- 1The European Forum for Research and Education in Allergy and Airway Diseases Scientific Expert Team Members, Brussels, Belgium
- 2Otolaryngology Department, Hospital Comarcal de la Línea de La Concepción, Cádiz, Spain
- 3Department of Allergy & Rhinology, Royal National ENT Hospital, London, United Kingdom
- 4Division of Immunity and Infection, University College, London, United Kingdom
Introduction: Aspirin desensitization (AD) and aspirin therapy after desensitization (ATAD) are therapeutic interventions for patients with aspirin-exacerbated respiratory disease (AERD). Our aim is to investigate whether its addition to endoscopic sinus surgery (ESS) improves the overall prognosis of the disease.
Methods: A systematic review of the current literature including adult patients with a positive diagnosis of AERD undergoing endoscopic sinus surgery (ESS) in the context or in absence of upper airway comorbidity, prior to AD + ATAD.
Conclusion: This review concludes that the surgical approach is beneficial in AERD, but its effects are short—lived. Surgery should be considered initially with subsequent AD + ATAD in AERD patients, due to the sustained improvement achieved compared to those receiving ESS alone.
Introduction
Non-steroidal anti-inflammatory drug (NSAID)-exacerbated respiratory disease (N-ERD), also known as Samter's triad or aspirin-exacerbated respiratory disease (AERD), is a chronic eosinophilic, inflammatory condition of the upper and lower airway tract that occurs in patients with Chronic Rhinosinusitis with Nasal Polyps (CRSwNP), asthma and hypersensitivity to COX-1 inhibiting drugs (1).
The disorder affects 0.6%–2.5% of the general population, 7% of patients with asthma and 15% of patients with severe asthma (2) and it is estimated that AERD will occur in around 40% of asthmatic patients with CRSwNP (3). The prevalence of aspirin (ASA) sensitivity is found in 16% of CRS cases, 28.3% in CRS without nasal polyps (CRSsNP) cases, and 38.5% in CRSwNP and asthma cases (4) and its peak onset occurs in the third and fourth decades of life (5).
CRS results in significant functional, emotional, and quality of life impairment with several associated comorbidities, some of them directly associated to its inflammatory nature and the concept of united airway such as allergic rhinitis or asthma, and others indirectly related such as diabetes, glaucoma, or obstructive sleep apnoea (6–8). AERD is one CRS phenotype that is less responsive to medical and/or surgical therapy compared to other phenotypes (9, 10). In addition, previous studies have found that AERD patients have objectively worse disease burden, poorer quality of life, and higher financial costs compared to their CRS counterparts (11).
Oral aspirin desensitization has demonstrated to be a safe and effective tool for the management of AERD (12) and has been shown to improve sinonasal outcomes measured by quality of life and need for revision surgery in multiple studies (13, 14).
On the other hand, Endoscopic Sinus Surgery (ESS) is key in the management of CRSwNP (15) in AERD and is primarily aimed at reducing tissue load and optimizing local medical treatment outcomes. However, the recurrence of nasal polyps after surgery is more frequent in AERD compared to CRSwNP patients without it (16) given a more extensive and aggressive sinonasal disease and higher rates of sinus surgery, and their polyps are more recalcitrant to both medical and surgical treatments (17, 18).
Typically, ESS is performed 2–4 weeks prior to starting aspirin desensitization and therapy to minimize the risk of polyp regrowth during the interval period and has been shown to be effective at controlling disease burden and symptoms (1, 2, 4). However, regardless of ESS technique and timing, aspirin desensitization followed by daily aspirin provides therapeutic benefits to most patients with AERD, including improved asthma control, decreased need for oral steroids and reduced nasal recurrence polyp (2).
This systematic review aims to investigate if endoscopic sinus surgery followed by AD + ATAD modifies the outcome, response or quality of life in adult patients with AERD and their comorbidities, compared to ESS alone (19, 20).
Methods
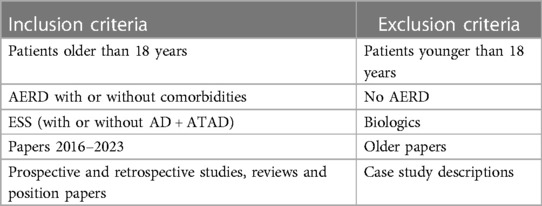
We conducted a systematic review following the PRISMA guidelines (21), and registered in PROSPERO under the protocol number CRD42023431414. Inclusion criteria were defined as adult patients with a positive diagnosis of AERD, undergoing endoscopic sinus surgery (ESS) as single treatment in the context or in absence of upper airway comorbidity, prior to AD + ATAD. Exclusion criteria are shown in Table 1.
