- 1Department of Surgery, Miri Hospital, Ministry of Health Malaysia, Miri, Sarawak, Malaysia
- 2Department of Surgery, Sibu Hospital, Ministry of Health Malaysia, Sibu, Sarawak, Malaysia
- 3Department of Surgery, Faculty of Medicine and Health Sciences, Universiti Malaysia Sabah, Kota Kinabalu, Sabah, Malaysia
Rectal foreign bodies often constitute an arduous diagnosis and perplexing management. A 72-year-old gentleman who is mentally sound was brought to the emergency department for severe epigastric pain of a 1-week duration. On examination, he was pyrexial and in sepsis. The abdomen was guarded. A digital rectal examination was normal. Erect chest radiography revealed air under the diaphragm and abdominal radiography showed neither dilated bowel nor foreign body. A diagnostic laparoscopy was performed which revealed a yellow hard rod-shaped foreign body at the pelvis. Upon conversion to midline laparotomy, the foreign body was found to be a toothbrush with intraperitoneal rectal perforation of 1 cm in length. The brush was removed and the perforation was repaired primarily. A diverting transverse loop colostomy was created. Rectal foreign bodies may cause life-threatening rectal injuries including lacerations, bleeding, perforation, and obstruction. It is deemed crucial that any patient with rectal foreign body demands an orderly approach with the intention of diagnosis, management, and post-extraction evaluation.
Background
Rectal foreign bodies often lead to a challenging diagnostic and management dilemma, starting from the initial evaluation in the emergency department and continuing through the post-extraction period. We report a rare case of rectal perforation secondary to a toothbrush in an elderly gentleman who was initially suspected of a perforated gastric ulcer. Based on the English literature review, up to date, there was only one case report on rectal perforation secondary to a toothbrush (1). We highlight a 72-year-old gentleman who presented with an acute abdomen and sepsis with pneumoperitoneum and we discuss our management plan.
Case Presentation
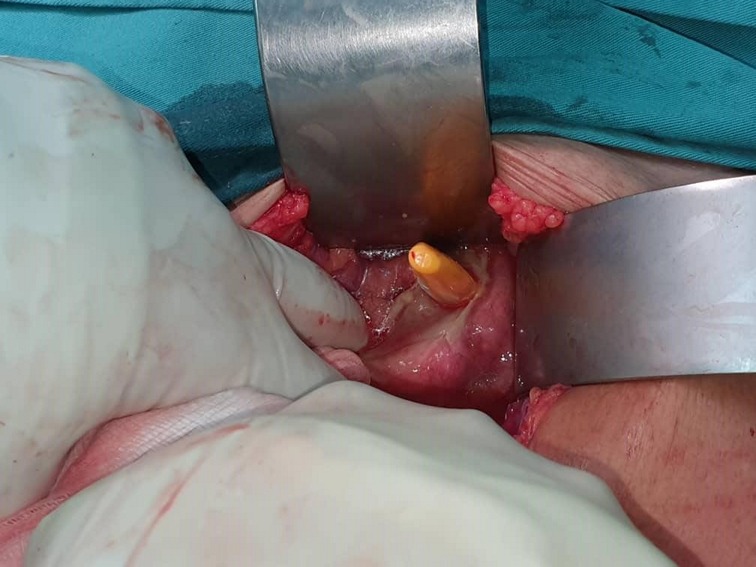
A 72-year-old gentleman was brought by family members for severe epigastric pain of 1-week duration. He is mentally sound and ADL independent prior to presentation. On examination, the abdomen was guarded. A digital rectal examination was normal. The patient is pyrexial and in sepsis. Erect chest radiography revealed air under the diaphragm and abdominal radiography showed neither dilated bowel nor foreign body. He then underwent a laparoscopy which revealed a yellow hard rod-shaped foreign body at the pelvis. The foreign body (Figures 1, 2) appeared to perforate the rectum.
Upon conversion to midline laparotomy, the foreign body was found to be a toothbrush. The rectal perforation was intraperitoneal with 1 cm in length. The brush was removed and the perforation was repaired primarily. In view of extensive contamination, a diverting transverse loop colostomy was created. The patient improved well on a postoperative day one and was allowed orally. In further history, he revealed a habit of using a toothbrush to assist in defecation and was unable to retrieve it back on one occasion. He did not reveal it to family members to avoid embarrassment. He was then referred to a psychiatrist for proper assessment. A colonoscopy after two months revealed no abnormality and he was planned for reversal of stoma.
Discussion
Rectal foreign bodies are widely documented in literatures. It is possible to occur after self-insertion for anorectal disease, concealment, criminal assault or accidental causes, or (most commonly) for sexual purposes including sexual gratification and anal erotism (2). Various objects involved, including fruits and vegetables, light bulbs, bottles, impulse body spray cans, and sex devices that have been described as retained rectal foreign bodies. Since there numerous types of objects and the sequelae of trauma it can cause to local tissues of the rectum and distal colon, it is crucial to rely on a systematic approach to the diagnosis and management of rectal foreign bodies.
