
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Allergy , 24 September 2021
Sec. Food Allergy
Volume 2 - 2021 | https://doi.org/10.3389/falgy.2021.711945
This article is part of the Research Topic Food Allergy: Why Good Nutrition Matters Throughout the Life Course View all 4 articles
The prevalence of food allergies (FA) is increasing worldwide. Generally, the onset of allergies, including FA, begins in early childhood and may persist and/or develop through the life-course. Even though epidemiological studies have focused mainly on children, allergies can also occur for the first-time during adulthood. Within the prolongation of life, it is expected that allergies will be encountered more often even in older people. Recent findings suggest that an early exposure to diverse food antigens may promote the development of immune tolerance. Accordingly, diet diversity during the first year of life or even earlier may have a positive impact on the prevention of allergies. The anti-inflammatory properties of some dietary nutrients may positively contribute to a tolerogenic immune environment too. Diet diversity is associated with a more favorable microbiome, and increasing evidence suggests a promising role of gut microbiota manipulation in inducing immune tolerance. Unjustified avoidance of allergenic foods may expose to intakes of some nutrients below recommended levels through the life-course, even more in cases of self-diagnosis and treatment of presumed forms of food intolerance. Nutritional strategies including the early exposure to a variety of food antigens are a promising area of research for preventive purposes through the life-course possibly extending positive outcomes to older stages. The aim of this paper is to highlight the role of diet diversity in preventing the development of FA starting in early life, as well as to provide an overview of the main strategies to prevent related nutritional issues throughout the life-course.
Over the last decades, the presence of allergies such as food allergies (FA), asthma, atopic dermatitis (AD) and eczema has become a prevalent issue for healthcare systems, especially in Western countries (1, 2). Meta-analyses estimated an increase in prevalence of FA even in adults, ranging from 3.5 to 35%. However, literature about FA in older people is still scarce and based on self-reported symptoms (3–6). The reasons for the increase in allergic sensitization, allergic reactions, as well as allergy severity, is multifactorial with environmental, epigenetic and genetic factors all playing a role in the origin and development of the disease (7). As a response, healthcare systems are now focused on a better understanding of the various modifiable eliciting factors of allergic diseases, which may then serve as targets for allergies primary prevention (8). Modifications in eating habits and nutrient intakes, which have accompanied the rise of modern societies, are well-recognized influencing factors on the growing prevalence of non-communicable diseases, including allergies. Indeed, nutrition may represent a key factor contributing to health throughout the life-course, as it is a fundamental cofactor for the development and maintenance of body composition and body functions (9, 10). In the case of allergies, many nutritional factors and dietary interventions have been studied for their function in promoting immune system maturation and immune tolerance to allergens. Among all, vitamins (A, C, D, and E), omega-3 long chain polyunsaturated fatty acids (n-3 LC-PUFA), copper, zinc, selenium, prebiotics, and probiotics have all sparked interest for their immunomodulatory functions, potentially promoting allergy prevention (11). Most recently, the concept that diet diversity (i.e., the variety of food being eaten) may itself influence allergic outcomes has also been proposed (12). Accordingly, the promotion of a more diverse diet may exert its influence on allergic outcome either directly, through the promotion of a healthy gut microbiome, and indirectly, with the introduction of potentially immunomodulatory nutrients (12, 13).
In infants and children, a preeminent role among allergic diseases is acted by food allergy (FA) which can occur as early as during the first year of life. Historically, this has led to the hypothesis that the exposition of potentially highly allergenic foods, such as hen's egg, peanuts and cow's milk should be avoided until the end of the first year of life. The basis of such recommendation was the belief that a certain degree of mucosal immunologic immaturity, present in infants, could negatively influence the challenge of the local immune cells with food antigens, ultimately resulting in increase of food allergen sensitization (14). However, this “late introduction” strategy has been weakened by the epidemiological evidence that tolerance to food allergens may more favorably be modulated by an early exposure to food allergens, even at 4–6 months of age. Later exposure, outside this “critical early window” may otherwise lead to oral tolerance failure, rising the risk of FA, coeliac disease, as well as autoimmunity phenomena (15). Accordingly, new guidelines for FA prevention have been issued proposing an earlier introduction of foods with proteins carrying a higher allergenic potential during complementary feeding as a better option to prevent and/or contrast the development of FA in the youngest population. Newer recommendations advise against delaying the introduction of solid foods after 4–6 months of age, while contextually discouraging early exposure to food allergens before 4 months of age (16, 17). Notably, the new recommendations are valid for all, regardless of the a priori hereditary predisposition of developing allergic reactions, as for the case of children with atopic dermatitis (AD). Indeed, the European Academy of Allergy and Clinical Immunology (EAACI) specifically recommends the “introduction of complementary foods after the age of 4 months for all children irrespective of atopic heredity” (16). The effectiveness of this early introduction strategy has yet to be clarified, with a recent review arguing that a positive effect in reducing FA occurrence has only been shown for early introduction of peanuts in infant diets. The potential positive effect of an early introduction of allergenic foods other than peanuts should be further investigated with randomized controlled trials (RCT) (1). The involvement of primary care pediatric centers and family pediatricians in RCT studies investigating more systematically early food allergens exposure and development of FA would be of great value also to understand the mechanisms responsible for FA. Whilst an earlier introduction of allergenic proteins has still to be challenged with most “at risk” foods, the delay in their introduction seems to be definitely out of any positive advantage (14).