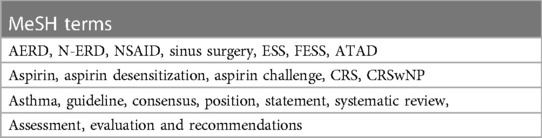
The search was conducted between April and May 2023, in PubMed, Scopus, Cochrane and Web of Science databases and designed using key Medical Subject Headings (MeSH) terms as referenced in PubMed Medical Subject Headings (Table 2).
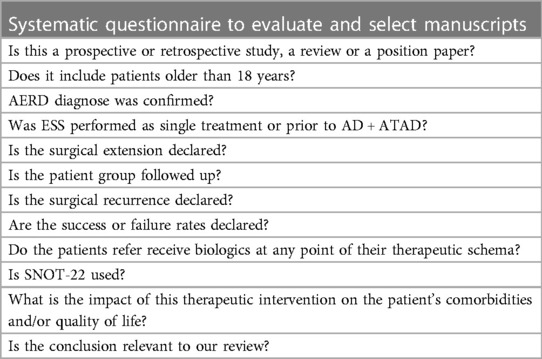
Two researchers independently reviewed the titles and abstracts using Rayyan webpage (22, 23), including papers that might meet the inclusion criteria, identified whether each item was assessed and whether the final conclusions had strict relation with the objective of this work, and discarded those that did not fulfil it (Table 3). In case of conflict, a third researcher solved it. In order to evaluate each manuscript systematically, we designed a questionnaire to be fulfilled by the authors. The risk of bias and quality assessment was made following the ROBINS-I (“Risk Of Bias In Non-randomized Studies—of Interventions”) tool from Cochrane® (24).
Results
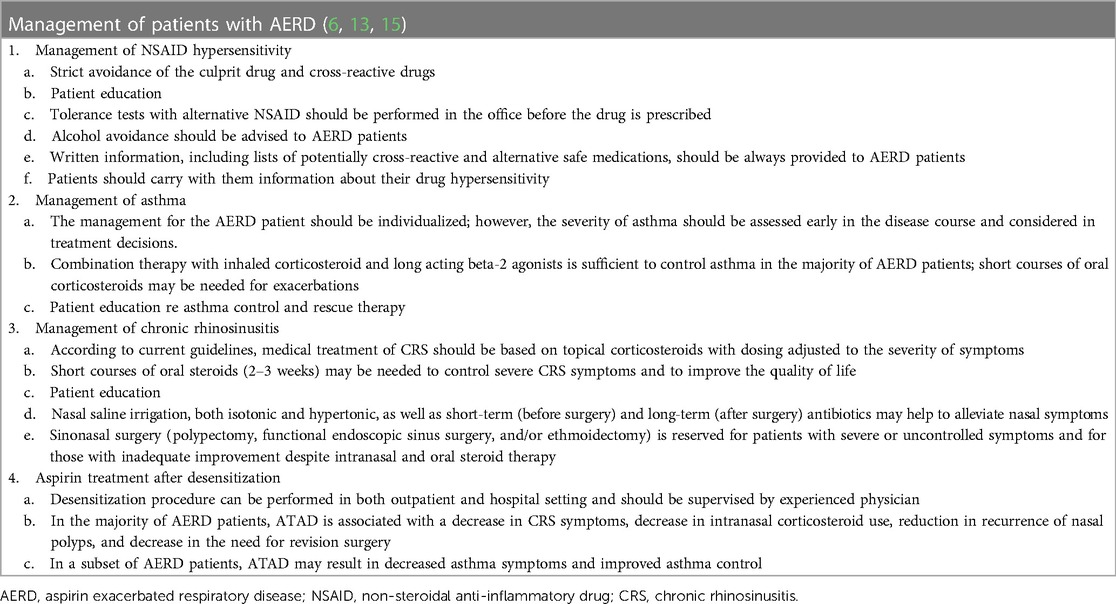
The treatment regimens presently available for the therapeutic management of patients with AERD are varied, as exemplified in Table 4. Therefore, we have selected to concentrate exclusively on the selection criteria discussed above, since they align with the aim of our review.
