- Physical Activity and Sport Sciences Research Group (GICAFE), Institute for Educational Research and Innovation (IRIE), University of the Balearic Islands, Palma, Spain
The current randomized controlled trial aimed to investigate the effects of a postural education program on daily life habits related to low back pain (LBP) in children. Reducing the disease burden of unspecific LBP in children is of major public health relevance, as children with episodes of LBP tend to experience chronic back pain in adulthood. The study was performed in Majorca (Spain), with 253 primary school children aged between 10 and 12 years. The sample was selected from different clusters (schools) using convenience sampling and randomly distributed into an experimental group (5 schools) or a control group (5 schools). Individual postural items did not improve after the intervention in the experimental group, nor did they improve in the control group. Neither did they improve postural habits score in both groups after the intervention. In conclusion, this telematic intervention has not managed to improve postural habits in children. Nevertheless, there is a lack of evidence to determine whether it is feasible to carry out telematics intervention that promotes lifestyle changes in children.
Introduction
Low back pain (LBP) is the leading cause of disability in the world, and it is on the rise. Reducing the disease burden of unspecific LBP in children is of major public health relevance, as children with episodes of LBP tend to experience chronic back pain in adulthood. According to current evidence, the lifetime prevalence of nonspecific LBP in children aged 7 years old is 33.3% (Miñana-Signes et al., 2021a), and it is larger among children aged 13–15 years old (59.9% in boys and 69.3% in girls) (Kovacs et al., 2003). These data suggest the need to address possible determinants of LBP early, in primary school children, and thus be able to prevent and/or delay its occurrence.
Low back pain is now classified as a biopsychosocial disorder caused by a combination of physical, psychological, and social factors (Marin et al., 2017). For this reason, and from the perspective of LBP prevention, the acquisition of healthy habits in terms of postural education from an early age is considered essential. A habit is a stable mechanism over time, which creates skills or abilities and can be used in various situations of daily life. A set of habits form the customs and forms of behavior of people in various situations of daily life, and therefore influence long-term behavior patterns and have an impact on the state of health and wellbeing (Ministerio de Educación y Deportes, 2017; Fernández et al., 2018). The acquisition of healthy habits should be carried out, especially during childhood, and also during adolescence, with the aim that the habits that are acquired from the beginning are healthy (da Cuña Carrera et al., 2017), since it is more advantageous and easier than trying to change already-established unhealthy habits in adulthood (Centers for Disease Control and Prevention, 2018). Some aspects to take into account that will facilitate the acquisition of these habits and favor their permanence in the long term are: motivation, understanding of the benefits, freedom in decision-making on the part of the child, and having examples to follow in their close environments, such as the family and the educational community, emphasizing that schools perform a fundamental role in promoting the acquisition of healthy habits (Ministerio de Educación y Deportes, 2017).
In addition to education in healthy habits, health education, such as postural education, is also important. Previous studies have concluded that health education helps students to acquire the knowledge, attitudes, and skills necessary to adopt health-enhancing behaviors and to become agents of health promotion in their communities (Lewallen et al., 2015).
In accordance with the above, it is considered necessary to carry out postural education interventions in schools to promote healthy postural habits (Miñana-Signes et al., 2021b; World Health Organization, 2010). However, it is currently difficult to carry out a face-to-face intervention in schools, due to the COVID-19 pandemic. While it is certain that other studies on habit change have been carried out telematically (mHealth interventions) (Free et al., 2013; Abbate et al., 2021), to the best of our knowledge, none have been carried out in child population (Valenciano et al., 2020), due to the complexity involved in interventions with children, such as the limited use of personal mobile phones, or the need to involve families in the interventions, due to their fundamental role in shaping their children’s health choices (Cardon et al., 2002).
At the moment, the results on the positive effects of acquiring knowledge and postural habits found in the studies are inconclusive (Valenciano et al., 2020). The present study hypothesizes that postural education will improve the children’s postural habits and that these improved postural habits will result in a lower prevalence of LBP, preventing its onset at an early age and reducing the intensity and frequency of pain in those cases where LBP is already present. The current study aimed to investigate the effects of a postural education program on daily life habits related to LBP in children aged 10–12 years.
Materials and Methods
Sample
The present study reports the effect of the intervention on the postural habits of the child population, nested in the PEPE randomized controlled trial (Spain). This interventional study aims to prevent LBP in school children and has been described elsewhere (Borras and Vidal-Conti, 2022). In brief, the study was performed in Majorca (Spain), with 253 primary school children. The target group consisted of children aged between 10 and 12 years, who belonged to the fifth and sixth grades. The rationale for choosing this age group was based on the previous literature.
