- 1Department of Pediatrics, Oklahoma State University Center for Health Sciences, Tulsa, OK, United States
- 2Department of Epidemiology and Public Health, Yale University, New Haven, CT, United States
Adverse childhood experiences (ACEs) refer to a collection of traumatic life events that can derail future development, impact physical/mental health, and affect learning/behavior into adulthood. In the United States, it is estimated that two-thirds of children and teens will experience traumatic ACEs by the age of 16. Schools can represent one domain in a child’s life where trauma-informed approaches (TIAs) could be helpful to curtail effects of ACEs. This systematic review aimed to identify some positive commonalities/facilitators (e.g., drivers of change) among existing TIAs implemented in US schools. The secondary objectives aimed to evaluate the confidence of qualitative data using GRADE-CERQual and to highlight potential challenges/barriers associated with the implementation process of TIAs in schools. This manuscript presents a thorough overview of the current state of trauma-informed practices in US schools and concludes with a forward-thinking discussion on key implications for enhancing the field of education.
Background
Introduction of adverse childhood experiences
Encountering adversity in early childhood can have a long-term negative impact on the health and wellbeing of children (Felitti et al., 1998). Adverse childhood experiences [ACEs1 (Centers for Disease Control and Prevention, 2019a)] refer to a collection of preventable, potentially traumatic life events that can derail normal development, alter brain architecture by excessive activation of the body’s stress response, and ultimately impact physical health, mental health, learning, and behavior (Finkelhor et al., 2015; Centers for Disease Control and Prevention, 2019a). Felitti et al. (1998) conducted the groundbreaking ACE study to assess the relationship between childhood abuse/household dysfunction and adult health risk factors/behaviors (pg. 248). These researchers asked questions across three main ACE categories of negative childhood experiences encompassing abuse, neglect, and household dysfunction (Felitti et al., 1998). Participants were given a score of 1 for each ACE category that they experienced prior to their 18th birthday. The results of this original ACE study and subsequent research have shown that “as ACE scores increased, so did the risk of developing physical health issues (e.g., heart disease, chronic lung disease, stroke, diabetes, cancers, and shortened lifespan) and mental health problems” (e.g., depression, anxiety, behavioral disorders, and suicidality) (Felitti et al., 1998; Felitti, 2002; Chapman et al., 2004; Metzler et al., 2017). Young individuals experiencing ACEs are “at risk to suffer from poorer physical and mental health in adulthood” […] with increased morbidity and mortality (Bellis et al., 2015, 2017). According to the Substance Abuse and Mental Health Services Administration (SAMHSA) (Substance Abuse and Mental Health Services Administration, National Center for Trauma- Informed Care, 2015), “more than two thirds of children reported at least 1 adverse traumatic event by age 16,” which is congruent with similar data from the Centers for Disease Control and Prevention (CDC) that reported 60% of adults experienced >1 ACEs before age 18 (Centers for Disease Control and Prevention, 2019a).
General strategies to prevent adverse childhood experiences
The CDC has adopted a holistic approach to prevent ACEs by utilizing six general strategies derived from the best available evidence (Centers for Disease Control and Prevention, 2019b). As outlined in the CDC’s prevention toolkit, Preventing Adverse Childhood Experiences (ACEs): Leveraging the Best Available Evidence, these strategies focused on primary prevention methods. The six strategies outlined: (1) strengthening economic supports for families (e.g., earned income tax credits, family-friendly work policies); (2) promoting social norms that protect against violence and adversity (e.g., public education campaigns to support parents and positive parenting, bystander approaches to support healthy relationship behaviors); (3) ensuring a strong start for children (e.g., early childhood home visitation, high quality and affordable childcare, preschool enrichment programs); (4) teaching skills to help youth and parents handle stress, (5) connecting youth to caring adults and activities, and (6) intervening to lessen immediate and long-term harms (e.g., advancement of trauma-informed care for children and young adults with a history of exposure to ACEs) (Centers for Disease Control and Prevention, 2019b). Since ACEs can span from childhood to young adulthood, disrupting cognitive, social, emotional/behavioral development, and learning (Crosby, 2015), the theme of this systematic review aligned closely with strategy #6.
Impact of adverse childhood experiences on learning
While some degree of adversity is normal and an essential part of human growth and development, exposure to frequent and prolonged stress, in the absence of positive/protective factors, can result in toxic stress to the body (Centers for Disease Control and Prevention, 2019a). In children, when adverse reactions such as feelings of intense fear, terror, and helplessness are activated repeatedly, stress hormones can accumulate and interrupt normal physical and mental development, which can lead to behavioral/emotional difficulties and learning disorders (Sameroff et al., 2003; Moore and Ramirez, 2016; Bethell et al., 2017). A growing body of research indicates that children with chronic changes to their brain architecture from toxic stress (i.e., higher ACEs) may develop problems related to attention, impulsivity, and decision-making (Shonkoff et al., 2012; Reavis et al., 2013; Brunzell et al., 2015). More alarming is the notion that trauma effects can be cumulative—youth who experience two or more ACEs are at increased risk for developing worse adverse outcomes in adulthood (Chartier et al., 2010). These same young individuals are 3 times more likely to repeat a grade and have a 10-fold increased risk for developing a learning deficit/disorder in the future (Burke et al., 2011).
The origins of being “trauma-informed”
Four elements of trauma-informed care
Most of the modern programs/initiatives surrounding trauma-informed practice in U.S. schools are guided by SAMHSA’s guidelines (Substance Abuse and Mental Health Services Administration, National Center for Trauma- Informed Care, 2015). SAMHSA defines trauma-informed care, using “the 4 R’s” (four key elements), as “programs, organizations, and/or systems that realize the widespread impact of trauma and understands potential paths for recovery; recognize the signs and symptoms of trauma in clients, families, staff, and others involved; and respond by fully integrating knowledge about trauma into policies, procedures, and practices, and seeks to actively resist re-traumatization,” all the while examining assumptions and biases associated with inequality and trauma (Substance Abuse and Mental Health Services Administration, National Center for Trauma- Informed Care, 2015). In addition, the guidelines for implementation of trauma-informed care are based on six SAMHSA principles (safety, trustworthiness/transparency, peer support, collaboration and mutuality, empowerment/voice/choice, and cultural/historical/gender issues). Together, the four key elements and six SAMHSA principles of trauma-informed care assume a continuum of trauma-informed approaches (TIAs) ranging from prevention methods to more intensive trauma-specific interventions (Substance Abuse and Mental Health Services Administration, National Center for Trauma- Informed Care, 2015). The concept of trauma-informed care first emerged within health care settings in the early 2000s (Harris and Fallot, 2001), then was later adopted by child welfare and juvenile justice systems in Ko et al. (2008).
