- Medical Faculty, Centre for Health and Society, Institute of Medical Sociology, Heinrich Heine University Düsseldorf, Düsseldorf, Germany
Due to the demanding work environment, healthcare workers are often affected by mental health problems. Besides negative effects on individual wellbeing, mental health problems can reduce professional effort and increase turnover rates in healthcare. Those who develop mental health problems often receive necessary treatment with a great time delay. Two reasons for this are low mental health literacy and stigma. However, empirical investigations regarding the role of workplace mental health literacy and stigma on help-seeking and help-outreach intentions of healthcare workers in the workplace are currently missing. To bridge this gap, survey data was collected among trainees of different healthcare professions in Germany. The variables of interest were measured separately with the help of two times of measurement to avoid common method bias and to strengthen the causal interpretability of the hypothesized model. The response rate of the questionnaire was 21% (Nt1 = 525, Nt2 = 112). For measuring subjective mental health literacy at the workplace the MHL-W-G was used. Results of the structural equation modeling (SEM) indicate that workplace mental health literacy increases workplace help-seeking intention and help-outreach intention significantly. Further, it indicates that workplace mental health literacy decreases self-stigma and that personal stigma decreases overall workplace help-outreach intention. In order to uncover underlying mechanisms of the relationship between the mental health literacy and workplace help-seeking intention and help-outreach intention, the mediation of mental health stigma was tested, but could not be confirmed. The present study reduces the lack of empirical information regarding mental health help-seeking and help-outreach in the workplace. Therefore, the research contributes to the relevance of social contacts in the working context as potential gatekeepers to professional mental health support. Further, the study provides important insights into the way that mental health help-seeking and help-outreach intentions at the workplace are affected by mental health literacy and into the role of personal and self-stigma in healthcare profession. The results are of particular importance in light of the increased need for healthcare workers and the rising prevalence of mental diseases.
Introduction
Over the last years, job demands and job complexity in the healthcare sector have increased (Uchiyama et al., 2013; Mehta and Pandit, 2018), which has additionally elevated during the COVID-19 pandemic (Barello et al., 2020; Mahmud et al., 2021). Healthcare workers in care and nursing functions (e.g., nurses, midwives, and surgical assistants) are frequently confronted with conflicts, role ambiguity and patient aggression (Lim et al., 2010). Accordingly, working in a healthcare profession increases the relative risk of developing an affective or stress-related disorder compared to other branches (Wieclaw et al., 2006; Gärtner et al., 2010). Due to the demanding work environment, healthcare workers often report mental health problems such as anxiety, depression and burnout (Gärtner et al., 2010; Perry et al., 2015; O’Connor et al., 2018). Along with mental health problems of healthcare workers, the risk for healthcare associated errors, patient mortality (Gärtner et al., 2010; Dyrbye et al., 2017a) and turnover rates increase (Aiken et al., 2012; Dyrbye et al., 2017a). Therefore, the protection and promotion of mental health in the healthcare profession is of high importance for individuals, organizations and society.
With the current global public health crisis due to the COVID-19 pandemic, the mental health of healthcare workers received particular attention in research and the media. Global reviews and meta-analyses indicate, that the current emergency situation increases the existing high job demands of healthcare workers further and adds new ones such as the fear of infection/infecting others, ethical dilemmas, and the exposure to much higher numbers of death (Benzinger et al., 2021; Cordoba, 2021; Leo et al., 2021). As a result, the prevalence of anxiety, depression, burnout, sleep disorders, and stress level among healthcare workers has been rising (Sampaio et al., 2020; Leo et al., 2021; Mahmud et al., 2021).
Although the mental health of healthcare workers is an issue of major importance, addressing mental health problems in the working context is complex (Moll et al., 2013; Hudson et al., 2021). As two sides of the same coin, seeking help when suffering from mental health problems and reaching out for people who are in need, are described as the two “key mental health access behaviors” for early prevention (Moll et al., 2015, p. 2). Surprisingly, seeking help and offering help to others is as challenging for healthcare workers as for anyone else, even though they have professional knowledge (Wang et al., 2005; Gärtner et al., 2010). As a consequence, affected individuals hesitate to address formal or informal sources for help (Wang et al., 2005). Therefore, only few affected individuals receive necessary treatment within a timely manner (Wang et al., 2007; Rickwood et al., 2012). This delay leads to a progression of the mental health problem (Kessler et al., 2003; World Health Organization [WHO], 2017) and reduces the chances of recovery (Wang et al., 2005).
Mental health help-seeking in the workplace can be a dilemma across all occupational groups. On the one hand, revealing mental health problems at work is often associated with a violation of privacy and can affect career prospects as well as job security due to stigmatization (Wheat et al., 2010; Brohan et al., 2012; Hastuti and Timming, 2021). On the other hand, disclosing a mental health problem in the working context can increase the self-esteem of affected people and help them to cope better with the disease (Rüsch et al., 2005; Brohan et al., 2012; Hastuti and Timming, 2021). For healthcare workers further challenges occur, as a recent review assembled (Hudson et al., 2021): Firstly, healthcare workers could face licensing issues, when disclosing a mental health problem at the workplace. Secondly, healthcare workers may feel that their professional identity is threatened if they disclose a mental health problem at the workplace, which is critical as the occupation is associated with high responsibility. Last but not least, healthcare workers are especially worried of letting their team down with regard to high workloads in healthcare professions. To sum it up, there are reasonable disadvantages of seeking help for a mental health problem in the workplace, which is why many healthcare workers remain silent (Moll et al., 2013).
Most studies on mental health help-seeking and help-outreach and their antecedents focus on the private environment investigating the role of informal sources, such as family and friends, as well as formal sources, such as psychiatrists (Rossetto et al., 2016; Jung et al., 2017; Schnyder et al., 2017; Benuto et al., 2020; Thompson et al., 2022). The working context, covering colleagues and supervisors as sources of help, has rarely been studied. Due to their proximity and daily interaction, colleagues and supervisors might recognize changes in mental health even before family or friends. And—despite all disadvantages of disclosure mentioned—they can offer valuable social support at the workplace in challenging times (Schug et al., 2021). As affected people are more likely to seek help if suggested by others (Cusack et al., 2004; Vogel et al., 2007a), help-outreach by colleagues as well as supervisors could play a central role in early prevention at the workplace (Kunyk et al., 2016; Moll et al., 2017; Geuijen et al., 2020) and lower the economic and social burden of mental health problems on companies and society (Aiken et al., 2012; Rebscher et al., 2016; Dyrbye et al., 2017a).
To gain a better understanding of help-seeking and help-outreach behavior for a mental health problem, it is necessary to consider their antecedents. Two major barriers are discussed in the literature, which decrease help-seeking and help-outreach behavior for a mental health problem: On the one hand, poor mental health literacy (Corrigan, 2004; Rickwood et al., 2005; Smith and Shochet, 2011), which is defined as “knowledge and beliefs about mental disorders” (Jorm et al., 1997, p. 182), keeps individuals from recognizing mental problems in themselves and others. On the other hand, mental health stigma, defined as the process of labeling affected people with negative stereotypes (Corrigan, 2000; Link and Phelan, 2001), is discussed as another major barrier (Schnyder et al., 2017; Stolzenburg et al., 2018). Although these barriers are described in the literature, research regarding mental health literacy (Moll et al., 2015, 2017, 2018) and stigma (Ross and Goldner, 2009; Verhaeghe and Bracke, 2012) of healthcare workers is limited. Surprisingly, few studies examined the impact of mental health stigma on the willingness to seek or provide help for mental health problems among healthcare workers in the working context (for exceptions see Moll et al., 2015; Moll et al., 2018). Further, most research examined mental health literacy and mental health stigma separately instead of investigating the relationship of both in order to predict help-seeking and help-outreach behavior (for an exception see Cheng et al., 2018 and Wang et al., 2019). Without the understanding of the relationship between these two major barriers, it remains unclear which mechanism underlies the help-seeking and help-outreach behavior of healthcare workers.
Studies revealed mixed results regarding the relationship of mental health literacy and stigma (Jung et al., 2017; Moll et al., 2018). In fact, some empirical results indicate that there is no relationship between mental health literacy and stigma (Cheng et al., 2018), whereas others showed a decrease in stigma for better mental health literacy (Milin et al., 2016; Morgan et al., 2018; Schomerus et al., 2018). Regarding healthcare workers, the relationship of the constructs becomes even more complex. Due to their profession, healthcare workers tend to have high mental health literacy but are not necessarily low in stigmatizing attitudes (Bourget and Chenier, 2007). The present study contributes to a better understanding of help-seeking and help-outreach behavior in the healthcare profession and, therefore, also supports the protection and promotion of mental health of professionals and their patients (Wiederkehr, 2012). This is particularly critical with regard to the increasing demand for the health workforce as well as the rising prevalence of mental diseases (Aiken et al., 2012; Dyrbye et al., 2017a; Kuhlmann et al., 2018).
Against this background, the aim of this study is to examine the role of mental health literacy and stigma on help-seeking and help-outreach intentions of healthcare workers in the workplace.
Conceptual Background and Development of Hypotheses
Help-Seeking Behavior and Help-Outreach Behavior
Research on help-seeking for mental health issues has been of great interest as it is the key to break the vicious circle of silence and untreated mental health problems. There are different conceptualizations of help-seeking behavior (Cauce et al., 2002; Rickwood et al., 2005; Cornally and McCarthy, 2011). A commonly shared definition described it as a “complex decision-making process instigated by a problem that challenges personal abilities” (Cornally and McCarthy, 2011, p. 280). Further, help-seeking when facing a mental health problem requires to interact and to communicate with others in order to get support “in terms of understanding, advice, information [and] treatment” (Rickwood et al., 2005, p. 4). Cauce et al. (2002) introduced a model for mental health help-seeking, which has originally been intended to explain adolescents’ pathways into mental health services. The model includes three interrelated phases: (1) problem recognition, (2) decision to seek help and (3) service selection (Cauce et al., 2002). Based on that model for mental health help-seeking, it is crucial that: (1) an individual recognizes changes in mental health or first symptoms of a mental health problem in order to be able to seek help. If the problem is (2) defined as undesirable and prolonged, the individual plans to seek help and (3) decides which informal or formal sources should be approached.
