
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Educ. , 23 December 2020
Sec. Leadership in Education
Volume 5 - 2020 | https://doi.org/10.3389/feduc.2020.567421
This article is part of the Research Topic Education Leadership and the COVID-19 Crisis View all 21 articles
The COVID-19 pandemic has fundamentally altered the pre-clerkship, clerkship, and research experiences for medical students. Although these changes impact all specialties, we highlight the unique challenges faced by neurology education and discuss methods by which our institution is adapting to these changes at the epicenter of the pandemic in the U.S. We include a few examples of how some neurology departments around the country have altered their teaching methods in the COVID-19 era and capitalize on lessons learned by proposing new strategies for moving neurology education forward.
Located in New York City at the epicenter of the COVID-19 pandemic in the U.S., Weill Cornell Medicine (WCM) has continuously reassessed the balance between patient care, medical education, and research. In March 2020, in consultation with its primary teaching hospital system, New York-Presbyterian, WCM made the difficult but necessary decision to suspend all medical student teaching in clinical care settings, creating changes for medical students at all phases of their education. For pre-clerkship students, all lectures became virtual, and preceptorship sessions, which previously allowed students to engage in clinical settings, were either postponed or canceled. Clerkship students who depended on a year of complete clinical immersion could no longer participate in in-person patient encounters. More senior medical students struggled with the cancellation of away electives and sub-internships, along with the uncertain implications of these changes on the residency application process.
These COVID-19-driven changes in medical teaching have created rippling effects for neurology education. The focus of the pre-clerkship curriculum is on building a strong foundational understanding of the basic sciences gathered through faculty lectures and small-group participation. To foster student learning during COVID-19, the WCM neurology department offered continuing medical education (CME) courses inclusive of medical students highlighting neurodegenerative disease and basic neurosciences. Moreover, to maintain students' early clinical exposure to neurology, traditionally obtained through in-person preceptorships and physical diagnosis sessions, the WCM neurology department began including students virtually in daily Morning Report sessions.
For students in the clerkship phase, the focus of the medical school curriculum shifts from foundational science to clinical application. WCM began offering seven 2–4 week remote telehealth and four 2–4 week clinical research electives to keep students engaged in patient care during the pandemic, albeit from afar. These electives included COVID-related patient care, research and clinical care in OB/GYN, psychiatry research and virtual liaison services, medical pedagogy, as well as structured and independent research. A 2-week teleneurology virtual elective was also created for students to engage with neurology patients in subspecialty fields like stroke, neuro-intensive care, movement disorders, neuro-oncology, and memory disorders. This reflects previous reports demonstrating the long-ranging potential of teleneurology to provide access to diverse groups of neurology patients (Dorsey et al., 2018; Al Kasab et al., 2020; Klein and Busis, 2020). Platforms such as EPIC, a commonly used electronic medical record system, and video conferencing applications allow medical students to join virtual visits; this virtual clinical experience is not only being incorporated at WCM but also at other institutions across the country.
These clinical electives are not only essential for students interested in neurology to explore this field, but also for students applying to other specialties. Though only 2.2% of U.S. MD seniors applied to neurology or child neurology in the 2020 Match and 2% of 2018–2019 U.S. DO students planned to apply to neurology residency (American Association of Colleges of Osteopathic Medicine, 2019; National Resident Matching Program, 2020), patients exhibiting neurological symptoms such as headache, vision changes, and sensory or motor deficits can be found in almost all specialties, making the neurology curriculum essential to general medical student education.
The American Academy of Neurology (AAN) Synapse forum, which is an online discussion board of the AAN, has brought WCM medical students in contact with national leaders in neurology education. Through this forum, medical students nation-wide have access to online educational meetings and workshops. Two examples include the National Resident Lecture Series initiated by St. Louis University and the Johns Hopkins Virtual Neurology Chats. The National Resident Lecture Series allows medical students around the country to attend meetings typically reserved for residents and to obtain expert perspectives in various neurology subspecialties. Similarly, the Johns Hopkins Virtual Neurology Chats integrates faculty lectures, virtual rounds, and case presentations into an elective course. WCM students interested in neurology, particularly first and second-year students, have also taken part in some of these educational interventions offered by other institutions.