The role of trauma-informed schools
Schools and child-serving agencies represent natural environments that can help prevent and reduce the adverse effects of ACEs (Day et al., 2015). Trauma-informed school is an umbrella term used to describe approaches that share common proposals for “change” and more effectively “engage” students in the learning process. In the past decade, the Administration for Children and Families (ACF), Centers for Medicare and Medicaid Services (CMS), the Department of Justice (DOJ), the Department of Education, and the CDC have recognized the impact of ACEs on youth development and wellbeing. These organizations have launched initiatives and implemented policies to promote the use (and expansion) of TIAs across schools and child-serving agencies (Lang et al., 2015). As a result, the provision of TIAs is growing at a rapid rate among school systems in America (Maynard et al., 2019) with various program adaptations in at least 17 states (Lang et al., 2015). At least another dozen states have passed legislation encouraging or requiring schools and its staff members to receive supplementary training on the impacts of childhood trauma (Chriqui et al., 2019).
Goals of trauma-informed approaches
The main goals of TIAs in schools are to ameliorate the effects of ACEs, support healing, growth and change by leveraging all aspects of the school system (inclusive of policies and procedures) that create safe learning environments (Bateman et al., 2013). Furthermore, these TIAs should support the health and development of all students, enabling them to regulate their emotions, focus their attention, and succeed academically/socially (Cole et al., 2013).
Primary and secondary objectives
The primary objective of this systematic review aimed to identify commonalities and facilitators (i.e., drivers of change) among TIAs implemented in four schools located in distinct US geographic regions. The secondary objectives aimed to (1) evaluate the confidence of qualitative data using the GRADE-CERQual framework and (2) highlight potential challenges/barriers associated with the implementation of TIAs.
Methodology
Information sources
The author conducted a comprehensive search for published/unpublished papers and gray literature inclusive of the targeted topics surrounding TIAs in US school systems. The set timeframe was between January 2015 and March 2022 given the relative newness of trauma-informed practices and program developments and the publication of SAMHSA’s guidelines in July 2014. The following interdisciplinary databases were searched: American College of Physicians (ACP) Journal Club, Cochrane Central Register of Controlled Trials (CENTRAL), Cochrane Database of Systematic Reviews (CDSR), EBSCO Research Platform, Education Resources Information Center (ERIC), GOOGLE Scholar, National Center for Biotechnology Information (NCBI) PubMed, OVID Medline, ProQuest Central, and ProQuest Education.
Search strategy
The search strategy was organized around subtopics that were focused on “K-12 disadvantaged schools” (i.e., complex school systems that predominantly served students with the highest needs, from low socioeconomic backgrounds, etc.). Key search terms were linked to the following headings and subheadings: (1) trauma (e.g., trauma informed, trauma sensitive, and trauma aware), (2) schools (e.g., school-wide approaches, school, complex school systems, and K-12 general or special education), and models/interventions (e.g., framework, multidisciplinary framework, multi-tiered approaches, interventions, programs, strategies, organization(s), school policies, pedagogy, teaching practices, special education, custodial/humanistic approach, social circumstances, and social contexts). The author uploaded all potentially relevant citations and studies to the Covidence database, a systematic review software, for further screening by two independent reviewers. These two reviewers then screened each of the full-text reports, abstracts, keywords, and titles using a screening instrument.
Inclusion criteria
Each of the trauma-informed schools/programs identified through the comprehensive search above must also satisfy at least two of the three inclusion criteria (per SAMHSA’s guidelines) (Substance Abuse and Mental Health Services Administration, National Center for Trauma- Informed Care, 2015).
1) Workforce development—components of trauma-informed schools/models are designed to increase knowledge and awareness of the workforce (e.g., teachers and staff members) on the impact, signs and symptoms of trauma, including secondary traumatization. Workforce development did not need to be provided to all staff members, but some form of a continual professional development program must be incorporated.
2) Trauma-focused services—trauma-informed schools/models must implement changes in practice behaviors across the entire school, including trauma-specific assessment screening, prevention and/or intervention services (if resources available).
3) Organizational environment and practices—this element must include school-wide policies/procedural changes, and/or strategic changes intended to promote a more trauma-informed environment (as outlined by SAMHSA) (Substance Abuse and Mental Health Services Administration, National Center for Trauma- Informed Care, 2015).
Results
The synthesis of search results, screening, and initial evaluation of evidence revealed 32 articles (e.g., randomized or quasi-experimental study design, conducted in a school setting serving K-12 or equivalent students, assessed the effects of TIA, measured student-level outcome related to trauma symptoms/academic performance/behavior, English language). Most of these articles were ultimately excluded because they did not incorporate/examine the effects of trauma-informed approaches in the programs, or they did not meet at least two of the three inclusion criteria of SAMHSA’s guidelines. Only four schools with TIAs met eligibility criteria for this systematic review. Each of the four schools were located in distinct geographic locations across the US and served students ranging from 6 to 18 years old.
1) Healthy Environments and Response to Trauma in Schools [HEARTS (Dorado et al., 2016)]—located in California, USA
2) Trust-Based Relational Intervention [TBRI (Parris et al., 2015)]—located in Texas, USA
3) Heart of Teaching and Learning [HTL (Day et al., 2015)] Compassion, Resiliency, and Academic Success—located in Michigan, USA
4) New Haven Trauma Coalition [NHTC (Perry and Daniels, 2016)]—located in Connecticut, USA
The HEARTS program in California promoted school success for trauma-impacted students through a school-wide approach utilizing the response to intervention multi-tiered framework (Dorado et al., 2016). It had the largest number of participants across multiple sites (students in K-Grade 8). The TBRI program in Texas examined trust-based relational interventions in a secondary charter school for at-risk youth (Parris et al., 2015). School staff of the TBRI program created conditions to help students succeed behaviorally with strategies grouped into principles of empowering, connecting, and correcting (students in Grades 7–12). The HTL program in Michigan was a joint curriculum and intervention program designed to increase trauma-informed practices in education settings that exclusively served court-involved youth placed in residential treatment (students in Grades 5–6 but age ranged from 14 to 18 years old). The HTL program measured students’ perceptions of teachers and there were no statistically significant changes observed before and after curriculum implementation (Day et al., 2015). Finally, the NHTC program in Connecticut utilized a mixed methods approach to implement three separate direct service components (e.g., services professional development, care coordination, and clinical services) (Perry and Daniels, 2016). It was a pilot program consisting of a 3-day workshop series for 5th and 6th graders in New Haven, Connecticut.
