- 1Cardiovascular Center, Children’s Hospital of Fudan University, Shanghai, China
- 2Fujian Key Laboratory of Neonatal Diseases, Xiamen Children’s Hospital, Fujian, China
- 3Shanghai Key Laboratory of Birth Defects, Shanghai, China
- 4Unit of Early Intervention of Genetically Related Childhood Cardiovascular Diseases, Shanghai, China
Introduction: Noncardiac anomalies (NCAs) in patients with congenital heart defects (CHDs) are crucial for perioperative management and etiology studies. This study aimed to investigate NCAs in Chinese children with CHDs.
Methods: Medical records for CHD-diagnosed children hospitalized from 1 January 2015 to 31 December 2019 were collected and subjected to retrospective analyses to excavate potential association rules between CHDs and noncardiac malformations.
Results: A total of 3,788 CHD patients were included in this study. The main phenotypes of CHD were Ventricular Septal Defect (VSD, 33.69%), Atrial Septal Defect (ASD, 12.72%), and Tetralogy of Fallot (TOF, 5.54%). A total of 887 (23.42%) cases showed noncardiac anomalies, which were mainly associated with the central nervous system (34.61%), nose/ear/mandibular/face (19.39%), genitourinary system (15.78%), and musculoskeletal system (15.56%). Compared to other CHD subtypes, septal defects had a lower percentage of associated NCAs (P = 3.7 × 10−9) while AVSD had a higher percentage (P = 0.0018).
Disscussion: NCAs are prevalent among CHD-diagnosed children in China, and the spectrums of NCAs in different CHD subcategories were different.
1. Introduction
Congenital heart defects (CHDs) are a leading cause of infant mortality and the most commonly diagnosed major congenital anomaly worldwide (1, 2) with a prevalence of 8.98 per 1,000 live births in China (3). Although diagnostic capabilities and surgical strategies have significantly advanced, CHD remains a costly and onerous disease burden in many countries (4, 5). CHDs manifest as diverse structural abnormalities of the heart and great vessels that arise during embryonic development. The complexity of structural anomalies, defect severity, and the presence of comorbidities are essential determinants of CHD outcomes (6).
It is important to identify whether a CHD presents as an isolated condition or has developed in combination with noncardiac anomalies, as is frequently the case. Multiple organs originate from a common germ layer and can be regulated by shared signaling pathways (7). Moreover, chromosomal aberrations, which represent a leading cause of CHDs, alter the activities of multiple genes that may have different functions in embryogenesis. CHD comorbidities affecting other systems have a significant impact on clinical course. Despite advances in cardiac surgery and perioperative management, Eskedal et al. (8) reported that survival has not improved for CHD-diagnosed children with extracardiac anomalies. A 15-year follow-up study showed that noncardiac anomalies (NCAs) had a more significant effect on mortality in patients with CHDs than potential heart disease (9). Indeed, some have recommended that prediction modeling of thoracic surgery mortality risk for CHD patients could be augmented by adding a covariate that represents noncardiac congenital anatomic abnormalities (10). NCAs can increase the risk of postoperative complications, such as respiratory complications with heterotaxy (11), and children with CHD undergoing noncardiac surgery can have an increased mortality risk (12). Consequently, to identify optimal perioperative and long-term management of patients with CHDs and to elucidate the etiology of congenital defects, a detailed description of coexisting NCAs in children with CHD is necessary.
Reported frequencies of NCAs in CHD-diagnosed patients range widely from 4.53% to 50% (13–15). Different types of CHD are associated with distinct incidences of extracardiac comorbidities. For example, the NCA risk has been reported to be elevated among CHD patients with a cardiac looping defect, conotunal defect (CTD), or atrial septal defect (ASD) and reduced among CHD patients with a ventricular septal defect (VSD) or Ebstein anomaly (16, 17). Moreover, specific associations have been identified between common truncus and limb reduction defects and between great vessel-transposition and situs inversus (18). Piran found a trend toward a higher prevalence of major congenital extracardiac anomalies involving the musculoskeletal and genitourinary systems in adults with tetralogy of Fallot (TOF) (19). Thus far, there are limited data in the literature regarding the occurrence of NCAs in CHD-diagnosed children in China, and this study aimed to describe the proportions and distributions of NCAs in Chinese children of Han ethnicity who have been diagnosed with a CHD.
2. Materials and methods
2.1. Study population
Children diagnosed with a CHD and hospitalized in the Department of Cardiac Surgery, Children's Hospital of Fudan University from 1 January 2015 to 31 December 2019 were eligible for inclusion. Data collection and analysis processes were conducted with the permission of and under the guidance of the ethics committee. Written informed consent to participate was obtained from the guardians. Medical histories, surgical records, imaging data, outpatient medical records, and genetic test results of enrolled patients were collected and examined retrospectively. CHD diagnoses were confirmed by clinical assessment, echocardiography, cardiac catheterization, and, if necessary, surgical observations. Patent foramen ovale, patent ductus arteriosus (PDA) in premature infants, and a PDA that resolved within 3 months after birth were excluded. The analyses did not include patients with cardiomyopathies, cardiac arrhythmias, or primary pulmonary hypertension.