An interesting insight on the potential mechanism underlying early development of FA or, on opposite, food tolerance has been provided by the recent “Dual allergen exposure hypothesis,” which proposes that the immune system response to food allergens may differ depending on the allergens first site of exposure during the first year of life (intestinal mucosal = food tolerance; percutaneous exposure = allergic sensitization) (1). The hypothesis is based on the observation that infants with skin problem, like as AD or eczema, may experience early percutaneous exposure to food antigens. Such early exposure, bypassing intestinal tolerance, may elicit a T helper type 2 (Th2) dominant response, leading to development of allergic sensitization. Consequently, avoiding oral introduction of food allergens, while still having environmental exposure to them, might elicit the occurrence of FA through transcutaneous sensitization, rather than prevent it (1, 18). According to this hypothesis, an earlier introduction of allergenic proteins should be supported to prevent a first environmental incidental exposure through the skin.
Besides conditions genetically predisposing to allergies (as for the case of children with AD) the rise of FA in recent years has also been linked to environmental factors, which may affect food tolerance. Specifically, unhealthy lifestyles and diet may negatively influence the intestinal microbiome and immune responses, as well as lead to nutritional imbalances concerning vitamins, antioxidants, fibers and fatty acids dietary intakes (19). The resident gastrointestinal microbiota has a modulatory role on the human immune system and can potentially influence allergies' occurrence, including FA (20). Indeed, prenatal life and early infancy are crucial for microbiome colonization and immune tolerance promotion. A healthy colonization may positively influence the development and maturation of the immune system and immune tolerance, eventually protecting the individual from allergic reaction, once complementary feeding is introduced (8, 21, 22). On the contrary, an unfavorable gut microbiota composition (i.e., microbial dysbiosis, commensal bacteria disruption, diversity reduction) has been associated with an increased risk of immune system dysregulation and allergies development (1, 23–25). To ameliorate the gut microbiota health in the perspective to prevent/manage some age relate conditions including FA, supplementations with prebiotics (i.e., Bifidobacterium breve M-16V) and probiotics (i.e., Lactobacillus rhamnosus GG) are being considered as promising strategies with potential implications in the prevention/management of FA, despite evidence on efficacy, particularly at long term, is still limited (26).
Food allergies are usually regarded as a pediatric problem. However, it is expected that FA will be encountered more often even in older people given the increase in prevalence seen in the last decades (27). Unfortunately, literature about food allergies in older people (i.e., people aged 60 and older) is very scarce, leading to the impression that food allergies cannot be present and/or arise later in life (28). Nevertheless, FA may both persist in old age as well as they may occur for the first time during the later stages of life (29). Several changes occurring with aging have been suggested to play a role in mediating FA. In particular, the physiological decline in many functions and comorbidities related to aging itself may contribute to mask symptoms of FA (27, 30). To date, immune senescence has been evoked as one of the mechanisms underlying FA in older people. With aging, there is a decline in both innate and adaptive immune responses often associated to a pro-inflammatory profile (i.e., inflamm-aging) (31, 32). Indeed with aging a shift toward a pro-allergenic Th2 profile (27, 33, 34) may take place, at the point that a Th2 profile may not only be characteristic of childhood, but also be present in mid-to-later life (35, 36) therefore influencing the development of FA in older people (28). Even if an oral tolerance established during early life seems to be retained in older life, the ingestion of new dietary proteins may lead to de novo sensitization in older people (27, 28, 37–39). Recently, Gupta et al. (40) reported an estimated prevalence of FA of 8.8% among U.S. adults aged 60 and older, with the 5.5% of them developing FA as adults. Interestingly, they reported that shellfish allergy prevalence is nearly the same among individuals aged 18–29 years (i.e., 2.8 %) and among people aged 60 and older (i.e., 2.6 %), indirectly confirming a high rate of persistence through the life-course of this food allergy. The authors also reported a prevalence of milk allergy of 1.9% in adults aged 60 and above, in line with the other age groups considered. Another contributing factor for FA in older people is represented by the progressive alteration of intestinal permeability (41). Indeed, chronic low-grade inflammation seen with aging can increase the permeability of the tight junctions (42) resulting in a dysregulation of the mechanism of tolerance (27, 43). Additionally, atrophic gastritis commonly seen