- 1Institute of Neurology of Senses and Language, Hospital of St. John of God, Linz, Austria
- 2Research Institute for Developmental Medicine, Johannes Kepler University Linz, Linz, Austria
- 3Institute of Linguistics, University of Graz, Graz, Austria
- 4Division of Social Psychiatry, Medical University of Vienna, Vienna, Austria
Background: Social communication difficulties are often associated with neurodevelopmental disorders such as language disorder, intellectual development disorder, attention deficit hyperactivity disorder and autism spectrum disorder, which impedes the investigation of the specific role of social communication problems in mental health outcomes.
Aims: We investigated the association between conversation difficulties and increased risk of mental health problems in schoolchildren with hearing loss. It can be assumed of this sample that conversation difficulties are primarily due to limited auditory access to language rather than neurobiological deficits.
Methods: Five complete birth cohorts of Carinthian children (n = 53) with significant hearing loss and an intelligence quotient over 70 were assessed in terms of language abilities in standardized tests and in terms of their conversation skills by use of a short teacher checklist developed by the authors. Mental health problems were assessed by means of the Strengths and Difficulties Questionnaire by parents and teachers.
Results: Conversation deficits were significantly correlated with lower SDQ emotional problems and total problem scores as rated by parents and lower peer problems scores as rated by teachers. Controlling for degree of hearing loss, maternal education and language skills, confirmed the specific value of conversation skills as a predictor of emotional problems (p = 0.010).
Conclusion: With regard to mental health, our results suggest a focus on the assessment of conversation skills in addition to language abilities.
Introduction
Effective communication requires more than knowledge of vocabulary and grammatical rules. It includes conversation skills, such as initiating conversations, maintaining a topic or shifting topics, taking turns and keeping a conversation balanced and requesting or responding to conversational repair (Norbury et al., 2013). Conversation skills are a domain of social communication. The concept of social communication additionally includes the use of language for a variety of purposes in social situations (e.g., greeting, sharing or requesting information, asking for help or arguing) and the adaptation of verbal and non-verbal communication to the interlocutor and situation [e.g., adapting communication to the anticipated interests or pre-knowledge of the interlocutor (American Speech-Language-Hearing Association (ASHA), 2021)]. Although the term “social communication” is often used interchangeably with “pragmatic language,” social communication must be considered a broader and more functional concept including non-verbal communication (Adams and Gaile, 2015).
In the field of developmental disorders, difficulties using language in social situations are gaining increasing attention, since they are often associated with language disorders and with other neurodevelopmental disorders, such as attention deficit hyperactivity disorder (ADHD), intellectual disability (ID) and autism spectrum disorders (ASD). In children with language impairment, disproportionate problems in the social use of language rather than in structural language skills (e.g., knowledge of vocabulary or grammar) have been found to be associated with mental health problems, such as conduct and hyperactive symptoms, and with problems with peers (Mok et al., 2014; Sarimski et al., 2015). Furthermore, adverse outcomes in adult life, particularly problems in establishing friendships, have been described (Whitehouse et al., 2009). These findings for individuals with language impairment support the assumption that social communication deficits might be a risk factor for the emergence of mental health problems in any population. In the population based Avon longitudinal study (Law et al., 2015) pragmatic language difficulties at the age of nine were found to partially mediate the relation between social risk factors and emotional and behavioral problems in adolescence even after controlling for intelligence. The influence of other neurodevelopmental confounders was not taken into account. For the same representative birth cohort, social communication difficulties (in addition to other key factors) were found to predict exclusion from school (Paget et al., 2015). In a Dutch community sample of 1,364 children aged 4 years, Ketelaars et al. (2010) found that communicative competence (pragmatic language)—rather than structural language problems—correlated highly with behavioral problems mainly of an externalizing nature (specifically hyperactivity). Again, the influence of neurobiological variables was not considered (Ketelaars et al., 2010). In summary, there are indications from epidemiological studies that social communication difficulties contribute to mental health problems. Nevertheless, due to a large overlap with neurodevelopmental difficulties (seen also in community samples) the specific role of conversation skills in the prediction of increased rates of mental health problems remains unclear. Deaf and hard-of-hearing children grow up with limited access to spoken language, which very often causes limited mastery of spoken language. As a consequence of delayed language development and limited participation in a range of natural social communication situations, higher rates of problems, particularly in the use of language in personal interactions, have been identified than for typically hearing peers (Most et al., 2010; Goberis et al., 2012; Tobey, et al., 2013). Paatsch and Toe (2013) investigated free conversations of 20 school-age children with cochlea implants with their hearing peers and found that they tended to dominate conversations (unbalanced conversations) and to initiate more topics (problems in topic maintenance; Paatsch and Toe, 2013). Similarly, Most et al. (2010) compared linguistic interactions between either children with hearing loss or children with normal hearing and familiar adults by means of direct observation. Significantly more often, the hearing-impaired sample demonstrated inappropriate social use of language, for instance, problems with maintaining the topic of the adults’ preceding utterance and adding information to it (Most et al., 2010). Hearing loss can be regarded as a unique natural experiment that provides the opportunity to observe an increased rate of conversation difficulties which are a consequence of limited access to conversational exchanges with the environment due to restricted audibility rather than an expression of neurodevelopmental deficits observed in children with developmental language disorder, ADHD or ASD. In a German study of 66 children attending special schools for the deaf, Hintermair et al. (2015) found significant correlations between communication skills measured by the Children’s Communication Checklist (Bishop, 1998) and behavioral problems rated by teachers using the Strengths and Difficulties Questionnaire (Goodman, 1997). However, the sample was not representative, and no clinical assessment of language, hearing or nonverbal intelligence was performed (Hintermair et al., 2015).
