- 1Department Biology, UAntwerpen, Antwerpen, Belgium
- 2Division Ecology, Evolution, and Biodiversity Conservation, KU Leuven, Leuven, Belgium
- 3KU Leuven Department of Microbiology, Immunology and Transplantation, Allergy and Clinical Immunology Research Group, KU Leuven, Leuven, Belgium
- 4Institut de Recherche Santé et Societé, UC Louvain, Louvain-la-Neuve, Belgium
- 5Department of Epidemiology and Public Health, Sciensano, Brussels, Belgium
- 6Department of Translational Physiology, Infectiology, and Public Health, Ghent University, Merelbeke, Belgium
- 7Department of Geography, University of Namur, Namur, Belgium
- 8Mycology and Aerobiology, Sciensano, Brussels, Belgium
- 9Risk and Health Impact Assessment, Sciensano, Brussels, Belgium
The increasing burden of pollen allergy
Allergic rhinitis, conjunctivitis, and asthma are common manifestations of allergies (1). These allergic disorders are associated with a relative high health burden for modern societies because of their high prevalence, often life-long morbidity, and impact on mental health and well-being. Therefore, they are a major public health problem (2). The past decades, the allergy prevalence and sensitization rates have globally increased (1, 3–7). This prevalence is expected to even further increase in the following decades.
On the one hand, the increase is expected through a better general population understanding of allergy that will increase the number of patients seeking help (8). Also, the implementation of better diagnostic methods may increase the number of patients getting diagnosed. Even so, an increasing prevalence over the years has already been observed with traditional skin-prick testing, a longstanding standard of care for respiratory allergy diagnosis (7). On the other hand, a rise in allergic diseases is also expected as a result of various interactions between changes in the environment and modern lifestyle (1, 9–11).
One such interaction is the air pollution, that accompanies the global increase in urbanization, which exacerbates airway diseases including allergic rhinitis as a consequence of pollen exposure (12). Several mechanisms have been described by which air pollution can affect pollen allergens and their ability to induce allergenic symptoms in patients. Firstly, rising environmental ozone (O3) and ambient CO2 concentrations have been documented to alter allergenic properties of pollen grains in grasses and in tree species (4, 13–15). Secondly, air pollutants can also cause respiratory inflammation and epithelial barrier damage, therefore priming the airways and facilitate allergen access (16). Furthermore, brief exposure to nitrogen dioxide (NO2) has resulted in an enhanced eosinophilic activity in response to allergens by pollen-allergenic asthmatics (17). Also, nitrogen dioxide exposure in a mouse model was able to induce an allergenic response to aerosolized OVA, an innocuous protein that by itself does not trigger an immune response (18). Pollen exposed to ozone and NO2 have also shown an increased activation of oxidative defense mechanisms which was associated with increased IgE recognition (19). In addition, air pollutants can affect allergen protein structure by inducing post-translational modifications e.g., protein nitration, leading to increased allergen specific IgE levels (20, 21). Finally, air pollutant exposure has been associated with sensitization to pollen allergens and with pollen-allergic symptoms (22–25).
These effects might be species dependent and while decreasing the pollen load for some species, it might also increase for others. Allergic sensitization in patients also results in different seasonal profiles and varies among different regions. The overall effect can result in pollen allergy patients that are exposed to more of certain pollen types and potentially increasingly potent pollen and this often over longer time periods. This escalates the burden of allergic diseases and the costs for society. Additionally, in the context of the recent global pandemic, pollen allergy patients may be more susceptible to infectious diseases including COVID-19, as pollen exposure weakens the innate defense against respiratory viruses (26) and unmanaged hay fever may increase the risk of viral dissemination, for instance through excessive sneezing (27).
Environmental nitrogen pollution causing increasing prevalence of allergy?