2.2. Phenotype classification
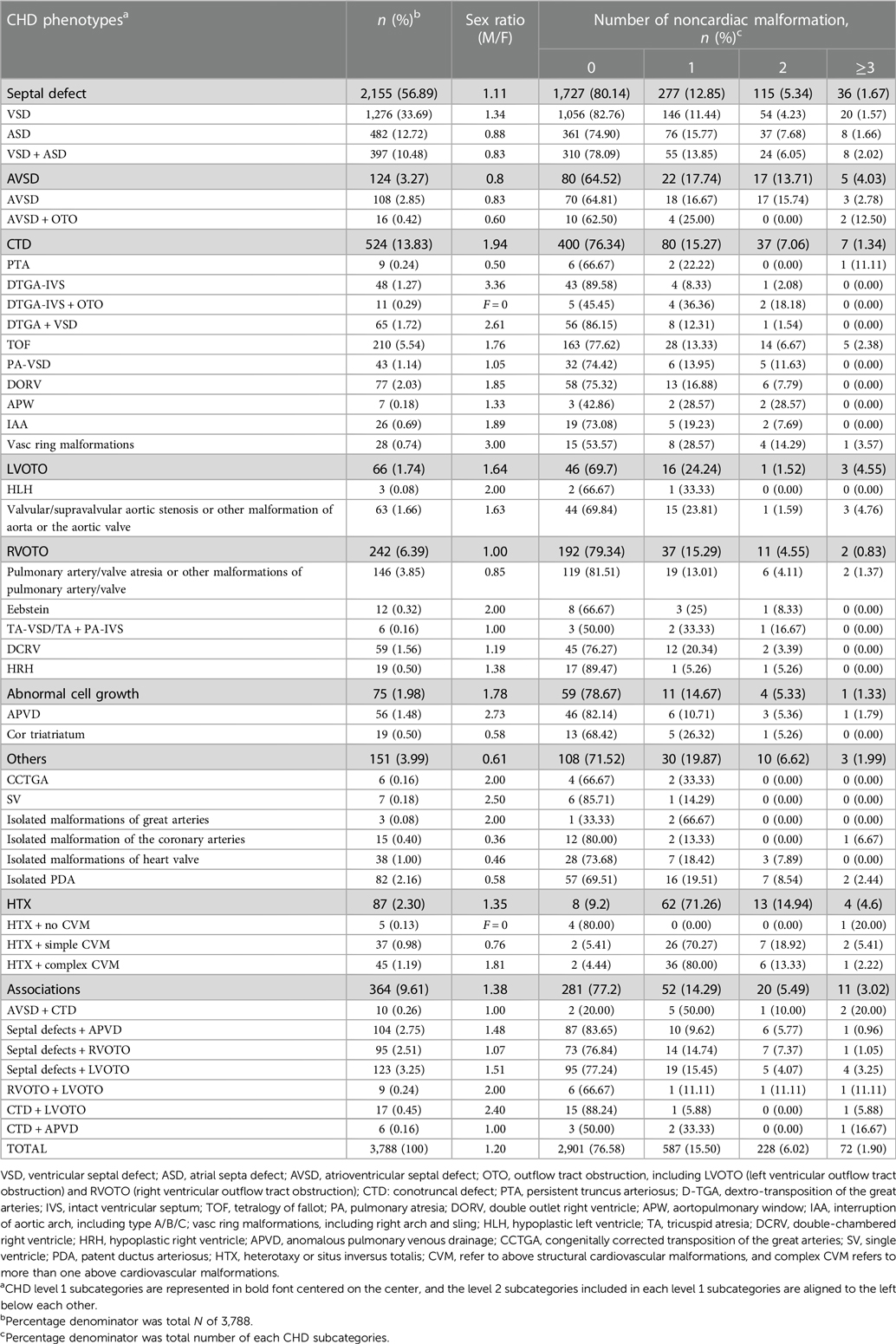
Individual patients' CHDs were classified based on anatomy and etiology (20–23) into the level 1 and 2 categories (Table 1), where the latter are subcategories of the former. Level 1 categories included the following: septal defects, atrioventricular canal defect (AVSD), conotruncal cardiac defect (CTD), left ventricular outflow tract obstruction (LVOTO), right ventricular outflow tract obstruction (RVOTO), abnormal cell growth, heterotaxy (HTX), others, and associations.
Diagnosed NCAs were summarized and aggregated according to affected systems. All developmental delays, including growth retardation, intellectual disability, mental delays, learning difficulties, and language/motor deficits, were classified as central nervous system (CNS) anomalies (24). We ignored syndrome diagnoses to focus on phenotypes. Syndrome-associated noncardiac phenotypes were disassociated and classified according to their respective affected systems. Anomalies within the same affected system were counted as one. CHD cases with and without NCAs are referred to as associated CHD cases and isolated CHD cases, respectively.
2.3. Statistical analysis
R (version 4.1.2), R Studio (version 1.4.1717), and SPSS (IBM version 20) were used for statistical analysis. Analysis of description was used to provide the whole picture of CHD and NCAs; Pearson's χ2 test or Fisher's exact test was applied to compare the proportions of isolated CHD between different genders and different CHD subtypes. The apriori principle (25) was used to analyze CHD diagnosis-to-NCA association, setting thresholds for support and confidence at 0.01 and 0.1, respectively. Rules with a lift ≥ 3 were considered of value.
