- 1College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia
- 2King Abdullah International Medical Research Center, Jeddah, Saudi Arabia;
- 3Ministry of the National Guard-Health Affairs, Jeddah, Saudi Arabia
- 4College of Science and Health Professions, King Saud bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia
Background: Food allergy is an increasing health concern. Studies have shown that food allergy knowledge is lacking among people, especially in areas related to distinction between food allergy and intolerance, symptoms recognition, and current means of management. This knowledge gap puts allergic patients at more risk of getting fatal anaphylactic reactions, which occur mostly in public areas. Locally, Public's knowledge and attitudes of food allergy was not sufficiently investigated. Therefore, we aim to assess food allergy knowledge and attitudes among Jeddah population in Saudi Arabia.
Methods: We adopted The Chicago Food Allergy Research Survey for the General Public (CFARS-GP) and used it as a data collection tool. We hosted the questionnaire on Google Forms and distributed the link through social media outlets targeting individuals of Jeddah population who are 18 years old and above.
Results: A total of 510 individuals completed the survey. The respondents answered 56% of the knowledge-based items correctly. Knowledge was strongest in symptoms/severity and definition/diagnosis, while it was weakest in susceptibility and prevalence, distinction between food allergy and intolerance, and food allergy management. Higher knowledge was significantly associated with prior training in food allergy, food-allergic acquaintance (i.e., having food allergy or knowing an allergic patient), and being a relative of a health care worker. For the attitudes, respondents thought that food allergy negatively affects patients' quality of life, and that schools should establish policies to protect allergic children; however, they downplayed stigma associated with food allergy.
Conclusion: Increased food allergy knowledge among the general public is needed especially in areas related to susceptibility and prevalence, distinction between food allergy and intolerance, triggers and environmental risks, and the management of food allergy. Prior experience with food allergy through (1) training, (2) food-allergic acquaintance, or (3) being a relative of a health care worker increases food allergy knowledge significantly. Thus, targeted educational interventions might have a significant effect in improving food allergy knowledge among the general population.
Introduction
Food Allergy is defined as an immune-mediated response that is initiated by IgE antibodies upon exposure to a given food allergen (1). Food allergy has been known to be more prevalent among the pediatric population. Osborne and colleagues found that 10% of 1 year old infants in Australia have IgE-mediated food allergy that is proven by oral food challenge (2). Furthermore, it was reported that one in every twelve children in the United States has IgE-mediated food allergy (3). However, an increase in the prevalence of this condition has been reported among adults as well. For instance, a cross-sectional study in the United States estimated that one out of every ten adults has IgE-mediated food allergy (4).
Food is the most common trigger of anaphylaxis, an acute life-threatening systemic allergic reaction (1, 5). Death is a rare outcome of food-induced anaphylaxis that is caused mainly by accidental exposures to allergens. Additionally, poor management of food-induced anaphylactic reactions is a contributing factor to fatality. Several studies indicated that the incidence rate of fatal food anaphylaxis among the general population was low (0.03–0.3 deaths per million person per year), and that delayed use of intramuscular epinephrine injections has resulted in fatality in most of these cases (6–8).
Moreover, Pouessel and colleagues found that fatal anaphylactic reactions occur primarily following an unintentional exposure to food allergens outside home, such as in restaurants and schools (9). Thus, in order to deal with such cases, members of the general population should have sufficient food allergy knowledge, especially in management and epinephrine injections use. Despite the important role of the general population in the management of food-induced anaphylaxis, global and local data suggest that their food allergy knowledge is lacking. Gupta and et al. assessed food allergy knowledge among the US population and found that knowledge was weakest in areas related to current means of treating food allergy (10). Similarly, data from the limited number of available local studies suggest that there is an inadequate food allergy knowledge among the general public in Saudi Arabia with management being one of the major areas of poor knowledge (11, 12).
Poor food allergy knowledge among members of the general population, especially in areas related to symptoms recognition and current means of management, increases the risk of mortality among allergic individuals because they commonly experience anaphylactic reactions in public areas. Also, people who cannot differentiate between food allergy and other food related adverse reactions might label themselves as allergic patients and unnecessarily avoid some food. Therefore, the primary aim of this study is to assess the general public's knowledge and attitudes toward food allergy in Jeddah, Saudi Arabia.
Materials and methods
Study design
This is a cross sectional study that collected data using convenience sampling via an online questionnaire in both Arabic and English versions. We hosted the questionnaire on Google Forms webpage and distributed the link through social media channels targeting individuals of the general population of Jeddah city (aged 18 years and above) from May to August 2021. Participation was voluntary, and we administered an informed consent alongside the questionnaire. It is estimated that 3,457,794 individuals currently reside in the city of Jeddah (13). We calculated the targeted sample size considering the following criteria: (1) 95% confidence level; (2) 5% margin of error; and (3) 50% response rate and had resulted in a sample of 385 individuals. The institutional review board of King Abdullah International Medical Research Center (KAIMRC) approved this study. (approval No: JED-21-427780-49687).
Study instrument
A questionnaire of 47 items divided into 3 sections was used as a data collection tool (Supplementary Survey). The first section collected demographical characteristics of the participants (e.g., age and gender) using 11 items. In one of the questions in this section, an answer option was accidentally deleted from the Arabic version of the online survey that was distributed to the participants (Supplementary Table S1). The second section assessed the participants' knowledge of food allergy via a 17-item quiz (14 true/false and 3 multiple choice questions) which consists of 5 domains: definition and diagnosis, symptoms and severity, triggers and environmental risks, susceptibility and prevalence, and treatment and use of health care. For example, the participants were asked whether milk intolerance is the same as food allergy, and if lactating mothers could pass allergens to their babies through breast feeding. The third section assessed the attitudes and beliefs of the participants towards food allergy using 19 items (13 5-point Likert-scale with response options ranging from1 = Strongly Disagree to 5 = Strongly Agree, 4 multiple choice, and 2 Dichotomous styled questions with Yes/No response options). This section assessed the participants' attitudes towards stigma and acceptability, quality of life, current means of treatment and management, and policy issues related to this condition. For instance, we asked the participants if they agree that food allergy is a serious health concern locally, and that food allergy patients can eat safely at restaurants. Both the second and third sections were adopted from the Chicago Food Allergy Research Survey for General Public (CFARS-GP) developed by Gupta and colleagues (14). Minor modifications were made on the questionnaire to meet the study criteria. Forward and backward translations followed by an extensive review were made to ensure the quality of the translated version. With regard to the survey translation, a group member has translated the original survey into the Arabic language (forward translation). Then another group member who was blinded to the original survey has translated the Arabic version back into English (backward translation). The new English version was then compared with the original survey, and adjustments were made accordingly. This process was done to avoid literal translation and to ensure that all respondents perceive the questions in the same way regardless of the language they use to fill the survey.