The risk for respiratory allergic diseases may also be exacerbated by global environmental change. Indeed, environmental change can alter plant species distribution ranges, pollen amounts and pollen traits, the onset and length of pollen seasons, and the atmospheric pollen distribution patterns (7, 10, 28–30). For instance, rising global temperatures have caused long-term changes in the timing and increases in the duration and the intensity of a series of allergenic pollen seasons in Europe, for instance for birch, alder and hazel trees (31–34). Thus, depending on the plant species and their susceptibility to climatic forces, the duration and intensity of human pollen exposure has changed.
A potentially important yet underexplored global change driver that may drive increasing aeroallergens and allergy prevalence is environmental nitrogen pollution. Emissions from the combustion of fossil fuels and intensive agriculture have caused a twofold increase of biologically reactive nitrogen worldwide (35, 36). The anthropogenic perturbation of the global nitrogen cycle is therefore identified as one of the largest threats to the global biosphere integrity and human health (37–40). In high nitrogen emission regions, total inorganic nitrogen deposition rates are well above 50 kg N ha−1 yr−1 (41). In the Atlantic biogeographic region of Europe, current atmospheric nitrogen deposition levels range between 2.4 and 43.5 kg N ha−1 yr−1 depending on land use and land cover (42), with the highest levels associated with intensive agriculture, urbanization, and industry (43). The health risks associated with atmospheric nitrogen pollution, such as the risks of allergic inflammatory diseases and asthma associated with atmospheric NOx, are well recognized (44–48). However, the potential impacts of nitrogen pollution on human health via increased soil nitrogen availability and subsequent plant uptake of nitrogen, have not yet been quantified and the mechanisms are poorly understood (39, 49, 50). Yet, here we argue that this may represent important unexplored pathways for increased pollen allergy prevalence.
The ecological effects of environmental nitrogen enrichment include biodiversity loss, changes in plant community composition, ecosystem simplification, and loss of ecosystem service provisioning capacity (51–54). Specifically, nitrogen pollution leads to more productive ecosystems, which tend to become species-poor and dominated by a few, highly competitive plant species (52, 55–57). For example, in acidic grasslands surveyed across a nitrogen deposition gradient in the Atlantic biogeographic region of Europe, plant species richness decreased by 21.7% for each increment of 10 kg total inorganic nitrogen deposition ha−1 yr−1 [OR = 0.78 (42)]. Importantly in the context of pollen allergy, nitrogen pollution in heathlands and grasslands worldwide is associated with an increase in productivity of grasses (for instance Molinia caerulea) that become dominant at the expense of forbs and dwarf shrubs (52, 58–59). As grass pollen are among the world's most harmful aeroallergens (60), it is easy to conceive that nitrogen pollution may thus change pollen allergenic landscapes to the detriment of the societal burden of respiratory disease. In forests also, nitrogen pollution can cause an increase in tree productivity (61), that subsequently may also lead to increases in airborne tree pollen and the burden of allergy.
It has been hypothesized before that changes in plant community composition and primary productivity may affect airborne pollen distributions and abundances with subsequent potential knock-on effects for pollen allergy patients (60, 62). However, to our knowledge, changes in plant community composition and productivity driven by environmental nitrogen pollution remain to be linked with changes in the severity of pollen allergy. Yet, in an era of ever increasing nitrogen pollution (39, 49, 50) and of allergic disorders (1, 3–6), we feel that it is urgently needed to quantify this pathway.
In addition to changes in plant communities driven by nitrogen pollution, experiments have shown that the biochemical composition of plant pollen is significantly altered following nitrogen fertilization (63, 64). These biochemical changes may very well affect the allergen potency of pollen with important human health consequences, even if plant pollen productivity and community composition of allergenic plant species would be unaffected by nitrogen pollution. Unfortunately, data on biochemical changes in pollen following nitrogen enrichment is very scarce and the potential effect on allergy response remains a broad knowledge gap. We hypothesize that nitrogen-induced biochemical changes in pollen allergenicity could be associated with more severe allergy symptoms, indicated by increased IgE-specific reactivity (in vitro) or increased allergy symptom severity scores (in vivo).
