- 1School of Nursing, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia
- 2School of Nursing, Institute of Health Sciences, Jimma University, Jimma, Ethiopia
Introduction: Asthma, a global chronic respiratory condition, varies in patient autonomy due to limited resources, health literacy, and cultural beliefs, emphasizing the importance of understanding this autonomy for improved asthma management.
Methods: A cross-sectional study was conducted at Jimma University Comprehensive Specialized Hospital, involving face-to-face interviews with 175 patients. Data was collected on sociodemographic characteristics, clinical factors, and autonomy levels using a validated Patient Autonomy Preference Index. Descriptive statistics and binary logistic regression analysis were used.
Results: A total of 175 participants were recruited, out of them 41.7% (95% CI: 31.19, 40.41)) of participants were autonomous in managing their asthma exacerbation. 127 (72.6%) of study participants were female, with a mean age of 47.51 (SD ± 13.96), 101(57.7%) were live in urban areas, 54 (30.9%) had no formal education, 140 (80%) were married, 112 (64%) had health insurance, and 102(83.3%) obtained health information about their condition from healthcare workers. Reside in an urban area (AOR = 3.24; 95% CI: 1.40–7.49, p < 0.006), have health insurance (AOR = 4.30; 95% CI: 1.76–10.51, p < 0.001), those doing regular exercise (AOR = 4.79; 95% CI: 1.69–13.64, p < 0.003), have family history (AOR = 7.47; 95% CI: 1.61–34.60, p < 0.01), have a duration above five years since diagnosis (AOR = 0.44; 95% CI: 1.04–1.26, p < 0.003), and participants with a high level of health literacy (AOR = 1.10; 95% CI: 1.00–1.20, p < 0.042) become associated with being autonomous in managing asthma exacerbation.
Conclusion and recommendation: Only around forty-two percent of study participants were autonomous in managing their asthma exacerbation. Thus healthcare providers should give due attention to those who reside in rural areas, are not insured, recently diagnosed with asthma, and with low health literacy to enhance patient autonomy and self-management practices, ultimately improving health outcomes for individuals with asthma.
Highlights
• This study reveals that urban patients have significantly better autonomy in managing bronchial asthma compared to their rural counterparts. This finding emphasizes the impact of geographical location on health management practices, which has not been extensively highlighted in previous research.
• The research underscores the role of access to healthcare facilities and educational resources in enhancing patient autonomy.
• This study contributes valuable new insights into the dynamics of patient autonomy in asthma management while reinforcing established knowledge in the field
Introduction
Asthma is a chronic respiratory condition causing shortness of breath and chest tightness. Environmental factors can worsen symptoms, necessitating prompt intervention (1). Autonomy in healthcare decision-making is crucial for patient-centered care and empowering patients to manage their condition independently (2).
Asthma remains a significant global health burden, affecting over 262 million people and causing nearly 455,000 deaths annually (3, 4). The management of asthma requires both clinical interventions and patient-centered approaches, emphasizing the importance of patient autonomy in managing chronic conditions like asthma which requires timely decision-making is crucial to prevent exacerbations and reduce mortality (1).
Patient autonomy in asthma management varies across healthcare settings, with high-income countries emphasizing it as a core component of chronic disease management, encouraging decision-making and independent treatment (5). In low and middle income countries, asthma management autonomy is often hindered by limited healthcare resources, low health literacy, and patient empowerment (6).
Ethiopia's asthma prevalence is between 4.6% and 9.1%, influenced by healthcare system challenges such as limited access to medications, infrastructure, and patient education, and cultural factors causing delayed interventions (7, 8). Asthma patients are at risk of severe acute attacks due to rapid air changes, necessitating prompt intervention and medication administration, and promoting patient autonomy in treatment (2, 9).
Ethiopia's healthcare system faces challenges in asthma management due to limited access to essential medications, supply chain issues, and cost (10), underdeveloped infrastructure, especially in rural areas (11), lack of patient education on asthma management can lead to delayed diagnosis and treatment and affects the level of decision-making by themselves (12).
Cultural beliefs and practices in Ethiopia may contribute to a paternalistic approach to healthcare, where patients defer to healthcare providers rather than actively participate in their care (7). In Ethiopia, there is a lack of resources for self-management of asthma, particularly during exacerbations, as many patients lack the necessary training to monitor symptoms, use inhalers correctly, and recognize medical help (13).
Misconceptions among Ethiopian asthma patients include the belief that immediate intervention is necessary for exacerbations, underestimating daily asthma management, and lacking understanding about inhalers, and cultural beliefs and stigma can further misunderstanding asthma as a transient or non-serious condition (12–14).
Poor asthma patients’ decision-making autonomy leads to exacerbations, higher healthcare utilization, reduced quality of life, poor treatment adherence, and increased healthcare costs (13, 15, 16).
