- 1School of Health Services Management, Xi'an Medical University, Xi'an, Shaanxi, China
- 2Institute of Chinese Medical Sciences, State Key Laboratory of Quality Research in Chinese Medicine, University of Macau, Taipa, Macao SAR, China
Objectives: This study aimed to explore the rationality of the social networks-depression-cognitive impairment pathway and to provide recommendations for the development of mild cognitive impairment intervention strategies.
Methods: A cross-sectional survey was conducted in 2021. Sixteen urban communities in Xi 'an, Shaanxi China were selected as sample sites. The cognitive function, social networks and depression were measured by the Montreal Cognitive Assessment (MoCA), the Lubben Social Network Scale-6 (LSNS-6) and the Geriatric Depression Scale-15 (GDS-15), respectively. The generalized linear model was used to analysis the impact of social networks on cognitive impairment, and further analysis the mediating effect of depression.
Results: A total of 745 elderly people aged 60 and above was included in this survey, with an average age of 68.90 ± 6.00 years. The prevalence of cognitive impairment was 18.52%, and the prevalence of cognitive impairment increased with age. According to the generalized linear model, poor social networks (relative network, friend network) was associated with higher risk of cognitive impairment (OR = 2.08, 95% CI: 1.27–3.41), and this association was more significant in women and older adults <70 years of age. Mediation analysis results showed that depression was the mediating path between social networks and cognitive impairment, with the indirect effects accounting for 34.44%.
Conclusion: Social isolation increases the risk of cognitive impairment and depression has a significant mediating effect on the relationship between social isolation and cognitive impairment.
1 Introduction
Cognitive impairment (Kuang et al., 2021), as a chronic non-communicable disease, is becoming an important public health problem in China. Cognitive impairment refers broadly to various degrees of cognitive impairment from various causes, ranging from mild cognitive impairment (MCI) to dementia. Dementia is the most severe stage of cognitive impairment and is the leading cause of disability in people over 60 years of age worldwide. To date, there are no effective treatments for these diseases due to the unclear pathogenic mechanisms and failures in clinical trials for drugs developed. Therefore, early intervention before conversion to dementia becomes an important strategy for dementia prevention.
MCI, a potentially transformative state between normal aging and dementia, is recognized as a precursor to Alzheimer's disease (AD) and other types of dementia, providing a unique “window of time” for secondary prevention of dementia. Epidemiological studies have shown that the risk of progression to dementia in MCI patients is 10 times higher than in normal older adults. Some scholars have used models to estimate the influence of a 10% or 25% reduction in risk factors on the prevalence of dementia. Using an estimate of 7.7 million new cases per year, it was concluded that a 10% reduction in risk factor exposure would have resulted in 250,000 (3.3%) fewer new cases per year globally, whereas a 25% reduction in risk factor exposure would have prevented 680,000 (8.8%) new cases per year (Rost et al., 2022). It has been shown that modification of 12 risk factors may prevent or delay up to 40% of dementia (Luttenberger et al., 2012). Since the AD process is irreversible, it is significant to explore possible influencing factors and influencing mechanisms at the MCI stage and to develop appropriate intervention strategies.
Social networks are of particular interest among numerous intervention strategies because improving factors associated with social networks is a relatively simple and feasible way to improve cognitive function. The association of social network as an independent variable with cognitive health outcomes has been partially confirmed (Houtjes et al., 2014). A rich social network has been shown to be a particularly effective intervention for delaying dementia and MCI. Studies have shown that being socially active, even at an advanced age, can delay the onset of dementia by more than a year (Paillard-Borg et al., 2012). There is growing evidence that older adults who have been in a resourceful social network exhibit better cognitive abilities than their socially disengaged peers (Kuiper et al., 2015). However, few studies have elucidated the mechanisms underlying the relationship between social networks and cognitive impairment in older adults. With the increased emphasis on the biopsychosocial model, it is of great relevance whether social networks could play a role in cognitive health through a psychological pathway.
While an association has been found between social networks and MCI, the underlying factors and psychological mechanisms remain largely unexplored. Currently, only a few epidemiological studies have examined the link between social networks and cognitive health. Findings from empirical studies have shown that the quality rather than the quantity of social networks is protective against cognitive decline (Krueger et al., 2009) and that the emotional support appears to be more beneficial than instrumental support (Amieva et al., 2010). It can therefore be hypothesized that depression is a better predictor of MCI than social networks. It is expected that this mechanism is an indirect one, particularly since the outcome of cognitive function is being explained by the perceived rather than directly received quality of social networks. By investigating cognitive function, social networks and depression status of the elderly population in urban communities, this study aimed (1) to investigate the current prevalence of cognitive impairment in older adults in the community, (2) to explore the direct effects of social networks on cognitive function in older adults, (3) to explore the rationale for the Social Network-Depression-Cognitive Impairment pathway, to provide recommendations for the development of MCI intervention strategies, and to provide an important theoretical framework for clinical practice and public health efforts to prevent dementia in older adults. Exploring the mediating pathways between social networks and MCI could help find more effective ways to provide useful information for early detection and prevention of MCI.