Data analysis
All the collected data were stored in an excel sheet. We cleaned the data by screening the Excel sheet manually and excluding both incomplete responses and responses that did not meet the inclusion criteria. In addition, all data entry mistakes were identified and corrected. With regards to outliers, some were identified in the knowledge scores of respondents, but they were not deleted because they did not influence the data significantly. In addition, we coded the data with the same order of options that appears in the questionnaire. Both the cleaning and coding were done prior to the analysis. We used JMP®, Version 15. SAS Institute Inc., Cary, NC, 1989–2021 in the analysis. Data were described by frequency and percentage distributions. We calculated mean and standard deviation for scale items. We used independent samples t-test to compare the mean knowledge score between 2 independent groups. Additionally, we used Analysis of Variance (ANOVA) to compare the mean knowledge score between three or more independent groups. We used independent samples t-test and ANOVA because the data were normally distributed. The overall knowledge score was defined as the percentage of each respondent's true answers out of total items in the knowledge component. Both false and I don't know responses were considered as not true answers. A P value less than 0.05 was considered significant.
Results
Participant's characteristics
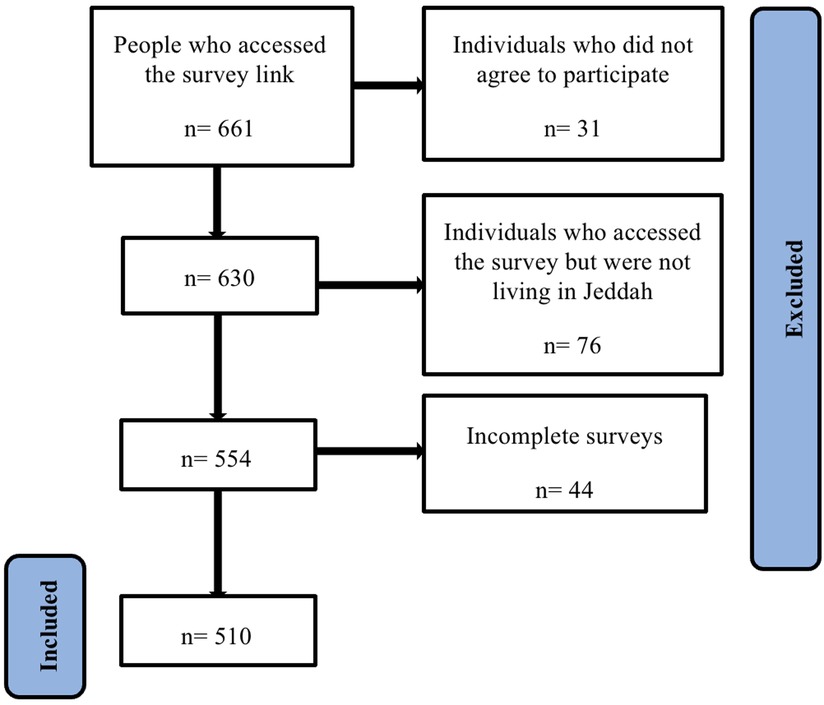
Initially, our target was to collect 385 complete responses. We expected that both the non-response rate, and the number of incomplete responses to be high, so we decided to distribute the survey to as much people as possible. We closed the survey when we did not get any more responses for one week. After closing the survey, the number of people who accessed it was 661 individuals. After excluding the individuals who did not agree to participate (n = 31), those who accessed the survey but were not living in Jeddah (n = 76), and incomplete surveys (n = 44), we got 510 complete responses, and we included them in the analysis (Figure 1). This exceeded our initial target of 385 responses.
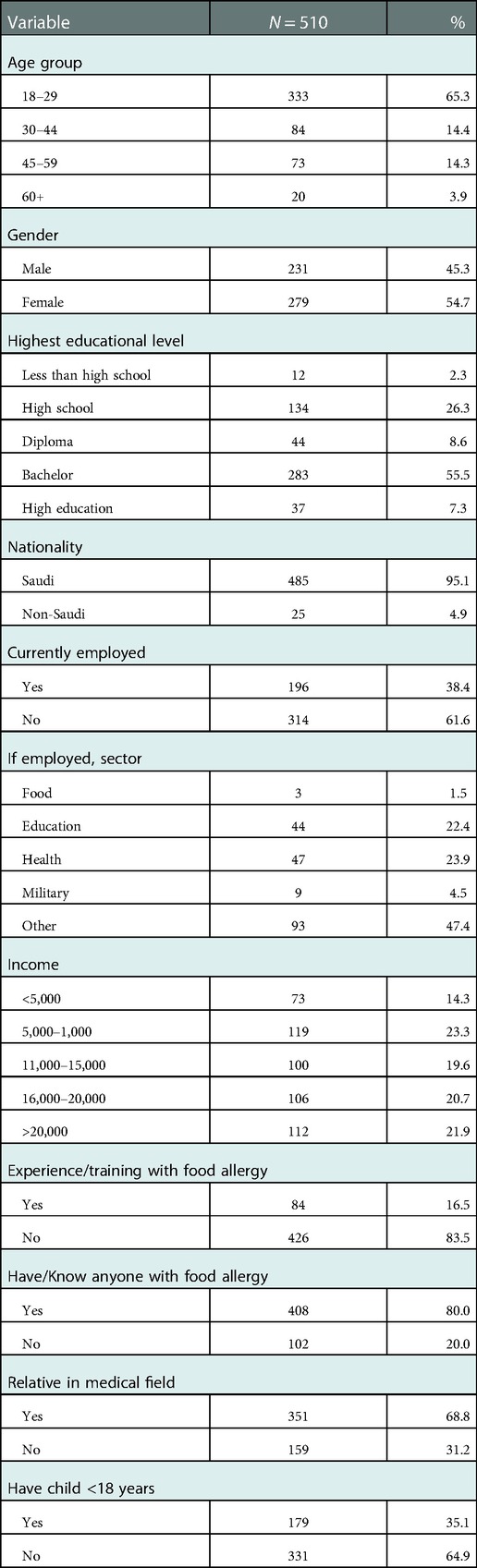
Table 1 shows that more females (54.7%) have responded to the survey compared with men (45.3%). About two thirds of the participants were young adults (<30 years), had a Bachelor degree or higher, were unemployed, and had a middle income (5,000–20,000 SAR/Month). Approximately, half of those who were employed had a job either in the health (n = 47) or the educational (n = 44) sectors. A large proportion of the participants (68.8%) had a relative in the health sector. Nearly 80% of the respondents had food allergy or knew someone with this condition. The majority of the respondents had no prior experience/training with food allergy through their jobs or work (83.5%).