The mental health help-seeking process is shaped by different factors that facilitate or reduce the progression of the process (Cauce et al., 2002; Rickwood et al., 2005). One major barrier is individual’s mental health literacy (Corrigan, 2004; Rickwood et al., 2005; Smith and Shochet, 2011), which refers to the ability to recognize mental health problems, knowledge and attitudes that contribute to the prevention, detection, and treatment, as well as skills, to support others who are displaying symptoms of mental illness (Jorm et al., 1997; Jorm, 2011). Research has shown that high mental health literacy significantly promotes help-seeking (Jorm et al., 2000; Rüsch et al., 2011; Bonabi et al., 2016) and help-outreach (Hadlaczky et al., 2014; Rossetto et al., 2016), as it facilitates the initial problem recognition (Cauce et al., 2002). If mental health literacy is high, individuals are able to recognize mental health problems both in themselves and in others and respond adequately (Moll et al., 2015, 2017, 2018). In general, healthcare workers are expected to have a high level of mental health literacy (Moll et al., 2015). However, mental health knowledge and skills can vary among healthcare workers due to their different training backgrounds and varying degree of contact with mental disorders. According to Moll et al. (2015), high mental health literacy significantly promotes help-seeking and help-outreach behavior in the workplace as it enables individuals to recognize changes in own mental health and those of others. Further, people with high mental health literacy can assist affected people with the service selection. As a proxy for help-seeking behavior, intentions to seek help can be used (Rüsch et al., 2011; Angermeyer et al., 2013; Ando et al., 2018). Accordingly, hypothesis 1a is formulated as follows:
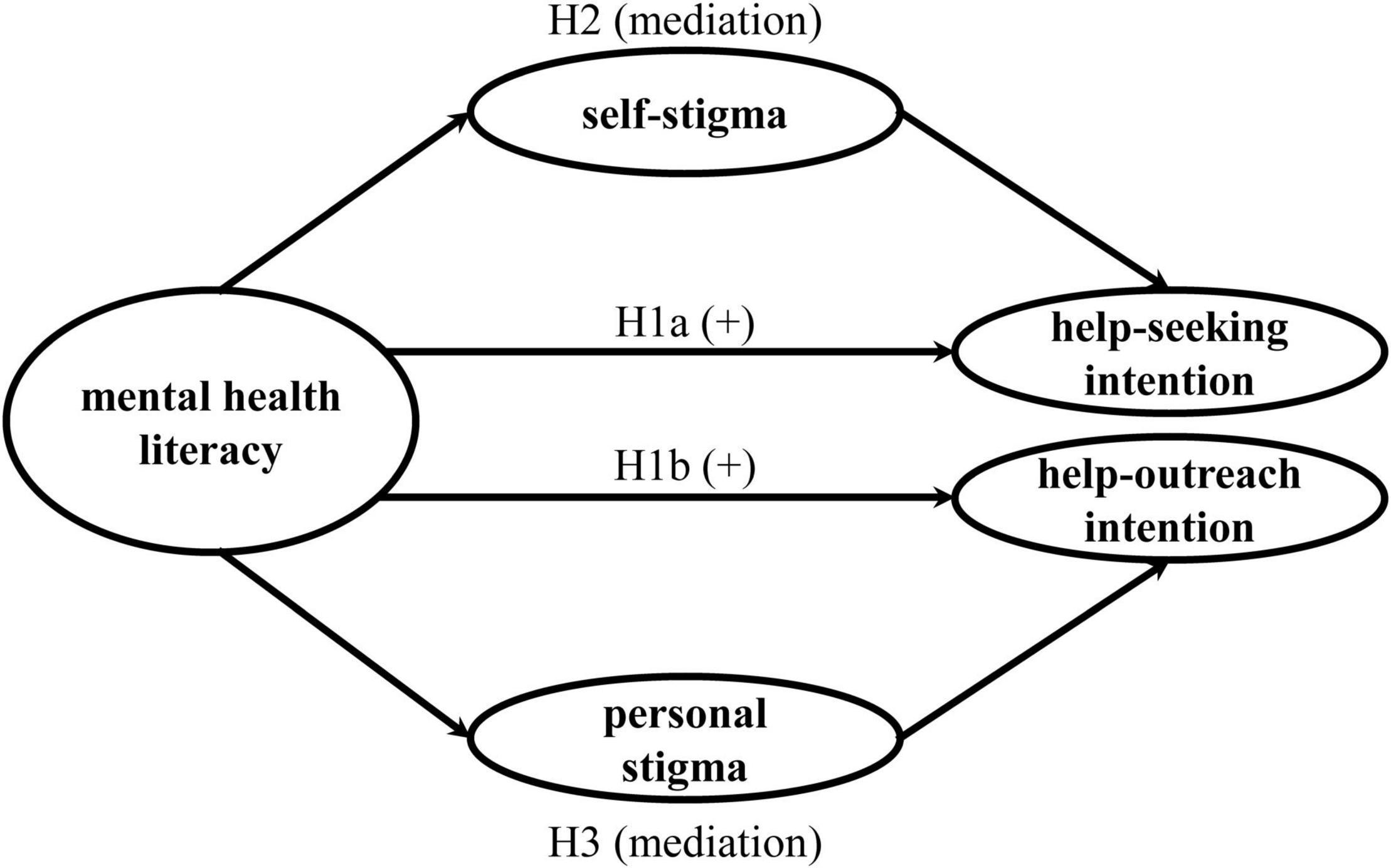
H1a: Mental health literacy is positively associated with help-seeking intention in the workplace of healthcare workers.
Affected individuals may not always recognize or acknowledge their own evolving or manifested mental health condition or may lack information about how to access professional support. Therefore, social contacts like friends, family or colleagues could be of great value in the mental health help-seeking process (Langlands et al., 2008; Moll et al., 2015; Rossetto et al., 2016). Social contacts‘ help-outreach behavior is a form of limited, non-professional support until “appropriate professional help is received or the crisis resolves” (Langlands et al., 2008, p. 435). Based on the idea of “mental health first aid” (Langlands et al., 2008, p. 435), social contacts could provide useful help along the mental health help-seeking process. Initially, help-outreach supports the awareness of changes in mental state by addressing and informing affected individuals in the recognition phase (Jorm et al., 2010; Moll et al., 2015). Further, social contacts support affected individuals during the decision to seek help and in the service selection by referring them to professional support, employee assistance programs, self-help groups or even offer their own support during a crisis (Jorm et al., 2010; Moll et al., 2015). For example, a review by Kunyk et al. (2016) shows that especially colleagues appear to be a source of help for healthcare workers with an addiction. However, social contacts could only function as gatekeeper to professional support when they have the necessary knowledge, mindset and skills to provide appropriate help. As mentioned above, intention to offer help can be used as a proxy for help-outreach behavior (Rüsch et al., 2011; Angermeyer et al., 2013; Ando et al., 2018). Accordingly, hypothesis 1b is formulated as follows:
H1b: Mental health literacy is positively associated with help-outreach intention in the workplace of healthcare workers.
The Role of Stigma for Help-Seeking Behavior and Help-Outreach Behavior
The public tends to stigmatize people suffering from a mental disorder, e.g., depression or psychosis, more than people with a physical disorder (Corrigan et al., 2001). Stigma has various pathways through which it can develop and interfere with the lives of affected individuals. For that reason, mental health stigma is discussed as a key barrier to the mental health help-seeking process. The decision to seek help is shaped by the extend of one’s mental health stigma (Cauce et al., 2002; Cheng et al., 2018). Also, the potential support of colleagues depends on their levels of mental health stigma (Moll et al., 2017). Mental health stigma refers to the “process of objectifying and dehumanizing a person known to have or appearing to have a mental disorder” (Mendoza et al., 2015, p. 209) by labeling affected people with negative stereotypes (Corrigan, 2000; Link and Phelan, 2001). Those negative stereotypes or prejudices of mentally ill are rooted in the performance-oriented values of societies (Parsons, 1951; Siegrist, 2005) and can be found in most modern cultures (Arboleda-Flórez, 2002). A particularly strong and harmful stereotype portrays people with mental disorders as perilous and unpredictable. From a behavioral perspective, negative stereotypes or pejudice on the mentally ill can manifest as discrimination against affected people in forms of withdrawal and avoidance (Corrigan and Bink, 2016). As a part of the socialization process, most stereotypes are learned by the individual in the first years of life (Link and Phelan, 2013). During life course, individuals have the chance to reflect on learned stereotypes and prejudices, increase their mental health knowledge and gain their own experiences in contact with affected people (Aronson et al., 2014). Even though stereotypes and stigmatizing attitudes are difficult to change, negative stereotypes can be modified (Weber and Crocker, 1983) and mental health stigma can be reduced (Holmes et al., 1999).
Although mental health stigma of the public is a social burden that must be addressed, research shows that internalized prejudice and stigmatizing attitudes toward oneself have the biggest impact on mental health help-seeking (Eisenberg et al., 2009; Schomerus et al., 2009; Vogel et al., 2013; Schnyder et al., 2017). Self-stigma “is the reduction of an individual’s self-esteem or self-worth caused by the individual self-labeling herself or himself as someone who is socially unacceptable” (Vogel et al., 2006, p. 325). According to the Modified Labeling Theory, negative collective beliefs about people with mental health problems could have a negative impact on the self-esteem of people facing a mental health problem (Link et al., 1987). Personal stigma describes “personal attitudes toward members of a stigmatized group and can find a behavioral expression in the desire for social distance” (Schnyder et al., 2017, p. 261). According to a meta-analysis, personal stigma reduces the willingness to interact with affected people and is negatively associated with help-outreach behavior (Schnyder et al., 2017). However, Jung et al. (2017) showed in a sample of public employees, that self-stigma predicted attitudes toward mental health help-seeking, whereas personal stigma did not.
Mental health stigma is a common phenomenon even among healthcare workers. In contrast to the general public, healthcare workers tend to have a more negative point of view regarding the course of mental disorders, long-term outcomes and the likelihood of discrimination (Jorm et al., 1999; Hugo, 2001; Magliano et al., 2004). This is explained by their increased contact with chronically ill people. Stigmatizing attitudes regarding mental illness of healthcare workers can have a negative impact on their own mental health help-seeking behavior (Ross and Goldner, 2009; Knaak et al., 2017; Søvold et al., 2021) as well as their mental health help-outreach behavior toward affected colleagues (Moll et al., 2015; Knaak et al., 2017). An increased perception of mental health stigma in healthcare comes along with higher self-stigma as affected healthcare workers often attribute their mental illness to personal weakness or character defects (Smith and Hukill, 1996). Based on their professional self-conception on helping others they might feel guilt or shame (Davidson et al., 2018), which discourages affected healthcare workers to seek help from a colleague (Knaak et al., 2017). Further, research shows that personal stigma of healthcare workers also turns against affected colleagues in the workplace (Ross and Goldner, 2009; Knaak et al., 2017). As personal stigma finds expression in the desire for social distance (Link and Phelan, 2001), the help-outreach behavior to affected colleagues can be reduced. Same results can be found for the medical profession (e.g., physicians) (Chew-Graham et al., 2003; Adams et al., 2010; Wallace, 2012).
Prior research on mental health help-seeking mainly examined mental health literacy and mental health stigma separately instead of focusing on the relationship and potential interplay of both in order to predict help-seeking and help-outreach behavior (for an exception see Cheng et al., 2018 and Wang et al., 2019). The scarce research on the interplay of mental health literacy and mental health stigma shows heterogeneous results. Direct effects are reported, such as a lack of knowledge regarding mental health help could increase personal and self-stigma (Jorm et al., 2010; Milin et al., 2016; Morgan et al., 2018; Schomerus et al., 2018). However, Cheng et al. (2018) and Wang et al. (2019) found no interaction between mental health literacy and stigma in the prediction of help-seeking of college and high school students.
Following Cauce et al. (2002), high mental health literacy promotes the recognition and identification of one’s own mental health problem as the first step of the mental health help-seeking model. However, the decision to actually seek help for that problem in the workplace can be reduced by fears of rejection and low self-esteem caused by self-stigma. Since individual mental health literacy may also help to protect from self-stigma, it can make seeking help for a mental health problem more likely. Hence, the second hypothesis to be tested is:
H2: The positive association between mental health literacy and help-seeking intention in the workplace of healthcare workers is mediated by self-stigma.
Along with the previous explanations, it is conceivable that the positive relationship between mental health literacy and help-outreach behavior could be diminished by the presence of personal stigma. More precisely, high mental health literacy promotes the recognition and identification of changes in a colleague’s mental health condition (Cauce et al., 2002), but the decision to actually offer help to a colleague in the workplace can be lowered by the desire for social distance as an expression of personal stigma (Schnyder et al., 2017). Since individual mental health literacy may also help to reduce personal stigma, reaching out to help affected people is more likely. Therefore, it is hypothesized:
H3: The positive association between mental health literacy and help-outreach intention in the workplace of healthcare workers is mediated by personal stigma.
The full research model is displayed in Figure 1.
Materials and Methods
Participants and Procedure
On account of country-specific differences (Ridic et al., 2012; Rafferty et al., 2019), the healthcare setting and the education of healthcare workers in Germany will be briefly outlined. The healthcare system in Germany is divided into outpatient and inpatient care. Inpatient treatment is provided by 1,914 hospitals (Destatis, 2022a). In 2021, Germany’s bed capacity (7.9 hospital beds per 1,000 population) was the highest in Europe (OECD, 2021). Also the number of nurses and physicians for its population is high compared to other EU-countries. Currently 5.7 million people work in healthcare in Germany, the majority is female (75.6%) (Destatis, 2022b). Given the high number of beds, the nurse to bed ratio is among the lowest in the EU (OECD, 2021). Since 1990 the German hospital sector has been restructured and privatized (Schulten, 2006), which led to a reduction of healthcare workers in hospitals. The demographic change is an additional factor that further aggravates the growing demand for care in Germany (Rafferty et al., 2019). Although different reforms were implemented to fight the shortage of skilled health workers (OECD, 2021), Germany is facing a tremendous shortage of healthcare workers just as other countries nowadays (Oulton, 2006; World Health Organization [WHO], 2016; Rafferty et al., 2019).
The debate about the shortage of skilled health workers highlights the need for attracting and training young professionals. The dual vocational training in Germany is a combination of on-the-job training and vocational school. Trainees attend the theoretical training in nursing schools mostly on the hospital campus, while practical training takes place at different hospitals wards. In Germany, the focus of healthcare workers’ training lies on practical work experience. Within the 3 years of apprenticeship, trainees complete 2,500 hours of practical work in hospital, which is more than in most other EU countries (Rafferty et al., 2019). Therefore, healthcare trainees gain work experience early in their careers while sharing the same challenging working conditions as their registered co-workers (Lim et al., 2010; Wazqar et al., 2017; Guo et al., 2018). With the new Nurse Professions Reform Act implemented in 2020, the qualification of healthcare professionals is recognized by other EU states (Rafferty et al., 2019).