2 Methods
2.1 Data sources and study population
This study was a cross-sectional survey conducted in Xi'an, which was located in the middle of the Guanzhong Plain. Using a stratified sampling method, two districts were first randomly selected from among the districts of Xi'an, two streets were randomly selected in each district, and four communities were randomly selected in each street, resulting in a total of sixteen communities being selected. In each community, 45 older adults were selected with the following inclusion and exclusion criteria.
Inclusion criteria: ≥60 years of age; no intellectual disability, able to understand and answer questions; no major illnesses in the past year. Exclusion criteria: inability to complete the questionnaire independently/assisted; refusal to sign the informed consent form.
The sample size was calculated using the sample size calculation formula of the cross-sectional survey, which was as follows:
With a maximum response distribution rate (P = 0.5, e = 0.1p) and 95% confidence level (z = 1.96), 385 samples were needed in this study. In addition, considering the stability of the regression model, which usually requires 10–15 times the independent variable, the final sample size of this study should be 140–210. Finally, 745 older adults were surveyed in this study, which meets the sample size requirement.
2.2. Social networks, cognitive impairment and depression
Cognitive function was measured using the MoCA (Beijing version). The scale includes cognitive dimensions such as visuospatial ability, naming, attention, language, abstract reasoning, memory, and orientation to time and place. The scale consists of 30 items. The higher the score, the better the neurocognitive function.
Social networks were assessed using LSNS-6. The LSN-6 measures the social isolation of older adults by measuring perceived social support from both family and friends, with each section consisting of three equally weighted items, each consisting of “none,” “1,” “2,” “3–4,” “5–8,” and “9, or more,” with a higher score indicating more social engagement. A total score of less than 12 is considered to have social impairment.
Mental health was measured using GDS-15. The scale has 15 items, each of which is scored as 0 or 1, with a maximum score of 15, with higher scores indicating more pronounced depressive symptoms and ≥5 indicating possible depression.
2.3 Covariance
The covariates involved in this study and their grouping included gender (male, female), age (<70, ≥70), marital status (married, others), night shift work (no, yes), living alone (no, yes), smoking status (no, yes), drinking status (no, yes), regular exercise (no, yes), sleep duration (<7, 7–9, ≥9), SES (poor, medium, good). In this study, education level, occupation and income were adopted to reflect the SES of the subjects.
2.4. Statistical analysis
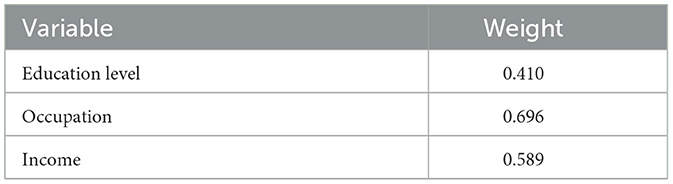
The basic characteristics of the study population were presented using descriptive statistics, with continuous variables statistically described using mean (x) ± standard deviation (SD) and categorical variables using frequency (n) and composition ratio (%). The factors influencing cognitive impairment were modeled using a generalized linear model. Two models were created, model 1 adjusting nothing and model 2 adjusting covariates. The effects of different social network types (relative network and friend network) on cognition were further analyzed. Principal component analysis was used to construct the SES, and the corresponding weight was shown in Table 1. SES were divided into three groups based on quantile. Social network was the independent variable, cognitive impairment was the outcome variable, and depression was the mediating variable. The commanding sgmediation2 was employed to conduct mediation analysis, and the calculation was based on “product of coefficients” approach. All statistical procedures were completed using STATA 15.1, and all tests were two-sided, a = 0.05.
