- 1School of Education, University of California, Riverside, Riverside, CA, United States
- 2TNTP, New York, NY, United States
- 3Autism Society of California, San Diego, CA, United States
Introduction: During the early beginnings of COVID-19, service providers were forced to close their doors and move their services online, causing significant disruptions for many families and communities, such as those with intellectual and developmental disabilities (IDD). In this study, we examined the extent to which COVID-19 disrupted services for the IDD community in California.
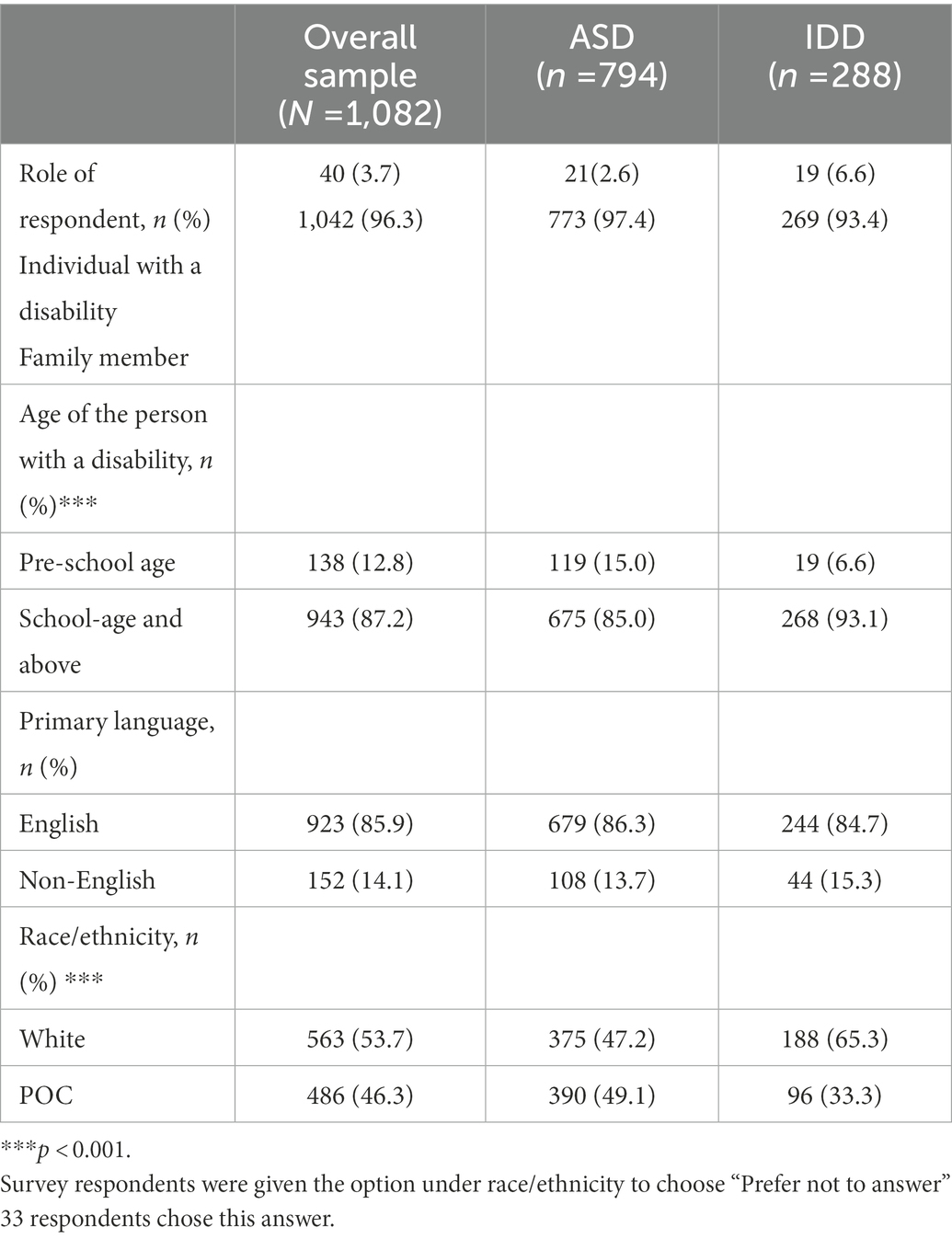
Methods: Secondary data were analyzed from a survey (N = 1,082) disseminated by the Autism Society of California in May 2020. Respondents were placed into two categories: autism spectrum disorder (ASD) only (n = 794) and IDD other than ASD (n = 288).
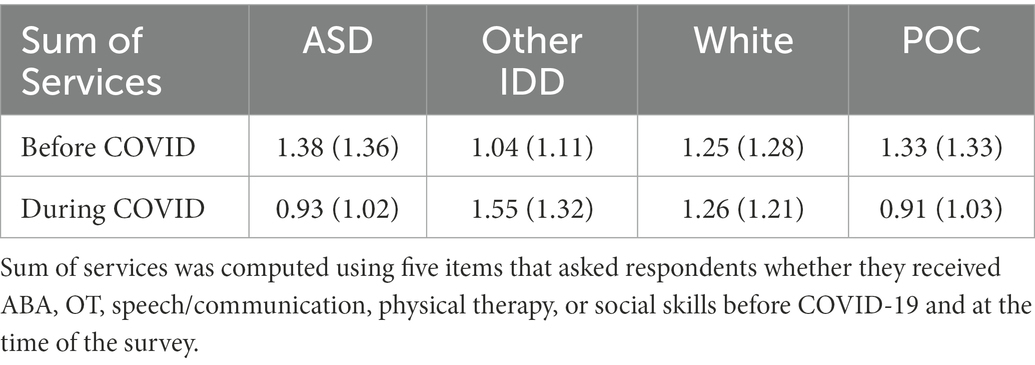
Results: There were significant differences in services between diagnostic groups (<.05). There was a threefold difference in loss of respite services in the ASD (4.3%) versus the IDD group (12.9%). In the ASD group, 48.5% reported no change at all in respite services received, whereas in the IDD group, 71.5% reported no change. Before the pandemic, a higher mean number of medical and therapeutic services was reported as received in the ASD group (M = 1.38) than in the IDD group (M = 1.04). However, at the time of the survey, the IDD group reported a higher mean number of such services (M = 1.32) than the ASD group (M = 1.02). Differences were also seen by race/ethnicity. Before lockdown, there were no significant differences in the mean number of services reported by race/ethnicity among the full sample. However, at the time of the survey, a significantly higher mean number of services was reported by respondents who identified as White (M = 1.26) compared to people of color (M = .91), p < .05.
Discussion: To our knowledge, this study is the first to compare services received by IDD diagnostic groups during COVID-19. Findings help elucidate the negative impact of COVID-19 on the IDD community in California, as well as inform strategies for the ongoing and post-pandemic periods.
1. Introduction
In December 2019, the coronavirus (or COVID-19) was first identified in Wuhan, China which later spread across the world, including the United States, creating nationwide lockdowns and quarantine orders (Li et al., 2020). During this period, service providers were forced to close their doors and move their services online, causing significant disruptions for many families and communities (Ameis et al., 2020). Such closures particularly affected individuals with intellectual and developmental disabilities (IDD) and their families, who have been identified as a vulnerable population to pandemic-related issues, such as greater risk of infection and lack of access to medical information (Courtenay and Perera, 2020).
1.1. Needs of the intellectual and developmental disabilities community and families
Intellectual and developmental disabilities are pervasive, life-long conditions. Within this diagnostic group, persons with intellectual disability (ID) have impairments in intellectual and adaptive functioning (American Psychiatric Association, 2013), while those with developmental disabilities can have difficulties in one or more global domains, such as learning, physical abilities, language, and behavior (Zablotsky et al., 2019). Among IDDs, autism spectrum disorder (ASD) is frequently diagnosed, with 1 in 44 children identified by age 8 (Maenner et al., 2021). Individuals with ASD experience challenges with social communication and restricted and repetitive behaviors (American Psychiatric Association, 2013).
As part of the law in the United States, caregivers of children with IDDs are granted access to free educational and related services until age 21/22 (Individuals With Disabilities Education Improvement Act, 2004). Services such as applied behavior analysis, speech therapy, and respite care are one of the many services that could be provided to families. Such services have been shown to be beneficial for children with IDD and reduce caregiver stress (Harper et al., 2013; Grenier-Martin et al., 2022). Although these services are mandated by law to be provided to families that qualify for them, families of children with IDD have historically experienced challenges in accessing appropriate services and support to address their children’s social, behavioral, and developmental needs (Vohra et al., 2014), including long waitlists and limited access to specialists (Mayer, 2006; Pletcher et al., 2010; Chiri and Warfield, 2012; Vohra et al., 2014).