In order to test the hypotheses, survey data was collected among trainees of different healthcare professions in six German hospitals from autumn 2018 to spring 2019. The variables of interest were measured separately at two points of measurement to avoid common method bias (Podsakoff et al., 2003) and to strengthen the causal interpretability of the hypothesized model (Maxwell and Cole, 2007).
The first measurement (t1) was carried out as a paper-pencil-questionnaire in the classrooms (Nt1 = 525). The paper-pencil-questionnaire included measures of the independent variable and was distributed by the instructed schoolteachers. Additionally, participants were asked to provide their email addresses in a separate form to contact them for the second measurement. The second measurement (t2) was conducted via an online-questionnaire 2 weeks after t1 (response rate of 21%). The online-questionnaire included measures for the mediator and dependent variables among others. In order to match the data of t1 and t2, a self-generated identification code for participants was used. The final sample consists of participants who filled out both the paper-pencil-questionnaire and the online-questionnaire (Nt2 = 112).
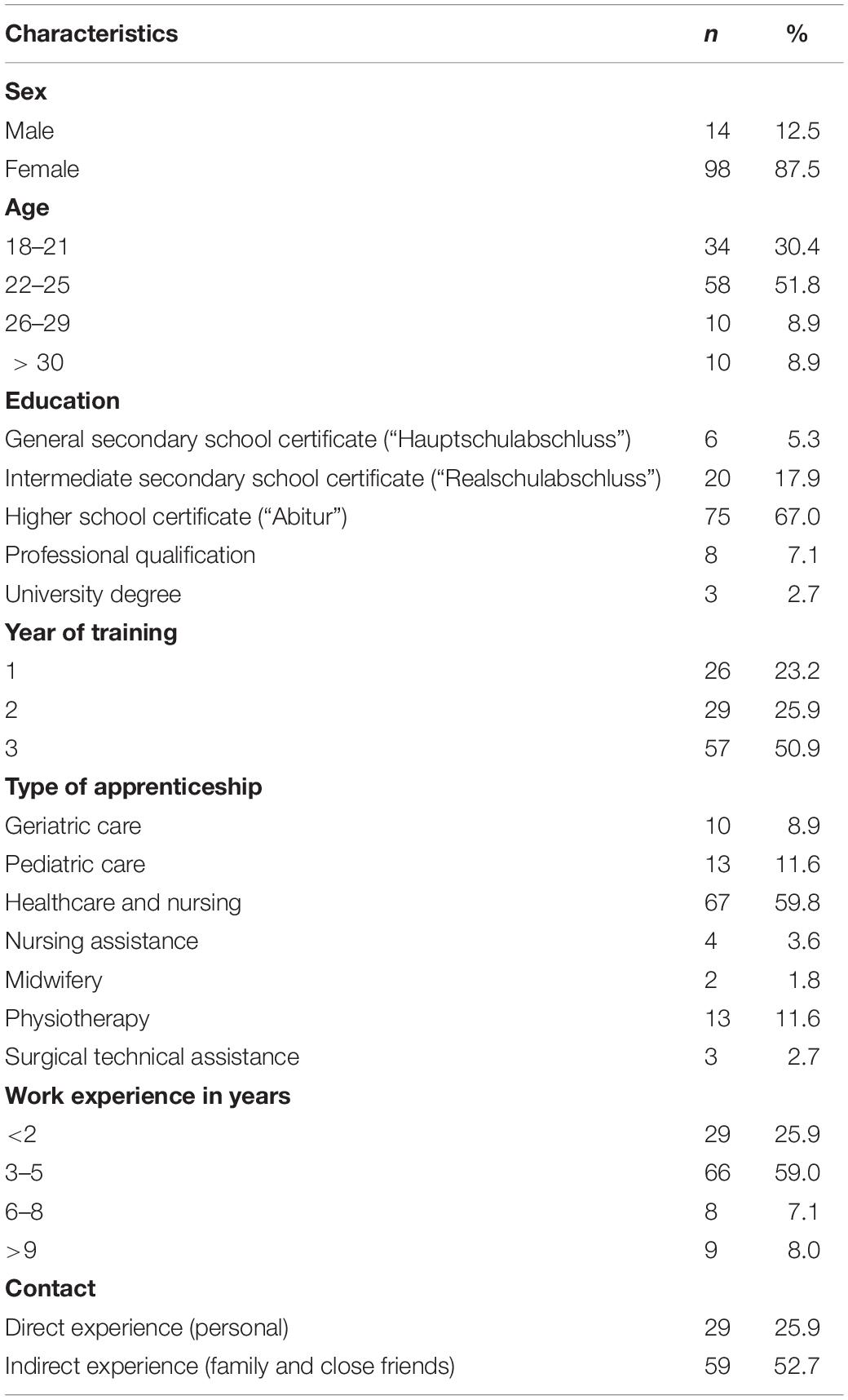
The participants of the final sample were mostly enrolled in healthcare and nursing (59.8%). According to the occupational group studied, the majority of participants were female (12.5% males). The average age was 24.02 years (SD = 6.35). At the time of the online-questionnaire (t2), most participants were in their third and last year of training (50.9%), although 25.9% were in their second year and 23.2% in their first year. The mean of work experience (including apprenticeship) was 4.19 years (SD = 5.27). In total, most of the sample hold a higher school certificate (67%, German “Abitur”), although 17.9% an intermediate secondary school certificate (German “Realschulabschluss”), 5.3% a general secondary school certificate (German “Hauptschulabschluss”), 7.1% completed another vocational training and 2.7% have a university degree. More than 25% of the participants reported direct experience with mental health problems and approximately 53% indicate indirect experience though family and close friends. See Table 1 for detailed sample characteristics.
Throughout the study, the ethical standards of the American Psychological Association (2022) were followed and a written informed consent was given. As an incentive, four online shopping vouchers of 25 euro each were raffled among the participants of the second measurement.
Measurements
Workplace Mental Health Literacy
In this study, the German Version of the mental health literacy tool for the workplace (MHL-W-G, Wulf and Ruhle, 2020) was used to measure workplace mental health literacy (t1). MHL-W-G is a subjective, vignette-based tool with 16 items measuring the perceived mental health competence in the work context. Rather than measuring the correct classification of a mental disorder (Wei et al., 2015), workplace mental health literacy refers to the self-assessment of individual mental health competence in the working context (Moll et al., 2017). Therefore, the four vignettes describe job-related situations with colleagues who struggle with a potential mental health problem. After having read the vignettes participants were asked to rate their competence on a five-point Likert scale (1 = strongly disagree to 5 = strongly agree) regarding (a) the assessment of the described situation, (b) risk factors and prevention, (c) handling the situation, and (d) helpful sources and interventions (Moll et al., 2017). Higher sum scores indicate higher levels of mental health literacy. Cronbach’s alpha was 0.89.
Self-Stigma
To measure self-stigma, the German translation by Drabek (2010) of the Self Stigma of Seeking Psychological Help Scale (SSOSH) (Vogel et al., 2006) was used (t2). Participants were asked to rate their attitudes toward psychological help-seeking if needed with 10 items (sample item: “I would feel inadequate if I went to a therapist for psychological help.”) on a five-point Likert scale (1 = strongly disagree to 5 = strongly agree). Five items were reverse coded. Higher sum scores indicate higher levels of self-stigma. Cronbach’s alpha was 0.84.
Personal Stigma
To measure personal stigma, the German translation of the Social Distance Scale (SDS) (Link et al., 1987) by Angermeyer and Matschinger (1997) was used (t1), which consists of seven items. Good psychometric properties have been reported for this scale, capturing attitudes toward the mentally ill (Angermeyer and Matschinger, 2003). Participants were asked, if they would accept the person described in the situation rated on a five-point Likert scale (1 = in any case to 5 = not at all; sample item: “To what extent would you be okay with having someone with a mental health problem as a neighbor?”). Higher sum scores indicate higher levels of personal stigma. Cronbach’s alpha was 0.87.
Help-Seeking Intention
The help-seeking intention for a mental health problem from different sources was measured (t2) with the German translation of the General Help-Seeking Questionnaire (GHSQ) (Wilson et al., 2005) by Hanschmidt (2018). As suggested by the authors of the GHSQ, help sources were modified for the purpose of the study (Wilson et al., 2005). Participants were asked to rate the likelihood of seeking help from different sources in the private environment, workplace and professional services on a seven-point Likert scale (1 = extremely unlikely to 7 = extremely likely, 8 = does not apply). Cronbach’s alpha in this sample was 0.71. Beside the GHSQ, one self-developed item measured the overall workplace help-seeking intention when facing a mental health issue on a seven-point Likert scale (1 = extremely unlikely to 7 = extremely likely; sample item: “to what extent would you seek help in the working context in case of a personal or mental health problem?”).
Help-Outreach Intention
The measurement of help-outreach intention was based on a modified behavior-list of the mental health first aid (MHFA) training (Jorm et al., 2010) described by Moll et al. (2015). For the purpose of this study, the English items were translated into German and back-translated into English by two independent persons. The 13 items (t2) cover general (e.g., “time to listen”) as well as work context-specific help-outreach behaviors (e.g., “offer support with job task fulfillment”). Participants were asked to rate the likelihood of performing each behavior on a seven-point Likert scale (1 = extremely unlikely to 7 = extremely likely). Cronbach’s alpha for this study was 0.82. Additionally, one self-developed item measured the overall workplace help-outreach intention on a seven-point Likert scale (1 = extremely unlikely to 7 = extremely likely), “to what extent would you offer help regarding a personal or mental health problem in the work context (e.g., an affected colleague)?”
Control Variables
Demographic data were gathered in both times of measurement (gender, age, education, healthcare profession, year of training, and work experience). Also, the contact with people facing mental health problems was measured in t1, as it can shape attitudes toward them (Stadler, 2010). Lacking a standardized measure to operationalize contact to mentally ill people, participants were asked to rate their direct (personal) and indirect (family and close friends) experience with mental health problems on a dichotomy scale (1 = yes and 2 = no).
Statistical Analyses
For data preparation and the calculation of frequencies, means, standard deviations, Cronbach’s α, correlations, distribution characteristics and t-tests, IBM SPSS Statistics 25 was used. Factor analyses for each construct were tested with IBM SPSS AMOS 25, as, due to the small sample size, it was not possible to examine all variables at once.
Prior of testing hypotheses, two analysis steps were conducted: First, Pearson correlations of the variables were calculated. Second, factor structure of main study variables was validated. In order to test the proposed research model, SEM was applied and alternative SEM models were compared to test the mediation hypotheses (Anderson and Gerbing, 1988). The assessment of the model fit was based on χ2 difference tests and fit indices including CFI, GFI, TLI, RMSEA, AIC, and BIC (West et al., 2012). Adequate model fit is described by Schermelleh-Engel et al. (2003) with: CFI > 0.95, GFI > 0.90, TLI > 0.95, RMSEA < 0.08 and the lowest values for BIC and AIC.
Due to the small sample size, it was not possible to include all measures as latent variables. Thus, the mean sum scores for self-stigma and personal stigma were used to test and estimate the proposed research model. Referring to Wulf and Ruhle (2020), the second-order structure of workplace mental health literacy was added to the model as latent variable. Regarding the robustness of the results it can be reported, that there are only minor changes in the results when using latent variables for the mediator variable and a mean sum score for workplace mental health literacy.
Results
Responder Analysis
In order to control for non-response bias in the second measurement, socio-demographic and occupational characteristics of participants reported at t1 were compared by independent samples t-tests (for continuous variables) and chi-square tests (for categorical variables). No statistically significant differences were found according to age, education, healthcare profession, work experience, contact (direct/indirect), and workplace mental health literacy. However, participants who took part in the paper-pencil and online-questionnaire are in higher years of training (M = 2.30, SD = 0.86, n = 112) than trainees (M = 1.98, SD = 0.82, n = 525) who only took part in the paper-pencil questionnaire in the classroom, t(525) = −3.62, p < 0.000. The effect size of d = 0.44 was calculated referring to Lenhard and Lenhard (2016) and can be described as medium according to Cohen (1988, p. 25–26). Also, less men took part in t2 than women (t1 and t2: M = 0.88, n = 112, only t1: M = 0.79, n = 525), χ2 = 3.958, p = 0.047. The effect size is small with Cramer’s V w = 0.087 (Cohen, 1988). To sum it up, the used sample seems not to be inflated by non-response bias as the means of the independent variable (workplace mental health literacy) are statistically equal between participants and non-participants of t2.