3 Results
3.1 Sociodemographic characteristics of the subjects
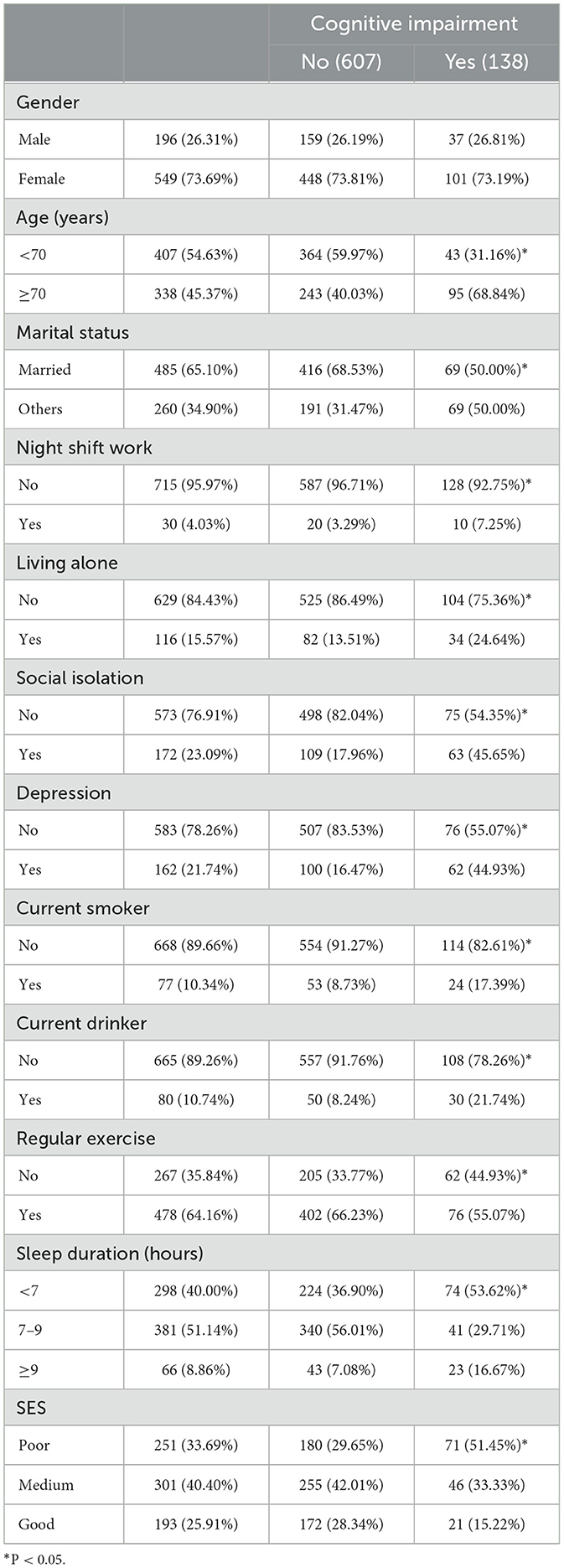
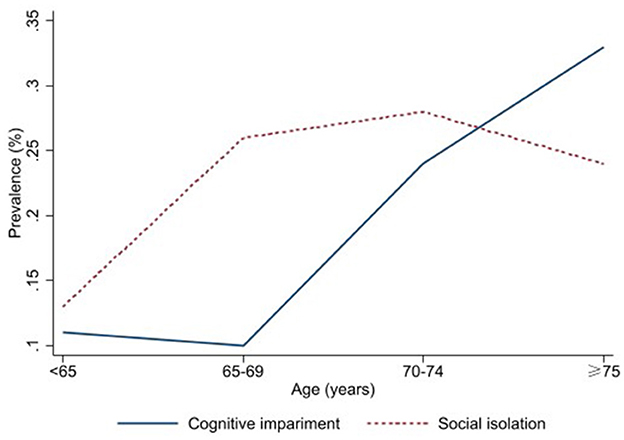
A total of 745 participants with an average age of 68.90 ± 6.00 years were included in this study, among whom 73.69% were female, 65.10% were married, 10.34% smoked, and 10.74% drank alcohol. Other socio-demographic information was shown in Table 2. The prevalence of cognitive impairment and social isolation in the study subjects was 18.52% and 23.09%, respectively. Figure 1 showed the prevalence of cognitive impairment and social isolation among different age groups. The analysis of factors influencing cognitive impairment showed differences in the prevalence of cognitive impairment by age, living alone, social isolation, alcohol consumption, exercise, sleep duration, and SES groups (Table 2).
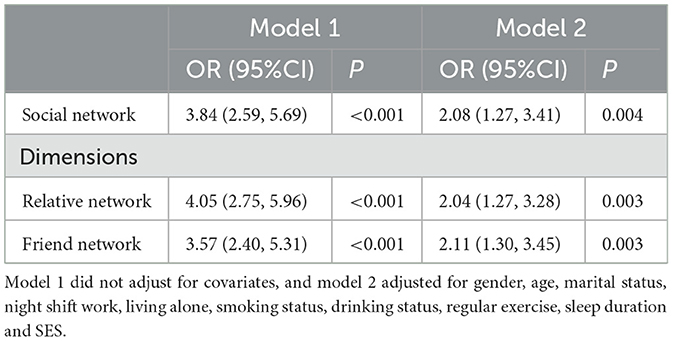
3.2. The correlation between cognitive impairment and social network
The prevalence of cognitive impairment was higher in those with poor social network (OR = 2.08, 95% CI: 1.27–3.41). Relative network 2.04 (95% CI: 1.27–3.28) and friend network 2.11 (95% CI: 1.30–3.45) were also associated with higher cognitive impairment (Table 3). We also analyzed the correlation between social networks and cognitive impairment among different groups. Male with poorer social networks had a higher risk of cognitive impairment, OR = 1.34 (95% CI: 0.51–3.52), but the results were not statistically significant, considering the lack of statistical power due to the small sample size. Similar results were found in women, OR = 2.35 (95% CI: 1.25–4.42), which also showed that the positive health effects of social networks appear to be more pronounced for women. The results for more subgroups were shown in Figure 2.
