
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Educ. , 03 October 2022
Sec. Educational Psychology
Volume 7 - 2022 | https://doi.org/10.3389/feduc.2022.939809
This article is part of the Research Topic Advancing Teaching and Learning in Health Sciences Across Healthcare Professionals View all 11 articles
Background: As medical knowledge continues to expand at an accelerated rate, healthcare professionals face a significant challenge in remaining up-to-date. The goal of this narrative review was to present evidence-based learning strategies that could aid postgraduate clinical education.
Design: Articles were sought for using PubMed, Ovid, PsychINFO, ERIC databases and only included if relevant to the review objective.
Results: A total of 103 articles, chapters, and books were used to compose this narrative review. An additional 135 articles and chapters were examined in full for context. The review is divided into two sections: (1) strategies that can help foster a learning mind-set; and (2) high-yield practical tools that are effective in formal or informal learning domains.
Conclusion: Individual learning is a cornerstone of clinical performance, which influences the quality of care that one can deliver. This review offers a comprehensive set of learning tools for individuals across a variety of settings.
By the end of 2020, the “doubling period,” defined as the time taken for the total amount of medical knowledge to double, shortened to just 73 days (Densen, 2011). It is a challenge for clinicians to remain up-to-date with this growing body of information, whilst maintaining a busy clinical practice.
Indeed, the time and resources required for healthcare professionals to digest and employ such information in clinical practice are lacking. To meet imminent healthcare demands, service provision is frequently prioritised over workplace learning (Dornan, 2012). Healthcare professionals face various profession-specific challenges that can make workplace learning difficult. These include: changing patterns of shift work, the physical and emotional burdens of caring for sick patients, administrative responsibilities, and the inconsistent quality and quantity of employer-provided educational opportunities.
If we wish to assimilate and apply new knowledge, we need to develop effective and time-efficient learning skills. Unfortunately we are often ill-prepared to develop new learning methods for clinical practice after graduation (Brown et al., 2007), despite the potential for such methods to impact on our performance (Marsick and Watkins, 2001), and the organisations we work in (Senge, 1991). Learning skills nurtured in university may be inappropriate or unsuitable in healthcare contexts (Tynjälä, 2008; Demiroren et al., 2021). For example, the skills required to engage with a lecture are different to the skills required to distil practical learning points from a ward-round. Learning strategies that are adapted to environments where “formal” learning opportunities are scarce are urgently needed.
Much attention has been given in the educational literature towards improving the environment in which we learn (Spouse, 2001). Organisational factors such as the institutional customs and values, characteristics of the practice environment, subspeciality of the professional and characteristics of their set of patients can readily influence learning behaviour and professionalism (West and Shanafelt, 2007). In contrast, methods that encourage cognitive and knowledge-based learning at an individual level are often neglected. This narrative review attempts to meet this demand, and do so with minimal technical jargon. General strategies are first presented that would enable us to foster a successful learning mindset in the workplace. Practical, high-yield learning tools and enhanced technological solutions which can aid our ongoing medical education are then outlined.
Journal articles (original retro- or prospective studies, technical notes and reviews) and book chapters were identified using PubMed, Ovid, PsychINFO, ERIC, and other medical and non-medical databases. Search parameters included combinations of: “workplace-learning”; “life-long learning”; “continued professional development” OR CPD OR “continuing medical education” OR CME and “self-directed learning.” Combinations of medical subject headings (MeSH) corresponding to the search parameters were also used. English-only articles were sought and could be related to any healthcare discipline. The principal focus of this review was to narrate learning strategies focused on improving information gathering and learning methods in the workplace.
The search was performed on January 10th 2022, and repeated 3 months later to ensure newer articles were not missed. Using related references from the initial search data and subject matter experts, additional literature was identified. Using the search terms above, approximately 1,100 titles and abstracts were screened, of which 135 articles and book chapters were examined in full for context. This included literature related to learning theory, undergraduate education and workplace learning in other industries. A total of 103 articles, chapters and books were included and have been used to compose and support this narrative review. Articles were only included if relevant to the objectives, and were excluded if related to technical skills. Articles focused on communication skills and other soft skills, while equally important, were excluded for this review as they were not part of the intended study objective.
The General Medical Council states in “Good Medical Practice, Domain 1: Knowledge, skills and performance” that “we must keep our professional knowledge and skills up to date; we must regularly take part in activities that maintain and develop our competence and performance” (General Medical Council, 2020). Similarly, the Nursing and Midwifery Council state we must “keep our knowledge and skills up to date, taking part in appropriate and regular learning and professional development activities that aim to maintain and develop our competence and improve our performance” (Nursing and Midwifery Council, 2018). Yet the majority of clinicians find their contractual obligation to engage in life-long post-graduation learning to be an ineffective learning driver.
Why is it important to recognise our learning drivers? Knowledge of why we want to learn provides insight into our learning processes and how best to enjoy the learning. Being aware of our learning drivers, even superficial ones, can help internalise learning motivation, and help learning to become a conscious choice rather than an external obligation (Deci et al., 1991).
Each individual likely responds well to different learning drivers (Table 1). External drivers reward completed learning. For example, learning via formal appraisals and faculty examinations (General Medical Council, 2012) are often rewarded with career progression. Although examinations can drive learning (Wormald et al., 2009), such learning can be superficial in nature–geared only towards passing the assessment (McLachlan, 2006), and can fail to provide long-term knowledge retention and behavioural change. Internal drivers are allied to our desire for autonomy, sense of curiosity, and educational values. Individuals’ optimal development, according to self-determination theory, result from actions motivated by intrinsic interests rather than external reinforcements (Deci et al., 1991). There is evidence to suggest that the greater the influence of our internal motivating drivers, the more likely we are to succeed academically and keep up-to-date (Abrahamson et al., 1999; Snelgrove and Slater, 2003).