Furthermore, youth with ASD experience significantly more challenges receiving quality care and services than those with other IDDs (Magaña et al., 2012). In a study of the National Survey of Children with Special Health Care Needs, caregivers of children with ASD were more likely to report poor outcomes on health care quality measures relative to the overall sample of children with other IDDs (Magaña et al., 2012). For example, these caregivers reported that healthcare providers did not provide enough information or spend enough time with their children and were not sensitive to the family’s values and customs. The study also found a significant effect for race/ethnicity across all quality-of-care outcomes, suggesting that negative outcomes were exacerbated for persons of color (POC), particularly Latine and Black families of children with ASD (Magaña et al., 2012).
Additionally, prior work has identified mental health concerns among caregivers of children with IDD who are responsible for childcare duties (Singer, 2006; Hayes and Watson, 2013); thus respite care has been employed to relieve caregivers of caretaking duties and stress (Harper et al., 2013; Dyches et al., 2016). Respite care can be provided through a professional that comes into the home temporarily, or caregivers can request that another family member provide the respite care within the home. In California, regional center clients can request respite care through their caseworker (Services for the Developmentally Disabled, Welfare and Institutions, 1977). These temporary short breaks have been found to reduce stress for caregivers of children with disabilities (Robertson et al., 2011) and to improve psychological adjustment and lessen fatigue (Remedios et al., 2015). During the pandemic, respite care may have been particularly important for these families.
1.2. COVID-19 impact on the intellectual and developmental disabilities community
At the height of the pandemic, many young children were unable to receive early intervention services because of limited support staff and safety concerns during the early stages of the pandemic, and these children may have missed out on weeks of intervention during critical periods (Guralnick, 2011; Zwaigenbaum et al., 2015). Moreover, during lockdowns and social distancing, service providers switched to online administration (e.g., telehealth), forcing caregivers to acclimate to new methods. Some families may not have had the necessary resources (e.g., access to technology) to engage feasibly, reliably, and comfortably in online services (Stavropoulos et al., 2022).
Furthermore, caregivers of children with IDD may face even more mental health concerns than caregivers of children with other disabilities (Singer, 2006; Hayes and Watson, 2013) and those without disabilities (Scherer et al., 2019). In the context of the pandemic, studies found that caregivers of children with IDD experienced mental health issues, such as higher amounts of anxiety (Friesen et al., 2021), strain on caregiver well-being (Ersoy et al., 2020; Lee et al., 2021), elevated levels of stress and depression (Linehan et al., 2022). Some explanations for the rise in mental health issues during the pandemic pertain to financial hardships and loss of services (Friesen et al., 2021), as well as to disruptions in routines (Ameis et al., 2020). Caregivers may have been particularly burdened as they, primarily mothers, had to balance working from home while facilitating their children’s learning at home (Parenteau et al., 2020). Not only were caregivers impacted by the pandemic but so were their children by these rapid changes due to the pandemic. For example, many children with ASD insist on sameness in their routines, but the shifting to online schooling created some distress for children who were not used to these new changes (Ameis et al., 2020). These added stressors have also been found to impact other behaviors associated with ASD, such as an increase in behavioral meltdowns, sensory issues, and self-stimming behaviors (Genova et al., 2021). Given these challenges faced by both caregivers and children with ASD, it is important to examine ASD and other IDD groups separately, and in comparison to each other.
Other explanations for the increase in mental health issues pertain to behavioral challenges of children with IDD. Young et al. (2021) published a case study report recognizing that caregivers of youth with IDD faced caregiver burnout before the pandemic. The report found that stay-at-home orders exacerbated caregiver burnout among children with significant behavioral challenges. Similarly, in a study of Italian caregivers (n = 527) of children with ASD, children who presented with behavioral problems before the pandemic had a statistically significant higher risk for more frequent and intense behavioral problems during the pandemic (Colizzi et al., 2020). Qualitative interviews with 15 caregivers of children with ASD in the United States also support findings of increased child behavior problems since COVID-19 (Parenteau et al., 2020). Two months after the COVID-19 lockdown in the United States (May–June-2020), children with ASD experienced more psychiatric problems (Vasa et al., 2021), including ADHD-related symptoms and disruptive behavior. This increase was correlated with children’s understanding of COVID-19, whether someone in the household had been diagnosed with COVID-19, higher caregiver-reported psychopathology symptoms, and lower income. Pre-pandemic literature has consistently demonstrated that children’s behavioral problems can negatively impact family daily routines (Rodriguez et al., 2019). These findings are alarming, given that children with IDD likely experienced changes in support services during the pandemic, a time when these services may have been needed most.
Studies found that service disruptions resulting from the pandemic, such as medical and educational service changes, have been a cause of strain on individuals with IDD and their caregivers. In a large survey of 6,000 caregivers and caregivers of children with ASD in the United States, over 70% of respondents reported disruptions to school services (Bhat, 2021). School closures also widened inequities for children with disabilities and those within underserved communities (Armitage and Nellums, 2020; Termine et al., 2021). Neece et al. (2020) interviewed 77 Latine caregivers of children with ASD or other developmental disabilities from March to May 2020. They found that about 78% of caregivers reported decreased services for their children. These findings are consistent with other survey data that investigated the healthcare and educational services of individuals with neurodevelopmental and genetic disorders during the early stay-at-home orders. They found that over 70% of the survey respondents who resided in the United States had lost at least one therapy or educational service (Jeste et al., 2020).
Similarly, a global survey disseminated in August–September of 2020 found that 34.6% of caregivers reported receiving a new or alternative service to replace canceled or reduced services caused by the pandemic (Linehan et al., 2022). The disruption of services affected children as well as adults with IDD. Rosencrans et al. (2021) surveyed adults in July 2020 who were over the age of 18 with IDD (N = 404) about their access to state-operated services (e.g., mental health, developmental services). The study found that 81% of adults with IDD reported having state-operated services before COVID-19. Among this subgroup, 71% reported still receiving services, while 19% reported not receiving services at the time of the survey. Over a quarter of respondents (31%) reported having difficulties accessing services, and 44% reported changes in their services. Adults with IDD who no longer received state-operated services were more likely to report mental health symptoms than those who continued receiving services. This demonstrates that COVID-19 had an immediate impact on the IDD community. The current study examines the impact of the pandemic on access and receipt of medical, therapeutic, and respite service care for families of youth with ASD and IDD, paying particular attention to sociodemographic factors (e.g., race/ethnicity, age) that may influence service disruption (i.e., respite and other medical therapeutic services).
1.3. Current study
The current study is a secondary data analysis of service access and use among families of youth with IDD in California during May 2020. During this time, California had been in lockdown for approximately 3 months, and the United States had surpassed 100,000 COVID-19 deaths (Centers for Disease Control and Prevention, 2021). The purpose of the study was to examine the extent to which COVID-19 disrupted services for the IDD community in California, a state that comprises roughly 12% of the United States population (United States Census Bureau, 2022) and accounts for 15% of the country’s total GDP (Buchholz, 2022). We compared data from respondents with a primary diagnosis of ASD to those with other IDDs (referred to as the IDD group). The reason for doing this was three-fold: First, previous research has shown that families of children with ASD experience significantly more difficulties in accessing services and quality care compared to families of children with IDD (Magaña et al., 2012). Second, children with ASD are reported to have significantly more persistent and pervasive behavior problems than same-age children with IDD (e.g., Mayes et al., 2012). As a result of high levels of behavior problems, families of children with ASD are often more negatively impacted than those of children with other IDDs (Rodriguez et al., 2019). Third, from preliminary studies of COVID-19, the ASD population continues to show poorer outcomes compared to other disability groups and the general population (Ersoy et al., 2020; Lee et al., 2021).
Two primary research questions were addressed in the context of these data collected during the pandemic: (1) How did COVID-19 disrupt medical or therapy services for the ASD and IDD community in California? (2) What were predictors of service access, receipt, and perceived support for ASD and IDD regional center clients? We addressed these questions by utilizing survey data from persons with IDD and their family members in California. For each question, we examined sociodemographic correlates of stakeholder needs, experiences, and concerns. We hypothesized that there would be differences in key outcomes by disability group.
2. Methods
The current study involved secondary data analysis utilizing an online survey distributed by the Autism Society of California (ASC) to individuals with IDD and their family members. Institutional Review Board approval was granted by the University of California, Riverside to access and analyze the gathered data in May 2020.
