
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Educ., 21 November 2022
Sec. Digital Education
Volume 7 - 2022 | https://doi.org/10.3389/feduc.2022.1025600
This article is part of the Research TopicEducational Digital Transformation: New Technological Challenges for Competence DevelopmentView all 22 articles
 Aidos K. Bolatov1,2*
Aidos K. Bolatov1,2* Telman Z. Seisembekov1
Telman Z. Seisembekov1 Ernur Dauyenov3
Ernur Dauyenov3 Meiramgul D. Zhorokpayeva4
Meiramgul D. Zhorokpayeva4 Dariga S. Smailova5
Dariga S. Smailova5 Dainius Pavalkis6
Dainius Pavalkis6Background: The coronavirus disease (COVID-19) pandemic has affected medical education and psychosomatic health of medical students. In this follow-up study, conducted 1 year after the transition to online learning (OL), we aimed to investigate changes in student mental health and identify factors associated with academic burnout and changes in medical education caused by the pandemic.
Materials and methods: This study compares the burnout rate and psychosomatic status (depression, anxiety, somatic symptoms) of medical students at Astana Medical University using an online questionnaire-based repeated cross-section design of the pre-pandemic period (September–November 2019), the initial period of the pandemic (April 2020), and the current study (March 9–30, 2021). In the pre-pandemic period, students studied only in a face-to-face format. Moreover, the current study (March, 2021) analyzed factors associated with academic burnout and changes in medical education caused by the pandemic. Statistical methods included mean comparison, frequency, and regression analysis.
Results: Data from a representative sample of undergraduate students were analyzed (n = 975, 58% of them participated in the previous study). The burnout rate was found to be lower compared with the period of traditional education (pre-COVID-19) and did not significantly differ from the initial period of the introduction of online learning (the initial period of the COVID-19 pandemic). The levels and prevalence of depression and anxiety also showed similar patterns. The prevalence of somatic symptoms has increased compared to the initial period of the pandemic, although it has not reached the level obtained in the pre-COVID-19 period. The negative changes caused by OL in medical education and learning effectiveness have been associated with burnout. Factors associated with burnout, learning effectiveness, dissatisfaction with the quality of OL organization, and deterioration of medical education have been identified.
Conclusion: The medical education and mental health of medical students has undoubtedly undergone changes in the transition to OL due to the COVID-19 pandemic. Factors such as changing the content of education, the organization of the educational process and support from the school, the nature of student-teacher, student-school and student-student relationships, the possibility of mastering various skills and financial problems caused by the pandemic, played a significant role in the academic life of students. The results obtained have potential applications in organizing and improving the quality of continuing medical education in an era of global healthcare crises such as the COVID-19 pandemic.
Relating to the coronavirus disease (COVID-19) pandemic, all medical schools moved to online learning (OL) format. The pandemic has led to unprecedented disruptions in medical training (Yuen and Xie, 2020). Given the low-quality evidence for OL efficacy in medical education (Kyaw et al., 2019) and the sudden enforced transition, medical students have had to adapt to OL in difficult situations. Moreover, it is known that the mental health status of medical students is already poorer than that of the general population, and academic stress is a major predictor, therefore such changes are likely to have a significant impact on these students (O’Byrne et al., 2021). It is also noted that high levels of perceived stress and burnout are inevitable during a pandemic, and OL can contribute to their strengthening (Silistraru et al., 2022).
The COVID-19 pandemic has exacerbated the mental health problems seen globally (Wu et al., 2021), including among medical students; the prevalence of depression, anxiety, and stress has increased during the pandemic (Huckins et al., 2020; Islam et al., 2020; Lyons et al., 2020; Saraswathi et al., 2020; Wang et al., 2020; Ihm et al., 2021; Li et al., 2021; Nikolis et al., 2021). There was a significant association between reporting stress and transition to OL and online assessment formatting. And those who reported that lower levels of stress are associated with an adequate response of the medical school to the crisis, shows the importance of medical school’s programs to manage the COVID-19 pandemic-related changes in education (O’Byrne et al., 2021). The changes in the psychosomatic state of students during a pandemic may be caused by social distancing, self-isolation, financial hardship, academic delays, worry about family member’s health, and social media exposure (Nurunnabi et al., 2021; Patwary et al., 2022).
In one of the studies in Cyprus, the authors argued that OL was associated with significant risks, namely the deterioration of mental health, and as a component of burnout, the level of cynicism increased due to the COVID-19 pandemic (Zis et al., 2021). Simultaneously, Lasheras et al. (2020) found no change in the prevalence of anxiety before and during the pandemic, although anxiety was correlated with COVID-19 stressors. Moreover, Pereira et al. (2022) resulted stability in medical students’ mental health. A recent meta-analysis found a lower overall prevalence of student burnout during the COVID-19 pandemic (11.5%) compared to the overall prevalence of student burnout (12.2%) before the pandemic (Kaggwa et al., 2021). For instance, a study from Croatia indicates that the transition to OL did not affect the level of emotional burnout among medical students or their perception of their curriculum (Žuljević et al., 2021).
Previous research conducted in April 2020 indicated a decreasing prevalence and level of burnout, depression, anxiety, and somatic symptoms after transitioning to OL (Bolatov et al., 2021a). However, this study was conducted in the early stages of a pandemic and therefore has several limitations (Pereira et al., 2022). Moreover, there is a need for more information on the long-term effects of the COVID-19 pandemic on medical students and their education (Žuljević et al., 2021). In this regard, we aimed to investigate changes in students’ mental health a year after the transition to OL and identify factors associated with academic burnout and changes in medical education caused by the pandemic.
This study compares the burnout level and psychosomatic status of undergraduate medical students through a repeated cross-sectional design based on online questionnaire at Astana Medical University: Time 1 for pre-pandemic (September–November 2019), Time 2 for the initial period of pandemic (April 2020) (Bolatov et al., 2021a), and Time 3 for the current study (March 9–30, 2021). The study participants received invitations via the different “messenger” apps to complete an online survey created on the 1ka platform.1 Participation in the study was voluntary and all students had the opportunity to get acquainted with the study aim and objectives. After reading the information about the study, students were asked to go to the next page, thereby expressing their informed consent to participation. By blocking repeated IP addresses, the study was protected from duplicate responses.
At the time of the study (Time 3), 3,989 undergraduates (1–5-year of study) were learning at the university. During the study, we received answers from 1,419 students, among whom 975 completed the survey (response rate = 68.7%).
On average, respondents spent 18 min on a survey that included the following tools and measures:
• Sociodemographic data: sex, age, year of study, living conditions, part-time job (medical and non-medical), volunteering associated with COVID-19, diagnosis of COVID-19, and participation in a previous study conducted in April 2020.
• Questionnaire regarding variables related to education during the COVID-19 pandemic: satisfaction with online learning (OL) format, attitudes of students toward training during a pandemic, and changes in learning associated with the transition to OL. Satisfaction with the quality of the OL organization was assessed using a 5-point Likert type scale; the responses “Dissatisfied” and “Very dissatisfied” indicated dissatisfaction. Students’ attitudes toward OL were assessed using a 5-point Likert type scale; the responses “Agree” and “Strongly agree” indicated agreement. The change in learning associated with the transition to OL and deterioration in learning efficiency was assessed using a 5-point Likert scale; the responses “Deterioration” and “Considerable deterioration” were used to determine negative changes.
• Fear of COVID-19: Fear of COVID-19 was assessed using a 3-item adapted Snell’s questionnaire (Snell’s questionnaire regarding fear of AIDS) (Snell and Finney, 1998; Bolatov et al., 2021a). The questionnaire included the following: “Thinking about COVID-19 makes me feel anxious”; “I feel tense when I think about the threat of COVID-19”; and “I feel quite anxious about the possibility of another outbreak of COVID-19.” Each question had five possible answers and ratings ranging from 1 (not at all) to 5 (very).