Perhaps the most important driver to consider is our attitude towards learning itself, and whether we have accepted responsibility for our own professional development (Ericsson, 2004; Teunissen and Dornan, 2008). Whilst all regulated healthcare professionals are involved in continuing professional development (CPD) activities, these should not be viewed as isolated one-off activities (Stinson et al., 2009). Commitment to being a lifelong learner is central to individual development, and is associated with a wide range of personal and professional benefits (Laal and Salamati, 2012). Research in continuing medical education shows that doctors learn most when they are motivated to identify their own learning needs, and meet those needs at their own pace (Mazmanian and Davis, 2002).
Identifying one’s specific learning needs represents a fundamental aspect of self-directed learning in workplace medicine (Fox and Bennett, 1998). The more explicitly these are articulated, the more likely effective learning will take place (Knowles, 1973). But how do healthcare professionals know what they need to know?
Healthcare workers generally have professional curricula, appraisal, and CPD requirements which represent a template upon which to accrue knowledge and gain competencies. However, learning objectives only offer a narrow view of what is required (Grant, 2002) and shift the focus to be able to work competently and independently, rather than to achieve clinical and personal excellence. Additionally, we have limited insight into our own learning needs, and so this should be done with the support of educational supervisors. Recognising the multitude of sources to stimulate learning, and that feedback and guidance are available from mentors, peers, and patients is key (Walsh, 2006). Below, we present a succinct framework to assess learning needs (Figure 1), according to their source, i.e., whether they are instigated by ourselves or by interactions with others. Here, learning needs are shown to be on a spectrum: from an essential knowledge or skill gap that must be filled, to an opportunity for greater competence, autonomy, and clinical excellence. For a more extensive list, please see The Good CPD Guide which outlines over 40 different methods of assessment (Walsh, 2006; Grant and Zilling, 2017).
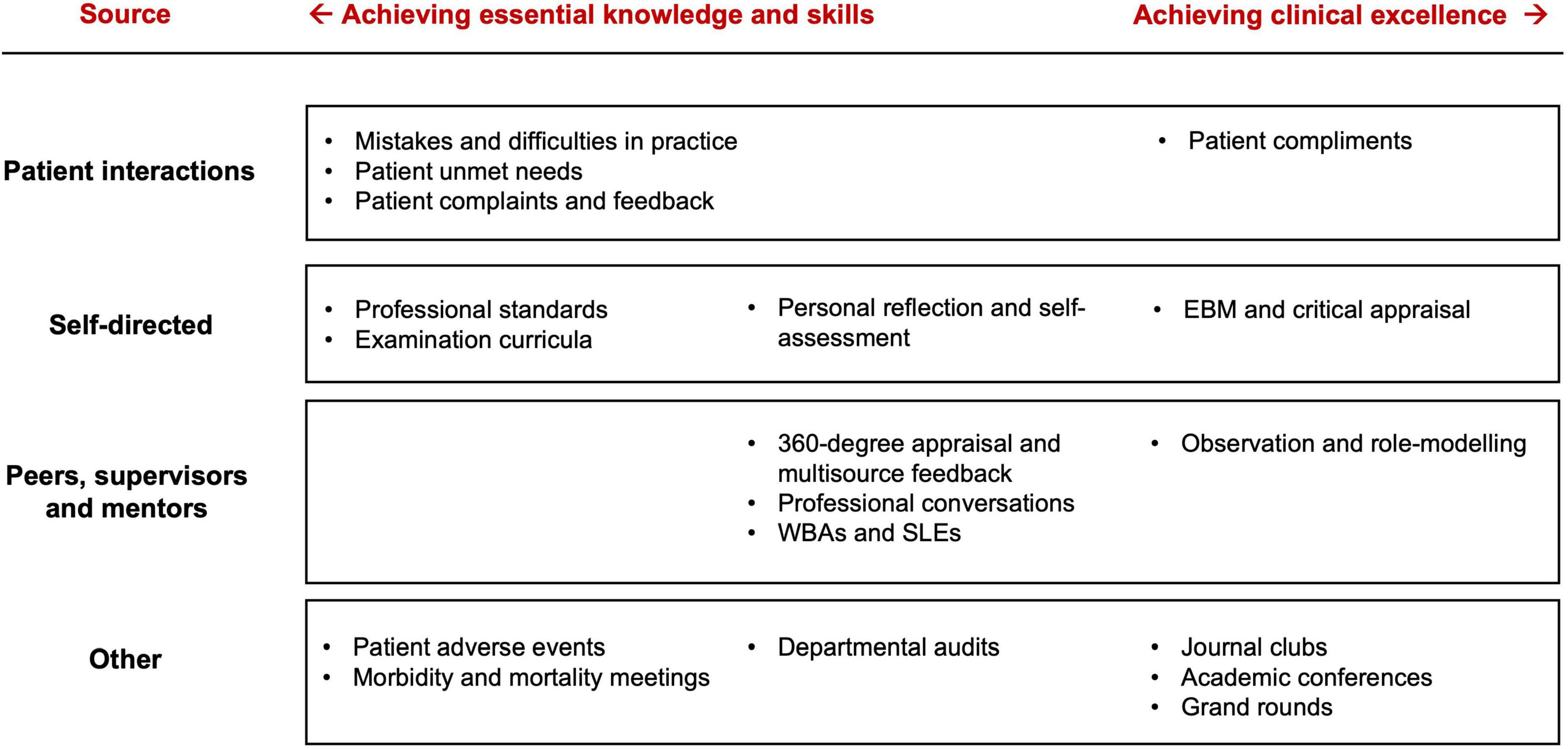
Figure 1. What do I need to learn? A framework of workplace and educational activities which can help identify learning needs. WBA, workplace-based assessment; SLE, supervised learning event; EBM, evidence-based medicine.
