
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 21 September 2022
Sec. Atherosclerosis and Vascular Medicine
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.943229
Background: We have recently developed the Coronary Artery Tree description and Lesion EvaluaTion (CatLet©) angiographic scoring system, which is capable of accounting for the variability in coronary anatomy, and risk-stratifying patients with coronary artery disease. This study aimed to clarify whether the CatLet score had a predictive value for long-term prognosis in patients with acute myocardial infarction (AMI) presenting > 12 h after symptom onset.
Materials and methods: The CatLet score was calculated for 1,018 consecutively enrolled AMI patients, who were divided into 3 groups according to the CatLet score tertiles. The primary endpoint was major adverse cardiac events (MACEs), defined as a composite of myocardial infarction, cardiac death, and ischemia-driven revascularization; secondary endpoints were all-cause death, cardiac death, myocardial infarction, and ischemia-driven revascularization.
Results: The CatLet score was capable of predicting long-term prognosis at a median 4.9-year follow-up alone or after adjustment for risk factors. Multivariable-adjusted hazard ratios (95% CI)/unit higher score were 1.06 (1.05–1.08) for MACEs, 1.05 (1.03–1.07) for all-cause death, 1.06 (1.04–1.09) for cardiac death, 1.06 (1.04–1.08) for myocardial infarction, and 1.06 (1.04–1.08) for revascularization. The univariate model showed good calibration (χ2 = 8.25, P = 0.4091) and good discrimination (area under ROC curve = 0.7086) for MACEs.
Conclusion: The CatLet score is an independent predictor of long-term clinical outcomes of patients with AMI presenting > 12 h after symptom onset (http://www.chictr.org.cn; Registry Number: ChiCTR2000033730).
A lesion that causes coronary artery flow limitation has been considered as an important prognostic factor (1, 2). The Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX) score, an anatomic coronary scoring system, has been developed to grade the severity and complexity of coronary artery disease (CAD) (3). However, the SYNTAX score, solely based on the dichotomized left or right coronary dominance, has failed to adequately describe the variability of coronary anatomy (4, 5). Although the SYNTAX score has been widely used in risk stratification and selection of revascularization strategies, there are studies questioning its predictive value in CAD patients (6–9). We have recently developed a novel Coronary Artery Tree description and Lesion EvaluaTion (CatLet©) angiographic scoring system, which can be utilized to account for the variability in coronary anatomy, and to risk-stratify patients with CAD (10, 11).
Our prior study showed that the CatLet score better predicted the long-term prognosis among patients who survived AMI presenting at ≤ 12 h and received primary PCI than the SYNTAX score, with a satisfactory inter- or intra-observer reproducibility (11–13). The current study aimed to validate that the CatLet score remained a useful tool for outcome prediction in patients with AMI presenting > 12 h after symptom onset.
Patients with AMI presenting > 12 h after symptom onset were consecutively enrolled in this study between January 2012 and September 2015. Exclusion criteria included: (a) poor image quality; (b) coronary artery embolism; (c) abnormal coronary anatomy; (d) normal CAG results; and (e) lost to follow-up.
We have described the CatLet score in detail elsewhere (10–12). In short, it is a new scoring system that attempts to adequately consider coronary variability and risk-stratify patients with coronary artery disease. In the CatLet score, both the left anterior descending artery (LAD) and diagonals (Dx) were classified into three types, and the right coronary artery (RCA) was classified into six types. As a result, a total of 54 (3*3*6) types of coronary circulation pattern were generated. Weighting factors were assigned to each coronary segment according to its subtended myocardial territory. Lesions with diameter stenosis ≥ 50% in vessels ≥ 1.5 mm were scored. For lesions with 50–99% diameter stenosis, we defined the coefficient as 2.0; for lesions with total occlusion, the coefficient was defined as 5.0. Non-occlusive lesions were scored straightforward; in patients whose infarct-related artery is completely occluded, wiring or use of a small balloon is helpful in revealing the downstream lesion anatomy (14); and persistently poor blood flow that failed to allow adequate visualization of the lesion was scored as a total occlusive one. The total score is the sum of individual lesion scores. The CatLet score calculator is available at www.catletscore.com.
Phone interviews were conducted for all living patients or their immediate relatives with specific questions about major adverse cardiac events (MACEs). All patients were interviewed until the date of the MACEs or the end of this study (September 2019), whichever came first. Medical records, discharge summaries, and angiographic data were systematically reviewed for a patient with an adverse event. Death information was obtained from household registration management systems, hospitals, or the next of kin.
The primary endpoint was MACEs at a median of 4.9 years, which was defined as a composite of myocardial infarction, cardiac death, and ischemia-driven repeat revascularization. Secondary endpoints were myocardial infarction, all-cause death, cardiac death, and ischemia-driven repeat revascularization. All-cause death was defined as death from any cause. Deaths were considered cardiac unless a non-cardiac cause could be identified (15). AMI was defined according to the third universal definition of myocardial infarction (16). Ischemia-driven repeat revascularization was defined as revascularization due to clinical ischemic symptoms with a diameter stenosis ≥ 50% or ≥ 70% even in the absence of ischemic symptoms. Clinical factors were defined according to our previous study (17).