• Academic burnout: The Copenhagen Burnout Inventory developed by Kristensen et al. (2005), adapted for students by Campos, Carlotto, and Maroco (CBI-S) (Campos et al., 2013), and translated and validated by authors (Bolatov et al., 2021b) with a cut-off point of >50 (Borritz et al., 2006), was used to assess burnout syndrome. A feature of this scale is the measurement of exhaustion in four life-domains: Personal Burnout (PB), Studies-related Burnout (SRB), Colleague-related Burnout (CRB), and Teacher-related Burnout (TRB).
• Psychosomatic state: The Patient Health Questionnaire-9 (PHQ-9) contains nine items and assesses symptoms of depression based on symptoms over a 2-week period. The total PHQ-9 score ranges from 0 to 27 (Kroenke and Spitzer, 2002). The Generalized Anxiety Disorder 7-item scale (GAD-7) was used to assess anxiety symptoms, with total scores ranging from 0 to 21 (Spitzer et al., 2006). Somatic symptoms were investigated using the Patient Health Questionnaire-15 (PHQ-15), which consists of 15 somatic symptoms with scores ranging from 0 to 30 (Kroenke et al., 2002). Higher scores on these scales reflect higher severity levels of depressive symptoms, anxiety, and somatic symptoms, respectively, with a cutoff point of >10 (Kroenke et al., 2010). Translated versions of the PHQ-9, GAD-7, and PHQ-15 scales were obtained from the www.phqscreeners.com.
Sociodemographic data and respondents’ answers on the CBI-S, PHQ-9, GAD-7, and PHQ-15 scales were collected at all time intervals (Time 1–3), while fear of COVID-19 was assessed only during the initial period of the pandemic (Time 2) and in the current study (Time 3). Internal consistencies of the scales at Time 3 were reliable to excellent: Cronbach’s α for fear of COVID-19 (0.886), CBI-S (0.939), PHQ-9 (0.906), GAD-7 (0.924), and PHQ-15 (0.881) (Taber, 2018).
Statistical analysis was performed using IBM SPSS Statistics 20.0 and Jamovi version 1.6.16.0. Statistics included descriptive methods [frequency, means (M), and standard deviations (SD)], comparative analysis using the t-test or ANOVA with the Bonferroni post-hoc test (when more than two groups were compared, e.g., any scale in three times), frequency analysis, and determination of independent associations between variables using chi-square and regression analysis. A mediation model was applied to explore the pathway from dissatisfaction with the quality of OL organization via different factors related to OL to academic burnout. The level of statistical significance adopted was 5% (p < 0.05).
A representative sample of 975 respondents was obtained; among them, 569 (58.5%) participated in the previous study (Time 2). Sociodemographic characteristics of the study population are presented in Table 1. The study included 753 (77.2%) female students and 222 (22.8%) male students. The average age was 19.9 (SD = 1.94).
The overall prevalence of burnout was 15.3%: PB (40.2%), SRB (40.0%), CRB (11.2%), and TRB (17.4%), with average scores 43.1 (SD = 21.9) for PB, SRB – 43.5 (SD = 22.3), CRB – 20.0 (SD = 21.4), TRB – 25.1 (SD = 21.8), and 32.9 (SD = 31.4) for CBI. There were no significant gender and academic year differences in burnout prevalence; however, females had 1.288 times more often PB and 1.302 times more often SRB (p < 0.05) than male students. The prevalence of burnout in the three time periods with distributions by burnout dimensions, year of study, and sex are illustrated in Figure 1.
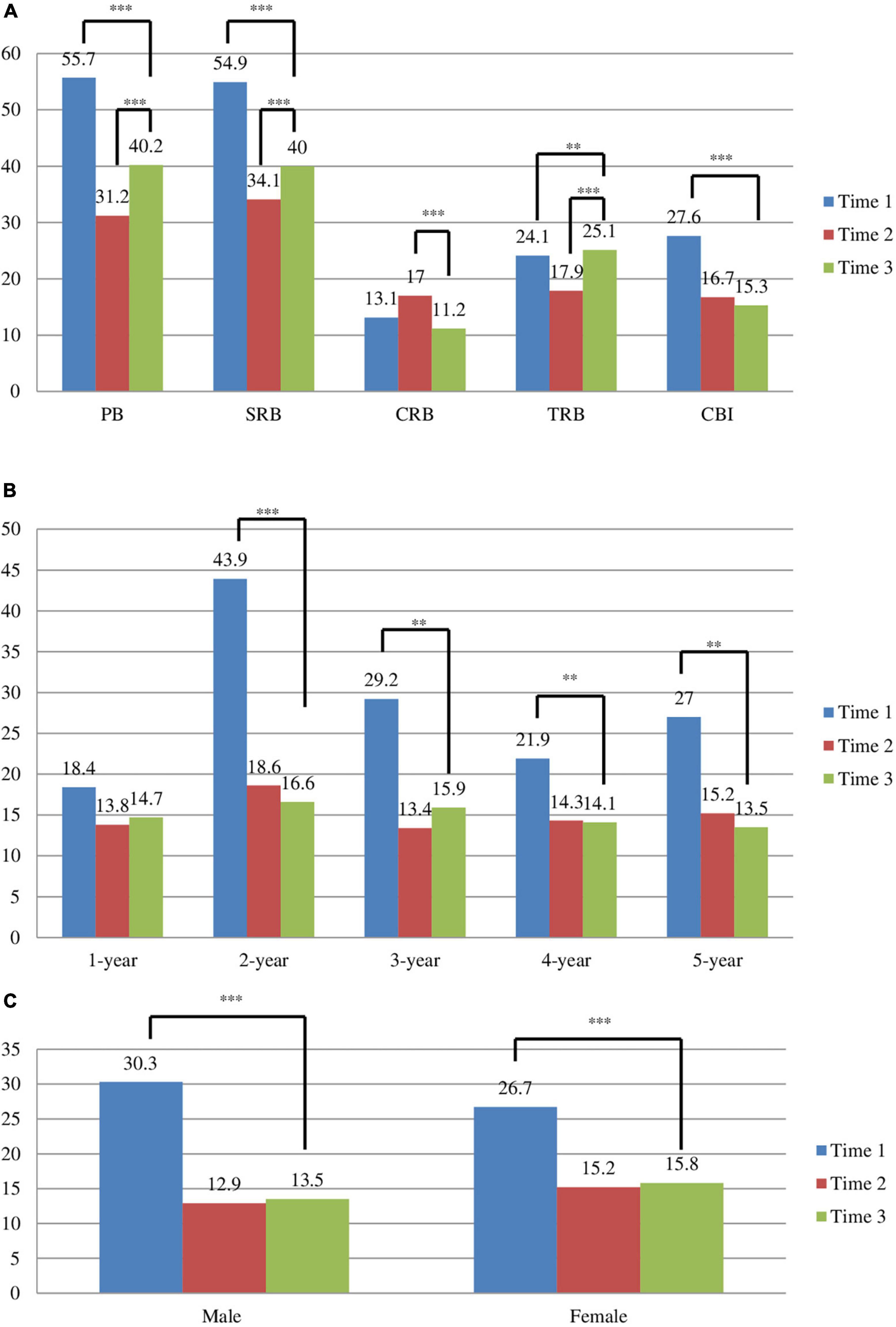
Figure 1. The prevalence of burnout and CBI mean scores before OL (Time 1), in initial period of online learning (OL) (Time 2) and after 1 year of OL (Time 3) caused by the COVID-19 pandemic distributed by: (A) CBI dimensions; (B) years of study; (C) gender. Data on burnout prevalence in Time 1 and Time 2 based on previous research (Bolatov et al., 2021a). **p < 0.05, ***p < 0.001.