As students we were in an enviable position, in which it was socially acceptable not to know things. We were encouraged to be curious, to ask questions, clarify doubts, to seek feedback, and to further our interests (Dyche and Epstein, 2011). In other words, we were encouraged to pursue an “active learning mindset.” Now as health care staff, patients and their families often expect us to behave with absolute certainty (Teunissen and Dornan, 2008). One may feel compelled to hide any uncertainty, for fear it may cause a loss of trust and confidence. The heavy demands of the clinical working day can often lead to negative mental states such as “hurry-up syndrome” and cognitive “overload” (McElhatton and Drew, 1993). Consequently, we can unconsciously switch off to learning during interactions or any activity not clearly signposted as learning. If our mindset remains fixed in this way, not only is our capacity for learning stunted, but may be associated with maladaptive cognitions and stress (Ding et al., 2019). Fortunately, this fixed mindset can be changed (Dweck, 2017).
If we feel overloaded, a simple method can be to take a short pause, even as brief as 10 s (Rall et al., 2008), to interrupt our current mental state, reframe our present experience, and enhance learning (Lee et al., 2021). This can be useful when dealing with unexpected events, anticipating difficult ones, and during long, attentionally-demanding tasks (Vesta and Smith, 1979; Ruhl et al., 1987; Moulton et al., 2010; Lee et al., 2021).
All clinical encounters have the potential to stimulate curiosity and desire to learn, but do require active participation. Active learning is defined as any instructional activity “that involves students doing things and thinking about the things they are doing” (Bonwell and Eison, 1991) and involves efforts to “actively construct knowledge” (Carr et al., 2015). Graffam (2009) describes active learning being made up of three interrelated components: engagement, observation, and reflection. Engagement is influenced by our degree of participation, it is also dependent on our attentional state (Torralba and Doo, 2020). Attention can be recruited by recalling prior knowledge and experience, creating an “educational scaffold.” This allows learning to be both contextual and meaningful (Torralba and Doo, 2020). After a clinical interaction, we can reflect critically to identify ways in which we could have improved, acted differently, or acknowledge what we found particularly interesting. Such reflection can prompt curiosity, and engage learning motivation (Ménard and Ratnapalan, 2013; Eve, 2020). A practical way to maintain a learning mind-set is to keep a real-time diary of topics or observed problems that require clarification. Later, when we have an opportunity to talk with a colleague or access medical resources, we can fill-in the previously identified knowledge gaps.
Despite possessing an effective skill set, if we are sleep-deprived, under-nourished and stressed, learning will be a challenge. Eating a balanced, healthy diet, and ensuring one is sufficiently rested are beneficial for learning and memory (Stickgold et al., 2001; Dani et al., 2005; Gais et al., 2006).
The hours in a day is a finite resource, but the level of our personal energy and motivation has the capacity for renewal (Schwartz, 2007). Energy levels fluctuate during the day, and it may be difficult to study in the limited time period after a clinical shift. Practically speaking, we should cultivate habits to maintain stamina during the shift so as not to be bereft of energy afterwards. Such habits might include taking regular breaks, to utilise breaks to completely disengage from clinical activity (such as going for a short walk off the ward or outside), eating smaller, more frequent meals, and keeping hydrated (Oliver, 2020). We should try to capitalise on business-day-period learning opportunities, such as ward rounds, clinics, and meetings (see Section “Non-formal and informal learning”).
Burnout, occupational stress, and mental health are well-known amongst healthcare professionals (Vijendren et al., 2015) and are associated with decreased patient safety and professional performance (Hall et al., 2016). Stress negatively affects how we learn and remember (Vogel and Schwabe, 2016), whereas feeling relaxed and attentive positively affects cognitive performance. Although it is beyond the scope of this review to offer a comprehensive account of how to manage workplace stress, a simple practice is the use of slow, deep, diaphragmatic breathing to diffuse negative emotional states such as anxiety, impatience, or frustration (Loehr and Schwartz, 2003; Schwartz, 2007; Hopper et al., 2019). Paced breathing has been shown to enhance working memory and motor skill acquisition (Khng, 2016; Yadav and Mutha, 2016). For more lasting positive psychological change, cognitive behavioural therapy and mindfulness-based interventions as stress-reduction techniques have shown particular benefit for healthcare professionals (Vogel and Schwabe, 2016; Clough et al., 2017).
Formal learning typically constitutes a structured program in which set objectives (typically designated by an institution) are met through discrete learning experiences. It entails didactic teaching in the classroom or lecture theatre, induction courses, virtual webinars, and e-learning. Below, we outline a set of evidence-based skills useful in formal learning contexts (Dunlosky, 2013; Sumeracki and Weinstein, 2018) and provide relevant programs and links (Table 2).