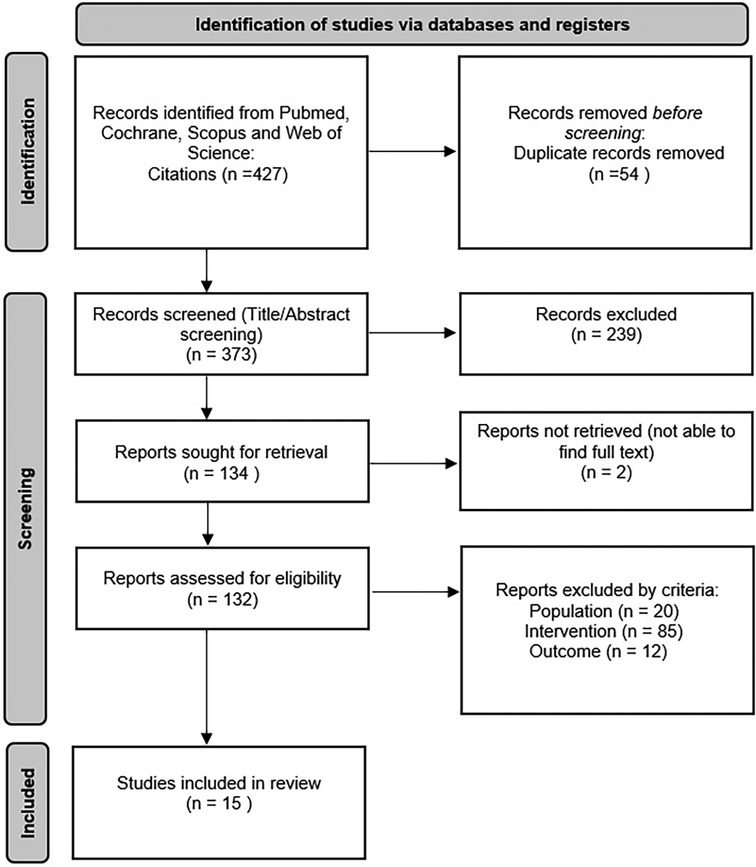
The search strategy identified 427 articles. Once 54 duplicates were removed, all abstracts were screened. Ultimately, 15 papers were selected for review (Figure 1).
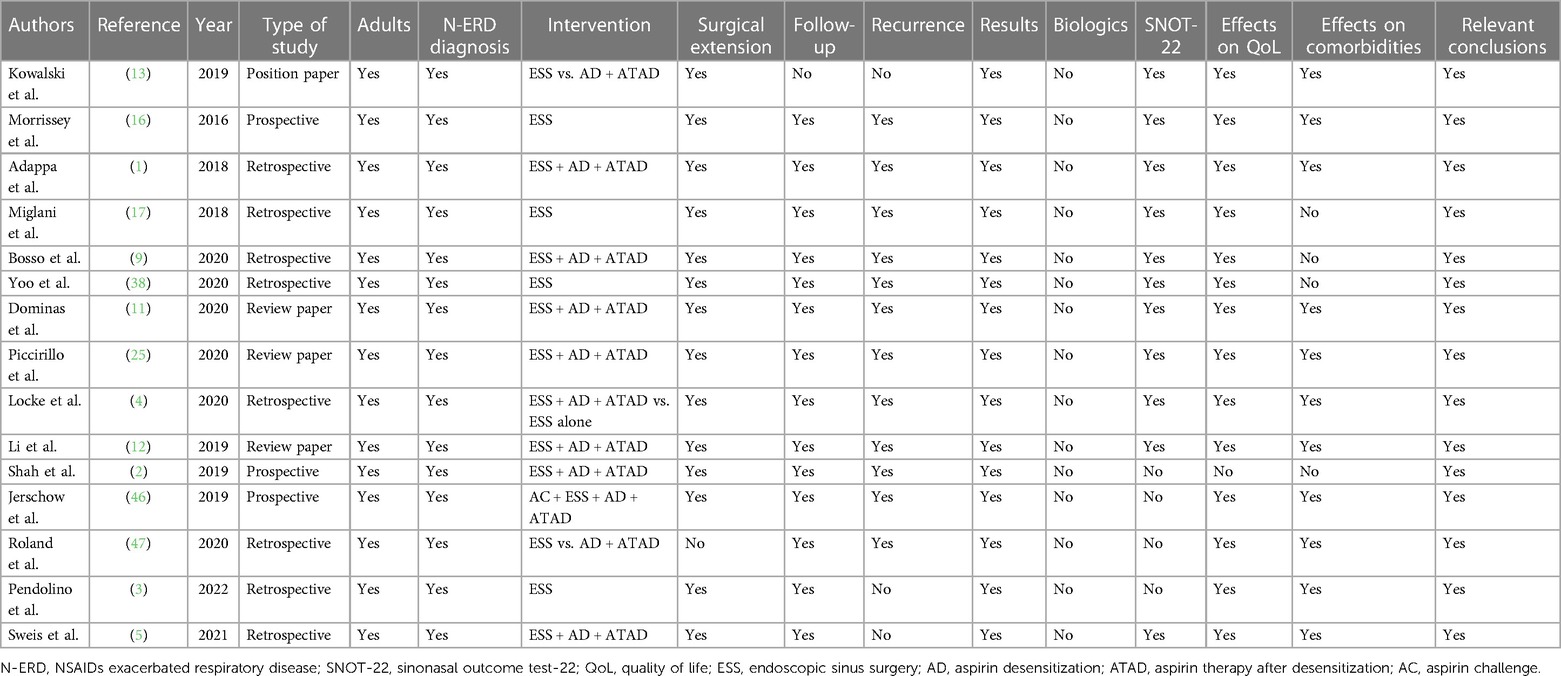
The data extraction outcome is shown in Table 5.