The burnout rate did not depend on living conditions; however, respondents living alone (M = 33.3, SD = 33.9) demonstrated a higher level of CRB than those who lived with their parents (M = 19.7, SD = 21.1) or friends (M = 15.1, SD = 12.7), p < 0.05. Non-medical part-time job students showed higher level of burnout in all dimensions compared to students with no job: CBI (39.8 vs. 31.0), PB (49.1 vs. 41.2), SRB (50.7 vs. 41.5), CRB (26.9 vs. 18.4), and TRB (32.2 vs. 23.0), p < 0.001. Simultaneously, the level of burnout among participants with medical part-time jobs did not differ from that of the unemployed. Volunteering during the pandemic did not affect the level or prevalence of burnout. Confirmed and suspected diagnoses of COVID-19 were associated with PB in reference to not diagnosed (rate ratio = 1.545**; 1.281*), SRB (RR = 1.291*; 1.125), TRB (RR = 1.532*; 1.536*), and CBI (RR = 1.527*; 1.354), respectively (note: *, p < 0.05; **, p < 0.001).
The average PHQ-9 score at Time 3 was 7.56 (SD = 6.17). Compared to Time 3 at Time 1, the PHQ-9 level was 10.46 (SD = 6.76) and 7.13 at Time 2 (SD = 5.96). Post-hoc tests revealed significant differences in PHQ-9 levels between Time 1 and Time 2 and Time 1 vs. Time 3 (p < 0.001). The prevalence of depression was 24.9%, according to severity, as follows: minimal, 37.0%; mild, 34.8%; moderate, 14.7%; moderately severe, 7.3%; and severe, 6.2%. The mean value of the PHQ-9 at Time 3 was higher among female students (M = 7.88, SD = 6.28) than among males (M = 6.45, SD = 5.67), p < 0.05.
GAD-7 average value at Time 1 was 7.80 (SD = 5.93), 4.78 at Time 2 (SD = 4.99), and 5.33 at Time 3 (SD = 5.19). Post-hoc tests revealed significant differences in GAD-7 levels between Time 1 and Time 2 and Time 1 vs. Time 3 (p < 0.001). In this study, the prevalence of anxiety was 15.1% and was distributed by severity as follows: minimal, 58.9%; mild, 26.05%; moderate, 9.0%; and severe, 6.05%. The mean value of GAD-7 at Time 3 was higher among female students (M = 5.60, SD = 5.23) than among male students (M = 4.44 SD = 4.94), p < 0.05.
The PHQ-15 scale average value in Time 1 was 11.75 (SD = 5.89), 5.41 at Time 2 (SD = 5.16), and 7.86 at Time 3 (SD = 5.72); post-hoc test revealed significant differences in all comparisons (p < 0.001). The mean value of GAD-7 at Time 3 was higher among female students (M = 8.52, SD = 5.68) than males (M = 5.62, SD = 5.28), p < 0.001. Moreover, somatic symptoms were more prevalent among females (33.2%) than that for males (16.7%) (χ2 = 22.6, p < 0.001).
Figure 2 demonstrated average values of PHQ-9, GAD-7, PHQ-15, and prevalence somatic symptoms.
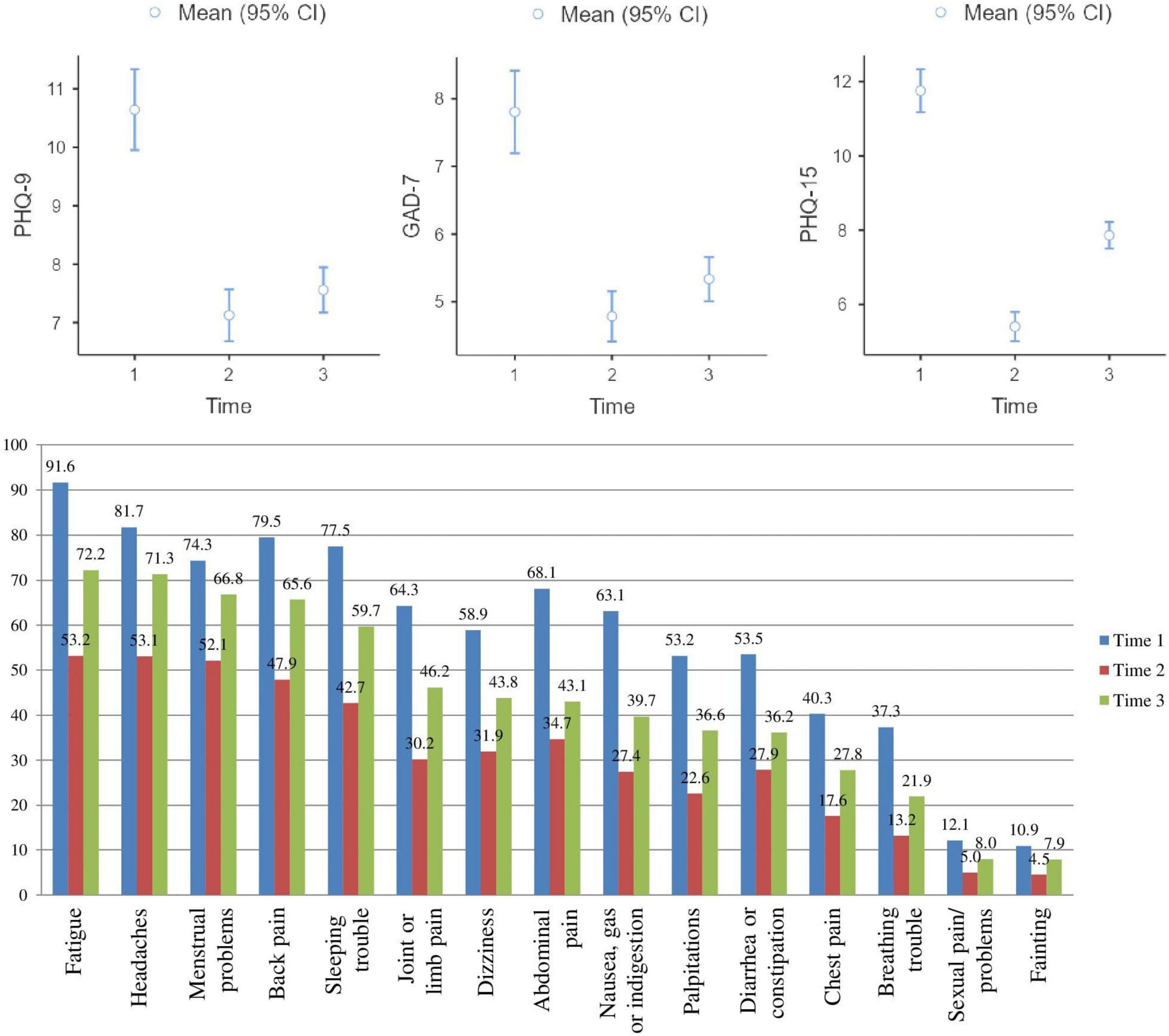
Figure 2. Average values in PHQ-9, GAD-7, and PHQ-15 scale, and prevalence of somatic symptoms in Time 1, 2, and 3.
The average value for fear of COVID-19 was 2.91 (SD = 1.25). Female students demonstrated higher levels of fear than males (M = 2.98, SD = 1.22 vs. M = 2.68, SD = 1.32, p < 0.05). Volunteering students (M = 3.22, SD = 1.30 vs. M = 2.87, SD = 1.23, p < 0.05) and those diagnosed with COVID-19 (M = 3.14, SD = 1.22 vs. M = 2.89, SD = 1.23, p < 0.05) had more pronounced fear. Of the respondents, 52.5% experienced fear of COVID-19. Moreover, the mean on the fear scale was higher at Time 3 than at Time 2 (M = 2.91, SD = 1.25 vs. M = 2.61, SD = 1.25, p < 0.001). The correlations among the main indicators used in this study are presented in Table 2.