Continuous variables were expressed as median (inter-quartile range, IQR). Categorical variables were expressed as frequencies (percentages). Testing for trends in event rates across the tertiles was completed with the STATA procedures opartchi. Missing values were filled in using the multiple imputation methods. The Kaplan–Meier method was employed to generate event-free survival curves, and survival between groups was compared using the trend test. A Cox regression survival analysis was performed to identify the independent predictors of clinical outcomes. ROC curves and calibration plots were used to evaluate the performance of the models. Sensitivity analysis was performed by excluding patients, 1 at a time, with missing values of left ventricular ejection fraction, serum creatinine, and serum albumin. The interaction between the CatLet score on a continuous scale and other risk factors was examined by the z test (18). All analyses were performed using Stata version 15.1. All p-values and confidence intervals were two-sided.
A total of 1,212 patients were consecutively enrolled for potential analysis. From the original data set, 1 was excluded for poor images, 5 for coronary embolism, 7 for abnormal coronary anatomy, 140 for normal CAG results, and 41 for loss to follow-up. As a result, all 1,018 patients were finally included in the current study.
The CatLet score ranged from 2 to 47.5, with a median of 14 (interquartile range, IQR, 10–21). Patients were divided into three groups according to the CatLet tertiles (CatLet_low ≤ 12, CatLet_mid 13–18, and CatLet_top ≥ 19). Clinical data and angiographic characteristics are shown in Table 1 and in online Supplementary Table 1.
Figure 1 illustrates that risk stratification was overall balanced between the CatLet score tertiles. The CatLet score predicted clinical outcomes significantly on a continuous or categorical scale as shown in Table 2. After adjustment for age, serum creatinine, LVEF, the CatLet score remains an independent predictor of long-term clinical outcomes. Multivariable-adjusted hazard ratios (95% CI)/unit higher score were 1.06 (1.05–1.08) for MACEs, 1.05 (1.03–1.07) for all-cause death, 1.06 (1.04–1.09) for cardiac death, 1.06 (1.04–1.08) for myocardial infarction, and 1.06 (1.04–1.08) for revascularization. See details in online Supplementary Table 2.
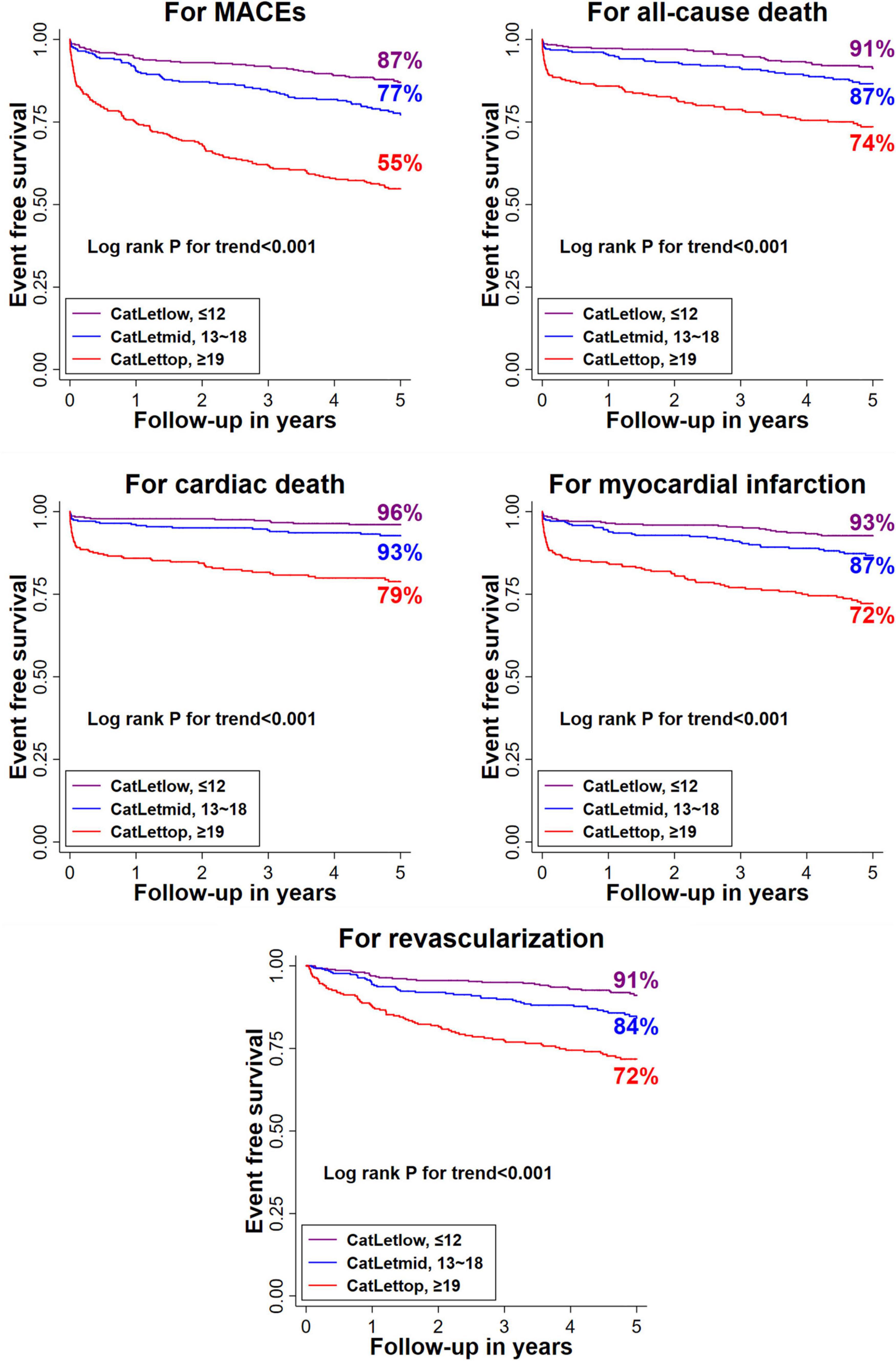
Figure 1. Kaplan–Meier curves for clinical outcomes at 5 years according to the CatLet score tertiles. MACE, major adverse cardiac events.