Descriptive Statistics
Workplace Mental Health Literacy
Participants’ answers to the workplace mental health literacy scale ranged from 36 to 80 with a mean of 56 (SD = 9.47, n = 112). In comparison with other study results the participants of this study had on average a slightly higher workplace mental health literacy value: Wulf and Ruhle (2020) reported for a working convenience sample M = 54 (SD = 9.74, n = 317). Moll et al. (2017) reported M = 52 (SD = 12.40, n = 192) before and M = 66 (SD = 8.77, n = 192) after a mental health literacy-related intervention for experienced healthcare workers.
Help-Seeking Intention
Participants indicated that they would most likely seek help from someone in the private environment or contact a professional service for help (for full list see Supplementary Table 1). In the working context, the source of first choice were colleagues. The likelihood of not seeking any help for a mental health problem was rather high (M = 5.31, SD = 1.73, n = 90).
Help-Outreach Intention
Based on a list of different behaviors participants rated their intention to provide help to a colleague with a mental health problem (for full list see Supplementary Table 1). Participants would most likely spend time listening to a colleague’s problem. Participants were less likely to report talking to him/her about possible suicidal thoughts. Further the likelihood of not offering help to an affected colleague was rather low (M = 1.37, SD = 0.92, n = 112). Overall, participants were more likely to offer help to their colleagues than to ask for help themselves.
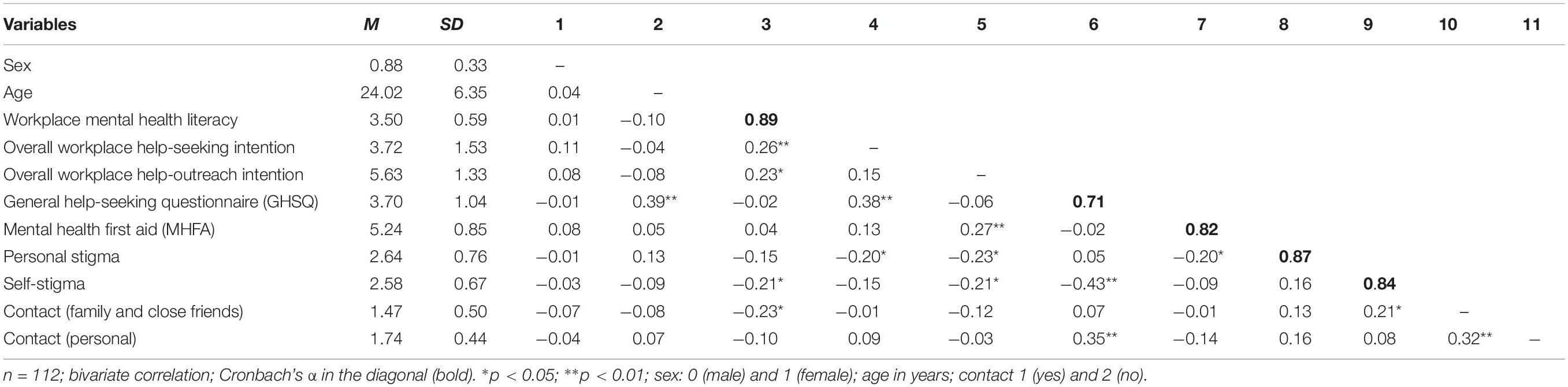
Correlations Between Variables
Table 2 shows the means, standard deviations and correlations for all relevant variables of the two measurements. The data refers to the participants who took part in both questionnaires. Both overall workplace help-seeking intention and outreach-behavior intention measures showed that the corresponding scales of GHSQ and MHFA were positively and significantly related to them. As expected, workplace mental health literacy also correlated positively and significantly with both overall intention measures. As anticipated, the two stigma measures were not correlated with each other, indicating distinct constructs. Further, self-stigma, and personal stigma were negatively correlated with workplace mental health literacy, but only the correlation with self-stigma was statistically significant. Surprisingly, self-stigma was only negatively and significantly associated with overall workplace help-outreach intention, whereas personal stigma was negatively and significantly correlated with overall workplace help-seeking intention and overall workplace help-outreach intention.
Factor Analysis
Prior to hypothesis testing, CFA was performed with main study variables (MHL-W-G, SSOSH, SDS, GHSQ, and MHFA) in order to test the factorial structure of the constructs (Byrne, 2016). For the independent variable workplace mental health literacy, the second order structure as described by Wulf and Ruhle (2020) could be replicated in AMOS with an adequate model fit: χ2(76, n = 112) = 99.393, p = 0.037, CFI = 0.970, GFI = 0.901, TLI = 0.953, RMSEA = 0.053 [90% confidence interval (CI):0.014,0.079]. However, both CFA of the dependent variables GHSQ and MHFA showed inadequate model fits. For this reason, in the next analysis step the one-item measures, determining overall workplace help-seeking intention and help-outreach intention, were used as dependent variables instead of the whole scale of GHSQ and MHFA.
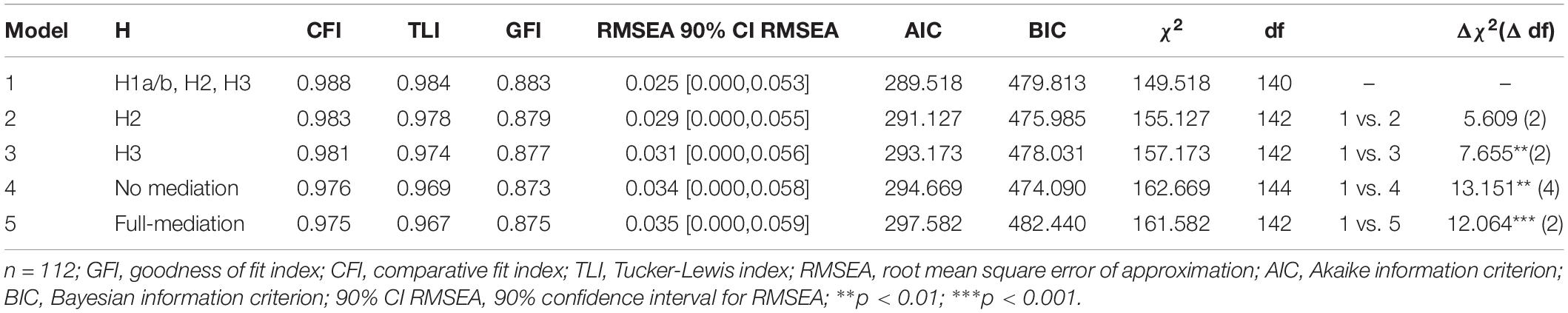
Path Model and Hypothesis Testing
Table 3 shows the test of different models, including all measures as noted above: In comparison to alternative models, the measurement model 1 indicates good model fit: χ2(140, n = 112) = 149.518, p = 0.276, CFI = 0.988, TLI = 0.984, GFI = 0.883, AIC = 289.518, BIC = 479.813, RMSEA = 0.025 [0.000,0.053]. Model 1 explained R2 = 0.09 of variance in overall workplace help-seeking intention and R2 = 0.11 of variance in overall workplace help-outreach intention. The standard coefficients of the model displayed in Figure 2 show that workplace mental health literacy increases the overall workplace help-seeking intention and help-outreach intention significantly. These results provide support for hypothesis H1a and H1b. Further, it indicates that workplace mental health literacy decreases self-stigma and that personal stigma decreases overall workplace help-outreach intention. In the final model, further variables of interest (age, education, job tenure, healthcare profession, and personal experience with mental health problems) were included but showed no effect. Therefore, those variables were excluded in the described analyses.
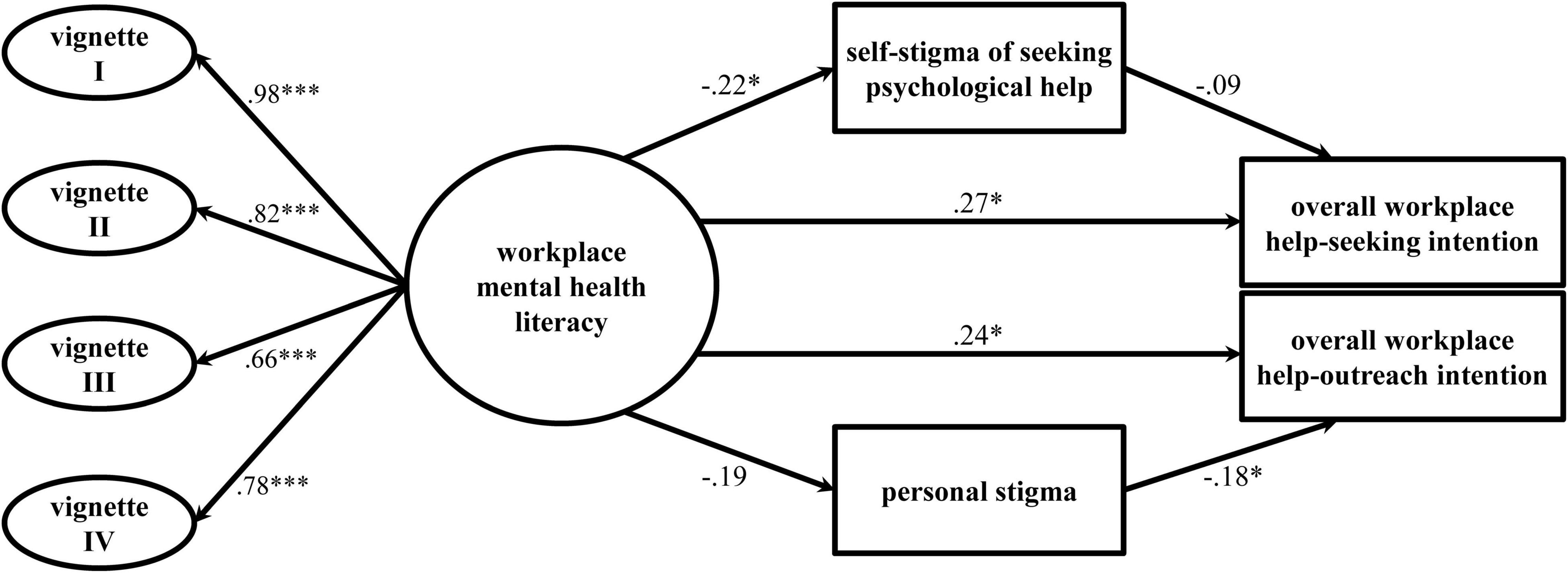
Figure 2. Workplace mental health literacy as predictor of overall workplace help-seeking intention and help-outreach intention. n = 112, path model with standardized beta coefficients and without error terms. *p< 0.05; **p < 0.01; ***p< 0.001.
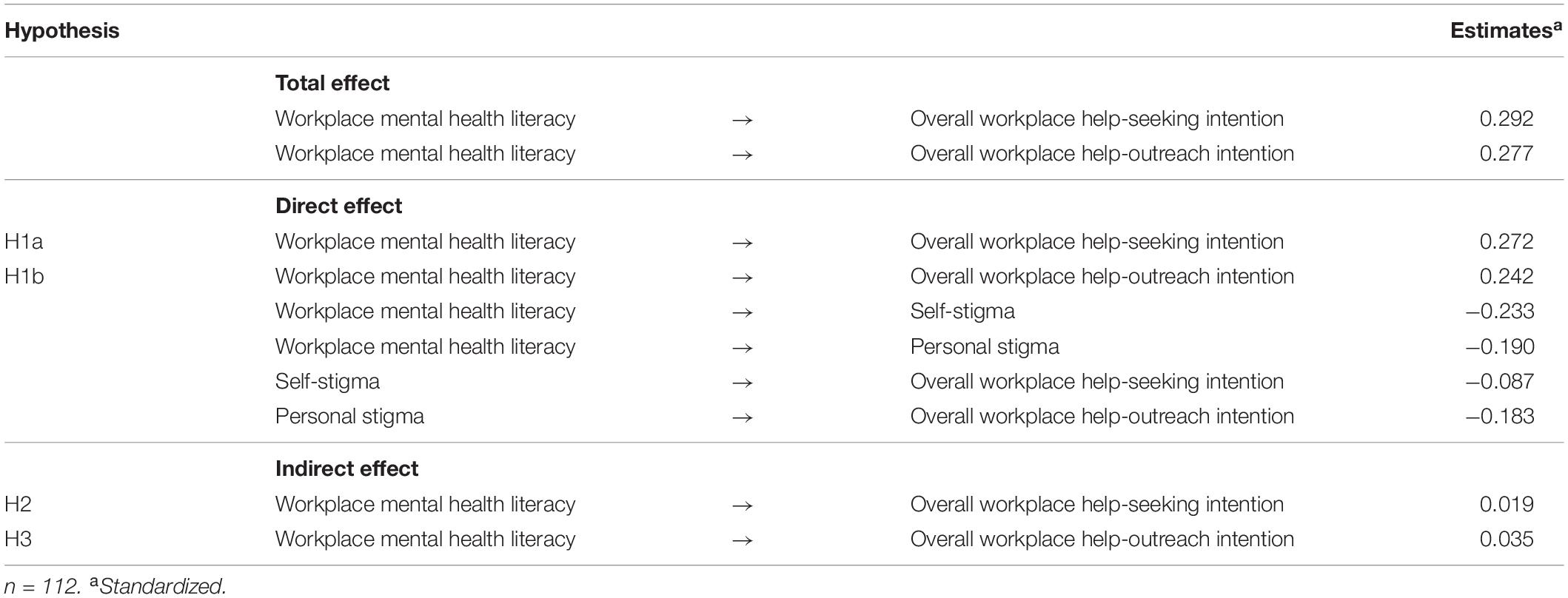
Additionally, the mediation hypotheses 2 and 3 were tested via the comparison of the standardized total effect with the standardized indirect effect of the dependent variables (see Table 4). The standardized indirect effects due to self-stigma and personal stigma were almost equal to the standardized total effects of overall workplace help-seeking intention and overall workplace help-outreach intention. Thus, hypotheses 2 and 3 can be rejected.