Knowledge of food allergy
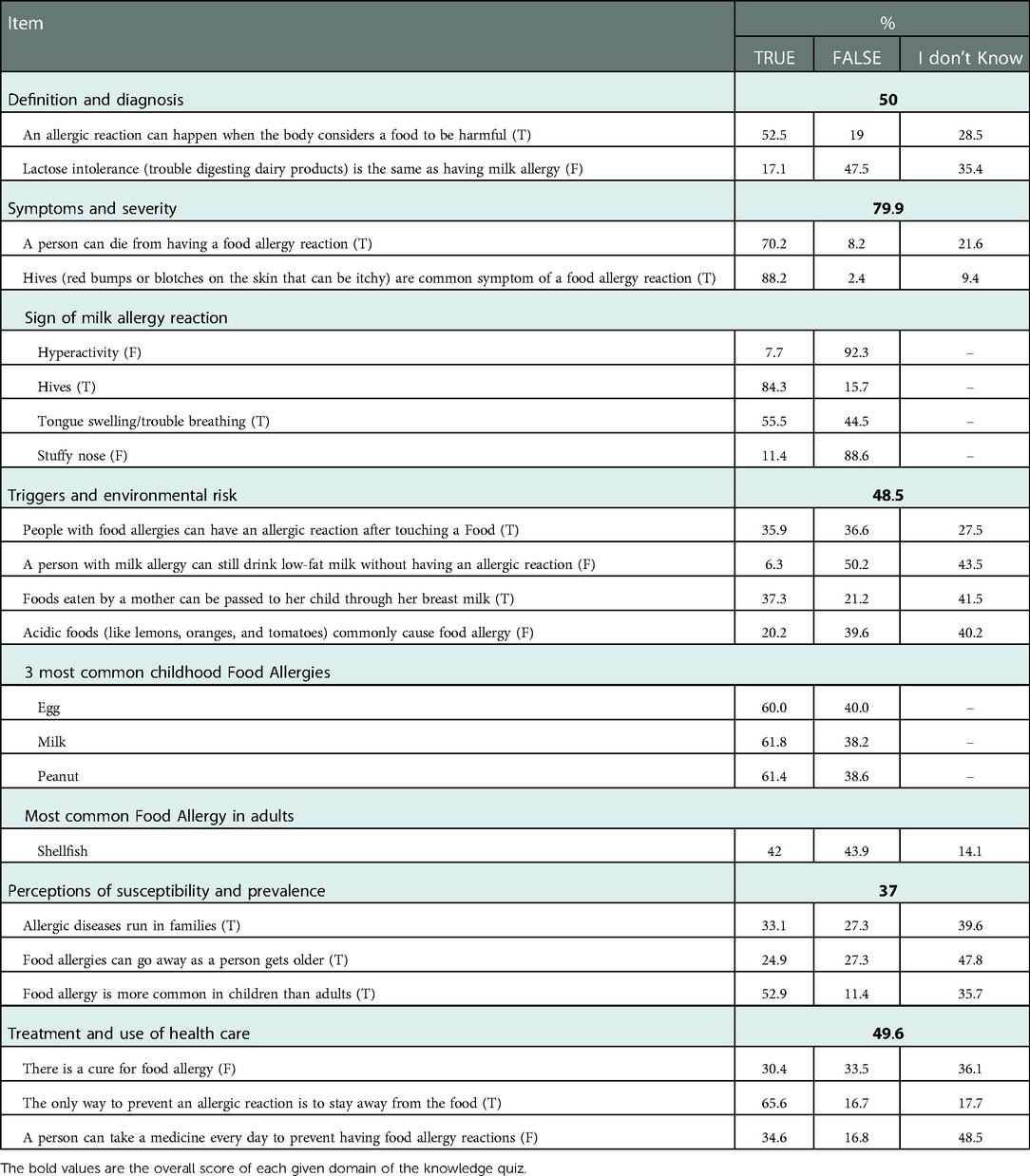
The participants answered 56% of the knowledge-based items correctly. We assessed their knowledge of food allergy in 5 major domains: (1) definition and diagnosis, (2) symptoms and severity, (3) triggers and environmental risks, (4) susceptibility and prevalence, and (5) treatment and use of health care. The knowledge of the participants was highest in the symptoms and severity domain (79.9%), while it was weakest in the susceptibility and prevalence domain (37%). Table 2 shows the knowledge score for each domain and its related items. For the definition and diagnosis, even though about half of the participants knew the definition of food allergy, only a small proportion of them (17.1%) could distinguish between food allergy and food intolerance. With regards to symptoms and severity, more than two thirds of the participants (70.2%) knew that food allergy could be fatal. The majority of the participants were aware of all the common symptoms of food allergy except for tongue swelling and trouble breathing (they were not identified by about half the participants). In the triggers and environmental risk domain, only a small proportion of the participants (35.9%) knew that touching an allergenic food may trigger food allergy and that breast feeding might pass allergenic food, consumed by the mother, into children (37.3%). A small proportion of the participants (20.2%) knew that acidic foods (ex: lemons, oranges) do not trigger food allergy. A large proportion of the participants (≥60%) indicated that egg, peanut, or milk is among the 3 most common food allergens in children. On the other hand, less than half of them considered shellfish as the most common food allergen in adults. For the susceptibility and prevalence, a minor proportion of the participants (33.1%) knew that food allergy could be heritable, and that it can go away by age (24.9%). In addition, only half of the participants knew that food allergy is more common in children. Regarding the treatment and use of healthcare, only one third of the participants knew that food allergy is not curable. However, the majority of them (65.6%) were aware that the only way to prevent allergic reactions is to avoid allergenic food.
