
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Aging, 06 September 2022
Sec. Interventions in Aging
Volume 3 - 2022 | https://doi.org/10.3389/fragi.2022.960986
This article is part of the Research TopicInsights in Aging Interventions: 2022View all 12 articles
 Junaidah B. Barnett1,2,3*†
Junaidah B. Barnett1,2,3*† Wu Zeng4,5†
Wu Zeng4,5†Objective: Older adults face many chronic health issues including heart disease and osteoporosis, which are preventable through changes in lifestyle behaviors. The Healthy Eating for Successful Living in Older Adults™ (HESL) is a 6-week community education program designed specifically for persons aged ≥60 years, to promote behavioral changes toward a healthy lifestyle. Our objective is to evaluate the HESL. This is the first official evaluation of the HESL since its initiation in 2005.
Study Design: A cluster randomized controlled trial.
Method: Program implementation and evaluation took place between July 2018 and January 2020. Twenty-nine sites, with 292 participants aged ≥60 years from across five states (mostly from Massachusetts), were randomized into the intervention group (IG) (16 sites; n = 150 participants) and control group (CG) (13 sites; n = 142 participants). The HESL workshops followed a scripted curriculum including information from the USDA’s MyPlate™ and the USDA 2015–2020 dietary guidelines. Intervention elements included goal setting, self-assessment, group support, and problem solving through brainstorming. The CG received no intervention. Outcome measures were collected in both groups at baseline, 2 weeks postintervention (week 8), and 6 months postintervention. These included self-reported lifestyle behaviors, a composite healthy behavior index (HBI), body mass index [weight (kg)/height (m2)], and waist-to-hip circumference ratio (WHR). Mixed-effects regression models were used to examine the impact of the intervention.
Results: The IG showed significantly improved responses to most healthy lifestyle behavior questions at week 8 compared to the CG. However, not all improved responses were sustained at month 6. Significant improvements detected at month 6 included responses to the question on making food choices that are healthy for the heart, using MyPlate™ tools for food choices, reading nutrition labels when shopping/planning meals, and confidence in managing own health (p < 0.001 in most cases). HBI was significantly improved at week 8 and month 6 (p < 0.001). WHR decreased significantly (p < 0.05) at month 6.
Conclusion: Positive changes in lifestyle behaviors and WHR were observed in older adults due to the HESL intervention.
Clinical Trial Registration: clinicaltrial.gov, Identifier: NCT04991844; https://clinicaltrials.gov/ct2/show/NCT04991844
Greater than 60% of adults over the age of 65 have been reported to have more than one chronic condition (Ward and Schiller, 2013), including heart disease, cancer, stroke, diabetes, osteoporosis, obesity, and Alzheimer’s disease (Kirkman et al., 2012; Halter et al., 2014; Mark Mather and KelvinPollard, 2015; Arauco Lozada et al., 2021; Fahimfar et al., 2021; Falaschi et al., 2021); these diseases have devastating effects on their functional capability and quality of life. By 2049, functional disability, such as hip fractures and stroke, due to chronic diseases in older persons, is expected to increase at least 300 percent (Boult et al., 1996). Severe, immediate, and progressive disabilities lead to the inability of older adults to care for themselves (Fried and Guralnik, 1997). In addition, health care costs for older adults with chronic diseases and functional impairments, including home care expenses, are high and continue to grow (Stuck et al., 2004; Medical Spending of the Elderly, 2015). The burden of various chronic diseases such as heart disease and osteoporosis can be reduced with changes in lifestyle behaviors. Changes in lifestyle behaviors such as making healthy food choices, increasing physical activity, improving sleep quality, smoking cessation, and maintaining a healthy body weight have been shown to help prevent, slow, stop, or even reverse various chronic diseases (Barnard et al., 1994; Ornish et al., 1998; Hu and Willett, 2002; Roberts and Barnard, 2005; Ornish et al., 2008; Barnard et al., 2009; Frates, 2016; Orenstein et al., 2016; Benjamin et al., 2017) and to increase life expectancy (Loef and Walach, 2012), with great potential to improve quality of life and reduce health care costs. It is therefore important to help empower older adults toward self-care and well-being. This can be accomplished with the development of effective evidence-based interventions that are safe, relatively low-cost, and scalable and have the most potential for the largest impact (Frieden, 2014).
To address this need, in 2005, Hebrew SeniorLife and its associated partners designed and piloted a new program for older adults focused on nutrition and healthy lifestyle behaviors. The program—Healthy Eating for Successful Living in Older Adults™ (HESL)—provides older adults with needed knowledge on healthy food choices and lifestyle behaviors and tools that support behavioral changes (details of the HESL intervention are described below). At present, HESL serves more than 1,000 older persons yearly. The program is available in English, Spanish, and Russian, with plans to translate the intervention for Chinese and Portuguese speakers. The program is now disseminated through its training center at AgeSpan, previously known as the Elder Services of the Merrimack Valley and North Shore, located in Lawrence, Massachusetts. AgeSpan licenses and trains councils on aging, senior centers, congregate housing sites, neighborhood health centers, community centers, faith-based organizations, and others to deliver the program to the older persons in their communities. The program, available in both in-person and remote delivery models, is currently being offered in all 14 counties including 50% of cities and towns in Massachusetts, as well as in 13 additional states.
This study presents data on an evaluation of the HESL and examines the impact of the intervention on factors such as healthy behaviors, food choices, and quality of life at 2 weeks post-intervention (week 8) and 6 months post-intervention. This is the first official evaluation of the HESL since its initiation in 2005.
