- 1Department of Public Health, AUT University, Auckland, New Zealand
- 2Department of Psychotherapy, AUT University, Auckland, New Zealand
Key drivers of change in the 21st century—pandemic, technology advance, social disparity—are shaping the public health industry, including employment and education. In 2020, COVID-19 brought rapid change to the teaching of public health in higher education. In this reflective essay, we move beyond the delivery of existing curricula shifting from classroom to online, and consider the greater agenda of a transformative educational paradigm. This is broadly conceptualized as a shift from a “factory model education” to one of “personalized learning” with an emphasis on fostering creativity and heutagogical (student-driven) models, underpinned by technology, and real world application involving problem and project-based learning in a changing industry. Such change has stemmed both from the impact of COVID-19 on the education system, and in response to a more momentous transformation in public health careers and societal expectations of a public health workforce.
Introduction
The face of public health is changing in response to local and global trends of rapid technological development and worsening inequities (Mays et al., 2012; Dahlgren and Whitehead, 2015), both of which have been highlighted in the face of COVID-19 and prior global pandemics. Public health jobs reflect these shifts, emphasizing a need for greater collaboration and online projects, complex problem solving, and more fluid work patterns. Concurrently, education across the sector is in a process of transformation reflecting similar concerns to that of the public health industry. This change is paradigmatic and evolving, often conceptualized as one that is involves a move from that of factory model education to personalized learning.
Factory model education, described as originating in the industrialization era, is one in which students are grouped according to ability and taught the necessary skills, with an emphasis on predictable, standardized tasks, required to become successful workers (Levine, 2020; Moving Our Education System Forward, 2020). The model applies well to academia (Levine, 2020) where teachers typically deliver standardized lectures to large numbers of anonymized students, and standardized assessments are managed for large student populations through a Learning Management System (LMS) (Levine, 2020; Moving Our Education System Forward, 2020). Globally, commentators have called for a transformation within higher education to adopt personalized learning, a concept coined by education psychologist Benjamin Bloom in 1984 (Asfa-Wossen, 2020; Levine, 2020). Personalized learning, also referred to as future learning and 21st century learning, empowers students by drawing upon their individual strengths, skills, and interests (Campbell et al., 2007; Asfa-Wossen, 2020; Levine, 2020). Such an approach emphasizes fostering creativity, promoting student-driven or heutagogical models, and accentuates real world application involving problem and project-based learning. Technology is increasingly the means to facilitate this transformation by a move away from standardization to a greater degree of customization and personalization (Campbell et al., 2007; Prain et al., 2013; Asfa-Wossen, 2020). It is no surprise then that evolving terms for the present into future include the digital age, the third-into-fourth industrial revolution, 21st century capitalism (Reich, 1992; Rifkin, 2015; Ross, 2016).
Pre-COVID-19, public health education in Aotearoa New Zealand, as with higher education locally and globally, relied mainly on analog ways of teaching and learning; that is, using “chalk and board” lecture and traditional assessment models, with a limited online, interactive presence. COVID-19 rapidly pushed higher education toward remote teaching and learning, involving difficult-to-imagine/or re-imagined pedagogy, at a time when organizations, professionals, and community understandings were not prepared for such a widespread change. However, whilst moving online has been a significant challenge, it has provided opportunities to extend the current paradigm and envision transformative change. Transformation, although difficult to achieve, as it requires development on several fronts simultaneously, must be at the fore of higher education advancement. For public health education, transformation involves changing how we respond as practitioners to significant global challenges such as pandemics; and how we respond as educationalists to the significant societal change brought about by the demands of the digital age (Bolstad et al., 2012; Gilbert, 2017; Robinson, 2020).
The public health team at Auckland University of Technology (AUT) is undertaking curriculum redesign to build an agile workforce, reflecting changing trends in higher education and public health in the 21st century. Public health at AUT is situated at a campus south of the city; in an area of Auckland that has a high proportion of Mâori and Pacific residents, giving rise to high numbers of Mâori and Pacific students enrolled in the program. Mâori and Pacific peoples experience inequity in morbidity and mortality in the face of influenza pandemics and other communicable disease (Jefferies et al., 2020). This context provides great opportunity for redesigning curricular that forefronts personalized learning, integrates indigenous and community perspectives driven by local public health solutions; as well as individual student choices and strengths. Such change is of significance, both nationally and internationally, in influencing the delivery of public health education to ensure it is responsive to community needs.