Of the students, 719 (73.7%) were satisfied with their academic performance. Students were asked, “How has your academic performance changed after switching to online learning?” The responses were as follows. Of the students, 348 (35.7%) indicated that their academic performance improved after switching to OL; 167 (17.1%) noted deterioration, and 460 (47.2%) did not change. Among those who indicated that the transition to OL improved their academic performance, 256 (73.5%) indicated that their studying improved during the OL period; 26 (7.5%) responded that improvements in academic performance were associated with higher scores during OL compared with TL; 35 (10.1%) indicated both reasons; and 31 (8.9%) did not indicate either. Students who responded that their academic performance deteriorated with the transition to OL indicated the following reasons: 70 (41.9%) found their studies worsened, 49 (29.3%) felt teachers began giving lower grades, 22 (13.2%) indicated both reasons, and 26 (15.6%) did not indicate either. Of the participants, 378 (38.8%) experienced OL difficulties. Of the students, 736 (75.5%) indicated that they were satisfied with the quality of the OL organization. Dissatisfaction with academic performance and OL quality were associated with burnout (RR = 2.06 and 1.83, respectively; p ≤ 0.001), while dissatisfaction with academic performance was associated with depression (RR = 1.16, p < 0.05). However, changes in academic performance were not found to be associated with burnout, depression, or anxiety. However, any change in academic performance, such as deterioration (RR = 1.57) or improvement (RR = 1.75), was significantly associated with TRB (p < 0.05).
Table 3 presents data on students’ agreement with certain statements according to the OL during the COVID-19 pandemic, as well as their relationship with burnout and dissatisfaction with the quality of the OL organization, calculated using regression analysis. Examining these items as mediators between OL dissatisfaction and burnout (Figure 3), Items 1 and 8 showed statistically significant effects at a level of p < 0.001.
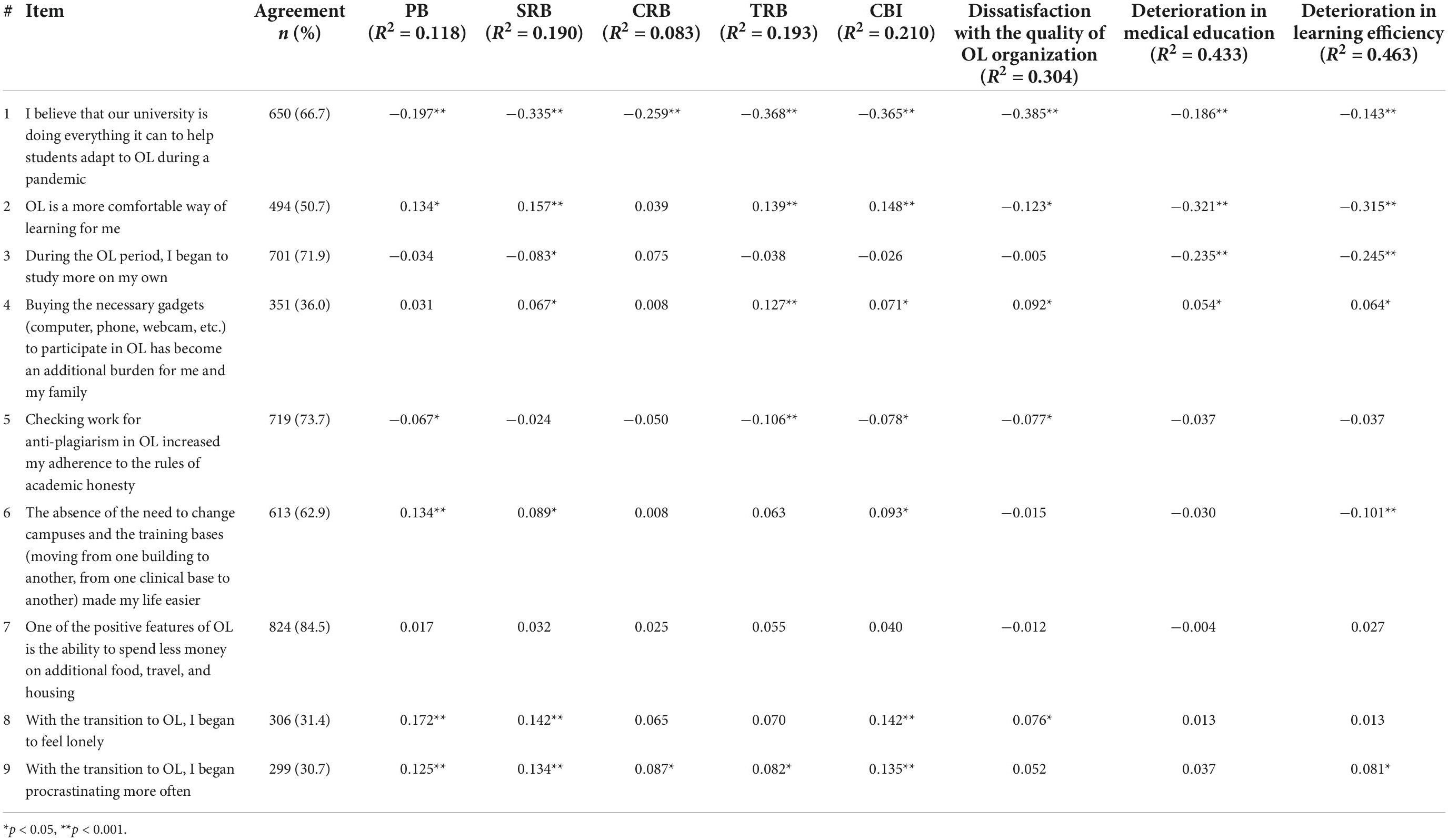
Table 3. The degree of students’ agreement with statements about OL during the COVID-19 pandemic and their association with burnout, dissatisfaction with the quality of OL organization, and deterioration in medical education and learning efficiency on linear regression analysis (N = 975).

Figure 3. Mediating effect of university support and loneliness in the relation between dissatisfaction with OL and academic burnout (N = 975) during the COVID-19 pandemic. Note: all significance level at p < 0.001; all presented effects are unstandardized; a1 – the effect of dissatisfaction with OL on university support; b1 – the effect of academic life satisfaction on academic burnout; a2 – the effect of dissatisfaction with OL on loneliness; b2 – the effect of loneliness on academic burnout; c’ is the direct effect of dissatisfaction with OL on academic burnout, and c is the total effect of dissatisfaction with OL on academic burnout.
The changes associated with the transition to OL due to the COVID-19 pandemic and the association of deterioration with burnout and dissatisfaction are presented in Table 4. Deterioration in medical education and learning efficiency caused by OL were positively associated with academic burnout (OR = 1.85 and 1.58, respectively) and dissatisfaction with the quality of training organization (OR = 5.61 and 5.86, respectively; p < 0.001).