The influence of demographical factors on the knowledge of food allergy
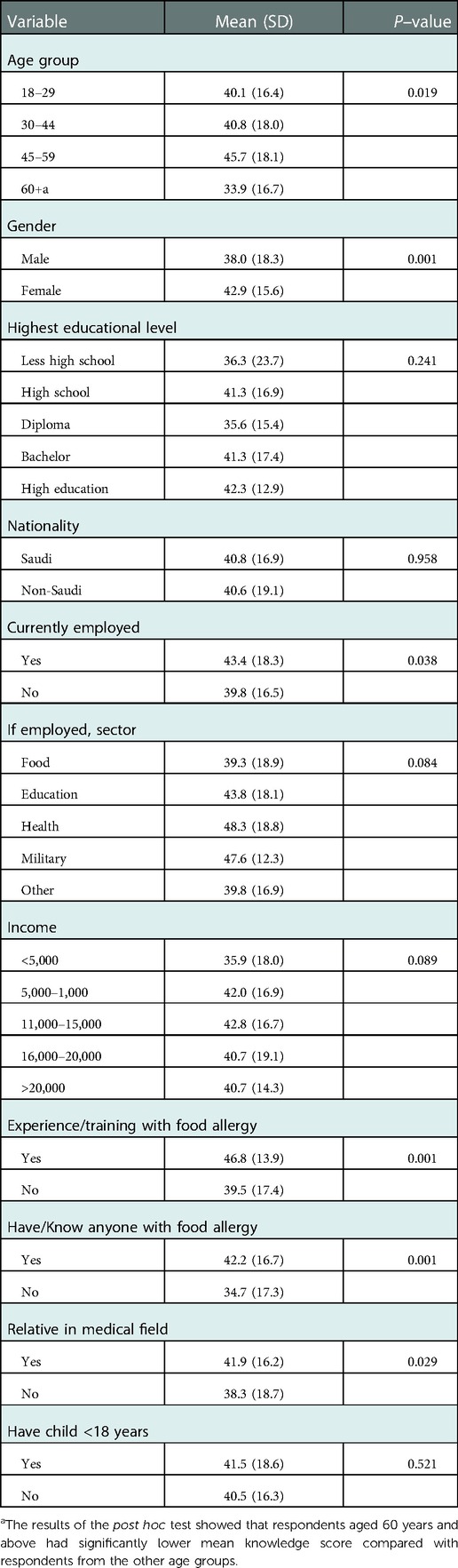
Table 3 shows how demographical factors influenced food allergy knowledge among the participants. The data suggest that (1) females, (2) those who were employed, (3) people with a prior experience/training with food allergy through job or work, (4) those with food allergy acquaintance (i.e., have food allergy or know someone with the condition), and (5) those who have relatives working in the medical field had significantly higher food allergy knowledge (P < 0.05). In addition, we found that age has a statistically significant influence on the knowledge score of the respondents (F-ratio = 3.335, P = 0.019). The results of the post hoc test showed that individuals who are 60 years old and above have significantly lower knowledge scores compared with individuals from the other age groups. Regarding the employment sector, individuals who were employed in the health sector had the highest mean knowledge score (M = 48.3, SD = 18.8), yet this finding was not statistically significant (F-ratio = 0.09, P = 0.084). Moreover, the influence of some factors, such as educational level, Income, and having school-aged children did not reach a statistical significance (P < 0.05).
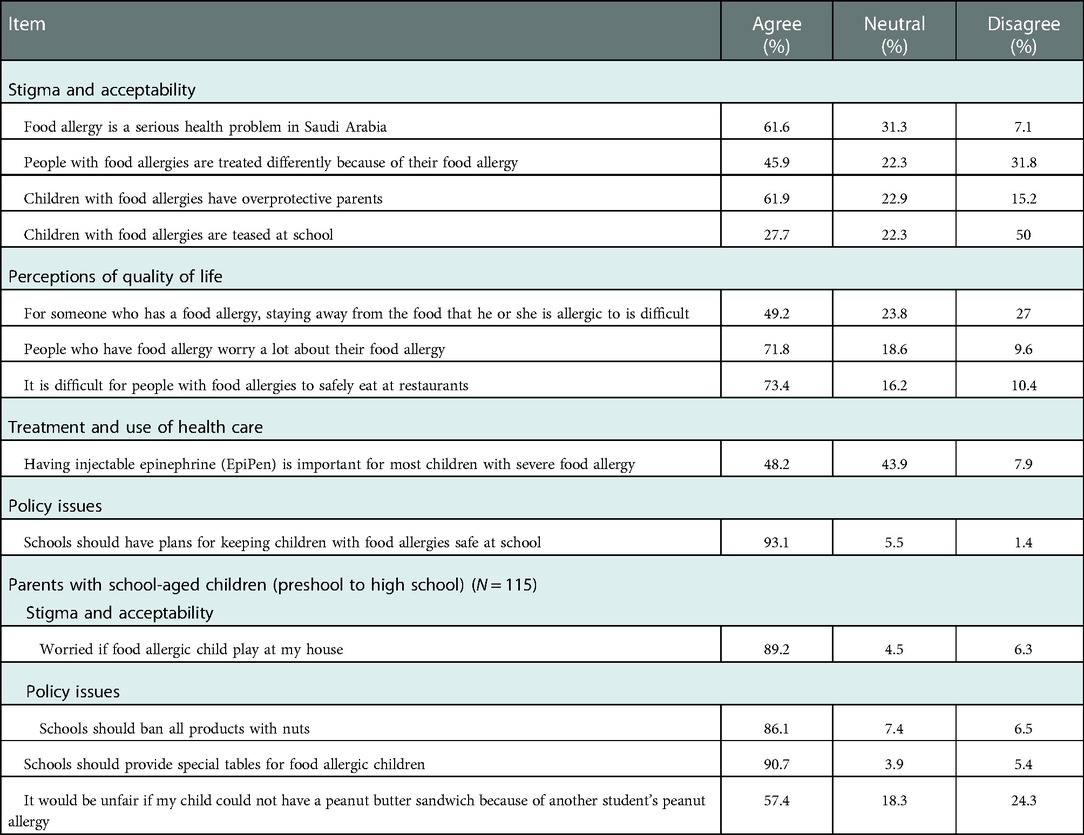
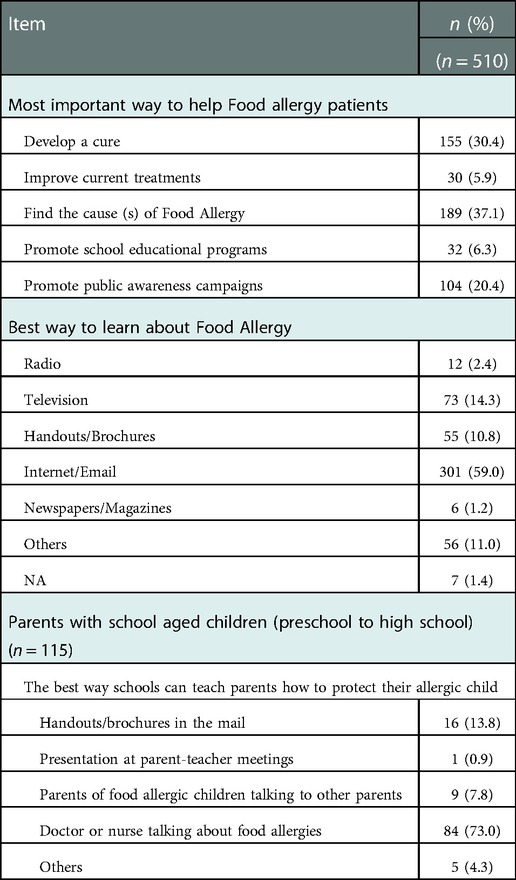
Food allergy attitudes and beliefs
We assessed the attitudes of the participants towards (1) the stigma associated with food allergy, (2) the quality of life of allergic patients, (3) current means to treat and manage the condition, (4) policy issues related to the condition. Table 4 shows each one of these domains along with its related items. With regards to stigma and acceptability, even though about two thirds of the participants thought that food allergy is a serious health problem in Saudi Arabia, a small proportion of them agreed that food allergy causes stigma for allergic patients. For instance, only 27.7% of the participants agreed that children with food allergy are bullied at school due to their allergy. In addition, less than half of the respondents (45.9%) agreed that allergic patients are treated differently due to their allergy. For the effect of food allergy on quality of life, most of the participants thought that food allergy has a negative impact on the quality of life of allergic patients. For example, a large proportion of the respondents (73.4%) agreed that allergic patients cannot eat safely at restaurants. Moreover, 71.8% agreed that allergic patients worry a lot about their food allergy. Regarding the treatment and use of health care, less than half of the participants (48.2%) agreed that epinephrine injections are important for the management of severe allergic reactions. For policy Issues, almost all the respondents (93.1%) thought that schools must make policies to keep allergic children safe. When parents of school-aged children were asked further questions regarding policy issues, the majority of them agreed on banning products with nuts (86.1%) and on providing special tables for allergic children at schools (90.1%). Additionally, the participants indicated that finding the cause of food allergy is the most effective way to help allergic patients (Table 5). Furthermore, they mostly preferred to learn about food allergy through internet and/or email (59.0%). Parents of school-aged children chose lectures given by health care providers as the most effective way to learn about food allergy at schools.