Active note-taking describes the process of recording information from teaching sessions for storage and to aid personal encoding. The effectiveness of note-taking can be enhanced by adding material of personal relevance, linking with concrete examples, annotating, and highlighting points of importance, and creating summaries (Hartley and Davies, 2006). Spaced repetition is essential to meaningful learning and retention. Opportunities to re-study learning materials can consolidate understanding and help identify educational gaps (Ausubel and Youssef, 2010). Electronic flashcard applications can prompt repetition, with timing based on algorithms that enhance recall by both distributing and interleaving learning sessions (Wozniak and Abramowicz, 1997). Active reading uses elaborative interrogation and self-explanation to increase our engagement with reading materials, and are of particular use given the vast amount of written information healthcare staff are exposed to. One well-known active reading system is Robinson’s “SQ3R.” This system requires readers to sequentially survey, question, read, recite, and review reading materials (Robinson, 1970). Mind-maps are network diagrams that organise information and identify relationships (Buzan, 2018). The use of mind-maps increase information retention, integrate clinical thinking, and facilitate problem solving (Noonan, 2013).
Non-formal learning constitutes learning that occurs outside of a set curriculum, but is organised in some way. Informal or incidental learning is defined as self-directed learning that has no organisational intention, and is frequently embedded within the work environment. It has been described as “unstructured, unintended, and opportunistic” (Yardley et al., 2012) and can comprise up to 80% of workplace learning (Cross, 2007). Outlined are non-formal and informal learning activities that healthcare professionals frequently participate in, and tips on how to maximise their utility (Table 3).
Many clinicians have been exposed to reflective learning through written experiences in portfolios, but these are often mandated for appraisal and can become a check-box exercise. Personal reflection is essential to the development of expert, life-long learners (Davis et al., 2014) and is one of the most important tools for generating behavioural change. It can help clinicians increase awareness of their understanding, and how they can integrate new skills (Ertmer and Newby, 1996). Although it is important to reflect on errors, it is equally important to recognise when things have gone well. If time is short, reflections can be done rapidly using voice recordings, a reflective selfie, or a brief note written contemporaneously to capture an experience (Grant et al., 2017).
The apprenticeship model remains an important part of clinical education despite the demands of the modern postgraduate environment. An apprentice is shown how to perform their role by an expert, and is assisted before becoming fully independent (Sheehan et al., 2010). An academic coach can help the learner in all stages of the learning cycle: to identify learning needs, facilitate goal setting and accountability, and to assess and contextualise learned skills and knowledge. Experts have a vast wealth of tacit knowledge which the apprentice can learn through observation and role-modelling (Eraut, 2000; Rassie, 2017).
Evidence-based medicine (EBM) has become the approach of choice in appraising, assimilating, and applying new published evidence in modern healthcare. Developing a research question using the population-intervention-comparison-outcome (PICO) format, and establishing the validity and relevance of the derived information remains central (Swanson et al., 2010), but this is time-consuming and ill-suited at the bedside. For this reason, focusing on a select number of questions that are most important in one’s practice is suggested (Slawson and Shaughnessy, 2005). Two methods can make EBM-related practices easier. First, critical appraisal of primary literature can be done in small groups or journal clubs where the workload can be shared. Journal clubs enable postgraduates to keep up to date of new research findings, to enhance their critical appraisal methods, and facilitate greater contextual understanding than what may be achieved alone (Ebbert et al., 2012). Second, software can retrieve relevant and valid evidence automatically (Table 3).
Accessing evidence at the point-of-care via pre-synthesised sources, during or after ward-rounds or consultations, enables evidence-based, patient-orientated decisions to be made quickly and shortens the gap between the identification and fulfilment of a learning need (Slawson and Shaughnessy, 2005). Nowadays, guidelines and digestible “best-practice” information are readily accessible via the use of smartphones without having to perform extensive critical appraisal.
Workplace based assessments (WBAs) and supervised learning events (SLEs) include structured case-based discussions and directly observed procedures. WBAs can promote self-directed learning (Liu, 2012). Learners must apply critical thinking and decision making, and independently formulate a plan or demonstrate clinical and procedural competencies. There are a number of concerns with regards to their implementation, including a lack of clarity about their purpose and the quality of trainer feedback (Massie and Ali, 2016). While much of the onus to deal with these shortcomings will be on assessors and institutions, learners can be more assertive and see WBAs as more than just another hoop to jump through.
Our daily professional learning environment is dominated by discussions of patients and practice (Grant and Zilling, 2017) ranging from case discussion within multidisciplinary meetings to informal conversations in the coffee room. Peer discussion, by engaging in impromptu conversations with colleagues, can digest clinical experiences and clarify difficult topics. In a more organised way, peer-associated learning can be an effective method for postgraduate education (Lockspeiser et al., 2008; Thampy and Kersey, 2017). Peers can better understand the needs of their fellow learners and facilitate a more informal, non-threatening environment in which to learn (Lockspeiser et al., 2008; Thampy and Kersey, 2017).
Social media platforms (Twitter®, Facebook®, WhatsApp®) provide extensive opportunities to foster collaborative learning and engagement from any internet-capable device (Cheston et al., 2013; Jalali et al., 2015). Knowledge sharing on news feeds is particularly useful as a communication medium for healthcare-related updates (Jalali et al., 2015; Jeong and Jalali, 2019). Speciality-specific online forums can be used to discuss difficult cases anonymously, and to learn from the experiences of others (Woods et al., 2019). Media-sharing platforms including Youtube® and audio podcasts offer an almost encyclopaedic amount of contemporaneous educational material. The quality is limited by the knowledge of those creating the content, and is generally not peer-reviewed. To help overcome some of these shortcomings we curate a list of postgraduate-focused podcasts, well-rated by online users (see Supplementary material).