Aims of the study
To investigate the specific value of conversation difficulties assessed by a brief symptom checklist by teachers in predicting mental health difficulties in a representative sample of schoolchildren with hearing loss, taking into account possible confounders such as degree of hearing loss, language skills and parental educational level.
Materials and methods
Measurements
Performance IQ was measured by means of the nonverbal subtests of the Kaufmann Assessment Battery for children (Melchers and Preuß, 2009). Expressive vocabulary was assessed with the WWT (Wortschatz-und Wortfindungstest; Test of vocabulary and word finding) 6–10, a picture-naming test for children aged 6 to 10 years (Glück, 2007). The German version of the TROG (Test of Reception of Grammar; Fox, 2006) was used to assess comprehension of spoken language grammar in a face-to-face situation. A standardized test of sentence repetition was selected as an economical procedure for measuring expressive grammatical skills (Heidelberger Sprachentwicklungstest: Imitation von Satzstrukturen; Imitation of sentences; Grimm and Schöler, 1998). Audiological records made within a maximum of 1 year before assessment were used to calculate the degree of hearing loss based on the average hearing threshold in the frequencies 0.5, 1, 2, and 4 kHz. Behavioral, emotional and social problems were rated by parents and teachers using the corresponding versions of the Strengths and Difficulties Questionnaire, which has been used extensively in the investigation of mental health in children with hearing loss (for a meta-analysis see Stevenson et al., 2015). Sociodemographic data on child and family were obtained from structured parent interviews.
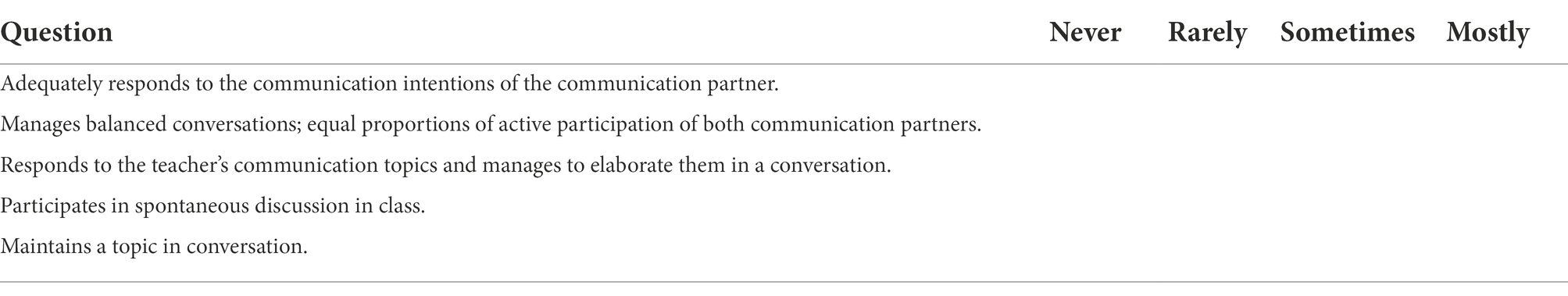
For the assessment of conversation skills, we developed a brief teacher checklist of five questions based on the current theoretical underpinnings of conversational aspects of pragmatics (Bishop, 1998; Ketelaars et al., 2010) and combined them with a more comprehensive teacher questionnaire. Teachers were required to answer the questions using a four-point Likert scale. The five questions pertain to conversation skills, such as responsiveness to speaker’s intentions and communication topics, balance of expressive and receptive communication, topic maintenance and participation in group communication (Table 1).
For our sample of children with significant bilateral hearing loss reliability of the set of five questions was good (Cronbach’s alpha = 0.86), demonstrating internal consistency of the items.