Students nearing graduation face yet another set of uncertainties amidst the COVID-19 pandemic. It is unknown how the lack of in-person preparation for residency interviews and the cancellation of away rotations will impact residency applications and specialty choice. With residents and faculty turning their attention to COVID-related efforts in patient care, students may have fewer mentors to guide them in their career choices. Moreover, institutions are responding by implementing virtual residency interviews. Measuring the efficacy of the virtual interview would be highly beneficial to residency programs across specialties and national organizations seeking to streamline the application process. These efforts will become increasingly important given the state of flux concerning standardized testing. To receive their medical license, medical students must complete the USMLE Step 1 exam, which focuses on applying scientific concepts to medicine. They must also complete the USMLE Step 2 exam, which tests clinical knowledge (Step 2 CK) and clinical skills (Step 2 CS), and the Step 3 exam which tests the ability to function as an independent medical practitioner. With the upcoming transition of the USMLE Step 1 examination to a pass/fail system1 and the recent postponement of USMLE Step 2 CS of over a year2, uncertainty will continue to build for both students and residency directors. Program directors will need to devise new means of filtering through large pools of applicants.
For students, this is yet another change to which they must adapt. When obstacles like inadequate exposure to neurology (Gupta et al., 2013) and neurophobia (Humbert and Chang, 2014; Abushouk and Duc, 2016; Sandrone et al., 2019a) already threaten the neurology pipeline, it is crucial to identify factors impacting neurology specialty choice during COVID-19. Recent survey data have identified cancellations of networking opportunities, changes in board exam scoring, and limited clinical experiences due to COVID-19 as major concerns for students applying into neurosurgery residency (Garcia et al., 2020; Guadix et al., 2020). Similar methods can be used to outline concerns of neurology-minded medical students at each stage of their training to which specific interventions can be tailored.
Transferring clinical education to a telehealth platform poses new challenges to neurology, a specialty that is highly dependent on physical interaction with the patient and the intricacies of the neurological exam. Certain parts of the exam are easily translatable to the digital interface, such as mental status, eye movement/facial symmetry evaluations, gait exam, and parts of the standardized movement disorders exam such as evaluation of tremor and bradykinesia. However, components such as the sensory exam, formal muscle strength testing, tone, and reflex evaluation, do not translate as easily. These limitations lessen the efficacy of learning the exam through a virtual format. At the same time, history taking skills can still be honed by having students independently take patient histories and observing them during the virtual encounter. Going forward, it will be essential to obtain data on the efficacy of these teaching methods through surveys and objective measures that elicit participant perspectives and educational impact. By doing so, we can better identify which virtual teaching strategies have been most effective, potentially incorporating elements of virtual learning into the post-COVID curriculum.
After a forced hiatus in basic science research beginning in early March, WCM laboratories began the process of re-opening in June with restrictions on personnel capacity. In place of lab-based research, neurology clinical research electives at WCM helped students stay current with a continually evolving body of literature during the pandemic. One example is a 4-week movement disorders research elective examining attitudes of patients with Parkinson's disease toward deep brain stimulation. Designed with the goal of submitting results for publication at the end of the 4-week period, this elective provided a structured research experience for students to engage with and contribute to the existing neurology literature.
A further consequence of the COVID-19 pandemic for research-minded students is the movement of major research conferences to online platforms such as those hosted by the American Academy of Neurology and the American Neurological Association (ANA). Conference cancellations have recently been cited as a significant concern, particularly for students early in their medical training who may miss vital networking opportunities with leaders in the neurosciences (Guadix et al., 2020). A potential strategy to complement the AAN and ANA virtual conferences that provides medical students with a platform to showcase their work is encouraging medical student presentations at departmental virtual Grand Rounds. Already adopted by various WCM departments, this method creates natural opportunities for networking among students and faculty and for students to receive immediate feedback from faculty members over a virtual conferencing platform.