A cluster unblinded randomized controlled trial in persons aged ≥60 years, recruited from community-based settings, was conducted between July 2018 and January 2020. The intervention group (IG) was compared with the control group (CG) receiving no intervention to evaluate the effects of the 6-week HESL intervention on outcome measures of interest at week 8 (i.e., at 2 weeks post-intervention), and at 6 months post-intervention. These time points were selected because of interest to determine the short-term or more immediate impact of the intervention, as well as the longer-term impact of 6 months post-intervention.
A biostatistician who was independent of the program implementers conducted the randomization at the site level [i.e., senior centers (n = 14), housing authorities (n = 4), churches (n = 3), assisted living facilities (n = 6), and library (n = 2)]. A total of 29 sites across five states (Massachusetts, Maryland, Florida, Rhode Island, and Michigan) were randomly assigned to the HESL IG and CG, using a single randomization approach with computerized random numbers. Sixteen sites were assigned to the IG, and 13, to the CG. All participants recruited in the IG sites were assigned as IG participants, and those recruited in the CG sites were assigned CG participants by the program implementers. Figure 1 shows the consort diagram of the study. The sample size was determined based on the assumption that the intervention would increase the mean fiber intake (g/day) by 30%, an indicator for a parallel study. With a type I error of 5% and a type II error of 80%, as well as a 25% loss of follow-up, we estimated a sample size of 125 per group.
Participant inclusion criteria included: 1) male or female aged ≥60 years, 2) English speaking, and 3) willing to participate and complete all study activities following randomization into the IG or CG. Those eligible, interested, and able to participate were recruited into the study.
Both IG and CG met at three specified time points, i.e., at baseline, week 8, and month 6, for the completion of study questionnaires and to provide anthropometric measures. In addition, the IG met weekly to receive the intervention outlined below.
The protocol was approved by the New England Institutional Review Board, and written informed consent was obtained from all participants. This study was registered at clinicaltrial.gov with identifier: NCT04991844. https://clinicaltrials.gov/ct2/show/NCT04991844.
The HESL intervention was developed with strategies aimed to promote changes in lifestyle factors in adults aged ≥60 years.
The IG met once a week, for 2.5 h, with 10–16 participants/group, over a period of 6 weeks for the HES workshops. The HES workshops, offered in English, followed a scripted curriculum that incorporated information from the USDA’s MyPlate™, and the USDA 2015–2020 dietary guidelines (U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2015). The HESL was designed to increase knowledge of healthy eating habits and identify food choices for healthy bones and heart, and for overall health. Participants were taught how to select healthier foods using the MyPlate™ app and to read labels, plan menus, and prepare meals in a lively interactive session of learning as a group. Among others, MyPlate™ emphasizes the importance of eating a variety of foods, eating foods from five major food groups (fruits, vegetables, grains, protein, and dairy), covering half their plates with fruits and vegetables, making half of the grain intake whole grains, choosing low or no fat dairy products, choosing foods with less added sugar and salt, avoiding transfat and saturated fat, reducing intake of cholesterol, eating more fiber, and being physically active. MyPlate™ is also individualized for each person based on his/her age, gender, and level of physical activity. Participants were thus guided on how to determine their caloric requirements and what to eat.
Participants were also taught goal setting, problem solving through brainstorming, group support, self-assessment, and management of dietary and physical activity patterns. At the end of every session, each participant was asked to set a goal for the new week related to healthy eating. The goals were focused on a nutrition challenge the participant would like to address and felt confident was achievable before the next week’s session. Participants were taught to formulate their own SMART goals, i.e., goals that are specific, measurable, action-oriented, realistic, and time-sensitive, which incorporate accountability and monitoring (Frates et al., 2019). Participants kept a food and physical activity journal to monitor changes and identify problem areas in their eating habits and physical activity. By monitoring food choices, and physical activity type and intensity through the completion of a food and physical activity journal, participants were in a position to identify healthy changes made in their dietary and physical activity patterns as well as identify barriers to reaching goals. This self-assessment component is an important factor of the intervention.
These workshops were led by program leaders who were trained and certified to present materials and support brainstorming to solve a problem or overcome barriers to success, identified by participants, using culturally relevant solutions, as well as the promotion of socialization and group interaction. These are also important components of the intervention. In addition, participants were given supporting materials such as a “Participant Manual” with clear dietary intake and physical activity guidelines. Participants were also provided with information on the availability of community nutrition and health education resources. The intervention also included various “hands-on” activities such as visiting a grocery store, learning to read food labels, and making healthy choices in preparing meals and at a restaurant. A Registered Dietitian/Nutritionist was available to help answer questions that remained unanswered by the workshop leaders, and responses were brought back to participants the following week. Table 1 provides a summary of the workshops’ weekly curricula.
Participant’s age, gender (male = 1, female = 0), race (seven categories; recoded as 1 for White; 0, otherwise), education (eight categories, recoded as 1 for those with a college degree and above; 0, otherwise), and marital status (eight categories; recoded as 1 for married or having domestic partnership; 0, otherwise). Information on household income was excluded as almost 80% of participants did not respond to this question.
These self-reported healthy behavior questions were formulated and used in-house to specifically evaluate the impact of the HESL intervention in the past. These questions and their transformations into binary variables are listed in Table 2. In addition, we generated a composite healthy behavior index (HBI) by summing the dichotomous items. HBI scores ranged between 0 and 10; a higher score indicates more healthy behaviors.
This was measured using the Berkman–Syme Social Connectedness Survey (Berkman and Syme, 1979), which contained 11 items, with questions such as “How many close friends do you have?” We generated a continuous score using the same approach as done by Salinas et al. (2017); a high score implies greater social connectedness. Evidence for the predictive validity of this self-reported survey is available in Berkman and Breslow (1983).