The four trauma-informed schools/models chosen for review had mostly positive results across a range of qualitative data outcomes such as improvement of childhood trauma symptoms, self-esteem, descriptive behavioral changes, and increased staff awareness/recognition of childhood trauma. Overall, the positive commonalities and facilitators identified were (a) ongoing professional staff development training, (b) organizational drivers of culture change, (c) incorporation of students’ views (and their family/cultural needs), and (d) screening assessment of trauma pre-/post-provision of trauma-specific therapy or intervention. These findings are summarized in Supplementary Appendix Table A1.
The challenges and barriers associated with implementing TIAs in these four complex school systems were (a) unknown exact duration and/or length of TIA programs/models required to be considered “effective,” (b) which trauma-informed programs were sustainable, and (c) which specific TIAs contributed to what positive outcome results (and under what social circumstances). Only two of the four programs lasted beyond 12 months. Thus, program sustainability and reproducibility were not assessed in this review. Challenges and barriers were evaluated using the GRADE-CerQual Framework (see Supplementary Appendix Table A2). Assessments of methodological limitations, relevance, coherence, adequacy of data, and overall quality of evidence were reviewed and graded for each of these commonalities/facilitators and challenges/barriers, shown in Supplementary Appendix Tables A1, A2, respectively.
Variations among the four programs included the use of validated measurement tools, data collection methods, and outcomes assessments. All four programs seemed to utilize school administrative data of behavioral incidents pre- and post-intervention as the central feature of outcomes evaluation. Specifically, three of the four programs used the “number of office referrals” for behavioral incidents as the primary measure of outcomes. The use of administrative data in education research is gaining traction in recent times because researchers can study the heterogeneous effects of school-wide policies and practice. Hence, with very large administrative data observations, it becomes possible to evaluate whether effects are similar across different groups of students, and, if they differ, how they differ and for whom (Figlio et al., 2017). Only the HEARTS program had a large enough sample size of students (N = 1,243) and teaching participants (N = 175) to distribute pre- and post-tests. However, the HEARTS program was implemented across multiple school sites with variable length of program intervention and unknown duration of psychotherapy treatments, which ultimately impacted its final school-wide outcome comparison.
Dicussion
Commonalities/facilitators and challenges/barriers
The opportunity for ongoing professional staff development training was emphasized in all four schools/models as one of the primary motivators to help teachers/staff reframe challenging or problematic student behaviors and promote staff awareness on topics related to childhood trauma. Indeed, teachers and staff members can play a vital role in identifying and supporting vulnerable (at-risk) children. They are often perceived as effective mediators within trauma-informed school environments (Larkin et al., 2014).
The inclusion theme of school-wide organizational change closely aligned with one of SAMSHA’s principles of “collaboration and mutuality” (Figure 1). The theme of “organizational culture change” was incorporated in three of the four models, which helped to create a shift away from the punishment paradigm to an enforcement of rules/consequences with accountability: thereby elevating trauma-informed thinking and practices (Cole et al., 2005) among those schools.
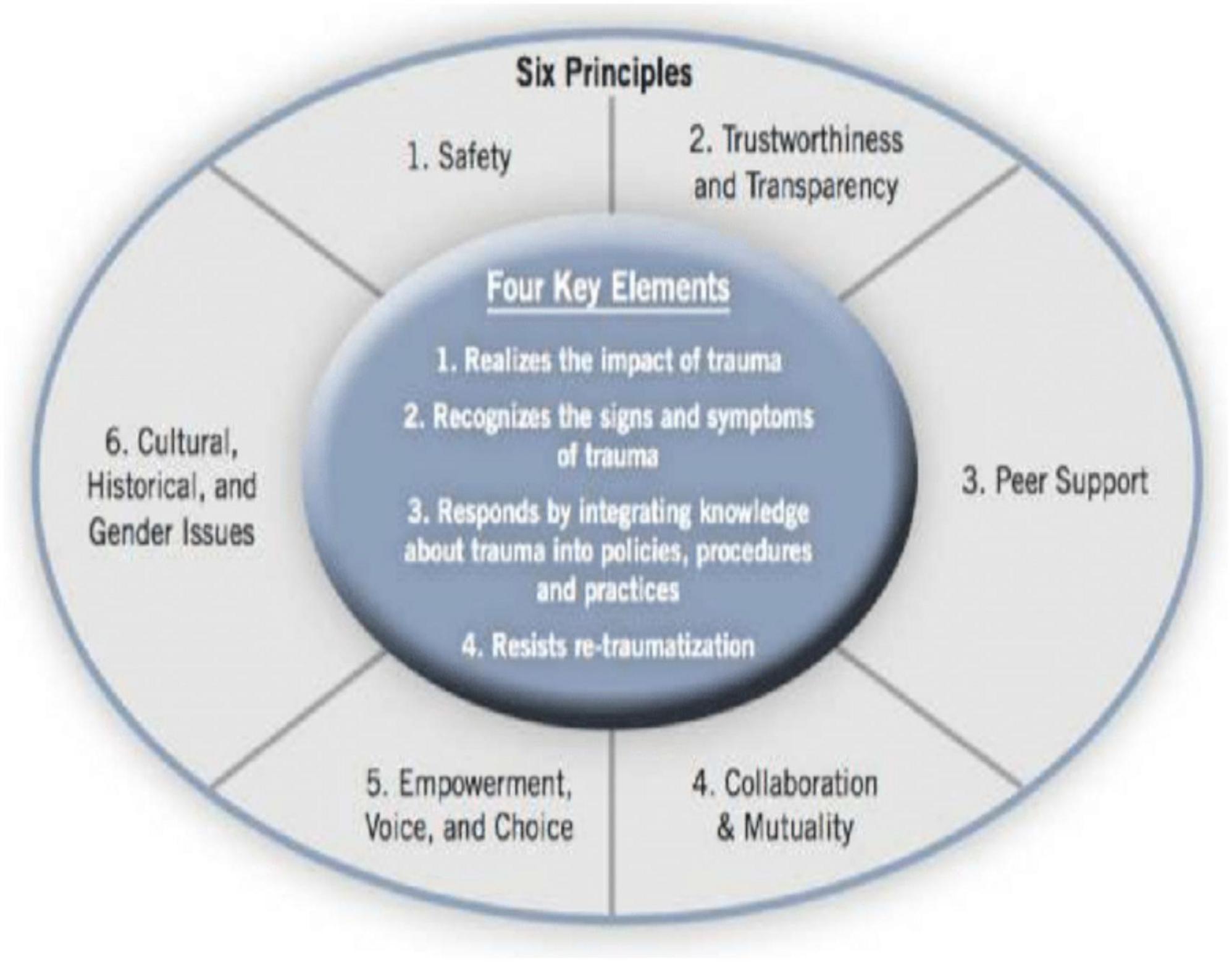
Figure 1. Substance Abuse and Mental Health Services Administration’s (SAMHSA’s) concept of trauma-informed and guidelines (Substance Abuse and Mental Health Services Administration, National Center for Trauma- Informed Care, 2015).