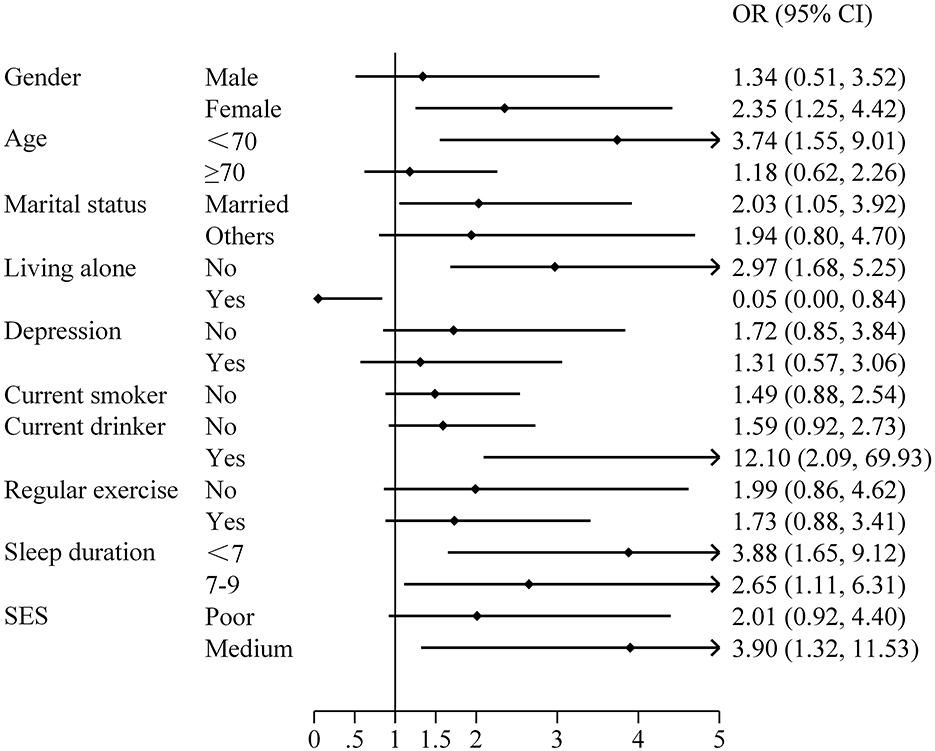
Figure 2. Correlation analysis between social network and cognitive impairment among different groups.
3.3. Mediated effects analysis
We further took cognitive impairment as the outcome variable, social isolation as the independent variable, depression as the mediating variable, and control related covariates to conduct the mediated effects analysis and found that the total effect (OR = 1.20, 95% CI: 1.11, 1.29) and direct effect (OR = 1.13, 95% CI: 1.04,1.22) of social network on cognitive impairment were significant. The indirect effect was statistically significant (OR = 1.06, 95% CI: 1.03, 1.10), which suggested the mediating effect of depression, and the proportion of mediating effect mediated by depression was 34.44% (Table 4).
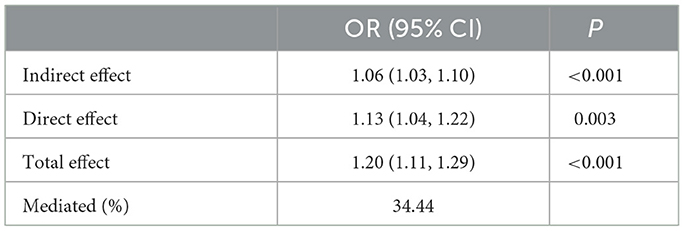
Table 4. Total, direct, and indirect effects of social networks on cognitive impairment through depression.
4 Discussion
Although the link between social networks, depression, and cognitive impairment in older adults is well established, the exact nature of their relationship has not been conclusively determined. Using empirical data, this study found that depression has a significant mediating effect on the relationship between social isolation and cognitive impairment, suggesting that engaging in more social activity may reduce cognitive impairment by improving depressive status. This mediating effect accounts for about 1/3 of the total effect. In addition, we also found that the prevalence of cognitive impairment is high in the elderly, and social isolation increases the risk of cognitive impairment.