The ASC collected survey data every 2 years, since 2012; the current version was developed in English and translated into Spanish. Topics addressed in the survey were based on historical precedent as well as issues affecting the community at the time, as reported by the nine ASC chapters. This survey was disseminated by the ASC with the overall purpose of understanding how COVID-19 has affected the daily lives of families who have children and youth with IDD, e.g., how COVID-19 disrupted the IDD community’s medical, educational, and regional center service access. Survey items also addressed barriers to reintegration after COVID-19 and what individual families desired to help them feel safe. The goal of the survey was to help inform re-engagement and planning strategies that were being developed during COVID-19.
2.1. Survey procedure
The survey was distributed electronically through Survey Monkey. Nine ASC chapters and community partners such as regional centers, Easter Seals, and the Arc of California, United Cerebral Palsy, and smaller community-based organizations were asked to distribute electronic surveys (email) to families within their network. Multiple reminders were sent to families to respond to the survey. We do not know the exact number of times each community-based organization sent out reminders, nor the exact number sent out. The invitation to participate included a description of the survey, study aims, and procedures. Completion of the survey was regarded as informed consent. Upon completing the survey, respondents were given the option to enter their names into a drawing for a $150 gift card. The survey was open for 2 weeks.
2.2. Study sample
In total, 1,111 individuals (persons with IDD [ASD, ID, and other developmental disabilities] and their family members) responded to the survey. Survey data (n = 29) were omitted if respondents: (a) identified as a person with a disability and a family member of a person with a disability due to concerns about the accuracy of respondents’ answers (n = 11); (b) reported being under 18 years of age (n = 11); and (c) identified as being a service provider (n = 1). Open-ended responses were systematically searched to eliminate responses that: (d) provided identical answers on any of the items due to concerns that the same person completed the survey more than once (n = 5); and (e) indicated that the respondent did not live in California (n = 1). The final sample consisted of 1,082 participants.
2.3. Instrument
The survey was designed by the ASC to assess the service needs and concerns of the IDD population in California during COVID-19. The survey consisted of three general sections: demographic information, services (i.e., regional center, school, employment, day services), and family life. The current study focuses on items related to regional center services. It should be noted that not all respondents (n = 174) were regional center clients but were receiving similar services and were thus eligible for this study.
There were 39 questions in the original survey, but our secondary analysis included those pertaining to regional centers and medical and therapeutic services (i.e., 17 of the 39 questions). Out of the 17 questions used, 15 were categorical (five included an “other please specify)” option where respondents could provide further information. There were two open-ended questions which asked respondents what regional center they were associated with and what county they lived in. There were no questions with continuous variables. The original survey can be made available upon request.
Demographic information was collected through multiple-choice questions for respondent type, primary diagnosis of the person with a disability, primary language spoken at home, age of the person with a disability, and race/ethnicity of the person with a disability. For analysis, respondents who identified as a family member, guardian, or spouse of a person with a disability were grouped as “family member.” A minority of respondents reported being a person with a disability (3.7%). Primary diagnosis was coded as a dichotomous variable: autism spectrum disorder (‘ASD’ as 1) versus all other diagnoses (‘Other IDD’ as 0). Other diagnoses included individuals with cerebral palsy, developmental delay, epilepsy, or intellectual disability, all of whom had cognitive needs commensurate with intellectual disability but no ASD.
Primary language, age, and race/ethnicity were used as predictor variables. Survey response options on these variables are shown in Table 1. Primary language was coded as English (1) and all else (0). Age was dichotomized as 0–5 years (i.e., pre-school age [1]) and 6 years or older (i.e., school-age and above [0]). Race/Ethnicity was coded as a dichotomous variable (White [1] vs. persons of color (POC) [0]) for analyses. Responses were coded as ‘White’ if respondents reported being White/Caucasian only or in addition to any other race.
Respondents were asked about their regional center status, including questions pertaining to: whether they were registered with a regional center (i.e., “As of today, is the person with a disability a regional center client?”), which regional center they were affiliated with (if any); whether they had contact with their regional center caseworker since the start of stay-at-home orders during the early pandemic period; level of satisfaction with caseworker (i.e., “Do you feel you received adequate support from your caseworker since COVID-19?”); and whether they accessed respite services provided through a regional center.
Respondents were asked whether specific services were received in the 3 months before COVID-19 and during the early pandemic period. The five medical services/therapies that were asked about were applied behavior analysis (ABA), occupational therapy (OT), communication therapy (e.g., speech, language, augmentative and alternative communication), social skills groups, and physical therapy (PT). Respondents were able to select more than one medical service/therapy.
2.4. Data analytic plan
All analyses were conducted using SPSS software (Version 26.0; IBM Corp, Armonk, NY, United States). Multi-category demographic variables were collapsed to create binary measures, and descriptive statistics were calculated, including percentages and means. Potential correlates (i.e., primary language, age, and race/ethnicity) of service needs and receipt were explored using chi-square tests by disability group. Post-hoc analysis involved pairwise comparisons with a Bonferroni correction. Significant findings (p < 0.05) at the bivariate level were deemed robust with an effect size ≥0.1 (i.e., Cramer’s V ≥ 0.1; Cohen, 1992).
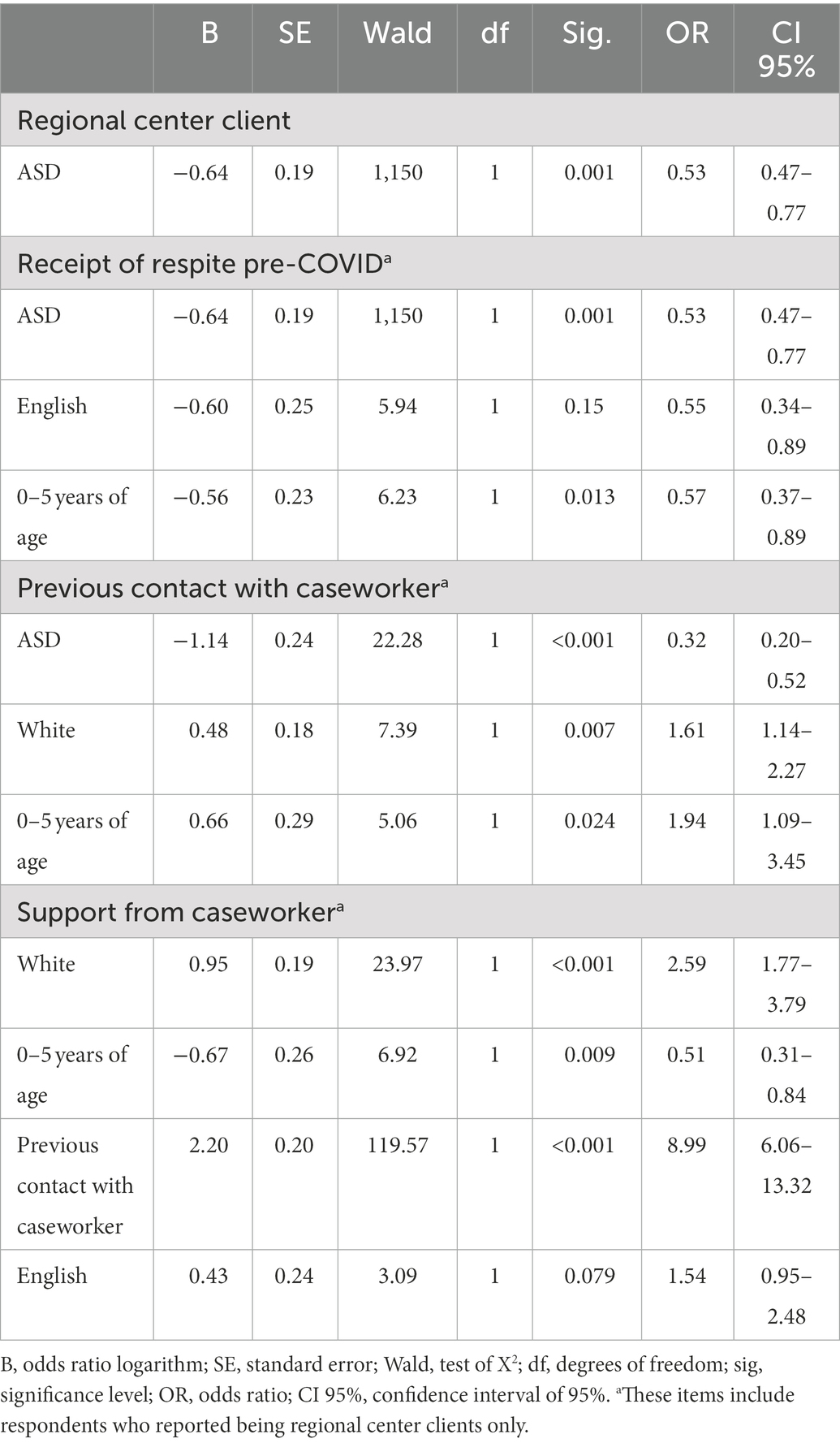
Binary logistic regression models were conducted to examine whether sociodemographic variables (i.e., diagnosis, age, language, race) significantly influenced (1) whether individuals with IDD were regional center clients, (2) whether they received respite care prior to COVID-19, (3) whether they had contact with their regional center caseworker in the early pandemic period, and (4) whether they felt supported by their caseworker. In addition, receipt of respite services before the pandemic was examined as a predictor of contact by the caseworker and experienced support from a caseworker during the early pandemic period; contact by the caseworker was also examined as a predictor of experienced support from a caseworker.