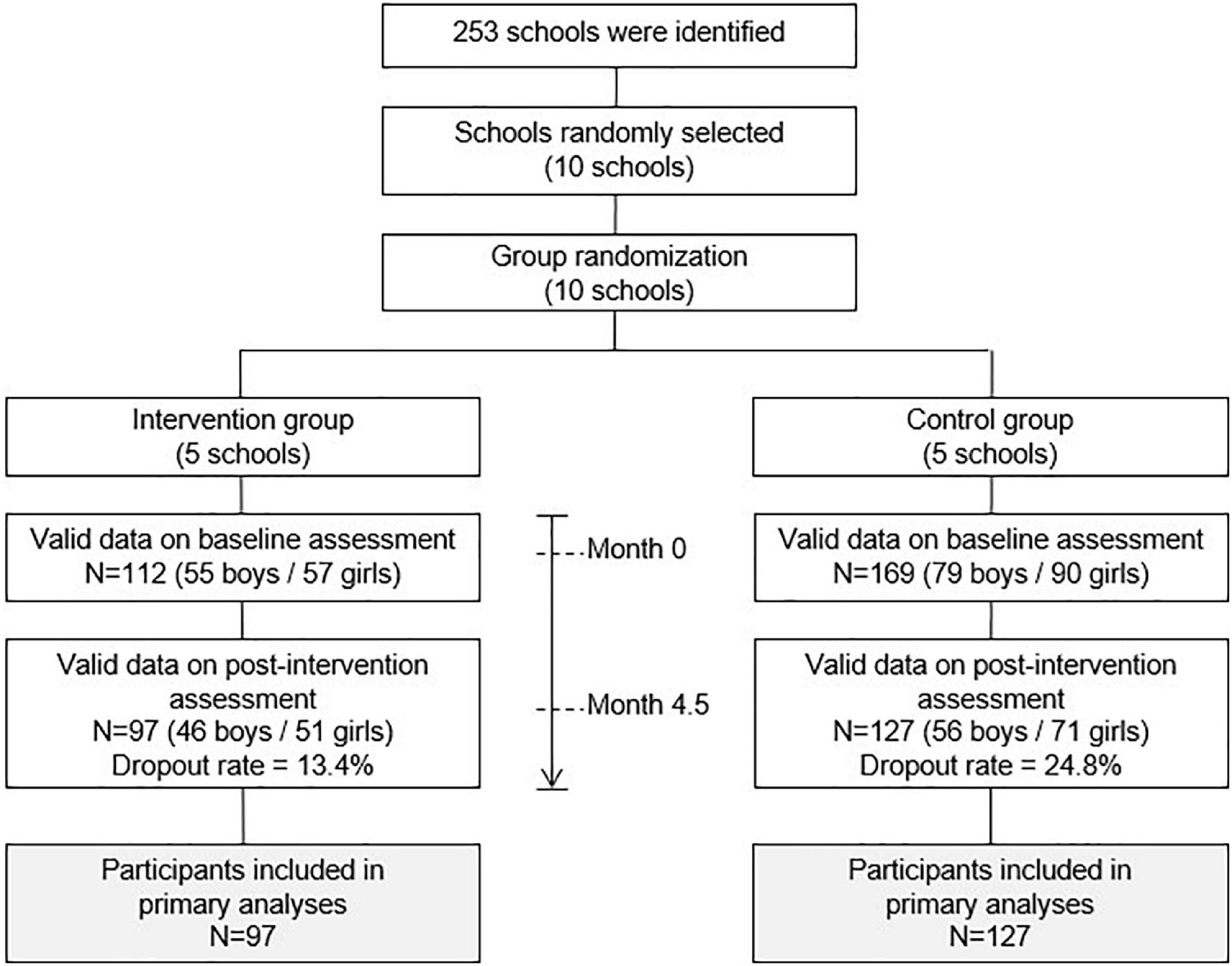
The sample was selected from different clusters (schools) using convenience sampling and randomly distributed into the experimental group (5 schools) or the control group (5 schools). The study flow is depicted in Figure 1.
The inclusion criteria were as follows: students must be aged between 10 and 12 years old and attending fifth-grade or sixth-grade primary school. Exclusion criteria were as follows: students whose parents or tutors did not return the informed consent form signed and those who did not participate due to illness or disability.
Study Design
A 4.5-month intervention program was implemented. Participants were evaluated two times: before the intervention (baseline, month 0) and after the intervention (post-test, month 4.5). All participants (students, teachers, and parents) were informed about the purpose of the study and its procedure. Moreover, students’ parents or tutors were requested to give their consent for children to participate in the study. An informative session was held with the teachers to explain in detail the procedures, aims, and characteristics of the intervention program. Written information was also delivered to the teachers and parents, and a webpage1 was created ad hoc for this study.
Intervention
The overall strategy for developing the project was based on (1) intervention of classroom teachers, physical education teachers, and the school management team; (2) awareness of the educational community (teachers, students, and families); (3) teacher training; and (4) a continuous intervention throughout the academic year. Therefore, the intervention is not carried out directly on children, but in their school environment. The professionals in charge of carrying out the intervention were sports scientists. The research group trained the schools’ teaching staff, both physical education teachers and classroom teachers (tutors of each group) so that it was the teachers who developed the intervention on postural habits with the children.