Currently AUT delivers undergraduate and postgraduate public and environmental health programs, including health promotion and disaster management. The teaching philosophy is underpinned by public health values of equity and social determinants (i.e., the economic, social, and physical conditions that influence health status), with an emphasis on the principles of the Treaty of Waitangi, the key national statement guiding policy and practice; supporting mâtauranga Mâori (Mâori values, principles, and knowledge) through utilizing Mâori health and well-being models. These include Te Whare Tapa Whâ, te Wheke, and te Pae Mâhutonga. All models encompass the importance of the health of people—their physical, mental, social health and wellbeing—and their natural environment (Ministry of Health/Manatû Hauora, 2002). While the program philosophy remains vital, the challenges to education are centered on delivery of content and what this will mean in a society where digital literacy is becoming a necessary skill to manage individual wellbeing as well as delivery of public health.
The Changing Face of Public Health
Throughout history, humanity has been plagued by disease and illness. The shift to agrarian communities followed by widespread trade, generated opportunities for human and animal interaction and marked a dramatic increase in the scale and spread of disease (LePan, 2020). Beginning with the Antonine Plague (165–180AD), other major outbreaks—epidemics and pandemics—have included the Black Death (1347–1351), Cholera outbreaks (1817–1923), Spanish Flu (1918–1919), and SARS (2002–2003). Within the last decade (2010-2020) there have been three notable outbreaks—Swine Flu (2009–2010); Ebola (2014–2016); MERS (2016-present); and currently, COVID-19 (LePan, 2020). Despite the continued occurrence of such outbreaks, improvements in public health systems (e.g., vaccination campaigns and improved sanitation), have resulted in a gradual reduction in overall death rates. However, preparing for and combatting epidemics and pandemics remains a significant public health issue. Indeed, the Centers for Disease Control and Prevention (2020) have posited that “stronger public health systems mean faster, smarter response to contain potential pandemics.”
Reflective of the complexity in tackling a pandemic, over the past decades key movements in public health have employed a complex systems approach to design, implement, and evaluate interventions for change. Examples include New Public Health (Baum, 2008) and the World Health Organization (2008) Social Determinants of Health to Sustainable Development Goals (United Nations, 2020). These adopt an intersectoral and interdisciplinary focus on improving and protecting the environments in which people live and work, as well as the social conditions that contribute to health. However, while still highly relevant, these approaches are insufficient as a means of informing the future of public health as they inadequately address significant developments in the societal context.
New models of public health include precision population or public health alongside a personalized medicine revolution and place greater emphasis on: precisely targeting population groups using big data; and individualized health consumption or empowered prosumer models of preventive health (Vogenberg et al., 2010; Mesko, 2015; Topol, 2015; Conn et al., 2017; Lyles et al., 2018). These models are technology based developments and are perceived as offering opportunities to be more responsive to the needs of individuals and communities. An example of this transformational change can be seen in the context of Aotearoa New Zealand where a serious public health concern is that of high prevalence of asthma and rheumatic fever linked to determinants of health such as poverty, unhealthy housing, and polluted neighborhoods. In the future, as a result of technology developments, addressing these issues could shift from broad population based interventions to a more precise and, indeed, potentially cost-effective population health approach where data from artificial intelligence (AI) are used to identify community patterns of poverty and ill health more specifically and provide information for policy action (Lyles et al., 2018). One element of a response might involve sensors and mapping technology to measure indicators of poor housing, such as damp, mold, and heat loss, offering opportunities to target resources accordingly (Lyles et al., 2018). Personalized medicine, integrated with a population based approach, will also contribute to public health solutions with technology offering opportunities for better individual health management; largely through smartphone technologies (Mesko, 2015; Topol, 2015). However, these changes mean that public health students, as future practitioners, will need high levels of digital literacy as well as skills that accommodate complex systems changes.