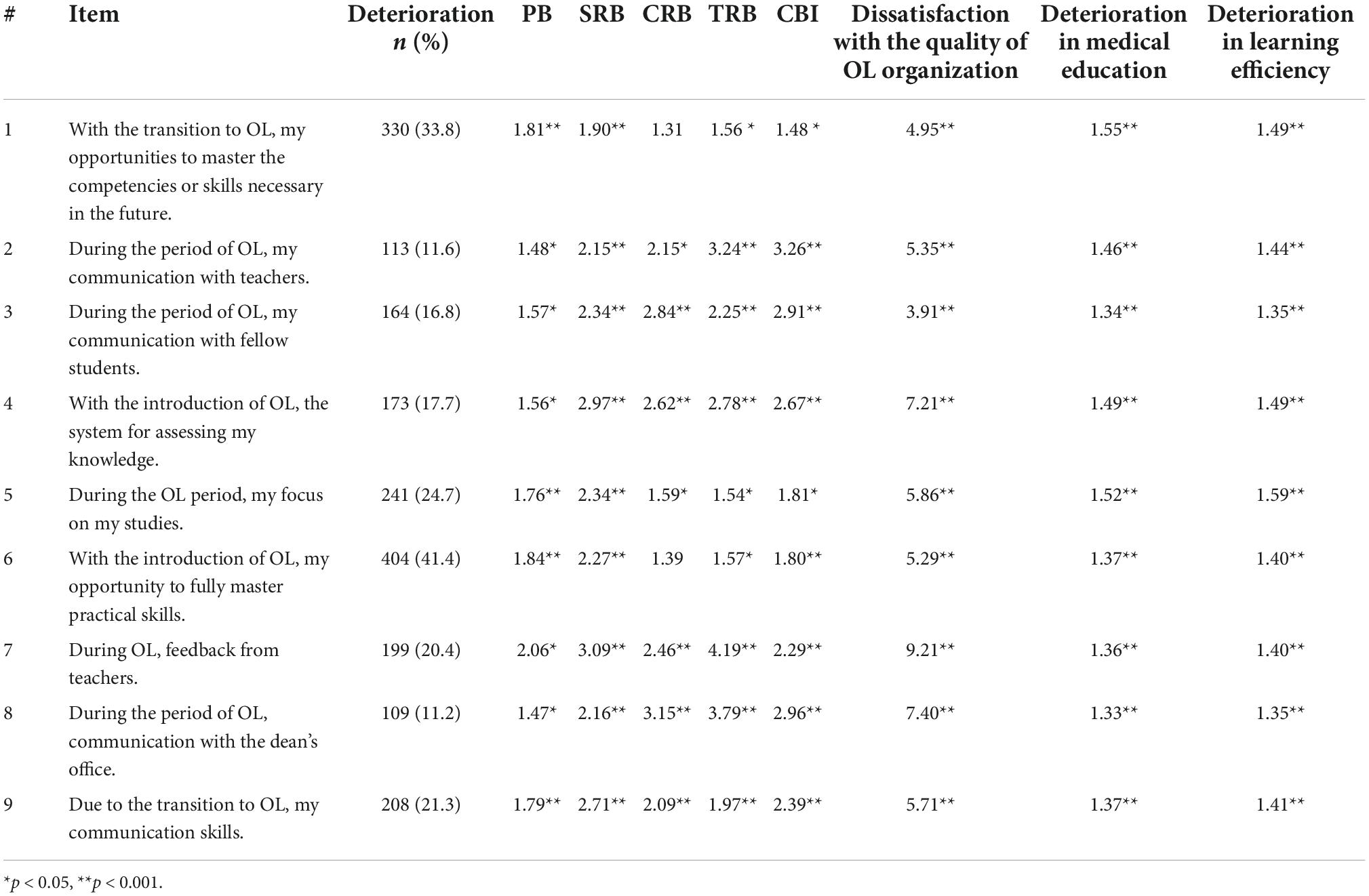
Table 4. Changes associated with the transition to OL during the COVID-19 pandemic and the association of deterioration with burnout, dissatisfaction with the quality of OL organization, and deterioration in medical education and learning efficiency on log-linear regression analysis (N = 975).
Cronbach’s α values for the items in Tables 3, 4 were 0.744 and 0.938, respectively. The “good” to “excellent” levels of internal consistency (Borritz et al., 2006) of the questions from Tables 3, 4 makes it possible to consider them scales for assessing students’ attitudes toward online learning and changes in learning associated with the transition to OL.
Of the students, 388 (39.8%) indicated that, due to the COVID-19 pandemic, they decided to become healthcare workers to a greater extent, while 48 (4.9%) indicated that they wanted to leave the healthcare system; 539 (55.3%) indicated that the pandemic did not affect their choice of profession. Students who indicated that they changed their minds to be healthcare workers were 2.2 times more likely to experience burnout than students whose choice had not changed (p < 0.05) and 2.6 times more likely to burn out than students who strengthened their preferences in the profession due to the pandemic (p < 0.001). Respondents who indicated that they made a convincing decision to become healthcare workers (M = 3.12, SD = 1.29) had a higher level of fear of COVID-19 than those who were uninfluenced by the pandemic in their career choices (M = 2.78, SD = 1.19), p < 0.001.
At the time of the current study, over a year has passed since medical students switched to OL due to the COVID-19 pandemic. Previous research has shown that with the transition to OL, the psychosomatic state of medical students in Kazakhstan improved, and the level of academic burnout decreased (Bolatov et al., 2021a). However, these results were obtained in the early period, almost immediately after entering a new type of distance education, especially for undergraduate students and their educators, as distance education was previously practiced in post-graduate and refresher courses. It was assumed that such positive changes were initially associated with the period of adaptation and the disorganization of the university’s online educational services. The workload on the teaching staff has especially increased, as follows: (1) adaptation to new methods of teaching and assessing students, (2) mastering electronic gadgets, (3) increasing the scope of checking written works and constantly checking them for anti-plagiarism, (4) the severity of evaluating practical and communication skills, and (5), because some teachers joined the front line in the fight against COVID-19, the hourly workload on the remaining teachers increased (Johnson and Coleman, 2021; Lizana et al., 2021; Billett et al., 2022; Rǎducu and Stanculescu, 2022; Westphal et al., 2022; Klusmann et al., 2023). On the other hand, stressors were also observed among students through (1) buying the necessary gadgets to participate in classes and (2) adapting to new learning environments and technologies (O’Byrne et al., 2021). Perhaps in the initial period of the immediate introduction of OL, such stressors could be mitigated by certain adversaries on the part of the university administration in the control of education; however, after the renewal of all educational technologies, such stressors did not cease to affect the student-teacher relationship. Because the era of pandemics tends to repeat itself over time, it is imperative to create an educational system that is safe and sustainable in the long term (Althwanay et al., 2020). Thus, the authors conducted a repeated study after 1 year to assess the psychosomatic state of students and identify the relationship between these indicators and the main components of OL and changes associated with this transition.
Thus, in the course of the repeated study, it was found that, regardless of the academic year and gender, the overall prevalence and level of academic burnout, depression and anxiety were significantly lower than during the period of TL, and remained approximately at the same level as in the initial period of transition to OL. It was also found that academic burnout was associated with the diagnosis and fear of COVID-19, adaptation to the OL format, living conditions, and the presence and nature of additional work during the pandemic. At the same time, the observed increase in somatic symptoms a year after the onset of the pandemic was most likely associated with the long-term consequences of the new format of learning and life in general.
Medical education has undoubtedly undergone changes during the transition to OL due to the pandemic, and factors such as changes in the content of education, the organization of the educational process and support from the school, the nature of student-teacher, student-school and student-student relationships, the availability of clinical practice and financial problems caused by the pandemic played a significant role in the academic life of students.
The overall prevalence of burnout was 15.3%, which was significantly lower than that during the period of traditional learning (TL, Time 1) and approximately at the same level as the initial period of transition to OL (Time 2). This pattern was observed regardless of school year and gender and was also seen when comparing the mean values on the CBI scale (M = 32.9, SD = 31.4 in Time 3 vs. M = 39.77**, S. D. = 17.98 at Time 1 and M = 32.65, SD = 17.64 in Time 2). In comparison, Zis et al. (2021) showed that burnout prevalence did not differ significantly between the pre-COVID-19 and COVID-19 periods; however, it dropped in Year 4 but increased in Year 6.
The prevalence of PB, SRB, and TRB at Time 3 (after 1 year of OL) was lower than that at Time 1 but higher than that at Time 2; however, this pattern in the average level of burnout was significant only for PB (M = 43.1, SD = 21.9 in Time 3 vs. M = 38.46, SD = 21.16 in Time 2, p < 0.001). Such changes in PB can be attributed to the pandemic’s overall impact on student well-being. This was confirmed by the presence of a positive correlation between burnout and fear of COVID-19, while other burnout dimensions were not significantly correlated (Table 2). Moreover, a diagnosis of COVID-19 is positively associated with burnout. The increase in the prevalence of SRBs and TRBs (Figure 1) can be explained by the adaptability of teachers and the education quality control system a year after the transition to OL. The situation differs from CRB, which increased at Time 2 compared to Time 1 but decreased at Time 3 (Figure 1). This indicates that, over time, students have been able to learn how to communicate and work together on online platforms.