National health policies may not fully emphasize patient autonomy in chronic disease management, leading to a lack of systematic efforts to promote autonomy among patients. Understanding how patients perceive their role in managing their condition and the barriers they face can inform strategies to enhance patient autonomy, ultimately leading to better asthma outcomes reduced healthcare costs, and ultimately enhancing patient outcomes and quality of life. Therefore, this study aims to assess the autonomy preferences of asthma patients and its associated factors in a tertiary hospital setting at Jimma University compressive specialized hospital in managing their condition.
Methods and materials
Study area and period
This research was carried out in a tertiary Hospital at Jimma University Comprehensive Specialized Hospital, Oromia, Ethiopia. Jimma city is the capital of the Jimma zone found at 356 Km from Addis Ababa, the capital city of Ethiopia, in the Southwestern part of the country. Jimma University Comprehensive Specialized Hospital is one of the oldest public hospitals in the country and it is the only teaching and referral hospital in the south-western part of the country. It provides services for approximately 19,000 inpatients, 160,000 outpatient attendances, 5,000 delivery, and 11,000 emergency cases annually. It has a bed capacity of 800 and an estimated total number of 14,000 adult patients admitted annually. The hospital has 1,600 staff members, 23 service delivery units, 698 Staff nurses, 125 pharmacy staff and different working units like medical, surgical, maternity, Gynecology, oncology, ophthalmology, psychiatry, and the like. Approximately, 19,000 patients attend the follow-up clinic for NCDs, in a year (82).
The study was conducted from May 1 to June 1 2023.
Study design
A cross-sectional institutional research approach was employed.
Source population
All adult patients with chronic asthma diseases at Jimma University Comprehensive Specialized Hospital.
Study population
All selected adult patients with chronic asthma diseases were regularly followed up at Jimma University Comprehensive Specialized Hospital during the data collection period.
Inclusion criteria
All adult patients aged ≥18 years who were regularly followed up for at least six months with chronic asthma diseases were able to respond.
Exclusion criteria
Patients who were critically ill.
Sample size determination
The research used a single-population proportion formula to determine the appropriate sample size, considering the level of perceived autonomy in chronic disease in Ethiopia at Mettu was 60.5% (17), with a 95% confidence interval, and a 5% margin of error. The sample size for primary potential predictors was also calculated using Epi Info Version 7.2.0.1. Subsequently, the largest sample size was selected from both methods. Later on 5% nonresponse rate was added, and the ultimate sample size was 349. Participants were recruited over two months until the allotted number was reached.
Sampling procedure
All adult patients aged ≥18 years with chronic asthma diseases on regular follow-ups at Jimma University Comprehensive Specialized Hospital were selected during the data collection period. The study participants were consecutively recruited from April 1 to July 1, 2023.
Dependent Variable
Perceived level of autonomy in decision-making.
Independent variables
Sociodemographic Variables (age, sex, monthly family income, area where they live, educational level, marital status, occupation, and source of information), clinically related variables (type and stage of the disease, family history, informal caregiver, duration of disease, type of treatment, and presence of comorbidity), health-related factors (smoking cigarettes, alcohol users, physical inactivity), patient health literacy, healthcare provider-related factors (healthcare professional role and types of healthcare profession and their role), and health information and communication (language barriers, jargon medical words, and decisional aid materials).
Operational definitions and definitions of the terms
Autonomy in the decision-making process refers to a patient's ability and right to make informed, independent choices regarding their healthcare without undue influence or coercion from healthcare providers (18).
Autonomous: If the patients with scores above the median of the autonomy index (17).
Not Autonomous: If the patients with scores at or below the median (17).
Data collection tools
The study used a Patient Autonomy Preference Index questionnaire, which has been proven to be effective in determining the level of patient autonomy in self-management. The questionnaire consists of four sections and 59 items, including socio-demographic, illness-related, health literacy, and Patient Autonomy Preference Index questionnaires (19). The Patient Autonomy Preference Index questionnaires were rated on a five-point Likert scale, with participants rating their agreement with each statement. The results were then categorized as high or low based on the mean score of each question. The instrument has improved in validity and reliability over time, making it the most effective tool for gauging patient participation in healthcare decision-making.
Data collection techniques
Patients with brachial asthma who had been monitored for at least six months following their service completion during the data collection period were interviewed face-to-face. Two BSc nurses from Shenan Gibe Hospital were chosen based on their prior expertise in gathering data. Patient cards were used to collect clinical factor data on the patients.