Nitrogen-induced changes in plant species composition, in combination with altered allergenic properties of plants, could therefore result in landscapes with elevated allergy risks relative to landscapes free of nitrogen pollution. In addition, the combination of higher allergy risks at the level of the landscape and increased allergy symptom severity escalates the burden of allergic disease (Figure 1).
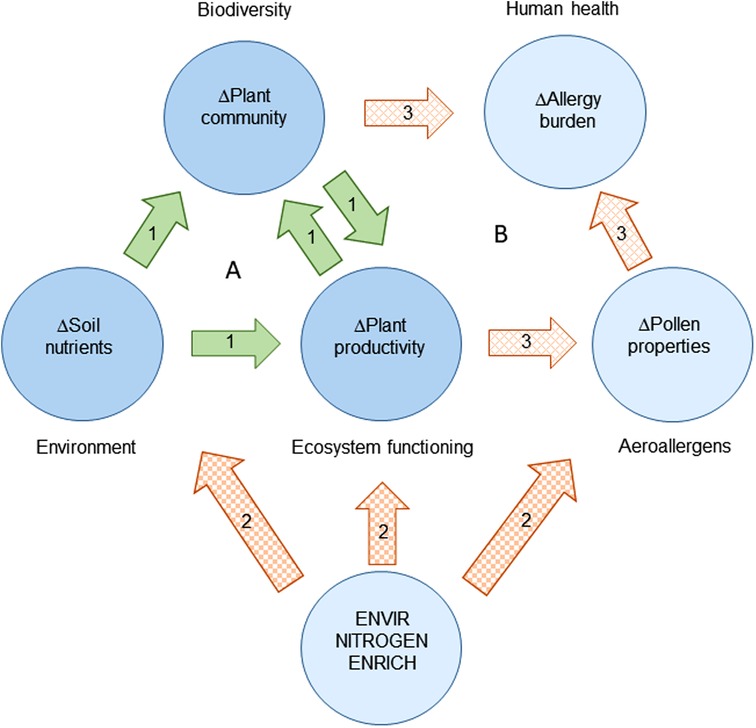
Figure 1. Environmental nitrogen pollution and the burden of allergic disease in the light of environment, biodiversity, and ecosystem functioning. (A) Under the present “biodiversity-ecosystem functioning” paradigm, biodiversity and environmental variation drive ecosystem functioning, such as plant productivity (arrow set 1). (B) Environmental nitrogen pollution may drive changes in the burden of pollen allergies through a combination of direct changes (arrow set 2) and indirect changes (arrow set 3) in the abiotic environment, plant species composition, plant productivity, airborne pollen species composition and abundance, and, importantly, allergen potency.
Conclusion
Environmental nitrogen pollution may have important direct and indirect impacts on plant species composition and productivity on the one hand, and on allergenicity of pollen aeroallergens on the other. Consequently, nitrogen pollution may change the prevalence, incidence, and severity of allergic disease by modifying the places where people live into landscapes with higher pollen exposure, resulting in elevated allergy risks, and increased allergy symptom severity.
Nitrogen pollution worldwide urges us to determine the effects on allergy prevalence, allergenicity and symptom severity to understand, prevent, and control these unexplored pathways of nitrogen-driven allergy risks to public health.
We argue that these insights are needed to better inform environmental policy with respect to reduction of environmental nitrogen pollution, which at present only aims to reduce the direct impact of air pollution on respiratory health and to support biodiversity conservation. It does not take into account the potential effects on public health we have outlined here. Yet, improved policy measures may not only help to maintain the favourable conservation status of biodiversity and vulnerable habitats, but also help to sustain the habitability of areas prone to nitrogen pollution, such as urbanized and industrialized regions and regions with intensive agriculture—indeed the places where most people live.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication. All authors contributed to the article and approved the submitted version.