A 16-week intervention program was carried out between February and June 2021 based on the following components:
(1) Online theoretical training in postural education for teachers through nine recorded videos (10–15 min of duration each) uploaded on the Internet, one per week from the beginning of the intervention. The following topics were addressed: scientific evidence of LBP, human anatomy and physiology, LBP risk factors, healthy physical exercise, ergonomics, postural hygiene, analysis of the use of schoolbags, healthy habits, back care recommendations for Physical Education subjects, and how to develop health-promoting school projects.
(2) Implementation of active breaks for classroom teachers. Teachers were trained to learn how to apply active breaks in their classes throughout the school day during the whole intervention. In addition, a support manual was provided.
(3) Development of a postural education teaching unit for physical education. The duration of the teaching unit was 3 weeks (6 sessions), implemented during weeks 7–9 of the intervention.
(4) Information and awareness campaign implemented by the school (i.e., via posters, school website, social networks, etc.). The dissemination of the information was carried out throughout the 16 weeks of the intervention.
All these resources are available on the website created for this purpose (see text footnote 1).
Instruments
The study was based on two structured and self-administered questionnaires to investigate the prevalence of LBP and the daily postural habits in a population of children aged between 10 and 12 years. Questionnaires were fulfilled by the children at the two measurement times (baseline and post-test) and were administered at school or home. Teachers gave away the questionnaires at the school’s classroom using laptops or provided families with a guide to filling the questionnaires. The questionnaires were available on Google Forms.