with aging and determining a decreased digestive ability, may lead to the persistence of undigested proteins developing as potential allergens (44, 45). Atrophic gastritis can also develop from alcohol abuse or chronic ingestion of proton pump inhibitors or antacids, further enhancing gastrointestinal permeability (46–48). In fact, age related modifications in the gut microbiota have been suggested as major contributors in mediating FA in older people (27). In particular, the gut microbiota has repeatedly been evoked as a mediator of a wide variety of age-related changes, ranging from innate immunity and sarcopenia up to cognitive function and, more broadly, frailty in general (49). In addition to unhealthy diets, antibiotic therapies, and prolonged treatments with proton pump-inhibitors, which are frequently (and often improperly) prescribed to older people, and even self-prescribed out of any medical advice, are known to negatively affect gut microbiota composition. Nutritional deficiencies typical of older ages, such as micronutrient deficiencies - including low levels vitamin D, zinc and iron - may play an additional role in sensitization to food allergens in older people (43). These micronutrients modulate immune responses and have antioxidant properties (39). For instance, zinc deficiency results in a reduction of T helper type 1 (Th1) cytokines, with a net shift toward Th2 responses, potentially favoring the occurrence of FA in older people (50, 51). Also vitamin D deficiency may influence the development of allergic reactions. In its active form (i.e., calcitriol), vitamin D has immunomodulatory properties through influencing both innate and adaptive immunity. In fact, calcitriol through T cells and antigen presenting cells promotes tolerance by inhibiting inflammatory processes and promoting the maturation of regulatory T cell subpopulations (52). Finally, iron deficiency is associated to a reduced antibody response, mainly in the IgG4 subclass, that inhibits the activation of effector cells through incorporating allergens before it binds to the IgE (28).
Food allergies and the consequent dietary restriction resulting from the avoidance of allergenic foods may have negative effects on either short- and long-term outcomes. The development of FA in early life may negatively impact growth and more generally body composition. Moreover, an unsupervised dietary restriction has been correlated to presence of eating disorders later in life (i.e., adolescence) (53). Therefore, basic anthropometric and body composition indexes should be measured routinely in allergic subjects, or at least in those subgroups followed up in Centers where these sophisticated resources are available and/or feasible, in order to anticipate possible growth deviations and/or reduce the risk of malnutrition and malnutrition related comorbidities in later life (54, 55). Likewise, bone health should be regularly monitored in children who have a restricted diet, particularly in milk and milk-derived products, due to an allergic sensitization/disease to make sure that peak bone mass is attained and to prevent the consequences of poor bone health (i.e., fractures and skeletal pain) in later life (56). Given that the mainstay of the management of FA is based on the dietary elimination of major food allergens, attention should be paid to the risk of nutritional deficiencies. Inadequate intakes of specific nutrients may also be exacerbated by the anxiety of avoiding even minimal amounts of offending allergens in industry-based food preparations (57). Since a FA developed during childhood may persist also in adult life, this may determine a lifetime cumulative exposure to nutritional deficiencies, negatively affecting the functional reserves of the individual. For instance, older people need more proteins to counteract the age-related muscle decline (58, 59) and the avoidance of allergenic foods which are a major source of proteins (i.e., milk, egg, fish) may contribute to an inadequate protein intake (57). FA may be potentially regarded also as determinants of the so-called “anorexia of aging.” In fact, physiological changes seen with the aging process like as gastrointestinal alterations, which are frequently seen in FA, are well-recognized contributing factors to the anorexia of aging, thus augmenting the risk of malnutrition, frailty and sarcopenia (60, 61). Lastly, it is well-established that the exclusion of individual food categories from the diet may expose to other micronutrient deficiencies (i.e., calcium, selenium, iron, zinc, vitamin D, B vitamins). Ensuring an appropriate dietary quality, as well as adequate intakes of all macro- and micronutrients is therefore of pivotal importance in the management of FA. Indeed, as pointed out just recently by the “EAACI position paper on diet diversity in pregnancy, infancy and childhood,” studies from both developed and developing countries have shown that an increase in diet diversity is linked with an increase in nutrient adequacy (62). Under these premises, the importance of diet diversity may emerge as a novel strategy not only to prevent but also to manage FA throughout the life-course (57).