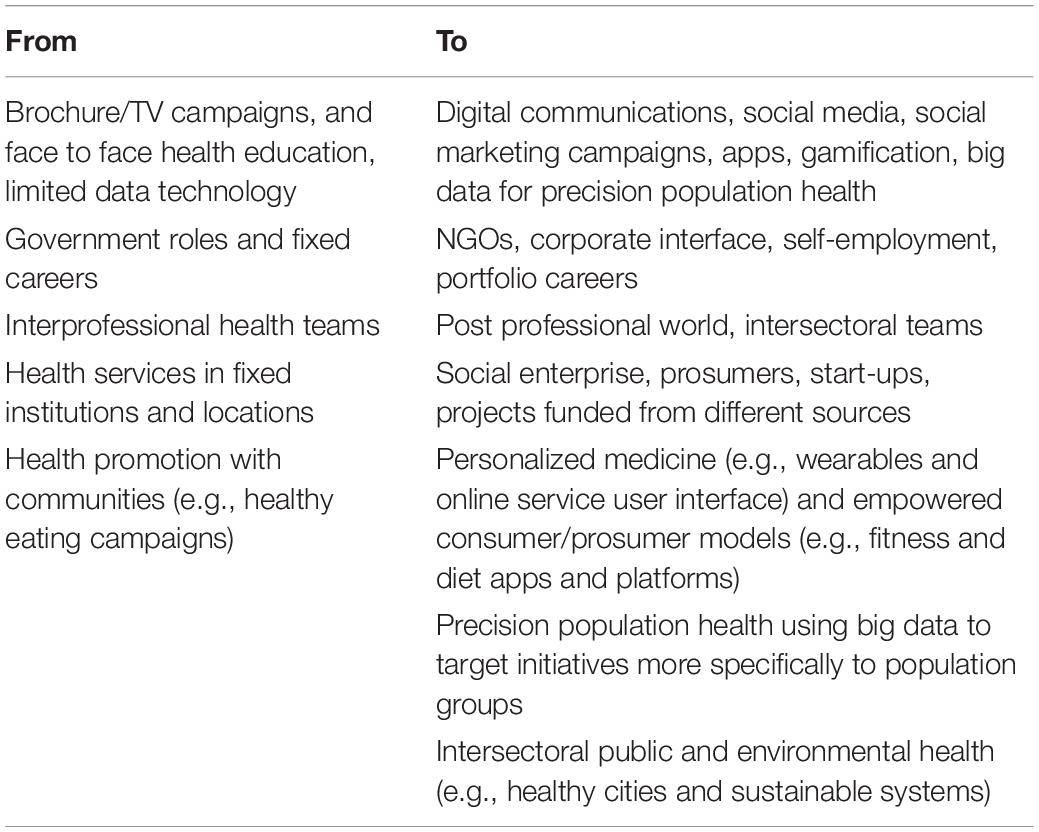
In relation to future employment the response to a changing society has resulted in a greater reliance on the internet and digital skills, and the ramping up of online work spaces with increased use of AI for tasks such as big data management, greater use of social media, social marketing, app design, and gamification. These changes broadly describe a shift from fixed career, lifelong white-collar work involving routine processing to portfolio careers whereby creative problem solving are combined with digitally enhanced cognitive and interpersonal skills (Reich, 1992; Rifkin, 2015; Ross, 2016). Increasingly, public health jobs are to be found in a variety of non-traditional spaces, such as social enterprises, “start-ups” and prosumer initiatives. These general trends fit well with inexorable trends in the 21st century public health industry (see Table 1).
Godin noted that empowered consumers are increasingly dismissive of traditional persuasion campaigning and demand a model where, as prosumers, they are engaged in debates and design, and have greater ownership and choice over the issue at hand (Godin, 2011). This personal portfolio revolution must be seen alongside governments having greater control over population health through big data and surveillance, which is a feature of precision population health (Lyles et al., 2018). Thus, pandemics, such as COVID-19, will necessarily demand increased intensive government involvement, requiring the training of a workforce able to implement the interventions needed at a population level; alongside other areas of public health (e.g., obesity management). This transformation will need to incorporate spaces and tools that are new to the public health scene and involve new marketing techniques and information exchange such as that of the user-controlled YouTube model.