Funding
The authors acknowledge funding of the NITROPOL-BE project (B2/212/P1/NITROPOL-BE, coordinated by RA) by the Belgian Science Policy Office (BELSPO) in the framework of Belgian Research Action through Interdisciplinary Networks (BRAIN-be 2.0). RS is supported by a FWO senior clinical investigator fellowship (1805518N). Funders had no role in the design and preparation of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gilles S, Akdis C, Lauener R, Schmid-Grendelmeier P, Bieber T, Schäppi G, et al. The role of environmental factors in allergy: a critical reappraisal. Exp Dermatol. (2018) 27:1193–200. doi: 10.1111/exd.13769
2. Lake IR, Jones NR, Agnew M, Goodess CM, Giorgi F, Hamaoui-Laguel L, et al. Climate change and future pollen allergy in Europe. Environ Health Perspect. (2017) 125:385–91. doi: 10.1289/EHP173
3. Brożek JL, Bousquet J, Agache I, Agarwal A, Bachert C, Bosnic-Anticevich S, et al. Allergic rhinitis and its impact on asthma (ARIA) guidelines—2016 revision. J Allerg Clin Immunol. (2017) 140:950–8. doi: 10.1016/j.jaci.2017.03.050
4. D’Amato G, Cecchi L, Bonini S, Nunes C, Annesi-Maesano I, Behrendt H, et al. Allergenic pollen and pollen allergy in Europe. Allergy. (2007) 62:976–90. doi: 10.1111/j.1398-9995.2007.01393.x
5. D’Amato G, Vitale C, Lanza M, Molino A, D’Amato M. Climate change, air pollution, and allergic respiratory diseases: an update. Curr Opin Allergy Clin Immunol. (2016) 16:434–40. doi: 10.1097/ACI.0000000000000301
6. Newson RB, van Ree R, Forsberg B, Janson C, Lötvall J, Dahlén SE, et al. Geographical variation in the prevalence of sensitization to common aeroallergens in adults: the GA(2) LEN survey. Allergy. (2014) 69:643–51. doi: 10.1111/all.12397
7. Beutner C, Werchan B, Forkel S, Gupta S, Fuchs T, Schön MP, et al. Sensitization rates to common inhaled allergens in Germany – increase and change patterns over the last 20 years. J Dtsch Dermatol Ges. (2021) 19:37–44. doi: 10.1111/DDG.14312
8. Zuberbier T, Lötvall J, Simoens S, Subramanian SV, Church MK. Economic burden of inadequate management of allergic diseases in the European union: a GA(2) LEN review. Allergy. (2014) 69(10):1275–9. doi: 10.1111/all.12470
9. Pfefferle PI, Keber CU, Cohen RM, Garn H. The hygiene hypothesis – learning from but not living in the past. Front Immunol. (2021) 12:635935. doi: 10.3389/FIMMU.2021.635935
10. D’Amato G, Cecchi L. Effects of climate change on environmental factors in respiratory allergic diseases. Clin Exp Allergy. (2008) 38:1264–74. doi: 10.1111/j.1365-2222.2008.03033.x
11. Reinmuth-Selzle K, Kampf CJ, Lucas K, Lang-Yona N, Fröhlich-Nowoisky J, Shiraiwa M, et al. Air pollution and climate change effects on allergies in the anthropocene: abundance, interaction, and modification of allergens and adjuvants. Environ Sci Technol. (2017) 51:4119–41. doi: 10.1021/acs.est.6b04908
12. Lee YG, Lee PH, Choi SM, An MH, Jang AS. Effects of air pollutants on airway diseases. Int J Environ Res Public Health. (2021) 18(18):9905. doi: 10.3390/IJERPH18189905
13. Beck I, Jochner S, Gilles S, McIntyre M, Buters JTM, Schmidt-Weber C, et al. High environmental ozone levels lead to enhanced allergenicity of birch pollen. PLoS One. (2013) 8:e80147. doi: 10.1371/journal.pone.0080147