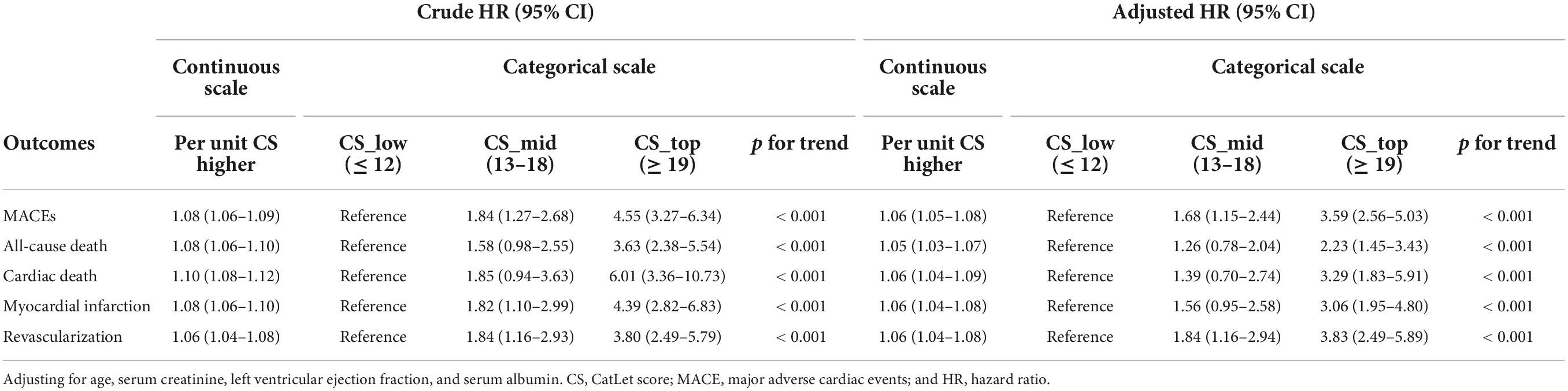
Table 2. Univariable or multivariable-adjusted HR (95% CI) for higher CatLet score with respect to clinical outcomes on a categorical or continuous scale.
The CatLet score alone performed well in discrimination with respect to clinical outcomes as shown in Figure 2. Areas under the receiver operating characteristic (ROC) curve ranged between 0.6421 and 0.728.