3. Results
3.1. Proportions of congenital heart defects
A total of 3,788 CHD-diagnosed children were identified retrospectively, of which 2,065 (54.51%) were male and 1,723 were female (45.49%) with a median age of 3.96 years (IQR, 2.56–5.39). The proportions of level 1 and level 2 diagnostic classifications are reported in Table 1 with sex ratios and the number of co-occurring anomalies. The most common level 1 diagnoses were septal defect (56.89%), CTD (13.83%), and RVOTO (6.39%); besides different septal defects TOF (5.54%), pulmonary artery/valve atresia or other malformations of the pulmonary artery/valve (3.85%), DORV (2.03%), valvular/supravalvular aortic stenosis or other malformation of the aorta or the aortic valve (1.66%), and dextro-transposition of the great arteries (D-TGA, 1.27%) were common level 2 diagnoses. Furthermore, 3.25% children had both septal defects and LVOTO and 2.75% children had septal defects and RVOTO.
3.2. Noncardiac malformations in children with CHDs
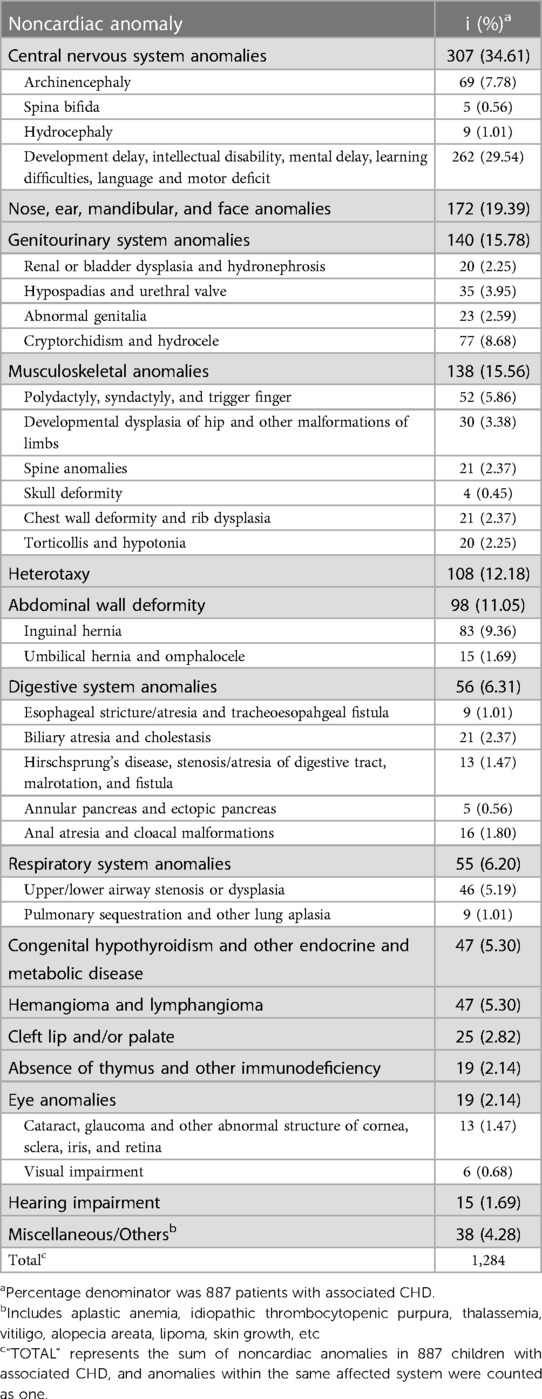
A total of 887 (23.42%) cases of CHD were associated with noncardiac malformations, comprising 587 (15.50%) with one malformation, 228 (6.02%) with two malformations, and 72 (1.90%) with three or more malformations (Table 1).There were 1,284 noncardiac malformations among the 887 children, including 307 (34.61%) in the nervous system, 172 (19.39%) in the nose/ear/mandibular/face, and 140 (15.78%) in the musculoskeletal system (Table 2). The most common discrete NCA phenotype by far was developmental delay (n = 262, 29.54%), inguinal hernia (n = 83, 9.36%), and cryptorchidism and hydrocele (n = 77, 8.68%).
3.3. NCA spectra for CHD subcategories
The level 1 diagnoses with the highest percentages of isolated CHDs were septal defects, wherein about four fifths of each were isolated (Table 1). Conversely, besides heterotaxy, the diagnosis with the greatest percentage of associated CHDs was AVSD, wherein almost two fifths of the patients have associated CHDs (Table 1). Statistical analysis proved that septal defects, especially VSD (P = 3.7 × 10−9) and D-TGA with an intact ventricular septum (D-TGA + IVS, P = 0.038), are less likely to associated with NCAs. Furthermore, there were a higher probability of combined NCAs in children with AVSD (P = 0.002) and vasc ring malformations (P = 0.007).