Using a physical activity questionnaire, participants reported their average amount of time spent per week (ranging from 0 min to ≥11 h) during the previous month doing various activities. Using the classification by Ainsworth et al. (1993), metabolic equivalent task (MET)-hours/week were estimated by multiplying the MET score for each activity by the reported hours per week and summing across all activities (Colditz et al., 2003; Eliassen et al., 2010). This self-reported physical activity measure is used extensively in research studies and has been validated in both men and women (Al-Shaar et al., 2022; Pernar et al., 2022).
Participants provided data on their height at baseline, weight, and waist and hip circumferences (WC and HC) measures at all time points. Body mass index (BMI, kg/m2) and waist-to-hip circumference ratio (WHR) were computed. Self-reported anthropometric measures such as weight, height, and WC and HC have been observed to be valid measures in men and women (Rimm et al., 1990; Hodge et al., 2020). In this study, the workshop leaders trained the study participants on how to take their anthropometric measures and were there to supervise and assist participants with taking their measurements. A weighing scale was made available to participants at the workshop to take their weights, and a tape measure was given to each participant to take both their WC and HC.
Quality of life was measured using the Euro-QoL-5D-5L questionnaire (Janssen et al., 2013). The questionnaire solicits responses on mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Participants provided a rating of their own health on a scale of 0–100, where 0 means “death” and 100 means “the best health.” This self-reported quality of life questionnaire is available in more than 150 languages and is used as a quantitative measure of health outcomes that reflects the patient’s own judgment (Group E, 2022).
Descriptive analyses for all measures between the IG and CG at baseline, week 8, and month 6 were conducted using the student t-test for continuous variables or the chi-square test for categorical variables. The impact of the intervention at week 8 and month 6 without adjusting for covariates were estimated using a difference in differences (DID) approach (unadjusted DID) using the following linear regression model A:
where ycit represents outcome measure of interest (continuous or binary variables) specified in the data collection section above, for individual i, at time t, in cluster (or site) c; t implies the three study time points; group is the variable indicating whether the individual belongs to the IG (group = 1) or CG (group = 0); week 8 and month 6 indicate whether the measure is at the respective time points; group*week 8 and group*month 6 are the interaction terms between group and these time points, respectively; and
The impact of the intervention at week 8 and month 6 adjusting for covariates and addressing repeated measures (adjusted DID) were estimated using linear mixed-effects regression models by adding covariates of
By including
Although our outcome measures contain binary variables, we opted to use linear models for both DID models to ease the interpretation of our findings. However, we also presented the results from logit mixed-effects models (Rich-Edwards et al., 2019) for binary variables in Supplementary Table S1, which shows that there were no major differences in findings between the linear mixed-effects and logit mixed-effects models in terms of the significance of coefficients and the direction of the intervention impact. In addition, we presented relevant results between groups for participants who provided data at all three time points in Supplementary Tables S2,S3. All the analyses were conducted with Stata 16.0 software (STATA Corp, College Station, TX; Stata, RRID:SCR_012,763).
Table 3 shows the baseline characteristics of the participants (N = 292) in the CG (N = 142) and IG (N = 150) (Figure 1). Most participants lived in Massachusetts. There were no statistical differences in age, marital status, and gender between groups. However, the IG had significantly more White participants compared with the CG (p < 0.001). The IG also had more participants with some college education or above than the CG (p < 0.05).
Findings from the unadjusted linear regression model A are presented in Table 4. Compared to findings at week 8, most improvements in the unadjusted values were sustained at month 6, except for making food choices for healthy bones. Significantly more participants in the IG compared with the CG indicated that they read nutrition labels at 6 months (p < 0.001).
The impact of the intervention controlling for age, gender, race, educational and marital status, as well as baseline differences, on health behaviors are also presented in Table 4. (adjusted DID using model B). In general, findings remain consistent compared with the results from the unadjusted analyses for both week 8 and month 6. However, in contrast to the unadjusted findings, reading nutrition labels when shopping/planning meals and having fairly good or very good sleep quality were shown to be significantly improved in the adjusted results at week 8 (p < 0.05 in both cases). Adjusted findings also showed that at week 8, the IG showed significantly improved responses to these questions: making food choices that are healthy for bones (p < 0.001) and heart (p < 0.001), using MyPlate™ (p < 0.001), confidence in managing own health (p < 0.001), and playing an active role in managing their own health care and well-being (p < 0.05). A similar pattern was observed at month 6, except for responses to making healthy food choices for bones and sleep quality, where significant differences were no longer detected between groups in the adjusted results. The degree to which participants understood and found useful the information provided by their doctors and nurses about their health problems and concerns, at week 8 and month 6, was also not found to be statistically significant between groups in the adjusted findings. The continuous composite HBI scores showed a significant improvement at week 8 (p < 0.001) and month 6 (p < 0.001).
We used a logit mixed-effects model to examine the impact of the intervention on the binary variables as a sensitivity analysis. In general, we found similar results in the logit mixed-effects model (Supplementary Table S1). Adjusted findings on participants who provided data at all three time points are presented in Supplementary Table S2.
Table 5 presents unadjusted and adjusted results of our analyses showing the effects of the intervention on BMI, WC, HC, WHR, physical activity level, social connectedness, and quality of life at week 8 and month 6. Similar to the results from the unadjusted analyses, the adjusted analyses results did not show a significant impact of intervention at week 8 nor at month 6, except for a significant decrease in WHR at month 6 (p < 0.05) in the IG, in comparison with the CG. Adjusted findings on participants who provided data at all three time points are presented in Supplementary Table S3.