Sample
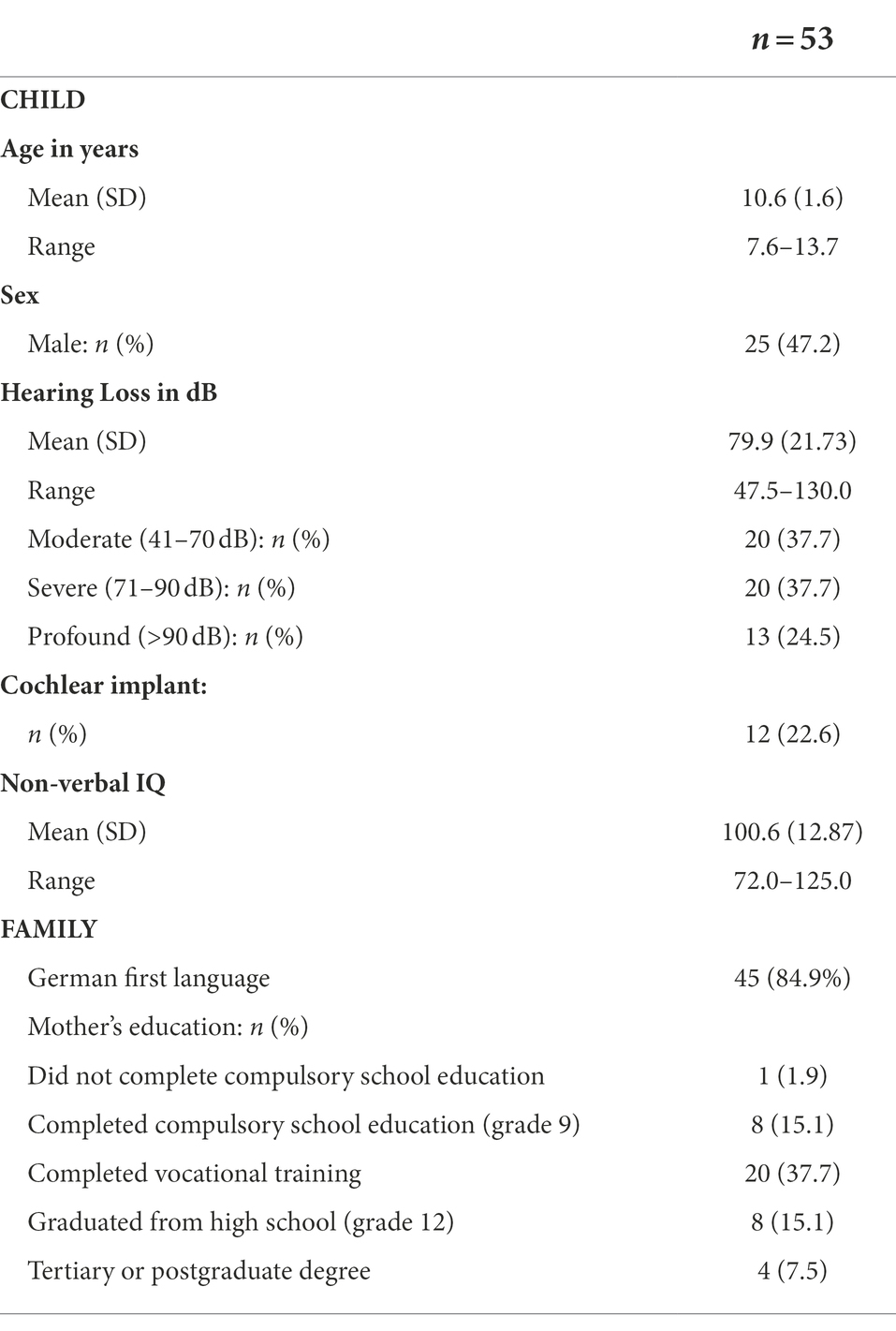
This cross-sectional cohort study targeted all children with significant hearing loss born between January 1997 and December 2001 in the Austrian federal state of Carinthia with a total population of about 560.000 (Holzinger et al., 2016). Since all school-age children with hearing loss are registered with the Centre for Special Education for Children with Hearing Impairments, an epidemiologically complete sample was available. Teachers of the Centre for Special Education invited all parents of children from grades one to seven to participate in this study. All parents of the five birth cohorts from 1997 to 2001 (n = 68) followed this invitation and gave written permission for study participation of their children. After exclusion of 15 children with either permanent conductive hearing loss (seven children) or intellectual disability (eight children with performance IQ below 70) or both (one child), the final sample consisted of 53 children with significant sensorineural hearing loss (hearing threshold above 40 db in the better ear). There was no child with a known diagnosis of an autism spectrum disorder in the sample. All interviews and assessments except audiometry were performed in the child’s local school by four teachers of the Deaf and two qualified psychologists. Table 2 summarizes demographic and audiological characteristics of the study sample.
About a quarter of the sample had a profound hearing loss, most of whom used a cochlear implant (72.2%). Sexes were equally distributed. About 15% of the children grew up with German as their second language. After exclusion of children with intellectual disabilities, the average performance IQ of the sample was 100.6, with a standard deviation of 12.9. Eight children (13.1%) had at least one parent with hearing loss, five of whom (8.2% of the total sample) were from families in which both parents had a hearing loss. The percentage of mothers who had at least completed high school (22.6%) was similar to that in the general Carinthian population (27.9%, p = 0.282). Preferred mode of communication was sign language or simultaneous communication (speaking and signing) for four children.
Statistical analysis
All data analyses were conducted using SPSS 15. Hypotheses of association were tested using Pearson’s correlation coefficient r. Following Cohen (1992), r-values between 0.1 and 0.3 correspond to small effects, values between.3 and.5 to medium effects and values >0.5 to large effects. We used a stepwise linear regression model to control for confounders when describing the association between conversation skills and mental health symptoms as measured by the SDQ parental rating.
Ethical standards
All parents of the five birth cohorts from 1997 to 2001 (n = 68) gave written informed consent for participation. This study was part of a more comprehensive evaluation of outcomes of deaf education and was approved by the educational authorities of Carinthia.
Results
Language results were below average and strongly negatively correlated with the degree of hearing loss for all the linguistic dimensions measured, as shown in Table 2. The severity of language delay is evidenced by the high percentage of those with language scores corresponding to at least one standard deviation below the norm (Table 3).