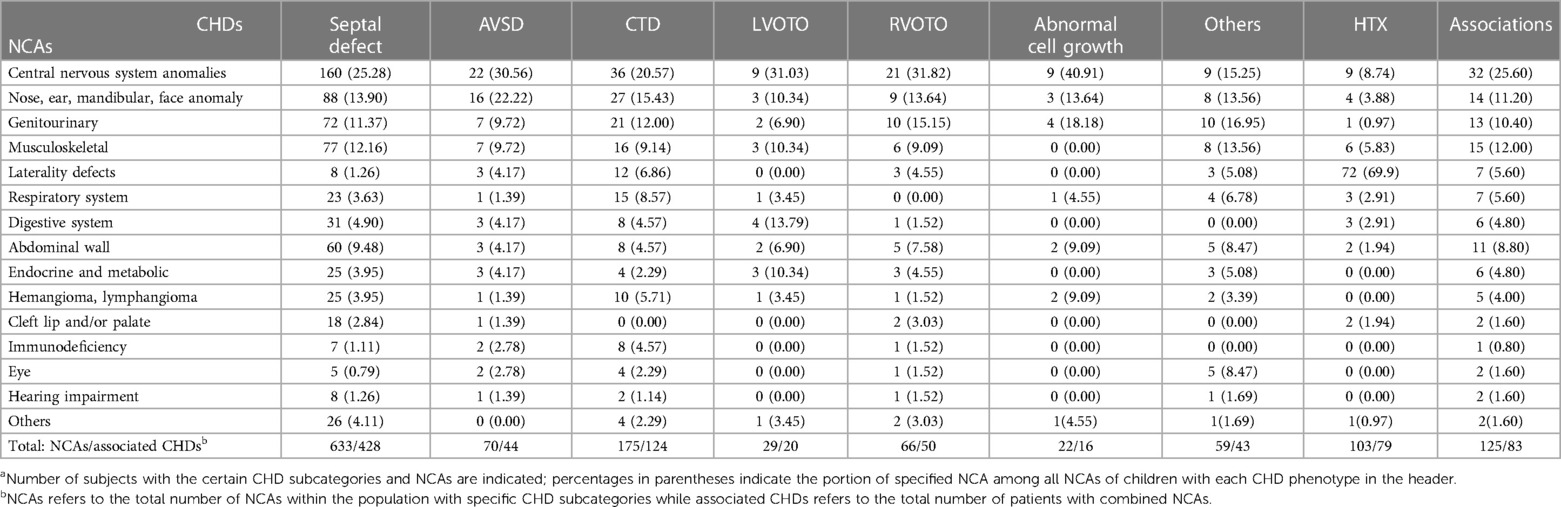
Although NCAs involving the CNS, nose/ear/mandibular/face, genitourinary system, and musculoskeletal system were common for most CHD subtypes, the distribution of NCAs differed slightly (Table 3). NCAs affecting the CNS were most frequently observed in AVSD and RVOTO cases, wherein approximately one third of patients were affected. Nose/ear/mandibular/face anomalies were observed in more than one fifth of AVSD cases. Children in groups of septal defects or groups of associations showed relatively larger proportions of combined musculoskeletal anomalies (12.16% and 12.00%) and abdominal wall deficiency (9.48% and 8.80%). Genitourinary malformations were less prevalent in LVOTO-diagnosed children whereas respiratory system NCAs and digestive system NCAs were apparently common in children with CTD and LVOTO, respectively. Laterality defects were notably common in heterotaxy cases and, albeit to a lesser extent, CTD cases (Table 3). Furthermore, taking gender into account, among children with septal defects, especially those with VSD, PA-VSD, pulmonary artery/valve atresia, or other malformation of the pulmonary artery/valve and double-chambered right ventricule (DCRV), males were more likely to have associated CHD than females (P < 0.05), whereas the situation is opposite in LVOTO and RVOTO diagnostic groups.