Discussion
Theoretical Implications
The aim of the study was to examine the role of mental health literacy and stigma on help-seeking and help-outreach intentions of healthcare workers in the workplace. Study findings indicate that the mental health help-seeking and help-outreach intentions of healthcare workers in the working context increases with mental health literacy. Therefore, the first hypothesis was confirmed, which is in line with Moll et al. (2015, 2018). In contrast to mental health help-seeking, offering support for a mental health problem has hardly been addressed in previous studies. This especially applies to the working context of healthcare workers. Hence, study results contribute to a broader understanding of the workplace as a relevant setting for early prevention of mental health problems. With regard to the healthcare profession, the young employees of the present study indicated higher mean scores for offering help to an affected colleague than for seeking help at the workplace themselves in case of a mental health problem. This result can be compared to findings of private networks, which are known to positively influence the individual’s decision to seek help for a mental problem (Cusack et al., 2004; Vogel et al., 2007a). A review revealed that a pivotal event typically initiates the help-seeking process of healthcare workers for severe substance use disorders (Kunyk et al., 2016). As self-reporting for most addicted individuals is uncommon, being addressed by colleagues is more likely to lead healthcare workers into treatment (Kunyk et al., 2016). Beside this, people with a mental health problem tend to have limited sources in their private network to ask for help, therefore, their social network in the working context may sometimes be the only access point to social support (Simmons, 1994). For this reason, the present study emphasizes the importance of colleagues as potential sources for help in the workplace. Affected individuals have the opportunity to receive initial support, for example, by colleagues who listen and provide emotional encouragement or in terms of support in job task fulfillment.
In general, participants reported high mean scores of not seeking help in case of a mental health problem. This is in line with previous studies, which showed that most people do not seek help or do so rather late (Wang et al., 2007; Rickwood et al., 2012). Regarding the different sources of help, participants indicated that they would prefer seeking help in the private environment or contact a professional source rather than asking for help in the working context. Recently, Hastuti and Timming (2021) come to a similar result in their interdisciplinary review, which focusses on mental illness disclosure in the workplace across all occupations. Revealing mental health problems at work can have negative consequences on chances of getting hired, career prospects, job security and therefore prevent seeking help (Wheat et al., 2010; Brohan et al., 2012; Hastuti and Timming, 2021). This especially applies for occupations such as healthcare profession with strict occupational regulations (Hastuti and Timming, 2021). In fact, nursing and medical staff are refusing to seek help for a mental problem out of fear of consequences regarding receiving or renewing their license (Chew-Graham et al., 2003; Dyrbye et al., 2017b; Brower, 2021; Weston and Nordberg, 2021). According to national legislation, these concerns are justified, as the disclosure of mental health problems in healthcare may result in restrictions, obligatory surveillance and evaluation of mental health status and (temporary) loss of license (Hudson et al., 2021). For young employees the situation is even more complicated, as they need to apply for a permanent job at the end of their apprenticeship. In Germany, trainees are often given the chance to be taken on by the company providing the apprenticeship directly after graduation (Schönfeld et al., 2020). Therefore, young employees will think twice about disclosing mental health problems in order not to affect future job opportunities negatively. This may also help to explain why the participants in the present study indicate that they rather aim to seek help from colleagues than from the employer side.
Further, participants indicate that they would less likely approach institutions like the employee representation and labor union, which are less favored sources for seeking mental help. That could be explained by the fact, that at the beginning of the professional career young employees hardly know representatives of these institutions, which makes it more difficult to ask for help than in the immediate working environment. Additionally, the distant relationship with those institutions is associated with higher expectations of stigmatization and represent the left hand distribution of the u-shaped relationship between stigma and familiarity (Corrigan and Nieweglowski, 2019). In summary, colleagues seem to be a potential source of help for affected people, as their relationships tend to not be as close as those with family members but also not as distant as those with institutions in the working context and therefore less mental health stigmatization can be expected.
Regarding the second and third hypothesis, no mediating effect of either self-stigma or personal stigma on the association between mental health literacy and help-seeking intention in the workplace could be confirmed. These results could be explained with regard to other types of stigma, e.g., the perceived stigma from others (Pedersen and Paves, 2014; Jennings et al., 2015; Schnyder et al., 2017), which could also have an impact on the relationship between mental health literacy and help-seeking and help-outreach behavior in the workplace. For personal stigma, social distance measures are widely used in the help-seeking context (Jung et al., 2017), but as research regarding help-outreach behavior is scarce, it is possible that other stigma types, which were not included in this study, could also play a role. Regarding self-stigma, prior studies reported that self-stigma of seeking psychological help is of greater importance in the mental health help-seeking process than other stigma types (Vogel et al., 2006, 2007b; Cheng et al., 2018; Wang et al., 2019). Against this background, one possible explanation regarding the missing association between self-stigma and overall help-seeking intention refers to the small sample size and statistical power. Complex models, like the present model, require larger sample sizes (>200) in order to be able to test efficiently for indirect effects on the generally accepted probability level of 0.05% (Hoyle and Gottfredson, 2015).
Even though no mediating effects of stigma could be found in this study, direct effects are reported. There was a negative direct effect of personal stigma on overall help-outreach intention, thus help-outreach intentions of healthcare workers decrease with personal stigma in the working context. This result is in line with prior research: In a vignette study, Jorm et al. (2005) showed that adults over 18 years, who are high in personal stigma, report less mental health first aid responses (e.g., listening, talking and supporting). In contrast, Mason et al. (2015) found only small negative effects of personal stigma on mental health first aid intentions in high school students with an average age of 16. In this study, personal stigma was identified as an important barrier to help-outreach intention in the workplace of young employees, although the direct effect of personal stigma was not as strong as the direct effect of mental health literacy on help-outreach intention in the workplace.
From previous studies, it is known that young employees are particularly vulnerable for mental health problems (Kessler et al., 2005; Rickwood et al., 2005; Patel et al., 2007) as first work experience is an important life event and socialization process, which can be extremely stressful. This especially applies to young employees in jobs as physically and emotionally demanding as the healthcare profession (Frögéli et al., 2019). For example, younger age of nurses was found to be a predictor of professional burnout in a meta-analysis (Gómez-Urquiza et al., 2017). At the same time, as participants of the present study recently started to work, their contact with chronically mentally ill patients has been limited and as a result stigmatizing attitudes may not be as severe as in employees with more work experiences (Jorm et al., 1999; Hugo, 2001). Besides this, it is plausible to assume, that especially young employees hold a high level of professional self-conception in their first working years, in the sense of helping and caring for those in need. Therefore, the mental health help-seeking process of young employees may be less dependent on their (lower) mental health stigma than on their newly acquired knowledge. This assumption can be supported by the fact that the participants of the present study reported a medium level of self-stigma and personal stigma, contrasting the generally high level of stigma in healthcare found in other studies (Jorm et al., 1999; Hugo, 2001). This is in line with DeBord et al. (2019), who found low levels of self-stigma of seeking mental healthcare for a psychological problem in a sample of nursing students (18–29 years).
Practical Implications
The findings of the present study offer several implications for current practice. Firstly, the main implications relate to mental health literacy building. In line with World Health Organization [WHO]’s (2019) call for action, mental health education is key to enable employees to address the topic of mental health at the workplace. As study results indicate colleagues as preferred sources of help in the workplace, training content should cover what to say when noticing that a colleague is in need, as well as giving an overview of local service offers and professional services. The MHFA training serves all of the points mentioned and is already implemented in over 24 countries (MHFA, 2022). A recent review showed small to moderate effects of the MHFA training on knowledge improvement, the recognition of mental health problems and help-outreach intentions (Morgan et al., 2018). A MHFA program was also recently launched in Germany (Zentralinstitut für Seelische Gesundheit Mannheim, 2022).
Secondly, it can be noted, that even though the curriculum of healthcare workers regularly includes knowledge about the development and treatment of mental health disorders, it is maybe not applicable to the workplace of healthcare workers. Combined with the fact that experienced healthcare workers generally tend to be high in mental health stigma, interventions aiming to increase mental health literacy could be a promising way to improve the mental health help-seeking and help-outreach behavior of a strongly exposed occupational group. Therefore, trainings in healthcare should not only focus on patients’ mental health, but also on professionals’ mental health conditions and those of colleagues. Given the early onset of most mental disorders and the provided evidence of the present study, the mental health education of health professionals should preferably start early in working life. In Germany, young employees learn by example of experienced healthcare workers in the practical part of the vocational training. This also applies for handling mental health problems in the working context. Thus, specific trainings for registered nurses are equally relevant.
Thirdly, with the first application of the MHL-W-G in a German sample of healthcare workers, the study supports the development of a robust, multi-lingual tool measuring subjective mental health literacy (Wulf and Ruhle, 2020). Therefore, the vignette-based questionnaire might be of use in organizations for measuring the need for mental health education and the success of trainings in the workplace. Further, the present study provides the opportunity to compare the results across countries as so far, the majority of studies regarding healthcare workers were conducted in Canada and United States (e.g., Moll et al., 2017, 2018; DeBord et al., 2019).
Last but not least, the mental health of healthcare workers should receive special attention due to the particularly high job demands in the COVID-19 pandemic. Even though this study refers to the situation of healthcare workers before the pandemic, the relevance of social support in the workplace provided by colleagues and supervisors becomes even more evident in the current emergency situation (Greenberg and Tracy, 2020; Schug et al., 2021). Hence, colleagues and supervisors should be particularly sensitive to psychological distress and be aware of early warning signs of mental health problems in themselves and their co-workers. Given the pandemic-related limitations of professional services for people with mental health problems and the decrease in private contacts due to, for example, imposed contact restrictions, the role of colleagues and supervisors in the mental health help-seeking process might become even more relevant.
Limitations and Future Research
The participants in this study were a convenience samples of trainees of different healthcare professions. Therefore, these sample may not be representative of healthcare workers in general. The young employees were mostly at the beginning of their professional careers, even if they already had work experience in the hospital sector and the majority had already had direct or indirect experiences with mental health problems.
The data of the present study was collected on two measurement points in order to avoid common method bias (Podsakoff et al., 2003) and to strengthen the causal interpretability of the tested model (Maxwell and Cole, 2007). However, a common limitation of plural measurements is a high drop-out rate (Bortz and Döring, 2016), which was also a limitation in the present study. One explanation for the high drop-out rate is that the paper-pencil-questionnaire (t1) was carried out during working hours, while the online-questionnaire (t2) was conducted outside of working hours. Also, the loss of participants can possibly be explained by the relatively small incentive (raffled vouchers).
Another limitation concerns the inadequate model fits of the measures of workplace help-seeking intention (GHSQ; Wilson et al., 2005; Hanschmidt, 2018) and help-outreach intention (MHFA; Jorm et al., 2010; Moll et al., 2015). An explanation for these findings lies in the adaption of the items for the purpose of the present study without proper validation before application. As a result, both scales showed the lowest reliability of all used scales. Accordingly, the one-item measure of overall help-seeking and overall help-outreach intentions were used in the SEM. One-items measures for overall attitudes toward help-seeking for a mental health problem have already been used in previous studies (Britt et al., 2011; Jennings et al., 2015). Nevertheless, a need for validated scales in the German language to measure workplace help-seeking intention and help-outreach intention can be identified.