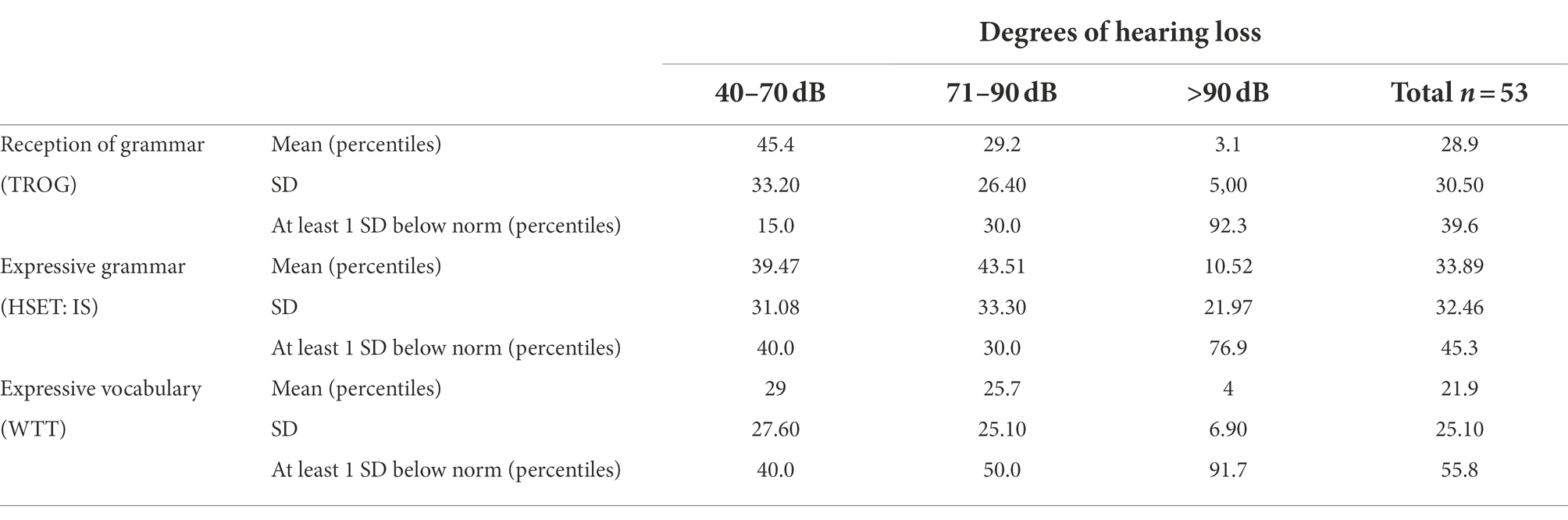
Table 3. Language results by degree of hearing loss (means and standard deviations in percentiles and percentage below 1 SD).
The mean score for Conversation Skills rated by teachers using 4-point Likert scales was found to be high (3.49, SD 0.67, min 1.0; max 4.0), with 18 children (34%) attaining the maximum score. Since the ratings were intended to be used to identify conversation problems (as a screening instrument), the uneven distribution was deliberate. Results of the SDQ parent and teacher reports and data of the corresponding norm groups are shown in Table 4. German norms were used for the parent version. Since there are no German norms available for the teacher version, English norm group data are presented.
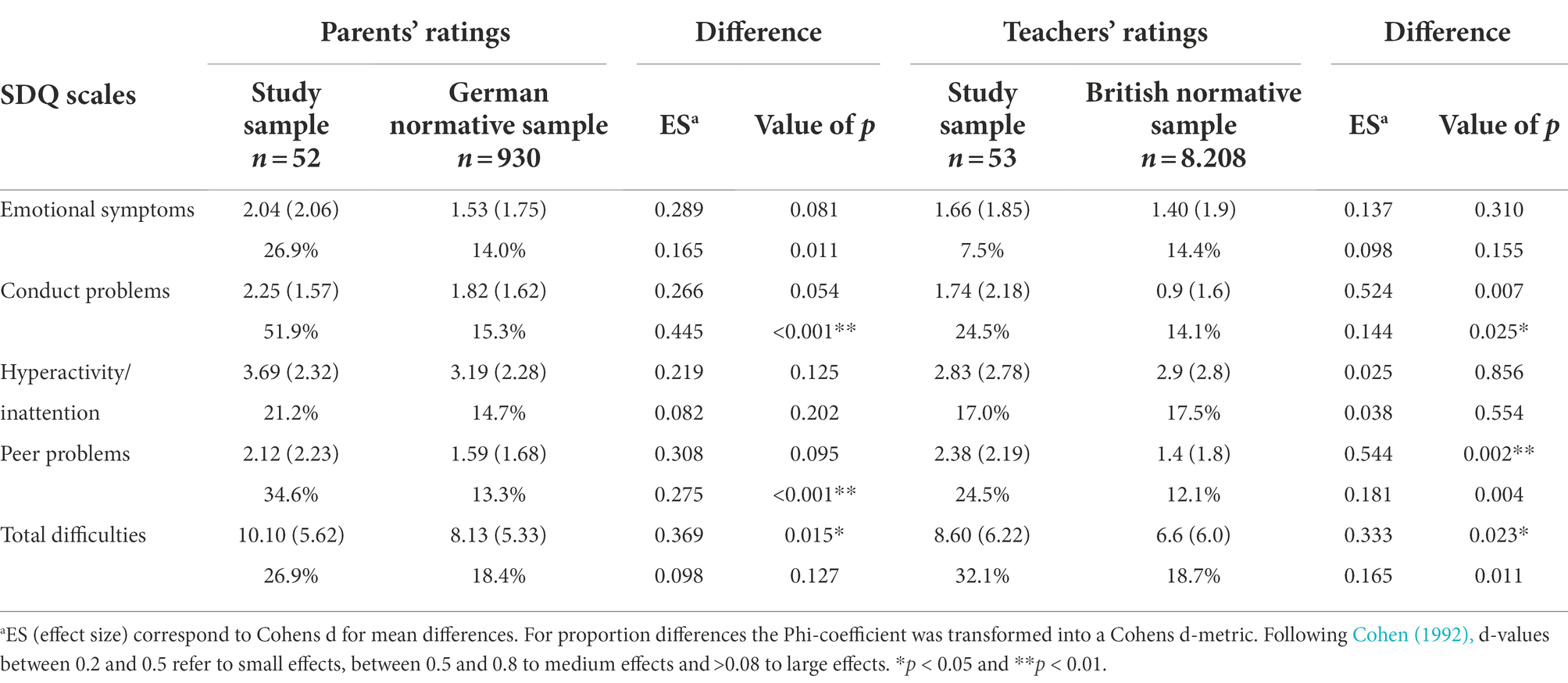
Table 4. SDQ results from parent and teacher reports compared with normative samples (means and SD and percentage in borderline and abnormal range).