The data related to back pain were obtained using a validated questionnaire (Palou et al., 2010) that included lifetime prevalence (never/just once/sometimes/frequently/almost constantly), last 7-day prevalence (yes/no), point prevalence (yes/no), and also included sex (boy/girl) and age (date of birth). In addition, height and weight were included in the questionnaire to determine the body mass index.
Daily postural habits were assessed using the Spanish version (Miñana-Signes et al., 2021c) of the Back Pain and Body Posture Evaluation Instrument (BackPEI) (Noll et al., 2013). The data included sitting position when writing, sitting position on a chair when talking, sitting position when using a computer, the position adopted when lifting an object from the floor, and the type of backpack and how children carry it. Each item was coded as 0 = incorrect and 1 = correct. A sum score was computed from the 6 items, namely, the daily postural habits score (range from 0 to 6), so that the higher the score the healthier daily habits related to LBP.
Statistical Analysis
The analyses were performed with those participants who had complete data at the two measurement points (baseline and post-test) using PASW (Predictive Analytics SoftWare, formerly SPSS), version 23.0 SPSS Inc., Chicago, IL, United States. The level of significance was set at <0.05 for all the analyses. The one-way ANOVA or chi-squared tests were performed, as appropriate, to study group differences at baseline, in continuous and nominal variables, respectively. To examine the effect of the intervention, Student’s t-test and McNemar test were used to analyze baseline and post-test group differences in continuous and nominal variables, respectively.