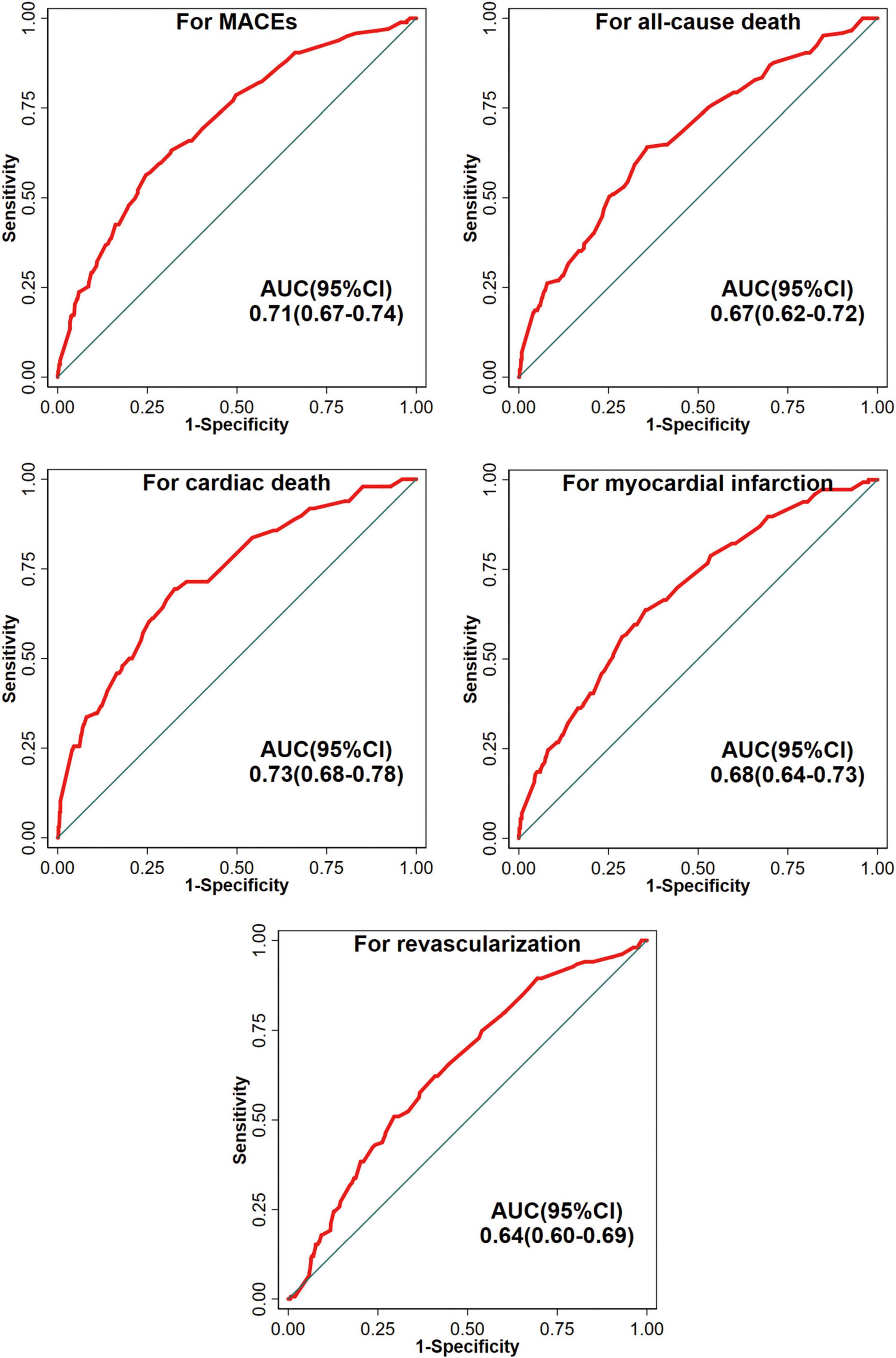
Figure 2. The ROC curves of univariate models for clinical outcomes. MACE, major adverse cardiac events; AUC, Receiver Operating Characteristic (ROC) curve; and CI, confidence interval.
In terms of calibration, the model with the CatLet score was robust as shown in Figure 3.
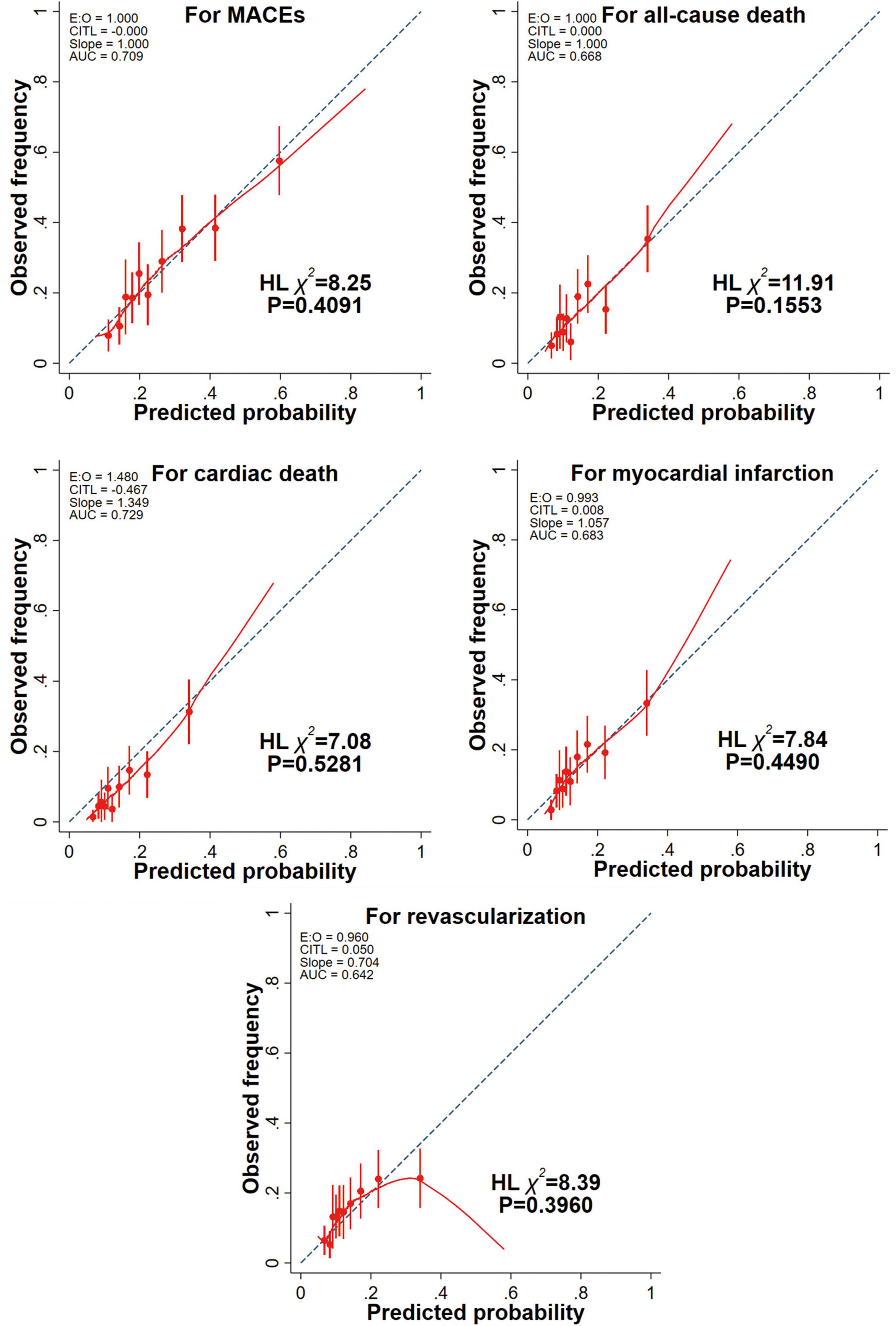
Figure 3. Calibration plots of univariate models for clinical outcomes. A red lowess smoothing curve was added to each calibration plot. Intercept of 0 and slope of 1 indicate perfect prediction. Negative and positive intercepts indicate overestimation and underestimation, respectively. MACE, major adverse cardiac events; HL, Hosmer-Lemeshow test.