14. Buters J, Prank M, Sofiev M, Pusch G, Albertini R, Annesi-Maesano I, et al. Variation of the group 5 grass pollen allergen content of airborne pollen in relation to geographic location and time in season. J Allergy Clin Immunol. (2015) 136:87–95. doi: 10.1016/j.jaci.2015.01.049
15. Kim KR, Oh J-W, Woo S-Y, Seo YA, Choi YJ, Kim HS, et al. Does the increase in ambient CO2 concentration elevate allergy risks posed by oak pollen? Int J Biometeorol. (2018) 62:1587–95. doi: 10.1007/s00484-018-1558-7
16. D’Amato G, Cecchi L, D’Amato M, Liccardi G. Urban air pollution and climate change as environmental risk factors of respiratory allergy: an update. J Investig Allergol Clin Immunol. (2010) 20(2):95–102. https://www.jiaci.org/issues/vol20issue2/1.pdf
17. Barck C, Lundahl J, Halldén G, Bylin G. Brief exposures to NO2 augment the allergic inflammation in asthmatics. Environ Res. (2005) 97(1):58–66. doi: 10.1016/j.envres.2004.02.009
18. Bevelander M, Mayette J, Whittaker LA, Paveglio SA, Jones CC, Robbins J, et al. Nitrogen dioxide promotes allergic sensitization to inhaled antigen. J Immunol. (2007) 179(6):3680–8. doi: 10.4049/JIMMUNOL.179.6.3680
19. Galveias A, Arriegas R, Mendes S, Ribeiro H, Abreu I, Costa AR, et al. Air pollutants NO2- and O3-induced Dactylis glomerata L. Pollen oxidative defences and enhanced its allergenic potential. Aerobiologia. (2021) 37(1):127–37. doi: 10.1007/S10453-020-09676-2
20. Gruijthuijsen YK, Grieshuber I, Stöcklinger A, Tischler U, Fehrenbach T, Weller MG, et al. Nitration enhances the allergenic potential of proteins. Int Arch Allergy Immunol. (2006) 141(3):265–75. doi: 10.1159/000095296
21. Franze T, Weller MG, Niessner R, Pöschl U. Protein nitration by polluted air. Environ Sci Technol. (2005) 39(6):1673–8. doi: 10.1021/es0488737
22. Melén E, Standl M, Gehring U, Altug H, Antó JM, Berdel D, et al. Air pollution and IgE sensitization in 4 European birth cohorts—the MeDALL project. J Allergy Clin Immunol. (2021) 147(2):713–22. doi: 10.1016/j.jaci.2020.08.030
23. Riediker M, Monn C, Koller T, Stahel WA, Wüthrich B. Air pollutants enhance rhinoconjunctivitis symptoms in pollen-allergic individuals. Ann Allergy Asthma Immunol. (2001) 87(4):311–8. doi: 10.1016/S1081-1206(10)62246-6
24. Cabrera M, Subiza J, Fernández-Caldas E, Garzón García B, Moreno-Grau S, Subiza JL. Influence of environmental drivers on allergy to pollen grains in a case study in Spain (Madrid): meteorological factors, pollutants, and airborne concentration of aeroallergens. Environ Sci Poll Res Int. (2021) 28(38):53614–28. doi: 10.1007/s11356-021-14346-y
25. Feo Brito F, Mur Gimeno P, Martínez C, Tobías A, Suárez L, Guerra F, et al. Air pollution and seasonal asthma during the pollen season. A cohort study in puertollano and ciudad real (Spain). Allergy. (2007) 62(10):1152–7. doi: 10.1111/j.1398-9995.2007.01438.x
26. Gilles S, Blume W, Wimmer M, Damialis A, Meulenbroek L, Gökkaya M, et al. Pollen exposure weakens innate defense against respiratory viruses. Allergy. (2020) 75:576–87. doi: 10.1111/all.14047
27. Scadding GK, Hellings PW, Bachert C, Bjermer L, Diamant Z, Gevaert P, et al. Allergic respiratory disease care in the COVID-19 era: a EUFOREA statement. World Allergy Organ J. (2020) 13:100124. doi: 10.1016/j.waojou.2020.100124