Results
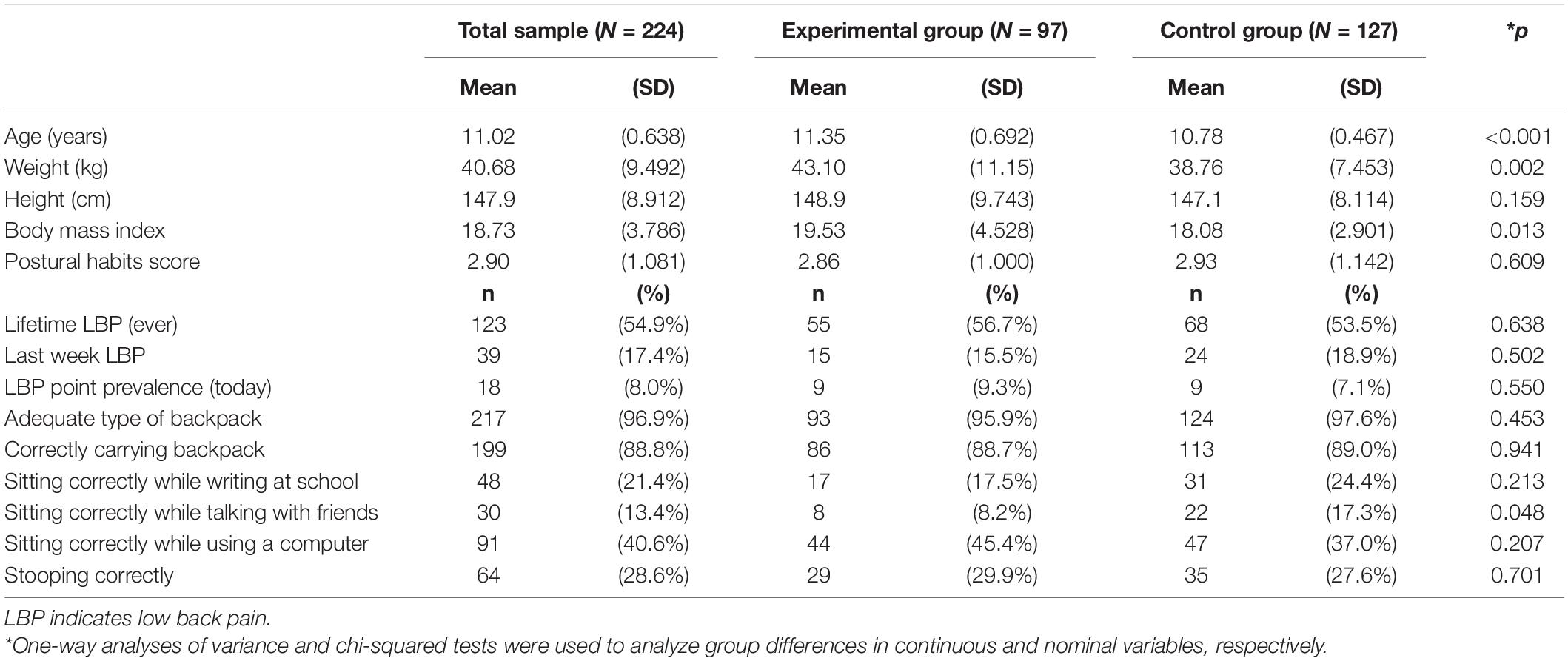
Characteristics of the study sample by the study group are shown in Table 1. Participants were 11.02 years old and had 40.7 kg, 147.9 cm, and 18.7 kg/m2 of weight, height, and body mass index, respectively. The lifetime LBP prevalence rate was 54.9% in the whole study sample. Last week LBP prevalence was 17.4% and LBP point prevalence was 8%. The percentage of children having healthy postural habits is also presented in Table 1.
Participants from both the study groups had similar characteristics at baseline, except for body mass index that was lower in the control group (∼1.5 kg/m2, P = 0.01). Low back pain prevalence and healthy postural habits did not differ between study groups, except for sitting correctly while talking with friends, which was more frequent in the control group (P = 0.048). No initial differences were observed in the postural habits score between the study groups (P = 0.61).
Figure 2 graphically shows how single postural items mostly did not improve after the intervention in the experimental group, and also in the control group. In Table 2 percentage of every single postural item is detailed.
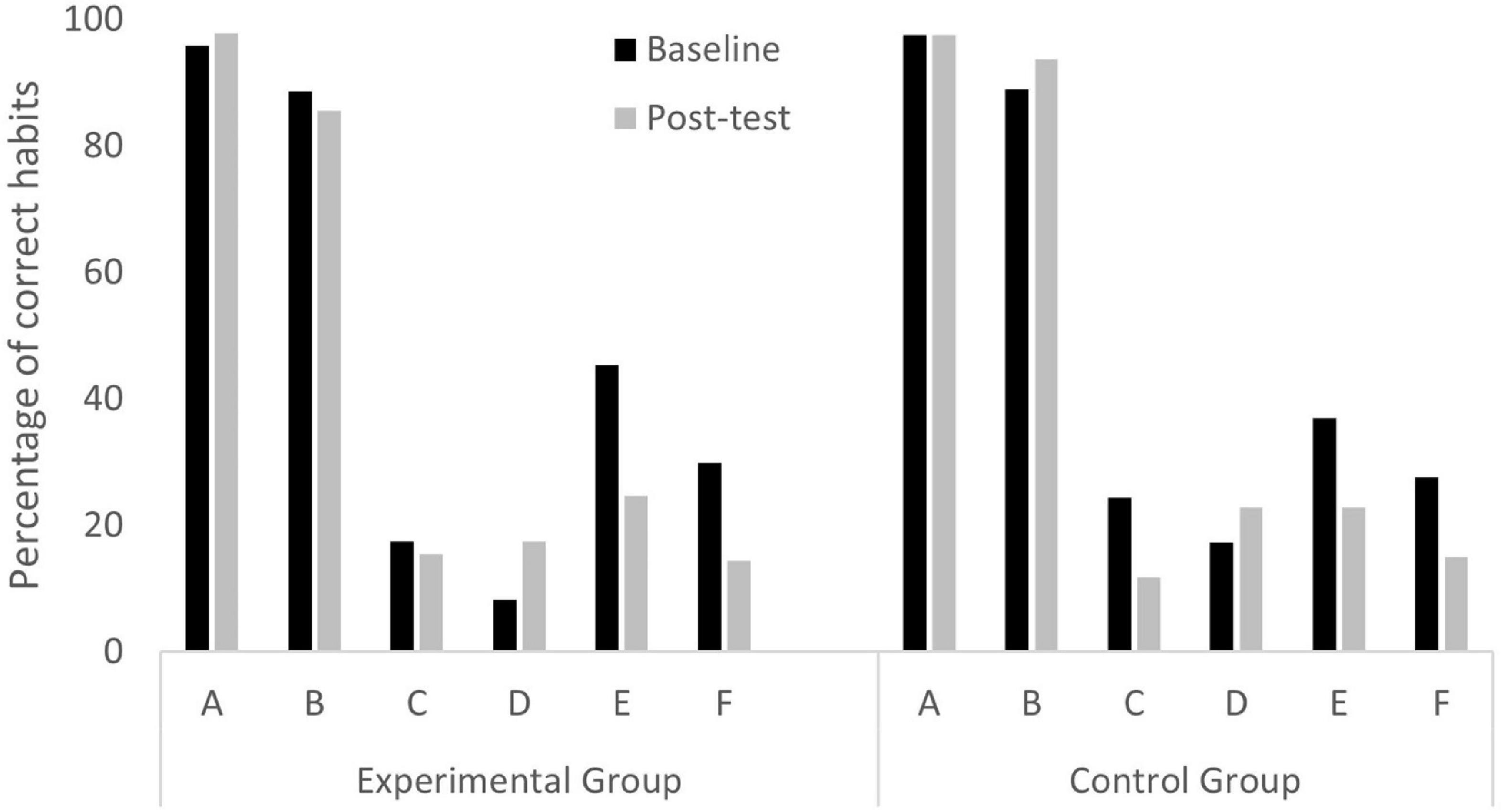
Figure 2. Percentage of participants having correct habits according to the study group at baseline and post-test. A = Adequate type of backpack; B = Correctly carrying backpack; C = Sitting correctly while writing at school; D = Sitting correctly while talking with friends; E = Sitting correctly while using a computer; F = Stooping correctly.
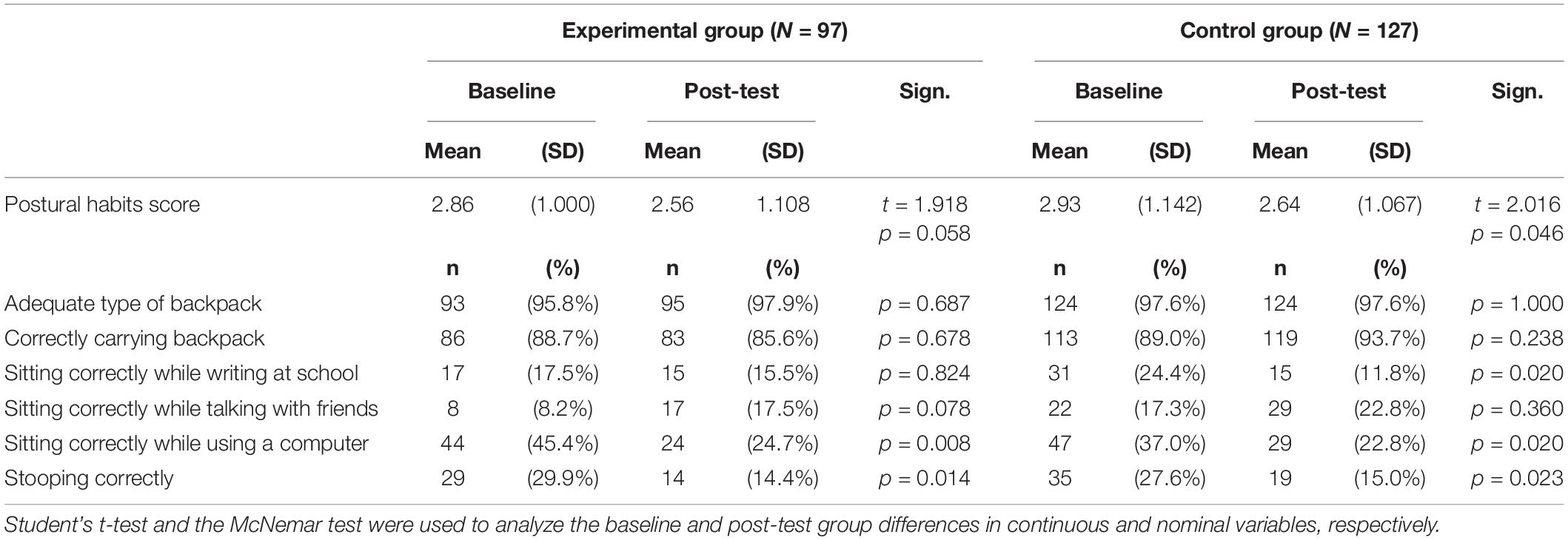
Table 2. Healthy habits score and all the single items at baseline and post-test by the study group.