Thus, while face-to-face working with communities is still vital, taking on a mixed approach with that of online social marketing techniques, mirrors significant change in health promotion paradigms (Godin, 2011; Conn et al., 2017). Increasingly, consumers expect marketing to meet their preferences, including high budget digital marketing of consumer products and personalized content. As a result, public health and public health media campaigns, with limited budget and digital skill set struggle to have an impact. Digital upskilling is, therefore, essential to equip newly graduated public health workers to engage in jobs that continue to emerge and become normalized in e-health social media, chat spaces, empowered groups of users, app creation and use, health related “serious” gamification, as well as use of big data to tackle complex problems (Institute of Medicine, 2003; Lyles et al., 2018).
While school leavers who may be more prepared to engage with technology for the purpose of learning, job seeking, and employment constitute a large portion of the higher education system; the number of mature students, lifelong or continuous learners, continues to grow. Continuous learners (many of those choosing to study public health are already working in the health industry), want to work and study, they need flexibility and seek choice and relevance and are employment oriented (Susskind and Susskind, 2015; Gallagher, 2016). However, students in Aotearoa New Zealand currently seem to have limited awareness of the changes described in this essay, likely reflecting the struggle faced by society in keeping up with the rapid changes taking place, and how it should inform their choices. Indeed, what they should demand from universities. Students are, though, “voting with their feet” in relation to remote working, demanding more convenience from their study through online lectures and resources, as the pressures to combine work, study, and volunteering ramp up.
Transforming Public Health Education
The call for root and branch change to curricula and delivery mechanisms across the education sector has been characterized as a shift from an industrial age “one size fits all” model (Levine, 2020; Moving Our Education System Forward, 2020; Robinson, 2020) to become that of 21st century learning systems which are fit for purpose. A key element of this call for transformative change is that the learner should be placed at the center of the educational system (Blaschke, 2012). This heutagogical paradigm differs from the more familiar teacher driven pedagogical paradigm of the learning experience being about the explication by a teacher to students on a given topic (see Table 2). Gilbert (2015) described this as “aboutism;” that is, education predominantly having a focus on imparting information on a given subject which is less about skills development and creative expression, project and problem-based study in real world settings, and where student preference is not considered central.
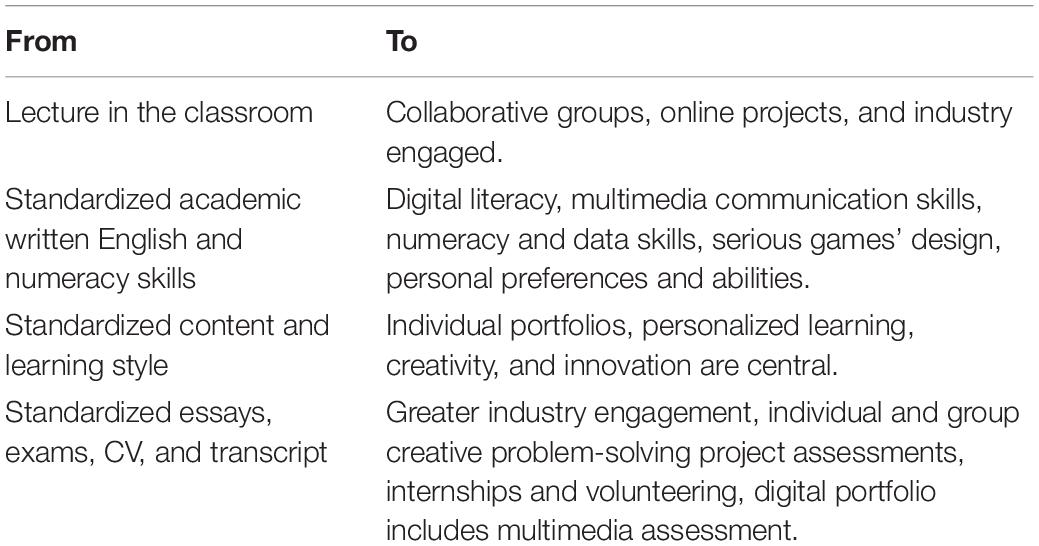
Table 2. From factory model education to personalized learning: implications for public health education in the 21st century.
There appear to be strong synergies between these general concerns for higher education curricula and the specific circumstances of public health education. Public health scholars are now being asked to transform their skills from those of presenting a subject to being facilitators of student driven learning and choices, facilitating students finding out about a topic for themselves, having a range of new online and digital skills that fit with this new paradigm of education that promotes personal choice, and that is linked to real world scenarios. This poses a significant learning challenge for public health academics and points to a need for stronger links with industry in order to develop projects that facilitate student learning while being of benefit to the community.