Subgroup/sensitivity analysis revealed the consistent associations of the CatLet score with the clinical outcomes, without significant interactions across subgroups as shown in Figure 4 and in online Supplementary Table 2.
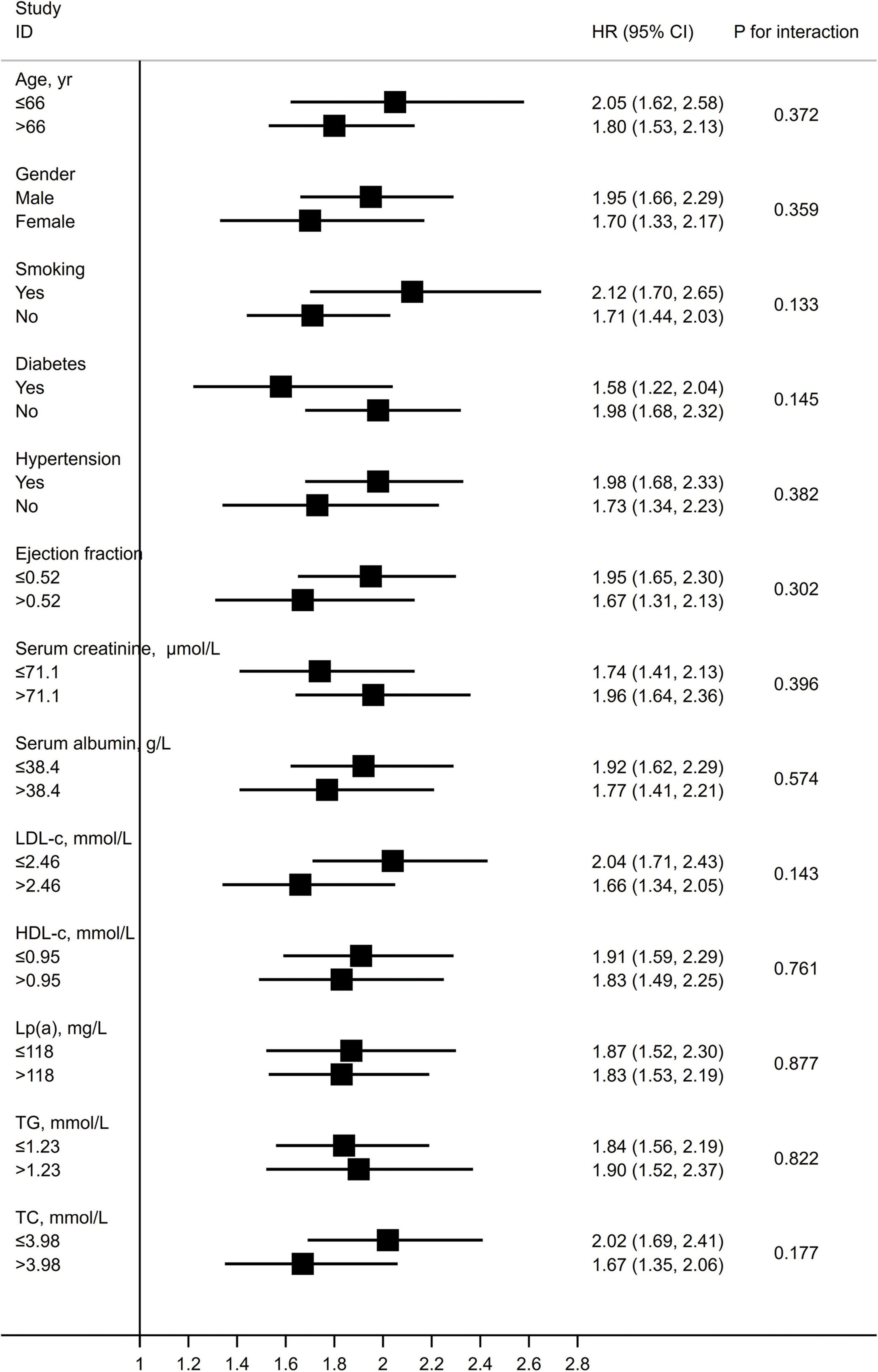
Figure 4. Hazard ratios for MACEs per 10 units higher CatLet score stratified by risk factors, categorically or medially. LDL-c, low density lipoprotein cholesterol; HDL-c, high density lipoprotein cholesterol; Lp(a), lipoprotein(a); TG, triglycerides; and TC, total cholesterol.