Discussion
Due to the high prevalence of LBP in children (MacDonald et al., 2017), adolescents (Calvo-Muñoz et al., 2018), and adults (Fatoye et al., 2019), and also disability and costs attributed to LBP (Hartvigsen et al., 2018), it is important to invest time, effort, and economic resources on preventing LBP. In this context, much research is still needed to establish the potential of a school-based postural education program on incident LBP.
The present results suggest that a postural education program applied to children should be face-to-face. The present clinical trial was designed to be a face-to-face intervention, but due to the COVID-19 pandemic, modifications had to be made and the intervention was carried out remotely. The results obtained show that there are no differences in the intervention group between the pre-test and the post-test, and no differences between the intervention group and the control group. In fact, the present intervention, carried out at a distance, has not succeeded in improving the postural habits of the 10–12-year-old school population. A telephone-based intervention aimed at modifying lifestyle habits has found similar difficulties and has not succeeded in changing habits (Williams et al., 2018).
In terms of neuroscientific implications, the present study could improve the neurocognitive functions with the sensorimotor intervention (Scandola et al., 2019) and could be associated with the activation of specific brain networks (Perruchoud et al., 2016) and corticospinal pathways (Perruchoud et al., 2018). Further studies are needed to determine the effect of sensorimotor interventions on neurocognitive functions and corticospinal pathways.
Our results are not consistent with other investments in children and adolescents to prevent LBP through improving knowledge about back care (Geldhof et al., 2006; Miñana-Signes et al., 2019; Minghelli et al., 2021). These interventions were carried out face-to-face in schools, and combined interventions on theoretical knowledge and practical interventions, where physical exercise was performed (Vidal et al., 2013; Minghelli et al., 2021).
As mentioned above, the present intervention has consisted, due to the pandemic situation, of a telematic intervention. On the one hand, it is important to highlight the novelty of the intervention, since to the best of our knowledge, no telematic interventions to promote habit changes in schools have been carried out so far. On the other hand, it is necessary to highlight the difficulty of the intervention to produce improvements in the postural habits of the children, as no significant results were obtained after the intervention, nor when comparing the intervention arms. It could be due to the proposed intervention is not powerful enough to trigger behavioral changes detectable by the used evaluation tools.
Otherwise, there are face-to-face interventions that have neither obtained improvements in children’s postural habits (Dullien et al., 2018) nor in the adult population (Demoulin et al., 2012), so more research is needed to clarify which aspects are key to guarantee the success of interventions to prevent and reduce LBP in children and adolescents. According to the literature, it seems that the most beneficial actions for the prevention of LBP are interventions that combine theoretical knowledge with practical interventions on postural hygiene and physical fitness (Demoulin et al., 2012; Miñana-Signes et al., 2019; Minghelli et al., 2021). In this line, the present intervention has complied with these guidelines, going further and involving tutors teachers, physical education teachers, and families, so that the whole environment of the child was involved in the change of habits. Another cause that may explain the lack of results in habit change interventions related to LBP may be the lack of theoretical knowledge offered to the participants (Demoulin et al., 2012). In this sense, the information offered in this intervention was broad and diverse in topics, to address the prevention of LBP from multiple perspectives: scientific evidence of LBP, human anatomy and physiology, LBP risk factors, healthy physical exercise, ergonomics, postural hygiene, among others. In addition, future research needs to be adapted to the new post-pandemic reality, where telematic interventions have gained a lot of strength, and it will be necessary to determine their viability in child and adolescent populations.
Limitations and Strengths
This study has several limitations. The use of self-reported postural behavior can be a limitation. Future studies should consider the possibility to improve the precision of the measure. Another limitation could be the inexistence of follow-up, which will provide information about how long the effects of an intervention can be retained by the children. A marked strength of this study was the use of a large sample of girls and boys of school age, from 10 different schools, combining schools from different geographical areas, which increases the representativeness of the sample. Furthermore, questionnaires used in this study were previously tested for the correct understanding of the children, validity, and reliability in a sample of similar characteristics.
Conclusion
The data from this study lead to the conclusion that the present intervention, based on postural education and carried out telematically, has not managed to improve postural habits in children. There is a lack of evidence to determine whether it is feasible to carry out a telematics intervention that promotes lifestyle changes in children, and if not, how to adapt interventions for children in pandemic situations that do not allow close contact with this population.
Data Availability Statement
The datasets presented in this article are not readily available because due to participant’s individual consent for using data only for scientific purposes within the research group. Requests to access the datasets should be directed to JV-C: am9zZXAudmlkYWxAdWliLmVz.
Ethics Statement
The study was approved by the Research Ethics Committee of the University of the Balearic Islands (reference number: 130CER19). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author Contributions
AG-P and JV-C prepared the manuscript. AG-P had a major role in conducting the analyses. JV-C has contributed to the funding acquisition and project administration. Both authors contributed to the article and approved the submitted version.
Funding
Grant (RTI2018-101023-A-I00) funded by the Ministry of Science and Innovation MCIN/AEI/10.13039/501100011033 and the “European Regional Development Fund (ERDF) a way of making Europe.”