Data quality management
The questionnaires were translated into Afaan Oromo and Amharic, and then back into English to ensure reliability. A pre-test was conducted on 10% of the sample (α = 0.87), including 33 participants, at Agaro General Hospital to assess data clarity, feasibility, applicability, understandability, reliability, and coherence. Data collectors received two days of training to ensure common understanding and follow the same interview procedures. The principal investigator conducted continuous follow-ups, daily reviews, and questionnaire checks to ensure accuracy and consistency throughout the data-gathering process.
Data processing and analyses
Before being imported into Epi Data version 4.6 and exported to SPSS version 26, the data was cleaned, verified, and coded. Descriptive and inferential statistics were used to find a linear correlation between independent variables. To test for multicollinearity, tolerance, and variance inflation factors were used. None of the variables produced a variance inflation factor >10 and tolerance <0.1 (variance inflation factor ≤2.91, and tolerance ≥0.343) were excluded. The study used binary logistic regression to determine the relationship between dependent and independent variables, and multivariable logistic regression analysis to identify factors related to patients’ autonomy in managing asthma exacerbation. The model was fit when the omnibus test was significant (p = 0.00), and the Hosmer-Lemeshow test was negligible (p = 0.406). 95% confidence intervals and odds ratios were calculated to gauge the strength of the correlation. The statistical significance threshold was established at a p-value less than 0.05. The findings were presented using the proper tables, charts, figures, graphs, and narrative prose.
Ethical consideration
This study received ethical approval from the Jimma University Research and Ethics Review Board (reference number JUIH/IRB/371/23), which also accepted the research protocol's ethics. A formal letter of collaboration was also provided, and the study was submitted to the chronic follow-up unit. Participants signed an informed consent form after being made aware of the purpose of the study. They were also told that their participation would be unaffected by their departure and that confidentiality and privacy would be upheld.
Result
Sociodemographic characteristics of the respondents
A total of 175 participants were recruited. Among them, 127 (72.6%) were female, the mean age was 47.51 with a standard deviation of 13.96, 92(52.6%) were Muslim followers, 101(57.7%) lived in urban areas, 54 (30.9%) had no formal education, 56(32%) of their occupation was housewife, 140 (80%) were married, 100(57.1%) had monthly income <2,500 Ethiopian Birr, 112 (64%) had health insurance, 102(83.3%) obtained health information about their condition from healthcare workers, 134(76.6%) got information from Doctors and nurses, and around 12(6.9%) not differentiate types of health care provided they receive the care and information (Table 1).
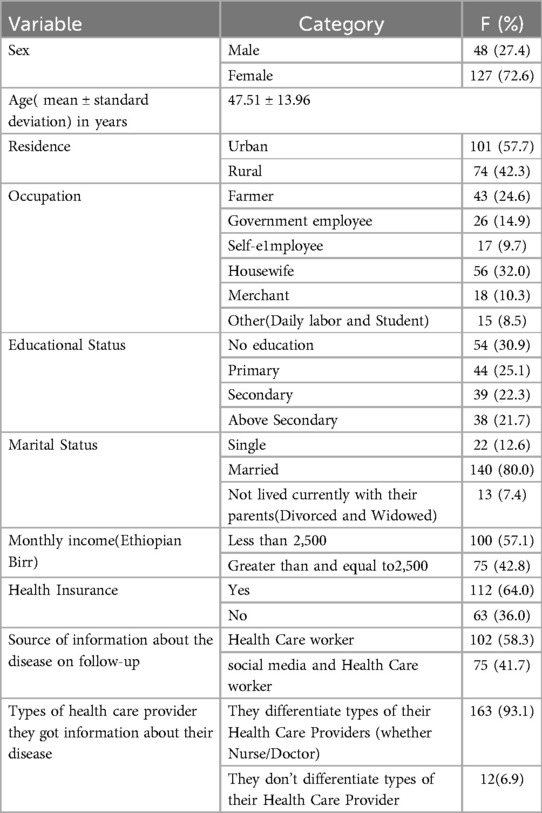
Table 1. Socio-demographic characteristics of adult bronchial asthma patients at the tertiary hospital of Jimma University, Ethiopia, 2023.
Risk health behavior of the adult with bronchial asthma
Regarding risky health behavior, 172(98.3%) were non-cigarette smokers, 18(10.3%) were non-alcohol users, from those who used alcohol 23 (8.6%) drank alcohol for more than five years, 39(22.3%) engaged in regular physical exercise and from those 37(21.1%) was doing physical exercise less than 30 min, and 99(56.6%) not done regular exercise due to not have interest with doing exercise (Table 2).