History taking in these patients might be misleading due to their embarrassment and reluctance to seek medical care. Moreover, in the emergency room, patients may often be dishonest on the reason for their visit, thus leading to extensive and unnecessary workups and further delays (3). Hence, routine imaging and laboratory investigations are crucial. An abdominal radiograph would be helpful to look for radioopaque objects by assessing their shape, nature, and location (4). However, for certain objects, they are radiolucent under x-ray such as in our case. A high index of suspicion is needed to accurately diagnose their condition. In addition, the utmost degree of professionalism is required by the attending physician in managing this condition (5).
A retained rectal foreign body can be categorised as either high- or low-lying relative to the rectosigmoid junction. A palpable object on a digital rectal examination is considered low-lying and may be considered for bimanual extraction at the bedside provided no evidence of perforation (6). High-lying retained rectal foreign body on the other hand usually necessitates endoscopic or surgical intervention. Several factors must be considered before making the decision between primary repair with or without colostomy in the surgical management of colorectal injuries. These include the site and cause of the injury, physiologic stability of the patient, and the use of antibiotic. Among all of these considerations in surgical management, the grade of colorectal injury has been most widely discussed (7). In this patient advanced age and peritoneal contamination lead us to decide on the diverting colostomy. Moreover, this is the safest approach for this patient because we were unsure of the nature of the injury distal to the perforation.
In conclusion, rectal foreign bodies can cause potentially fatal injuries which include lacerations, haemorrhage, perforation, and distal obstruction. A systematic approach is required for the diagnosis, treatment, and post-extraction assessment in a patient with rectal foreign body.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Written informed consent was obtained from the individual for the publication of any potentially identifiable images or data included in this article.
Author Contributions
KA prepared and wrote this article. SYL and AJAH were involved in managing the patient besides preparing the intraoperative pictures. THC wrote and reviewed this manuscript. FH wrote and revised the manuscript as well as acted as the corresponding author. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rashid A, Khuroo S, Nazir S. Rectal perforation due to a lost toothbrush. Ann Saudi Med. (2013) 33:514–5. doi: 10.5144/0256-4947.2013.514
2. Koomstra JJ, Weersma RK. Management of rectal foreign bodies: Description of a new technique and clinical practice guidelines. World J Gastroenterol. (2008) 14:4403–6. doi: 10.3748/wjg.14.4403
3. Goldberg JE, Steele SR. Rectal foreign bodies. Surg Clin N Am. (2010) 90:173–84. doi: 10.1016/j.suc.2009.10.004
4. Ng CY, Hayati F, Ali AA, Che Ani MF, Zakaria AD. Rectal foreign bodies: sexual gratification turned misery. Brunei Int Med J. (2020) 16:73–6.
5. Coskun A, Erkan N, Yakan S, Yıldirim M, Cengiz F. Management of rectal foreign bodies. World J Emerg Surg. (2013) 8:11. doi: 10.1186/1749-7922-8-11
6. Gan DEY, Chan KH, Veerappan P, Sun KJ, Hayati F. Rectal foreign body: A successful removal at the bedside and detailing of a stepwise management. Am J Case Rep. (2021) 17:e930967. doi: 10.12659/AJCR.930967
Keywords: foreign bodies, pneumoperitoneum, radiography, rectum, case report
Citation: Aimanan K, Lim SY, Ahmad Hamidi AJ, Chieng TH and Hayati F (2022) Case Report: Rectal Perforation Secondary to a Toothbrush in an Elderly Man. Front. Surg. 9:921843. doi: 10.3389/fsurg.2022.921843
Received: 16 April 2022; Accepted: 25 May 2022;
Published: 10 June 2022.
Edited by:
Amit Gupta, All India Institute of Medical Sciences, IndiaReviewed by:
Andee Dzulkarnaen Zakaria, Universiti Sains Malaysia, MalaysiaRuhi Fadzlyana Jailani, Universiti Sains Islam Malaysia, Malaysia
Copyright © 2022 Aimanan, Lim, Ahmad Tamidi, Chieng and Hayati. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Firdaus Hayati ZmlyZGF1c2hheWF0aUBnbWFpbC5jb20=; bV9maXJkYXVzQHVtcy5lZHUubXk=
Specialty section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
 Karthigesu Aimanan
Karthigesu Aimanan Soon Yee Lim
Soon Yee Lim Ahmad Junaidi Ahmad Hamidi1
Ahmad Junaidi Ahmad Hamidi1 Firdaus Hayati
Firdaus Hayati