The main findings in the current study are as follows: in patients with AMI presenting > 12 h after symptom onset, (a) the CatLet score in isolation independently predicted the 5-year clinical outcomes; (b) the CatLet score remained significantly predictive of 5-year clinical outcomes even after adjustment for important clinical explaining variables, and (c) models with the CatLet score had a robust calibration with respect to clinical outcomes in patients with AMI.
Expectedly, patients with higher CatLet score tertiles were older, had higher rates of diabetes, and had lower serum albumin levels and LVEF, which was consistent with our previous studies (11, 12). Interestingly, in the current study, current smokers had lower CatLet scores, namely “smoker’s paradox.” A similar phenomenon also appeared in our previous studies and some studies of the SYNTAX score (11, 12, 14, 19). Possible explanations include the younger age and fewer cardiovascular risk factors in smokers compared with non-smokers (20). In the current study, patients in the higher CatLet tertiles are younger than those in the lower ones, and age is the strongest predictor of clinical outcomes. Thus, the “smoker’s paradox” appearing in this study can be explained. This association of smoking with clinical outcomes also disappeared after adjusting for covariates (Supplementary Table 2).
In the current study, the AUCs for the CatLet score alone were 0.7289 and 0.6677 for cardiac death and all-cause death, respectively. For the SYNTAX score, another anatomic scoring tool, a meta-analysis including 26 studies indicated that the pooled C-statistics for 1- and 5-year all-cause deaths were 0.65 and 0.62, respectively (21). The performance of the CatLet score is overall better than the SYNTAX score with respect to mortality prediction. These results are wholly anticipated considering that (a) the CatLet score has adequately accounted for the coronary artery trees in its diversity while the SYNTAX score, solely based on the dichotomized right or left coronary dominance, and (b) the CatLet score has simultaneously reflected two aspects of a lesion: the stenosis degree and the myocardial territory (weighting) subtended by the stenotic coronary artery. Our head-to-head comparative study has also shown that the CatLet score had better discrimination and calibration than the SYNTAX score in terms of 4.3-year mortality prediction [C-index, 0.73 (95% CI, 0.66–0.79) vs. 0.69 (0.61–0.77)] (11).
The good discriminatory capacity of the CatLet score between the lower two tertiles as demonstrated in our previous study has been reproduced in the current study (11). By contrast, the SYNTAX score was poor in discriminating between the lower two tertiles (11, 22). Furthermore, large-scale studies on the SYNTAX score did not eliminate this phenomenon (23). We think that it is related to the inherent fallacies of the SYNTAX score with its failure to account for the variable coronary anatomy (11).
Multivariate analyses have been suspected of producing problematic results if fewer outcome events are available relative to the number of independent variables analyzed in the model (24). Therefore, backward stepwise cox regression has been applied to select variables in the current study. Age, serum creatinine, LVEF, and serum albumin were previously reported to be strong predictors of prognosis, and were all finally retained in the multivariate model as well as the CatLet score (Supplementary Table 3) (25–28). Subgroup/sensitivity analysis also did not alter the status of the CatLet score as an independent predictor of clinical outcomes.
There are several limitations to the current study. First, the current study is an observational one in design. Therefore, the findings revealed in this study should be considered as hypothesis-generating. Second, this is a single-centered study enrolling only AMI patients presenting > 12 h after symptom onset. Therefore, our findings warrant further confirmation from different centers and in different CAD populations. Third, like the SYNTAX score, lesions with diameter stenosis ≥ 50% were scored in the CatLet score. However, only 35% of the intermediate (50–70%) angiographic stenosis was hemodynamically relevant as defined by fractional flow reserve (FFR) ≤ 0.80 (29). Further studies are needed to clarify whether the FFR-guided CatLet score is a better predictor of prognosis than the one just based on the visual assessment. Finally, our previous study has shown that the clinically adjusted CatLet score model has a better prognostic value in AMI patients receiving primary PCI (12). In the current study, we also found that clinical variables can in part explain clinical outcomes. Therefore, the effects of clinical variables on the prognostic value of the CatLet score remain to be clarified in AMI patients presenting > 12 h after symptom onset.