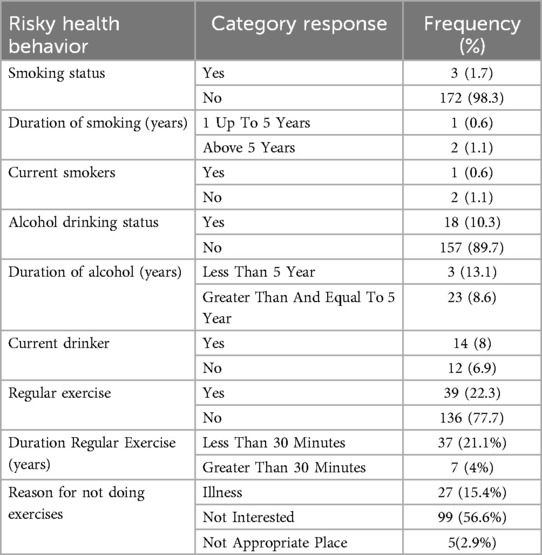
Table 2. Risk health behavior of adult bronchial asthma at the tertiary hospital of Jimma University, Ethiopia, 2023.
Clinical related factors of the participant of adult with bronchial asthma
From the total recruited participants 72(41.1%) had comorbid disease with asthma, 80(45.7%) had health information material for decision for disease on follow-up and 20(11.4%) for comorbid disease with asthma, 17(9.7%) had family history of the same illness, 43(24.6%) of their caregiver was family, 41(23.4%) has peer network with the same disease on follow-up, 108 (61.7%) diagnosed below five years after diagnosis, and 146 (83.4%) had a history of hospitalization for the disease on follow-up (Table 3).
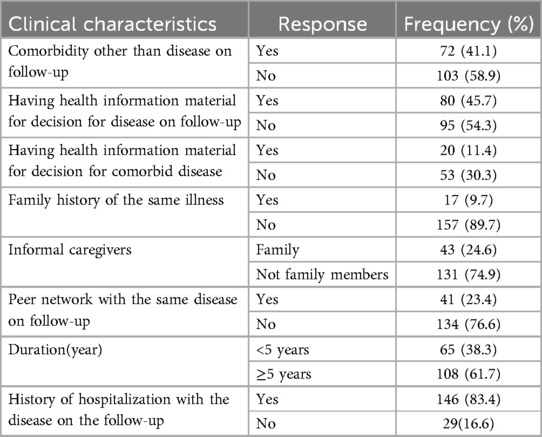
Table 3. Clinical features of participants with bronchial asthma disease at the tertiary hospital of Jimma University, Ethiopia, 2023.
Level of patient health literacy
Items related to health literacy, which were rated from one to five on a five-point Likert scale, were totaled and handled as continuous variables. The study participants’ health literacy mean and standard deviation was 20.923 (SD ± 5.31).
Patient preference for autonomy
The participants’ preference for autonomy in managing their asthma exacerbation was found to have a mean score and standard deviation of 43.87 (SD ± 10.49) with a range of 23–72. By dichotomizing based on their mean, 73(41.7%) [95% CI: 34.34, 49.09] Of study participants reported having autonomy in their self-management of asthma exacerbation.
Factors associated with patient autonomy in managing their asthma exacerbation
By adjusting for confounding factors, binary and multivariable logistic regression models were used to evaluate the relationship between independent variables and patient autonomy in self-management. Age, residence, educational status, marital status, occupation, health insurance, source of health information, types of health care provider in information sharing, alcohol, exercise, comorbidity, having decisional aid for disease on follow-up, Family history with the disease on follow up, peer network, duration since diagnosed, hospitalization, and patient health literacy were a candidate for multivariate logistic regression analysis. In the multivariate logistic regression analysis, only six variables (residence, health insurance, regular exercise, family history, duration of the disease since diagnosis, and patient health literacy became statistically significant (p < 0.05) (Table 4).

Table 4. Multivariable analysis of variables statistically significantly associated with asthma patient autonomy in their self-management at the tertiary hospital of Jimma University, Ethiopia, 2023.
Participants who live in the urban area has three times more likely autonomous in self-management of asthma exacerbation than those from rural areas (AOR = 3.24; 95% CI: 1.40–7.49), those participants had health insurance has four times more likely autonomous in self-management of asthma exacerbation than those has no health insurance (AOR = 4.30; 95% CI: 1.76–10.51), those doing regular physical exercise has around four point seven more likely autonomous in self-management of asthma exacerbation than those not doing regular physical exercise (AOR = 4.79; 95% CI: 1.69–13.64).
Participants those has family history of bronchial asthma seven ctimes more likely autonomous in self-management of asthma exacerbation than those has no family history of asthma (AOR = 7.47; 95% CI: 1.61–34.60), those participants diagnosed with bronchial asthma below five year duration was 56% less likely autonomous in self-management of asthma exacerbation than those five years and above since diagnosed with asthma (AOR = 0.44; 95% CI: 1.04–1.26).