All of the papers (100%) recommended performing ESS in the context of AERD treatment due to the beneficial effect on patient status, and quality of life reflected on indexes as the sinonasal outcomes test (SNOT-22) (25). However, none of them (0%) recommended ESS as single treatment due to the lack of a sustained effect in time. In addition, 100% of the cited papers proposed that additional measures (like AD + ATAD) should be taken.
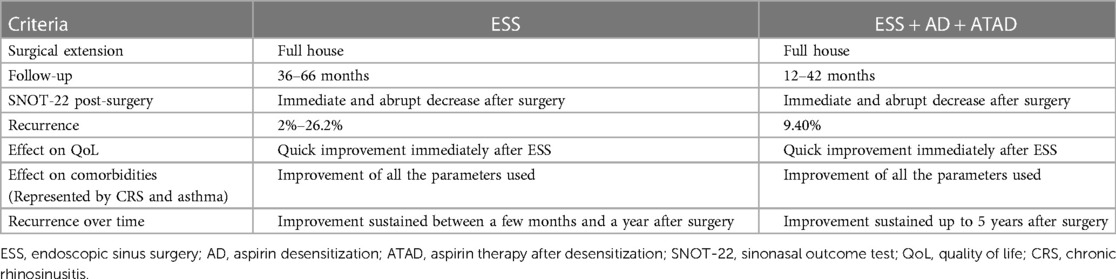
In Table 6, we show a comparison of ESS alone vs. ESS + AD + ATAD approaches.
Regarding the extent of the surgical procedure, almost all of the reviewed studies (93.3%) recommend a full-house approach as a therapeutic measure, without differentiation between groups. The same was found for the SNOT-22 post-operative indexes, where an immediate and abrupt significative decrease was observed in both groups. The mean score before ESS was 47.0, 15.2 for the 1-month post-ESS group, 20.7 for the 1-month post-desensitization group and 22.6 for the 30-month post-desensitization group (1).
Follow-up was extended from 36 to 66 months (average follow-up 51 months) in the ESS group and from 12 to 42 months in the ESS + AD + ATAD group (average follow-up 27 months), while recurrence and the need for reintervention ranged from 2% to 26.2% in the first group and 9.40% in the second.
Eleven out of fifteen papers (73.4%) mentioned an association between ESS and outcomes in patients’ comorbidities, regardless of the approach. All of them agreed on an improvement in all the indices used, including the patient's perception of the disease.
The main difference found was in the time it took to observe a relapse. While in the ESS group this was only a few months after surgery, in the ESS + AD + ATAD group the improvement was maintained up to 3 years after surgery.
Discussion
There are several pros and cons to be considered before suggesting an option to an individual patient. ESS is performed to remove polyps and alleviate symptoms, such as nasal congestion, runny nose, and facial pressure. It can improve sinus drainage, lower the risk of sinus infection, and improve respiratory function. A reduction in the required medications may result, but the patient should be advised that ESS is very rarely curative and that long term local treatment is necessary. Other considerations should be discussed in advance, such as the associated surgical risks (e.g., bleeding, infection, blindness, CSF leaks and anaesthesia-related problems), the need for revision surgery (due to the associated recurrence of the disease), the recovery time, and the direct and indirect associated costs.
Our review suggests that AD/ATAD probably extends the benefit of ESS in AERD, but there are significant problems with this conclusion.
There was no consensus on how to assess the effectiveness and/or evolution of treatment, nor on the surgical approach used. The SNOT-22 questionnaire and the criteria for the necessity and extent of any revision surgery have been the most commonly used outcomes (26, 27).
We have not found a consistent criterion on the proper timing to initiate AD + ATAD after ESS, nor have we identified a direct relationship between surgical extension and the timing of AD + ATAD. However, in all cases AD + ATAD was initiated between 2 and 6 weeks post-surgery.
The surgical extent proposed and evaluated was variable between studies, ranging from a targeted approach to a full house technique (28). Although there is no international consensus on the extent of the approach required, almost all reviewed studies recommend an aggressive initial surgical approach, such as full house. We conclude that the surgical extension could be explained by the fact that most of the recruited participants were patients with a history of previous ESS.