Even though in this study female participants reported on average the same mental health literacy value as male participants, future studies should examine possible gender differences. This relates to previous studies, which show that women tend to recognize mental illness better than men (Pescosolido et al., 2008; Wulf and Ruhle, 2020). Additionally, women are more willing to use professional help for a mental problem than men (Rüsch et al., 2014; Cheng et al., 2018). Therefore, more empirical research focusing on gender differences in the evaluation of mental health problems, as well as help-seeking and help-outreach tendencies is needed.
Conclusion
The present study reduces the lack of empirical information regarding mental health help-seeking and help-outreach in the workplace, which was noted at the beginning. As most studies focus on social contacts in the private environment and formal sources (Rossetto et al., 2016; Jung et al., 2017; Schnyder et al., 2017), the study contributes to the relevance of social contacts in the working context as potential gatekeepers to professional mental health support. Further, the study provides important insights into how mental health help-seeking and help-outreach intentions at the workplace are affected by mental health literacy and into the role of personal and self-stigma in healthcare profession. The results are of particular importance against the increased need for healthcare workers and the fact of the rising prevalence of mental diseases in this group.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the author, without undue reservation.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the Local Legislation and Institutional Requirements. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
IW was responsible for the conception and design of the study as well as the implementation of the research, performed the statistical analysis, and drafted the manuscript.
Funding
IW received funding for the open access publication fees from the Open Access Publication Fund of the Heinrich Heine University Düsseldorf.
Conflict of Interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
IW grateful to Sascha A. Ruhle, Mathias Diebig, Marvin Reuter, and Miriam Engels for their expertise and assistance throughout this study, and feedback regarding the manuscript.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/feduc.2022.856458/full#supplementary-material
References
Adams, E. F. M., Lee, A. J., Pritchard, C. W., and White, R. J. E. (2010). What stops us from healing the healers: a survey of help-seeking behaviour, stigmatisation and depression within the medical profession. Int. J. Soc. Psychiatry 56, 359–370. doi: 10.1177/0020764008099123
Aiken, L. H., Sermeus, W., van den Heede, K., Sloane, D. M., Busse, R., McKee, M., et al. (2012). Patient safety, satisfaction, and quality of hospital care. Cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ Clin. Res. 344, 1–14. doi: 10.1136/bmj.e1717
American Psychological Association (2022). Ethical Principles of Psychologists and Code of Conduct. Available online at: https://www.apa.org/ethics/code (accessed January 03, 2022).
Anderson, J. C., and Gerbing, D. W. (1988). Structural equation modeling in practice. A review and recommended two-step approach. Psychol. Bull. 103, 411–423. doi: 10.1037/0033-2909.103.3.411
Ando, S., Nishida, A., Usami, S., Koike, S., Yamasaki, S., Kanata, S., et al. (2018). Help-seeking intention for depression in early adolescents: associated factors and sex differences. J. Affect. Disord. 238, 359–365. doi: 10.1016/j.jad.2018.05.077
Angermeyer, M. C., and Matschinger, H. (1997). Social distance towards the mentally ill: results of representative surveys in the Federal Republic of Germany. Psychol. Med. 27, 131–141. doi: 10.1017/S0033291796004205
Angermeyer, M. C., and Matschinger, H. (2003). The stigma of mental illness. Effects of labelling on public attitudes towards people with mental disorder. Acta Psychiatr. Scand. 108, 304–309. doi: 10.1034/j.1600-0447.2003.00150.x
Angermeyer, M. C., Matschinger, H., and Schomerus, G. (2013). Attitudes towards psychiatric treatment and people with mental illness: changes over two decades. Br. J. Psychiatry 203, 146–151. doi: 10.1192/bjp.bp.112.122978
Aronson, E., Wilson, T. D., and Akert, R. M. (2014). Sozialpsychologie, 8th Edn. Hallbergmoos: Pearson.
Barello, S., Palamenghi, L., and Graffigna, G. (2020). Stressors and resources for healthcare professionals during the covid-19 pandemic: lesson learned from Italy. Front. Psychol. 11:2179. doi: 10.3389/fpsyg.2020.02179
Benuto, L. T., Casas, J., Gonzalez, F., and Newlands, R. (2020). The behavioral model of health: education, behavioral health factors, and stigma as predictors of help-seeking attitudes. Commun. Ment. Health J. 56, 1275–1283. doi: 10.1007/s10597-020-00601-y
Benzinger, P., Kuru, S., Keilhauer, A., Hoch, J., Prestel, P., Bauer, J. M., et al. (2021). Psychosoziale auswirkungen der pandemie auf pflegekräfte und bewohner von pflegeheimen sowie deren angehörige – ein systematisches review. Z. Gerontol. Geriatr. 54, 141–145. doi: 10.1007/s00391-021-01859-x
Bonabi, H., Müller, M., Ajdacic-Gross, V., Eisele, J., Rodgers, S., Seifritz, E., et al. (2016). Mental health literacy, attitudes to help seeking, and perceived need as predictors of mental health service use. A Longitudinal Study. J. Nerv. Ment. Dis. 204, 321–324. doi: 10.1097/NMD.0000000000000488
Bortz, J., and Döring, N. (2016). Forschungsmethoden und Evaluation für Human-und Sozialwissenschaftler. Limitierte Sonderausgabe, 5th Edn. Berlin: Springer.
Bourget, B., and Chenier, R. (2007). Mental Health Literacy in Canada: Phase One Draft Report Mental Health Literacy Project. Canadian Alliance on Mental Illness and Mental Health. Available online at: http://en.copian.ca/library/research/mhl/cover.htm (accessed January 03, 2022).
Britt, T. W., Bennett, E. A., Crabtree, M., Haugh, C., Oliver, K., McFadden, A., et al. (2011). The theory of planned behaviour and reserve component veteran treatment seeking. Military Psychol. 23, 82–96. doi: 10.1080/08995605.2011.534417
Brohan, E., Henderson, C., Wheat, K., Malcolm, E., Clement, S., Barley, E. A., et al. (2012). Systematic review of beliefs, behaviours and influencing factors associated with disclosure of a mental health problem in the workplace. BMC Psychiatry 12:11. doi: 10.1186/1471-244X-12-11
Brower, K. J. (2021). Professional stigma of mental health issues: physicians are both the cause and solution. Acad. Med. J. Assoc. Am. Med. Colleges 96, 635–640. doi: 10.1097/ACM.0000000000003998
Byrne, B. M. (2016). Structural Equation Modeling With AMOS: Basic Concepts, Applications, and Programming, 3. Edn. New York, NY: Routledge.
Cauce, A. M., Domenech-Rodríguez, M., Paradise, M., Cochran, B. N., Shea, J. M., Srebnik, D., et al. (2002). Cultural and contextual influences in mental health help seeking: a focus on ethnic minority youth. J. Consult. Clin. Psychol. 70, 44–55. doi: 10.1037/0022-006X.70.1.44
Cheng, H., Wang, C., McDermott, R. C., Kridel, M., and Rislin, J. L. (2018). Self-stigma, mental health literacy, and attitudes toward seeking psychological help. J. Counsel. Dev. 96, 64–74. doi: 10.1002/jcad.12178
Chew-Graham, C. A., Rogers, A., and Yassin, N. (2003). ‘I wouldn’t want it on my CV or their records’: medical students’ experiences of help-seeking for mental health problems. Med. Educ. 37, 873–880. doi: 10.1046/j.1365-2923.2003.01627.x
Cordoba, E. L. (2021). Well-being and mental health of healthcare workers before, during, and after COVID-19. Salud Ment. 44, 211–214. doi: 10.17711/sm.0185-3325.2021.027
Cornally, N., and McCarthy, G. (2011). Help-seeking behaviour. A concept analysis. Int. J. Nurs. Pract. 17, 280–288. doi: 10.1111/j.1440-172X.2011.01936.x
Corrigan, P. W. (2000). Mental health stigma as social attribution: implications for research methods and attitude change. Clin. Psychol. Sci. Pract. 7, 48–67. doi: 10.1093/clipsy.7.1.48
Corrigan, P. W. (2004). How stigma interferes with mental health care. Am. Psychol. 59, 614–625. doi: 10.1037/0003-066X.59.7.614
Corrigan, P. W., and Bink, A. B. (2016). The stigma of mental illness. Encyclopedia Ment. Health 2016, 230–234.
Corrigan, P. W., and Nieweglowski, K. (2019). How does familiarity impact the stigma of mental illness? Clin. Psychol. Rev. 70, 40–50. doi: 10.1016/j.cpr.2019.02.001
Corrigan, P. W., River, L. P., Lundin, R. K., Penn, D. L., Uphoff-Wasowski, K., Campion, J., et al. (2001). Three strategies for changing attributions about severe mental illness. Schizophr. Bull. 27, 187–195. doi: 10.1093/oxfordjournals.schbul.a006865
Cusack, J., Deane, F. P., Wilson, C. J., and Ciarrochi, J. (2004). Who influence men to go to therapy? Reports from men attending psychological services. Int. J. Adv. Counsel. 26, 271–283. doi: 10.1023/b:adco.0000035530.44111.a8
Davidson, J. E., Mendis, J., Stuck, A. R., DeMichele, G., and Zisook, S. (2018). Nurse Suicide. Breaking the Silence. Available online at: https://nam.edu/nurse-suicide-breaking-the-silence/ (accessed January 03, 2022).
DeBord, L. F., Branstetter, M. L., and Smith, L. S. (2019). Working nursing students willing to seek psychological services. Psychiatr. Q. 90, 293–301. doi: 10.1007/s11126-018-9622-3
Destatis (2022a). Hospitals in Germany. Available online at: https://www.destatis.de/EN/Themes/Society-Environment/Health/Hospitals/_node.html;jsessionid=005ABDC44A6B0D237CDAF3A52F77990D.internet8712 (accessed February 16, 2022).
Destatis (2022b). Health Personnel. Available online at: https://www.destatis.de/EN/Themes/Society-Environment/Health/Health-Personnel/_node.html (accessed February 18, 2022)
Drabek, A. (2010). Determinanten Der Inanspruchnahme Sozialer Sowie Professioneller Psychologischer Unterstützung von Justizwachebeamten im Österreichischen Strafvollzug. Vienna: Universität Wien.
Dyrbye, L. N., Shanafelt, T. D., Sinsky, C. A., Cipriano, P. F., Bhatt, J., Ommaya, A., et al. (2017a). Burnout Among Health Care Professionals. A Call to Explore and Address this Underrecognized Threat to Safe, High-Quality Care. Available online at: https://nam.edu/burnout-among-health-care-professionals-a-call-to-explore-and-address-this-underrecognized-threat-to-safe-high-quality-care/ (accessed January 03, 2022).
Dyrbye, L. N., West, C. P., Sinsky, C. A., Goeders, L. E., Satele, D. V., and Shanafelt, T. D. (2017b). Medical licensure questions and physician reluctance to seek care for mental health conditions. Mayo Clin. Proc. 92, 1486–1493. doi: 10.1016/j.mayocp.2017.06.020
Eisenberg, D., Downs, M. F., Golberstein, E., and Zivin, K. (2009). Stigma and help seeking for mental health among college students. Med. Care Res. Rev. 66, 522–541. doi: 10.1177/1077558709335173
Frögéli, E., Rudman, A., and Gustavsson, P. (2019). The relationship between task mastery, role clarity, social acceptance, and stress: an intensive longitudinal study with a sample of newly registered nurses. Int. J. Nurs. Stud. 91, 60–69. doi: 10.1016/j.ijnurstu.2018.10.007
Gärtner, F. R., Nieuwenhuijsen, K., van Dijk, F. J., and Sluiter, J. K. (2010). The impact of common mental disorders on the work functioning of nurses and allied health professionals. A systematic review. Int. J. Nurs. Stud. 47, 1047–1061. doi: 10.1016/j.ijnurstu.2010.03.013
Geuijen, P., Rond, M., de Kuppens, J., Atsma, F., Schene, A., Haan, H., et al. (2020). Physicians’ norms and attitudes towards substance use in colleague physicians: a cross-sectional survey in the Netherlands. PLoS One 15:e0231084. doi: 10.1371/journal.pone.0231084
Gómez-Urquiza, J. L., Vargas, C., La Fuente, E. I, de Fernández-Castillo, R., and La Cañadas-De Fuente, G. A. (2017). Age as a risk factor for burnout syndrome in nursing professionals: a meta-analytic study. Res. Nurs. Health 40, 99–110. doi: 10.1002/nur.21774
Greenberg, N., and Tracy, D. (2020). What healthcare leaders need to do to protect the psychological well-being of frontline staff in the COVID-19 pandemic. BMJ Leader 4, 101–102. doi: 10.1136/leader-2020-000273
Guo, Y., Luo, Y., Lam, L., Cross, W., Plummer, V., and Zhang, J. (2018). Burnout and its association with resilience in nurses: a cross-sectional study. J. Clin. Nurs. 27, 441–449. doi: 10.1111/jocn.13952
Hadlaczky, G., Hökby, S., Mkrtchian, A., Carli, V., and Wasserman, D. (2014). Mental health first aid is an effective public health intervention for improving knowledge, attitudes, and behaviour: a meta-analysis. Int. Rev. Psychiatry 26, 467–475. doi: 10.3109/09540261.2014.924910
Hanschmidt, F. (2018). Deutsche Übersetzung des General Help Seeking Questionnaire (GHSQ). Berlin: Springer.