This study found that older adults with high social contact had better cognitive health and lower prevalence of MCI, which is consistent with many previous studies (Seeman et al., 2011; Hughes et al., 2013; Haslam et al., 2014; Glei et al., 2005; Conroy et al., 2010). This association between social networks and cognitive status can be explained by the “use it or lose it” theory. Social networks can stimulate the brain by providing social cues, organizing social gatherings, or engaging in complex social discourse, a form of mental exercise that enhances cognitive reserve and slows the process of pathophysiological changes in cognitive deterioration. There are several main hypotheses about how social networks affect cognitive state. The first is the cognitive reserve hypothesis. This hypothesis stems from the phenomenon that in some elderly populations, amyloid PET-CT molecular imaging reveals normal or only mildly impaired cognitive function despite the presence of large amounts of Aβ deposits in the brain [the main characteristic pathological change of AD is β-amyloid (Aβ) deposits]. Some scholars have therefore proposed the cognitive reserve hypothesis, which suggests that participation in social, cognitively, or intellectually stimulating activities and physical exercise activities in late middle age enhances synaptic activity and increases the capacity of the cognitive reserve, thus maintaining cognitive function at a state of MCI and delaying the clinical manifestation of dementia. The cognitive reserve hypothesis successfully explains that the nervous system can tolerate damage and pathology without manifesting clinically as functional impairment (Bennett et al., 2006). The second hypothesis is the stress hypothesis, with the observation that chronic stress increases the risk of dementia (Wilson et al., 2003), while extensive social networks may reduce stress and lower levels of hormones such as glucocorticoids and corticosteroids, which regulate brain function and slow the progression of MCI to dementia. The third hypothesis is the vascular hypothesis, which suggests that high-quality social network activity can broadly affect the biological system and reduce the risk of dementia by reducing cardiovascular disease risk factors associated with brain disease (Fratiglioni et al., 2004). In addition, a neurobiological model has been pointed out to illustrate the idea (Shen et al., 2022). Social networks can also affect cognitive function by activating neurobiological mechanisms that stimulate the hypothalamic-pituitary-adrenal axis as well as decreasing sleep quality. When a person is chronically exposed to a poor social network, he or she develops a high level of vigilance against the social environment and exhibits behaviors to stay away from it, and this self-protective escape behavior in turn deepens this prejudice against the social environment and activates neurobiological mechanisms leading to increased brain load and cognitive decline. However, findings are mixed and not all studies have reported this association (Saczynski et al., 2006; Zamora-Macorra et al., 2017; Holwerda et al., 2014). This may be due to factors such as different social environment characteristics of minority group members, differences in the composition and size of social networks, and differences in language and cultural status, which may lead to a nonsignificant relationship between social networks and cognitive impairment (Saczynski et al., 2006; Zamora-Macorra et al., 2017).
Depression is one of the most prevalent mental disorders among older adults is a global public health priority (Byers et al., 2010). Depression has a significant impact on the elderly population and is associated with higher all-cause mortality, suicide risk, and increased health service use (Manley et al., 2017). Systematic evaluations have shown that predictors of depression in older adults are cognitive impairment or less extensive social networks (Djernes, 2006). The association between social networks and depression has been widely recognized and may be a precursor to depression. Loss of interpersonal interactions in social networks, especially when combined with social exclusion, is a long recognized and valid risk factor for the development of major depression (Houtjes et al., 2014; Ford et al., 2011). A few studies have also reported no association between social networks and depression. The Descriptive Study of community-dwelling older adults by Frances et al. showed that depressed older adults were not socially isolated compared to the nondepressed group and that the depressed group reported significantly more contact with friends than the nondepressed group (Ford et al., 2011; Wilby, 2011). Two other studies also found no association between frequency of social contact and depression (Millán-Calenti et al., 2013). Depression is a well-established risk factor for MCI (Barnes et al., 2006; Teo et al., 2013). Numerous studies have confirmed that the more severe the depressive symptoms, the greater the likelihood of progression from a normal cognitive state to MCI or from MCI to dementia (Donovan et al., 2014; Rosenberg et al., 2013). Even the lowest levels of depressive symptoms induce persistent pathophysiological effects. Research by Donovan et al. (2015) pointed out that very low depressive states were an important predictor of the transition to MCI and the occurrence of neurodegenerative brain changes in a cognitively normal elderly population. Donovan et al. (2017) showed that the risk of progression from normal cognition to MCI was doubled in those with depression scores equal to or above the threshold.