The CatLet score is an independent predictor of long-term prognosis in patients with AMI presenting > 12 h after symptom onset. Our study has extended the application value of the CatLet angiographic scoring system to different AMI populations.
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
This study was reviewed and approved by the Institute Review Board of Soochow University.
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
This work was supported by Sci-Tech Supporting Program of Jiangsu Commission of Health (M2021019) and Medical Sci-Tech Innovation Program for Medical Care of Suzhou City (SKY2021005).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.943229/full#supplementary-material
1. van Nunen LX, Zimmermann FM, Tonino PA, Barbato E, Baumbach A, Engstrøm T, et al. Fractional flow reserve versus angiography for guidance of PCI in patients with multivessel coronary artery disease (FAME): 5-year follow-up of a randomised controlled trial. Lancet. (2015) 386:1853–60.
2. De Bruyne B, Pijls NH, Kalesan B, Barbato E, Tonino PA, Piroth Z, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. (2012) 367:991–1001.
3. Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K, et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. (2005) 1:219–27.
4. He YM, Shen L, Ge JB. Fallacies and possible remedies of the SYNTAX score. J Intervent Cardiol. (2020) 2020:8822308. doi: 10.1155/2020/8822308
5. Leaman DM, Brower RW, Meester GT, Serruys P, van den Brand M. Coronary artery atherosclerosis: severity of the disease, severity of angina pectoris and compromised left ventricular function. Circulation. (1981) 63:285–99.
6. Gerber RT, Ielasi A, Al-Lamee R, Latib A, Airoldi F, Ferraro M, et al. Long-term follow-up of multivessel percutaneous coronary intervention with drug-eluting stents for de novo lesions with correlation to the SYNTAX score. Cardiovasc Revasc Med. (2011) 12:220–7. doi: 10.1016/j.carrev.2010.10.002
7. Gannot S, Fefer P, Kopel E, Kochkina K, Beigel R, Raanani E, et al. Higher Syntax score is not predictive of late mortality in “real-world” patients with multivessel coronary artery disease undergoing coronary artery bypass grafting. Israel Med Assoc J. (2014) 16:764–7.
8. Chakravarty T, Buch MH, Naik H, White AJ, Doctor N, Schapira J, et al. Predictive accuracy of SYNTAX score for predicting long-term outcomes of unprotected left main coronary artery revascularization. Am J Cardiol. (2011) 107:360–6.
9. Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization.. Europ Heart J. (2019) 40:87–165.
10. Xu MX, Teng RL, Ruddy TD, Schoenhagen P, Bartel T, Di Bartolomeo R, et al. The CatLet score: a new coronary angiographic scoring tool accommodating the variable coronary anatomy for the first time. J Thoracic Dis. (2019) 11:5199–209. doi: 10.21037/jtd.2019.12.18
11. Xu MX, Ruddy TD, Schoenhagen P, Bartel T, Di Bartolomeo R, von Kodolitsch Y, et al. The CatLet score and outcome prediction in acute myocardial infarction for patients undergoing primary percutaneous intervention: a proof-of-concept study. Catheter Cardiovasc Interv. (2020) 96:E220–9. doi: 10.1002/ccd.28724
12. Teng RL, Liu M, Sun BC, Xu JP, He Y, He YM. Age, serum creatinine, and left ventricular ejection fraction improved the performance of the catlet angiographic scoring system in terms of outcome predictions for patients with acute myocardial infarction: a median 4.3-year follow-up study. Cardiology. (2021) 146:690–7. doi: 10.1159/000515759
13. Liu JM, He Y, Teng RL, Qian XD, Dai YL, Xu JP, et al. Inter- and intra-observer variability for the assessment of coronary artery tree description and lesion EvaluaTion (CatLet©) angiographic scoring system in patients with acute myocardial infarction. Chin Med J. (2020) 134:425–30. doi: 10.1097/CM9.0000000000001208
14. Magro M, Nauta S, Simsek C, Onuma Y, Garg S, van der Heide E, et al. Value of the SYNTAX score in patients treated by primary percutaneous coronary intervention for acute ST-elevation myocardial infarction: the MI SYNTAXscore study. Am Heart J. (2011) 161:771–81. doi: 10.1016/j.ahj.2011.01.004
15. Hicks KA, Mahaffey KW, Mehran R, Nissen SE, Wiviott SD, Dunn B, et al. 2017 cardiovascular and stroke endpoint definitions for clinical trials. J Am Coll Cardiol. (2018) 71:1021–34.
16. Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. Circulation. (2012) 126:2020–35.
17. Cai DP, He YM, Yang XJ, Zhao X, Xu HF. Lipoprotein (a) is a risk factor for coronary artery disease in Chinese Han ethnic population modified by some traditional risk factors: a cross-sectional study of 3462 cases and 6125 controls. Clin Chim Acta. (2015) 451:278–86. doi: 10.1016/j.cca.2015.10.009
18. Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. (2003) 326:219.