Hastuti, R., and Timming, A. R. (2021). An inter-disciplinary review of the literature on mental illness disclosure in the workplace: implications for human resource management. Int. J. Hum. Resour. Manag. 32, 3302–3338. doi: 10.1080/09585192.2021.1875494
Holmes, E. P., Corrigan, P. W., Williams, P., Canar, J., and Kubiak, M. A. (1999). Changing attitudes about schizophrenia. Schizophr. Bull. 25, 447–456. doi: 10.1093/oxfordjournals.schbul.a033392
Hoyle, R. H., and Gottfredson, N. C. (2015). Sample size considerations in prevention research applications of multilevel modeling and structural equation modeling. Prevent. Sci. 16, 987–996. doi: 10.1007/s11121-014-0489-8
Hudson, E., Arnaert, A., and Lavoie-Tremblay, M. (2021). Healthcare professional disclosure of mental illness in the workplace: a rapid scoping review. J. Ment. Health [Epub ahead of print]. doi: 10.1080/09638237.2021.1979485
Hugo, M. (2001). Mental health professionals’ attitudes towards people who have experienced a mental health disorder. J. Psychiatr. Ment. Health Nurs. 8, 419–425. doi: 10.1046/j.1351-0126.2001.00430.x
Jennings, K. S., Cheung, J. H., Britt, T. W., Goguen, K. N., Jeffirs, S. M., Peasley, A. L., et al. (2015). How are perceived stigma, self-stigma, and self-reliance related to treatment-seeking? A three-path model. Psychiatr. Rehabil. J. 38, 109–116. doi: 10.1037/prj0000138
Jorm, A. F. (2011). Mental health literacy: empowering the community to take action for better mental health. Am. Psychol. 67, 231–243. doi: 10.1037/a0025957
Jorm, A. F., Kitchener, B. A., Fischer, J., and Cvetkovski, S. (2010). Mental health first aid training by e-learning: a randomized controlled trial. Austral. New Zeal. J. Psychiatry 44, 1072–1081. doi: 10.3109/00048674.2010.516426
Jorm, A. F., Korten, A. E., Jacomb, P. A., Christensen, H., and Henderson, S. (1999). Attitudes towards people with a mental disorder: a survey of the Australian public and health professionals. Austral. New Zeal. J. Psychiatry 33, 77–83. doi: 10.1046/j.1440-1614.1999.00513.x
Jorm, A. F., Korten, A. E., Jacomb, P. A., Christensen, H., Rodgers, B., and Pollitt, P. P. (1997). “Mental health literacy”: a survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med. J. Austral. 166, 182–186. doi: 10.5694/j.1326-5377.1997.tb140071.x
Jorm, A. F., Medway, J., Christensen, H., Korten, A. E., Jacomb, P. A., and Rodgers, B. (2000). Public beliefs about the helpfulness of interventions for depression. Effects on actions taken when experiencing anxiety and depression symptoms. Austral. New Zeal. J. Psychiatry 34, 619–626. doi: 10.1080/j.1440-1614.2000.00761.x
Jorm, A. F., Nakane, Y., Christensen, H., Yoshioka, K., Griffiths, K. M., and Wata, Y. (2005). Public beliefs about treatment and outcome of mental disorders: a comparison of Australia and Japan. BMC Med. 3:14. doi: 10.1186/1741-7015-3-1
Jung, H., Sternberg, K., and von Davis, K. (2017). The impact of mental health literacy, stigma, and social support on attitudes toward mental health help-seeking. Int. J. Ment. Health Promot. 19, 252–267. doi: 10.1080/14623730.2017.1345687
Kessler, R., Berglund, P., Demler, O., Jin, R., Koretz, D., Merikangas, K., et al. (2003). The epidemiology of major depressive disorder. J. Am. Med. Assoc. 289, 3095–3105. doi: 10.1001/jama.289.23.3095
Kessler, R., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., and Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 62, 593–602. doi: 10.1001/archpsyc.62.6.593
Knaak, S., Mantler, E., and Szeto, A. (2017). Mental illness-related stigma in healthcare. Barriers to access and care and evidence-based solutions. Healthcare Manag. Forum 30, 111–116. doi: 10.1177/0840470416679413
Kuhlmann, E., Batenburg, R., Wismar, M., Dussault, G., Maier, C. B., Glinos, I. A., et al. (2018). A call for action to establish a research agenda for building a future health workforce in Europe. Health Res. Policy Syst. 16, 5–8. doi: 10.1186/s12961-018-0333-x
Kunyk, D., Inness, M., Reisdorfer, E., Morris, H., and Chambers, T. (2016). Help seeking by health professionals for addiction: a mixed studies review. Int. J. Nurs. Stud. 60, 200–215. doi: 10.1016/j.ijnurstu.2016.05.001
Langlands, R. L., Jorm, A. F., Kelly, C. M., and Kitchener, B. A. (2008). First aid recommendations for psychosis: using the Delphi method to gain consensus between mental health consumers, carers, and clinicians. Schizophr. Bull. 34, 435–443. doi: 10.1093/schbul/sbm099
Lenhard, A., and Lenhard, W. (2016). Berechnung von Effektstärken. Available online at: https://www.psychometrica.de/effektstaerke.html (accessed January 03, 2022).
Leo, C. G., Sabina, S., Tumolo, M. R., Bodini, A., Ponzini, G., Sabato, E., et al. (2021). Burnout among healthcare workers in the COVID 19 Era: a review of the existing literature. Front. Public Health 9:750529. doi: 10.3389/fpubh.2021.750529
Lim, J., Bogossian, F., and Ahern, K. (2010). Stress and coping in Australian nurses: a systematic review. Int. Nurs. Rev. 57, 22–31. doi: 10.1111/j.1466-7657.2009.00765.x
Link, B. G., Cullen, F. T., Frank, J., and Wozniak, J. F. (1987). The social rejection of former mental patients. Understanding why labels matter. Am. J. Sociol. 92, 1461–1500. doi: 10.1086/228672
Link, B. G., and Phelan, J. C. (2001). Conceptualizing stigma. Annu. Rev. Sociol. 27, 363–385. doi: 10.1146/annurev.soc.27.1.363
Link, B. G., and Phelan, J. C. (2013). “Labeling and stigma,” in Handbook of the Sociology of Mental Health, eds C. S. Aneshensel and J. C. Phelan (Berlin: Springer), 525–541.
Magliano, L., Fiorillo, A., Rosa, C., de Malangone, C., and Maj, M. (2004). Beliefs about schizophrenia in Italy: a comparative nationwide survey of the general public, mental health professionals, and patients’ relatives. Can. J. Psychiatry Rev. Can. Psychiatr. 49, 322–330.
Mahmud, S., Hossain, S., Muyeed, A., Islam, M. M., and Mohsin, M. (2021). The global prevalence of depression, anxiety, stress, and, insomnia and its changes among health professionals during COVID-19 pandemic: a rapid systematic review and meta-analysis. Heliyon 7:e07393. doi: 10.1016/j.heliyon.2021.e07393
Mason, R. J., Hart, L. M., Rossetto, A., and Jorm, A. F. (2015). Quality and predictors of adolescents’ first aid intentions and actions towards a peer with a mental health problem. Psychiatry Res. 228, 31–38. doi: 10.1016/j.psychres.2015.03.036
Maxwell, S. E., and Cole, D. A. (2007). Bias in cross-sectional analyses of longitudinal mediation. Psychol. Methods 12, 23–44. doi: 10.1037/1082-989X.12.1.23
Mehta, N., and Pandit, A. (2018). Concurrence of big data analytics and healthcare. A systematic review. Int. J. Med. Inform. 114, 57–65. doi: 10.1016/j.ijmedinf.2018.03.013
Mendoza, H., Masuda, A., and Swartout, K. M. (2015). Mental health stigma and self-concealment as predictors of help-seeking attitudes among Latina/o College Students in the United States. Int. J. Adv. Counsel. 37, 207–222. doi: 10.1007/s10447-015-9237-4
MHFA (2022). International Mental Health First Aid Programs. Available online at: http://www.mhfainternational.org/international-mhfa-programs.html (accessed July 27, 2021)
Milin, R., Kutcher, S., Lewis, S. P., Walker, S., Wei, Y., Ferrill, N., et al. (2016). Impact of a mental health curriculum on knowledge and stigma among high school students: a randomized controlled trial. J. Am. Acad. Child Adolesc. Psychiatry 55, 383–391. doi: 10.1016/j.jaac.2016.02.018
Moll, S., Eakin, J. M., Franche, R., and Strike, C. (2013). When health care workers experience mental ill health. Institutional practices of silence. Qual. Health Res. 23, 167–179. doi: 10.1177/1049732312466296
Moll, S. E., Patten, S. B., Stuart, H., Kirsh, B., and MacDermid, J. C. (2015). Beyond silence. Protocol for a randomized parallel-group trial comparing two approaches to workplace mental health education for healthcare employees. BMC Med. Educ. 15:78. doi: 10.1186/s12909-015-0363-9
Moll, S. E., Patten, S. B., Stuart, H., MacDermid, J. C., and Kirsh, B. (2018). Beyond silence. A randomized, parallel-group trial exploring the impact of workplace mental health literacy training with healthcare employees. Can. J. Psychiatry 3, 826–833. doi: 10.1177/0706743718766051
Moll, S. E., Zanhour, M., Patten, S. B., Stuart, H., and MacDermid, J. C. (2017). Evaluating mental health literacy in the workplace: development and psychometric properties of a vignette-based tool. J. Occup. Rehabil. 27, 601–611. doi: 10.1007/s10926-017-9695-0
Morgan, A. J., Ross, A., and Reavley, N. J. (2018). Systematic review and meta-analysis of Mental Health First Aid training: effects on knowledge, stigma, and helping behaviour. PLoS One 13:e0197102. doi: 10.1371/journal.pone.0197102
O’Connor, K., Neff, D. M., and Pitman, S. (2018). Burnout in mental health professionals. A systematic review and meta-analysis of prevalence and determinants. Eur. Psychiatry 53, 74–99. doi: 10.1016/j.eurpsy.2018.06.003
OECD (2021). Germany: Country Health Profile 2021. State of Health in the EU. Available online at: https://www.oecd.org/health/country-health-profiles-eu.htm (accessed February 24, 2022).
Oulton, J. A. (2006). The global nursing shortage: an overview of issues and actions. Policy Polit. Nurs. Pract. 7, 34S–39S. doi: 10.1177/1527154406293968
Patel, V., Flisher, A. J., Hetrick, S., and McGorry, P. (2007). Mental health of young people. A global public-health challenge. Lancet 369, 1302–1313. doi: 10.1016/S0140-6736(07)60368-7
Pedersen, E. R., and Paves, A. P. (2014). Comparing perceived public stigma and personal stigma of mental health treatment seeking in a young adult sample. Psychiatry Res. 219, 143–150. doi: 10.1016/j.psychres.2014.05.017
Perry, L., Lamont, S., Brunero, S., Gallagher, R., and Duffield, C. (2015). The mental health of nurses in acute teaching hospital settings. A cross-sectional survey. BMC Nurs. 14:8. doi: 10.1186/s12912-015-0068-8
Pescosolido, B. A., Jensen, P. S., Martin, J. K., Perry, B. L., Olafsdottir, S., and Fettes, D. (2008). Public knowledge and assessment of child mental health problems. Findings from the National Stigma Study-Children. J. Am. Acad. Child Adolesc. Psychiatry 47, 339–349. doi: 10.1097/CHI.0b013e318160e3a0
Podsakoff, P. M., MacKenzie, S. B., Lee, J., and Podsakoff, N. P. (2003). Common method biases in behavioural research: a critical review of the literature and recommended remedies. J. Appl. Psychol. 88, 879–903. doi: 10.1037/0021-9010.88.5.879
Rafferty, A. M., Busse, R., Zander-Jentsch, B., Sermeus, W., and Bruyneel, L. (2019). Strengthening Health Systems Through Nursing. Evidence from 14 European Countries (Health Policy Series). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK545724/ (accessed February 24, 2022).