This study also indicated, for every one-point increase in a participant's health literacy score, the Log odds that the participants will have autonomous in self-management of asthma exacerbation increases by 1.1(β = 0.093, AOR = 1.1, 95% CI: 1.00–1.20) on average (Table 4).
Discussion
This research was done at the Jimma Comprehensive Specialized Hospital in Jimma, Oromia, Ethiopia, to evaluate patient autonomy in self-management of asthma exacerbation and the related variables among patients with asthma. According to the study's results, 73 participants, or 41.7%, were autonomous in self-management of their disease. This finding is relatively similar to other studies conducted in Turkey reported that only 35.6% of asthma patients demonstrated autonomy in self-management decisions (20), in Malaysia found that 39.3% of asthma patients exhibited autonomy in managing their condition (21), and Mettu Karl Hospital in Ethiopia reported that only 29.5% of asthma patients were autonomous in self-management (17). This due to educational, cultural, socioeconomic, and healthcare system-related factors, limiting informed health decisions. So it needs to enhance asthma management knowledge, train healthcare providers, reduce socioeconomic barriers, provide affordable medications, strengthen primary healthcare, incorporate psychosocial support, and prioritize patient autonomy in chronic disease management.
The findings of this study showed that participants from urban areas were more likely to be reported as having autonomy in self-management of asthma exacerbation than those from rural areas, similar to findings in previous studies in Ethiopia (22), Nigeria (23), and Malawi (24). The study highlighted that urban patients had better access to healthcare facilities, educational resources, and information, which contributed to better self-management practices and decision-making autonomy. Thus healthcare providers should increase the availability and accessibility of healthcare services in rural areas by enhancing infrastructure, establishing more clinics, and providing mobile health units.
According to the study's findings, participants with health insurance were more likely to be autonomous in managing their asthma attacks than those without insurance. These findings are consistent with research done in Nigeria (25), the UK (26), and Chicago (27). The reasons were that insured patients often benefit from better access to medications, regular medical follow-ups, and health education programs, allowing more frequent interactions with healthcare providers, which enhances patient education and self-management skills. By expanding insurance coverage and improving access to essential healthcare resources, patient autonomy in asthma management can be significantly enhanced.
The study found a correlation between the status of regular exercise and patients’ autonomy in self-managing asthma, which is consistent with findings from studies conducted in the United States (28), Canada (29), and Finland (30). These studies indicated that regular exercise enhances patients’ confidence and ability to manage asthma independently due to improved lung function and physical fitness. Healthcare providers incorporate tailored exercise routines into asthma management plans. These programs should be designed to improve lung function and physical fitness, thereby boosting patients’ confidence and autonomy in managing their condition. Educating patients on safe and appropriate exercises, along with regular follow-ups, can further reinforce self-management skills.
The study's findings indicate that individuals with a family history of asthma exhibit greater autonomy in managing asthma attacks compared to those without such a history. This aligns with several studies that emphasize the role of family dynamics in asthma management as studies done in the UK (31), Ecuador (32), and Pakistan (33). These findings collectively underscore the importance of familial influence in asthma management, suggesting that family history may foster better self-management practices. This encourages healthcare providers to actively engage families in asthma education and management plans, especially for patients with a family history of the condition. Involving family members in care routines, decision-making, and educational sessions can enhance patient autonomy by fostering a supportive environment that reinforces effective self-management practices.
The results of this study demonstrated that individuals who were diagnosed with asthma more than five years ago are more autonomous in managing their asthma attacks than their counterparts, which is similar to the findings of studies conducted in Ecuador (32), Indonesia (34, 35), UK (36). This is due to individuals with a longer duration of asthma typically having more experience managing their condition, they develop and refine self-management skills, often learn to adapt their treatment plans based on their evolving needs and develop greater self-efficacy or confidence in their ability to manage their health. Offer continuous self-management training and education programs for patients at various stages of their asthma journey, empowering them with the necessary experience and confidence for autonomous disease management.
According to the study's findings, asthmatic patients become more autonomous in managing asthma attacks as their health literacy level rises. These results are consistent with those found in Australia (37), UK (38), Nepal (39), and Germany (40) highlighting that improved health literacy significantly influences decision-making in accessing emergency healthcare for asthma exacerbations, emphasizing the role of self-management strategies developed through past experiences and education. This collectively shows the importance of health literacy in empowering asthmatic patients to manage their condition effectively. Implement health literacy programs to educate patients on asthma management, treatment options, and emergency response strategies, empowering them to make informed decisions and manage asthma independently, tailored to different literacy levels.