As expected, total difficulties mean scores were found to be significantly higher in the parent and teacher ratings for children with hearing loss. Parents reported significantly higher rates of children with abnormal or borderline scores in the subdomain of emotional symptoms. Both teacher and parent ratings showed higher rates of conduct and peer relationship problems. In the domain of hyperactivity, no significant difference from the norm groups with normal hearing was found.
We then investigated correlations between conversation skills and child and family characteristics on the one hand and mental health problems on the other (Table 5).
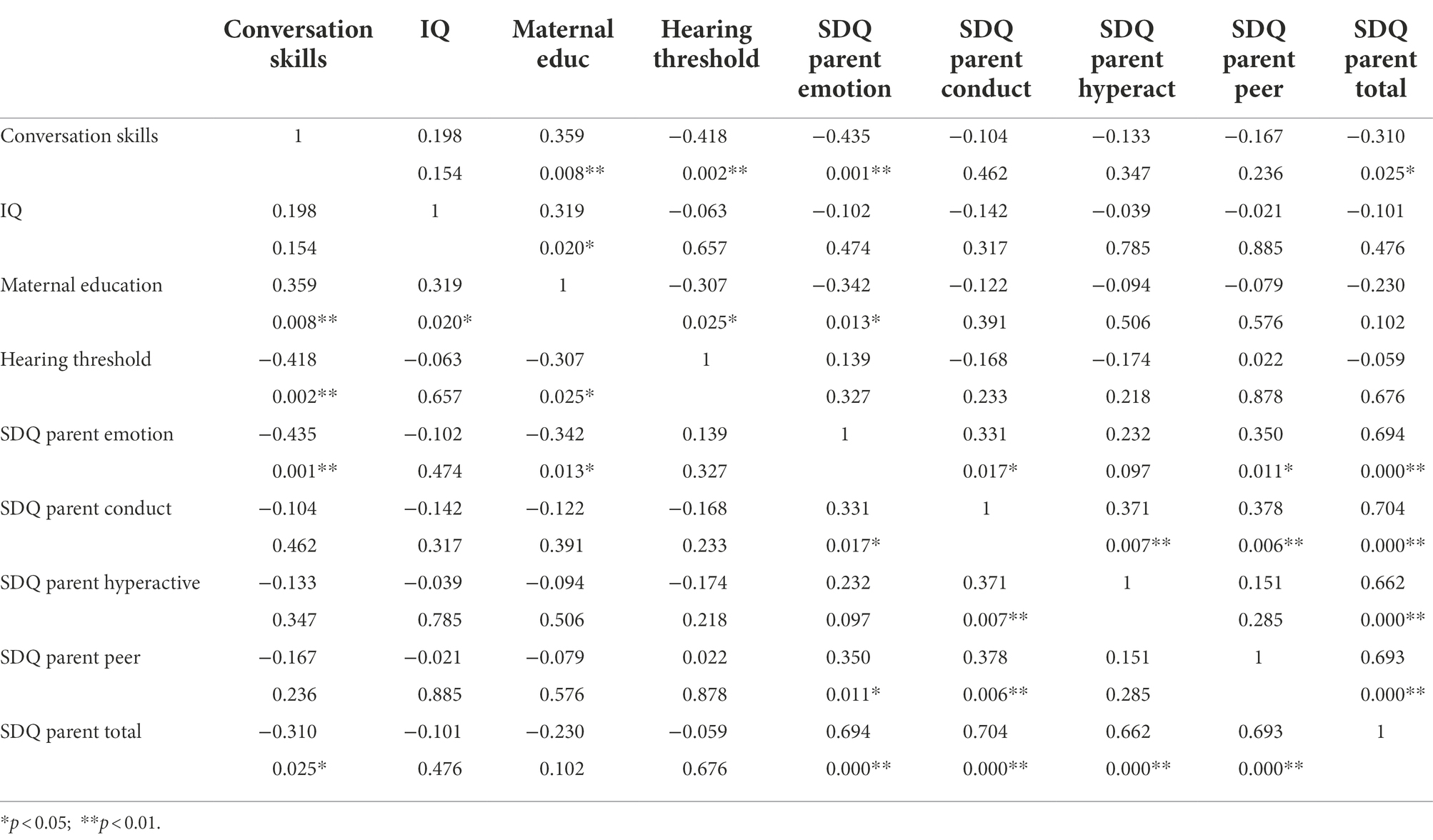
Table 5. Pearson correlations and value of p between conversation skills, child and family characteristics and mental health problems reported by parents (n = 53).
Conversation skills were significantly correlated with lower SDQ emotional problem and total problem scores as rated by parents and lower rates of peer relationship problem scores as reported by teachers (r = −0.409, p = 0.002). Notably, none of the SDQ domains of mental health problems relating to externalizing behavioral problems (conduct problems, hyperactivity/inattention) were found to be significantly related with conversation competence.