Rebscher, H., Marschall, J., Hildebrandt-Heene, S., Sydow, H., and Nolting, H. (eds) (2016). Schwerpunkt: Gender und Gesundheit. Heidelberg: Springer.
Rickwood, D., Deane, F. P., Wilson, C. J., and Ciarrochi, J. (2005). Young people’s help-seeking for mental health problems. Austral. J. Adv. Ment. Health 4, 218–251. doi: 10.5172/jamh.4.3.218
Rickwood, D. J., Thomas, K., and Bradford, S. (2012). Help-Seeking Measures in Mental Health: A Rapid Review. An Evidence Check review brokered by the Sax Institute for Beyondblue. Available online at: http://www.saxinstitute.org.au (accessed January 03, 2022).
Ridic, G., Gleason, S., and Ridic, O. (2012). Comparisons of health care systems in the United States, Germany and Canada. Mat. Socio Med. 24, 112–120. doi: 10.5455/msm.2012.24.112-120
Ross, C. A., and Goldner, E. M. (2009). Stigma, negative attitudes and discrimination towards mental illness within the nursing profession. A review of the literature. J. Psychiatr. Ment. Health Nurs. 16, 558–567. doi: 10.1111/j.1365-2850.2009.01399.x
Rossetto, A., Jorm, A. F., and Reavley, N. J. (2016). Predictors of adults’ helping intentions and behaviours towards a person with a mental illness: a six-month follow-up study. Psychiatry Res. 240, 170–176. doi: 10.1016/j.psychres.2016.04.037
Rüsch, N., Angermeyer, M. C., and Corrigan, P. W. (2005). Das Stigma psychischer Erkrankung: Konzepte, Formen und Folgen. Psychiatr. Praxis 32, 221–232. doi: 10.1055/s-2004-834566
Rüsch, N., Evans-Lacko, S. E., Henderson, C., Flach, C., and Thornicroft, G. (2011). Knowledge and attitudes as predictors of intentions to seek help for and disclose a mental illness. Psychiatr. Serv. 62, 675–678. doi: 10.1176/ps.62.6.pss6206_0675
Rüsch, N., Müller, M., Ajdacic-Gross, V., Rodgers, S., Corrigan, O., and Rössler, W. (2014). Shame, perceived knowledge and satisfaction associated with mental health as predictors of attitude patterns towards help-seeking. Epidemiol. Psychiatr. Sci. 23, 177–187. doi: 10.1017/S204579601300036X
Sampaio, F., Sequeira, C., and Teixeira, L. (2020). Nurses’ mental health during the Covid-19 outbreak: a cross-sectional study. J. Occup. Environ. Med. 62, 783–787. doi: 10.1097/JOM.0000000000001987
Schermelleh-Engel, K., Moosbrugger, H., and Müller, H. (2003). Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Methods Psychol. Res. 8, 23–74.
Schnyder, N., Panczak, R., Groth, N., and Schultze-Lutter, F. (2017). Association between mental health-related stigma and active help-seeking. Systematic review and meta-analysis. Br. J. Psychiatry 210, 261–268. doi: 10.1192/bjp.bp.116.189464
Schomerus, G., Matschinger, H., and Angermeyer, M. C. (2009). Attitudes that determine willingness to seek psychiatric help for depression: a representative population survey applying the theory of planned behaviour. Psychol. Med. 39, 1855–1865. doi: 10.1017/S0033291709005832
Schomerus, G., Stolzenburg, S., Freitag, S., Speerforck, S., Janowitz, D., Evans-Lacko, S., et al. (2018). Stigma as a barrier to recognizing personal mental illness and seeking help: a prospective study among untreated persons with mental illness. Eur. Arch. Psychiatry Clin. Neurosci. 269, 469–479. doi: 10.1007/s00406-018-0896-0
Schönfeld, G., Wenzelmann, F., Pfeifer, H., Risius, P., and Wehner, C. (2020). Ausbildung in Deutschland - eine Investition gegen den Fachkräftemangel. Available online at: https://www.bibb.de/dienst/veroeffentlichungen/de/publication/show/16551 (accessed February 20, 2022).
Schug, C., Morawa, E., Geiser, F., Hiebel, N., Beschoner, P., Jerg-Bretzke, L., et al. (2021). Social support and optimism as protective factors for mental health among 7765 healthcare workers in Germany during the COVID-19 pandemic: results of the VOICE study. Int. J. Environ. Res. Public Health 18:3827. doi: 10.3390/ijerph18073827
Schulten, T. (2006). Liberalisation, Privatisation and Regulation in the German Healthcare Sector/Hospitals. Düsseldorf: The Institute of Economic and Social Research (WSI).
Simmons, S. (1994). Social networks: their relevance to mental health nursing. J. Adv. Nurs. 19, 281–289. doi: 10.1111/j.1365-2648.1994.tb01082.x
Smith, C. L., and Shochet, I. M. (2011). The impact of mental health literacy on help-seeking intentions. Results of a pilot study with first year psychology students. Int. J. Ment. Health Promot. 13, 14–20. doi: 10.1080/14623730.2011.9715652
Smith, G. B., and Hukill, E. (1996). Nurses impaired by emotional and psychological dysfunction. J. Am. Psychiatr. Nurses Assoc. 2, 192–200. doi: 10.1177/107839039600200603
Søvold, L. E., Naslund, J. A., Kousoulis, A. A., Saxena, S., Qoronfleh, M. W., Grobler, C., et al. (2021). Prioritizing the mental health and well-being of healthcare workers: an urgent global public health priority. Front. Public Health 9:e679397. doi: 10.3389/fpubh.2021.679397
Stadler, S. M. (2010). Einstellungen und Soziale Distanz gegenüber psychisch Kranken. Z. Psychiatr. Psychol. Psychother. 58, 265–273. doi: 10.1024/1661-4747/a000037
Stolzenburg, S., Freitag, S., Evans-Lacko, S., Speerforck, S., Schmidt, S., and Schomerus, G. (2018). Individuals with currently untreated mental illness. Causal beliefs and readiness to seek help. Epidemiol. Psychiatr. Sci. 28, 446–457. doi: 10.1017/S2045796017000828
Thompson, C. M., Pulido, M. D., and Caban, S. (2022). Why is it difficult for social network members to support people living with mental illnesses?: linking mental illness uncertainty to support provision. Health Commun. 37, 202–213. doi: 10.1080/10410236.2020.1831166
Uchiyama, A., Odagiri, Y., Ohya, Y., Takamiya, T., Inoue, S., and Shimomitsu, T. (2013). Effect on mental health of a participatory intervention to improve psychosocial work environment. A cluster randomized controlled trial among nurses. J. Occup. Health 55, 173–183. doi: 10.1539/joh.12-0228-OA
Verhaeghe, M., and Bracke, P. (2012). Associative stigma among mental health professionals. Implications for professional and service user well-being. J. Health Soc. Behav. 53, 17–32. doi: 10.1177/0022146512439453
Vogel, D. L., Bitman, R. L., Hammer, J. H., and Wade, N. G. (2013). Is stigma internalized? The longitudinal impact of public stigma on self-stigma. J. Counsel. Psychol. 60, 311–316. doi: 10.1037/a0031889
Vogel, D. L., Wade, N. G., and Haake, S. (2006). Measuring the self-stigma associated with seeking psychological help. J. Counsel. Psychol. 53, 325–337. doi: 10.1037/0022-0167.53.3.325
Vogel, D. L., Wade, N. G., Wester, S. R., Larson, L., and Hackler, A. H. (2007a). Seeking help from a mental health professional. The influence of one’s social network. J. Clin. Psychol. 63, 233–245. doi: 10.1002/jclp.20345
Vogel, D. L., Wade, N. G., and Hackler, A. H. (2007b). Perceived public stigma and the willingness to seek counseling: the mediating roles of self-stigma and attitudes toward counseling. J. Counsel. Psychol. 54, 40–50. doi: 10.1037/0022-0167.54.1.40
Wallace, J. E. (2012). Mental health and stigma in the medical profession. Health 16, 3–18. doi: 10.1177/1363459310371080
Wang, C., Cramer, K. M., Cheng, H., and Do, K. A. (2019). Associations between depression literacy and help-seeking behaviour for mental health services among high school students. Sch. Ment. Health 11, 707–718. doi: 10.1007/s12310-019-09325-1
Wang, P. S., Angermeyer, M., Borges, G., Bruffaerts, R., Chiu, W. T., Girolamo, G., et al. (2007). Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 6, 177–185.
Wang, P. S., Berglund, P., Olfson, M., Pincus, H. A., Wells, K. B., and Kessler, R. C. (2005). Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 62, 603–613. doi: 10.1001/archpsyc.62.6.603
Wazqar, D. Y., Kerr, M., Regan, S., and Orchard, C. (2017). An integrative review of the influence of job strain and coping on nurses’ work performance: understanding the gaps in oncology nursing research. Int. J. Nurs. Sci. 4, 418–429. doi: 10.1016/j.ijnss.2017.09.003
Weber, R., and Crocker, J. (1983). Cognitive processes in the revision of stereotypic beliefs. J. Pers. Soc. Psychol. 45, 961–977. doi: 10.1037/0022-3514.45.5.961
Wei, Y., McGrath, P. J., Hayden, J., and Kutcher, S. (2015). Mental health literacy measures evaluating knowledge, attitudes and help-seeking: a scoping review. BMC Psychiatry 15:9. doi: 10.1186/s12888-015-0681-9
West, S. G., Taylor, A. B., and Wu, W. (2012). “Model fit and model selection in structural equation modeling,” in Handbook of Structural Equation Modeling, ed. R. H. Hoyle (New York, NY: Guilford Press), 209–231.
Weston, M. J., and Nordberg, A. (2021). Stigma: a barrier in supporting nurse well-being during the pandemic. Nurse Lead. 20, 174–178. doi: 10.1016/j.mnl.2021.10.008
Wheat, K., Brohan, E., Henderson, C., and Thornicroft, G. (2010). Mental illness and the workplace: conceal or reveal? J. R. Soc. Med. 103, 83–86. doi: 10.1258/jrsm.2009.090317
Wieclaw, J., Agerbo, E., Mortensen, P. B., and Bonde, J. P. (2006). Risk of affective and stress related disorders among employees in human service professions. Occup. Environ. Med. 63, 314–319. doi: 10.1136/oem.2004.019398
Wiederkehr, G. (2012). Betriebliche Gesundheitsförderung – Bedeutung der Entwicklung von Gesundheitskompetenz von Pflegepersonen. Österreichische Pflegezeitschrift 2, 21–24.
Wilson, C. J., Deane, F. P., Ciarrochi, J., and Rickwood, D. (2005). Measuring help-seeking intentions. Properties of the general help seeking questionnaire. Can. J. Counsel. Psychother. 39, 15–28.
World Health Organization [WHO] (2016). Global Strategy on Human Resources for Health: Workforce 2030. Geneva: World Health Organization.
World Health Organization [WHO] (2017). Depression and Other Common Mental Disorders. Geneva: World Health Organization.
World Health Organization [WHO] (2019). Mental Health in the Workplace. Geneva: World Health Organization.
Wulf, I. C., and Ruhle, S. A. (2020). Psychische Gesundheitskompetenz am Arbeitsplatz – Validierung und Anpassung einer deutschsprachigen Version des Mental Health Literacy Tool for the Workplace. Diagnostica 66, 50–61. doi: 10.1026/0012-1924/a000237
Zentralinstitut für Seelische Gesundheit Mannheim (2022). MHFA Ersthelfer. Available online at: https://www.mhfa-ersthelfer.de/de/was-ist-mhfa/ (accessed January 03, 2022).
Keywords: mental health literacy, workplace, help-seeking, help-outreach, stigma, healthcare, mental health literacy tool for the workplace, MHL-W-G
Citation: Wulf IC (2022) Help-Seeking and Help-Outreach Intentions of Healthcare Workers—The Role of Mental Health Literacy and Stigma in the Workplace. Front. Educ. 7:856458. doi: 10.3389/feduc.2022.856458
Received: 17 January 2022; Accepted: 11 March 2022;
Published: 06 May 2022.
Edited by:
Francisco Sampaio, Fernando Pessoa University, PortugalReviewed by:
Christine Grové, Monash University, AustraliaHyejin Jung, The University of Texas at El Paso, United States
Copyright © 2022 Wulf. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ines Catharina Wulf, aW5lcy53dWxmQGhodS5kZQ==
 Ines Catharina Wulf
Ines Catharina Wulf