The call for less “aboutism” (Gilbert, 2015) also highlights an issue: that of what public health content has traditionally been “about” and what it needs to transform to become. Globally, including in Aotearoa New Zealand, public health education has been dominated by biomedical and western health system norms (Trilling and Fadel, 2009; Coombe et al., 2020). Greater choice to explore subjects and paradigms allows for those which have been excluded, such as Mâori and Pacifica models of health and equity. Also, crucially, it allows students to choose or personalize curricula and assessment to their interest areas. In an interdisciplinary public health education, students from diverse backgrounds (e.g., ethnicity, age, gender, and personal interests) can shape the curricula and assessment to their preferences and evolving portfolios as well as to their context. This may include focusing on specific populations and their needs, as well as embracing multiple novel ways of developing strengths-based solutions.
Changes to curricula and delivery mechanisms to facilitate students in their efforts to prepare for the 21st century workplace have been documented to include: moving from a knowledge transfer paradigm to developing collaborative, communicative, cross-disciplinary skills which promote creativity and innovation (Trilling and Fadel, 2009). Further, there seems to be broad support for promoting digital literacy and use of e-learning, online, and blended learning to a greater extent. These general developments in educational delivery seem highly applicable to public health given the emphasis on greater choice, convenience, and cost-effectiveness for students. This needs to extend beyond delivery and curricular, to encompass the range of credentials available to students.
In 2017, the New Zealand Productivity Commission (2017) called for a radical transformation in higher education, suggesting that students be able to take individual courses and certificates which could be combined into qualifications, and which would come closer to meeting the needs of future employment. Given the increasing potential for portfolio careers, with less fixed roles and employment, and the need to keep up with technological change, international researchers have argued a flexible approach to credentials would support people to continuously upskill and stay current in order to meet the needs of their employers (Gallagher, 2016; Jorre de St Jorre and Oliver, 2018). Variously discussed as microcredits, nano degrees, badges and other new terminology (Gallagher, 2016), “micro-credentials enable learners to access specific knowledge and skills in a cost-effective and time-efficient way” (NZQA, 2018). This flexible approach to credentials would be ideal for public health which is applied and interdisciplinary and lends itself well to fitting with professional communities which could undertake study in short bursts at their own convenience. Indeed, the New Zealand Qualifications Authority have argued that such a “system will help ensure that the New Zealand education and training system remains relevant in a period of fast paced social, economic and technological changes” (NZQA, 2018).
In the changing climate of higher education, it is important that digital and technological change is driven by pedagogical change wherein technology reframes the types of student skills and attributes; thereby, moving beyond simply being a different method of delivering the same content. Despite some technological progress, it appears that truly transformative change within the university system is lacking. While a number of colleges have started to adopt micro-credentials, universities are seriously lagging in their response and implementation. There may be various reasons for this: bureaucratic structures wedded to old style compliance, slow rate of response, an emphasis on research over teaching, lack of student demand for change. Further challenges faced by tertiary education globally were exposed by the disruption wrought by COVID-19 and include diminished resources and demand for improved infrastructure to support continued distance and blended learning models (World Bank Group Education, 2020). However, the public health industry is also lagging. The government funded health sector is similar in nature to higher education: it is not designed to manage rapid shifts, guidelines and competencies are outdated, and public sector jobs are few.
The slowness to change may be a reflection of traditional credentialing which was based on long-term knowledge exchange; whereas micro-credentialing is shorter and targeted, concerned more with creativity, new skills, and industry engagement. Delaying the shift to adopting micro-credentialing within higher education, however, may prove costly—socially and fiscally. At present, Aotearoa New Zealand students borrow significant amounts of money upfront to pay for a degree assuming that a relatively fixed pathway will enable them to pay off the loan and benefit from the education over their working life time. Yet, as organizations, jobs, and skills become more fluid, and society requires workers who can learn new skills throughout their working lives, this brings into question the upfront high cost of a 3 or 4 year degree. This is especially relevant for students from lower socio-economic backgrounds, such as that of south Auckland communities, who have less financial backing and for whom investment in education is a major sacrifice, and currently must be combined with work.