Discussion
In this study, we assessed food allergy knowledge in 5 areas: (1) definition and diagnosis, (2) symptoms and severity, (3) triggers and environmental risks, (4) susceptibility and prevalence, and (5) treatment and use of health care. We found that the participants' knowledge varied between these areas, with symptoms and severity being the area of strongest knowledge (79.9% of its related items were answered correctly), and susceptibility and prevalence being the area of weakest knowledge (37% of related items answered correctly). In general, the participants were unaware of the absence of cure to food allergy, the role of age in the remission of food allergy, the heritability of the condition, the difference between food allergy and intolerance, the possibility to trigger food allergy by touch, and the transmission of food allergens through breast feeding. Regarding the attitudes, most of the respondents agreed that food allergy negatively impacts the quality of life of allergic patients, and that schools should make policies to protect allergic children. Although nearly 62% of the respondents agreed that food allergy is a serious health problem in Saudi Arabia, they downplayed the stigma associated with this condition. Furthermore, we found that gender, age, prior training with food allergy, food allergy acquaintance (i.e., have food allergy or know someone with the condition), having relatives working in the medical field, and employment status influenced knowledge of food allergy significantly compared with employment sector, educational level, income, and having a school-aged child whose influence did not reach a statistical significance.
Knowledge of food allergy
Research has shown that people tend to over-report food allergy among themselves because its clinical presentation is similar to some other food related conditions (ex: intolerance, oral allergy syndrome) (3, 4, 15, 16). For example, Gupta et al. found that the prevalence of food allergy using self or parents reporting is 19% and 11.4% among adults and children respectively. However, after further evaluation, the researchers indicated that the convincing food allergy cases are 10.8% and 7.6% for adults and children, respectively (3, 4). Similarly, our data suggest that the participants overestimated food allergy among themselves. Even though 80% of the participants reported food allergy acquaintance (i.e., either have the condition or know someone with it), about 50% of them did not know the difference between milk allergy and lactose intolerance. Overestimation of food allergy might lead to unnecessary avoidance of food, which negatively impacts the quality of life of these individuals. All these findings suggest that access to health care providers is necessary to provide an appropriate diagnosis to patients and to educate them about the difference between food allergy and other forms of adverse food reactions, which could prevent unnecessary avoidance of food for those who do not have food allergy.