3.4. Co-occurrence of CHDs and NCAs
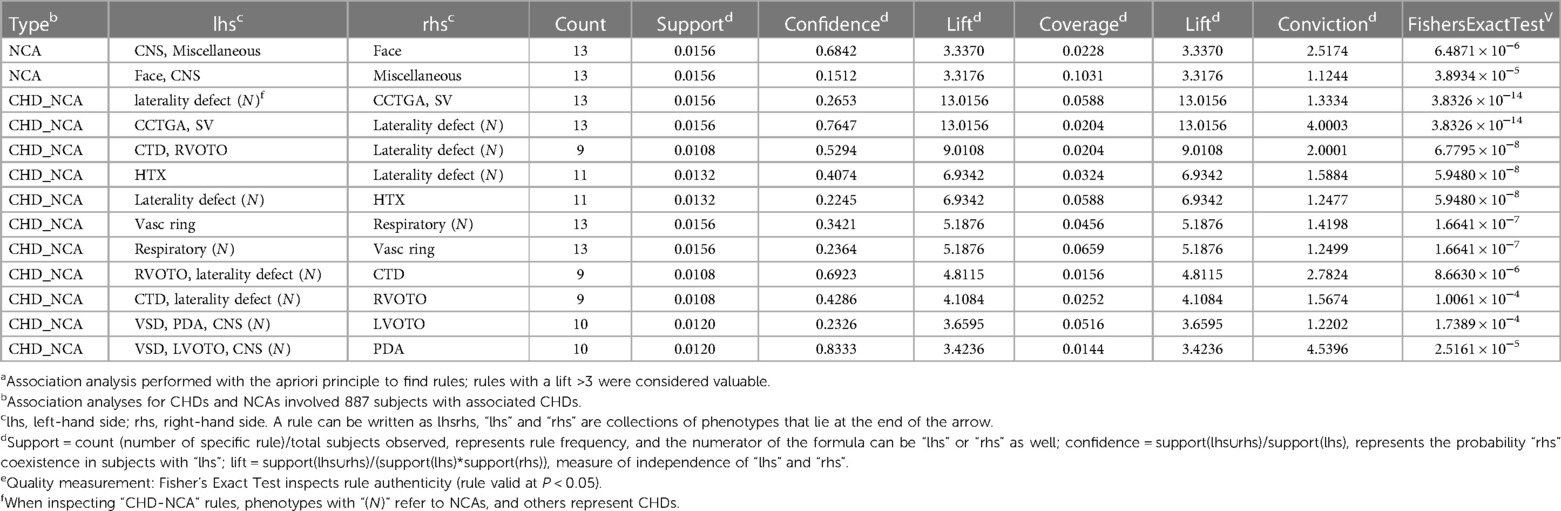
With support and confidence levels set to 0.01 and 0.1, respectively, we attained 213 rules between CHD subtypes and NCAs. After filtering out low-value rules (lift < 3), 11 rules were retained (Table 4), showing the reliability or value of the rule which indicated the following potential CHD–NCA co-occurrence relationships: CCTGA-SV–laterality defect (lift = 13.02); CTD, RVOTO–laterality defect NCA (lift = 9.01); heterotaxy–laterality defect NCA (lift = 6.93); vasc ring malformations–respiratory system NCA (lift = 5.19); VSD, PDA, and CNS anomalies-LVOTO (lift = 3.66).
4. Discussion
In the present study sample, 23.42% of CHD diagnosed children had coexisting NCAs, a value about midway between the wide range of percentages reported in the literature (4.53%–50%) (13–15) and somewhat similar to percentages obtained in extensive studies conducted in the city of Atlanta, GA in the USA (28.7%), the province of Alberta in Canada (25%), and Croatia (14.5%) (16, 26, 27). The wide range of findings reported in this regard may be attributed to different classifications, inclusion/exclusion criteria, and screening strategies. Stoll and colleagues reported that the incidence of NCAs co-occurring with CHDs was 24.2% in live births, 66.3% in stillbirths, and 69.4% in abnormal pregnancy terminations (21). The subjects in our study were all live births. The definition of associated CHD differs between studies as well. Some defined an associated CHD as an extracardiac or genetic abnormality (16, 21). In our study, we included anomalies affecting other organs but not genetic abnormalities. Consequently, the data are not fully comparable across different studies due to different methodologies. Nevertheless, the proportion of congenital defects was dramatically more significant than the prevalence of congenital defects for China's population as a whole (191.84/10,000) (28), which suggests that CHDs may be a risk factor for other defects and that a considerable number of children with CHDs have NCAs.
Our findings indicating that the most common NCAs observed were CNS anomalies, nose/ear/mandibular/face anomalies, genitourinary system anomalies, and musculoskeletal system anomalies are largely in agreement with previous reports (14, 21, 29–31). However, we observed relatively low percentages of gastrointestinal anomalies (6.31%) and respiratory system anomalies (6.20%), the ranges for which in the literature are 8%–35% and 2%–14%, respectively, but a relatively high percentage of nose/ear/mandibular/face anomalies (19.39%) (8, 14, 15, 18, 32–39). Divergences from prior reports may have several underlying causes. Firstly, we excluded stillbirths, fetal deaths, and pregnancy terminations, which are more likely to involve lethal and major anomalies than live births. Secondly, we included several minor NCAs that are often excluded in other literature (e.g., low set ears, atypical facial appearance, and high arched palate) because how little of an effect they have on prognoses. Lastly, we deconstructed phenotypes of known syndromes as discrete NCAs. Most syndromes that commonly present with CHDs—including Down syndrome, DiGeorge syndrome, and Turner syndrome—have clinically significant NCAs, such as development delays, atypical facial features, skeletal deformities, and genitourinary system anomalies (40); these syndromes explain in part the top four NCAs in our results. CNS anomalies, including development delays, account for a large portion of the NCAs observed in our study (Table 2). Because neurodevelopment is highly sensitive to oxygen, any cardiac defect that disturbs hemodynamics and oxygen transport has the potential to cause CNS anomalies. In addition, development delays continue to manifest with increasing child age; our study sample has a median age of 3.96 years (IQR, 2.56–5.39), providing recognition of NCAs with progressive symptoms that are not yet apparent in the fetal and infant stages. Furthermore, adverse neurodevelopmental outcomes after surgical repair of CHDs represent a clinically significant cause of morbidity. Indeed, neuropsychological deficits may occur in as many as 50% of children who undergo CHD repairs by the time they reach school age (41). Early diagnosis of CNS anomalies in this patient population would be of great benefit to perioperative management.