COVID-19 has fundamentally changed the nature of medical education in the past few months. While it has taken students away from the clinical setting, it has also provided a powerful impetus to think creatively about neurology education and patient care in the 21st century. Neurology departments have begun to respond by creating telehealth courses and providing virtual lecture series for interested students. Initiatives designed by the WCM neurology department to maintain student engagement as described above are summarized in Table 1.
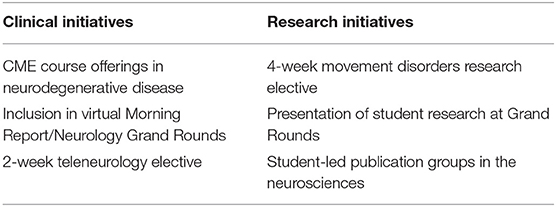
Table 1. Clinical and research initiatives offered for students by the neurology department at Weill Cornell Medicine during COVID-19.
Despite these impressive innovations in medical education, COVID-19 has also created new personal challenges for students, such as caring for family members affected by the virus and coping with death for the first time. Students may be facing these difficulties during a time of profound isolation from the support network in their medical school community, with those of minority background and lower socioeconomic status likely being hit the hardest (Galea, 2020). Medical student burnout has been cited in 45–71% of medical students at major institutions and has been linked to clerkship disorganization and low perceived levels of support from faculty (Ishak et al., 2013). It is reasonable to assume that burnout is likely exacerbated during these isolative and anxiety-producing circumstances (Shaw, 2020). These difficulties highlight the necessity of bringing medical student wellness to the forefront of education. In response, WCM has increased student and faculty access to virtual psychotherapy services. The WCM psychiatry liaison service, besides offering a student elective, also hosted virtual town halls to raise student and faculty awareness of psychiatry resources, while providing support in coping with stress, guilt, and loss during the pandemic.
Furthermore, isolation and distance learning have limited peer-to-peer learning traditionally found in small group-based settings. Increasing collaboration between student groups at different institutions, such as through Student Interest Group in Neurology (SIGN) chapters, could be a powerful intervention moving forward. Virtual inter-institutional SIGN meetings can bring together students from around the country, providing a collaborative learning space and forum to express concerns resulting from COVID-19. The wide-reaching SIGN network can also improve access to neurological subspecialties in a time when students across the country face restrictions in completing away electives. Student town halls during inter-institutional SIGN meetings can also help acknowledge and alleviate anxieties during this time, while simultaneously offering a platform for students to dialogue with supportive faculty mentors and brainstorm educational solutions. For example, in 2019, WCM hosted an inaugural SIGN inter-institutional event, which provided a space for students in the NYC area to share their research in the neurosciences with their peers, residents, and faculty sponsors. This can be re-imagined virtually on a larger scale during the COVID-19 era for peer-to-peer learning in neurology. In addition, the formation of student-led publication groups has increased student research productivity during this time in other departments (Chae et al., 2020). SIGN groups can implement the publication group model either intra- or inter-institutionally.