The last commonality observed in two of four programs was the incorporation of students’ views and their family/cultural needs—respect for students’ views and active family involvement, gaining insights from students and their families about their own needs, and strengths. This element corresponded to one of the SAMSHA principles of “recognizing cultural/historical/gender issues” (Figure 1).
There was insufficient data from this systematic review to determine the program duration, and unclear which specific TIAs contributed to what positive outcomes (and under what social circumstances/contexts). These challenges are further discussed in the next section.
Can the Consolidated Framework for Implementation Research framework help guide implementation of trauma-informed approaches in other schools?
It is worth mentioning that not all children will experience traumatic life experiences in the same manner and certainly not all will go on to develop adverse outcomes following ACEs. Given that schools are generally the first line of defense in buffering the impact of ACEs, how can the Consolidated Framework for Implementation Research (CFIR) be utilized to help translate evidence into implementation of TIAs in other US schools (with similar demographics and social contexts)? The CFIR framework includes five domains of influence derived from a consolidation of terms/concepts generated by implementation researchers: (1) intervention characteristics (e.g., evidence strength, quality, adaptability), (2) outer setting (e.g., patient needs, resources, external policies, incentives), (3) inner setting (e.g., implementation climate, readiness for implementation), (4) individuals involved (e.g., self-efficacy, knowledge and beliefs about the intervention), and (5) the implementation process (e.g., engaging members of the organization, executing the innovation) (Damschroder et al., 2009). One of the major advantages of CFIR is that it can assist with differentiating the core components from the adaptive components of a behavioral intervention/program, which is essential when assessing TIAs implemented across different school settings. CFIR is also a valuable tool because it has a more comprehensive approach to synthesizing implementation research, given the interactions of the five domains and its ability to predict determinants of implementation outcomes (Damschroder et al., 2009).
In Figure 2, CFIR was applied by using the same commonalties/drivers of change and juxtaposing the challenges/barriers to extrapolate real-world insights and predict the determinants of implementation outcomes and sustainability in a similar hypothetical school located in Oklahoma, USA.2
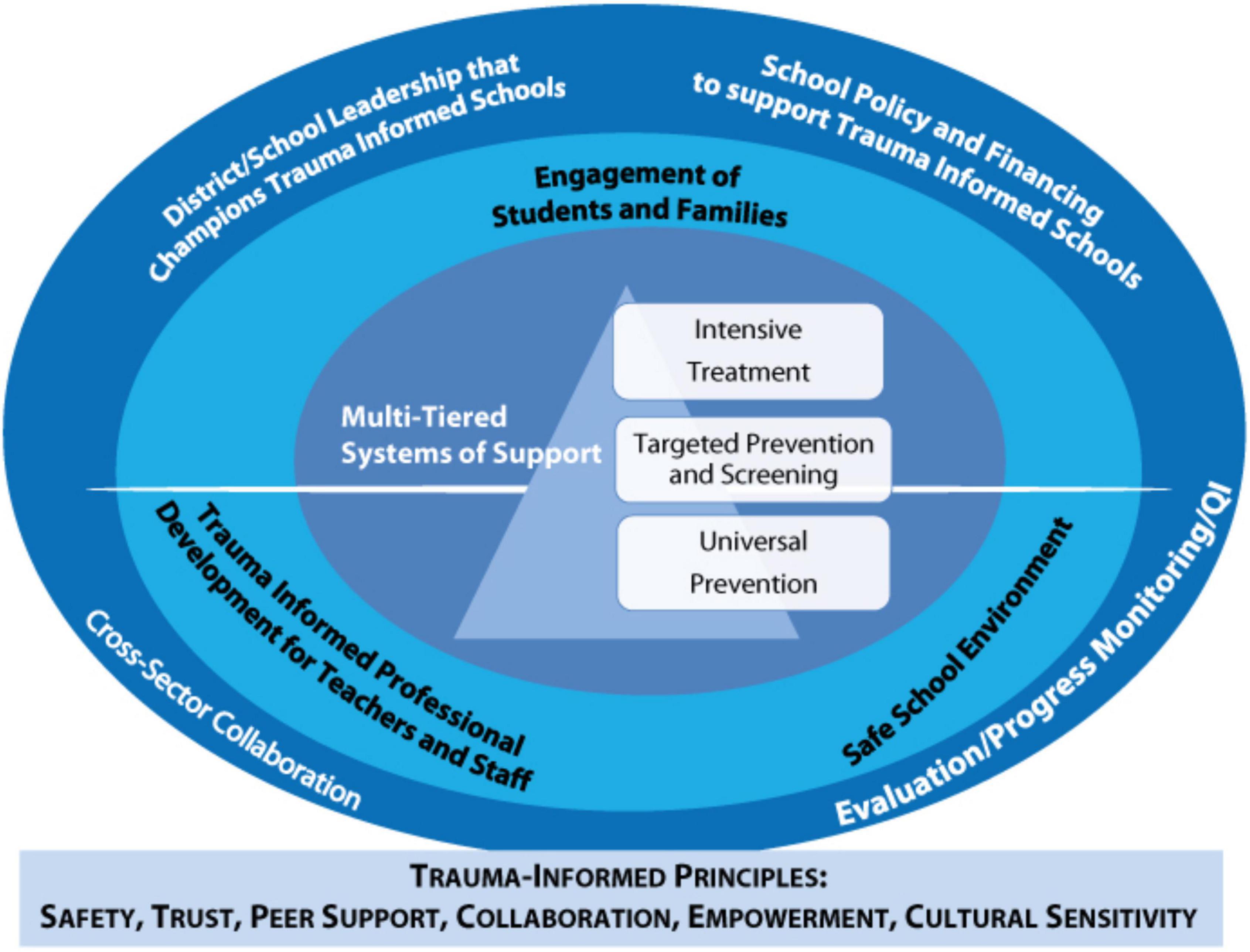
Figure 2. Consolidated Framework for Implementation Research (CFIR) to guide trauma-informed approaches in schools. This figure was adapted from SAMHSA’s concept of trauma and guidance for a trauma-informed approach and publication by Crosby (2015) and Kataoka et al. (2018).