The term “diet diversity” comprises two possible definitions (1) the variety of food being eaten or, (2) the number of different foods or groups of foods eaten over a reference period of time. Over the last decades, it has been observed that there is a positive association between diet diversity and numerous health outcomes. Most recently the same positive association has been investigated even between diet diversity and the occurrence of allergic diseases, including FA (12). The concept that diet diversity may have a positive influence on FA outcomes mainly derives from the observation that the promotion of diet diversity (and early food antigen introduction) in the first year of life is negatively associated with the occurrence of allergies, including FA. In particular, the relation of FA with diet diversity has been investigated in few recent studies so far. Indeed, regarding this lack of studies investigating the relationship between diet diversity and FA outcome, EAACI experts have claimed that there is a “true deficiency in the literature” (62). A negative association between increased diverse food intake in the first year of life and FA outcomes up to 6 years of age was first reported by Roduit et al. in 2014 (63). In the same year, in a case-control study, Grimshaw et al. observed that, compared to children diagnosed with FA by the age of 2 years, control children had a healthier diet in the first year of life, characterized by a higher introduction of fruit, vegetables, and home-made food (64). Most recently, Venter et al. (65) have examined four different (but internationally recognized) measurements' methods to define diet diversity and found that, regardless of the method applied, FA outcomes over the first 10 years of life were always reduced in children with higher diet diversity scores in the first year of life. Additional information on the importance of diet diversity in the prevention of FA derives from a paper by Nicklaus et al., who reported that increased diversity of cheese consumed at 18 months might have a protective effect on the development of FA (as well as AD) by the age of 6 years (66). An overview of the studies is presented in Table 1. Altogether, the studies here examined may suggest preliminary evidence that diet diversity should be promoted from very young ages, as early as with the beginning of complementary feeding. Diet diversity is also associated with a more favorable gut microbiome, so reinforcing the concept of the promising role of gut microbiota manipulation (either directly or indirectly) in inducing immune tolerance (67). Not only gut microbiome is responsible for the maintenance of the intestinal mucosa integrity, but it also explicates a regulatory action on the immune system. Therefore, diet diversity may promote allergy prevention and food tolerance by favoring the diversity of gut microbiome (12, 68). Diet diversity should be encouraged even after the “critical window” of the first year of life, in which diet diversity is believed to exert the most of its immunomodulatory effects, for the potential ability to modulate the tolerance to food allergens through the gut microbiome and its potential efficacy throughout the life-course. Lastly, diet diversity may additionally promote food tolerance favoring the introduction of immune-modulatory nutrients, such as omega-3 LC-PUFA and fibers, as well as vitamins and other substances with antioxidant properties, that are mostly represented in a diet funded on “diverse” foods (67). Given that a more diverse diet is associated with a healthier diet, regardless of age, the promotion of diet diversity should therefore be supported in both children and adults to prevent FA on one hand, and as much as possible in those subjects with FA still following food restricted diets. Within this perspective, new dieto-therapeutic approaches should be challenged in clinical trials in the forthcoming years, at all ages, through the life span.
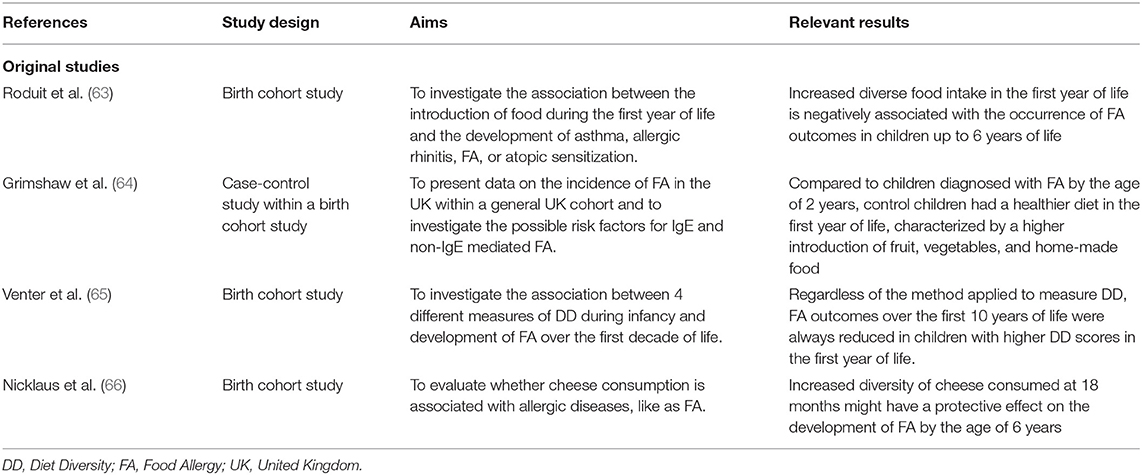
Table 1. Overview of the original studies exploring the effects of diet diversity for the prevention of food allergy.