The indirect association, in addition to this direct association, was found to be mediated by depressive symptoms. People with high social exposure were in better psychological condition and thus had better cognitive status. Depression mediated the association between social networks and MCI, which is consistent with the findings of several previous studies (Conroy et al., 2010; Balouch et al., 2019; Boss et al., 2015). This can be explained by a conceptual model of a social process proffered by Berkman and colleagues in the year 2000 (Fratiglioni et al., 2004). This theory suggests that extensive social contact can further influence cognitive health through mediating factors such as psychological distress. Not only does extensive social contact provide older adults with good moods, such as a sense of belonging, it can also provide timely advice and help when they experience stressful events and emergencies, which in turn reduces symptoms of depression and further hinders the progression of MCI. The study by McHugh et al. suggests that social network has an indirect effect on cognitive health through psychological stress, confirming that cognitive health mediates the association between social networks and MCI (McHugh Power et al., 2018). Demonstrating this mediation is also an important addition to further understanding of the ways in which social networks affect cognition.
There are some limitations in empirical studies. First, since the data are based on self-report, recall bias may exist. Second, because this is a cross-sectional study, the direction of the association between social networks and cognitive function cannot be determined. Third, this study used MoCA to identify cognitive impairments, which has been shown to be unstable when providing domain-specific information. Fourth, although it meets the required sample size, the small sample size may still lead to unstable research results. Fifth, the causal relationship between social networks and depression is not clear, which somewhat limits our conclusions. Sixth, we note that other social variables may be associated with cognitive health. Future research could extend the current findings by examining the role of other social factors associated with cognitive performance. Future studies in different settings are needed to validate our findings regarding the association between social networks, depression, and cognitive impairment.
5 Conclusion
Social isolation increases the risk of cognitive impairment and depression has a significant mediating effect on the relationship between social isolation and cognitive impairment. The discovery of the social networks-depression-cognitive impairment pathway suggests that the cognitive health of older adults can be improved by focusing on their social network status and mental health status.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Xi'an Medical University Ethics Approval Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
ZZ: Conceptualization, Formal analysis, Methodology, Resources, Writing – original draft, Writing – review & editing. YB: Conceptualization, Data curation, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was funded by three research grants awarded to YB from the University of Macau (MYRG2019-00044-ICMS, QRCM-IRG2022-001, and SKL-QRCM-IRG2023-032), the fifth batch of school-level key discipline construction project of Xi'an Medical University (12202310), three Undergraduate Training Programs for Innovation and Entrepreneurship (S202311840072S, S202411840057S, and 121524141), and two school-level scientific research fund from Xi'an Medical University (2023BS21 and 2023BS27). The funding body played no role in the design of the study and the collection, analysis, and interpretation of data and in writing the manuscript.
Acknowledgments
We sincerely thank all participants of this study, as well as the dedicated staff who facilitated the fieldwork coordination and the investigators who contributed to data collection.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Amieva, H., Stoykova, R., Matharan, F., Helmer, C., Antonucci, T. C., Dartigues, J. F., et al. (2010). What aspects of social network are protective for dementia? Not the quantity but the quality of social interactions is protective up to 15 years later. Psychosom. Med. 72, 905–911. doi: 10.1097/PSY.0b013e3181f5e121
Balouch, S., Rifaat, E., Chen, H. L., and Tabet, N. (2019). Social networks and loneliness in people with Alzheimer's dementia. Int. J. Geriatr. Psychiatry 34, 666–673. doi: 10.1002/gps.5065