The outermost circle of Figure 2 depicts all the macro levels of collaboration necessary for successful implementation of TIAs in Oklahoma. For context, recent data compiled from the 2019 National Survey of Children’s Health (NSCH) and Child and Adolescent Health Measurement Initiative (CAHMI) showed that 28.5% of children in Oklahoma have experienced 2 or more ACEs (United Health Foundation, 2022). Although down from 32.9% in 2016, Oklahoma remains the state with the highest prevalence of children experiencing two or more ACEs per capita (United Health Foundation, 2022). Thus, macro level recognition of ACEs is not only necessary but it’s congruent with the commonalities/facilitators theme: “organizational drivers of change.” In real-world translation, this means district leadership or school officials must simultaneously champion for trauma-informed schools, implement school-wide policy to support TIAs, and engage in cross sector collaboration with the community.
The next inner circle of Figure 2 underscores how trauma-informed practices within a school system might positively influence its culture, if done correctly. The culture of a school is affected by first and foremost, by having a safe environment to learn, high engagement levels from students (and their families), and ongoing professional activities for teachers and staff members to stay informed. It’s also important to recognize that the prevalence of ACEs is often layered with racial and ethnic disparities. As reported by the 2016 NSCH—63% of African American children and 51% of Hispanic children reported one or more ACEs compared to 41% of white children (Sacks and Murphey, 2018). Data from the 2011–2012 NSCH showed that Native American children were twice as likely than white children to have experienced 2 or more ACEs, 40% vs. 21% (Kenney and Singh, 2016). This inner circle is especially relevant for teachers and staff members who have not received training in responding to at-risk students, and/or feel poorly equipped to support students who have experienced adversities due to racial and ethnic inequalities (Baweja et al., 2016).
Children in the child welfare system, the juvenile justice system, and those living in poverty-stricken or violent neighborhoods are more likely to experience higher ACEs (Baglivio et al., 2014). One program called the Fragile Families and Child Wellbeing Study revealed that nearly 80% of children living in poverty-stricken environments had experienced at least one ACE by the age of five (Hunt et al., 2017). In Oklahoma, similar inequities attributable to historical, social, and economic environments exist against a backdrop of an even higher percentages of children living in poverty with learning disorders and developmental/behavioral issues (Larkin et al., 2014; Hunt et al., 2017). These psychosocial factors may coalesce and exacerbate the vicious cycle of ACEs among Oklahoman students (e.g., physical, sexual and emotional abuse; physical and emotional neglect; domestic violence; parental divorce; household mental illness; incarceration and substance abuse). Therefore, the innermost circle of the CFIR framework represents a multi-tiered systems of support (e.g., screenings, intensive treatments, targeted preventions, and interventions) that would theoretically be well-suited for modern day Oklahoman students with the highest needs.
Key implications for enhancing the field of education
Enhancing the quality of evidence for trauma-informed approaches
Martin et al. (2017) suggests that “becoming a trauma-informed school involves a shift in culture, practice, and theoretical framework” (Martin et al., 2017). Yet, there is currently no formally agreed upon framework for trauma-informed practices (Thomas et al., 2019) […] and the quality of existing empirical evidence for TIAs is surprisingly low. While there are numerous resources available on TIAs, literatures that can help to inform evidence-based practices to guide program implementation is not organized in a systematic manner (Cole et al., 2013). Educators seeking information for general TIAs, and practices might easily locate advocacy/policy recommendations, guides, toolkits, and best anecdotal practices. These resources frequently build upon existing literature created to support the initial push for integrating trauma-informed practices in schools, but few actually include high quality, externally validated empirical evidence to corroborate on those findings (Day et al., 2015).
Adopting more standardized trauma-informed terminologies
The GRADE-CerQual framework analysis revealed that a recurring weakness among TIAs in schools was the lack of “trauma-specific interventions and linked outcomes.” This point was highlighted in the challenges/barriers related to the implementation of TIAs in schools (refer to Supplementary Appendix Table A2). The overlapping terminologies and methodologies of trauma-informed approaches vs trauma-specific interventions are making it more challenging to connect the links between interventions and its expected outcomes. SAMHSA defines a trauma-informed approach (which the agency uses interchangeably with “trauma-informed care”) as incorporating key trauma principles into the organizational culture of the program, agency, or system (Crosby, 2015). In theory, a true TIA school is analogous to a multi-tiered framework and is based on incorporating four key elements and six principles, generalizable to any setting […] that are infused across all levels of an organization rather than just implementing a set of practices or interventions (Substance Abuse and Mental Health Services Administration, National Center for Trauma- Informed Care, 2015; Figure 1). A trauma-specific intervention, such as Trauma-Focused Cognitive Behavioral Therapy, is defined as an intervention used to treat trauma-related symptoms and disorders (Substance Abuse and Mental Health Services Administration, National Center for Trauma- Informed Care, 2015).
In essence, a trauma-informed approach is not a standalone intervention that can be delivered in silo, but rather a framework to help guide complex systems such as schools and learning agencies. A TIA can, however, include trauma-specific interventions, but these interventions are not seen as sufficient for achieving optimal outcomes or to influence service systems (Substance Abuse and Mental Health Services Administration, National Center for Trauma- Informed Care, 2015). What is essential to a TIA has not always been clearly operationalized, and previous adaptations have been referred to in varying terminologies (Maynard et al., 2019) (e.g., trauma-informed care, trauma-sensitive, trauma-informed system). At the time of writing, the author found no broad consensus on the use of these terminologies, which made efforts to assess, analyze, and evaluate the empirical evidence of TIAs in schools rather challenging.
Translating evidence of trauma-informed approaches in complex school systems
The casual loop diagram (shown in Supplementary Appendix Figure A1) depicts some of the positive and negative factors that can potentially complicate implementation of TIAs in complex school systems. These interdependent loops may provide additional nuanced insights as to why TIAs in modern school systems have low-quality empirical evidence and poor external validity (i.e., generalizability). The list of possible interdependent causal factors highlighted is not exhaustive. Caution is warranted when translating evidence of TIAs and applying those concepts into complex school systems, as mentioned earlier with the proxy example used for the state of Oklahoma. The iterative process to ideate, develop, implement, and maintain TIAs in schools may span over many years and will require a multi-pronged stepwise approach.
Firstly, implementing TIAs in schools require full buy-in from multiple stakeholders—students’ views, parents/caregivers, teachers, and staff and administrators—in addressing and responding to children’s potential traumatic stress (Halladay Goldman et al., 2020). Though not explicitly shown in this causal loop, the accuracy of future outcome results could be improved via the triangulation of data and cross verification from multiple stakeholders’ viewpoints.