The ways in which individuals learn new knowledge can differ dramatically. Learning depends on a variety of factors including personality, how we process information (Hayes and Allinson, 1994), subspeciality (Curry and Adams, 1991), and prior experiences (Fleming, 2001). Finding a workplace learning strategy that embraces the above and allows us to assimilate and recall critical information is an iterative endeavour. It may take several attempts before finding clinical opportunities that we readily engage with and facilitate effective learning. Generating a workplace personal development plan (PDP) may generate goals which address learning needs. However, they can be rigid and time-limited, may not factor our capacity for informal learning or learning preferences, or take into account the time and energy resources we have available (Jennings, 2007).
While the evidence for individual learning styles remains inconsistent and controversial (Lujan and DiCarlo, 2006; Samarakoon et al., 2013; Kirschner, 2017; Husmann and O’Loughlin, 2019), it is more likely that we engage with, and learn more effectively during, some activities rather than others. If we know our preferred learning strategy, we can select strategy-specific activities to improve our overall learning efficacy. We need to be aware that activities that are less compatible with our preferred learning strategy, will require greater attention and effort. Enhancing our PDP with this information is likely to bring about more effective learning. Following an analysis of a national survey of paediatric residents, Li et al. (2010) proposed a useful paradigm to help achieve learning goals and promote self-directed lifelong learning within a learner’s PDP. The model can be remembered as the mnemonic “ISMART” (Important, Specific, Measurable, Accountable, Realistic, and on a Timeline). Given the information provided in this review, we elaborate on aspects of their model (Table 4).
Common to all effective learning strategies is the reinforcement of knowledge by application in the clinical environment, incorporating this learning into “daily routine” (Table 4). Learning in this way mirrors many of the processes required to become a “Master Adaptive Learner” (Cutrer et al., 2018). To help offer the reader practical ways to assimilate the content of this narrative review, we describe several case scenarios regarding clinicians at various stages of training all of whom have the common desire of improving their learning and the strategies and tools used in each case (see Supplementary material).
This review offers a comprehensive palette of learning tools across a variety of settings and although intended for healthcare postgraduates, students of different disciplines may also find value. Common factors are identified that contribute to positive learning outcomes in formal and informal learning contexts.
This review is however, not without limitations. First is the contemporary nature of some of the resources cited. While attempts have been made to “future-proof” the methods cited, materials including podcasts and types of work-based assessment are likely to change with time. Second, it is likely that further review of other non-medical databases would have identified other useful, relevant learning methods. Third, the review lacks depth in certain areas, in order to provide the reader with a broad armamentarium of tools which, if suitable, can be explored in greater detail.
Technical innovation and changes in healthcare delivery will continue to occur [12], and therefore lifelong learning should be at the core of our thinking (Gopee, 2005; Teunissen and Dornan, 2008). Healthcare staff need to be motivated to learn, and to actively engage with the learning process by recognising their learning drivers and needs. One must assimilate and apply new information in clinical practice contexts.
The author confirms being the sole contributor of this work and has approved it for publication.
The author was supported by a Royal College of Surgeons (England) Research Fellowship. This did not influence the design or outcome of the review.
The author thanks to Mr. Hani Marcus, Miss Lauren Harris, Dr. Paren Chohan, and Dr. Jui Khashu for their comments and suggestions for the manuscript.
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/feduc.2022.939809/full#supplementary-material
Abrahamson, S., Baron, J., Elstein, A. S., Hammond, W. P., Holzman, G. B., Marlow, B., et al. (1999). Continuing medical education for life. Acad. Med. 74, 1288–1294. doi: 10.1097/00001888-199912000-00008
Algiraigri, A. H. (2014). Ten tips for receiving feedback effectively in clinical practice. Med. Educ. Online 19:25141. doi: 10.3402/meo.v19.25141
Ausubel, D. P., and Youssef, M. (2010). The effect of spaced repetition on meaningful retention. J. Gen. Psychol. 73, 147–150. doi: 10.1080/00221309.1965.9711263
Bonwell, C., and Eison, J. (1991). Active learning: Creating excitement in the classroom. ASHE-ERIC higher education reports. Washington, DC: School of Education and Human DevelopmentThe George Washington University.
Brown, J., Chapman, T., and Graham, D. (2007). Becoming a new doctor: A learning or survival exercise? Med. Educ. 41, 653–660. doi: 10.1111/j.1365-2923.2007.02785.x
Buzan, T. (2018). Mind map mastery: The complete guide to learning and using the most powerful thinking tool in the universe, 1st Edn. Minnesota, MN: Watkins.
Carr, R., Palmer, S., and Hagel, P. (2015). Active learning: The importance of developing a comprehensive measure. Act. Learn. High Educ. 16, 173–186. doi: 10.1177/1469787415589529
Cheston, C. C., Flickinger, T. E., and Chisolm, M. S. (2013). Social media use in medical education. Acad. Med. 88, 893–901. doi: 10.1097/acm.0b013e31828ffc23
Clough, B. A., March, S., Chan, R. J., Casey, L. M., Phillips, R., and Ireland, M. J. (2017). Psychosocial interventions for managing occupational stress and burnout among medical doctors: A systematic review. Syst. Rev. 6:144. doi: 10.1186/s13643-017-0526-3
Cross, J. (2007). Informal learning: Rediscovering the natural pathways that inspire innovation and performance. Hoboken, NJ: John Wiley and Sons.