Most of the participants (≥60%) thought that milk, peanut, or egg is one of most common childhood food allergens, while 42% considered shellfish as the most common adult food allergen. These allergens, except for egg, are the most common in western countries (3, 4, 10). However, the aforementioned food allergens are not necesserly the most common in other countries because the variation in diets affects how common an allergen is (17). Additionally, because data from the available local studies about common food allergens vary, we could not know whether or not these allergens are the most common locally. For example, Althumiri and colleagues found that the most common food allergens among adults were egg (3.7%), shellfish (3.1%), and peanut (3.0%). On the other hand, milk, egg white, and wheat were reported in another study as the 3 most common food allergens (18, 19). Even though shellfish was not reported as the most common food allergen in the aforementioned studies we considered it as the most common allergen in our study because Jeddah is a coastal city, where seafood is more common in diet compared with most of the other regions of the kingdom. Thus, we expected that shellfish is probably more common than all the other allergens including egg and milk. Also, data regarding common food allergens among children are lacking. Therefore, more studies have to be conducted to identify common food allergens locally, which will benefit allergic patients and will help concerned bodies to pay more attention to these allergens in food labeling.
Less than half the participants (48.2%) in our study were aware of the role of epinephrine injections in managing food-induced anaphylaxis. In addition, other local studies have reported similar results (12, 20). These findings are alarming because epinephrine injections are the only available agents to manage food-induced anaphylactic reactions currently. Research has shown that the increase in epinephrine injections use has caused a plateau in mortality rate related to food-induced anaphylaxis (21–28). Further, poor knowledge of epinephrine injections delays the management of anaphylactic reactions causing an increase in the risk of mortality (25, 26, 29, 30). Sampson et al. found that fatal anaphylactic reactions were associated with delayed use of epinephrine injections for at least 30 min after the onset of anaphylaxis (31). Thus, education campaigns have to be established to increase the awareness of these injections in the management of food-induced anaphylaxis.
Eating food prepared outside home is part of the modern lifestyle that many people follow nowadays (32). Consuming food prepared outside home might increase the risk of having allergic reactions for individuals with food allergy. Pumphrey et al. indicated that 76% of fatal anaphylactic reactions happened upon consuming food outside home (33). Our data suggest that participant's knowledge of triggers and environmental risks of food allergy was low (48.5%) compared with the subjects of a similar study conducted in the US (64.7%) (10). Only about 36% of the respondents knew that touching an allergenic food might trigger food allergy. Nearly half the participants (50.2%) only, knew that low fat milk triggers allergy for individuals with milk allergy. Poor knowledge of food allergy triggers increases the possibility of getting anaphylactic reactions while eating outside home.
Attitudes towards food allergy
The majority of the participants in our study agreed that food allergy has a negative impact on the quality of life of allergic patients. Nearly 72% agreed that allergic patients are anxious due to their food allergy. Furthermore, 73.4% of the respondents agreed that eating safely at restaurants is difficult for allergic patients. Similarly, other studies indicated that food allergy is costly, and it negatively impacts the quality of life of allergic patients. Regarding the economic burden, Gupta et al. estimated the overall costs on families of allergic children at $20.5 billion annually. Further, they indicated that a large proportion of the money is spent on allergen-free diet (34). Regarding quality of life, Warren et al. found that the constant vigilance due to continuous food allergen avoidance is a major source of stress for allergic patients and their families (35, 36).
Regarding policy issues, the vast majority of respondents (93.1%) agreed that schools need to establish better policies to keep allergic children safe. Additionally, participants with school-aged children further agreed on the implementation of specific policies on schools to protect allergic children. Schools are among the most common sites where anaphylactic reactions occur. It was reported that nearly 18% of children with food allergy had at least 1 allergic reaction at school within 2 years (37). These findings might explain why the majority of participants in our study agreed on establishing policies concerning food allergy at schools.
The influence of demographical factors on knowledge of food allergy
The data show that having a prior experience with food allergy, food allergy acquaintance, and having a relative in the medical field influenced knowledge score significantly (P < 0.05). Likewise, a nationwide study conducted in the US found that the influence of prior food allergy training and food allergy acquaintance on knowledge is statistically significant (10). These findings suggest that targeted educational interventions might have a significant effect in eliminating the knowledge gap among the general population.
Moreover, participants who were 60 years old or more had significantly less knowledge compared with younger participants. We attribute this finding to the high illiteracy rate (60%) among the Saudi population in 1970. In addition, while today's illiteracy rate is only 5.6%, it is believed that the elderly constitutes a majority of that percentage (38).
Furthermore, the influence of educational level on knowledge, surprisingly, was not statistically significant. We attribute this finding to the small sample size included in our study.
Limitations and future direction
The present study does have some limitations. One of them is limiting the survey distribution to the population of Jeddah, in which case the results from this study cannot be generalized to the whole population of Saudi Arabia. The other limitation is the use of convenient sampling technique in distributing the survey, which could introduce sampling bias. This might affect the representativeness of our sample and, therefore, limit our ability to generalize the results to the entire population of Jeddah. However, due to the scarcity of data regarding food allergy in Saudi Arabia, the present study might be considered as an initial assessment that could help other researchers and experts to start their own investigations regarding food allergy in Saudi Arabia. Therefore, future studies on a nationwide level and with an appropriate sampling technique are recommended.
Conclusion
In conclusion, our findings demonstrate that the knowledge of food allergy among the members of Jeddah population varied, with strengths and weaknesses identified across different areas. Participants were aware of the severity of food allergy and of its signs and symptoms. However, increased knowledge is required in areas related to the management, the role of age in the remission of food allergy, the heritability of the condition, the difference between food allergy and intolerance, the possibility to trigger food allergy by touch, and the transmission of food allergens through breast feeding. We found that prior training in food allergy, food allergy acquaintance, and having connections with health care workers are associated with significantly higher knowledge of food allergy, which indicates that targeted educational interventions might have a significant effect in eliminating the knowledge gap among the general population.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the King Abdullah International Medical Research Center (KAIMRC) Institutional review board. (approval No: JED-21-427780-49687). The patients/participants provided their written informed consent to participate in this study.
Author contributions
All the listed authors have made a substantial contribution to this work, and approved it for publication.