Strengths and limitations of the study
The study used a cross-sectional institutional research design to examine patient autonomy in self-management, specifically in asthma patients. The research was conducted in a tertiary hospital, allowing for a diverse patient population. The Patient Autonomy Preference Index was used to understand decision-making and self-management preferences. The study included patients with at least six months of regular follow-up, ensuring reliability and exploring the relationship between autonomy and asthma management. However the exclusion of critically ill patients may limit the applicability of the findings to a broader patient population, the cross-sectional design does not allow for causal inferences, as it captures data at a single point in time, and Potential biases in self-reported data could affect the accuracy of the results, as patients may overestimate their autonomy.
The study's limitation is the use of the Patient Autonomy Preference Index, which may not be specific to bronchial asthma management. The tool does not account for unique aspects of asthma care, such as adherence to individualized action plans or specific guidelines. The study also did not evaluate adherence behaviors, such as medication use or proper inhaler technique. Future research should adapt Patient Autonomy Preference Index to better reflect asthma care and recruit a larger cohort to further validate these findings and enhance their generalizability.
Implications for nursing practice
Nurses should be aware of the factors influencing patient autonomy, such as health literacy and access to healthcare, to better support patients in self-management and also Training programs focusing on enhancing communication skills can empower nurses to facilitate shared decision-making with patients, particularly in rural settings where barriers exist.
Conclusion and recommendation
Only around forty-two percent of study participants were autonomous in managing their asthma exacerbation. Thus healthcare providers should give due attention to those who reside in rural areas, are not insured, recently diagnosed with asthma, and with low health literacy to enhance patient autonomy and self-management practices, ultimately improving health outcomes for individuals with asthma.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study received ethical approval from the Jimma University Research and Ethics Review Board (reference number JUIH/IRB/371/23), which also accepted the research protocol's ethics. A formal letter of collaboration was also provided, and the study was submitted to the chronic follow-up unit. Participants signed an informed consent form after being made aware of the purpose of the study. They were also told that their participation would be unaffected by their departure and that confidentiality and privacy would be upheld.
Author contributions
SA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. FK: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Global Initiative for Asthma. Global initiative for asthma: Global strategy for asthma management and prevention. CiNii Research. (2023). Available online at: https://cir.nii.ac.jp/crid/1571417124559903616 (cited 2024 August 8).
2. Sharma AE, Huang B, Knox M, Willard-Grace R, Potter MB. Patient engagement in community health center leadership: how does it happen? J Community Health. (2018) 43:1069–74. doi: 10.1007/s10900-018-0523-z
3. Venkatesan P. GINA report for asthma. Lancet Respir Med. (2023) 11(7):589. doi: 10.1016/S2213-2600(23)00230-8
4. Merhej T, Zein JG. Epidemiology of asthma: prevalence and burden of disease. In: Brasier AR, Jarjour NN, editors. Precision Approaches to Heterogeneity in Asthma. Cham: Springer International Publishing (2023). p. 3–23. (Advances in Experimental Medicine and Biology; vol. 1426). Available online at: https://link.springer.com/10.1007/978-3-031-32259-4_1 (cited 2024 August 9).
5. Lewis J, Holm S. Patient autonomy, clinical decision making, and the phenomenological reduction. Med Health Care Philos. (2022) 25(4):615–27. doi: 10.1007/s11019-022-10102-2
6. Olufadewa I, Adesina M, Ayorinde T. Global health in low-income and middle-income countries: a framework for action. Lancet Glob Health. (2021) 9(7):e899–900. doi: 10.1016/S2214-109X(21)00143-1
7. Yimer G, Tadesse Z, Alemayehu T. Prevalence of multidrug-resistant bacteria in Ethiopia: a systematic review and meta-analysis—ScienceDirect. (2023). Available online at: https://www.sciencedirect.com/science/article/pii/S2213716521001375 (cited 2024 August 9).
8. Mulugeta E, Ayele T, Zeleke G, Tesfay G. Asthma control and its predictors in Ethiopia: systematic review and meta-analysis—PMC. (2022). Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8758033/ (cited 2024 August 9).
9. Sullivan MD. Caring for patients with chronic illness: is respecting patient autonomy enough or must we promote patient autonomy as well? Fam Pract. (2023) 66:cmad066. doi: 10.1093/fampra/cmad066
10. Tesfay FH, Zorbas C, Alston L, Backholer K, Bowe SJ, Bennett CM. Prevalence of chronic non-communicable diseases in Ethiopia: a systematic review and meta-analysis of evidence. Front Public Health. (2022) 10:936482. doi: 10.3389/fpubh.2022.936482
11. Tola Gemeda A, Regassa LD, Weldesenbet AB, Merga BT, Legesse N, Tusa BS. Adherence to antihypertensive medications and associated factors among hypertensive patients in Ethiopia: systematic review and meta-analysis. SAGE Open Med. (2020) 8:2050312120982459. doi: 10.1177/2050312120982459
12. Birhanu Z, Abamecha F, Berhanu N, Dukessa T, Beharu M, Legesse S, et al. Patients’ healthcare, education, engagement, and empowerment rights’ framework: patients’, caretakers’ and health care workers’ perspectives from Oromia, Ethiopia. PLoS ONE. (2021) 16(8):e0255390. doi: 10.1371/journal.pone.0255390
13. World Health Organization. Asthma. Asthma. (2023). Available online at: https://www.who.int/news-room/fact-sheets/detail/asthma (cited 2024 August 9).