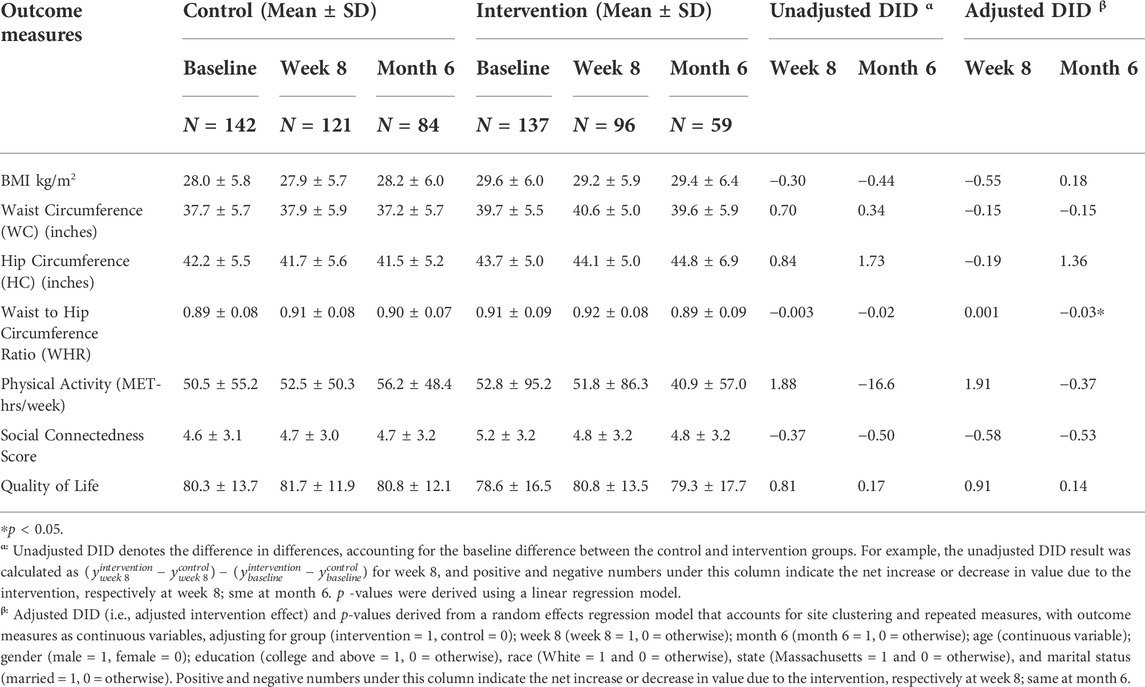
TABLE 5. Intervention impact on body mass index, waist-to-hip circumference ratio, physical activity, social connectedness, and quality of life (all participants).
The IG showed significantly improved responses to most healthy lifestyle behavior questions at week 8 compared with the CG. However, not all improved responses were sustained at month 6. Significant improvements detected at month 6 included responses to the question on making food choices that are healthy for the heart, using MyPlate™ tools for food choices, reading nutrition labels when shopping/planning meals, and confidence in managing own health. The HESL intervention was also associated with a statistically significant increase in the composite HBI at week 8 and month 6 and a significant decrease in WHR at month 6.
Various elements of the HESL intervention that contribute to its improvement in changing a healthy lifestyle include promoting changes in habits through small increments by setting goals for the week at the end of each session. As described, participants were taught to formulate their own SMART goals, i.e., goals that are specific, measurable, action-oriented, realistic, and time-sensitive, which incorporate accountability and monitoring (Frates et al., 2019). By monitoring food choices, as well as physical activity type and intensity through the completion of a food and physical activity journal, participants were in a position to identify changes made in their dietary and physical activity patterns as well as identify barriers to reaching goals. Brainstorming to solve problems or overcome barriers to success using culturally relevant solutions and the promotion of socialization and group interaction were also likely to be contributing factors. In addition, participants were given supporting materials such as a “Participant Manual” with clear dietary intake and physical activity guidelines. Participants were also provided with information on the availability of community nutrition and health education resources. Further, workshop leaders had access to a registered dietitian/nutritionist who helped answer questions raised by participants that remain unanswered during the workshops.
Although the IG showed statistically significant improvement in making food choices that are healthy for bones at week 8, this improvement was not sustained at 6 months, and it is unclear why. The 2015–2020 USDA dietary guidelines for healthy bones include promoting the consumption of dairy products, including whole and skim milk, at least 2 to 3 times/day (U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2015). However, it is questionable if such guidelines are protective of bone health, and there are concerns that such recommendations may actually increase adverse health outcomes (Ganmaa et al., 2002; Ganmaa and Sato, 2005; Qin et al., 2009; Aune et al., 2015; Willett and Ludwig, 2020). It may be too much for some participants to consume large amounts of dairy products daily long term, especially for those who are lactose intolerant or who may not like the taste of milk. However, HESL does promote the consumption of other sources of calcium, including plant-based calcium sources such as tofu, nuts beans, broccoli, and kale (Messina and Mangels, 2001; American Dietetic and Dietitians of, 2003), as well as calcium supplements, to promote healthy bones.
Although participants were instructed on the health benefits of physical activity of various types including endurance, strength, flexibility, and balance exercises, during the intervention, we did not find a significant increase in the level of physical activity. We were informed by AgeSpan that the intervention did not focus on physical activity as much as it did on making dietary changes and that some participants opted out of the physical activity component.