Secondly, extra attention to program fidelity and research design (i.e., power of studies, larger sample sizes, longitudinal studies, reducing the risk of bias, etc.) is paramount in the pursuit of scaling programs and generating high-quality strong empirical evidence for TIAs. Given the inherent complexities of school systems (e.g., lack of resources/funding, scalability of programs, program fidelity, etc.), it would be especially challenging to apply the same rigor to studies in schools that do not lend themselves easily to the normal randomized clinical trials approach (Maynard et al., 2019). This is perhaps an avenue where future application of implementation science can help play a role to advance the translation of knowledge into practice (Proctor, 2012).
Careful integration of TIAs, positive (non-punitive) and restorative responses to problematic behaviors, system-wide policy and procedural changes (Oehlberg, 2008; Chafouleas et al., 2016), ongoing opportunities for teacher/school staff development, thoughtful considerations for multifaceted social contexts, and a strong cross-system collaboration among teachers, staff, and mental health professionals were some of the focus points highlighted in the GRADE CERqual analysis which received “moderate” to “high” confidence ratings.
Lastly, the schools/models selected for this review did not consistently reveal qualitative data on teacher feedback/communication. It was unclear whether teachers were provided with similar longitudinal feedback, or how that feedback may have influenced their trauma-informed teaching practices in the classroom settings. Ensuring that teachers, educators and staff members are given the same opportunities to provide/receive feedback, and likewise receive care for their own mental health/wellbeing is an essential area in complex school systems that can sometimes be overlooked. Future iterations of TIAs in schools should address teacher feedback/communication during the implementation phase by utilizing validated psychometric tools (e.g., identify personal needs/strengths, culture readiness for change, assess/re-assess teachers’ mindset, teaching pedagogies, etc.). The wellness of teachers and staff members can be supported by incorporating regular check-in protocols to help detect and respond to warning signs of secondary stress, while simultaneously providing them with equal access to non-judgmental support and stigma-free health services (Lever et al., 2017).
The current state of trauma-informed approaches in US schools
Even though there is a growing imperative among policymakers, state officials, researchers, educators, parents, and students want to increase the capacity of schools to address childhood trauma (Donisch et al., 2016), the current systematic review highlighted a lack of robust modern trauma-informed schools/models in the US. The assessment of overall impact was very constrained due to the limited details on data collection methodologies, small sample size of participants (across all four schools/models reviewed), lack of uniform control for confounders (e.g., pre-intervention self-esteem assessments, presence/absence of underlying psychological harm, or physical abuse and neglect, plus other psychosocial external influences in addition to the specific interventions), and scarcity of trauma-informed program evaluations. Based on the systematic analysis of available data findings, the author found the overall strength of evidence for trauma-informed schools/models was low. Future research effort and analysis of TIAs in schools must be guided by an awareness and understanding that complex issues of trauma will require more flexible, tailored, and nuanced approaches, which may (or may not) complicate traditional scientifically driven research protocols. Nevertheless, a concerted multidisciplinary effort is urgently needed to determine what TIAs will contribute to what specific outcomes, for which student(s) TIAs will benefit, and under what social contexts.
COVID-19 and parentally bereaved students
Childhood trauma has been labeled “America’s hidden public health crisis” because of its increased prevalence in children and teens (ACEs Connection, 2016). Over the past two and a half years, the ongoing COVID-19 pandemic has accelerated instances of childhood trauma, including separation from parents/caregivers, parental/caregiver loss of employment, and the death of loved ones. Tragically, at least 204,000 US children and teens have lost parents and other in-home caregivers due to COVID-19 related deaths—more than 1 in every 360 youth, according to COVID Collaborative, an interdisciplinary group of experts that is raising awareness and support for COVID-19 bereaved children (DeAngelis, 2022). At the moment, emerging TIAs are rapidly being implemented across a continuum from locally targeted trauma-specific interventions to more comprehensive trauma-informed schools/models like the ones chosen for review in this manuscript. Ongoing research and program design in this area should be guided by the acknowledgment that implementation of TIAs in (and through) complex school systems will require meticulous considerations to the individual school’s social contexts (Chafouleas et al., 2016). Moreover, the implementation process of TIAs will need to incorporate support programs for parentally bereaved children and teens either through brief evidence-based interventions and/or longer-term psychotherapy treatments during (and beyond) the COVID-19 pandemic.
Author contributions
The author is solely responsible for the conceptualization, curation, writing—draft preparation, policy analysis, and performing review/edit of this manuscript.
Acknowledgments
The author would like to thank Dr. Kristina Talbert-Slagle, Ph.D., Assistant Professor at the Yale School of Medicine; Associate Director of Faculty Mentorship and Academic Programs at the Yale Institute for Global Health, for her classroom instructions, mentorship and guidance.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/feduc.2022.1040980/full#supplementary-material
Footnotes
- ^ ACEs are divided into 3 categories: (1) childhood abuse (physical, emotional, sexual abuse), (2) childhood neglect (physical and emotional neglect), and (3) household/environmental challenges (parental separation/divorce, parent treated violently, household mental illness, drug/substance abuse, incarcerated relative).
- ^ Oklahoma, USA was used as a proxy pilot example due to its similarities in student demographics, higher prevalence of ACEs, and lack of existing integrated TIAs in schools.
References
ACEs Connection (2016). A community-of-practice social network. Childhood trauma: America’s hidden health crisis. Available online at: http://www.acesconnection.com/clip/childhood-trauma-america-s-hidden-health-crisis (accessed October 20, 2022).
Avery, J. C., Morris, H., Galvin, E., Misso, M., Savaglio, M., and Skouteris, H. (2020). Systematic review of school-wide trauma-informed approaches. J. Child Adolesc. Trauma 14, 381–397. doi: 10.1007/s40653-020-00321-1
Baglivio, M. T., Epps, N., Swartz, K., Huq, M. S., Sheer, A., and Hardt, N. S. (2014). The prevalence of adverse childhood experiences (ace) in the lives of juvenile offenders. J. Juv. Justice 3, 1–17.
Bateman, J., Henderson, C., and Kezelman, C. (2013). Trauma-informed care and practice: Towards a cultural shift in policy reform across mental health and human services in Australia. A national strategic direction. Position paper and recommendations of the National Trauma-Informed Care and Practice Advisory Working Group. Lilyfield, NSW: Mental Health Coordinating Council.