Acknowledgments
We would like to thank Alaa Althubaity, and Faisal Zaidi for their support in the initial steps of the project. Also, we thank the members of the research unit at King Saud bin Abdulaziz University for Health Sciences for their contribution and support. We would like to acknowledge Wejdan Alnahdi for the proofreading of the translated survey.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/falgy.2022.1002694/full#supplementary-material.
References
1. Boyce JA, Assa’a A, Burks AW, Jones SM, Sampson HA, Wood RA, et al. Guidelines for the diagnosis and management of food allergy in the United States: summary of the NIAID-Sponsored Expert Panel Report. Nutrition. (2011) 27(2):253–67. doi: 10.1016/j.nut.2010.12.001
2. Osborne NJ, Koplin JJ, Martin PE, Gurrin LC, Lowe AJ, Matheson MC, et al. Prevalence of challenge-proven IgE-mediated food allergy using population-based sampling and predetermined challenge criteria in infants. J Allergy Clin Immunol. (2011) 127(3):668–76.e1-2. doi: 10.1016/j.jaci.2011.01.039
3. Gupta RS, Warren CM, Smith BM, Blumenstock JA, Jiang J, Davis MM, et al. The public health impact of parent-reported childhood food allergies in the United States. Pediatrics. (2018) 142(6):e20181235. doi: 10.1542/peds.2018-1235
4. Gupta RS, Warren CM, Smith BM, Jiang J, Blumenstock JA, Davis MM, et al. Prevalence and severity of food allergies among US adults. JAMA Netw Open. (2019) 2(1):e185630. doi: 10.1001/jamanetworkopen.2018.5630
5. Wood RA, Camargo CA Jr, Lieberman P, Sampson HA, Schwartz LB, Zitt M, et al. Anaphylaxis in America: the prevalence and characteristics of anaphylaxis in the United States. J Allergy Clin Immunol. (2014) 133(2):461–7. doi: 10.1016/j.jaci.2013.08.016
6. Umasunthar T, Leonardi-Bee J, Turner PJ, Hodes M, Gore C, Warner JO, et al. Incidence of food anaphylaxis in people with food allergy: a systematic review and meta-analysis. Clin Exp Allergy. (2015) 45(11):1621–36. doi: 10.1111/cea.12477
7. Umasunthar T, Leonardi-Bee J, Hodes M, Turner PJ, Gore C, Habibi P, et al. Incidence of fatal food anaphylaxis in people with food allergy: a systematic review and meta-analysis. Clin Exp Allergy. (2013) 43(12):1333–41. doi: 10.1111/cea.12211
8. Turner PJ, Jerschow E, Umasunthar T, Lin R, Campbell DE, Boyle RJ. Fatal anaphylaxis: mortality rate and risk factors. J Allergy Clin Immunol Pract. (2017) 5(5):1169–78. doi: 10.1016/j.jaip.2017.06.031
9. Pouessel G, Turner PJ, Worm M, Cardona V, Deschildre A, Beaudouin E, et al. Food-induced fatal anaphylaxis: from epidemiological data to general prevention strategies. Clin Exp Allergy. (2018) 48(12):1584–93. doi: 10.1111/cea.13287
10. Gupta RS, Kim JS, Springston EE, Smith B, Pongracic JA, Wang X, et al. Food allergy knowledge, attitudes, and beliefs in the United States. Ann Allergy Asthma Immunol. (2009) 103(1):43–50. doi: 10.1016/S1081-1206(10)60142-1
11. Alotaibi N, Habib L, Alyamani W, Borah R, Alquwayz R, Bin Nashar B. Food allergy awareness among parents of food allergic child in Saudi Arabia. J Biochem Tech. (2020) 11(4):110–18. doi: 10.51847/MGYOG7GV2E
12. Gohal G. Food allergy knowledge and attitudes among school teachers in jazan, Saudi Arabia. Open Allergy J. (2018) 9:1–7. doi: 10.2174/1874838401809010001
13. General Authority for Statistics. Detailed results for Makkah (general population and housing census 2010–1431) (2010). Available from: https://www.stats.gov.sa/sites/default/files/en-makkah-pulation-by-gender-govnernorate-nationality_0.pdf [Accesssed December 25, 2021].
14. Gupta RS, Kim JS, Springston EE, Pongracic JA, Wang X, Holl J. Development of the Chicago food allergy research surveys: assessing knowledge, attitudes, and beliefs of parents, physicians, and the general public. BMC Health Serv Res. (2009) 9:142. doi: 10.1186/1472-6963-9-142
15. Bangash SA, Bahna SL. Pediatric food allergy update. Curr Allergy Asthma Rep. (2005) 5(6):437–44. doi: 10.1007/s11882-005-0023-y
16. Di Costanzo M, Biasucci G, Maddalena Y, Di Scala C, De Caro C, Calignano A, et al. Lactose intolerance in pediatric patients and common misunderstandings about cow’s milk allergy. Pediatr Ann. (2021) 50(4):e178–85. doi: 10.3928/1938235920210312-01
17. Loh W, Tang MLK. The epidemiology of food allergy in the global context. Int J Environ Res Public Health. (2018) 15(9):2043. doi: 10.3390/ijerph15092043
18. Althumiri NA, Basyouni MH, AlMousa N, AlJuwaysim MF, BinDhim NF, Alqahtani SA. Prevalence of self-reported food allergies and their association with other health conditions among adults in Saudi Arabia. Int J Environ Res Public Health. (2021) 18(1):347. doi: 10.3390/ijerph18010347
19. Al Mesned RK, Shakoor Z, Ben Musibeeh N, Anazi S, Al Hassan G, Al Yahya M. Screening for food specific IgE antibodies among Saudi patients with clinical suspicion of food allergy. 7th International conference on allergy, asthma and clinical immunology; 2016 14–15 September; Amsterdam, Netherland (2016) p.34. doi: 10.4172/2155-6121.C1.002