All outcome variables were utilized as categorical (“Yes” [1] or “No” [0]) variables. The sociodemographic predictor variables were diagnosis (ASD [1] vs. Other IDD [0]), race (White [1] vs. POC [0]), age (under 5 years [1] vs. 6 years and older [0]), and language spoken at home (English [1] vs. non-English [0]). Predictors that did not contribute at the p < 0.10 level were removed to avoid overfitting the model. Hosmer-Lemeshow Test was used as a measure of goodness of fit based on the Chi-square test. We present the odds ratios (ORs) estimating the relationship between sociodemographic correlates and service access, receipt, and perceived support for ASD and IDD regional center clients; their 95% confidence intervals (CIs) can be found in Table 4.
2.5. Missingness
Among demographic items, only data on language were missing, and for only 0.6% of the 1,082 respondents. There were small numbers of missing data on the following items: “Have you had any contact with your regional center caseworker?” (4.8%); “Which regional center are you affiliated with?” (9.0%); “Did you feel you have received adequate support from your caseworker since COVID-19?” (6.4%); “Did you receive respite services before COVID-19?” (4.4%). Of the 635 respondents who indicated receiving respite services, less than 1% had missing data on only two items: “Since COVID-19, has your respite service: increased, remained the same, decreased, stopped for a while, stopped completely” (0.5%); and “Are you aware that you can also refer family members or friends to be respite staff?” (0.8%). Listwise deletion was used in all analyses to enhance transparency.
3. Results
The sample consisted of 1,082 participants: 794 responding with respect to ASD and 288 respondents with respect to IDD. Of the ASD group, 71.4% identified as a family member of a person with ASD (n = 773), and 1.9% as a person with ASD (n = 21). Of the IDD group, 24.9% identified as a family member of a person with IDD (other than ASD; n = 269), and 1.8% as a person with IDD (other than ASD; n = 19). There were 960 surveys completed in English and 122 in Spanish. Table 1 presents demographic information about the sample. Chi-square analysis revealed a significant difference between diagnosis and race, (1) = 27.6, p < 0.001, as well as diagnosis and age, (1) = 13.3, p < 0.001. These variables (diagnosis, race, and age) were used as correlates in subsequent analyses. No other significant differences were observed between disability groups on demographic variables.
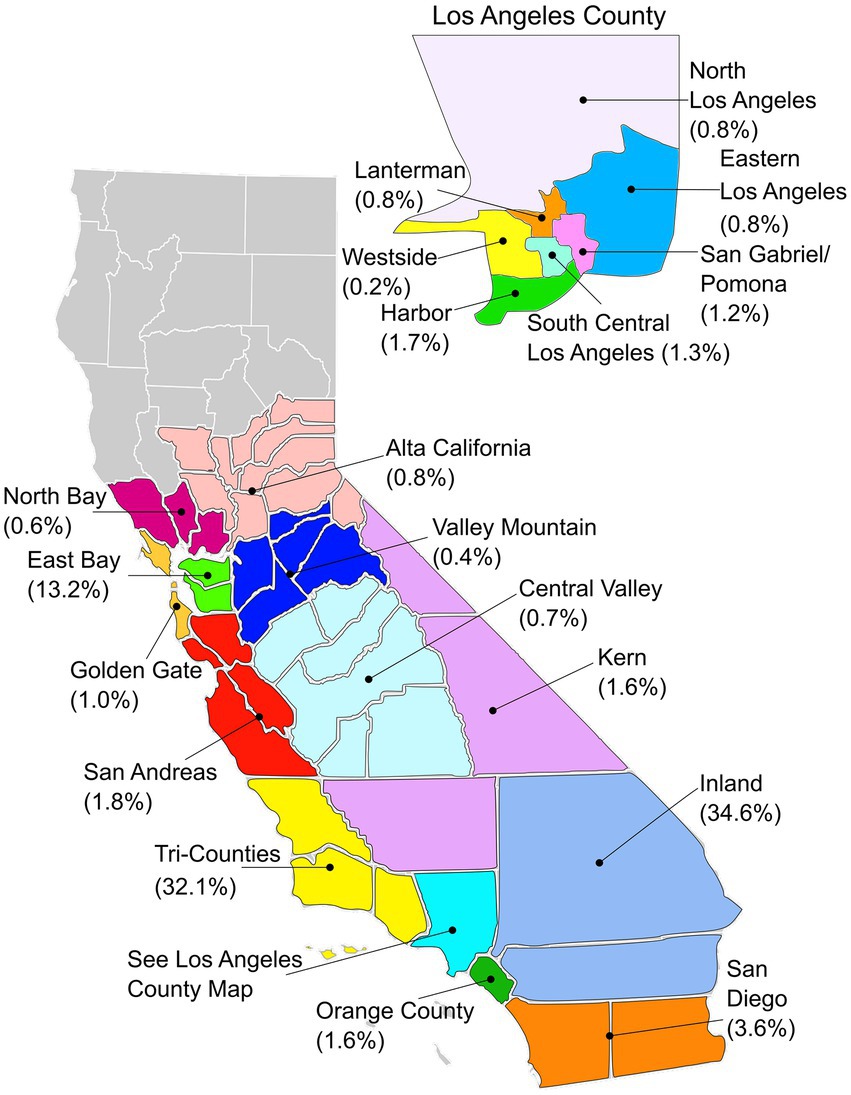
Of 1,082 participants, 908 (83.9%) reported that the person with a disability was a regional center client. While 147 (13.6%) respondents reported that the person with a disability was not a regional center client, 27 (2.5%) respondents were “not sure” about their status with regional center. When asked to indicate their affiliated regional center, 826 respondents responded to the question. Most respondents reported being registered with Inland Regional Center (34.6%), Tri-Counties Regional Center (32.1%), and Regional Center of the East Bay (13.2%); 0.7% were unsure of their regional center affiliation. Figure 1 displays the regional center catchment areas for the total sample. Overall, 615 (72.0%) respondents who were regional center clients reported receiving adequate support from their caseworker during the early pandemic, while 183 (21.2%) respondents reported not having any contact with their caseworker.
3.1. Receipt of medical or therapy services
This section covers service disruption to all respondents that participated in the survey, including regional center clients. The next section will cover predictors of service access.
3.1.1. Medical or therapy service delivery before and during COVID-19
All respondents were asked whether the person with IDD received specific medical services or therapies before COVID-19 and at the time of the survey during COVID-19. Frequencies and percentages of respondents who endorsed receiving any of the specific services are displayed in Table 2. Of the five services, only the receipt of OT and communication therapy decreased after the pandemic began. Service delivery via telehealth made up 73.8% of ABA, 93.3% of OT, 94.1% of communication, 91.9% of social skills groups, and 92.3% of PT services at the time of the survey.
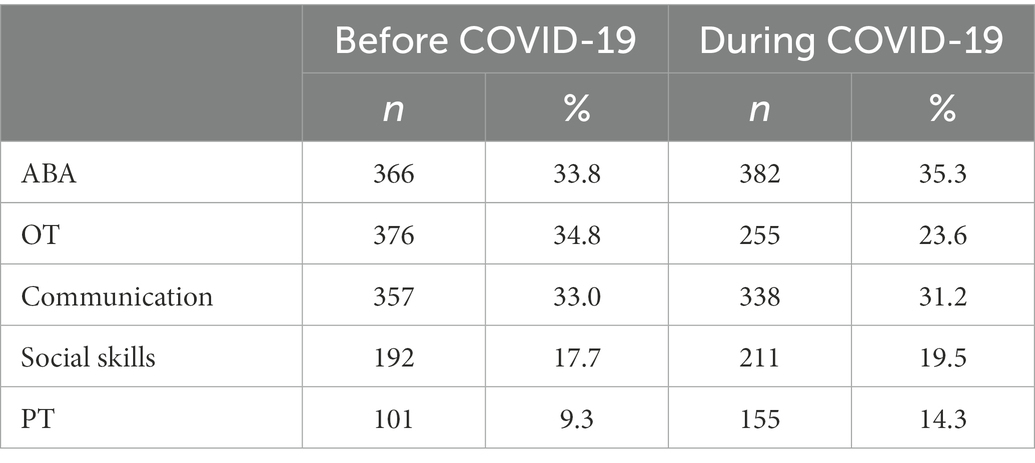
Table 2. Number and percentage of respondents who received specific services before and during COVID-19.