Moving Forward
Building a stronger public health system is dependent on having professionals who are well educated and prepared to think creatively and adopt innovative practices. An example of this might be drawn from response to the current pandemic. Worldwide, an important public health message has been social distancing to curb COVID-19, and resulted in quarantine for travelers and governments limiting the movement of people. In Aotearoa New Zealand, people are now required to use an app on their phone to track their movements in public settings (Baker et al., 2020). Growing public awareness of this public health initiative required collaborative industry engagement to implement the initiative nationally, personalized medicine and prosumer models of education to empower people to take responsibility for their health, as well as digital communication to provide the knowledge and skills needed for using the tool. A challenge in the Aotearoa New Zealand context has been a sheer lack of public health workers and a poorly resourced public health system for managing the pandemic (Gorman and Horn, 2020; Pennington, 2020), forcing the government officials to rapidly train health workers and others for contact tracing and quarantine management. This example reflects the wider issue of the need to grow and develop the national public health system to respond to a range of future challenges (e.g., pandemics and waste water monitoring), and the need to develop public health workers able to perform in complex, intersectoral, and technology oriented environments.
Personalizing Learning
In the short to medium term, COVID-19 has brought to the fore, yet again, the need for the future of public health and higher education to be more collaborative, community driven and embracing of opportunities for new kinds of jobs, underpinned by new kinds of education. Such education, characterized widely as “personalized learning,” would appear to be more attractive than the current standardized model, given the scope for individual choice and strengths base, the opportunities for personal and cultural expression, and for collaborative creativity. Indeed, a personalized learning model for public health education will offer greater relevance for public health students’ future lives and work and be more relevant and valuable to the wider society. Generic changes to employment and higher education are highly relevant to public health, perhaps because this subject is so transdisciplinary and wide ranging, lending itself to major trends (e.g., digital focus, collaborative working, and creative problem solving); while offering a wide range of choices for students’ preferences.
An Intersectoral Approach
Given the uncertainty of the future along with the legacy of slow organizational change, there needs to be an emphasis on partnership with the community and industry to create and nurture symbiotic relationships and to ensure future students and their families are part of, and aware of, the change conversation. This is particularly important when considering whether public health higher education is preparing people for employment in the long-term. Although dependent on widespread access to the internet and smartphones, alongside the skills and knowledge to utilize social media, apps and games, increasingly technology is being employed to help people meet health and wellbeing goals, with health practitioners to advise and support online (Mesko, 2015; Topol, 2015). Therefore, the promotion of digital literacy amongst individuals and communities; along with collaboration between organizations to ensure streamlined delivery of information is a high priority for higher education, particularly in the field of public health. In limiting classroom teaching, the COVID-19 pandemic has also challenged other aspects of higher education including networking and social content. “To remain relevant, universities will need to reinvent their learning environments so that digitalization expands and complements student-teacher and other relationships” (Schleicher, 2020, p. 4). With COVID-19 still presenting globally, and in anticipation of future pandemics, public health workers who have both interpersonal skills and are digitally literate will be an ongoing asset to society.
Summary
Prior to COVID-19, public health higher education primarily consisted of classroom based learning, with some online lectures and standardized assessment. These methods fulfilled the criteria of giving students much needed “knowledge;” however, the narrow approach was also reflected in graduates being trained to enter a workforce in which they were required to comply with standardized organizational processes that required them to learn how to “fit in.” While these methods met the needs of the educational institution, the limitations of such a model are increasingly highlighted. COVID-19 has demanded a complete change to education delivery to encompass online methods; and it also offers opportunities for the move toward creative, personalized learning that emphasize student choice, personal identity, and strengths. The public health sector is becoming more diffuse and complex with many different players joining in an intersectoral approach that is defined by a digital era; such change demands a more responsive approach to higher education.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author Contributions
CC: conceptualization and writing of public health and higher education. SN: writing and conceptualizing public health and higher education. MW: public health and higher education and mâtauranga Mâori. RC: public health and higher education and Pacifica learning. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Asfa-Wossen, L. (2020). The Rise of Personalised Learning. Available online at: https://www.studyinternational.com/news/personalised-learning/ (accessed November 29, 2020).
