parlar, S., Pedersen, L., et al. (2021). Child characteristics associated with educational placement of children on the autism spectrum. Educ. Train Autism Dev. Disabil. 56, 466–478.
Dankwa-Mullan, I., Pérez-Stable, E. J., Gardner, K. L., Zhang, X., and Rosario, A. M. (2021). The Science of Health Disparities Research. Hoboken, NJ: John Wiley & Sons, Incorporated.
Data Resource Center for Child Adolescent Health U.S. Department of Health Human Services Health Resources Services Administration, Maternal Child Health Bureau. (2021). Child and Adolescent Health Measurement Initiative. Child and Family Health Measures Content Map, 2020 National Survey of Children's Health. Available online at: https://www.childhealthdata.org/docs/default-source/nschdocs/2020-nschcontent-map_child-and-family-health-measures_cahmi_9-2421.pdf?sfvrsn=aac65f17_6 (accessed September 6, 2022).
Eddings, W., and Marchenko, Y. (2012). Diagnostics for multiple imputation in Stata. Stata J. 12, 353–367. doi: 10.1177/1536867X1201200301
Edwards, A. G., Brebner, C. M., McCormack, P. F., and MacDougall, C. J. (2018). From ‘parent' to ‘expert': How parents of children with autism spectrum disorder make decisions about which intervention approaches to access. J. Autism Dev. Disord. 48, 2122–2138. doi: 10.1007/s10803-018-3473-5
Ellerbeck, K., Smith, C., and Courtemanche, A. (2015). Care of children with autism spectrum disorder. Prim. Care 42, 85–98. doi: 10.1016/j.pop.2014.09.004
Hardt, J., Herke, M., Brian, T., and Laubach, W. (2013). Multiple imputation of missing data: A simulation study on a binary response. Open J. Stat. 3, 370–378. doi: 10.4236/ojs.2013.35043
Health Resources Administration Maternal Child Health (2020). Adverse Childhood Experiences: NSCH Data Brief . Available online at: https://mchb.hrsa.gov/sites/default/files/mchb/data-research/nsch-ace-databrief.pdf (accessed September 6, 2022).
Heeringa, S., West, B. T., and Berglund, P. A. (2017). Applied Survey Data Analysis, 2nd Edn. Boca Raton, FL: CRC Press.
Hoover, D., and Kaufman, J. (2018). Adverse childhood experiences in children with autism spectrum disorder. Curr. Opin. Psychiatry 31, 128–132. doi: 10.1097/YCO.0000000000000390
King, S., King, G., and Rosenbaum, P. (2004). Evaluating health service delivery to children with chronic conditions and their families: Development of a refined measure of processes of care (MPOC−20). Child Health Care 33, 35–57. doi: 10.1207/s15326888chc3301_3
Limbers, C. A., Gutierrez, A., and Cohen, L. A. (2020). The patient-centered medical home: Mental health and parenting stress in mothers of children with autism. J. Prim. Care Community Health 11, 2150132720936067. doi: 10.1177/2150132720936067
Lipkin, P. H., and Okamoto, J. (2015). The individuals with disabilities education act (IDEA) for children with special educational needs. Pediatrics 136, e1650–e1662. doi: 10.1542/peds.2015-3409
Long, W. E., Cabral, H. J., and Garg, A. (2013). Are components of the medical home differentially associated with child health care utilization, health, and health promoting behavior outcomes? Clin. Pediatr. 52, 423–432. doi: 10.1177/0009922813479161
McManus, M. A., Pollack, L. R., Cooley, W. C., McAllister, J. W., Lotstein, D., Strickland, B., et al. (2013). Status of transition preparation among youth with special needs in the United States. Pediatrics 131, 1090–1097. doi: 10.1542/peds.2012-3050
Montes, G., and Halterman, J. S. (2011). White-black disparities in family-centered care among children with autism in the United States: Evidence from the NS-CSHCN 2005–2006. Acad. Pediatr. 11, 297–304. doi: 10.1016/j.acap.2011.02.002
Raphael, J. L., Guadagnolo, B. A., Beal, A. C., and Giardino, A. P. (2009). Racial and ethnic disparities in indicators of primary care medical home for children. Acad. Pediatr. 9, 221–227. doi: 10.1016/j.acap.2009.01.011
Rizk, S., Ngui, E., Benevides, T., Moerchen, V. A., Khetani, M. A., Barnekow, K., et al. (2023). Adequacy of medical home primary care and factors associated with educational services use among children and youth with autism spectrum disorder (ASD). BMC Pediatri. 23, 3. doi: 10.1186/s12887-022-03776-3
Ronis, S. D., Baldwin, C. D., Blumkin, A., Kuhlthau, K., and Szilagyi, P. G. (2015). Patient-centered medical home and family burden in attention-deficit hyperactivity disorder. J. Dev. Behav. Pediatr. 36, 417–425. doi: 10.1097/DBP.0000000000000161
Shahidullah, J. D., Azad, G., Mezher, K. R., McClain, M. B., and McIntyre, L. L. (2018). Linking the medical and educational home to support children with autism spectrum disorder: Practice recommendations. Clin. Pediatr. 57, 1496–1505. doi: 10.1177/0009922818774344
Sobotka, S. A., Francis, A., and Vander Ploeg Booth, K. (2016). Associations of family characteristics with perceptions of care among parents of children with autism. Child Care Health Dev. 42, 135–140. doi: 10.1111/cch.12290
Toomey, S. L., Homer, C. J., and Finkelstein, J. A. (2010). Comparing medical homes for children with ADHD and asthma. Acad. Pediatr. 10, 56–63. doi: 10.1016/j.acap.2009.11.001
US Census Bureau (2019). National Survey of Children's Health. Methodology Report. United States Department of Commerce Economics and Statistics Administration. Available online at: https://www2.census.gov/programs-surveys/nsch/technical-documentation/methodology/2019-NSCH-Methodology-Report.pdf (accessed September 6, 2022).
Weedon, D., Carbone, P., Bilder, D., O'Brien, S., and Dorius, J. (2012). Building a person-centered medical home: Lessons from a program for people with developmental disabilities. J. Health Care Poor Underserved 23, 1600–1608. doi: 10.1353/hpu.2012.0175
Keywords: referral and consultation, decision-making, shared, autism spectrum, early intervention, educational, education, special
Citation: Rizk S, Benevides TW, Shiu CA, Berg KL and Khetani MA (2023) Medical home primary care components and current educational service use in children and youth on the autism spectrum. Front. Educ. 8:1125929. doi: 10.3389/feduc.2023.1125929
Received: 16 December 2022; Accepted: 24 March 2023;
Published: 18 May 2023.
Edited by:
Emily Hotez, UCLA Health System, United StatesReviewed by:
Brianne Tomaszewski, University of North Carolina at Chapel Hill, United StatesCopyright © 2023 Rizk, Benevides, Shiu, Berg and Khetani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sabrin Rizk, c3JpemtAdWljLmVkdQ==
†These authors have contributed equally to this work and share senior authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.