The five types of services received were summed to determine a total number. Descriptive statistics were calculated by disability group and race/ethnicity (shown in Table 3). Results of independent samples t-tests revealed that before COVID-19, a significantly higher mean number of services was reported in the ASD group than in the IDD group, t(619.13) = 4.10, p < 0.001. At the time of the survey, a significantly higher mean number of services was reported in the IDD group than in the ASD group, t(416.55) = 7.23, p < 0.001. No significant differences in the mean number of services was observed among the race/ethnicity categories before the pandemic. However, at the time of the survey, a significantly higher mean number of services was reported by respondents who identified as White compared to those who identified as persons of color (POC), t(1071.86) = 5.15, p < 0.001.
3.1.2. Regional center respite services disruption
Information was gathered from regional center clients about the frequency of respite care services received before the pandemic and changes that were incurred once stay-at-home orders were in place. Respite care is one in a menu of services regional centers offer. A large proportion of respondents (69.9%, n = 655) indicated receiving respite services before the pandemic. Notably, 14.0% (n = 127) of respondents indicated being unaware that they could utilize family members or friends as respite staff.
When asked about the frequency of respite services after the pandemic began, 101 (15.9%) respondents reported an increase in hours of services; 354 (55.7%) reported no change in how often they received respite; 14 (2.2%) reported a decrease in the number of hours; and 99 (15.6%) reported that while respite services stopped temporarily, they resumed. It is unknown how long respite services were temporarily halted or when they resumed during the 8-week period [i.e., since stay-at-home orders were mandated (March 19, 2020) until the time of survey completion (May 19, 2020)]. For 64 (10.1%) respondents, respite services stopped completely. Three respondents did not indicate the frequency of respite services (0.5%).
Changes in respite services since COVID-19 were compared by diagnostic group (ASD only vs. IDD). A chi-square test revealed significant differences in proportions across the two groups, (4) = 34.51, p < 0.001. A post hoc analysis involved pairwise comparisons using the z-test of two proportions with a Bonferroni correction found that a significantly smaller proportion of respondents in the ASD group (48.5%) reported having no change in respite services than those in the IDD group (71.5%), p < 0.05. The ASD group (12.9%) had a larger proportion of respondents whose respite services had stopped for a while but were later resumed compared to the IDD group (4.3%), p < 0.05. The percentage of respite services that stopped completely for the ASD group was more than double that of the IDD group (12.9% in the ASD group vs. 4.3% in the IDD group), p < 0.05. Figure 2 displays the change in respite services since COVID-19 as percentages between the two groups.
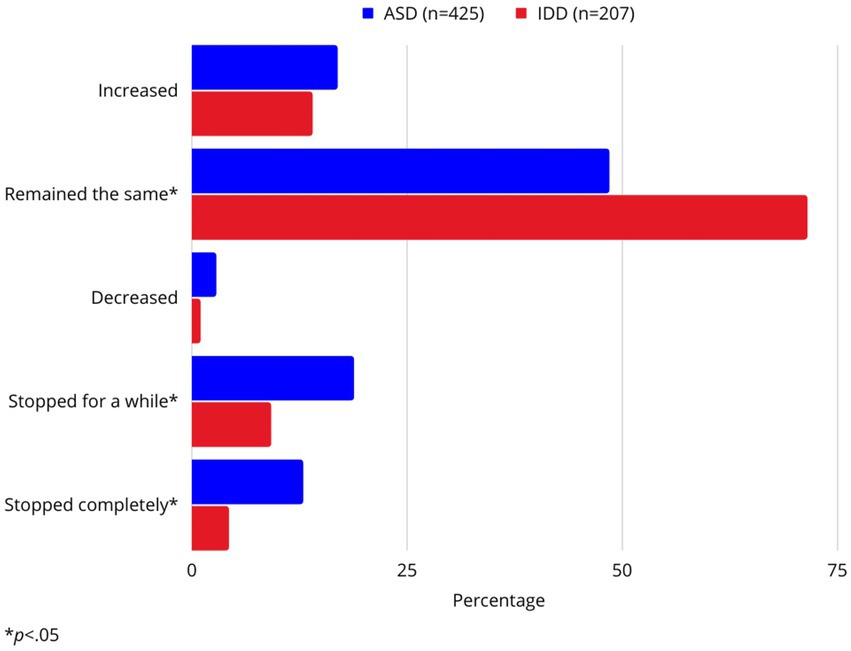
Figure 2. Percent of respondents by disability group reporting change in respite services since COVID-19.
3.1.3. Predictors of service access, receipt, and support from regional centers
Results from logistic regression models are shown in Table 4. All final models demonstrated acceptable fit based on the Hosmer-Lemeshow Test. First, a binary logistic regression indicated that disability significantly predicted the likelihood that respondents were regional center clients, X2(1) = 14.34, p < 0.001 and explained 2.2% (Nagelkerke R2) of the variance. Individuals with ASD had lower odds of having regional center status than those with IDD at the time of the survey (OR = 0.46). Race, age, and language were not significant predictors in the model (p > 0.10).
A binary logistic regression indicated that diagnosis and age significantly influenced whether respondents received respite services before the pandemic, X2(3) = 26.42, p < 0.001, explaining 4.4% (Nagelkerke R2) of the variance. Individuals were less likely to receive respite care if they were autistic (OR = 0.53) and fell in the 0–5 age bracket (OR = 0.57). Race and language were not significant predictors in the model (p > 0.10).
A binary logistic regression indicated that diagnosis, race, age, and pre-COVID receipt of respite services were significant predictors of contact with a regional center caseworker during the early pandemic period, X2(4) = 50.95, p < 0.001, explaining 9.0% (Nagelkerke R2) of the variance. Those who had contact with a caseworker were less likely to be autistic (OR = 0.32), more likely to identify as White (OR = 1.61), more likely to be in the 0–5 age bracket (OR = 1.94), and more likely to have received respite services before the pandemic (OR = 1.60). Language did not significantly contribute to the model.
Finally, a binary logistic regression indicated that race, age, and previous contact with a caseworker are significant predictors of support from the caseworker, X2(4) = 187.21, p < 0.001. Language approached significance at the p < 0.10 level and was retained in the model due to better model fit. All four predictors explained 28.9% (Nagelkerke R2) of the variance. Those who reported feeling supported by their caseworkers were more likely to identify as White (OR = 2.59), less likely to be 0–5 years of age (OR = 0.51), and more likely to have had previous contact with the caseworker (OR = 8.99). Disability, language, and pre-COVID receipt of respite were not significant predictors in the model at the p < 0.05 level.
4. Discussion
This survey study sheds light on the early impact of the COVID-19 crisis on service access and receipt for regional center clients with ASD and IDD in California. The first research question examined how respondents with ASD and IDD experienced changes in medical and therapy services resulting from COVID-19. Respondents were asked about medical services and therapies received before and after the COVID-19 stay-at-home orders. Approximately, 18–35% of individuals with IDD received services before COVID-19, which shifted to 14–35% after the outbreak. Telehealth service delivery was responsible for most services being received at the time of the survey.
Findings suggest that the medical and therapy services (i.e., OT, ABA, PT, not including respite) differed substantially across disability and racial groups. For instance, compared to the IDD group, the ASD group reported a higher mean number of services pre-COVID, and a lower mean number of services post-COVID. To our knowledge, this is the first study to compare services received in California by diagnostic groups (ASD vs. other IDD) during the pandemic. Children with ASD may require more services due to co-occurring diagnoses (Zablotsky et al., 2015), so it is concerning that the ASD group within our study experienced a decrease in services. One possible reason for these differences could be due to difficulties in implementing services through telehealth. For example, some families of children with ASD later discontinued telehealth due to difficulties (e.g., child did not benefit from telehealth, child could not sit still with camera). Also, professionals administering telehealth services reported that individuals with ASD sometimes refused to do telehealth and would remain out of vision from the camera (Spain et al., 2021), or simply lacked the social communication abilities to participate (White et al., 2021). Caregiver perspectives of telehealth with children with ASD suggest that they appreciate telehealth services but worry that this may not be as effective as in-person services (White et al., 2021). For caregivers of children with IDD, telehealth may require adaptations, such as caregivers being provided real-time coaching to provide the intervention or to facilitate participation in a diagnostic evaluation. On the other hand, studies indicate that some caregivers are comfortable with their participation in telehealth (Sutherland et al., 2019).