Regarding NCA risk among different CHD phenotypes, we found that AVSD, PTA, vasc ring malformations, LVOTO, and heterotaxy had relatively high incidences of associated NCAs, whereas VSD and APVD had relatively low incidences. It could be that CHDs that emerge in earlier stages of morphogenesis are more likely to be associated with multiple and complex defects (42). Boundaries between tissues are blurred in early development, and regulatory molecular signaling pathways affect the development of many organs simultaneously.
Our finding of a specific link between VSD/LVOTO/PDA presence and CNS anomalies should be explored. Interestingly, the impact of AVSDs on CNS anomalies and nose/ear/mandibular/face anomalies could potentially relate to the well-known correlation between AVSDs and Down syndrome (32, 43, 44). The finding that vasc ring anomalies (including right arch and sling) often co-occurred with malformations of the respiratory system was unsurprising given the oppression of the malformed arteries on the trachea. Theoretically, most CHD-associated NCAs should have an etiological explanation, such as a mesoderm differentiation event that causes CHD and musculoskeletal defects simultaneously (16). The detailed mechanisms underlying the breadth of co-occurring anomalies have yet to be delineated.
5. Limitation
It was difficult to conduct a stratified analysis to correct for confounding factors as we did not obtain data related to risk factors for birth defects. We also did not capture associated CHD patterns in rural China, where there is a high prevalence of unrecognized CHDs (32). Thirdly, our sample included relatively few rare CHDs and NCAs, which may weaken the analyses.
6. Conclusion
Han Chinese children with CHDs were found to have a high prevalence of NCAs, including CNS, nose/ear/mandibular/face, and musculoskeletal anomalies. Different CHD subtypes had different NCA probabilities and spectrums. Compared to other CHD subtypes, septal defects had a lower percentage of associated NCAs while AVSD had a higher percentage. Clinicians treating patients with CHDs should be attentive to the risk of NCAs, particularly for perioperative management but also for long-term prognosis determination.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Materials, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Fudan University Children's Hospita. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
XH: Data curation, Formal Analysis, Investigation, Writing – original draft. YG: Formal Analysis, Investigation, Methodology, Writing – original draft. WC: Project administration, Resources, Supervision, Writing – review & editing. WS: Formal Analysis, Project administration, Resources, Supervision, Writing – review & editing. GH: Conceptualization, Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This research was supported by the National Key Research and Development Program of China (grant no. 2021YFC2701000, 2016YFC1000500), the National Natural Science Foundation of China (grant no. 82270321, 81873482, 81873483), the Shanghai Natural Science Foundation of Science and Technology Innovation Action Plan (grant no. 20JC1418300), and the CAMS Innovation Fund for Medical Sciences (grant no. 2019-I2M-5-002).
Acknowledgments
The authors thank for the support from National Key Research and Development Program of China and National Natural Science Foundation of China. We also thank all the patients and families for their understanding and support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Nees SN, Chung WK. Genetic basis of human congenital heart disease. Cold Spring Harb Perspect Biol. (2020) 12(9):a036749. doi: 10.1101/cshperspect.a036749
2. Szot JO, Cuny H, Blue GM, Humphreys DT, Ip E, Harrison K, et al. A screening approach to identify clinically actionable variants causing congenital heart disease in exome data. Circ Genom Precis Med. (2018) 11(3):e001978. doi: 10.1161/CIRCGEN.117.001978
3. Zhao QM, Liu F, Wu L, Ma XJ, Niu C, Huang GY. Prevalence of congenital heart disease at live birth in China. J Pediatr. (2019) 204:53–8. doi: 10.1016/j.jpeds.2018.08.040
4. GBD 2017 Congenital Heart Disease Collaborators. Global, regional, and national burden of congenital heart disease, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet Child Adolesc Health. (2020) 4(3):185–200. doi: 10.1016/s2352-4642(19)30402-x
5. Sun M, Wang T, Huang P, Diao J, Zhang S, Li J, et al. Association analysis of maternal MTHFR gene polymorphisms and the occurrence of congenital heart disease in offspring. BMC Cardiovasc Disord. (2021) 21(1):298. doi: 10.1186/s12872-021-02117-z