Curry, L., and Adams, C. (1991). Patterns of learning style across selected medical specialties. Educ. Psychol. 11, 247–277. doi: 10.1080/0144341910110304
Cutrer, W. B., Atkinson, H. G., Friedman, E., Deiorio, N., Gruppen, L. D., Dekhtyar, M., et al. (2018). Exploring the characteristics and context that allow master adaptive learners to thrive. Med. Teach. 40, 1–6. doi: 10.1080/0142159x.2018.1484560
Dani, J., Burrill, C., and Demmig-Adams, B. (2005). The remarkable role of nutrition in learning and behaviour. Nutr. Food Sci. 35, 258–263. doi: 10.1108/00346650510605658
Davis, L., Taylor, H., and Reyes, H. (2014). Lifelong learning in nursing: A delphi study. Nurs. Educ. Today 34, 441–445. doi: 10.1016/j.nedt.2013.04.014
Deci, E. L., Vallerand, R. J., Pelletier, L. G., and Ryan, R. M. (1991). Motivation and education: The self-determination perspective. Educ. Psychol. 26, 325–346. doi: 10.1080/00461520.1991.9653137
Demiroren, M., Atilgan, B., Teker, G. T., and Turan, S. (2021). From the lens of the clinical residents: Undergraduate to postgraduate medical education and the transition process. Postgrad. Med. J. 97, 547–555. doi: 10.1136/postgradmedj-2020-138502
Densen, P. (2011). Challenges and opportunities facing medical education. Trans. Am. Clin. Clim. Assoc. 122, 48–58.
Ding, M., Babenko, O., Koppula, S., Oswald, A., and White, J. (2019). Physicians as teachers and lifelong learners. J. Contin. Educ. Health 39, 2–6. doi: 10.1097/ceh.0000000000000228
Dornan, T. (2012). Workplace learning. Perspect. Med. Educ. 1, 15–23. doi: 10.1007/s40037-012-0005-4
Driscoll, J. (2000). Practising clinical supervision: A reflective approach, 1st Edn. Amsterdam: Elsevier Health Sciences.
Dunlosky, J. (2013). Strengthening the student toolbox: Study strategies to boost learning. Am. Educ. 37, 12–21.
Dweck, C. S. (2017). Changing the way you think to fulfil your potential, 6th Edn. London: Robinson.
Dyche, L., and Epstein, R. M. (2011). Curiosity and medical education. Med. Educ. 45, 663–668. doi: 10.1111/j.1365-2923.2011.03944.x
Ebbert, J. O., Montori, V. M., and Schultz, H. J. (2012). The journal club in postgraduate medical education: A systematic review. Med. Teach. 23, 455–461. doi: 10.1080/01421590120075670
Eraut, M. (2000). Non-formal learning and tacit knowledge in professional work. Br. J. Educ. Psychol. 70, 113–136. doi: 10.1348/000709900158001
Ericsson, K. A. (2004). Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad. Med. 79, S70–S81. doi: 10.1097/00001888-200410001-00022
Ertmer, P. A., and Newby, T. J. (1996). The expert learner: Strategic, self-regulated, and reflective. Instr. Sci. 24, 1–24. doi: 10.1007/bf00156001
Fleming, N. D. (2001). Teaching and learning styles?: VARK strategies, 1st ed. Christchurch, NZ: Neil Fleming.
Fox, R. D., and Bennett, N. L. (1998). Continuing medical education: Learning and change: Implications for continuing medical education. BMJ 316:466. doi: 10.1136/bmj.316.7129.466
Gais, S., Lucas, B., and Born, J. (2006). Sleep after learning aids memory recall. Learn. Mem. 13, 259–262. doi: 10.1101/lm.132106
General Medical Council (2012). Continuing professional development: Guidance for all doctors. London: General Medical Council.
General Medical Council, (2020). Good medical practice. Available online at: https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/good-medical-practice (accessed January 10, 2022).
Gopee, N. (2005). Facilitating the implementation of lifelong learning in nursing. Br. J. Nurs. 14, 761–767. doi: 10.12968/bjon.2005.14.14.18553
Graffam, B. (2009). Active learning in medical education: Strategies for beginning implementation. Med. Teach. 29, 38–42. doi: 10.1080/01421590601176398
Grant, A., McKimm, J., and Murphy, F. (2017). Developing reflective practice: A guide for medical students, doctors and teachers, 1st ed. Hoboken, NJ: Wiley Blackwell.
Grant, J. (2002). Learning needs assessment: Assessing the need. BMJ 324:156. doi: 10.1136/bmj.324.7330.156
Grant, J., and Zilling, T. (2017). The good CPD guide. Boca Raton, FL: CRC Press, 69–105. doi: 10.1201/9781315379623-5
Hall, L. H., Johnson, J., Watt, I., Tsipa, A., and O’Connor, D. B. (2016). Healthcare staff wellbeing. burnout, and patient safety: A systematic review. PLoS One 11:e0159015. doi: 10.1371/journal.pone.0159015
Hartley, J., and Davies, I. K. (2006). Note-taking: A critical review. Innov. Educ. Train. Int. 15, 207–224. doi: 10.1080/0033039780150305
Hayes, J., and Allinson, C. W. (1994). Cognitive style and its relevance for management practice. Br. J. Manage. 5, 53–71. doi: 10.1111/j.1467-8551.1994.tb00068.x
Hopper, S. I., Murray, S. L., Ferrara, L. R., and Singleton, J. K. (2019). Effectiveness of diaphragmatic breathing for reducing physiological and psychological stress in adults: A quantitative systematic review. JBI Database System. Rev. Implement. Rep. 17, 1855–1876. doi: 10.11124/jbisrir-2017-003848
Husmann, P. R., and O’Loughlin, V. D. (2019). Another nail in the coffin for learning styles? Disparities among undergraduate anatomy students’ study strategies, class performance, and reported VARK learning styles. Anat. Sci. Educ. 12, 6–19. doi: 10.1002/ase.1777
Jalali, A., Sherbino, J., Frank, J., and Sutherland, S. (2015). Social media and medical education: Exploring the potential of twitter as a learning tool. Int. Rev. Psychiatr. 27, 140–146. doi: 10.3109/09540261.2015.1015502
Jennings, S. F. (2007). Personal development plans and self-directed learning for healthcare professionals: Are they evidence based? Postgrad. Med. J. 83:518. doi: 10.1136/pgmj.2006.053066
Jeong, D., and Jalali, A. (2019). Who tweets in academia? An overview of twitter use in higher education. Adv. Med. Educ. Pract. 10, 171–174. doi: 10.2147/amep.s189963
Khng, K. H. (2016). A better state-of-mind: Deep breathing reduces state anxiety and enhances test performance through regulating test cognitions in children. Cogn. Emot. 31, 1–9. doi: 10.1080/02699931.2016.1233095
Kirschner, P. A. (2017). Stop propagating the learning styles myth. Comput. Educ. 106, 166–171. doi: 10.1016/j.compedu.2016.12.006
Knowles, M. (1973). The adult learner: A neglected species, 1st ed. Houston, TX: Gulf Publishing Company.