There are equity issues highlighted by imposing telehealth on families, such as digital literacy barriers and unfamiliarity with technology. Rodriguez et al. (2021) found that medical patients with limited English proficiency tended to have lower rates of telehealth use in California compared to proficient English speakers. Other factors such as living in rural communities and being of lower socioeconomic status are associated with lower utilization of telehealth (Reiners et al., 2019).
Service receipt also differed by racial/ethnic groups. Respondents who identified as POC reported receiving fewer services than their White counterparts during the earlier parts of the pandemic. This finding confirms a previously reported racial/ethnic disparity in service delivery for children with IDD, especially those who already experienced poor health care quality (Magaña et al., 2012). Using data from regional centers in California, Harrington and Kang (2016) study found disparities in service utilization across regional centers, indicating that POC had lower odds of receiving services when compared to White individuals with IDD.
We examined the extent to which regional center clients with ASD and IDD experienced changes in respite services resulting from COVID-19. Over 80% of the sample were regional center clients, and of those respondents, 70% reported receiving respite services before the pandemic. However, disruptions in respite access were experienced by some, with respite services stopped temporarily for some and fully for others. In a study by Linehan et al. (2022), a global survey was disseminated to caregivers of individuals with IDD (n = 1,912) and staff working with individuals with IDD (n = 1,329) a few months following the survey conducted in this study. In their study, over 60% of caregivers reported the canceling or reduction of respite services.
Respite services can provide caregivers of children with IDD occasional relief from caretaking responsibilities. Studies showed that respite care can reduce stress and fatigue and improve mental health and quality of life for caregivers of children with disabilities (Robertson et al., 2011; Remedios et al., 2015), including ASD (Harper et al., 2013; Dyches et al., 2016). Having professional respite staff work in the home during the pandemic crisis may not have been utilized by some families; it is unclear whether all clients of regional center knew that they were allowed to use family and friends in this role. Clearly, access to respite services may improve family well-being by alleviating burnout brought on by the pandemic for families of youth with IDD, particularly those with high support needs.
Indeed, in an online survey study conducted in Michigan, 31% of caregivers of individuals with ASD expressed interest in receiving respite services during COVID-19, and this interest was significantly higher among those whose children had greater symptom severity (Manning et al., 2021). In the current study, respite services differed between families of youth with ASD and IDD. For example, when compared to the ASD group, a larger proportion of respondents in the IDD group reported having no changes in respite care services during the COVID-19 crisis period.
The second research question focused on predictors of service access, receipt, and perceived support by regional center clients in California with ASD and IDD during the pandemic. Diagnostic group was a persistent predictor across outcomes of service access and support. Individuals with ASD had a lower likelihood of being regional center clients and receiving respite care before the pandemic. They were also less likely to be in contact with their caseworker during the COVID-19 crisis period. Some possible reasons for these differences could be due to the eligibility criteria of regional centers: children must have a substantial disability in three or more areas for example self-care, receptive and expressive language, learning, mobility, and capacity for independent living (Services for the Developmentally Disabled, Welfare and Institutions, 1977). This could lead to some eligibility exclusions for children with ASD due to the heterogeneity of ASD symptomology. For example, some children might display greater difficulties across several domains in adaptive functioning (e.g., self-care, independent living, and daily living skills) and language/communication. Those with less severe symptoms may struggle in fewer than three domains, leaving them ineligible to qualify for the regional center.
The severity of the diagnosis may have also impacted the eligibility of autistic children for respite services during COVID. It is unclear how regional centers were redistributing services during this time, and it could be possible that clients who needed more assistance were prioritized. Notably, those with ASD in this study were less likely to be contacted by their caseworker, which is consistent with prior research. Vohra et al. (2014) reported that caregivers of children with ASD raised more issues with service and quality of care when compared to caregivers of children with other IDDs. Previous findings suggested that caregivers of children with ASD report greater caregiver stress than children with IDD (without ASD) and neurotypical children (Estes et al., 2009; McStay et al., 2014). As the pandemic placed a pause and interruption of services for some of these families of children with ASD, it is important to understand the effects this service disruption had on caregiver stress and well-being.
Prior work investigating disparities in regional centers, specifically in California, indicated that POC had lower odds of receiving services when compared to their White counterparts (Harrington and Kang, 2016). In the current study, when asked if respondents had received adequate support from their caseworker since COVID-19, POC were less likely to be in contact with a caseworker or feel supported by a caseworker compared to White respondents. This finding is unfortunately similar to studies identifying barriers that POC face within medical systems, such as health care providers spending less time with them and difficulties accessing services (Magaña et al., 2012). Given that the state of California is heavily diverse, improvements must be made to reach all families and ensure that POC has access to quality care and support.
Age was a significant predictor of the receipt of respite services. Although caregivers of young children were more likely to be in contact with a caseworker, they were less likely to receive respite services and feel supported by a caseworker in the early pandemic period. This contradicts findings indicating that caregivers of younger children with ID and severe behavioral problems use respite services more than caregivers of older adults (Weiss and Lunsky, 2010). However, other factors have been identified as influences of respite care, including child-related disability severity, challenging behaviors, and communication difficulties, as well as family stress and size (Chan and Sigafoos, 2000). More attention is needed to identify service utilization patterns specific to respite services and how they might differ by child age and severity for this population. Notably, Burke and Hodapp (2016) pointed out that caregiver advocacy tends to change over time depending on the stage or age of their child’s life. For example, when children are around 3–5 years old, caregivers tend to advocate more strongly for their children particularly as they transition to school-based services (Individuals With Disabilities Education Improvement Act, 2004). School-age children may also require more assistance with services, since the school years are critical periods for accessing intervention and support. These could be possible reasons why caregivers of school-age children were reaching out to their caseworker more often.
4.1. Implications
Findings from this study reveal evident racial disparities in the receipt of developmental disabilities services between White and POC within California. This disparity should be recognized and further investigated since the IDD community continues to be impacted by the pandemic. Indeed, COVID-19 has continued to show surges since the early pandemic period and has forced new restrictions during these surges within the state of California (Ibarra, 2022). For example, in California, the state had to reinforce mask mandates and limits in household gatherings. During these phases of the pandemic, caseworkers and service providers should provide all families the option of virtual visits if families did not feel comfortable with others in the home, rather than canceling visits or sessions completely. These virtual visits can allow caregivers to disclose how they are dealing with the pandemic and what they might need during this time. Caseworkers can provide caregivers with options of virtual support groups, local organizations that meet in outdoor spaces or training for themselves to help their youth or child. It is also important to know how caregivers managed the disruptions to support services and navigated the transition to remote service delivery, especially for those who were regional center clients. Regional centers should ensure that the pandemic does not continue to widen these gaps among racial and ethnic groups (Harrington and Kang, 2016).
There are also silver linings that point to best practices for the future. For instance, telehealth services (e.g., online evaluations) can become a viable option for families who cannot drive to nearby facilities or risk exposure to COVID-19 by attending in-person appointments (Ameis et al., 2020). Moreover, students with high-functioning ASD reported feeling “liberated” from the social and academic demands in school (Reicher, 2020). Caregivers identified the benefit of having more time to spend with family when having to be at home with their children (Neece et al., 2020). Thus, the multi-faceted impact of COVID-19 on families and youth with IDD requires service providers to support families during the continued crisis and beyond. Although the COVID-19 pandemic is coming to an end, there will likely be lasting effects for decades to come, and much can be learned from investigations like this as we move forward.
4.2. Limitations
As in all studies, there are some limitations here. First, we recognize that this study includes only California respondents. There were likely different approaches to the pandemic around stay-at-home orders and developmental disability services in other parts of the country in the early stages of the pandemic. Second, since this was an online survey, there is a concern for self-selection bias. Those who volunteered to be part of the survey could have been respondents who had either been very affected by the pandemic or had experienced little to no impact. Third, the survey did not collect response rates, so it is unclear how many individuals had originally viewed the survey. Lastly, as in most surveys, respondents self-reported their diagnosis or their child’s diagnosis, which could not be confirmed with an independent evaluation or standardized measures.