The burnout rate did not depend on the living conditions. However, students living alone experienced more pronounced CRB than those living with their parents or friends. Although Wong et al. (2020) indicated that there were few such students (n = 20) requiring additional support from the family and the university, living alone was associated with increased loneliness. Of the respondents, 31.4% indicated that with the transition to OL, they began to feel lonely, and this feeling was positively associated with burnout and dissatisfaction with OL (Table 3).
Because employed students must combine work and study, they are more susceptible to various stress effects and burnout (Yang, 2004; Perna, 2010). Current research reveals that students with non-medical part-time jobs showed higher levels of burnout than did unemployed students without any job. At the same time, the level of burnout among participants with medical part-time jobs (COVID-19-related or non-COVID-19) did not differ from those unemployed. In an earlier study prior to the COVID-19 pandemic, it was found that working part-time students have a higher level of PB (unpublished) regardless of the work. Perhaps working in the medical field during the COVID-19 health crisis had a positive effect on professional identity and did not contribute to depersonalization or a decrease in personal achievements. Moreover, altruistic behaviors such as volunteering during the pandemic did not affect the level and prevalence of burnout.
The levels of depression and anxiety on the PHQ-9 and GAD-7 scales, respectively, were lower than in the period before the pandemic and did not significantly differ from the initial period of the pandemic. The prevalence of depression and anxiety was 24.9 and 15.1%, respectively. These indicators were significantly lower than those in the pre-COVID-19 period (p < 0.001) and were not significantly different from those in the initial period of the pandemic (Bolatov et al., 2021a). A study conducted among US medical students showed that, compared to previous data during the COVID-19 era, anxiety and depression were 61 and 70% higher, respectively (Halperin et al., 2021). In comparison, a prospective study from Brazil showed stability in the medical students’ mental health (Pereira et al., 2022).
Based on the PHQ-15 scale, the severity of somatic symptoms was lower than that in the pre-COVID-19 period but increased after 1 year of OL. The prevalence of all somatic symptoms increased compared with the data obtained during the initial period of the pandemic. This is most likely because of the long-term impact of the pandemic on students’ lives. Harries et al. (2021) indicated that pandemics had moderate effects on stress among medical students. Gica et al. (2020) reported increased psychosomatic symptom levels after the COVID-19 outbreak compared to before.
Three-quarters (75.5%) of respondents indicated that they were satisfied with the quality of the organization of the OL during the COVID-19 pandemic, and about the same (73.7%) were satisfied with academic performance, as it was higher than that in the OL initial period (Bolatov et al., 2021a). In this study (Time 3), over one-third (35.7%) of the respondents indicated an improvement in academic performance, most of whom (73.5%) attributed this to the fact that their studies improved after switching to OL. With the transition to OL, slightly more than half (51.1%) of the students indicated that the system of knowledge assessment did not change, and 17.7% indicated that it had deteriorated, which was positively associated with burnout. Dissatisfaction with academic performance and the quality of OL organization is associated with burnout. A study conducted among Jordanian university students showed that 81.5% of the respondents agreed that using digital learning tools was responsible for low academic performance (Haider and Al-Salman, 2020).
Online learning requires students to have electronic devices, such as computers, laptops, and webcams. However, not all students were financially ready for the transition to OL, which contributed to certain financial problems in their acquisition, especially for bachelor’s students who had no previous experience with the distance learning format. Thirty-six percent of study participants indicated that buying the necessary gadgets has become an additional burden for them and their families; this was positively associated with dissatisfaction with online learning and burnout, and, to a greater extent, with TRB, indicating 1.15 times more negative changes in education and 1.16 times more negative changes in study efficiency.
One of the main components of medical education is students’ clinical practice. At the time of the study, Astana Medical University did not have its own university clinic, and students were trained at the bases of various medical institutions scattered throughout the city, which could lead to additional financial costs and wasting of students’ personal time and, in turn, to stress. OL may remove such inconveniences; moreover, with the transition to OL, students have begun to spend less money on moving, renting an apartment, and eating. The cost savings associated with moving to OL were not associated with burnout or learning satisfaction. At the same time, the absence of the need to change the training corpus was positively associated with burnout, especially personal burnout. This can be explained by the negative impact of the lack of clinical practice. The above conditions created by the OL can potentially affect the comfort of learning. Half of the respondents (50.7%) indicated that OL was a more comfortable form of learning. While it was positively associated with OL satisfaction and reduced negative changes in medical education and study efficiency, it was also positively associated with burnout, especially SRBs and TRBs. Shreffler et al. (2020) recommended finding comfortable places to study to combat burnout, and Costa et al. (2012) found that students who felt uncomfortable with course activities experienced a high prevalence of burnout. However, our results indicate the opposite, most likely owing to the online form of education.
The lack of personal interaction with OL creates problems in the relationship between the student and the teacher (Wilson and Shankar, 2021). Of the respondents, 22.4% indicated that online learning worsened feedback from teachers; 16.8 and 11.6% noted weakened relationships with fellow students and with teachers, respectively; and 11.2% of students noted deterioration in feedback from the dean’s office. These changes were strongly associated with burnout and deterioration of the effectiveness of learning and education.
The COVID-19 pandemic has caused unprecedented disruption in medical education worldwide (Alsoufi et al., 2020). In this study, a quarter of the students indicated that their medical education deteriorated with the introduction of OL, which were 1.85 times more likely to experience burnout. The determinants of the deterioration in medical education are presented in Tables 3, 4. With the transition to OL, students’ opportunities to master the competencies or skills necessary in the professional future decreased, as indicated by a third of the respondents. To a lesser extent, deterioration affected communication skills (21.4%), and, to a greater extent, practical skills (41.5%). Regardless, any impairment in mastering the necessary skills was associated with burnout and deterioration in education, which can lead to problems in the professional development of students.
The higher the learning efficiency, the less time it takes for students to achieve competence (Bruce, 2004). With the transition to online learning, the learning efficiency did not change in 38.9%, improved in 38.3%, and worsened in 22.5% of students. The determinants of deterioration in learning efficiency are presented in Tables 3, 4.
The rapid and unusual transition to OL requires support from the university. Social support is vital to students’ mental health and should be effectively offered and carefully maintained during isolation and quarantine (Aristovnik et al., 2020). Two-thirds of the respondents believed that the university is doing everything it can to help students adapt to OL during a pandemic. University support was negatively associated with burnout and reduced the negative impact of COVID-19-caused OL on learning efficiency and medical education, as evidenced by its mediating role in the relationship between dissatisfaction with OL and academic burnout, while loneliness worsened it.
The transition to OL helped strengthen the policy of academic integrity at medical universities in Kazakhstan. Before the pandemic, the threshold of permissible plagiarism was imposed only on post-graduates to write their theses; then, with the transition to the online format, additions were made for undergraduate students regardless of the form of work, especially for written controls. The syllabi of the disciplines included items on observance of academic integrity, thresholds for plagiarism, and measures applied to violate these orders. Thus, 73.3% of the respondents indicated that checking their work for anti-plagiarism during OL enforced their adherence to the rules of academic honesty; such students were less likely to experience deterioration in their education. However, it negatively affected the student-teacher relationship and contributed to TRB. This can be explained by the fact that, starting from school education, students were not given such requirements; this practice only began to be introduced into the education system of Kazakhstan in recent years. During the OL period, the university purchased the programs on anti-plagiarism and proctoring in full, making it possible for Kazakhstan’s higher educational institutions to move to a new level of academic policy and compliance with international educational standards.
This study has several limitations. First, it was not prospective; comparison at three time intervals was based on a repeated cross-sectional study of representative samples from the same population (medical students at Astana Medical University). Second, because the results were based on a cross-sectional design, it was not possible to identify causal relationships. Finally, the results couldn’t be generalized as these studies were applied in only one institution.