Laal, M., and Salamati, P. (2012). Lifelong learning; why do we need it? Procedia. Soc. Behav. Sci. 31, 399–403. doi: 10.1016/j.sbspro.2011.12.073
Lee, J. Y., Szulewski, A., Young, J. Q., Donkers, J., Jarodzka, H., and Van Merriënboer, J. J. G. (2021). The medical pause: Importance, processes and training. Med. Educ. 55, 1152–1160. doi: 10.1111/medu.14529
Li, S.-T. T., Paterniti, D. A., Co, J. P. T., and West, D. C. (2010). Successful self-directed lifelong learning in medicine; a conceptual model derived from qualitative analysis of a national survey of pediatric residents. Acad. Med. 85, 1229–1236. doi: 10.1097/acm.0b013e3181e1931c
Liu, C. (2012). An introduction to workplace-based assessments. Gastroenterol. Hepatol. Bed Bench 5, 24–28.
Lockspeiser, T. M., O’Sullivan, P., Teherani, A., and Muller, J. (2008). Understanding the experience of being taught by peers: The value of social and cognitive congruence. Adv. Health Sci. Educ. 13, 361–372. doi: 10.1007/s10459-006-9049-8
Loehr, J., and Schwartz, T. (2003). The power of full engagement: Managing energy, not time, is the key to high performance and personal renewal. New York, NY: The Free Press.
Lujan, H. L., and DiCarlo, S. E. (2006). First-year medical students prefer multiple learning styles. Adv. Physiol. Educ. 30, 13–16. doi: 10.1152/advan.00045.2005
Marsick, V. J., and Watkins, K. E. (2001). Informal and incidental learning. New Dir. Adult Contin. Educ. 2001, 25–34. doi: 10.1002/ace.5
Massie, J., and Ali, J. M. (2016). Workplace-based assessment: A review of user perceptions and strategies to address the identified shortcomings. Adv. Health Sci. Educ. 21, 455–473. doi: 10.1007/s10459-015-9614-0
Mazmanian, P. E., and Davis, D. A. (2002). Continuing medical education and the physician as a learner: Guide to the evidence. JAMA 288, 1057–1060. doi: 10.1001/jama.288.9.1057
McElhatton, J., and Drew, C. (1993). Hurry-up syndrome. ASRS directline. Available online at: https://asrs.arc.nasa.gov/publications/directline/dl5_hurry.htm (accessed January 5, 2022).
McLachlan, J. C. (2006). The relationship between assessment and learning. Med. Educ. 40, 716–717. doi: 10.1111/j.1365-2929.2006.02518.x
Ménard, L., and Ratnapalan, S. (2013). Reflection in medicine: Models and application. Can. Fam. Physician 59, 105–106.
Moulton, C., Regehr, G., Lingard, L., Merritt, C., and MacRae, H. (2010). ‘Slowing down when you should’: Initiators and influences of the transition from the routine to the effortful. J. Gastrointest. Surg. 14, 1019–1026. doi: 10.1007/s11605-010-1178-y
Noonan, M. (2013). Mind maps: Enhancing midwifery education. Nurs. Educ. Today 33, 847–852. doi: 10.1016/j.nedt.2012.02.003
Nursing and Midwifery Council (2018). The code: Professional standards of practice and behaviour for nurses, midwives and nursing associates. London: Nursing and Midwifery Council.
Oliver, D. (2020). David Oliver: Staff hydration matters more than keeping up appearances. BMJ 368:l7088. doi: 10.1136/bmj.l7088
Patel, R., Green, W., Shahzad, M. W., and Larkin, C. (2015). Use of mobile clinical decision support software by junior doctors at a UK teaching hospital: Identification and evaluation of barriers to engagement. JMIR mHealth uHealth 3:e80. doi: 10.2196/mhealth.4388
Rall, M., Glavin, R. J., and Flin, R. (2008). The ‘10-seconds-for-10-minutes principle’: Why things go wrong and stopping them getting worse. Bull. R. Coll. Anaesth. 51, 2614–2616.
Rangachari, D., Brown, L. E., Kern, D. E., and Melia, M. T. (2016). Clinical coaching: Evolving the apprenticeship model for modern housestaff. Med. Teach. 39, 1–3. doi: 10.1080/0142159x.2016.1270425
Rassie, K. (2017). The apprenticeship model of clinical medical education: Time for structural change. N. Z. Med. J. 130, 66–72.