Baker, M. G., Kvalsvig, A., and Verrall, A. J. (2020). New Zealand’s COVID-19 elimination strategy. Med. J. Aust. 213, 198–200. doi: 10.5694/mja2.50735
Blaschke, L. M. (2012). Heutagogy and lifelong learning: a review of heutagogical practice and self-determined learning. Int. Rev. Res. Open Distance Learn. 13, 56–71. doi: 10.19173/irrodl.v13i1.1076
Bolstad, R., Gilbert, J., McDowall, S., Bull, A., Boyd, S., and Hipkins, R. (2012). Supporting Future-Oriented Learning & Teaching – A New Zealand Perspective. Wellington: Ministry of Education.
Campbell, R. J., Robinson, W., Needlands, J., Hewston, R., and Mazzoli, L. (2007). Personalised learning: ambiguities in theory and practice. Br. J. Edu. Stud. 55, 135–154. doi: 10.1111/j.1467-8527.2007.00370.x
Centers for Disease Control and Prevention (2020). Global Health Protection and Security. Available onlie at: https://www.cdc.gov/globalhealth/healthprotection/fieldupdates/winter-2017/why-it-matters.html (accessed November 17, 2020).
Conn, C., Nayar, S., Lubis, D., Maibvisira, C., and Modderman, K. (2017). Vulnerable Youth as Prosumers in HIV Prevention: studies using participatory action research. JMIR Public Health Surveill. 3:e53. doi: 10.2196/publichealth.7812
Coombe, L., Severinsen, C., and Robinson, P. (2020). Practical competencies for public health education: a global analysis. Int. J. Public. Health 65, 1159–1167. doi: 10.1007/s00038-020-01459-3
Dahlgren, D., and Whitehead, M. (2015). European Strategies for Tackling Social Inequalities in Health: Levelling Up Part 2. Copenhagen: World Health Organization.
Gallagher, S. R. (2016). The Future of University Credentials: New Developments at the Intersection of Higher Education and Hiring. Cambridge, MA: Harvard Education.
Gilbert, J. (2015). Transforming science education for the Anthropocene – is it possible? Res. Sci. Edu. 46, 187–201. doi: 10.1007/s11165-015-9498-2
Gilbert, J. (2017). Back to the future? Aims and ends for future-oriented science education policy – the New Zealand context. Knowl. Cult. 5, 74–95. doi: 10.22381/KC5620176
Gorman, D., and Horn, M. (2020). On New Zealand’s weak, strong and muddled management of a COVID-19 epidemic. J. Intern. Med. 50, 901–904. doi: 10.1111/imj.14928
Institute of Medicine (2003). The Future of the Public’s Health in the 21st Century (Chapt 7). Washington, DC: The National Academies Press.
Jefferies, S., French, N., Gilkison, C., Graham, G., Hope, V., Marshall, J., et al. (2020). COVID-19 in New Zealand and the impact of the national response: a descriptive epidemiological study. Lancet Public Health 5, E612–E623. doi: 10.1016/S2468-2667(20)30225-5
Jorre de St Jorre, T., and Oliver, B. (2018). Want students to engage? Contextualise graduate learning outcomes and assess for employability. High. Educ. Res. Dev. 37, 44–57. doi: 10.1080/07294360.2017.1339183
LePan, N. (2020). Visualizing the History of Pandemics. Available online at: https://www.visualcapitalist.com/history-of-pandemics-deadliest/ (accessed November 17, 2020).
Levine, A. (2020). Digital Students, Industrial-Era Universities. Inside Higher Ed. Available online at: https://www.insidehighered.com/views/2010/06/14/digital-students-industrial-era-universities (accessed February 12, 2021).
Lyles, C. R., Lunn, M. R., and Obedin-Maliver, J. (2018). The new era of precision population health: insights for the All of Us research program and beyond. J. Transl. Med. 16:211. doi: 10.1186/s12967-018-1585-5
Mays, G., Isham, G., and Kaplan, R. (2012). Funding Public Health: A new IOM Report on Investing in a Healthier Future. Available online at: https://uknowledge.uky.edu/cgi/viewcontent.cgi?referer=https://www.google.com/&httpsredir=1&article=1042&context=hsm_present (accessed November 14, 2020).
Mesko, B. (2015). My Health Upgraded: Revolutionary Technologies to Bring a Healthier Future. Budapest: Webicina Kft.