Interestingly, language measures (vocabulary, expressive and receptive grammar), IQ and degree of hearing loss were not directly associated with SDQ problem scores. Receptive language and severity of hearing loss, however, were significantly correlated with conversation skills. As far as child and family influences on mental health are concerned, only higher maternal education correlated significantly with lower parent-reported emotional problem scores, and nonverbal intelligence showed significant negative correlation with problems with peers as reported by teachers (r = −0.324, p = 0.018).
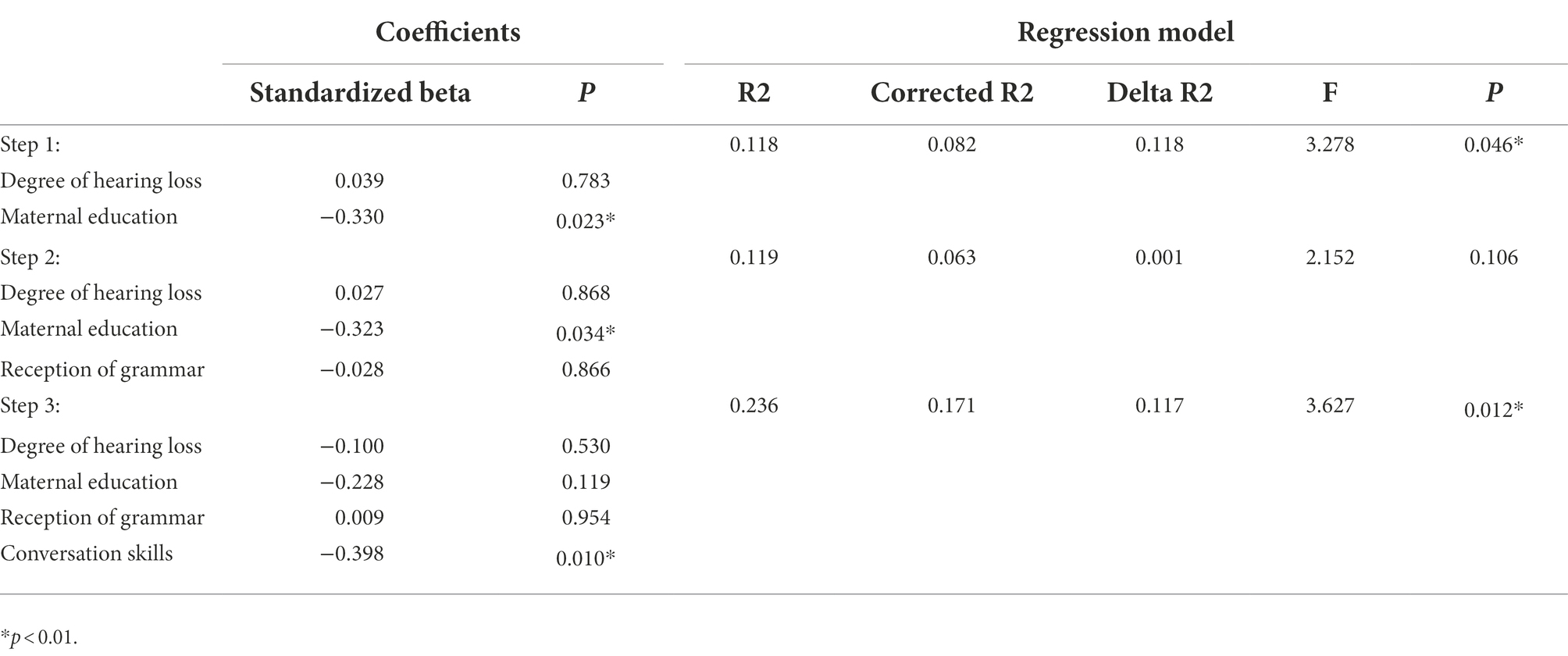
Finally, the specific role of conversation skills in the prediction of mental health problems was explored by means of regression analysis. In order to use independent information sources in rating conversation skills (evaluated by teachers) on the one hand and mental health on the other, only parental SDQ data on emotional problems were selected as an independent variable. In a linear regression analysis to predict SDQ emotional problem scores (Table 5), influences of degree of hearing loss and of maternal education were controlled for in the first step. In the second step, language comprehension results (TROG-D) were introduced to determine the role of language skills in the prediction of mental health problems. Conversation abilities were then introduced in Step 3.
As shown by Table 6, deficits in conversation skills specifically predicted emotional problems, whereas language skills per se did not contribute to the explanation of variance. After introducing conversation skills, maternal education was no longer significant. The overall explanation of variance by the model was 23.6% (corrected R2 = 0.171).
Discussion
This study investigated the role of conversation skills in the prediction of mental health outcomes in five complete birth cohorts of children with hearing loss. In the specific study sample at hand, conversation skills were related to the children’s delayed language acquisition due to limited access to spoken languages rather than to neurobiological confounders.