14. Alem K, Gebeyehu S, Arega Y. Risk factors and treatment types for asthma severity among adult patients. J Asthma Allergy. (2020) 13:167–77. doi: 10.2147/JAA.S246464
15. Negash M, Tsegabrhan H, Meles T, Tadesse DB, Gidey G, Berhane Y, et al. Determinants of acute asthma attack among adult asthmatic patients visiting hospitals of Tigray, Ethiopia, 2019: case control study. Asthma Res Pract. (2020) 6:1–7. doi: 10.1186/s40733-020-00054-w
16. Zewdie S, Mekuria B, Alemu BK, Bayked EM, Toleha HN, Ayenew W, et al. Prevalence of medication adherence among adult asthmatic patients in four African countries: a systematic review and meta-analysis. World Allergy Organ J. (2024) 17(2):100870. doi: 10.1016/j.waojou.2024.100870
17. Kassahun A, Zewdie A. Decision-making autonomy in maternal health service use and associated factors among women in Mettu District, Southwest Ethiopia: a community-based cross-sectional study. BMJ Open. (2022) 12(5):e059307. doi: 10.1136/bmjopen-2021-059307
18. Beauchamp TL, Childress JF. Principles of biomedical ethics—Paperback—Tom L. Beauchamp; James F. Childress—Oxford University Press. (2013). Available online at: https://global.oup.com/ushe/product/principles-of-biomedical-ethics-9780190640873?cc=us&lang=en& (cited 2024 August 10).
19. Bahrom NH, Ramli AS, Isa MR, Baharudin N, Badlishah Sham SF, Mohamed Yassin MS, et al. Validity and reliability of the patient activation measure® (PAM®)-13 malay version among patients with metabolic syndrome in primary care. Malays Fam Physician. (2020) 15(3):22–34.33329860
20. Kaya Z, Erkan F, Ozkan M, Ozkan S, Kocaman N, Ertekin BA, et al. Self-management plans for asthma control and predictors of patient compliance. J Asthma. (2009) 46(3):270–5. doi: 10.1080/02770900802647565
21. Lee YK, Ng CJ, Lee PY, Tong WT, Sa’at H. Shared decision-making in Malaysia: legislation, patient involvement, implementation and the impact of COVID-19. Z Für Evidenz Fortbild Qual Im Gesundheitswesen. (2022) 171:89–92. doi: 10.1016/j.zefq.2022.04.020
22. Fetensa G. Self-management practice and associated factors among asthmatic patients on follow-up care at public tertiary hospitals, South West, Ethiopia, 2022. PLoS One. (2024) 19:e0300589. doi: 10.1371/journal.pone.0300589
23. Desalu OO, Adeoti AO, Ojuawo OB, Aladesanmi AO, Oguntoye MS, Afolayan OJ, et al. Urban–rural differences in the epidemiology of asthma and allergies in Nigeria: a population-based study. J Asthma Allergy. (2021) 14:1389–97. doi: 10.2147/JAA.S333133
24. Amoah AS, McLean E, Price AJ, Amberbir A, Crampin AC. Factors associated with self-reported diagnosed asthma in urban and rural Malawi: observations from a population-based study of non-communicable diseases. PLoS Glob Public Health. (2024) 4(7):e0002952. doi: 10.1371/journal.pgph.0002952
25. Ozoh OB, Ayuk AC, Ukwaja KN, Desalu OO, Olufemi O, Aderibigbe SA, et al. Asthma management and control in Nigeria: the asthma insight and reality Nigeria (AIRNIG) study. Expert Rev Respir Med. (2019) 13(9):917–27. doi: 10.1080/17476348.2019.1651201
26. Miles C, Arden-Close E, Thomas M, Bruton A, Yardley L, Hankins M, et al. Barriers and facilitators of effective self-management in asthma: systematic review and thematic synthesis of patient and healthcare professional views. NPJ Prim Care Respir Med. (2017) 27:57. doi: 10.1038/s41533-017-0056-4
27. Codispoti CD, Greenhawt M, Oppenheimer J. The role of access and cost-effectiveness in managing asthma: a systematic review. J Allergy Clin Immunol Pract. (2022) 10(8):2109–16. doi: 10.1016/j.jaip.2022.04.025
28. Gardner EA, Kaplan BM, Collins P, Zahran H. Breathe well, live well: implementing an adult asthma self-management education program. Health Promot Pract. (2021) 22(5):702–13. doi: 10.1177/1524839920933259
29. DeSouza A. “Asthma is a part of you, it isn’t who you are” A qualitative study of parental perceptions, beliefs, and experiences when making decision regarding physical activity for children with asthma—ProQuest. (2017). Available online at: https://www.proquest.com/openview/d26afb1ba79feda0d3b8a8810f966dd8/1?pq-origsite=gscholar&cbl=18750 (cited 2024 August 17).