4.3. Conclusion
The present study suggests differences in service use for diagnostic groups, taking into account some sociodemographic factors. The ASD group reported receiving fewer services than the IDD group after stay-at-home orders were in place. In addition, POC reported fewer services being delivered than their White counterparts. It is critical to continue to investigate factors related to the inequity in services being delivered across disability and racial groups.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: This study was a secondary analysis of the original data collected by the Autism Society of California. Raw data are not publicly available, though a report of preliminary findings (group-level information) and recommendations based on these findings have been released by the Autism Society of California. Requests to access these datasets should be directed to corresponding author.
Author contributions
BB and ME designed the survey and disseminated it across the state. JB and YB initiated research collaboration with BB and ME. GS and YB conceptualized the analysis proposal and performed the statistical analysis and interpretation. GS drafted the manuscript under the supervision of YB and JB. BB and ME confirmed descriptions of the methodology. JB, YB, and GS discussed the results and contributed to the final manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to thank the families and individuals with IDD that participated in the survey. We would also like to thank Autism Society of California for sharing the survey data and collaborating with the SEARCH Center at the University of California, Riverside.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ameis, S. H., Lai, M. C., Mulsant, B. H., and Szatmari, P. (2020). Coping, fostering resilience, and driving care innovation for autistic people and their families during the COVID-19 pandemic and beyond. Mol. Autism. 11, 61–69. doi: 10.1186/s13229-020-00365-y
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders. 5th ed. eds. F. B. Michael and W. N. Maria, (VA: Editorial and coding consultants).
Armitage, R., and Nellums, L. B. (2020). Considering inequalities in the school closure response to COVID-19. Lancet Glob. Health 8:e644. doi: 10.1016/S2214-109X(20)30116-9
Bhat, A. (2021). Analysis of the SPARK study COVID-19 parent survey: early impact of the pandemic on access to services, child/parent mental health, and benefits of online services. Autism Res. 14, 2454–2470. doi: 10.1002/aur.2618
Buchholz, K. (2022). Which states are contributing the most to United States. GDP? Available at: https://www.statista.com/chart/9358/us-gdp-by-state-and-region/
Burke, M. M., and Hodapp, R. M. (2016). The nature, correlates, and conditions of parental advocacy in special education. Exceptionality 24, 137–150. doi: 10.1080/09362835.2015.1064412
Centers for Disease Control and Prevention (2021) COVID-19 timeline. Available at: https://www.cdc.gov/museum/timeline/covid19.html#Early-2020
Chan, J. B., and Sigafoos, J. (2000). A review of child and family characteristics related to the use of respite care in developmental disability services. Child Youth Care Forum 29, 27–37. doi: 10.1023/A:1009420206722
Chiri, G., and Warfield, M. E. (2012). Unmet need and problems accessing core health care services for children with autism spectrum disorder. Matern. Child Health J. 16, 1081–1091. doi: 10.1007/s10995-011-0833-6
Colizzi, M., Sironi, E., Antonini, F., Ciceri, M. L., Bovo, C., and Zoccante, L. (2020). Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: an online parent survey. Brain Sci. 10:341. doi: 10.3390/brainsci10060341
Courtenay, K., and Perera, B. (2020). COVID-19 and people with intellectual disability: impacts of a pandemic. Ir. J. Psychol. Med. 37, 231–236. doi: 10.1017/ipm.2020.45
Dyches, T. T., Christensen, R., Harper, J. M., Mandleco, B., and Roper, S. O. (2016). Respite care for single mothers of children with autism spectrum disorders. J. Autism Dev. Disord. 46, 812–824. doi: 10.1007/s10803-015-2618-z
Ersoy, K., Altın, B., Sarıkaya, B., and Özkardaş, O. (2020). The comparison of impact of health anxiety on dispositional hope and psychological well-being of mothers who have children diagnosed with autism and mothers who have normal children, in COVID-19 pandemic. Sosyal Bilimler Araştırma Dergisi. 9, 117–126.
Estes, A., Munson, J., Dawson, G., Koehler, E., Zhou, X. H., and Abbott, R. (2009). Parenting stress and psychological functioning among mothers of preschool children with autism and developmental delay. Autism 13, 375–387. doi: 10.1177/13623613091056
Friesen, K. A., Weiss, J. A., Howe, S. J., Kerns, C. M., and McMorris, C. A. (2021). Mental health and resilient coping in caregivers of autistic individuals during the COVID-19 pandemic: findings from the families facing COVID study. J. Autism Dev. Disord. 52, 3027–3037. doi: 10.1007/s10803-021-05177-4
Genova, H. M., Arora, A., and Botticello, A. L. (2021). Effects of school closures resulting from COVID-19 in autistic and neurotypical children. Fronts. Educ. 6:761485. doi: 10.3389/feduc.2021.761485
Grenier-Martin, J., Rivard, M., Patel, S., Lanovaz, M. J., and Lefebvre, C. (2022). Randomized controlled trial on an online training to support caregivers of young children with intellectual and developmental disability managing problem behaviors at home. J. Child Fam. Stud. 31, 3485–3497. doi: 10.1007/s10826-022-02440-9
Guralnick, M. J. (2011). Why early intervention works: a systems perspective. Infants Young Child. 24, 6–28. doi: 10.1097/IYC.0b013e3182002cfe
Harper, D., Dyches, T. T., Harper, J., Roper, S. O., and South, M. (2013). Respite care, marital quality, and stress in parents of children with autism spectrum disorders. J. Autism Dev. Disord. 43, 2604–2616. doi: 10.1007/s10803-013-1812-0
Harrington, C., and Kang, T. (2016). Disparities in service use and expenditures for people with intellectual and developmental disabilities in California in 2005 and 2013. Intellect. Dev. Disabil. 54, 1–18. doi: 10.1352/1934-9556-54.1.1
Hayes, S. A., and Watson, S. L. (2013). The impact of parenting stress: a meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. J. Autism Dev. Disord. 43, 629–642. doi: 10.1007/s10803-012-1604-y
Ibarra, A. (2022). California mandates masks again. Cal Matters. Available at: https://calmatters.org/health/coronavirus/2021/12/california-mandates-masks-again/
Individuals With Disabilities Education Improvement Act. (2004) P. L.108–446, 20 U.S.C. § 1400 et seq.