Conversation difficulties rated by teachers were found to be significantly correlated with emotional problems (r = −0.435) and total SDQ problem scores (r = −0.310) as rated by parents and with peer problem scores (r = −0.409) according to teacher reports. Interestingly, language development was associated with conversation skills, but did not show any direct significant influence on mental health. The specific role of conversation difficulties was confirmed by a linear regression analysis to predict emotional problems while controlling for influences of the degree of hearing loss, IQ, maternal education level and language skills. Our findings add to previous studies that highlighted associations between pragmatic language difficulties and externalizing behavioral problems. Ketelaars et al. (2010) reported moderate to high correlations between pragmatic deficits and externalizing behavioral problems (hyperactivity), and low correlations with emotional and conduct problems in a general-population sample of four-year-old children (Ketelaars et al., 2010). Hintermair et al. (2015) found significant correlations between pragmatic skills and all SDQ subdimensions, with the exception of emotional problems, in a sample of deaf/hard-of-hearing schoolchildren (Hintermair et al., 2015). The differences from our findings may be explained by the different age groups (Ketelaars et al., 2010) and use of different informants. Pragmatic problems are not fully developed at pre-school age and might be difficult to detect. In addition, teachers tend to observe lower rates of emotional problems than parents (Fellinger et al., 2008). Furthermore, in both studies the use of teacher questionnaires to evaluate both pragmatic skills and mental behavior may have led to a bias. Finally, Hintermair’s sample consisted of a non-representative group of children with hearing loss, most of whom attended special schools for the deaf (more than 90% of the sample), where a higher rates of neurobiological confounders are most likely, that were not taken into account (Hintermair et al., 2015).
Children with conversation difficulties have problems with everyday communication tasks within their environment of peers and caregivers; they tend to dominate in conversations (take too much control), not to respond to an interlocutor’s intention and topic, and experience problems with maintaining conversations or participating in group conversations. Considering these difficulties, restricted social participation and associations with emotional and peer problems are not unexpected as a consequence of social communication deficits. Our results are in line with Rißling et al.’s (2015) findings of stronger correlations between pragmatic problems and emotional and behavioral difficulties in children with language difficulties than with structural language (vocabulary, grammar) and speech production. Our results also accord with Mok et al.’s (2014) study, which reported the specific role of pragmatics in predicting peer problems in adolescence in individuals with a history of specific language impairment (Mok et al., 2014; Rißling et al., 2015). A recent study on 144 9-year-old children with hearing loss similarly found significant correlations between pragmatic rather than structural language skills and psycho-social abilities and quality of life (Ching et al., 2021).
Limitations
As a consequence of the cross-sectional design of this study, no claims can be made regarding the causal relations between conversation skills and mental health problems. Furthermore, the short questionnaire on conversation skills provides only an indirect measure of pragmatic competence. The use of teacher questionnaires to evaluate conversation skills and mental health (associations with peer problems) may have led to a bias. However, the main outcome of significant correlations between conversation deficits and emotional problems is based on results from multiple informants. While children with intellectual disability were excluded from the study sample and there were no comorbid autistic disorders, other possible neurobiological confounders (such as motor disorders) were not considered or excluded.
Conclusions and clinical implications
Our findings emphasize the particular and specific role conversation skills rather than language knowledge (vocabulary or grammar) may play in social and emotional functioning. Furthermore, the results for the sample of children with hearing loss indicate that conversation difficulties not (primarily) intertwined with neurodevelopmental pathology could specifically contribute to mental health problems. Screening for conversation skills – even by using a brief checklist of child communicative behaviors (Table 1)—may help to facilitate the early identification of children at risk for mental health problems. On the other hand, in children with emotional and peer problems, screening for conversation difficulties may indicate the need for treatment procedures that specifically address social communication behaviors (Adams et al., 2012). Since problems in language knowledge may contribute to problems in language use that are associated with mental health problems, assessment of conversation in addition to language should be considered an essential component in the diagnosis of any child with speech-language difficulties. This study needs to be replicated with a longitudinal design in a comparable population that takes thorough account of neurobiological confounders and uses both observational and proxy measures of conversation skills.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
DH and JF: study design and methodology, writing first draft, and review and editing. DH: methodology and formal analysis, data curation, and project administration. All authors contributed to the article and approved the submitted version.
Acknowledgments
We express our gratitude to the Centre for Special Education for Children with Hearing Impairments in Klagenfurt (Johann and Annette Weishaupt) for the data collection and to Christoph Weber (University of Education, Upper Austria) who checked the statistical analyses.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Adams, C., and Gaile, J. (2015). The SCIP manual: Social communication intervention Programme: Managing Children’s pragmatic and social communication needs in the early school years. Macclesfield: Napier Hill Press.
Adams, C., Lockton, E., Freed, J., Gaile, J., Earl, G., McBean, K., et al. (2012). The social communication intervention project: a randomized controlled trial of the effectiveness of speech and language therapy for school-age children who have pragmatic and social communication problems with or without autism spectrum disorder. Int. J. Lang. Commun. Disord. 47, 233–244. doi: 10.1111/j.1460-6984.2011.00146.x
American Speech-Language-Hearing Association (ASHA). (2021). Social Communication. Available at: https://www.asha.org/public/speech/development/social-communication (Accessed 10 January 2022).
Bishop, D. (1998). Development of the Children's communication checklist (CCC): a method for assessing qualitative aspects of communicative impairment in children. J. Child Psychol. Psychiatry Allied Discip. 39, 879–891. doi: 10.1017/S0021963098002832
Ching, T. Y., Cupples, L., Leigh, G., Hou, S., and Wong, A. (2021). Predicting quality of life and behavior and emotion from functional auditory and pragmatic language abilities in 9-year-old deaf and hard-of-hearing children. J. Clin. Med. 10:5357. doi: 10.3390/jcm10225357
Fellinger, J., Holzinger, D., Sattel, H., and Laucht, M. (2008). Mental health and quality of life in deaf pupils. Eur. Child Adolesc. Psychiatry 17, 414–423. doi: 10.1007/s00787-008-0683-y
Fox, A. (2006). Test zur Überprüfung des Grammatikverständnisses (TROG-D). Idstein: Schulz-Kirchner.