WHR showed a significant decrease of 0.03 at month 6 in the IG compared to the CG (Table 5). WHR is a measure of central obesity or visceral fat, whereas BMI is a measure of overall obesity (Paniagua et al., 2008). Central obesity as measured using WHR has been shown to be a stronger predictor of chronic diseases, including heart disease, diabetes, and cancer, as well as mortality, than measures of total body fat such as BMI (Lapidus et al., 1984; Fujimoto et al., 1999; Janssen et al., 2002; Vazquez et al., 2007; Mathieu et al., 2009; Czernichow et al., 2011). The significant decrease in WHR at month 6 suggests that the healthy behavioral changes due to the HESL intervention may have a protective impact on an important risk factor of chronic diseases. In a study by de Koning et al. (2007), a 0.01 increase in WHR has been shown to be associated with a 5% increase in the risk of incident CVD events. It is not clear if the decrease in WHR in this study was due to changes in the WC and/or HC. However, a non-significant increase in HC was observed (Table 5).
Given that there was no follow-up of participants between week 8 and month 6, it is noteworthy that several significant improvements to healthy lifestyle behaviors observed at week 8, remained significant at month 6 (Table 4). It is difficult to predict if participants will continue to maintain the positive changes made to their lifestyle behaviors due to the intervention beyond the 6-month period. Future evaluations to determine factors associated with longer-term (i.e., beyond 6 months) effectiveness of HESL on healthy lifestyle behaviors, disease outcomes, and quality of life, among others, as well as to identify barriers to continuing adoption of these behaviors, are needed. We were not able to evaluate the impact of the intervention beyond 6 months due to a lack of resources. However, healthy lifestyle and behavioral changes can be maintained long term (Ornish et al., 1998; Ornish et al., 2005). It has been shown that those who made the greatest changes showed the biggest improvement (Ornish et al., 1998). In the BROAD study, overweight participants in the IG were empowered with knowledge of the benefits of a plant-based diet and encouraged to incorporate it into their lifestyles (Wright et al., 2017). The CG, also overweight participants, received standard medical care. Although the study lasted only 3 months, the plant-based group not only lost significant weight but also achieved greater weight loss at 6 and 12 months, derived physical and mental benefits, and stopped taking many of their medications, even though no further instructions were given beyond the 3 months intervention (Wright et al., 2017; Greger, 2020). Sustainable changes in dietary habits and behavioral lifestyles beyond the intervention period are possible when changes result in increased benefits and pleasure and/or are associated with positive emotions that naturally motivate the rewiring of the brain toward the adoption of such behaviors (Frates, 2016; Esselstyn, 2017; Fogg, 2020; Greger, 2020). Healthful habits repeated over time become a way of life (Fogg, 2020; Greger, 2020) and should be the ultimate goal of all interventions aimed at improving dietary and health behaviors. Although there was considerable variation across participants and behaviors (Gardner et al., 2012), it has been shown that automaticity plateaued on average around 66 days after the first daily performance (Phillippa et al., 2010). Working effortfully on a new behavior for 2 to 3 months may be appealing to participants interested in turning that behavior into a habit (Gardner et al., 2012).
Overall, findings in this work suggest that the HESL intervention positively impacts the healthy behaviors of its targeted population. However, several limitations should be acknowledged. These include a sample size of predominantly female and White, making the findings of this study likely not generalizable to males and persons of other ethnic groups. The present study used largely self-reported measures that were previously validated. Available resources did not allow for use of objective health measures (e.g., blood biomarkers), which would help further strengthen the study findings. Another limitation is missing pre-existing conditions and other data which may bias findings. For example, income was not included in the regression model. Although requested, only 21% of participants provided income data. The analyses, however, controlled for educational status, which serves as a surrogate variable for household income. As such, this bias is likely mitigated. Biases of randomization not being blinded were also limitations. The large loss to follow-up was another limitation of the study. While not receiving the intervention may be a reason for leaving the CG by approximately 23% of the CG participants, it is not clear why the intervention lost approximately 43% of its IG participants. Characteristics of participants in both groups who were lost to follow-up were not found to be significantly different when compared with those in these groups who remained in the study at week 8 and month 6 (data not shown). Future evaluations need to reach out to participants leaving the intervention to identify reasons for leaving, so future programs can remedy the situation.
The present study was able to explore the impact of the intervention based on self-reported measures. Although limited, findings suggest that the intervention has a positive impact on study participants’ health behaviors as well as a risk factor of chronic diseases (WHR), as reported by the participants themselves. Objective outcome measures that directly point to bone, heart, and overall health, are needed to support and strengthen current study findings. As such incorporation of such measures is needed in future evaluations of this intervention.
A huge challenge in public health remains the need to minimize the large gap between existing evidenced-based knowledge on healthy diets and lifestyle behaviors and their actual adoption as a way of life by individuals in all age groups (Willett, 2019). Closing this gap requires multiple strategies. The HESL attempts to address this challenge in older adults through community education. The HESL program implementers will continue to adjust the program to optimize its effectiveness and its ability to change behaviors in the long term, beyond the intervention period, and to expand its reach to other states.
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the New England Institutional Review Board. The patients/participants provided their written informed consent to participate in this study.
JBB and WZ were responsible for conceptualizing and designing the evaluation component of the study as well as providing guidance on data collection. WZ was responsible for data analyses and wrote the first draft of the results section. JBB wrote the first draft of the article other than the results section. Both JBB and WZ were responsible for the interpretation of data, review of the overall article, and approval of the final paper for submission.
Funding for this work was provided by the American Association of Retired Persons (AARP) Foundation. The funder has no role in the design, methods, subject recruitment, data collection, analysis, and preparation of the paper.