In the last decades, the rise in allergic diseases, including FA, is becoming a prevalent issue for healthcare systems. Contrary to what is believed, FA are not only an issue mainly related to pediatric ages, as they can also persist or even occur for the first time in adult life. Although the mechanisms involved may differ at the two extremes of life, FA may be more difficult to identify in older people who are characterized by a high clinical complexity with multiple chronic comorbidities and mutually interactive syndromes. Indeed, FA in older life may be observed as a corollary of the aging process which is characterized by mechanisms like as inflamm-aging, immunosenescence and gut microbiota alterations. Diet diversity is emerging as a new strategy to prevent the occurrence of FA in early life with potential implications in later stages of the life too. Additionally, gut microbiota manipulation represents a promising approach in preventing and managing FA despite further evidence is needed.
DA and GS equally contributed to conceptualizing and writing the manuscript. CA and MC edited and revised the manuscript. All authors approved the final version of the manuscript.
This study was supported by a contribution from the Italian Ministry of Health (Istituto di Ricovero e Cura a Carattere Scientifico- IRCCS grant).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling Editor declared a past co-authorship with one of the authors CA.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Comberiati P, Costagliola G, D'Elios S, Peroni D. Prevention of food allergy: the significance of early introduction. Medicina (Kaunas). (2019) 55:323. doi: 10.3390/medicina55070323
2. Campbell DE, Mehr S. Fifty years of allergy: 1965-2015. J Paediatr Child Health. (2015) 51:91–3. doi: 10.1111/jpc.12806
3. Chafen JJS, Newberry SJ, Riedl MA, Bravata DM, Maglione MS, Sundaram VMJ, et al. Diagnosing and managing common food allergies: a systematic review. JAMA. (2010) 303:1848–56. doi: 10.1001/jama.2010.582
4. Rona RJ, Keil T, Summers C, Gislason D, Zuidmeer L, Sodergren E, et al. The prevalence of food allergy: a meta-analysis. J Allergy Clin Immunol. (2007) 120:638–46. doi: 10.1016/j.jaci.2007.05.026
5. Nwaru BI, Hickstein L, Panesar SS, Muraro A, Werfel T, Cardona V, et al. The epidemiology of food allergy in Europe: a systematic review and meta-analysis. Allergy. (2014) 69:62–75. doi: 10.1111/all.12305
6. Laia-Dias I, Lozoya-Ibanez C, Skypala I, Gama JMR, Nurmatov U, Lourenco O, et al. Prevalence and risk factors for food allergy in older people: protocol for a systematic review. BMJ Open. (2019) 9:e029633. doi: 10.1136/bmjopen-2019-029633
7. Hernandez CD, Casanello P, Harris PR, Castro-Rodriguez JA, Iturriaga C, Perez-Mateluna G, et al. Early origins of allergy and asthma (ARIES): study protocol for a prospective prenatal birth cohort in Chile. BMC Pediatr. (2020) 20:164. doi: 10.1186/s12887-020-02077-x
8. Trikamjee T, Comberiati P, D'Auria E, Peroni D, Zuccotti GV. Nutritional factors in the prevention of atopic dermatitis in children. Front Pediatr. (2020) 8:577413. doi: 10.3389/fped.2020.577413
9. Spolidoro GCI, Azzolino D, Shamir R, Cesari M, Agostoni C. Joint effort towards preventing nutritional deficiencies at the extremes of life during COVID-19. Nutrients. (2021) 13:1616. doi: 10.3390/nu13051616
10. Wells JC, Sawaya AL, Wibaek R, Mwangome M, Poullas MS, Yajnik CS, et al. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet. (2020) 395:75–88. doi: 10.1016/S0140-6736(19)32472-9
11. Rueter K, Prescott SL, Palmer DJ. Nutritional approaches for the primary prevention of allergic disease: an update. J Paediatr Child Health. (2015) 51:962–9; quiz 968–9. doi: 10.1111/jpc.12951