Moreover, these meetings would present a golden opportunity to implement the flipped classroom model in neurology, both for clinical topics as well as neuroscience research. The flipped classroom model, which moves knowledge gathering outside of the classroom and facilitated discussion into the classroom, gained traction around 2012 and has since become increasingly more popular in education (Sandrone et al., 2019b). Although in the past the flipped classroom has been shown to increase students' motivation and class attendance, students have cited the lack of time to complete prerequisite work as a significant barrier (Sandrone et al., 2019a). Thus, the increased flexibility of medical students' schedules during COVID-19 may make this model a particularly suitable approach (Sandrone and Schneider, 2020; Sandrone et al., 2020). In addition, virtual platforms with built-in chat functions and breakout rooms mimic small-group learning and may make students who felt socially inhibited from contributing in more traditional in-person settings more comfortable. Despite these advances, virtual learning through a flipped classroom model carries unique challenges. For example, as classrooms become increasingly more virtual, students and educators alike may suffer from fatigue and feel distanced from engaging with the conversations. One concrete way to implement the flipped classroom model into inter-institutional SIGN meetings would be to have students present neurology concepts and work through clinical cases through student-led workshops and problem-based learning sessions. The virtual medium would allow for collaboration among students from different institutions who approach problem from unique perspectives given their diverse training backgrounds.
At the national level, it is crucial for neurology organizations to engage in a dialogue with medical students to understand what educational interventions would be most beneficial for them at each stage of their medical education. Based on previous reports (Guadix et al., 2020), early-year students interested in the neurosciences would likely benefit from the expansion of virtual mentorship programs similar to those offered by the AAN, among other interventions. However, it is less clear what initiatives would be most beneficial to more senior medical students applying for neurology residency programs. Using a comprehensive, data-driven approach, medical student concerns and ideas can be gathered through nationwide surveys and focus groups to better understand how students feel their neurology education is being most impacted by COVID-19, broadening our single-center experience.
Despite the uncertainty, the COVID-19 pandemic has triggered a newfound spark for innovation in neurology education. It has also given medical students the space to reflect on what matters most to them, providing them with more flexibility to craft their own schedules. Students at large academic institutions such as WCM have had increasing opportunities to engage in teleneurology and neurology research from afar. Increased inter-institution collaboration would provide students from smaller institutions a chance to experience more diverse neurological cases and subspecialties. With these newfound opportunities, medical students can continue to pursue their interests in neurology and resume their development as future physicians during this uncertain time.
SG and CS: methodology, conceptualization, writing–original draft, and writing—review and editing. SS, JS, and HS: methodology, conceptualization, and writing—review and editing. All authors contributed to the article and approved the submitted version.
HS has financial disclosures unrelated to this work. She has received clinical trial support from Biogen, Lundbeck, Intec, Insightec, and Covance pharmaceuticals as well as some research support from the Michael J. Fox Foundation and the NIH. In addition, she has served as a consultant for Merz, Accorda, Neurocrine, and Amneal Pharmaceuticals.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. ^InCUS: Invitational Conference on USMLE Scoring. (n.d.). Retrieved from https://www.usmle.org/incus/.
2. ^Announcements. (n.d.). Retrieved from https://www.usmle.org/announcements/?ContentId=267.
Abushouk, A. I., and Duc, N. M. (2016). Curing neurophobia in medical schools: evidence-based strategies. Med. Educ. Online 21:32476. doi: 10.3402/meo.v21.32476
Al Kasab, S., Almallouhi, E., and Holmstedt, C. A. (2020). Optimizing the use of teleneurology during the COVID-19 pandemic. Telemed. J. E Health 26, 1197–1198. doi: 10.1089/tmj.2020.0109
American Association of Colleges of Osteopathic Medicine (2019). 2018–2019 Academic Year Graduating Seniors Summary Report. American Association of Colleges of Osteopathic Medicine.