Ministry of Health/Manatû Hauora (2002). He Korowai Oranga: Mâori Health Strategy. Available online at: https://www.health.govt.nz/publication/he-korowai-oranga-maori-health-strategy (accessed November 20, 2020).
Moving Our Education System Forward (2020). Factory Model of Education. Available online at: http://creativecurriculumisabella.weebly.com/the-factory-model-of-education.html (accessed November 29, 2020).
New Zealand Productivity Commission (2017). New Models of Tertiary Education. Available online at: https://www.productivity.govt.nz/assets/Documents/653521ea17/Overview-Tertiary-Education-v2.pdf (accessed November 29, 2020).
NZQA (2018). Micro-Credentials System Launched. Available online at: https://www.nzqa.govt.nz/providers-partners/approval-accreditation-and-registration/micro-credentials/ (accessed November 29, 2020).
Pennington, P. (2020). Covid-19: Huge shortfall in public health investment, College of Public Health says. Radio New Zealand. Available online at: https://www.rnz.co.nz/news/national/417715/covid-19-huge-shortfall-in-public-health-investment-college-of-public-health-says (accessed February 12, 2021).
Prain, V., Cox, P., Deed, C., Dorman, J., Edwards, D., Farrelly, C., et al. (2013). Personalised learning: lessons to be learnt. Br. Edu. Res. J. 39, 654–676. doi: 10.1080/01411926.2012.669747
Reich, R. (1992). The Work of Nations: Preparing Ourselves for 21st Century Capitalism. New York, NY: Vintage.
Rifkin, J. (2015). The Zero Marginal Cost Society: The Internet of Things, the Collaborative Commons, and the Eclipse of Capitalism. London: Macmillan.
Robinson, K. (2020). Changing Education Paradigms. Available online at: https://revisesociology.com/2017/07/30/ken-robinson-changing-education-paradigms/ (accessed November 29, 2020).
Schleicher, A. (2020). The Impact of COVID-19 on Education. Insights from Education at a Glance. Paris: OECD.
Susskind, R., and Susskind, D. (2015). The Future of the Professions: How Technology will Transform the Work of Human Experts. Oxford: Oxford University Press.
Topol, E. (2015). The Patient Will See You Now: The Future of Medicine in Your Hands. New York, NY: Basic Books.
Trilling, B., and Fadel, C. (2009). 21st Century Skills: Learning for Life in Our Times. New York, NY: John Wiley & Sons.
United Nations (2020). The 17 goals. Available online at: https://sdgs.un.org/goals (accessed November 15, 2020).
Vogenberg, F. R., Barash, C. I., and Pursel, M. (2010). Personalized medicine. Part 1: evolution and development into theranostics. Pharm. Ther. 35, 560–567.
World Bank Group Education (2020). The COVID-19 Crisis Response: Supporting Tertiary Education for Continuity, Adaptation, and Innovation. Available online at: http://documents1.worldbank.org/curated/en/621991586463915490/The-COVID-19-Crisis-Response-Supporting-Tertiary-Education-for-Continuity-Adaptation-and-Innovation.pdf (accessed November 12, 2020).
World Health Organization (2008). Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. Available online at: https://www.who.int/publications/i/item/WHO-IER-CSDH-08.1 (accessed November 24, 2020).
Keywords: workforce development, personalized learning, higher education, pedagogy, public health (MeSH [H02.403.720])
Citation: Conn C, Nayar S, Williams MH and Cammock R (2021) Re-thinking Public Health Education in Aotearoa New Zealand: Factory Model to Personalized Learning. Front. Educ. 6:636311. doi: 10.3389/feduc.2021.636311
Received: 01 December 2020; Accepted: 26 February 2021;
Published: 19 March 2021.
Edited by:
Geneviève Pagé, University of Quebec in Outaouais, CanadaReviewed by:
Leanne Coombe, The University of Queensland, AustraliaRosemary M. Caron, University of New Hampshire, United States
Copyright © 2021 Conn, Nayar, Williams and Cammock. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cath Conn, Y2F0aC5jb25uQGF1dC5hYy5ueg==
 Cath Conn
Cath Conn Shoba Nayar
Shoba Nayar Margaret Hinepo Williams1
Margaret Hinepo Williams1