Ruhl, K. L., Hughes, C. A., and Schloss, P. J. (1987). Using the pause procedure to enhance lecture recall. Teach. Educ. Spec. Educ. 10, 14–18.
Samarakoon, L., Fernando, T., Rodrigo, C., and Rajapakse, S. (2013). Learning styles and approaches to learning among medical undergraduates and postgraduates. BMC Med. Educ. 13:42. doi: 10.1186/1472-6920-13-42
Senge, P. M. (1991). The fifth discipline, the art and practice of the learning organization. Perform. Instr. 30, 37–37. doi: 10.1002/pfi.4170300510
Sheehan, D., Bagg, W., Beer, W., Child, S., Hazell, W., Rudland, J., et al. (2010). The good apprentice in medical education. N. Z. Med. J. 123, 89–96.
Slawson, D. C., and Shaughnessy, A. F. (2005). Teaching evidence-based medicine: Should we be teaching information management instead? Acad. Med. 80, 685–689. doi: 10.1097/00001888-200507000-00014
Snelgrove, S., and Slater, J. (2003). Approaches to learning: Psychometric testing of a study process questionnaire. J. Adv. Nurs. 43, 496–505. doi: 10.1046/j.1365-2648.2003.02747.x
Spouse, J. (2001). Work-based learning in health care environments. Nurs. Educ. Pract. 1, 12–18. doi: 10.1054/nepr.2001.0003
Stickgold, R., Hobson, J. A., Fosse, R., and Fosse, M. (2001). Sleep. Learning, and dreams: Off-line memory reprocessing. Science 294, 1052–1057. doi: 10.1126/science.1063530
Stinson, L., Pearson, D., and Lucas, B. (2009). Developing a learning culture: Twelve tips for individuals, teams and organizations. Med. Teach. 28, 309–312. doi: 10.1080/01421590600726433
Sumeracki, M. A., and Weinstein, Y. (2018). Six strategies for effective learning. Acad. Med. 93:666. doi: 10.1097/acm.0000000000002091
Swanson, J. A., Schmitz, D., and Chung, K. C. (2010). How to practice evidence-based medicine. Plast. Reconstr. Surg. 126, 286–294. doi: 10.1097/prs.0b013e3181dc54ee
Teunissen, P. W., and Dornan, T. (2008). Lifelong learning at work. BMJ 336:667. doi: 10.1136/bmj.39434.601690.ad
Thampy, H., and Kersey, N. (2017). Peer-assisted learning for foundation doctors. Clin. Teach. 14, 180–183. doi: 10.1111/tct.12586
Torralba, K. D., and Doo, L. (2020). Active learning strategies to improve progression from knowledge to action. Rheum. Dis. Clin. N. Am. 46, 1–19.
Tynjälä, P. (2008). Perspectives into learning at the workplace. Educ. Res. Rev. 3, 130–154. doi: 10.1016/j.edurev.2007.12.001
Vesta, F. J. D., and Smith, D. A. (1979). The pausing principle: Increasing the efficiency of memory for ongoing events. Contemp. Educ. Psychol. 4, 288–296. doi: 10.1016/0361-476x(79)90048-1
Vijendren, A., Yung, M., and Sanchez, J. (2015). Occupational health issues amongst UK doctors: A literature review. Occup. Med. 65, 519–528. doi: 10.1093/occmed/kqv088
Vogel, S., and Schwabe, L. (2016). Learning and memory under stress: Implications for the classroom. NPJ Sci. Learn. 1:16011. doi: 10.1038/npjscilearn.2016.11
Walsh, K. (2006). How to assess your learning needs. J. R. Soc. Med. 99, 29–31. doi: 10.1258/jrsm.99.1.29
West, C. P., and Shanafelt, T. D. (2007). The influence of personal and environmental factors on professionalism in medical education. BMC Med. Educ. 7:29. doi: 10.1186/1472-6920-7-29
Wilson, B., and Moffat, N. (2014). Clinical management of memory problems, 2nd Edn. London: Psychology Press.
Woods, J., Moorhouse, M., and Knight, L. (2019). A descriptive analysis of the role of a WhatsApp clinical discussion group as a forum for continuing medical education in the management of complicated HIV and TB clinical cases in a group of doctors in the Eastern Cape, South Africa. South Afr. J. HIV Med. 20:982. doi: 10.4102/sajhivmed.v20i1.982
Wormald, B. W., Schoeman, S., Somasunderam, A., and Penn, M. (2009). Assessment drives learning: An unavoidable truth? Anat. Sci. Educ. 2, 199–204. doi: 10.1002/ase.102
Wozniak, P. A., and Abramowicz, W. (1997). Systems development methods for the next century. Berlin: Springer, 341–344. doi: 10.1007/978-1-4615-5915-3_28
Yadav, G., and Mutha, P. K. (2016). Deep breathing practice facilitates retention of newly learned motor skills. Sci. Rep. 6:37069. doi: 10.1038/srep37069
Keywords: medical education, postgraduate, learning theory, continuing professional development, learning skills
Citation: Pandit AS (2022) Contemporary learning techniques for healthcare professionals: A narrative review. Front. Educ. 7:939809. doi: 10.3389/feduc.2022.939809
Received: 09 May 2022; Accepted: 12 September 2022;
Published: 03 October 2022.
Edited by:
Ana Grilo, Escola Superior de Tecnologia da Saúde de Lisboa (ESTeSL), PortugalReviewed by:
Hai-Hua Chuang, Chang Gung Memorial Hospital, TaiwanCopyright © 2022 Pandit. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anand S. Pandit, YS5wYW5kaXRAdWNsLmFjLnVr
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.