A study conducted a year after the forced introduction of OL due to the COVID-19 pandemic showed the stability of the burnout and mental health of students compared with the initial period of the pandemic and confirmed that this intervention contributed to the improvement of the students’ well-being compared to the pre-COVID-19 period, regardless of the pandemic’s impact on students’ academic life. However, there was a marked worsening of the somatic symptoms. This study identified factors associated with academic burnout during distance learning, including assessing the influence of sex, year of study, living conditions, job availability, student attitudes toward certain features of the online format, and changes associated with the transition to OL. Moreover, determinants of deterioration in medical education, effectiveness, and satisfaction during the OL period were identified. Thus, support from the school was negatively associated with the level of burnout and dissatisfaction with the online learning format. At the same time, the perceived comfort of the new learning format, loneliness and procrastination were positively associated with the level of burnout. And such deterioration in education caused by the pandemic, such as the possibility of mastering the necessary competencies, communication at various levels, and changes in the knowledge assessment system, were positively associated with the level of academic burnout, dissatisfaction with learning during the pandemic, and a general deterioration in medical education and learning efficiency. These results will improve the understanding of online teaching methods in medicine to take the necessary measures in organizing long-term education during crises, such as the COVID-19 pandemic.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Astana Medical University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
AB, TS, and DP: conceptualization. TS and DP: methodology and supervision. AB and ED: formal analysis and investigation. AB: writing – original draft preparation. MZ, DS, and DP: writing – review and editing. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Alsoufi, A., Alsuyihili, A., Msherghi, A., Elhadi, A., Atiyah, H., Ashini, A., et al. (2020). Impact of the COVID-19 pandemic on medical education: Medical students’ knowledge, attitudes, and practices regarding electronic learning. PLoS One 15:e0242905. doi: 10.1371/journal.pone.0242905
Althwanay, A., Ahsan, F., Oliveri, F., Goud, H. K., Mehkari, Z., Mohammed, L., et al. (2020). medical education, pre- and post-pandemic era: A review article. Cureus 12:e10775. doi: 10.7759/cureus.10775
Aristovnik, A., Keržič, D., Ravšelj, D., Tomaževič, N., and Umek, L. (2020). Impacts of the COVID-19 pandemic on life of higher education students: A global perspective. Sustainability 12, 1–34. doi: 10.3390/su12208438
Billett, P., Turner, K., and Li, X. (2022). Australian teacher stress, well-being, self-efficacy, and safety during the COVID-19 pandemic. Psychol. Sch. 1–21. doi: 10.1002/pits.22713
Bolatov, A. K., Seisembekov, T. Z., Askarova, A. Z., Baikanova, R. K., Smailova, D. S., Fabbro, E., et al. (2021a). Online-learning due to COVID-19 improved mental health among medical students. Med. Sci. Educ. 31, 183–192. doi: 10.1007/s40670-020-01165-y
Bolatov, A. K., Seisembekov, T. Z., Askarova, A. Z., Igenbayeva, B., Smailova, D. S., Hosseini, H., et al. (2021b). Psychometric properties of the copenhagen burnout inventory in a sample of medical students in Kazakhstan. Psychol. Russ. State Art 14, 13–22. doi: 10.11621/pir.2021.0202
Borritz, M., Rugulies, R., Villadsen, E., Villadsen, E., Mikkelsen, O. A., Kristensen, T. S., et al. (2006). Burnout among employees in human service work: Design and baseline findings of the PUMA study. Scand. J. Public Health 34, 49–58. doi: 10.1080/14034940510032275
Bruce, S. G. (2004). “Learning Efficiency Goes to College,” in Evidence-Based Educational Methods, eds D. J. Moran and R. W. Malott (Amsterdam: Elsevier), 267–275. doi: 10.1016/b978-012506041-7/50016-4
Campos, J. A. D. B., Carlotto, M. S., and Marôco, J. (2013). Copenhagen burnout inventory - student version: Adaptation and transcultural validation for Portugal and Brazil. Psicologia 26, 87–97. doi: 10.1590/S0102-79722013000100010
Costa, E. F., Santos, S. A., Santos, A. T., Melo, E. V., and Andrade, T. M. (2012). Burnout Syndrome and associated factors among medical students: A cross-sectional study. Clinics 67, 573–580. doi: 10.6061/clinics/2012(06)05
Gica, S., Kavakli, M., Durduran, Y., and Ak, M. (2020). The Effect of COVID-19 pandemic on psychosomatic complaints and investigation of the mediating role of intolerance to uncertainty, biological rhythm changes and perceived COVID-19 threat in this relationship: A web-based community survey. Psychiatry Clin. Psychopharmacol. 30, 89–96. doi: 10.5455/PCP20200514033022
Haider, A. S., and Al-Salman, S. (2020). Dataset of Jordanian university students’ psychological health impacted by using e-learning tools during COVID-19. Data Brief 32:106104. doi: 10.1016/j.dib.2020.106104
Halperin, S. J., Henderson, M. N., Prenner, S., and Grauer, J. N. (2021). Prevalence of anxiety and depression among medical students during the COVID-19 pandemic: A cross-sectional study. J. Med. Educ. Curric. Dev. 8:238212052199115. doi: 10.1177/2382120521991150
Harries, A. J., Lee, C., Jones, L., Rodriguez, R. M., Davis, J. A., Boysen-Osborn, M., et al. (2021). Effects of the COVID-19 pandemic on medical students: A multicenter quantitative study. BMC Med. Educ. 21:14. doi: 10.1186/s12909-020-02462-1
Huckins, J. F., da Silva, A. W., Wang, W., Hedlund, E., Rogers, C., Nepal, S. K., et al. (2020). Mental health and behavior of college students during the early phases of the COVID-19 pandemic: Longitudinal smartphone and ecological momentary assessment study. J. Med. Internet Res. 22:e20185. doi: 10.2196/20185
Ihm, L., Zhang, H., van Vijfeijken, A., and Waugh, M. G. (2021). Impacts of the Covid-19 pandemic on the health of university students. Int. J. Health Plann. Manag. 36, 618–627. doi: 10.1002/hpm.3145
Islam, M. S., Sujan, M. S. H., Tasnim, R., Sikder, M. T., Potenza, M. N., van Os, J., et al. (2020). Psychological responses during the COVID-19 outbreak among university students in Bangladesh. PLoS One 15:e0245083. doi: 10.1371/journal.pone.0245083
Johnson, M., and Coleman, T. (2021). Teachers in the Pandemic: Practices, Equity, and Wellbeing. Cambridge: Cambridge University Press.