Jeste, S., Hyde, C., Distefano, C., Halladay, A., Ray, S., Porath, M., et al. (2020). Changes in access to educational and healthcare services for individuals with intellectual and developmental disabilities during COVID-19 restrictions. J. Intellect. Disabil. Res. 64, 825–833. doi: 10.1111/jir.12776
Lee, V., Albaum, C., Tablon Modica, P., Ahmad, F., Gorter, J. W., Khanlou, N., et al. (2021). The impact of COVID-19 on the mental health and wellbeing of caregivers of autistic children and youth: a scoping review. Autism Res. 14, 2477–2494. doi: 10.1002/aur.2616
Li, Q., Guan, X., Wu, P., Wang, X., Zhou, L., Tong, Y., et al. (2020). Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 382, 1199–1207. doi: 10.1056/NEJMoa2001316
Linehan, C., Birkbeck, G., Araten-Bergman, T., Baumbusch, J., Beadle-Brown, J., Bigby, C., et al. (2022). COVID-19 IDD: findings from a global survey exploring family members' and paid staff's perceptions of the impact of COVID-19 on individuals with intellectual and developmental disabilities (IDD) and their caregivers. HRB Open Res. 5:27. doi: 10.12688/hrbopenres.13497.1
Maenner, M. J., Shaw, K. A., Bakian, A. V., Bilder, D. A., Durkin, M. S., Esler, A., et al. (2021). Prevalence and characteristics of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2018. MMWR Surveill. Summaries. 70, 1–16. doi: 10.15585/mmwr.ss7011a1
Magaña, S., Parish, S. L., Rose, R. A., Timberlake, M., and Swaine, J. G. (2012). Racial and ethnic disparities in quality of health care among children with autism and other developmental disparities. Intellect. Dev. Disabil. 50, 287–299. doi: 10.1352/1934-9556-50.4.287
Manning, J., Billian, J., Matson, J., Allen, C., and Soares, N. (2021). Perceptions of families of individuals with autism spectrum disorder during the COVID-19 crisis. J. Autism Dev. Disord. 51, 2920–2928. doi: 10.1007/s10803-020-04760-5
Mayer, M. L. (2006). Are we there yet? Distance to care and relative supply among pediatric medical subspecialties. Pediatrics 118, 2313–2321. doi: 10.1542/peds.2006-1570
Mayes, S. D., Calhoun, S. L., Aggarwal, R., Baker, C., Mathapati, S., Anderson, R., et al. (2012). Explosive, oppositional, and aggressive behavior in children with autism compared to other clinical disorders and typical children. Res. Autism Spectr. Disord. 6, 1–10. doi: 10.1016/j.rasd.2011.08.001
McStay, R. L., Dissanayake, C., Scheeren, A., Koot, H. M., and Begeer, S. (2014). Parenting stress and autism: the role of age, autism severity, quality of life and problem behavior of children and adolescents with autism. Autism 18, 502–510. doi: 10.1177/1362361313485
Neece, C., McIntyre, L. L., and Fenning, R. (2020). Examining the impact of COVID-19 in ethnically diverse families with young children with intellectual and developmental disabilities. J. Intellect. Disabil. Res. 64, 739–749. doi: 10.1111/jir.12769
Parenteau, C. I., Bent, S., Hossain, B., Chen, Y., Widjaja, F., Breard, M., et al. (2020). COVID-19 related challenges and advice from parents of children with autism spectrum disorder. SciMedicine J. 2, 73–82. doi: 10.28991/SciMedJ-2020-02-SI-6
Pletcher, B. A., Rimsza, M. E., Cull, W. L., Shipman, S. A., Shugerman, R. P., and O’Connor, K. G. (2010). Primary care pediatricians’ satisfaction with subspecialty care, perceived supply, and barriers to care. J. Pediatr. 156, 1011–1015.e1. doi: 10.1016/j.jpeds.2009.12.032
Reicher, D. (2020). Debate: remote learning during COVID-19 for children with high functioning autism spectrum disorder. Child Adolesc. Ment. Health. 25, 263–264. doi: 10.1111/camh.12425
Reiners, F., Sturm, J., Bouw, L. J., and Wouters, E. J. (2019). Sociodemographic factors influencing the use of eHealth in people with chronic diseases. Int. J. Environ. Res. Public Health 16:645. doi: 10.3390/ijerph16040645
Remedios, C., Willenberg, L., and Zordan, R. (2015). A pre-test and post-test study of the physical and psychological effects of out-of-home respite care on caregivers of children with life threatening conditions. Palliat. Med. 29, 223–230. doi: 10.1177/0269216314560008
Robertson, J., Hatton, C., Wells, E., Collins, M., Langer, S., Welch, V., et al. (2011). The impacts of short break provision on families with a disabled child: an international literature review. Health Soc. Care Community 19, 337–371. doi: 10.1111/j.1365-2524.2010.00977.x
Rodriguez, G., Hartley, S. L., and Bolt, D. M. (2019). Transactional relations between parenting stress and child autism symptoms and behavior problems. J. Autism Dev. Disord. 49, 1887–1898. doi: 10.1007/s10803-018-3845-x
Rodriguez, J. A., Saadi, A., Schwamm, L. H., Bates, D. W., and Samal, L. (2021). Disparities in telehealth use among California patients with limited English proficiency: study examines disparities in telehealth use among California patients with limited English proficiency. Health Aff. 40, 487–495. doi: 10.1377/hlthaff.2020.00823
Rosencrans, M., Arango, P., Sabat, C., Buck, A., Brown, C., Tenorio, M., et al. (2021). The impact of the COVID-19 pandemic on the health, wellbeing, and access to services of people with intellectual and developmental disabilities. Res. Dev. Disabil. 114:103985. doi: 10.1016/j.ridd.2021.103985
Scherer, N., Verhey, I., and Kuper, H. (2019). Depression and anxiety in parents of children with intellectual and developmental disabilities: a systematic review and meta-analysis. PLoS One 14:e0219888. doi: 10.1371/journal.pone.0219888
Services for the Developmentally Disabled, Welfare and Institutions. (1977). Code § 4500 et seq. Available at: https://leginfo.legislature.ca.gov/faces/codes_displaySection.xhtml?lawCode=WIC§ionNum=4512 [].
Singer, G. H. (2006). Meta-analysis of comparative studies of depression in mothers of children with and without developmental disabilities. Am. J. Ment. Retard. 111, 155–169. doi: 10.1352/0895-8017(2006)111[155:MOCSOD]2.0.CO;2
Spain, D., Mason, D., Capp, S. J., Stoppelbein, L., White, S. W., and Happe, F. (2021). “This may be a really good opportunity to make the world a more autism friendly place”: professionals’ perspectives on the effects of COVID-19 on autistic individuals. Res. Autism Spectr. Disord. 83:101747. doi: 10.1016/j.rasd.2021.101747
Stavropoulos, K. K.-M., Bolourian, Y., and Blacher, J. (2022). A scoping review of telehealth diagnosis of autism spectrum disorder. PLoS One 17:e0263062. doi: 10.1371/journal.pone.0263062
Sutherland, R., Trembath, D., Hodge, M. A., Rose, V., and Roberts, J. (2019). Telehealth and autism: are telehealth language assessments reliable and feasible for children with autism? Int. J. Lang. Commun. Disord. 54, 281–291. doi: 10.1111/1460-6984.12440
Termine, C., Dui, L. G., Borzaga, L., Galli, V., Lipari, R., Vergani, M., et al. (2021). Investigating the effects of COVID-19 lockdown on Italian children and adolescents with and without neurodevelopmental disorders: a cross-sectional study. Curr. Psychol. 1, 1–17. doi: 10.1007/s12144-021-02321-2
United States Census Bureau. (2022). California; United States. QuickFacts. Available at: https://www.census.gov/quickfacts/fact/table/CAUS#
Vasa, R. A., Singh, V., Holingue, C., Kalb, L. G., Jang, Y., and Keefer, A. (2021). Psychiatric problems during the COVID-19 pandemic in children with autism spectrum disorder. Autism Res. 14, 2113–2119. doi: 10.1002/aur.2574
Vohra, R., Madhavan, S., Sambamoorthi, U., and St Peter, C. (2014). Access to services, quality of care, and family impact for children with autism, other developmental disabilities, and other mental health conditions. Autism 18, 815–826. doi: 10.1177/1362361313512902
Weiss, J., and Lunsky, Y. (2010). Service utilization patterns in parents of youth and adults with intellectual disability who experienced behavioral crisis. J. Ment. Health Res. Intellect. Disabil. 3, 145–163. doi: 10.1080/19315864.2010.490617
White, S. W., Stoppelbein, L., Scott, H., and Spain, D. (2021). It took a pandemic: perspectives on impact, stress, and telehealth from caregivers of people with autism. Res. Dev. Disabil. 113:103938. doi: 10.1016/j.ridd.2021.103938
Young, E., Milligan, K., Henze, M., Johnson, S., and Weyman, K. (2021). Caregiver burnout, gaps in care, and COVID-19: effects on families of youth with autism and intellectual disability. Can. Fam. Physician 67, 506–508. doi: 10.46747/cfp.6707506
Zablotsky, B., Black, L. I., Maenner, M. J., Schieve, L. A., Danielson, M. L., Bitsko, R. H., et al. (2019). Prevalence and trends of developmental disabilities among children in the United States: 2009–2017. Pediatrics 144:e20190811. doi: 10.1542/peds.2019-0811
Zablotsky, B., Pringle, B. A., Colpe, L. J., Kogan, M. D., Rice, C., and Blumberg, S. J. (2015). Service and treatment use among children diagnosed with autism spectrum disorders. J. Dev. Behav. Pediatr. 36, 98–105. doi: 10.1097/DBP.0000000000000127
Keywords: intellectual disability, developmental disability, autism spectrum disorder, COVID-19, IDD community, California
Citation: Salinas G, Bolourian Y, Burt B, Eichelberger M and Blacher J (2023) The early impact of COVID-19 on the intellectual and developmental disabilities community in California. Front. Educ. 8:1079086. doi: 10.3389/feduc.2023.1079086
Edited by:
Kristina Rios, California State University, Fresno, United StatesReviewed by:
Nikki Adams, University of Louisville, United StatesMeghan Cosier, Chapman University, United States
Mohd Hanafi Mohd Yasin, National University of Malaysia, Malaysia
Alfred Sankoh, William Howard Taft University, United States
Copyright © 2023 Salinas, Bolourian, Burt, Eichelberger and Blacher. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jan Blacher, ✉ amFuLmJsYWNoZXJAdWNyLmVkdQ==
 Giselle Salinas
Giselle Salinas Yasamin Bolourian2
Yasamin Bolourian2