12. D'Auria E, Peroni DG, Sartorio MUA, Verduci E, Zuccotti GV, Venter C. The role of diet diversity and diet indices on allergy outcomes. Front Pediatr. (2020) 8:545. doi: 10.3389/fped.2020.00545
13. Mazzocchi A, Venter C, Maslin K, Agostoni C. The role of nutritional aspects in food allergy: prevention and management. Nutrients. (2017) 9:850. doi: 10.3390/nu9080850
14. Ferraro V, Zanconato S, Carraro S. Timing of food introduction and the risk of food allergy. Nutrients. (2019) 11:131. doi: 10.3390/nu11051131
15. Prescott SL, Smith P, Tang M, Palmer DJ, Sinn J, Huntley SJ, et al. The importance of early complementary feeding in the development of oral tolerance: concerns and controversies. Pediatr Allergy Immunol. (2008) 19:375–80. doi: 10.1111/j.1399-3038.2008.00718.x
16. Muraro A, Halken S, Arshad SH, Beyer K, Dubois AE, Du Toit G, et al. EAACI food allergy and anaphylaxis guidelines. Primary prevention of food allergy. Allergy. (2014) 69:590–601. doi: 10.1111/all.12398
17. Halken S, Muraro A, de Silva D, Khaleva E, Angier E, Arasi S, et al. EAACI guideline: preventing the development of food allergy in infants and young children (2020 update). Pediatr Allergy Immunol. (2021) 32:843–58. doi: 10.1111/pai.13496
18. Noti M, Kim BS, Siracusa MC, Rak GD, Kubo M, Moghaddam AE, et al. Exposure to food allergens through inflamed skin promotes intestinal food allergy through the thymic stromal lymphopoietin-basophil axis. J Allergy Clin Immunol. (2014) 133:1390–9, 1399.e1391–6. doi: 10.1016/j.jaci.2014.01.021
19. du Toit G, Tsakok T, Lack S, Lack G. Prevention of food allergy. J Allergy Clin Immunol. (2016) 137:998–1010. doi: 10.1016/j.jaci.2016.02.005
20. Ho H, Bunyavanich S. Role of the microbiome in food allergy. Curr Allergy Asthma Rep. (2018) 18:27. doi: 10.1007/s11882-018-0780-z
21. Peroni DG, Nuzzi G, Trambusti I, Di Cicco ME, Comberiati P. Microbiome composition and its impact on the development of allergic diseases. Front Immunol. (2020) 11:700. doi: 10.3389/fimmu.2020.00700
22. Marsland BJ, Trompette A, Gollwitzer ES. The gut-lung axis in respiratory disease. Ann Am Thorac Soc. (2015) 12(Suppl. 2):S150–156. doi: 10.1513/AnnalsATS.201503-133AW
23. Murk W, Risnes KR, Bracken MB. Prenatal or early-life exposure to antibiotics and risk of childhood asthma: a systematic review. Pediatrics. (2011) 127:1125–38. doi: 10.1542/peds.2010-2092
24. Toscano M, De Grandi R, Peroni DG, Grossi E, Facchin V, Comberiati P, et al. Impact of delivery mode on the colostrum microbiota composition. BMC Microbiol. (2017) 17:205. doi: 10.1186/s12866-017-1109-0
25. Dominguez-Bello MG, Costello EK, Contreras M, Magris M, Hidalgo G, Fierer N, et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc Natl Acad Sci USA. (2010) 107:11971–5. doi: 10.1073/pnas.1002601107
26. De Martinis M, Sirufo MM, Suppa M, Ginaldi L. New perspectives in food allergy. Int J Mol Sci. (2020) 21:474. doi: 10.3390/ijms21041474
27. De Martinis M, Sirufo MM, Viscido A, Ginaldi L. Food allergies and ageing. Int J Mol Sci. (2019) 20:580. doi: 10.3390/ijms20225580
28. Diesner SC, Untersmayr E, Pietschmann P, Jensen-Jarolim E. Food allergy: only a pediatric disease? Gerontology. (2011) 57:28–32. doi: 10.1159/000279756
29. De Martinis M, Sirufo MM, Ginaldi L. Allergy and aging: an old/new emerging health issue. Aging Dis. (2017) 8:162–75. doi: 10.14336/AD.2016.0831
30. Mohrenschlager M, Ring J. Food allergy: an increasing problem for the elderly. Gerontology. (2011) 57:33–6. doi: 10.1159/000316576
31. Ferrucci L, Fabbri E. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat Rev Cardiol. (2018) 15:505–22. doi: 10.1038/s41569-018-0064-2
32. Fulop T, Larbi A, Dupuis G, Le Page A, Frost EH, Cohen AA, et al. Immunosenescence and inflamm-aging as two sides of the same coin: friends or foes? Front Immunol. (2017) 8:1960. doi: 10.3389/fimmu.2017.01960