Patients with AERD who undergo more extensive ESS have been reported to have better outcomes than those who undergo more conservative sinus surgery, with lower recurrence and need for revision rates, and improved quality of life scores (29–31). We consider this is because large quantities of inflammatory tissue have been removed and because post-operative nasal patency facilitates appropriate subsequent pharmacological treatment. In addition, patients with AERD, compared with non-AERD patients, have twice as many sinus surgeries in their history and tend to be younger at the time of their first surgery (3). We consider that this is due to its association with asthma and other comorbidities, its highly eosinophilic nature and that the burden of the disease is greater with respect to CRSwNP alone.
It should be noted that targeted approaches were more common in patients undergoing their first ESS and full house technique was mostly performed in those undergoing a revision surgery. In any case, the extension of the surgical approach will be determined by the extent of the area involved and the experience and criteria of the surgeon (32–34).
Failure rates of standard ESS in these patients are reported to be as high as 90% at 5 years, while rates of revision surgery range from 38% to 89% at 10 years (3, 35).
As follow-up rates were not uniform between studies and, in some cases, very dissimilar, it is not possible to draw associations beyond a three-year postoperative period.
The case for recurrence rates on full house approaches was similar. Many papers did not declare these; however, from those that did we were able to establish a polyp recurrence of 58%. In addition, the need for revision surgery varied between 2% and 26.2%.
All papers described a symptomatic improvement, reflected in a marked decrease in SNOT-22, immediately after surgery (36–38). There was no consensus as to the duration of this therapeutic relief, which ranged from one year for the ESS group to three years for the ESS + AD + ATAD group, after which it tended to decrease and return to baseline (39).
In groups controlling for associated comorbidities, ESS has been shown to contribute to improvements in the severity and frequency of sinonasal and asthmatic symptoms (40–42), radiographic and endoscopic scores, and quality of life after surgery (43–45).
Jerschow et al. (46) found that prior to ESS, the diagnosis of AERD was confirmed in all patients in the study by aspirin tests that elicited hypersensitivity reactions. After ESS, aspirin reactions were less severe in all patients and twelve of twenty-eight patients (43%, p < 0.001) had no detectable reaction. This group proposes that the aspirin challenge would have a positive reinforcing effect on the surgical outcome, and the latter on the patient's response to aspirin exposure, justifying the low/zero levels of response seen after surgery.
Roland et al. (47) evaluated patients with AD on a two-months follow-up. Patients who underwent AD experienced a longer time between surgeries compared to patients who did not undergo AD.
Biologics have demonstrated their therapeutic efficacy in patients with AERD and their advent compels us to continue research into their precise indications in the upper and lower airways (13). Our knowledge and consensus on the therapeutic gold standard for these patients is likely to be revised in the short term and they may possibly become the new therapeutic gold standard. However, there is still a good case for initial use of ESS plus ATAD as it is considerably cheaper and very effective in some subjects (5, 48).
Conclusion
We conclude that while surgery plays a key role in the treatment of patients with AERD, as reflected by significant improvements in quality of life and comorbidities, the combination with postoperative AD + ATAD maintains this improvement in long-term follow-up, also reducing recurrence and revision surgery rates, so that a combined approach should always be considered.
Author contributions
All the authors have made substantial contributions to the conception or design of the work, the acquisition, analysis, and interpretation of data for the work. They have drafted the work and revised it critically for important intellectual content, have provided approval for publication of the content, and have agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors contributed to the article and approved the submitted version.
Conflict of interest
GS: Honoraria for articles, speaker and advisory boards: ALK, AstraZeneca, Capnia, Church & Dwight, Circassia, Noucor, GSK, Meda/Mylan/Viatris, Merck, Sanofi- Regeneron, Stallergenes. Scientific Chief Editor, Rhinology Section, Frontiers in Allergy. Board Member, Lead for Allergic Rhinitis, EUFOREA. Chair of Data Monitoring Board for Paediatric AR trials of HDM SLIT.
The remaining author(s) declare(s) that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AC, aspirin challenge; AD, aspirin desensitization; AERD, aspirin exacerbated respiratory disease; ASA, aspirin; ATAD, aspirin therapy after desensitization; CRS, chronic rhinosinusitis; CRSwNP, chronic rhinosinusitis with nasal polyps; EPOS, European position paper on rhinosinusitis and nasal polyps; ESS, endoscopic sinus surgery; FESS, functional endoscopic sinus surgery; N-ERD, NSAIDs exacerbated respiratory disease; NSAID, non-steroidal anti-inflammatory drug; QoL, quality of life; SNOT-22, sinonasal outcome test.