28. Beggs PJ. Impacts of climate change on aeroallergens: past and future. Clin Exp Allergy. (2004) 34:1507–13. doi: 10.1111/j.1365-2222.2004.02061.x
29. Barnes CS. Impact of climate change on pollen and respiratory disease. Curr Allergy Asthma Rep. (2018) 18:59. doi: 10.1007/s11882-018-0813-7
30. Demain JG. Climate change and the impact on respiratory and allergic disease: 2018. Curr Allergy Asthma Rep. (2018) 18:22. doi: 10.1007/s11882-018-0777-7
31. Ziello C, Sparks TH, Estrella N, Belmonte J, Bergmann KC, Bucher E, et al. Changes to airborne pollen counts across Europe. PLoS One. (2012) 7:e34076. doi: 10.1371/journal.pone.0034076
32. Bruffaerts N, De Smedt T, Delcloo A, Simons K, Hoebeke L, Verstraeten C, et al. Comparative long-term trend analysis of daily weather conditions with daily pollen concentrations in Brussels, Belgium. Int J Biometeorol. (2018) 62:483–91. doi: 10.1007/s00484-017-1457-3
33. Hoebeke L, Bruffaerts N, Verstraeten C, Delcloo A, De Smedt T, Packeu A, et al. Thirty-four years of pollen monitoring: an evaluation of the temporal variation of pollen seasons in Belgium. Aerobiologia. (2018) 34:139–55. doi: 10.1007/s10453-017-9503-5
34. Ziska LH, Makra L, Harry SK, Bruffaerts N, Hendrickx M, Coates F, et al. Temperature-related changes in airborne allergenic pollen abundance and seasonality across the northern hemisphere: a retrospective data analysis. Lancet Planet Health. (2019) 3(3):e124–31. doi: 10.1016/S2542-5196(19)30015-4
35. Galloway JN, Townsend AR, Erisman JW, Bekunda M, Cai Z, Freney JR, et al. Transformation of the nitrogen cycle: recent trends, questions, and potential solutions. Science. (2008) 320:889–92. doi: 10.1126/science.1136674
36. Peñuelas J, Sardans J, Rivas-Ubach A, Janssens IA. The human-induced imbalance between C, N and P in Earth's Life system. Global Change Biol. (2012) 189:5–8. doi: 10.1111/j.1365-2486.2011.02568.x
37. Rockström J, Steffen W, Noone K, Persson A, Stuart Chapin F III, Lambin EF, et al. A safe operating space for humanity. Nature. (2009) 461:472–5. doi: 10.1038/461472a
38. Steffen W, Richardson K, Rockström J, Cornell SE, Fetzer I, Bennett EM, et al. Planetary boundaries: guiding human development on a changing planet. Science. (2015) 347:1259855. doi: 10.1126/science.1259855
39. Kanter DR, Chodos O, Nordland O, Rutigliano M, Winiwarter W. Gaps and opportunities in nitrogen pollution policies around the world. Nat Sustain. (2020) 3:956–63. doi: 10.1038/s41893-020-0577-7
40. Nieder R, Benbi DK. Reactive nitrogen compounds and their influence on human health: an overview. Rev Environ Health. (2021) 24:229–46. doi: 10.1515/reveh-2021-0021
41. Zhang CH, Guo HR, Huang H, Ma TY, Song W, Chen CJ, et al. Atmospheric nitrogen deposition and its responses to anthropogenic emissions in a global hotspot region. Atmosph Res. (2020) 248:105137. doi: 10.1016/j.atmosres.2020.105137
42. Stevens CJ, Duprè C, Dorland E, Gaudnik C, Gowing DJG, Bleeker A, et al. Nitrogen deposition threatens species richness of grasslands across Europe. Environ Pollut. (2010) 158:2940–5. doi: 10.1016/j.envpol.2010.06.006