Barnes, D. E., Alexopoulos, G. S., Lopez, O. L., Williamson, J. D., and Yaffe, K. (2006). Depressive symptoms, vascular disease, and mild cognitive impairment: findings from the Cardiovascular Health Study. Arch. Gen. Psychiatry 63, 273–279. doi: 10.1001/archpsyc.63.3.273
Bennett, D. A., Schneider, J. A., Tang, Y., Arnold, S. E., and Wilson, R. S. (2006). The effect of social networks on the relation between Alzheimer's disease pathology and level of cognitive function in old people: a longitudinal cohort study. Lancet Neurol. 5, 406–412. doi: 10.1016/S1474-4422(06)70417-3
Boss, L., Kang, D. H., and Branson, S. (2015). Loneliness and cognitive function in the older adult: a systematic review. Int. Psychogeriatr. 27, 541–553. doi: 10.1017/S1041610214002749
Byers, A. L., Yaffe, K., Covinsky, K. E., Friedman, M. B., and Bruce, M. L. (2010). High occurrence of mood and anxiety disorders among older adults: the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 67, 489–496. doi: 10.1001/archgenpsychiatry.2010.35
Conroy, R. M., Golden, J., Jeffares, I., O'Neill, D., and McGee, H. (2010). Boredom-proneness, loneliness, social engagement and depression and their association with cognitive function in older people: a population study. Psychol. Health Med. 15, 463–473. doi: 10.1080/13548506.2010.487103
Djernes, J. K. (2006). Prevalence and predictors of depression in populations of elderly: a review. Acta Psychiatr. Scand. 113, 372–387. doi: 10.1111/j.1600-0447.2006.00770.x
Donovan, N. J., Amariglio, R. E., Zoller, A. S., Rudel, R. K., Gomez-Isla, T., Blacker, D., et al. (2014). Subjective cognitive concerns and neuropsychiatric predictors of progression to the early clinical stages of Alzheimer disease. Am. J. Geriatr. Psychiatry 22, 1642–1651. doi: 10.1016/j.jagp.2014.02.007
Donovan, N. J., Hsu, D. C., Dagley, A. S., Schultz, A. P., Amariglio, R. E., Mormino, E. C., et al. (2015). Depressive symptoms and biomarkers of Alzheimer's disease in cognitively normal older adults. J. Alzheimers Dis. 46, 63–73. doi: 10.3233/JAD-142940
Donovan, N. J., Wu, Q., Rentz, D. M., Sperling, R. A., Marshall, G. A., Glymour, M. M., et al. (2017). Loneliness, depression and cognitive function in older U.S. adults. Int. J. Geriatr. Psychiatry 32, 564–573. doi: 10.1002/gps.4495
Ford, E., Clark, C., and Stansfeld, S. A. (2011). The influence of childhood adversity on social relations and mental health at mid-life. J. Affect. Disord. 133, 320–327. doi: 10.1016/j.jad.2011.03.017
Fratiglioni, L., Paillard-Borg, S., and Winblad, B. (2004). An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurol. 3, 343–353. doi: 10.1016/S1474-4422(04)00767-7
Glei, D. A., Landau, D. A., Goldman, N., Chuang, Y. L., Rodríguez, G., Weinstein, M., et al. (2005). Participating in social activities helps preserve cognitive function: an analysis of a longitudinal, population-based study of the elderly. Int. J. Epidemiol. 34, 864–871. doi: 10.1093/ije/dyi049
Haslam, C., Cruwys, T., and Haslam, S. A. (2014). “The we's have it”: evidence for the distinctive benefits of group engagement in enhancing cognitive health in aging. Soc. Sci. Med. 120, 57–66. doi: 10.1016/j.socscimed.2014.08.037
Holwerda, T. J., Deeg, D. J., Beekman, A. T., van Tilburg, T. G., Stek, M. L., Jonker, C., et al. (2014). Feelings of loneliness, but not social isolation, predict dementia onset: results from the Amsterdam Study of the Elderly (AMSTEL). J. Neurol. Neurosurg. Psychiatr. 85, 135–142. doi: 10.1136/jnnp-2012-302755
Houtjes, W., van Meijel, B., van de Ven, P. M., Deeg, D., van Tilburg, T., Beekman, A., et al. (2014). The impact of an unfavorable depression course on network size and loneliness in older people: a longitudinal study in the community. Int. J. Geriatr. Psychiatry 29, 1010–1017. doi: 10.1002/gps.4091
Hughes, T. F., Flatt, J. D., Fu, B., Chang, C. C., and Ganguli, M. (2013). Engagement in social activities and progression from mild to severe cognitive impairment: the MYHAT study. Int. Psychogeriatr. 25, 587–595. doi: 10.1017/S1041610212002086
Krueger, K. R., Wilson, R. S., Kamenetsky, J. M., Barnes, L. L., Bienias, J. L., Bennett, D. A., et al. (2009). Social engagement and cognitive function in old age. Exp. Aging Res. 35, 45–60. doi: 10.1080/03610730802545028
Kuang, J., Zhang, P., Cai, T., Zou, Z., Li, L., Wang, N., et al. (2021). Prediction of transition from mild cognitive impairment to Alzheimer's disease based on a logistic regression-artificial neural network-decision tree model. Geriatr. Gerontol. Int. 21, 43–47. doi: 10.1111/ggi.14097