References
1. Adappa ND, Ranasinghe VJ, Trope M, Brooks SG, Glicksman JT, Parasher AK, et al. Outcomes after complete endoscopic sinus surgery and aspirin desensitization in aspirin-exacerbated respiratory disease. Int Forum Allergy Rhinol. (2018) 8(1):49–53. doi: 10.1002/alr.22036
2. Shah SJ, Abuzeid WM, Ponduri A, Pelletier T, Ren Z, Keskin T, et al. Endoscopic sinus surgery improves aspirin treatment response in aspirin-exacerbated respiratory disease patients. Int Forum Allergy Rhinol. (2019) 9(12):1401–8. doi: 10.1002/alr.22418
3. Pendolino AL, Bandino F, Navaratnam AV, Ross T, Qureishi A, Randhawa P, et al. The role of large cavity sinus surgery in the management of chronic rhinosinusitis in N-ERD: a single-centre experience and long-term outcomes. J Laryngol Otol. (2022):1–16. doi: 10.1017/S0022215122002468
4. Locke T, Sweis A, Lin T, Sweis B, Gleeson P, Kohanski M, et al. The impact of endoscopic sinus surgery and aspirin desensitization on psychological burden in aspirin-exacerbated respiratory disease. World J Otorhinolaryngol Head Neck Surg. (2020) 6(4):214–9. doi: 10.1016/j.wjorl.2020.07.008
5. Sweis AM, Locke TB, Ig-Izevbekhai KI, Lin TC, Kumar A, Douglas JE, et al. Effectiveness of endoscopic sinus surgery and aspirin therapy in the management of aspirin-exacerbated respiratory disease. Allergy Asthma Proc. (2021) 42(2):136–41. doi: 10.2500/aap.2021.42.210002
6. Fokkens WJ, Lund VJ, Hopkins C, Hellings PW, Kern R, Reitsma S, et al. European position paper on rhinosinusitis and nasal polyps 2020. Rhinology. (2020) 58(Suppl S29):1–464. doi: 10.4193/Rhin20.600. PMID: 32077450
7. De Prins L, Raap U, Mueller T, Schmid-Grendelmeier P, Haase CH, Backer V, et al. White paper on European patient needs and suggestions on chronic type 2 inflammation of airways and skin by EUFOREA. Front Allergy. (2022) 3:889221. (Erratum in: Front Allergy. 2022 Sep 09;3:1001078). doi: 10.3389/falgy.2022.889221
8. Claeys N, Teeling MT, Legrand P, Poppe M, Verschueren P, De Prins L, et al. Patients unmet needs in chronic rhinosinusitis with nasal polyps care: a patient advisory board statement of EUFOREA. Front Allergy. (2021) 2:761388. (Erratum in: Front Allergy. 2021 Oct 29;2:789425). doi: 10.3389/falgy.2021.761388
9. Bosso JV, Locke TB, Kuan EC, Tripathi SH, Ig-Izevbekhai KI, Kalaf LT, et al. Complete endoscopic sinus surgery followed by aspirin desensitization is associated with decreased overall corticosteroid use. Int Forum Allergy Rhinol. (2020) 10(9):1043–8. doi: 10.1002/alr.22604
10. Bayar Muluk B, Cingi C, Scadding GK, Scadding G. Chronic rhinosinusitis-could phenotyping or endotyping aid therapy? Am J Rhinol Allergy. (2019) 33(1):83–93. doi: 10.1177/1945892418807590
11. Dominas C, Gadkaree S, Maxfield AZ, Gray ST, Bergmark RW. Aspirin-exacerbated respiratory disease: a review. Laryngoscope Investig Otolaryngol. (2020) 5(3):360–7. doi: 10.1002/lio2.387
12. Li KL, Lee AY, Abuzeid WM. Aspirin exacerbated respiratory disease: epidemiology, pathophysiology, and management. Med Sci (Basel). (2019) 7(3):45. doi: 10.3390/medsci7030045
13. Kowalski ML, Agache I, Bavbek S, Blanca M, Bochenek G, et al. Diagnosis and management of NSAID-exacerbated respiratory disease (N-ERD)-a EAACI position paper. Allergy. (2019) 74(1):28–39. doi: 10.1111/all.13599
14. Pendolino AL, Scadding GK, Scarpa B, Andrews PJ. A retrospective study on long-term efficacy of intranasal lysine-aspirin in controlling NSAID-exacerbated respiratory disease. Eur Arch Otorhinolaryngol. (2022) 279(5):2473–84. doi: 10.1007/s00405-021-07063-2
15. Hellings PW, Fokkens WJ, Orlandi R, Adriaensen GF, Alobid I, Baroody FM, et al. The EUFOREA pocket guide for chronic rhinosinusitis. Rhinology. (2023) 61(1):85–9. doi: 10.4193/Rhin22.344