19. Garg S, Sarno G, Garcia-Garcia HM, Girasis C, Wykrzykowska J, Dawkins KD, et al. A new tool for the risk stratification of patients with complex coronary artery disease: the Clinical SYNTAX Score. Circ Cardiovasc Interv. (2010) 3:317–26.
20. Redfors B, Furer A, Selker HP, Thiele H, Patel MR, Chen S, et al. Effect of smoking on outcomes of primary PCI in patients with STEMI. J Am Coll Cardiol. (2020) 75:1743–54.
21. Chen J, Tang B, Lin Y, Ru Y, Wu M, Wang X, et al. Validation of the ability of SYNTAX and clinical SYNTAX scores to predict adverse cardiovascular events after stent implantation: a systematic review and meta-analysis. Angiology. (2016) 67:820–8. doi: 10.1177/0003319715618803
22. Valgimigli M, Serruys PW, Tsuchida K, Vaina S, Morel MA, van den Brand MJ, et al. Cyphering the complexity of coronary artery disease using the syntax score to predict clinical outcome in patients with three-vessel lumen obstruction undergoing percutaneous coronary intervention. Am J Cardiol. (2007) 99:1072–81. doi: 10.1016/j.amjcard.2006.11.062
23. Garg S, Sarno G, Serruys PW, Rodriguez AE, Bolognese L, Anselmi M, et al. Prediction of 1-year clinical outcomes using the SYNTAX score in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: a substudy of the STRATEGY (single high-dose bolus tirofiban and sirolimus-eluting stent versus abciximab and bare-metal stent in acute myocardial infarction) and MULTISTRATEGY (multicenter evaluation of single high-dose bolus tirofiban versus abciximab with sirolimus-eluting stent or bare-metal stent in acute myocardial infarction study) trials. JACC Cardiovasc Interv. (2011) 4:66–75. doi: 10.1016/j.jcin.2010.09.017
24. Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. (1996) 49:1373–9.
25. Nguyen OK, Makam AN, Clark C, Zhang S, Das SR, Halm EA. Predicting 30-day hospital readmissions in acute myocardial infarction: the AMI “READMITS” (renal function, elevated brain natriuretic peptide, age, diabetes mellitus, nonmale sex, intervention with timely percutaneous coronary intervention, and low systolic blood pressure) Score. J Am Heart Assoc. (2018) 7:e008882. doi: 10.1161/JAHA.118.008882
26. Plakht Y, Gilutz H, Shiyovich A. Decreased admission serum albumin level is an independent predictor of long-term mortality in hospital survivors of acute myocardial infarction. Soroka Acute Myocardial Infarction II (SAMI-II) project. Int J Cardiol. (2016) 219:20–4. doi: 10.1016/j.ijcard.2016.05.067
27. Sutton NR, Li S, Thomas L, Wang TY, de Lemos JA, Enriquez JR, et al. The association of left ventricular ejection fraction with clinical outcomes after myocardial infarction: findings from the Acute Coronary Treatment and Intervention Outcomes Network (ACTION) Registry-Get With the Guidelines (GWTG) Medicare-linked database. Am Heart J. (2016) 178:65–73. doi: 10.1016/j.ahj.2016.05.003
28. Yamaguchi J, Kasanuki H, Ishii Y, Yagi M, Ogawa H, Fujii SY, et al. Prognostic significance of serum creatinine concentration for in-hospital mortality in patients with acute myocardial infarction who underwent successful primary percutaneous coronary intervention (from the Heart Institute of Japan Acute Myocardial Infarction [HIJAMI] Registry). Am J Cardiol. (2004) 93:1526–8. doi: 10.1016/j.amjcard.2004.02.065
29. Van Belle E, Rioufol G, Pouillot C, Cuisset T, Bougrini K, Teiger E, et al. Outcome impact of coronary revascularization strategy reclassification with fractional flow reserve at time of diagnostic angiography: insights from a large French multicenter fractional flow reserve registry. Circulation. (2014) 129:173–85. doi: 10.1161/CIRCULATIONAHA.113.006646
Keywords: angiographic score, acute myocardial infarction, Percutaneous Coronary Intervention, major adverse cardiac events, prognosis
Citation: Wang H, He Y, Fan J-L, Li X, Zhou B-Y, Jiang T-B and He Y-M (2022) The predictive value of CatLet© angiographic scoring system for long-term prognosis in patients with acute myocardial infarction presenting > 12 h after symptom onset. Front. Cardiovasc. Med. 9:943229. doi: 10.3389/fcvm.2022.943229
Received: 13 May 2022; Accepted: 29 August 2022;
Published: 21 September 2022.
Edited by:
Turgay Celik, VM Medical Park Ankara (Keçiören), TurkeyReviewed by:
Mehmet Tolga Dogru, Kırıkkale University, TurkeyCopyright © 2022 Wang, He, Fan, Li, Zhou, Jiang and He. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yong-Ming He, aGV5b25nbWluZ0BzdWRhLmVkdS5jbg==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.