Kuiper, J. S., Zuidersma, M., Oude Voshaar, R. C., Zuidema, S. U., van den Heuvel, E. R., Stolk, R. P., et al. (2015). Social relationships and risk of dementia: a systematic review and meta-analysis of longitudinal cohort studies. Ageing Res. Rev. 22, 39–57. doi: 10.1016/j.arr.2015.04.006
Luttenberger, K., Hofner, B., and Graessel, E. (2012). Are the effects of a non-drug multimodal activation therapy of dementia sustainable? Follow-up study 10 months after completion of a randomised controlled trial. BMC Neurol. 12:151. doi: 10.1186/1471-2377-12-151
Manley, G., Gardner, A. J., Schneider, K. J., Guskiewicz, K. M., Bailes, J., Cantu, R. C., et al. (2017). systematic review of potential long-term effects of sport-related concussion. Br. J. Sports Med. 51, 969–977. doi: 10.1136/bjsports-2017-097791
McHugh Power, J., Tang, J., Lawlor, B., Kenny, R. A., and Kee, F. (2018). Mediators of the relationship between social activities and cognitive function among older Irish adults: results from the Irish longitudinal study on ageing. Aging Ment. Health 22, 129–134. doi: 10.1080/13607863.2016.1233935
Millán-Calenti, J. C., Sánchez, A., Lorenzo-López, L., Cao, R., and Maseda, A. (2013). Influence of social support on older adults with cognitive impairment, depressive symptoms, or both coexisting. Int. J. Aging Hum. Dev. 76, 199–214. doi: 10.2190/AG.76.3.b
Paillard-Borg, S., Fratiglioni, L., Xu, W., Winblad, B., and Wang, H. X. (2012). An active lifestyle postpones dementia onset by more than one year in very old adults. J. Alzheimers Dis. 31, 835–842. doi: 10.3233/JAD-2012-120724
Rosenberg, P. B., Mielke, M. M., Appleby, B. S., Oh, E. S., Geda, Y. E., Lyketsos, C. G., et al. (2013). The association of neuropsychiatric symptoms in MCI with incident dementia and Alzheimer disease. Am. J. Geriatr. Psychiatry 21, 685–695. doi: 10.1016/j.jagp.2013.01.006
Rost, N. S., Brodtmann, A., Pase, M. P., van Veluw, S. J., Biffi, A., Duering, M., et al. (2022). Post-stroke cognitive impairment and dementia. Circ. Res. 130, 1252–1271. doi: 10.1161/CIRCRESAHA.122.319951
Saczynski, J. S., Pfeifer, L. A., Masaki, K., Korf, E. S., Laurin, D., White, L., et al. (2006). The effect of social engagement on incident dementia: the Honolulu-Asia Aging Study. Am. J. Epidemiol. 163, 433–440. doi: 10.1093/aje/kwj061
Seeman, T. E., Miller-Martinez, D. M., Stein Merkin, S., Lachman, M. E., Tun, P. A., Karlamangla, A. S., et al. (2011). Histories of social engagement and adult cognition: midlife in the U.S. study. Gerontol. B Psychol. Sci. Soc. Sci.66, i141–i152. doi: 10.1093/geronb/gbq091
Shen, C., Rolls, E. T., Cheng, W., Kang, J., Dong, G., Xie, C., et al. (2022). Associations of social isolation and loneliness with later dementia. Neurology 99, e164–e175. doi: 10.1212/WNL.0000000000201564
Teo, A. R., Choi, H., and Valenstein, M. (2013). Social relationships and depression: ten-year follow-up from a nationally representative study. PLoS ONE 8:e62396. doi: 10.1371/journal.pone.0062396
Wilby, F. (2011). Depression and social networks in community dwelling elders: a descriptive study. J. Gerontol. Soc. Work 54, 246–259. doi: 10.1080/01634372.2010.540074
Wilson, R. S., Evans, D. A., Bienias, J. L., Mendes de Leon, C. F., Schneider, J. A., and Bennett, D. A. (2003). Proneness to psychological distress is associated with risk of Alzheimer's disease. Neurology 61, 1479–1485. doi: 10.1212/01.WNL.0000096167.56734.59
Zamora-Macorra, M., de Castro, E. F., Ávila-Funes, J. A., Manrique-Espinoza, B. S., López-Ridaura, R., Sosa-Ortiz, A. L., et al. (2017). The association between social support and cognitive function in Mexican adults aged 50 and older. Arch. Gerontol. Geriatr. 68, 113–118. doi: 10.1016/j.archger.2016.10.005
Keywords: social networks, cognitive impairment, depression, mediating effect, older Chinese adults
Citation: Zhang Z and Bian Y (2025) Association between social networks and cognitive impairment among older Chinese adults: the mediating effect of depression. Front. Aging Neurosci. 16:1495694. doi: 10.3389/fnagi.2024.1495694
Received: 16 September 2024; Accepted: 20 December 2024;
Published: 13 January 2025.
Edited by:
Sharad Purohit, Augusta University, United StatesReviewed by:
Amanda Selwood, University of New South Wales, AustraliaMaria Luca, Centre for Addiction, Italy
Copyright © 2025 Zhang and Bian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ying Bian, Ymlhbnlpbmd1bUAxNjMuY29t
 Zhuo Zhang
Zhuo Zhang Ying Bian2*
Ying Bian2*