16. Morrissey DK, Bassiouni A, Psaltis AJ, Naidoo Y, Wormald PJ. Outcomes of modified endoscopic lothrop in aspirin-exacerbated respiratory disease with nasal polyposis. Int Forum Allergy Rhinol. (2016) 6(8):820–5. doi: 10.1002/alr.21739
17. Miglani A, Divekar RD, Azar A, Rank MA, Lal D. Revision endoscopic sinus surgery rates by chronic rhinosinusitis subtype. Int Forum Allergy Rhinol. (2018) 8(9):1047–51. doi: 10.1002/alr.22146
18. Howe R, Mirakian RM, Pillai P, Gane S, Darby YC, Scadding GK. Audit of nasal lysine aspirin therapy in recalcitrant aspirin exacerbated respiratory disease. World Allergy Organ J. (2014) 7(1):18. doi: 10.1186/1939-4551-7-18
19. Hellings PW, Scadding G, Bachert C, Bjermer L, Canonica GW, Cardell LO, et al. EUFOREA treatment algorithm for allergic rhinitis. Rhinology. (2020) 58(6):618–22. doi: 10.4193/Rhin20.246
20. Scadding GK, Smith PK, Blaiss M, Roberts G, Hellings PW, Gevaert P, et al. Allergic rhinitis in childhood and the new EUFOREA algorithm. Front Allergy. (2021) 2:706589. doi: 10.3389/falgy.2021.706589
21. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71. doi: 10.1136/bmj.n71
22. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. (2016) 5(210). doi: 10.1186/s13643-016-0384-4
23. Clark J, Glasziou P, Del Mar C, Bannach-Brown A, Stehlik P, Scott AM. A full systematic review was completed in 2 weeks using automation tools: a case study. J Clin Epidemiol. (2020) 121:81–90. doi: 10.1016/j.jclinepi.2020.01.008
24. Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. Br Med J. (2016) 355:i4919. doi: 10.1136/bmj.i4919
25. Piccirillo JF, Edwards D, Haiduk A, et al. Psychometric and clinimetric validity of the 31-item rhinosinusitis outcome measure (RSOM-31). Am J Rhinol. (1995) 9(6):297–308. doi: 10.2500/105065895781808711
26. Muhonen EG, Goshtasbi K, Papagiannopoulos P, Kuan EC. Appropriate extent of surgery for aspirin-exacerbated respiratory disease. World J Otorhinolaryngol Head Neck Surg. (2020) 6(4):235–40. doi: 10.1016/j.wjorl.2020.07.005
27. Cai S, Lou H, Zhang L. Prognostic factors for post-operative outcomes in chronic rhinosinusitis with nasal polyps: a systematic review. Expert Rev Clin Immunol. (2023):1–15. doi: 10.1080/1744666X.2023.2218089
28. Ramkumar SP, Marks L, Lal D, Marino MJ. Outcomes of limited versus extensive surgery for chronic rhinosinusitis: a systematic review and meta-analysis. Int Forum Allergy Rhinol. (2023). doi: 10.1002/alr.23178
29. Fried J, Yuen E, Gudis DA, Schlosser RJ, Nguyen SA, Rowan NR. Changes in sleep quality following treatment for chronic rhinosinusitis: a systematic review and meta-analysis. Am J Rhinol Allergy. (2022) 36(3):386–96. doi: 10.1177/19458924211061442
30. Dhiman S, Dhiman A, Azad RK, Negi PC, Lal B, Thakur JS. Nasal polyposis and its association with cardiac functions. Med Princ Pract. (2021) 30(6):522–6. doi: 10.1159/000517976
31. Beswick DM, Ayoub NF, Mace JC, Mowery A, Hwang PH, Smith TL. Acute exacerbations in recurrent acute rhinosinusitis: differences in quality of life and endoscopy. Laryngoscope. (2020) 130(12):E736–41. doi: 10.1002/lary.28460
32. Gill AS, Alt JA, Detwiller KY, Rowan NR, Gray ST, Hellings PW, et al. Management paradigms for chronic rhinosinusitis in individuals with asthma: an evidence-based review with recommendations. Int Forum Allergy Rhinol. (2023). doi: 10.1002/alr.23130
33. Tiotiu A, Novakova P, Baiardini I, Bikov A, Chong-Neto H, de-Sousa JC, et al. Manifesto on united airways diseases (UAD): an interasma (global asthma association—GAA) document. J Asthma. (2022) 59(4):639–54. doi: 10.1080/02770903.2021.1879130
34. Ferris BG Jr, Mead J, Opie LH. Partitioning of respiratory flow resistance in man. J Appl Physiol. (1964) 19:653–8. doi: 10.1152/jappl.1964.19.4.653