The Healthy Eating for Successful Living in Older Adults™ (HESL) was implemented by AgeSpan (previously the Elder Services of the Merrimack Valley’s Healthy Living Center of Excellence Department), in collaboration with the Massachusetts Area Agency on Aging, Executive Office of Elder Affairs, Latino Health Insurance Project, Enhanced Asian Community on Health, and the Massachusetts Association of Councils on Aging. Data collection was overseen and managed by staff at AgeSpan. The authors, JBB and WZ, wish to extend their appreciation to the program implementers, and to all study participants.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fragi.2022.960986/full#supplementary-material
Ainsworth, B. E., Haskell, W. L., Leon, A. S., Jacobs, D. R., Montoye, H. J., Sallis, J. F., et al. (1993). Compendium of physical activities: classification of energy costs of human physical activities. Med. Sci. Sports Exerc. 25 (1), 71–80. doi:10.1249/00005768-199301000-00011
Al-Shaar, L., Pernar, C. H., Chomistek, A. K., Rimm, E. B., Rood, J., Stampfer, M. J., et al. (2022). Reproducibility, validity, and relative validity of self-report methods for assessing physical activity in epidemiologic studies: Findings from the women's lifestyle validation study. Am. J. Epidemiol. 191 (4), 696–710. doi:10.1093/aje/kwab294
American Dietetic, A., and Dietitians of, C. (2003). Position of the American dietetic association and dietitians of Canada: Vegetarian diets. Can. J. Diet. Pract. Res. Summer 64 (2), 62–81. doi:10.3148/64.2.2003.62
Arauco Lozada, T., Garrido Carrasco, P., and Farran Codina, A. (2021). Impact on the risk of malnutrition and depression of a clinical trial with nutritional educational intervention in non-institutionalized elderly subjects receiving a telecare service in Terrassa (Spain). Nutr. Hosp. 38 (2), 260–266. doi:10.20960/nh.03269
Aune, D., Navarro Rosenblatt, D. A., Chan, D. S., Vieira, A. R., Vieira, R., Greenwood, D. C., et al. (2015). Dairy products, calcium, and prostate cancer risk: a systematic review and meta-analysis of cohort studies. Am. J. Clin. Nutr. 101 (1), 87–117. doi:10.3945/ajcn.113.067157
Barnard, N. D., Katcher, H. I., Jenkins, D. J., Cohen, J., and Turner-McGrievy, G. (2009). Vegetarian and vegan diets in type 2 diabetes management. Nutr. Rev. 67 (5), 255–263. doi:10.1111/j.1753-4887.2009.00198.x
Barnard, R. J., Jung, T., and Inkeles, S. B. (1994). Diet and exercise in the treatment of NIDDM. The need for early emphasis. Diabetes Care 17 (12), 1469–1472. doi:10.2337/diacare.17.12.1469
Benjamin, E. J., Blaha, M. J., Chiuve, S. E., Cushman, M., Das, S. R., Deo, R., et al. (2017). Heart disease and stroke statistics-2017 update: A report from the American heart association. Circulation 135 (10), e146–e603. doi:10.1161/CIR.0000000000000485
Berkman, L. F., and Breslow, L. (1983). Health and the ways of living: The alameda county study. Oxford University Press.
Berkman, L. F., and Syme, S. L. (1979). Social networks, host resistance, and mortality: a nine-year follow-up study of alameda county residents. Am. J. Epidemiol. 109 (2), 186–204. doi:10.1093/oxfordjournals.aje.a112674
Boult, C., Altmann, M., Gilbertson, D., Yu, C., and Kane, R. L. (1996). Decreasing disability in the 21st century: the future effects of controlling six fatal and nonfatal conditions. Am. J. Public Health 86 (10), 1388–1393. doi:10.2105/ajph.86.10.1388
Colditz, G. A., Feskanich, D., Chen, W. Y., Hunter, D. J., and Willett, W. C. (2003). Physical activity and risk of breast cancer in premenopausal women. Br. J. Cancer 89 (5), 847–851. doi:10.1038/sj.bjc.6601175
Czernichow, S., Kengne, A. P., Huxley, R. R., Batty, G. D., de Galan, B., Grobbee, D., et al. (2011). Comparison of waist-to-hip ratio and other obesity indices as predictors of cardiovascular disease risk in people with type-2 diabetes: a prospective cohort study from ADVANCE. Eur. J. Cardiovasc. Prev. Rehabil. 18 (2), 312–319. doi:10.1097/HJR.0b013e32833c1aa3
de Koning, L., Merchant, A. T., Pogue, J., and Anand, S. S. (2007). Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: meta-regression analysis of prospective studies. Eur. Heart J. 28 (7), 850–856. doi:10.1093/eurheartj/ehm026
Eliassen, A. H., Hankinson, S. E., Rosner, B., Holmes, M. D., and Willett, W. C. (2010). Physical activity and risk of breast cancer among postmenopausal women. Arch. Intern. Med. 170 (19), 1758–1764. doi:10.1001/archinternmed.2010.363
Esselstyn, C. B. (2017). A plant-based diet and coronary artery disease: a mandate for effective therapy. J. Geriatr. Cardiol. 14 (5), 317–320. doi:10.11909/j.issn.1671-5411.2017.05.004
Fahimfar, N., Noorali, S., Yousefi, S., Gharibzadeh, S., Shafiee, G., Panahi, N., et al. (2021). Prevalence of osteoporosis among the elderly population of Iran. Arch. Osteoporos. 16 (1), 16. doi:10.1007/s11657-020-00872-8
Falaschi, P., Marques, A., and Giordano, S. (2021). “Osteoporosis and fragility in elderly patients,” in Orthogeriatrics: The management of older patients with fragility fractures. Editors P. Falaschi, and D. Marsh, 35–52.
Fogg, B. J. (2020). Tiny habits - the small changes that change everything. New York: Houghton Mifflin Harcourt Boston.