Kaggwa, M. M., Kajjimu, J., Sserunkuma, J., Najjuka, S. M., Atim, L. M., Olum, R., et al. (2021). Prevalence of burnout among university students in low- and middle-income countries: A systematic review and meta-analysis. PLoS One 16:e0256402. doi: 10.1371/journal.pone.0256402
Klusmann, U., Aldrup, K., Roloff-Bruchmann, J., Carstensen, B., Wartenberg, G., Hansen, J., et al. (2023). Teachers’ emotional exhaustion during the COVID-19 pandemic: Levels, changes, and relations to pandemic-specific demands. Teach. Teach. Educ. 121:103908. doi: 10.1016/j.tate.2022.103908
Kristensen, T. S., Borritz, M., Villadsen, E., and Christensen, K. B. (2005). The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work Stress 19, 192–207. doi: 10.1080/02678370500297720
Kroenke, K., and Spitzer, R. L. (2002). The PHQ-9: A new depression diagnostic and severity measure. Psychiatr. Ann. 32, 509–515. doi: 10.3928/0048-5713-20020901-06
Kroenke, K., Spitzer, R. L., and Williams, J. B. W. (2002). The PHQ-15: Validity of a new measure for evaluating the severity of somatic symptoms. Psychosom. Med. 64, 258–266. doi: 10.1097/00006842-200203000-00008
Kroenke, K., Spitzer, R. L., Williams, J. B. W., and Löwe, B. (2010). The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. Gen. Hosp. Psychiatry 32, 345–359. doi: 10.1016/j.genhosppsych.2010.03.006
Kyaw, B. M., Posadzki, P., Paddock, S., Car, J., Campbell, J., Tudor Car, L., et al. (2019). Effectiveness of Digital Education on Communication Skills Among Medical Students: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 21:e12967. doi: 10.2196/12967
Lasheras, I., Gracia-García, P., Lipnicki, D. M., Bueno-Notivol, J., López-Antón, R., de la Cámara, C., et al. (2020). Prevalence of anxiety in medical students during the COVID-19 pandemic: A rapid systematic review with meta-analysis. Int. J. Environ. Res. Public Health 17:6603. doi: 10.3390/ijerph17186603
Li, Y., Zhao, J., Ma, Z., McReynolds, L. S., Lin, D., Chen, Z., et al. (2021). Mental health among college students during the COVID-19 pandemic in china: A 2-wave longitudinal survey. J. Affect. Disord. 281, 597–604. doi: 10.1016/j.jad.2020.11.109
Lizana, P. A., Vega-Fernadez, G., Gomez-Bruton, A., Leyton, B., and Lera, L. (2021). Impact of the COVID-19 pandemic on teacher quality of life: A longitudinal study from before and during the health crisis. Int J. Environ. Res. Public Health 18:3764. doi: 10.3390/ijerph18073764
Lyons, Z., Wilcox, H., Leung, L., and Dearsley, O. (2020). COVID-19 and the mental well-being of Australian medical students: Impact, concerns and coping strategies used. Australas. Psychiatry 28, 649–652. doi: 10.1177/1039856220947945
Nikolis, L., Wakim, A., Adams, W., and Do, P. B. (2021). Medical student wellness in the United States during the COVID-19 pandemic: A nationwide survey. BMC Med. Educ. 21:401. doi: 10.1186/s12909-021-02837-y
Nurunnabi, M., Almusharraf, N., and Aldeghaither, D. (2021). Mental health and well-being during the COVID-19 pandemic in higher education: Evidence from G20 countries. J. Public Health Res. 9:2010. doi: 10.4081/jphr.2020.2010
O’Byrne, L., Gavin, B., Adamis, D., Lim, Y. X., and McNicholas, F. (2021). Levels of stress in medical students due to COVID-19. J. Med. Ethics [Epub ahead of print]. doi: 10.1136/medethics-2020-107155
Patwary, M. M., Bardhan, M., Disha, A. S., Kabir, M. P., Hossain, M. R., Alam, M. A., et al. (2022). Mental health status of university students and working professionals during the early stage of COVID-19 in Bangladesh. Int. J. Environ. Res. Public Health 19:6834. doi: 10.3390/ijerph19116834
Pereira, M. B., Casagrande, A. V., Almeida, B. C., Neves, B. A., da Silva, T., Miskulin, F., et al. (2022). Mental health of medical students before and during COVID-19 pandemic: A 3-year prospective study. Med. Sci. Educ. 32, 873–881. doi: 10.1007/s40670-022-01580-3
Perna, L. W. (2010). Understanding The Working College Student, Bulletin of the American Association of University Professors, Vol. 96. 30–33. Available online at: www.aaup.org/article/understanding-working-college-student#.XOxF2Y97ncc (accessed on May 12, 2021).
Rǎducu, C. M., and Stǎnculescu, E. (2022). Teachers’ burnout risk during the COVID-19 pandemic: Relationships with socio-contextual stress-a latent profile analysis. Front. Psychiatry 13:870098. doi: 10.3389/fpsyt.2022.870098
Saraswathi, I., Saikarthik, J., Kumar, K. S., Madhan Srinivasan, K., Ardhanaari, M., Gunapriya, R., et al. (2020). Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: A prospective longitudinal study. PeerJ 8:e10164. doi: 10.7717/peerj.10164
Shreffler, J., Huecker, M., Martin, L., Sawning, S., Thé, S., Shaw, M. A., et al. (2020). Strategies to combat burnout during intense studying: Utilization of medical student feedback to alleviate burnout in preparation for a high stakes examination. Health Prof. Educ. 6, 334–342. doi: 10.1016/j.hpe.2020.04.009
Silistraru, I., Olariu, O., Ciubara, A., Roşca, Ş, Roşca, R. O., Stanciu, S., et al. (2022). Burnout and online medical education: Romanian students in lockdown and their residency choices. Int. J. Environ. Res. Public Health 19:5449. doi: 10.3390/ijerph19095449
Snell, W. J., and Finney, P. (1998). “Multidimensional AIDS anxiety questionnaire,” in Handbook Of Sexuality-Related Measures, eds C. Davis, W. Yarber, and R. Bauserman (Thousand Oaks, CA: Sage), 351–353.
Spitzer, R. L., Kroenke, K., Williams, J. B. W., and Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Internal Med. 166, 1092–1097. doi: 10.1001/archinte.166.10.1092
Taber, K. S. (2018). The use of cronbach’s alpha when developing and reporting research instruments in science education. Res. Sci. Educ. 48, 1273–1296. doi: 10.1007/s11165-016-9602-2
Wang, X., Hegde, S., Son, C., Keller, B., Smith, A., Sasangohar, F., et al. (2020). Investigating mental health of US college students during the COVID-19 pandemic: Cross-sectional survey study. J. Med. Internet Res. 22:e22817. doi: 10.2196/22817
Westphal, A., Kalinowski, E., Hoferichter, C. J., and Vock, M. (2022). K-12 teachers’ stress and burnout during the COVID-19 pandemic: A systematic review. Front. Psychol. 13:920326. doi: 10.3389/fpsyg.2022.920326
Wilson, I., and Shankar, P. R. (2021). The COVID-19 pandemic and undergraduate medical student teaching/learning and assessment. MedEdPublish 10:44. doi: 10.15694/mep.2021.000044.1
Wong, S. Y. S., Zhang, D., Sit, R. W. S., Yip, B. H. K., Chung, R. Y., Wong, C. K. M., et al. (2020). Impact of COVID-19 on loneliness, mental health, and health service utilisation: A prospective cohort study of older adults with multimorbidity in primary care. Br. J. Gen. Pract. 70, e817–e824. doi: 10.3399/bjgp20x713021
Wu, T., Jia, X., Shi, H., Niu, J., Yin, X., Xie, J., et al. (2021). Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 281, 91–98. doi: 10.1016/j.jad.2020.11.117
Yang, H. J. (2004). Factors affecting student burnout and academic achievement in multiple enrollment programs in Taiwan’s technical-vocational colleges. Int. J. Educ. Dev. 24, 283–301. doi: 10.1016/j.ijedudev.2003.12.001
Yuen, J., and Xie, F. (2020). Medical education during the COVID-19 pandemic: Perspectives from UK trainees. Postgrad. Med. J. 96, 432–433. doi: 10.1136/postgradmedj-2020-137970
Zis, P., Artemiadis, A., Bargiotas, P., Nteveros, A., and Hadjigeorgiou, G. M. (2021). Medical studies during the COVID-19 pandemic: The impact of digital learning on medical students’ Burnout and mental health. Int. J. Environ. Res. Public Health 18, 1–9. doi: 10.3390/ijerph18010349
Keywords: COVID-19, medical education, medical students, mental health, burnout, online learning
Citation: Bolatov AK, Seisembekov TZ, Dauyenov E, Zhorokpayeva MD, Smailova DS and Pavalkis D (2022) Medical education during the coronavirus disease pandemic and students’ mental health: A one-year follow-up. Front. Educ. 7:1025600. doi: 10.3389/feduc.2022.1025600
Received: 23 August 2022; Accepted: 07 November 2022;
Published: 21 November 2022.
Edited by:
Antonio Palacios-Rodríguez, University of Seville, SpainReviewed by:
Vera Martins, University of Porto, PortugalCopyright © 2022 Bolatov, Seisembekov, Dauyenov, Zhorokpayeva, Smailova and Pavalkis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aidos K. Bolatov, Ym9sYXRvdmFpZG9zQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.