33. Rink L, Cakman I, Kirchner H. Altered cytokine production in the elderly. Mech Age Dev. (1998) 102:199–209. doi: 10.1016/S0047-6374(97)00153-X
34. Shearer GM. Th1:Th2 changes in aging. Mech Ageing Dev. (1997) 94:1–5. doi: 10.1016/S0047-6374(96)01849-0
35. Alberti S, Cevenini E, Ostan R, Capri M, Salvioli S, Bucci L, et al. Age-dependent modifications of Type 1 and Type 2 cytokines within virgin and memory CD4+ T cells in humans. Mech Ageing Dev. (2006) 127:560–6. doi: 10.1016/j.mad.2006.01.014
36. Di Lorenzo G. A study of age-related IgE pathophysiological changes. Mech Ageing Dev. (2003) 124:445–8. doi: 10.1016/S0047-6374(03)00020-4
37. Caetano de Faria AM, Madsen Ficker S, Speziali E, da Silva Menezes J, Stransky B, Silva Rodrigues V, Monteiro Vaz N. Aging affects oral tolerance induction but not its maintenance in mice. Mech Age Dev. (1998) 102:67–80. doi: 10.1016/S0047-6374(98)00024-4
38. Anto JM, Bousquet J, Akdis M, Auffray C, Keil T, Momas I, et al. Mechanisms of the development of allergy (MeDALL): introducing novel concepts in allergy phenotypes. J Allergy Clin Immunol. (2017) 139:388–99. doi: 10.1016/j.jaci.2016.12.940
39. Cardona V, Guilarte M, Luengo O, Labrador-Horrillo M, Sala-Cunill A, Garriga T. Allergic diseases in the elderly. Clin Transl Allergy. (2011) 1:11. doi: 10.1186/2045-7022-1-11
40. Gupta RS, Warren CM, Smith BM, Jiang J, Blumenstock JA, Davis MM, et al. Prevalence and severity of food allergies among US adults. JAMA Netw Open. (2019) 2:e185630. doi: 10.1001/jamanetworkopen.2018.5630
41. Ventura MT, Scichilone N, Gelardi M, Patella VER. Management of allergic disease in the elderly: key considerations, recommendations and emerging therapies. Expert Rev Clin Immunol. (2015) 11:1219–28. doi: 10.1586/1744666X.2015.1081564
42. Chung HY, Kim DH, Lee EK, Chung KW, Chung S, Lee B, et al. Redefining Chronic inflammation in aging and age-related diseases: proposal of the senoinflammation concept. Aging Dis. (2019) 10:367–82. doi: 10.14336/AD.2018.0324
43. Ventura MT, Casciaro M, Gangemi S, Buquicchio R. Immunosenescence in aging: between immune cells depletion and cytokines up-regulation. Clin Mol Allergy. (2017) 15:21. doi: 10.1186/s12948-017-0077-0
44. Burks W. Current understanding of food allergy. Ann NY Acad Sci. (2002) 964:1–12. doi: 10.1111/j.1749-6632.2002.tb04130.x
45. Untersmayr E, Jensen-Jarolim E. The role of protein digestibility and antacids on food allergy outcomes. J Allergy Clin Immunol. (2008) 121:1301–08; quiz 1309–10. doi: 10.1016/j.jaci.2008.04.025
46. Gonzalez-Reimers E, Santolaria-Fernandez F, Martin-Gonzalez MC, Fernandez-Rodriguez CM, Quintero-Platt G. Alcoholism: a systemic proinflammatory condition. World J Gastroenterol. (2014) 20:14660–71. doi: 10.3748/wjg.v20.i40.14660
47. Untersmayr E, Diesner SC, Bramswig KH, Knittelfelder R, Bakos N, Gundacker C, et al. Characterization of intrinsic and extrinsic risk factors for celery allergy in immunosenescence. Mech Ageing Dev. (2008) 129:120–8. doi: 10.1016/j.mad.2007.10.015
48. González-Quintela A, Gude F, Boquete O, Rey J, Meijide LM, Suarez M, et al. Association of alcohol consumption with total serum immunoglobulin E levels and allergic sensitization in an adult population-based survey. Clin Exp Allergy. (2003) 33:199–205. doi: 10.1046/j.1365-2222.2003.01582.x
49. O'Toole PW, Jeffery IB. Gut microbiota and aging. Science. (2015) 350:1214–5. doi: 10.1126/science.aac8469
51. Haase H, Rink L. The immune system and the impact of zinc during aging. Immun Ageing. (2009) 6:9. doi: 10.1186/1742-4933-6-9
52. Chambers ES, Hawrylowicz CM. The impact of vitamin D on regulatory T cells. Curr Allergy Asthma Rep. (2011) 11:29–36. doi: 10.1007/s11882-010-0161-8