43. Schaap M, Banzhaf S, Scheuschner T, Geupel L, Hendriks C, Kranenburg R, et al. Atmospheric nitrogen deposition to terrestrial ecosystems across Germany. Biogeosci Discuss. (2017):bg-2017-491. doi: 10.5194/bg-2017-491
44. Brauer M, Hoek G, Smit HA, de Jongste JC, Gerritsen J, Postma DS, et al. Air pollution and development of asthma, allergy and infections in a birth cohort. Eur Respir J. (2007) 29:879–88. doi: 10.1183/09031936.00083406
45. D’Amato G. Effects of climatic changes and urban air pollution on the rising trends of respiratory allergy and asthma. Multidiscip Respir Med. (2011) 6:28–37. doi: 10.1186/2049-6958-6-1-28
46. Kim KH, Jahan SA, Kabir E. A review on human health perspective of air pollution with respect to allergies and asthma. Environ Int. (2013) 59:41–52. doi: 10.1016/j.envint.2013.05.007
47. Miyazaki D, Fukagawa K, Fukushima A, Fujishima H, Uchio E, Ebihara N, et al. Air pollution significantly associated with severe ocular allergic inflammatory diseases. Sci Rep. (2019) 9:18205. doi: 10.1038/s41598-019-54841-4
48. Bettiol A, Gelain E, Milanesio E, Asta F, Rusconi F. The first 1000 days of life: traffic-related air pollution and development of wheezing and asthma in childhood. A systematic review of birth cohort studies. Environ Health. (2021) 20:46. doi: 10.1186/s12940-021-00728-9
49. Johnson PTJ, Townsend AR, Cleveland CC, Glibert PM, Howarth RW, McKenzie VJ, et al. Linking environmental nutrient enrichment and disease emergence in humans and wildlife. Ecol Appl. (2010) 20:16–29. doi: 10.1890/08-0633.1
50. Erisman JW, Galloway JN, Seitzinger S, Bleeker A, Dise NB, Petrescu AMR, et al. Consequences of human modification of the global nitrogen cycle. Phil Trans Royal Soc B-Biol Sci. (2013) 368:20130116. doi: 10.1098/rstb.2013.0116
51. Tilman D, Fargione J, Wolff B, D’Antonio A, Howarth R, Schindler D, et al. Forecasting agriculturally driven global environmental change. Science. (2001) 292:281–4. doi: 10.1126/science.1057544
52. Bobbink R, Hicks K, Galloway J, Spranger T, Alkemade R, Ashmore M, et al. Global assessment of nitrogen deposition effects on terrestrial plant diversity: a synthesis. Ecol Appl. (2010) 20:30–59. doi: 10.1890/08-1140.1
53. Stevens CJ, David TI, Storkey J. Atmospheric nitrogen deposition in terrestrial ecosystems: its impact on plant communities and consequences across trophic levels. Funct Ecol. (2018) 32:1757–69. doi: 10.1111/1365-2435.13063
54. Wang WJ, He HS, Thompson FR III, Spetich MA, Fraser JS. Effects of species biological traits and environmental heterogeneity on simulated tree species distribution shifts under climate change. Sci Total Environ. (2018) 634:1214–21. doi: 10.1016/j.scitotenv.2018.03.353
55. Damgaard C, Jensen L, Frohn LM, Borchsenius F, Nielsen KE, Ejrnæs R, et al. The effect of nitrogen deposition on the species richness of acid grasslands in Denmark: a comparison with a study performed on a European scale. Environ Pollut. (2011) 159:1778–82. doi: 10.1016/j.envpol.2011.04.003
56. Ceulemans T, Stevens CJ, Duchateau L, Jacquemyn H, Gowing DJG, Merckx R, et al. Soil phosphorus constrains biodiversity across European grasslands. Global Change Biol. (2014) 20:3814–22. doi: 10.1111/gcb.12650