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
Abbate, M., Fresneda, S., Yañez, A., Ricci-Cabello, I., Galmes-Panades, A. M., Aguilo, A., et al. (2021). Nurse-led telephone intervention for lifestyle changes on glycaemic control in people with prediabetes: study protocol for a randomized controlled trial. J. Adv. Nurs. 77, 3204–3217. doi: 10.1111/JAN.14842
Borras, P. A., and Vidal-Conti, J. (2022). An on-line school-based randomised controlled trial to prevent non-specific low back pain in children. Health Educ. J. 81, 352–362. doi: 10.1177/00178969221077408
Calvo-Muñoz, I., Kovacs, F. M., Roqué, M., Fernández, I. G., and Calvo, J. S. (2018). Risk factors for low back pain in childhood and adolescence: a systematic review. Clin. J. Pain 34, 468–484. doi: 10.1097/AJP.0000000000000558
Cardon, G., de Bourdeaudhuij, I., and de Clercq, D. (2002). Knowledge and perceptions about back education among elementary school students, teachers, and parents in Belgium. J. Sch. Health 72, 100–106. doi: 10.1111/j.1746-1561.2002.tb06524.x
Centers for Disease Control and Prevention (2018). Adolescent And School Health | CDC. Available online at: https://www.cdc.gov/healthyyouth/ (Accessed March 4, 2022).
da Cuña Carrera, I., Lantarón Caeiro, E. M., González González, Y., and Gutiérrez Nieto, M. (2017). Repercusión del sedentarismo en la respuesta cardiorrespiratoria en estudiantes universitarios/sedentarism impact on cardio-respiratory response in college students. Rev. Int. Med. Cienc. Act. Física Deporte 17, 367–378. doi: 10.15366/RIMCAFD2017.66.010
Demoulin, C., Marty, M., Genevay, S., Vanderthommen, M., Mahieu, G., and Henrotin, Y. (2012). Effectiveness of preventive back educational interventions for low back pain: a critical review of randomized controlled clinical trials. Eur. Spine J. 21, 2520–2530. doi: 10.1007/S00586-012-2445-2
Dullien, S., Grifka, J., and Jansen, P. (2018). Cluster-randomized, controlled evaluation of a teacher led multi factorial school based back education program for 10 to 12-year old children. BMC Pediatr. 18:312. doi: 10.1186/s12887-018-1280-y
Fatoye, F., Gebrye, T., and Odeyemi, I. (2019). Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol. Int. 39, 619–626. doi: 10.1007/S00296-019-04273-0
Fernández, J. C., Quiñones, I. T., Robles, ÁS., and Padilla, J. M. S. (2018). Revisión sistemática sobre los estudios de intervención de actividad física para el tratamiento de la obesidad (Systematic Review of Physical Activity Programs for the treatment of Obesity). Retos 33, 261–266. doi: 10.47197/RETOS.V0I33.52996
Free, C., Phillips, G., Galli, L., Watson, L., Felix, L., Edwards, P., et al. (2013). The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med. 10:e1001362. doi: 10.1371/JOURNAL.PMED.1001362
Geldhof, E., Cardon, G., de Bourdeaudhuij, I., and de Clercq, D. (2006). Effects of a two-school-year multifactorial back education program in elementary schoolchildren. Spine (Phila Pa 1976) 31, 1965–1973. doi: 10.1097/01.brs.0000228722.12968.d2
Hartvigsen, J., Hancock, M. J., Kongsted, A., Louw, Q., Ferreira, M. L., Genevay, S., et al. (2018). What low back pain is and why we need to pay attention. Lancet 391, 2356–2367. doi: 10.1016/S0140-6736(18)30480-X
Kovacs, F. M., Gestoso, M., Gil del Real, M. T., Lopez, J., Mufraggi, N., and Mendez, J. I. (2003). Risk factors for non-specific low back pain in schoolchildren and their parents: a population based study. Pain 103, 259–268. doi: 10.1016/S0304-3959(02)00454-2
Lewallen, T. C., Hunt, H., Potts-Datema, W., Zaza, S., and Giles, W. (2015). The whole school, whole community, whole child model: a new approach for improving educational attainment and healthy development for students. J. Sch. Health 85, 729–739. doi: 10.1111/JOSH.12310
MacDonald, J., Stuart, E., and Rodenberg, R. (2017). Musculoskeletal low back pain in school-aged children: a review. JAMA Pediatr. 171, 280–287. doi: 10.1001/JAMAPEDIATRICS.2016.3334
Marin, T. J., van Eerd, D., Irvin, E., Couban, R., Koes, B. W., Malmivaara, A., et al. (2017). Multidisciplinary biopsychosocial rehabilitation for subacute low back pain. Cochrane Database Syst. Rev. 6:CD002193. doi: 10.1002/14651858.CD002193.PUB2
Miñana-Signes, V., Monfort-Pañego, M., and Rosaleny-Maiques, S. (2019). Improvement of knowledge and postural habits after an educational intervention program in school students. J. Hum. Sport Exerc. 14, 47–60. doi: 10.14198/JHSE.2019.141.04
Miñana-Signes, V., Monfort-Pañego, M., Bosh-Bivià, A. H., and Noll, M. (2021a). Prevalence of low back pain among primary school students from the city of valencia (Spain). Healthcare 9:270. doi: 10.3390/healthcare9030270
Miñana-Signes, V., Monfort-Pañego, M., and Valiente, J. (2021b). Teaching Back health in the school setting: a systematic review of randomized controlled trials. Int. J. Environ. Res. Public Health 18:979.