Frates, B. B. J., Joseph, R., and Peterson, J. A. (2019). “Collaborating, motivating, goal-setting and tracking,” in Lifestyle medicine handbook: An introduction to the power of healthy habits monterey. Editor B. Frates (CA: Healthy Learning), 89–118.
Frates, E. P. (2016). Interview with award winners from ACLM 2015, nashville, Tennessee - dean ornish. Am. J. Lifestyle Med. 10 (5), 341–344. doi:10.1177/1559827616642399
Fried, L. P., and Guralnik, J. M. (1997). Disability in older adults: evidence regarding significance, etiology, and risk. J. Am. Geriatr. Soc. 45 (1), 92–100. doi:10.1111/j.1532-5415.1997.tb00986.x
Frieden, T. R. (2014). Six components necessary for effective public health program implementation. Am. J. Public Health 104 (1), 17–22. doi:10.2105/AJPH.2013.301608
Fujimoto, W. Y., Bergstrom, R. W., Boyko, E. J., Chen, K. W., Leonetti, D. L., NeweLL-Morris, L., et al. (1999). Visceral adiposity and incident coronary heart disease in Japanese-American men. The 10-year follow-up results of the Seattle Japanese-American Community Diabetes Study. Diabetes Care. Diabetes Care 22 (11), 1808–1812. doi:10.2337/diacare.22.11.1808
Ganmaa, D., Li, X. M., Wang, J., Qin, L. Q., Wang, P. Y., Sato, A., et al. (2002). Incidence and mortality of testicular and prostatic cancers in relation to world dietary practices. Int. J. Cancer 98 (2), 262–267. doi:10.1002/ijc.10185
Ganmaa, D., and Sato, A. (2005). The possible role of female sex hormones in milk from pregnant cows in the development of breast, ovarian and corpus uteri cancers. Med. Hypotheses 65 (6), 1028–1037. doi:10.1016/j.mehy.2005.06.026
Gardner, B., Lally, P., and Wardle, J. (2012). Making health habitual: the psychology of 'habit-formation' and general practice. Br. J. Gen. Pract. 62 (605), 664–666. doi:10.3399/bjgp12X659466
Greger, M. (2020). A whole food plant-based diet is effective for weight loss: The evidence. Am. J. Lifestyle Med. 14 (5), 500–510. doi:10.1177/1559827620912400
Group E (2022). EQ-5D-5L | about. Available at: https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/(Accessed 6 28, 2022).
Halter, J. B., Musi, N., McFarland Horne, F., Crandall, J. P., Goldberg, A., Harkless, L., et al. (2014). Diabetes and cardiovascular disease in older adults: current status and future directions. Diabetes 63 (8), 2578–2589. doi:10.2337/db14-0020
Hodge, J. M., Shah, R., McCullough, M. L., Gapstur, S. M., and Patel, A. V. (2020). Validation of self-reported height and weight in a large, nationwide cohort of U.S. adults. PLoS One 15 (4), e0231229. doi:10.1371/journal.pone.0231229
Hu, F. B., and Willett, W. C. (2002). Optimal diets for prevention of coronary heart disease. JAMA 288 (20), 2569–2578. doi:10.1001/jama.288.20.2569
Janssen, I., Heymsfield, S. B., Allison, D. B., Kotler, D. P., and Ross, R. (2002). Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous, and visceral fat. Am. J. Clin. Nutr. 75 (4), 683–688. doi:10.1093/ajcn/75.4.683
Janssen, M. F., Pickard, A. S., Golicki, D., Gudex, C., Niewada, M., Scalone, L., et al. (2013). Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual. Life Res. 22 (7), 1717–1727. doi:10.1007/s11136-012-0322-4
Kirkman, M. S., Briscoe, V. J., Clark, N., Florez, H., Haas, L. B., Halter, J. B., et al. (2012). Diabetes in older adults. Diabetes Care 35 (12), 2650–2664. doi:10.2337/dc12-1801
Lapidus, L., Bengtsson, C., Larsson, B., Pennert, K., Rybo, E., Sjostrom, L., et al. (1984). Distribution of adipose tissue and risk of cardiovascular disease and death: a 12 year follow up of participants in the population study of women in gothenburg, Sweden. Br. Med. J. 289 (6454), 1257–1261. doi:10.1136/bmj.289.6454.1257
Loef, M., and Walach, H. (2012). The combined effects of healthy lifestyle behaviors on all cause mortality: a systematic review and meta-analysis. Prev. Med. 55 (3), 163–170. doi:10.1016/j.ypmed.2012.06.017
Mark Mather, L. A. J., and KelvinPollard, M. (2015). Aging in the United States. Popul. Bull. 70 (2).
Mathieu, P., Poirier, P., Pibarot, P., Lemieux, I., and Despres, J. P. (2009). Visceral obesity: the link among inflammation, hypertension, and cardiovascular disease. Hypertension 53 (4), 577–584. doi:10.1161/HYPERTENSIONAHA.108.110320
Medical Spending of the Elderly (2015). Medical spending of the elderly. Natl. Bur. Econ. Res. Bull. Aging Health 2 (2), 2–3.