Baweja, S., Santiago, C. D., Vona, P., Pears, G., Langley, A., and Kataoka, S. (2016). Improving implementation of a school-based program for traumatized students: Identifying factors that promote teacher support and collaboration. School Ment. Health 8, 120–131. doi: 10.1007/s12310-015-9170-z
Bellis, M. A., Hughes, K., Hardcastle, K., Ashton, K., Ford, K., Quigg, Z., et al. (2017). The impact of adverse childhood experiences on health service use across the life course using a retrospective cohort study. J. Health Serv. Res. Policy 22, 168–177. doi: 10.1177/1355819617706720
Bellis, M. A., Hughes, K., Leckenby, N., Hardcastle, K. A., Perkins, C., and Lowey, H. (2015). Measuring mortality and the burden of adult disease associated with adverse childhood experiences in England: A national survey. J. Public Health 37, 445–454. doi: 10.1093/pubmed/fdu065
Bethell, C. D., Davis, M. B., Gombojav, N., Stumbo, S., and Powers, K. (2017). A national and across state profile on adverse childhood experiences among children and possibilities to heal and thrive. Available online at: http://www.cahmi.org/projects/adverse-childhood-experiences-aces/ (accessed March 8, 2022).
Boxley, B. (2018). Child attachment style as a predictive factor for internalization and externalization of witnessing community violence. Psychology 9, 578–587. doi: 10.4236/psych.2018.94036
Brunzell, T., Waters, L., and Stokes, H. (2015). Teaching with strengths in trauma-affected students: A new approach to healing and growth in the classroom. [Miscellaneous]. Am. J. Orthopsychiatry 85, 3–9. doi: 10.1037/ort0000048
Burke, N. J., Hellman, J. L., Scott, B. G., Weems, C. F., and Carrion, V. G. (2011). The impact of adverse child- hood experiences on an urban pediatric population. Child Abuse Negl. 35, 408–413. doi: 10.1016/j.chiabu.2011.02.006
Centers for Disease Control and Prevention (2019a). Preventing adverse childhood experiences (ACEs) to improve U.S. health. Available online at: https://www.cdc.gov/media/releases/2019/p1105-prevent-aces.html (accesses March 8, 2022).
Centers for Disease Control and Prevention (2019b). Preventing adverse childhood experiences (ACEs): Leveraging the best available evidence. Available online at: https://www.cdc.gov/violenceprevention/pdf/preventingACES.pdf (accessed March 9, 2022).
Chafouleas, S. M., Johnson, A. H., Overstreet, S., and Santos, N. M. (2016). Toward a blueprint for trauma-informed service delivery in schools. Sch. Ment. Health 8, 144–162. doi: 10.1007/s12310-015-9166-8
Chapman, D. P., Whitfield, C. L., Felitti, V. J., Dube, S. R., Edwards, V. J., and Anda, R. F. (2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. J. Affect. Disord. 82, 217–225. doi: 10.1016/j.jad.2003.12.013
Chartier, M. J., Walker, J. R., and Naimark, B. (2010). Separate and cumulative effects of adverse childhood experiences in predicting adult health and health care utilization. Child Abuse Negl. 34, 454–464. doi: 10.1016/j.chiabu.2009.09.020
Chriqui, J., Stuart-Cassel, T., Piekar-Porter, E., Temkin, D., Lao, K., Steed, H., et al. (2019). Using state policy to create healthy schools: Coverage of the whole school, whole community, whole child framework in state statutes and regulations, school year 2017–2018. Bethesda, MD: Child Trends.
Cole, S. F., Eisner, A., Gregory, M., and Ristuccia, J. (2013). Helping traumatized children learn: Creating and advocating for trauma-sensitive schools. Boston, MA: Massachusetts Advocates for Children.
Cole, S. F., O’Brien, J. G., Gadd, M. G., Ristuccia, J., Wallace, D. L., and Gregory, M. (2005). Helping traumatized children learn: Supportive school environments for children traumatized by family violence. Boston, MA: Massachusetts Advocates for Children.
Cook, A., Blaustein, M., Spinazzola, J., and van der Kolk, B. (Eds). (2003). Complex trauma in children and adolescents. Los Angeles, CA: National Child Traumatic Stress Network. doi: 10.1037/e404122005-001
Crosby, S. D. (2015). An ecological perspective on emerging trauma-informed teaching practices. Child. Sch. 37, 223–230. doi: 10.1093/cs/cdv027
Damschroder, L. J., Aron, D. C., Keith, R. E., Kirsh, S. R., Alexander, J. A., and Lowery, J. C. (2009). Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement Sci. 7:50. doi: 10.1186/1748-5908-4-50
Day, A., Somers, C., Baroni, B., West, S., Sanders, L., and Peterson, C. (2015). Evaluation of a trauma-informed school intervention with girls in a residential facility school: Student perceptions of school environment. J. Aggress. Maltreat. Trauma 24, 1086–1105. doi: 10.1080/10926771.2015.1079279
DeAngelis, T. (2022). Thousands of kids lost loved ones to the pandemic. Psychologists are teaching them how to grieve, and then thrive, Vol. 53. Washington, D.C: American Psychological Association, 69.
Donisch, K., Bray, C., and Gewirtz, A. (2016). Child welfare, juvenile justice, mental health, and education providers’ conceptualizations of trauma-informed practice. Child Maltreat. 21, 125–134. doi: 10.1177/1077559516633304
Dorado, J. S., Martinez, M., McArthur, L. E., and Liebovitz, T. (2016). Healthy environments and response to trauma in schools (HEARTS): A school-based, multi-level comprehensive prevention and intervention program for creating trauma-informed, safe and supportive schools. Sch. Ment. Health 8, 144–162. doi: 10.1007/s12310-016-9177-0
Felitti, V. J. (2002). The relation between adverse childhood experiences and adult health: Turning gold into lead. Perm. J. 6, 44–47. doi: 10.7812/TPP/02.994
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. Am. J. Prev. Med. 14, 245–258. doi: 10.1016/S0749-3797(98)00017-8
Figlio, A., Karbownik, K., and Salvanes, K. (2017). The promise of administrative data in education research. Educ. Finance Policy 12, 129–136. doi: 10.1162/EDFP_a_00229
Finkelhor, D., Turner, H. A., Shattuck, A., and Hamby, S. L. (2015). Prevalence of childhood exposure to violence, crime, and abuse: Results from the national survey of children’s exposure to violence. JAMA Pediatr. 169, 746–754. doi: 10.1001/jamapediatrics.2015.0676
Fondren, K., Lawson, M., Speidel, R., McDonnell, C. G., and Valentino, K. (2020). Buffering the effects of childhood trauma within the school setting: A systematic review of trauma-informed and trauma-responsive interventions among trauma-affected youth. Child. Youth Serv. Rev. 109:104691. doi: 10.1016/j.childyouth.2019.104691
Halladay Goldman, J., Danna, L., Maze, J. W., Pickens, I. B., and Ake, G. S. I. I. I. (2020). Trauma-Informed school strategies during COVID-19. Los Angeles, CA: National Child Traumatic Stress Network.