30. Jaakkola JJK, Aalto SAM, Hernberg S, Kiihamäki SP, Jaakkola MS. Regular exercise improves asthma control in adults: a randomized controlled trial. Sci Rep. (2019) 9(1):12088. doi: 10.1038/s41598-019-48484-8
31. Lewis G. A qualitative study explaining family-management of children’s and young people’s asthma in the changing COVID-19 context. (2023). Available online at: https://typeset.io/papers/a-qualitative-study-explaining-family-management-of-1930rmlxmd (cited 2024 August 17).
32. Ochoa-Avilés C, Peñaherrera-Vélez MJ, Morillo D, Andrade S, Peralta K, Verdugo NSL, et al. A conceptual framework for asthma self-management in Ecuadorian children and adolescents: a qualitative study. New Trends Qual Res. (2023) 16:e795. doi: 10.36367/ntqr.16.2023.e795
33. Dayo AR, Ghoto MA, Shah SM. Evaluation of asthma: aggravating factors and family history- a pro-spective observational study. Liaquat Med Res J. (2023) 5:67–73. doi: 10.38106/lmrj.2023.5.2-06
34. Ghozali MT, Urrohmah UA. Determining the relationship between the knowledge on self-management and levels of asthma control among adult asthmatic patients: a cross-sectional study. J Med Life. (2023) 16(3):442–6. doi: 10.25122/jml-2022-0333
35. Agustiyaningsih T, Rahayu EO, Purwanto E, Al Husna CH. Self-management in asthma patients: a systematic review. KnE Med. (2023) 3:435–66. doi: 10.18502/kme.v3i2.13078
36. Hodkinson A, Bower P, Grigoroglou C, Zghebi SS, Pinnock H, Kontopantelis E, et al. Self-management interventions to reduce healthcare use and improve quality of life among patients with asthma: systematic review and network meta-analysis. Br Med J. (2020) 370:m2521. doi: 10.1136/bmj.m2521
37. Stoneley A, Anderson J, Sutton C. The influence of health literacy and self-management on emergency healthcare access for rural asthmatics: a patient’s perspective. Cureus. (2023) 12:1–10. doi: 10.7759/cureus.50350
38. Han Y-Y, Gutwein AB, Apter A, Celedón JC. Health literacy and asthma: an update. J Allergy Clin Immunol. (2023) 153:1–8. doi: 10.1016/j.jaci.2023.12.007
39. Joshi HD, Kalauni BR, Bhusal K, Bhandari R, Subedi A, Bhandari B. (PDF) Health literacy among patients with non-communicable diseases at a tertiary level hospital in Nepal- a cross sectional study (2024) | Hari Datt Joshi. (2023). Available online at: https://typeset.io/papers/health-literacy-among-patients-with-non-communicable-4fe9iftyr9 (cited 2024 August 17).
40. Nock A, Petersen-Ewert C, Jürgensen I-N, Metzing S. Health literacy of patients with chronic diseases—quantitative results of a mixed methods study in primary healthcare/Gesundheitskompetenz von Menschen mit chronischer Erkrankung—quantitative Ergebnisse einer mixed-methods-studie in der primärversorgung. Int J Health Prof. (2024) 11:823–34. doi: 10.2478/ijhp-2024-0005
Keywords: patient, autonomous, asthma, self-management, Ethiopia
Citation: Abdulwehab S and Kedir F (2024) Patient autonomy in self-managing their bronchial asthma exacerbation and its associated factors, 2024. Front. Allergy 5:1483897. doi: 10.3389/falgy.2024.1483897
Received: 20 August 2024; Accepted: 7 October 2024;
Published: 25 October 2024.
Edited by:
Christine McCusker, McGill University Health Center, CanadaReviewed by:
Miguel Angel Tejedor-Alonso, Hospital Universitario Fundación Alcorcón, SpainJennifer L. P. Protudjer, University of Manitoba, Canada
Copyright: © 2024 Abdulwehab and Kedir. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sadik Abdulwehab, c2FkaWthYmR1bHdlaGFiQGdtYWlsLmNvbQ==
 Sadik Abdulwehab
Sadik Abdulwehab Frezer Kedir
Frezer Kedir