53. Wroblewska B, Szyc AM, Markiewicz LH, Zakrzewska M, Romaszko E. Increased prevalence of eating disorders as a biopsychosocial implication of food allergy. PLoS ONE. (2018) 13:e0198607. doi: 10.1371/journal.pone.0198607
54. Mehta H, Ramesh M, Feuille E, Groetch M, Wang J. Growth comparison in children with and without food allergies in 2 different demographic populations. J Pediatr. (2014) 165:842–8. doi: 10.1016/j.jpeds.2014.06.003
55. Christie L, Hine RJ, Parker JG, Burks W. Food allergies in children affect nutrient intake and growth. J Am Diet Assoc. (2002) 102:1648–51. doi: 10.1016/S0002-8223(02)90351-2
56. Doulgeraki AE, Manousakis EM, Papadopoulos NG. Bone health assessment of food allergic children on restrictive diets: a practical guide. J Pediatr Endocrinol Metab. (2017) 30:133–9. doi: 10.1515/jpem-2016-0162
57. Skypala IJ, McKenzie R. Nutritional Issues in Food Allergy. Clin Rev Allergy Immunol. (2019) 57:166–78. doi: 10.1007/s12016-018-8688-x
58. Bauer J, Biolo G, Cederholm T, Cesari M, Cruz-Jentoft AJ, Morley JE, et al. Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc. (2013) 4:542–59. doi: 10.1016/j.jamda.2013.05.021
59. Deutz NE, Bauer JM, Barazzoni R, Biolo G, Boirie Y, Bosy-Westphal A, et al. Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr. (2014) 33:929–36. doi: 10.1016/j.clnu.2014.04.007
60. Landi F, Calvani R, Tosato M, Martone AM, Ortolani E, Savera G, et al. Anorexia of aging: risk factors, consequences, and potential treatments. Nutrients. (2016) 8:69. doi: 10.3390/nu8020069
61. Leslie W, Hankey C. Aging, nutritional status and health. Healthcare (Basel). (2015) 3:648–58. doi: 10.3390/healthcare3030648
62. Venter C, Greenhawt M, Meyer RW, Agostoni C, Reese I, du Toit G, et al. EAACI position paper on diet diversity in pregnancy, infancy and childhood: Novel concepts and implications for studies in allergy and asthma. Allergy. (2020) 75:497–523. doi: 10.1111/all.14051
63. Roduit C, Frei R, Depner M, Schaub B, Loss G, Genuneit J, et al. Increased food diversity in the first year of life is inversely associated with allergic diseases. J Allergy Clin Immunol. (2014) 133:1056–64. doi: 10.1016/j.jaci.2013.12.1044
64. Grimshaw KE, Bryant T, Oliver EM, Martin J, Maskell J, Kemp T, et al. Incidence and risk factors for food hypersensitivity in UK infants: results from a birth cohort study. Clin Transl Allergy. (2015) 6:1. doi: 10.1186/s13601-016-0089-8
65. Venter C, Maslin K, Holloway JW, Silveira LJ, Fleischer DM, Dean T, et al. Different measures of diet diversity during infancy and the association with childhood food allergy in a UK birth cohort study. J Allergy Clin Immunol Pract. (2020) 8:2017–26. doi: 10.1016/j.jaip.2020.01.029
66. Nicklaus S, Divaret-Chauveau A, Chardon ML, Roduit C, Kaulek V, Ksiazek E, et al. The protective effect of cheese consumption at 18 months on allergic diseases in the first 6 years. Allergy. (2019) 74:788–98. doi: 10.1111/all.13650
67. Royal C, Gray C. Allergy prevention: an overview of current evidence. Yale J Biol Med. (2020) 93:689–98.
Keywords: allergy, tolerance, life-course, pediatrics, older people, diet, gut microbiota, malnutrition
Citation: Spolidoro GCI, Azzolino D, Cesari M and Agostoni C (2021) Diet Diversity Through the Life-Course as an Opportunity Toward Food Allergy Prevention. Front. Allergy 2:711945. doi: 10.3389/falgy.2021.711945
Received: 19 May 2021; Accepted: 02 September 2021;
Published: 24 September 2021.
Edited by:
Berber Vlieg-Boerstra, Onze Lieve Vrouwe Gasthuis (OLVG), NetherlandsReviewed by:
Kirsi Laitinen, University of Turku, FinlandCopyright © 2021 Spolidoro, Azzolino, Cesari and Agostoni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Carlo Agostoni, Y2FybG8uYWdvc3RvbmlAdW5pbWkuaXQ=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.