35. Zhang L, Zhang Y, Gao Y, Wang K, Lou H, Meng Y, Wang C. Long-term outcomes of different endoscopic sinus surgery in recurrent chronic rhinosinusitis with nasal polyps and asthma. Rhinology. (2020) 58(2):126–35. doi: 10.4193/Rhin19.184
36. Bengtsson C, Lindberg E, Jonsson L, Holmström M, Sundbom F, Hedner J, et al. Chronic rhinosinusitis impairs sleep quality: results of the GA2LEN study. Sleep. (2017) 40(1). doi: 10.1093/sleep/zsw021
37. Campbell AP, Phillips KM, Hoehle LP, Feng AL, Bergmark RW, Caradonna DS, et al. Depression symptoms and lost productivity in chronic rhinosinusitis. Ann Allergy Asthma Immunol. (2017) 118(3):286–9. doi: 10.1016/j.anai.2016.12.012
38. Yoo F, Schlosser RJ, Storck KA, Ganjaei KG, Rowan NR, Soler ZM. Effects of endoscopic sinus surgery on objective and subjective measures of cognitive dysfunction in chronic rhinosinusitis. Int Forum Allergy Rhinol. (2019) 9(10):1135–43. doi: 10.1002/alr.22406
39. Grose E, Lee DJ, Yip J, Cottrell J, Sykes J, Lee JK, et al. Surgical outcomes in aspirin-exacerbated respiratory disease without aspirin desensitization. Int Forum Allergy Rhinol. (2020) 10(10):1149–57. doi: 10.1002/alr.22626
40. Kominsky E, Liu KY, Ninan S, Arrighi-Allisan A, Filimonov A, Kidwai S, et al. Seeking an optimal dose of preoperative corticosteroids in chronic rhinosinusitis with nasal polyposis: a randomized controlled trial. Am J Otolaryngol. (2022) 43(4):103476. doi: 10.1016/j.amjoto.2022.103476
41. Chen S, Zhou A, Emmanuel B, Garcia D, Rosta E. Systematic literature review of humanistic and economic burdens of chronic rhinosinusitis with nasal polyposis. Curr Med Res Opin. (2020) 36(11):1913–26. doi: 10.1080/03007995.2020.1815683
42. Jiang RS, Liang KL. The influence of functional endoscopic sinus surgery on sleep related outcomes in patients with chronic rhinosinusitis. Int J Otolaryngol. (2019) 2019:7951045. doi: 10.1155/2019/7951045
43. Alt JA, Ramakrishnan VR, Platt MP, Schlosser RJ, Storck T, Soler ZM. Impact of chronic rhinosinusitis on sleep: a controlled clinical study. Int Forum Allergy Rhinol. (2019) 9(1):16–22. doi: 10.1002/alr.22212
44. Bengtsson C, Jonsson L, Holmström M, Svensson M, Theorell-Haglöw J, Lindberg E. Impact of nasal obstruction on sleep quality: a community-based study of women. Eur Arch Otorhinolaryngol. (2015) 272(1):97–103. doi: 10.1007/s00405-014-3067-6
45. Bengtsson C, Jonsson L, Holmström M, Franklin K, Gíslason T, et al. Incident chronic rhinosinusitis is associated with impaired sleep quality: results of the RHINE study. J Clin Sleep Med. (2019) 15(6):899–905. doi: 10.5664/jcsm.7846
46. Jerschow E, Edin ML, Chi Y, Hurst B, Abuzeid WM, Akbar NA, et al. Sinus surgery is associated with a decrease in aspirin-induced reaction severity in patients with aspirin exacerbated respiratory disease. J Allergy Clin Immunol Pract. (2019) 7(5):1580–8. doi: 10.1016/j.jaip.2018.12.014
47. Roland LT, Nagy C, Wang H, Moore R, Cahill KN, Laidlaw TM, et al. Treatment practices for aspirin-exacerbated respiratory disease: analysis of a national insurance claims database. Int Forum Allergy Rhinol. (2020) 10(2):190–3. doi: 10.1002/alr.22471
Keywords: AERD, N-ERD, ESS, FESS, sinus surgery, ATAD, aspirin desensitization, CRSwNP
Citation: Conti DM, Correa EJ and Scadding GK (2023) Is endoscopic sinus surgery sufficient to modify the evolution of adult AERD? Aspirin desensitization as a maintenance factor: systematic review. Front. Allergy 4:1250178. doi: 10.3389/falgy.2023.1250178
Received: 29 June 2023; Accepted: 28 August 2023;
Published: 8 September 2023.
Edited by:
Giancarlo Ottaviano, University of Padua, Italy© 2023 Conti, Correa and Scadding. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Diego M. Conti Y29udGkuZGllZ29tYXJjZWxvQGdtYWlsLmNvbQ==
 Diego M. Conti
Diego M. Conti Eduardo J. Correa2
Eduardo J. Correa2 Glenis K. Scadding
Glenis K. Scadding