Harris, M., and Fallot, D. (2001). Trauma-informed inpatient services. New Direct. Ment. Health Serv. 2001, 33–46. doi: 10.1002/yd.23320018905
Hunt, T. K., Slack, K. S., and Berger, L. M. (2017). Adverse childhood experiences and behavioral problems in middle childhood. Child Abuse Negl. 67, 391–402. doi: 10.1016/j.chiabu.2016.11.005
Kataoka, S. H., Vona, P., Acuna, A., Jaycox, L., Escudero, P., Rojas, C., et al. (2018). Applying a trauma informed school systems approach: Examples from school community-academic partnerships. Ethn. Dis. 28(Suppl 2), 417–426. doi: 10.18865/ed.28.S2.417
Kenney, M. K., and Singh, G. K. (2016). Adverse childhood experiences among American Indian/Alaska native children: The 2011-2012 national survey of children’s health. Scientifica 2016:7424239. doi: 10.1155/2016/7424239
Ko, S. J., Ford, J. D., Kassam-Adams, N., Berkowitz, S. J., Wilson, C., Wong, M., et al. (2008). Creating trauma-informed systems: Child welfare, education, first responders, health care, juvenile justice. Prof. Psychol. Res. Pract. 39, 396–404. doi: 10.1037/0735-7028.39.4.396
Kress, J. S., and Elias, M. J. (2006). “School-based social and emotional learning programs,” in Handbook of child psychology: Child psychology in practice, eds K. A. Renninger, I. E. Sigel, W. Damon, and R. M. Lerner (New York, NY: John Wiley & Sons Inc.), 592–618. doi: 10.1002/9780470147658.chpsy0415
Lang, J. M., Campbell, K., and Vanderploeg, J. J. (2015). Advancing trauma- informed systems for children. Farmington, CT: Child Health and Development Institute.
Larkin, H., Felitti, V. J., and Anda, R. F. (2014). Social work and adverse childhood experiences research: Implications for practice and health policy. Soc. Work Public Health 29, 1–16. doi: 10.1080/19371918.2011.619433
Lever, N., Mathis, E., and Mayworm, A. (2017). School mental health is not just for students: Why teacher and school staff wellness matters. Rep. Emot. Behav. Disord. Youth 17, 6–12.
Martin, S. L., Ashley, O. S., White, L., Axelson, S., Clark, M., and Burrus, B. (2017). Incorporating trauma-informed care into school-based programs. J. Sch. Health 87, 958–967. doi: 10.1111/josh.12568
Maynard, B. R., Farina, A., Dell, N. A., and Kelly, M. S. (2019). Effects of trauma-informed approaches in schools: A systematic review. Campb. Syst. Rev. 15:e1018. doi: 10.1002/cl2.1018
Metzler, M., Merrick, M. T., Klevens, J., Ports, K. A., and Ford, D. C. (2017). Adverse childhood experiences and life opportunities: Shifting the narrative. Child. Youth Serv. Rev. 72, 141–149. doi: 10.1016/j.childyouth.2016.10.021
Moore, K. A., and Ramirez, A. N. (2016). Adverse childhood experience and adolescent well-being: Do protective factors matter? Child Indic. Res. 9, 299–316. doi: 10.1007/s12187-015-9324-4
Parris, S. R., Dozier, M., Purvis, K. B., Whitney, C., Grisham, A., and Cross, D. R. (2015). Implementing trust-based relational intervention in a charter school at a residential facility for at-risk youth. Contemp. Sch. Psychol. 19, 157–164. doi: 10.1007/s40688-014-0033-7
Pennsylvania Commission on Crime and Delinquency School Safety and Security Committee (2019). Model trauma-informed approach plan: Guidelines for school entities. Available online at: https://www.pccd.pa.gov/schoolsafety/Pages/Model-Trauma-Informed-Approach-Plan.aspx (accessed March 10, 2022).
Perry, D. L., and Daniels, M. L. (2016). Implementing trauma-informed practices in the school setting: A pilot study. Sch. Ment. Health 8, 177–188. doi: 10.1007/s12310-016-9182-3
Proctor, E. (2012). Implementation science and child maltreatment. Child Maltreat. 17, 107–112. doi: 10.1177/1077559512437034
Reavis, J. A., Looman, J., Franco, K. A., and Rojas, B. (2013). Adverse childhood experiences and adult criminality: How long must we live before we possess our own lives? Perm. J. 17, 44–48. doi: 10.7812/TPP/12-072
Sacks, V., and Murphey, D. (2018). The prevalence of adverse childhood experiences, nationally, by state, and by race or ethnicity. Bethesda, MD: Child Trends Publication.
Sameroff, A., Gutman, L. M., and Peck, S. C. (2003). “Chap. 15: Adaptation among youth facing multiple risks: Prospective research findings,” in Resilience and vulnerability: Adaptation in the context of childhood adversities, ed. S. S. Luthar (New York, NY: Cambridge University Press), 364–391. doi: 10.1017/CBO9780511615788.017
Shonkoff, J. P., and Garner, A. S., Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, and Section on Developmental and Behavioral Pediatrics (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics 129, e232–e246. doi: 10.1542/peds.2011-2663
Substance Abuse and Mental Health Services Administration, National Center for Trauma- Informed Care (2015). Trauma-informed approach. Available online at: https://store.samhsa.gov/sites/default/files/d7/priv/sma14-4884.pdf (accessed March 11, 2022).
Thomas, M. S., Crosby, S., and Vanderhaar, J. (2019). Trauma-informed practices in schools across two decades: An interdisciplinary review of research. Rev. Res. Educ. 43, 422–452. doi: 10.3102/0091732X18821123
United Health Foundation (2022). America’s Health Rankings analysis of U.S. HHS, HRSA, Maternal and Child Health Bureau (MCHB), Child and Adolescent Health Measurement Initiative (CAHMI), National Survey of Children’s Health Indicator Data Set, Data Resource Center for Child and Adolescent Health. United Health Foundation. Available online at: https://AmericasHealthRanking.org (accessed March 8, 2022).
Keywords: adverse childhood experiences, trauma-informed approaches, childhood early intervention, GRADE-CERQual, CFIR framework
Citation: Phung B (2022) Potential challenges and future implications for trauma-informed approaches in schools. Front. Educ. 7:1040980. doi: 10.3389/feduc.2022.1040980
Received: 09 September 2022; Accepted: 04 November 2022;
Published: 28 November 2022.
Edited by:
Waganesh A. Zeleke, Duquesne University, United StatesReviewed by:
Siobhan Hugh-Jones, University of Leeds, United KingdomSharinaz Hassan, Curtin University, Australia
Copyright © 2022 Phung. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Binh Phung, YmluaC5waHVuZ0B5YWxlLmVkdQ==
 Binh Phung
Binh Phung