6. Chang CS, Hong SY, Kim SY, Kim YM, Sung JH, Choi SJ, et al. Prevalence of associated extracardiac anomalies in prenatally diagnosed congenital heart diseases. PLoS One. (2021) 16(3):e0248894. doi: 10.1371/journal.pone.0248894
7. Morton SU, Quiat D, Seidman JG, Seidman CE. Genomic frontiers in congenital heart disease. Nat Rev Cardiol. (2022) 19(1):26–42. doi: 10.1038/s41569-021-00587-4
8. Eskedal L, Hagemo P, Eskild A, Aamodt G, Seiler KS, Thaulow E. A population-based study of extra-cardiac anomalies in children with congenital cardiac malformations. Cardiol Young. (2004) 14(6):600–7. doi: 10.1017/S1047951104006043
9. Afilalo J, Therrien J, Pilote L, Ionescu-Ittu R, Martucci G, Marelli AJ. Geriatric congenital heart disease: burden of disease and predictors of mortality. J Am Coll Cardiol. (2011) 58(14):1509–15. doi: 10.1016/j.jacc.2011.06.041
10. Jacobs JP, O'Brien SM, Hill KD, Kumar SR, Austin EH 3rd, Gaynor JW, et al. Refining the society of thoracic surgeons congenital heart surgery database mortality risk model with enhanced risk adjustment for chromosomal abnormalities, syndromes, and noncardiac congenital anatomic abnormalities. Ann Thorac Surg. (2019) 108(2):558–66. doi: 10.1016/j.athoracsur.2019.01.069
11. Swisher M, Jonas R, Tian X, Lee ES, Lo CW, Leatherbury L. Increased postoperative and respiratory complications in patients with congenital heart disease associated with heterotaxy. J Thorac Cardiovasc Surg. (2011) 141(3):637–44. 44 e1-3. doi: 10.1016/j.jtcvs.2010.07.082
12. Faraoni D, Zurakowski D, Vo D, Goobie SM, Yuki K, Brown ML, et al. Post-operative outcomes in children with and without congenital heart disease undergoing noncardiac surgery. J Am Coll Cardiol. (2016) 67(7):793–801. doi: 10.1016/j.jacc.2015.11.057
13. Gonzalez JH, Shirali GS, Atz AM, Taylor SN, Forbus GA, Zyblewski SC, et al. Universal screening for extracardiac abnormalities in neonates with congenital heart disease. Pediatr Cardiol. (2009) 30(3):269–73. doi: 10.1007/s00246-008-9331-z
14. Wojtalik M, Mrowczynski W, Henschke J, Wronecki K, Siwinska A, Piaszczynski M, et al. Congenital heart defect with associated malformations in children. J Pediatr Surg. (2005) 40(11):1675–80. doi: 10.1016/j.jpedsurg.2005.06.004
15. Pastor-Garcia M, Gimeno-Martos S, Zurriaga O, Sorli JV, Cavero-Carbonell C. Congenital heart defects in the valencian community 2007–2014: the population-based registry of congenital anomalies. An Pediatr. (2020) 92(1):13–20. doi: 10.1016/j.anpedi.2018.12.019
16. Miller A, Riehle-Colarusso T, Alverson CJ, Frias JL, Correa A. Congenital heart defects and major structural noncardiac anomalies, Atlanta, Georgia, 1968–2005. J Pediatr. (2011) 159(1):70–8e2. doi: 10.1016/j.jpeds.2010.12.051
17. Pradat P, Francannet C, Harris JA, Robert E. The epidemiology of cardiovascular defects, part I: a study based on data from three large registries of congenital malformations. Pediatr Cardiol. (2003) 24(3):195–221. doi: 10.1007/s00246-002-9401-6
18. Pradat P. Noncardiac malformations at major congenital heart defects. Pediatr Cardiol. (1997) 18(1):11–8. doi: 10.1007/s002469900101
19. Piran S, Bassett AS, Grewal J, Swaby JA, Morel C, Oechslin EN, et al. Patterns of cardiac and extracardiac anomalies in adults with tetralogy of fallot. Am Heart J. (2011) 161(1):131–7. doi: 10.1016/j.ahj.2010.09.015
20. Riehle-Colarusso T, Strickland MJ, Reller MD, Mahle WT, Botto LD, Siffel C, et al. Improving the quality of surveillance data on congenital heart defects in the metropolitan Atlanta congenital defects program. Birth Defects Res A. (2007) 79(11):743–53. doi: 10.1002/bdra.20412
21. Stoll C, Dott B, Alembik Y, Roth MP. Associated noncardiac congenital anomalies among cases with congenital heart defects. Eur J Med Genet. (2015) 58(2):75–85. doi: 10.1016/j.ejmg.2014.12.002
22. Brodwall K, Greve G, Leirgul E, Tell GS, Vollset SE, Øyen N. Recurrence of congenital heart defects among siblings-a nationwide study. Am J Med Genet A. (2017) 173(6):1575–85. doi: 10.1002/ajmg.a.38237
23. Botto LD, Lin AE, Riehle-Colarusso T, Malik S, Correa A. National birth defects prevention study. Seeking causes: classifying and evaluating congenital heart defects in etiologic studies. Birth Defects Res A Clin Mol Teratol. (2007 Oct) 79(10):714–27. doi: 10.1002/bdra.20403
24. Savory K, Manivannan S, Zaben M, Uzun O, Syed YA. Impact of copy number variation on human neurocognitive deficits and congenital heart defects: a systematic review. Neurosci Biobehav Rev. (2020) 108:83–93. doi: 10.1016/j.neubiorev.2019.10.020
25. Kotu V, Deshpande B. Chapter 6 - association analysis. In: Kotu V, Deshpande B, editors. Predictive analytics and data mining. Boston: Morgan Kaufmann (2015). p. 195–216.