Miñana-Signes, V., Monfort-Pañego, M., Morant, J., and Noll, M. (2021c). Cross-cultural adaptation and reliability of the Back pain and body posture evaluation instrument (BackPEI) to the Spanish adolescent population. Int. J. Environ. Res. Public Health 18:854. doi: 10.3390/ijerph18030854
Minghelli, B., Nunes, C., and Oliveira, R. (2021). Back school postural education program: comparison of two types of interventions in improving ergonomic knowledge about postures and reducing low back pain in adolescents. Int. J. Environ. Res. Public Health 18:4434. doi: 10.3390/ijerph18094434
Ministerio de Educación y Deportes (2017). “Formación de hábitos alimentarios y de estilos de vida saludables,” in Currículo de Educación Inicial. Caracas, Ministerio de Educación y Deportes, República Bolivariana de Venezuela, 331–366.
Noll, M., Tarragô Candotti, C., Vieira, A., and Fagundes Loss, J. (2013). Back pain and body posture evaluation instrument (backpei): development, content validation and reproducibility. Int. J. Public Health 58, 565–572. doi: 10.1007/s00038-012-0434-1
Palou, P., Kovacs, F. M., Vidal, J., Gili, M., Borràs, P. A., Gestoso, M., et al. (2010). Validation of a questionnaire to determine risk factors for back pain in 10-12 year-old school children. Gazzetta Med. Italiana Arch. Sci. Med. 169, 199–205.
Perruchoud, D., Fiorio, M., Cesari, P., and Ionta, S. (2018). Beyond variability: subjective timing and the neurophysiology of motor cognition. Brain Stimul. 11, 175–180.
Perruchoud, D., Michels, L., Piccirelli, M., Gassert, R., and Ionta, S. (2016). Differential neural encoding of sensorimotor and visual body representations. Sci. Rep. 6:37259.
Scandola, M., Dodoni, L., Lazzeri, G., Arcangeli, C. A., Avesani, R., Moro, V., et al. (2019). Neurocognitive benefits of physiotherapy for spinal cord injury. J. Neurotrauma 36, 2028–2035.
Valenciano, P. J., Cibinello, F. U., de Jesus Neves, J. C., and Fujisawa, D. S. (2020). Effects of postural education in elementary school children: a systematic review. Rev. Paulista Pediatr. 39:e2020005.
Vidal, J., Borras, P. A., Ponseti, F. J., Cantallops, J., Ortega, F. B., and Palou, P. (2013). Effects of a postural education program on school backpack habits related to low back pain in children. Eur. Spine J. 22, 782–787. doi: 10.1007/s00586-012-2558-7
Williams, A., Wiggers, J., O’Brien, K. M., Wolfenden, L., Yoong, S. L., Hodder, R. K., et al. (2018). Effectiveness of a healthy lifestyle intervention for chronic low back pain: a randomised controlled trial. Pain 159, 1137–1146.
World Health Organization (2010). Recomendaciones Mundiales sobre Actividad Física para la Salud. Geneva: WHO Library Cataloguing-in-Publication, 1–58. Available online at: http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:Recomendaciones+Mundiales+sobre+actividad+FIsica+para+la+salud#4 (accessed March 4, 2022).
Keywords: low back pain, children, postural education, primary school, school health
Citation: Galmes-Panades AM and Vidal-Conti J (2022) Effects of Postural Education Program (PEPE Study) on Daily Habits in Children. Front. Educ. 7:935002. doi: 10.3389/feduc.2022.935002
Received: 03 May 2022; Accepted: 24 June 2022;
Published: 27 July 2022.
Edited by:
Matias Noll, Goiano Federal Institute (IFGOIANO), BrazilReviewed by:
Silvio Ionta, University of Lausanne, SwitzerlandVicente Miñana-Signes, University of Valencia, Spain
Bruna Da Rosa, Federal University of Rio Grande do Sul, Brazil
Copyright © 2022 Galmes-Panades and Vidal-Conti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Josep Vidal-Conti, am9zZXAudmlkYWxAdWliLmVz
 Aina Maria Galmes-Panades
Aina Maria Galmes-Panades Josep Vidal-Conti
Josep Vidal-Conti