Chae, J. K., Haghdel, A., Guadix, S. W., Winston, G. M., Younus, I., Radwanski, R., et al. (2020). Letter: COVID-19 Impact on the medical student path to neurosurgery. Neurosurgery 87, E232–E233. doi: 10.1093/neuros/nyaa187
Dorsey, E. R., Glidden, A. M., Holloway, M. R., Birbeck, G. L., and Schwamm, L. H. (2018). Teleneurology and mobile technologies: the future of neurological care. Nat. Rev. Neurol. 14, 285–297. doi: 10.1038/nrneurol.2018.31
Galea, S. (2020). Compassion in a time of COVID-19. Lancet 395, 1897–1898. doi: 10.1016/S0140-6736(20)31202-2
Garcia, R. M., Reynolds, R. A., Weiss, H. K., Chambless, L. B., Lam, S., Dahdaleh, N. S., et al. (2020). Letter: preliminary national survey results evaluating the impact of COVID-19 Pandemic on medical students pursuing careers in neurosurgery. Neurosurgery 87, E258–E259. doi: 10.1093/neuros/nyaa214
Guadix, S. W., Winston, G. M., Chae, J. K., Haghdel, A., Chen, J., Younus, I., et al. (2020). Medical student concerns relating to neurosurgery education during COVID-19. World Neurosurg. 139, e836–e847. doi: 10.1016/j.wneu.2020.05.090
Gupta, N. B., Khadilkar, S. V., Bangar, S. S., Patil, T. R., and Chaudhari, C. R. (2013). Neurology as career option among postgraduate medical students. Ann. Indian Acad. Neurol. 16, 478–482. doi: 10.4103/0972-2327.120427
Humbert, K. A., and Chang, B. S. (2014). In the beginning: how medical students choose (or do not choose) neurology. Ann. Neurol. 75, 487–489. doi: 10.1002/ana.24133
Ishak, W., Nikravesh, R., Lederer, S., Perry, R., Ogunyemi, D., and Bernstein, C. (2013). Burnout in medical students: a systematic review. Clin. Teach. 10, 242–245. doi: 10.1111/tct.12014
Klein, B. C., and Busis, N. A. (2020). COVID-19 is catalyzing the adoption of teleneurology. Neurology 94, 903–904. doi: 10.1212/WNL.0000000000009494
National Resident Matching Program (2020). Results and Data: 2020 Main Residency Match®. Washington, DC: National Resident Matching Program.
Sandrone, S., Berthaud, J. V., Carlson, C., Cios, J., Dixit, N., Farheen, A., et al. (2019a). Education research: flipped classroom in neurology: principles, practices, and perspectives. Neurology 93, e106–e111. doi: 10.1212/WNL.0000000000007730
Sandrone, S., Berthaud, J. V., Carlson, C., Cios, J., Dixit, N., Farheen, A., et al. (2020). Strategic considerations for applying the flipped classroom to neurology education. Ann. Neurol. 87, 4–9. doi: 10.1002/ana.25609
Sandrone, S., Berthaud, J. V., Chuquilin, M., Cios, J., Ghosh, P., Gottlieb-Smith, R. J., et al. (2019b). Neurologic and neuroscience education: mitigating neurophobia to mentor health care providers. Neurology 92, 174–179. doi: 10.1212/WNL.0000000000006716
Sandrone, S., and Schneider, L. D. (2020). Active and distance learning in neuroscience education. Neuron 106, 895–898. doi: 10.1016/j.neuron.2020.06.001
Shaw, S. (2020). Hopelessness, helplessness and resilience: The importance of safeguarding our trainees' mental wellbeing during the COVID-19 pandemic. Nurse education in practice, 44, 102780. https://doi.org/10.1016/j.nepr.2020.102780
Keywords: COVID-19, neurology, education, medical student, clerkship, virtual education, medical curriculum
Citation: Guadix SW, Sha C, Sandrone S, Safdieh JE and Sarva H (2020) The Impact of COVID-19 on Neurology Education: A Medical Student Perspective. Front. Educ. 5:567421. doi: 10.3389/feduc.2020.567421
Received: 29 May 2020; Accepted: 07 December 2020;
Published: 23 December 2020.
Edited by:
Michelle Diane Young, Loyola Marymount University, United StatesReviewed by:
Joe Donaldson, University of Missouri, United StatesCopyright © 2020 Guadix, Sha, Sandrone, Safdieh and Sarva. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sergio W. Guadix, c3dnNDAwMUBtZWQuY29ybmVsbC5lZHU=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.