Messina, V., and Mangels, A. R. (2001). Considerations in planning vegan diets: children. J. Am. Diet. Assoc. 101 (6), 661–669. doi:10.1016/s0002-8223(01)00167-5
Orenstein, L., Chetrit, A., and Dankner, R. (2016). Healthy lifestyle pattern is protective against 30-yr cancer incidence in men and women: A cohort study. Nutr. Cancer 68 (3), 410–419. doi:10.1080/01635581.2016.1153673
Ornish, D., Magbanua, M. J., Weidner, G., Weinberg, V., Kemp, C., Green, C., et al. (2008). Changes in prostate gene expression in men undergoing an intensive nutrition and lifestyle intervention. Proc. Natl. Acad. Sci. U. S. A. 105 (24), 8369–8374. doi:10.1073/pnas.0803080105
Ornish, D., Scherwitz, L. W., Billings, J. H., Brown, S. E., Gould, K. L., Merritt, T. A., et al. (1998). Intensive lifestyle changes for reversal of coronary heart disease. JAMA 280 (23), 2001–2007. doi:10.1001/jama.280.23.2001
Ornish, D., Weidner, G., Fair, W. R., Marlin, R., Pettengill, E. B., Raisin, C. J., et al. (2005). Intensive lifestyle changes may affect the progression of prostate cancer. J. Urol. 174 (3), 1065–1069. discussion 1069-70. doi:10.1097/01.ju.0000169487.49018.73
Paniagua, L., Lohsoonthorn, V., Lertmaharit, S., Jiamjarasrangsi, W., and Williams, M. A. (2008). Comparison of waist circumference, body mass index, percent body fat and other measure of adiposity in identifying cardiovascular disease risks among Thai adults. Obes. Res. Clin. Pract. 2 (3), I-II. doi:10.1016/j.orcp.2008.05.003
Pernar, C. H., Chomistek, A. K., Barnett, J. B., Ivey, K., Al-Shaar, L., Roberts, S. B., et al. (2022). Validity and relative validity of alternative methods of assessing physical activity in epidemiologic studies: Findings from the men's lifestyle validation study. Am. J. Epidemiol. 191, 1307–1322. doi:10.1093/aje/kwac051
Phillippa, L., van Jaarsveld, C. H. M., Potts, H. W. W., and Wardle, J. (2010). How are habits formed: Modelling habit formation in the real world. Eur. J. Soc. Psychol. 40 (6), 998–1009. doi:10.1002/ejsp.674
Qin, L. Q., He, K., and Xu, J. Y. (2009). Milk consumption and circulating insulin-like growth factor-I level: a systematic literature review. Int. J. Food Sci. Nutr. 60 (7), 330–340. doi:10.1080/09637480903150114
Rich-Edwards, J. W., Stuart, J. J., Skurnik, G., Roche, A. T., Tsigas, E., Fitzmaurice, G. M., et al. (2019). Randomized trial to reduce cardiovascular risk in women with recent preeclampsia. J. Womens Health 28 (11), 1493–1504. doi:10.1089/jwh.2018.7523
Rimm, E. B., Stampfer, M. J., Colditz, G. A., Chute, C. G., Litin, L. B., Willett, W. C., et al. (1990). Validity of self-reported waist and hip circumferences in men and women. Epidemiology 1 (6), 466–473. doi:10.1097/00001648-199011000-00009
Roberts, C. K., and Barnard, R. J. (2005). Effects of exercise and diet on chronic disease. J. Appl. Physiol.(1985) 98 (1), 3–30. doi:10.1152/japplphysiol.00852.2004
Salinas, J., Beiser, A., Himali, J. J., Satizabal, C. L., Aparicio, H. J., Weinstein, G., et al. (2017). Associations between social relationship measures, serum brain-derived neurotrophic factor, and risk of stroke and dementia. Alzheimers Dement. 3 (2), 229–237. doi:10.1016/j.trci.2017.03.001
Stuck, A. E., Beck, J. C., and Egger, M. (2004). Preventing disability in elderly people. Lancet 364 (9446), 1641–1642. doi:10.1016/S0140-6736(04)17365-0
U.S. Department of Health and Human Services and U.S. Department of Agriculture (2015). 2020 dietary guidelines for Americans. Available at: https://health.gov/our-work/nutrition-physical-activity/dietary-guidelines /previous-dietary- guidelines/2015 (Accessed 6, 28, 2022).
Vazquez, G., Duval, S., Jacobs, D. R., and Silventoinen, K. (2007). Comparison of body mass index, waist circumference, and waist/hip ratio in predicting incident diabetes: a meta-analysis. Epidemiol. Rev. 29, 115–128. doi:10.1093/epirev/mxm008
Ward, B. W., and Schiller, J. S. (2013). Prevalence of multiple chronic conditions among US adults: estimates from the national health interview survey, 2010. Prev. Chronic Dis. 10, E65. doi:10.5888/pcd10.120203
Willett, W. C. (2019). Crystal ball: Walter Willett. Eur. J. Clin. Nutr. 73 (4), 491–494. doi:10.1038/s41430-018-0279-7
Willett, W. C., and Ludwig, D. S. (2020). Milk and health. N. Engl. J. Med. 382 (7), 644–654. doi:10.1056/NEJMra1903547
Keywords: Healthy Eating for Successful Living in Older Adults™, HESl, older adults, lifestyle behaviors, evaluation, HESL community education program
Citation: Barnett JB and Zeng W (2022) Healthy Eating for Successful Living in Older Adults™ community education program—evaluation of lifestyle behaviors: A randomized controlled trial. Front. Aging 3:960986. doi: 10.3389/fragi.2022.960986
Received: 03 June 2022; Accepted: 11 July 2022;
Published: 06 September 2022.
Edited by:
Joris Deelen, Max Planck Institute for Biology of Ageing, GermanyReviewed by:
Arpit Sharma, Harvard University, United StatesCopyright © 2022 Barnett and Zeng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Junaidah B. Barnett, SkJhcm5ldHRAaGhyZXMub3Jn
†These authors have contributed equally to this work and share first, senior and last authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.