26. Lowry RB, Bedard T, Sibbald B, Harder JR, Trevenen C, Horobec V, et al. Congenital heart defects and major structural noncardiac anomalies in Alberta, Canada, 1995–2002. Birth Defects Res A Clin Mol Teratol. (2013) 97(2):79–86. doi: 10.1002/bdra.23104
27. Dilber D, Malcic I. Spectrum of congenital heart defects in Croatia. Eur J Pediatr. (2010) 169(5):543–50. doi: 10.1007/s00431-009-1064-3
28. Xie D, Yang T, Liu Z, Wang H. Epidemiology of birth defects based on a birth defect surveillance system from 2005 to 2014 in Hunan province, China. PLoS One. (2016) 11(1):e0147280. doi: 10.1371/journal.pone.0147280
29. Sørensen KM, El-Segaier M, Fernlund E, Errami A, Bouvagnet P, Nehme N, et al. Screening of congenital heart disease patients using multiplex ligation-dependent probe amplification: early diagnosis of syndromic patients. Am J Med Genet A. (2012) 158a(4):720–5. doi: 10.1002/ajmg.a.35214
30. Simons JS, Glidden R, Sheslow D, Pizarro C. Intermediate neurodevelopmental outcome after repair of ventricular septal defect. Ann Thorac Surg. (2010) 90(5):1586–91. doi: 10.1016/j.athoracsur.2010.06.082
31. Wallgren EI, Landtman B, Rapola J. Extracardiac malformations associated with congenital heart disease. Eur J Cardiol. (1978) 7(1):15–24.648575
32. Meberg A, Hals J, Thaulow E. Congenital heart defects–chromosomal anomalies, syndromes and extracardiac malformations. Acta Paediatr. (2007) 96(8):1142–5. doi: 10.1111/j.1651-2227.2007.00381.x
33. Ferencz C, Rubin JD, McCarter RJ, Boughman JA, Wilson PD, Brenner JI, et al. Cardiac and noncardiac malformations: observations in a population-based study. Teratology. (1987) 35(3):367–78. doi: 10.1002/tera.1420350311
34. Fung A, Manlhiot C, Naik S, Rosenberg H, Smythe J, Lougheed J, et al. Impact of prenatal risk factors on congenital heart disease in the current era. J Am Heart Assoc. (2013) 2(3):e000064. doi: 10.1161/JAHA.113.000064
35. Gallo P, Nardi F, Marinozzi V. Congenital extracardial malformations accompanying congenital heart disease. G Ital Cardiol. (1976) 6(3):450–9.1010196
36. Greenwood RD, Rosenthal A, Parisi L, Fyler DC, Nadas AS. Extracardiac abnormalities in infants with congenital heart disease. Pediatrics. (1975) 55(4):485–92.124046
37. Kenna AP, Smithells RW, Fielding DW. Congenital heart disease in liverpool: 1960–69. Q J Med. (1975) 44(173):17–44.125433
38. Stephensen SS, Sigfusson G, Eiriksson H, Sverrisson JT, Torfason B, Haraldsson A, et al. Congenital cardiac malformations in Iceland from 1990 through 1999. Cardiol Young. (2004) 14(4):396–401. doi: 10.1017/S1047951104004081
39. Baker K, Sanchez-de-Toledo J, Munoz R, Orr R, Kiray S, Shiderly D, et al. Critical congenital heart disease–utility of routine screening for chromosomal and other extracardiac malformations. Congenit Heart Dis. (2012) 7(2):145–50. doi: 10.1111/j.1747-0803.2011.00585.x
40. Pierpont ME, Brueckner M, Chung WK, Garg V, Lacro RV, McGuire AL, et al. Genetic basis for congenital heart disease: revisited: a scientific statement from the American heart association. Circulation. (2018) 138(21):e653–711. doi: 10.1161/CIR.0000000000000606
41. Albers EL, Bichell DP, McLaughlin B. New approaches to neuroprotection in infant heart surgery. Pediatr Res. (2010) 68(1):1–9. doi: 10.1203/PDR.0b013e3181df5402
42. Opitz JM, Zanni G, Reynolds JF Jr, Gilbert-Barness E. Defects of blastogenesis. Am J Med Genet. (2002) 115(4):269–86. doi: 10.1002/ajmg.10983
43. Bosi G, Garani G, Scorrano M, Calzolari E, Party IW. Temporal variability in birth prevalence of congenital heart defects as recorded by a general birth defects registry. J Pediatr. (2003) 142(6):690–8. doi: 10.1067/mpd.2003.243
Keywords: congenital heart defects, noncardiac anomalies, Chinese children, retrospective analyses, phenotype
Citation: Huang X, Gao Y, Chen W, Sheng W and Huang G (2023) Noncardiac anomalies in children with congenital heart disease. Front. Cardiovasc. Med. 10:1293210. doi: 10.3389/fcvm.2023.1293210
Received: 12 September 2023; Accepted: 27 October 2023;
Published: 20 November 2023.
Edited by:
Liqun Sun, University of Toronto, CanadaReviewed by:
Mingfu Wu, University of Houston, United StatesZhang Cheng, Chongqing Medical University, China
Kui Hu, Guizhou Provincial People’s Hospital, China
© 2023 Huang, Gao, Chen, Sheng and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weicheng Chen d2VpY2hlbmcuY2hlcm5AZ21haWwuY29t Wei Sheng c2hlbmdfd2VpQGZ1ZGFuLmVkdS5jbg== Guoying Huang Z3lodWFuZ0BzaG11LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
 Xianghui Huang
Xianghui Huang Yuan Gao
Yuan Gao Weicheng Chen
Weicheng Chen Wei Sheng1,3,4*
Wei Sheng1,3,4* Guoying Huang
Guoying Huang