57. van der Plas F. Biodiversity and ecosystem functioning in naturally assembled communities. Biol Rev. (2019) 94:1220–45. doi: 10.1111/brv.12499
58. Helsen K, Ceulemans T, Stevens CJ, Honnay O. Increasing soil nutrient loads of European semi-natural grasslands strongly alter plant functional diversity independently of species loss. Ecosystems. (2014) 17:169–81. doi: 10.1007/s10021-013-9714-8
59. Ceulemans T, Merckx R, Hens M, Honnay O. Plant species loss from European semi-natural grasslands following nutrient enrichment – is it nitrogen or is it phosphorus? Global Ecol Biogeogr. (2013) 22:73–82. doi: 10.1111/j.1466-8238.2012.00771.x
60. Brennan GL, Potter C, de Vere N, Griffith GW, Skjøth CA, Osborne NJ, et al. Temperate airborne grass pollen defined by spatio-temporal shifts in community composition. Nat Ecol Evol. (2019) 3:750–4. doi: 10.1038/s41559-019-0849-7
61. Thomas RQ, Canham CD, Weathers KC, Goodale CL. Increased tree carbon storage in response to nitrogen deposition in the US. Nat Geosci. (2010) 3:13–7. doi: 10.1038/ngeo721
62. Bernard-Verdier M, Seitz B, Buchholz S, Kowarik I, Mejía SL, Jeschke JM. Grassland allergenicity increases with urbanisation and plant invasions. Ambio. (2022) 51:2261–77. doi: 10.1007/s13280-022-01741-z
63. Townsend AR, Howarth RW, Bazzaz FA, Booth MS, Cleveland CC, Collinge SK, et al. Human health effects of a changing global nitrogen cycle. Front Ecol Environ. (2003) 1:240–6. doi: 10.1890/1540-9295(2003)001[0240:HHEOAC]2.0.CO;2
64. Ceulemans T, Hulsmans E, Vanden Ende W, Honnay O. Nutrient enrichment is associated with altered nectar and pollen chemical composition in Succisa pratensis moench and increased larval mortality of its pollinator Bombus terrestris L. PLoS ONE. (2017) 12:e0175160. doi: 10.1371/journal.pone.0175160
Keywords: allergic disease, biodiversity loss, environmental degradation, environmental pollution (including CO2 and SO2 emissions), epidemiology, nitrogen deposition, pollen allergy, respiratory health
Citation: Ceulemans T, Verscheure P, Shadouh C, Van Acker K, Devleesschauwer B, Linard C, Dendoncker N, Speybroeck N, Bruffaerts N, Honnay O, Schrijvers R and Aerts R (2023) Environmental degradation and the increasing burden of allergic disease: The need to determine the impact of nitrogen pollution. Front. Allergy 4:1063982. doi: 10.3389/falgy.2023.1063982
Received: 7 October 2022; Accepted: 12 January 2023;
Published: 2 February 2023.
Edited by:
Maria Pilar Plaza, Helmholtz Zentrum München, GermanyReviewed by:
Pawel Bogawski, Adam Mickiewicz University in Poznań, PolandCarl Alexander Frisk, Norwegian Institute of Bioeconomy Research (NIBIO), Norway
© 2023 Ceulemans, Verscheure, Shadouh, Van Acker, Devleesschauwer, Linard, Dendoncker, Speybroeck, Bruffaerts, Honnay, Schrijvers and Aerts. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Raf Aerts cmFmLmFlcnRzQHNjaWVuc2Fuby5iZQ==
Specialty Section: This article was submitted to Environmental & Occupational Determinants, a section of the journal Frontiers in Allergy
 Tobias Ceulemans
Tobias Ceulemans Paulien Verscheure
Paulien Verscheure Caroline Shadouh4
Caroline Shadouh4 Brecht Devleesschauwer
Brecht Devleesschauwer Niko Speybroeck
Niko Speybroeck Nicolas Bruffaerts
Nicolas Bruffaerts Rik Schrijvers
Rik Schrijvers Raf Aerts
Raf Aerts