20. Gomaa NI, Abdullah TI, Alharthi WM, Altowairqi AT, Binbaz SS, Alamri NM. Knowledge and awareness about food allergy among mothers with allergic children in taif city, Saudi Arabia. IJMDC. (2020) 4(1):49–53. doi: 10.24911/IJMDC.51-1569571928
21. Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. (2011) 128(1):e9–e17. doi: 10.1542/peds.2011-0204
22. Turner PJ, Gowland MH, Sharma V, Ierodiakonou D, Harper N, Garcez T, et al. Increase in anaphylaxis-related hospitalizations but no increase in fatalities: an analysis of United Kingdom national anaphylaxis data, 1992–2012. J Allergy Clin Immunol. (2015) 135(4):956–63.e1. doi: 10.1016/j.jaci.2014.10.021
23. Ma L, Danoff TM, Borish L. Case fatality and population mortality associated with anaphylaxis in the United States. J Allergy Clin Immunol. (2014) 133(4):1075–83. doi: 10.1016/j.jaci.2013.10.029
24. Dyer AA, Lau CH, Smith TL, Smith BM, Gupta RS. Pediatric emergency department visits and hospitalizations due to food-induced anaphylaxis in Illinois. Ann Allergy Asthma Immunol. (2015) 115(1):56–62. doi: 10.1016/j.anai.2015.05.006
25. Xu YS, Kastner M, Harada L, Xu A, Salter J, Waserman S. Anaphylaxis-related deaths in Ontario: a retrospective review of cases from 1986 to 2011. Allergy Asthma Clin Immunol. (2014) 10(1):38. doi: 10.1186/1710-1492-10-38
26. Mullins RJ, Wainstein BK, Barnes EH, Liew WK, Campbell DE. Increases in anaphylaxis fatalities in Australia from 1997 to 2013. Clin Exp Allergy. (2016) 46(8):1099–110. doi: 10.1111/cea.12748
27. Jerschow E, Lin RY, Scaperotti MM, McGinn AP. Fatal anaphylaxis in the United States, 1999–2010: temporal patterns and demographic associations. J Allergy Clin Immunol. (2014) 134(6):1318–28.e7. doi: 10.1016/j.jaci.2014.08.018
28. Clark S, Espinola J, Rudders SA, Banerji A, Camargo CA Jr. Frequency of US emergency department visits for food-related acute allergic reactions. J Allergy Clin Immunol. (2011) 127(3):682–3. doi: 10.1016/j.jaci.2010.10.040
29. Pumphrey RS, Gowland MH. Further fatal allergic reactions to food in the United Kingdom, 1999–2006. J Allergy Clin Immunol. (2007) 119(4):1018–9. doi: 10.1016/j.jaci.2007.01.021
30. Bock SA, Muñoz-Furlong A, Sampson HA. Further fatalities caused by anaphylactic reactions to food, 2001–2006. J Allergy Clin Immunol. (2007) 119(4):1016–8. doi: 10.1016/j.jaci.2006.12.622
31. Sampson HA, Mendelson L, Rosen JP. Fatal and near-fatal anaphylactic reactions to food in children and adolescents. N Engl J Med. (1992) 327(6):380–4. doi: 10.1056/NEJM199208063270603
32. Moneret-Vautrin DA, Kanny G. Update on threshold doses of food allergens: implications for patients and the food industry. Curr Opin Allergy Clin Immunol. (2004) 4(3):215–9. doi: 10.1097/00130832-200406000-00014
33. Pumphrey RS. Lessons for management of anaphylaxis from a study of fatal reactions. Clin Exp Allergy. (2000) 30(8):1144–50. doi: 10.1046/j.1365-2222.2000.00864.x
34. Gupta R, Holdford D, Bilaver L, Dyer A, Holl JL, Meltzer D. The economic impact of childhood food allergy in the United States. JAMA Pediatr. (2013) 167(11):1026–31. doi: 10.1001/jamapediatrics.2013.2376
35. Warren CM, Otto AK, Walkner MM, Gupta RS. Quality of life among food allergic patients and their caregivers. Curr Allergy Asthma Rep. (2016) 16(5):38. doi: 10.1007/s11882-016-0614-9
36. Walkner M, Warren C, Gupta RS. Quality of life in food allergy patients and their families. Pediatr Clin North Am. (2015) 62(6):1453–61. doi: 10.1016/j.pcl.2015.07.003
37. Nowak-Wegrzyn A, Conover-Walker MK, Wood RA. Food-allergic reactions in schools and preschools. Arch Pediatr Adolesc Med. (2001) 155(7):790–5. doi: 10.1001/archpedi.155.7.790
38. Alsalem A. Saudi Arabia approaching zero in illiteracy after 60 percent. Sabq (2020). Available from: https://sabq.org/pNyGxV.
Keywords: knowledge, attitudes, food allergy, igE-mediated food allergy, food-induced anaphylaxis, food intolerance, general public, Jeddah - Saudi Arabia
Citation: Takrouni AA, Omer I, Alasmari F, Islamuldeen S, Ghazzawi AY, Zahrani MI, Ahmed ME and Abushouk A (2022) Knowledge gaps in food allergy among the general public in Jeddah, Saudi Arabia: Insights based on the Chicago food allergy research survey. Front. Allergy 3:1002694. doi: 10.3389/falgy.2022.1002694
Received: 25 July 2022; Accepted: 2 December 2022;
Published: 23 December 2022.
Edited by:
Berber Vlieg-Boerstra, Onze Lieve Vrouwe Gasthuis (OLVG), NetherlandsReviewed by:
Audrey DunnGalvin, University College Cork, IrelandJohanna Smeekens, University of North Carolina at Chapel Hill, United States
Sandra Andorf, Cincinnati Children’s Hospital Medical Center, United States
© 2022 Takrouni, Omer, Alasmari, Islamuldeen, Ghazzawi, Zahrani, Ahmed and AbuShouk. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amir AbuShouk c2hvdWthQGtzYXUtaHMuZWR1LnNh
Specialty Section: This article was submitted to Food Allergy, a section of the journal Frontiers in Allergy
 Abdulrahman Ahmad Takrouni
Abdulrahman Ahmad Takrouni Ibrahim Omer
Ibrahim Omer Faisal Alasmari1,2
Faisal Alasmari1,2 Mohamed Eldigire Ahmed
Mohamed Eldigire Ahmed Amir Abushouk
Amir Abushouk