Glück, C. (2007). Wortschatz-und Wortfindungstestfür 6-bis 10-jährige kinder WWT 6–10 [vocabulary and wort finding test for 6-to 10-years-old children]. München: Elsevier.
Goberis, D., Beams, D., Dalpes, M., Abrisch, A., Baca, R., and Yoshinaga-Itano, C. (2012). The missing link in language development of deaf and hard of hearing children: pragmatic language development. Semin. Speech Lang. 33, 297–309. doi: 10.1055/s-0032-1326916
Goodman, R. (1997). The strengths and difficulties questionnaire: a research note. J. Child Psychol. Psychiatry 38, 581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x
Hintermair, M., Pilz, S., and Sarimski, K. (2015). Pragmatische Sprachkompetenzen und Verhaltensauffälligkeiten bei hörgeschädigten Kindern im Grundschulalter - eine Studie mit der "Children's Communication Checklist". Zeitschrift für Audiologie 54, 58–65.
Holzinger, D., Weishaupt, A., Fellinger, P., Beitel, C., and Fellinger, J. (2016). Prevalence of 2.2 per mille of significant hearing loss at school age suggests rescreening after NHS. Int. J. Pediatr. Otorhinolaryngol. 87, 121–125. doi: 10.1016/j.ijporl.2016.06.006
Ketelaars, M., Cuperus, J., Jansonius, K., and Verhoeven, L. (2010). Pragmatic language impairment and associated Behavioural problems. Int. J. Lang. Commun. Disord. 45, 204–214. doi: 10.3109/13682820902863090
Law, J., Rush, R., Clegg, J., Peters, T., and Roulstone, S. (2015). The role of pragmatics in mediating the relationship between social disadvantage and adolescent behaviour. J. Dev. Behav. Pediatr. 36, 389–398. doi: 10.1097/DBP.0000000000000180
Melchers, P., and Preuß, U. (2009). Kaufman assessment battery for children. Individualtest zur Messung von Intelligenz und Fertigkeiten bei Kindern. Deutschsprachige Fassung des Tests von AS Kaufman & NL Kaufman. Göttingen: Hogrefe.
Mok, P. L., Pickles, A., Durkin, K., and Conti-Ramsden, G. (2014). Longitudinal trajectories of peer relations in children with specific language impairment. J. Child Psychol. Psychiatry 55, 516–527. doi: 10.1111/jcpp.12190
Most, T., Shina-August, E., and Meilijson, S. (2010). Pragmatic abilities of children with hearing loss using Cochlear implants or hearing aids compared to hearing children. J. Deaf Stud. Deaf Educ. 15, 422–437. doi: 10.1093/deafed/enq032
Norbury, C., Gemmell, T., and Paul, R. (2013). Pragmatics abilities in narrative production: a cross-disorder comparison. J. Child Lang. 41, 485–510. doi: 10.1017/S030500091300007X
Paatsch, L. E., and Toe, D. M. (2013). A comparison of pragmatic abilities of children who are deaf or hard of hearing and their hearing peers. J. Deaf Stud. Deaf Educ. 19, 1–19. doi: 10.1093/deafed/ent030
Paget, A., Parker, C., Henley, W., Heron, J., Ford, T., and Emond, A. (2015). Which children and young people are excluded from school? Findings from the Avon longitudinal study of parents and children (ALSPAC). Lancet 44, 285–296. doi: 10.1111/cch.12525
Rißling, J., Melzer, J., Menke, B., Petermann, F., and Daseking, M. (2015). Sprachkompetenz und Verhaltensauffälligkeiten im Vorschulalter. Das Gesundheitswesen 77, 805–813. doi: 10.1055/s-0035-1564080
Sarimski, K., Röttgers, M., and Hintermair, M. (2015). Pragmatische Kompetenzen und sozial-emotionale Probleme spracherwerbsgestörter Kinder. L.O.G.O.S 23, 84–91.
Stevenson, J., Kreppner, J., Pimperton, H., Worsfold, S., and Kennedy, C. (2015). Emotional and behavioural difficulties in children and adolescents with hearing impairment: a systematic review and meta-analysis. Eur. Child Adolesc. Psychiatry 24, 477–496. doi: 10.1007/s00787-015-0697-1
Tobey, E. A., Thal, D., Niparko, J. K., Eisenberg, L. S., Quittner, A. L., Wang, N. Y., et al. (2013). Influence of implantation age on school-age language performance in pediatric cochlear implant users. Int. J. Audiol. 52, 219–229. doi: 10.3109/14992027.2012.759666
Keywords: conversation skills, social communication, pragmatic language, mental health, emotional problems, deaf, school children
Citation: Holzinger D and Fellinger J (2022) Conversation difficulties rather than language deficits are linked to emotional problems in school children with hearing loss. Front. Educ. 7:944814. doi: 10.3389/feduc.2022.944814
Edited by:
David Pérez-Jorge, University of La Laguna, SpainReviewed by:
Jose Luis Ramos Sanchez, Universidad de Extremadura, SpainAna Isabel González, University of Extremadura, Spain
Copyright © 2022 Holzinger and Fellinger. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Daniel Holzinger, ZGFuaWVsLmhvbHppbmdlckBiYmxpbnouYXQ=
 Daniel Holzinger
Daniel Holzinger Johannes Fellinger
Johannes Fellinger