- 1Department of Traumatic Orthopedics, Tianjin Hospital, Tianjin, China
- 2Department of Spine Surgery, Tianjin Hospital, Tianjin, China
- 3Department of Orthopedics, Tianjin Medical University General Hospital, Tianjin, China
- 4Department of Orthopaedics, Tianjin Hospital, Tianjin, China
Background: We performed a meta-analysis to evaluate the efficacy and safety of zoledronic acid combined with percutaneous kyphoplasty (PKP) in treating osteoporotic vertebral compression fractures (OVCFs).
Methods: Eligible scientific articles published prior to July 2020 were retrieved from the PubMed, Springer, ScienceDirect, and Cochrane Library databases. The statistical analysis was performed with RevMan 5.1.
Results: Three randomized controlled trials (RCTs) and 2 non-RCTs met the inclusion criteria. The present meta-analysis revealed that zoledronic acid combined with PKP is associated with a higher BMD, a better quality of life, less severe low back pain, and fewer additional vertebral body fractures than is percutaneous vertebral augmentation alone.
Conclusions: Compared with PKP only, zoledronic acid combined with percutaneous vertebral augmentation is beneficial for OVCFs.
Introduction
Osteoporotic vertebral compression fractures (OVCFs) are a major complication of osteoporosis and can result in severe back pain, spinal deformity, the loss of mobility, a decreased quality of life and even death (1, 2). Percutaneous kyphoplasty (PKP), introduced by Garfin et al., has been clinically justified by numerous studies as an effective treatment to quickly relieve pain, correct spinal kyphotic deformities and maintain spinal stabilization in patients with acute OVCFs with persistent and severe pain (3).
Bisphosphonates (BPs) have been confirmed to prevent bone loss and increase bone quality and density by inhibiting osteoclast-mediated bone resorption and decreasing bone turnover (4). To date, the administration of bisphosphonates to treat osteoporosis has been well-studied (5, 6). In theory, the application of anti-osteoporosis agents may improve outcomes in patients treated with PKP. In a retrospective study, Seo et al. (7) found that the administration of BPs reduced the occurrence of new fractures in patients with OVCFs treated with percutaneous vertebroplasty. Recently, several clinical studies have reported the treatment outcomes of zoledronic acid combined with PKP for OVCFs. However, whether zoledronic acid is safe and efficient when combined with PKP in treating OVCFs remains controversial. Therefore, this meta-analysis was conducted to evaluate the efficacy and safety of zoledronic acid combined with PKP in treating OVCFs by analyzing the current randomized controlled trials (RCTs) and non-RCTs.
Methods
Search Strategy
This meta-analysis was conducted in accordance with the relevant reported items for systematic reviews and meta-analyses (PRISMA) guidelines. Potentially relevant published academic articles published from the inception of the electronic databases searched to July 2020 were retrieved from the PubMed, Springer, ScienceDirect, and Cochrane Library databases. The references of the identified articles were also searched for relevant articles. None of the studies were excluded due to language restrictions. The key words used for the search were “osteoporosis,” “vertebral compression fractures,” “kyphoplasty,” and “zoledronic acid”.
Inclusion Criteria
Studies were considered eligible for inclusion if they met the following criteria: (1) the patients underwent PKP with OVCFs; (2) the intervention was the use of zoledronic acid, control group did not use zoledronic acid; (3) the outcomes included pain assessment, function assessment, BMD, bone metabolism parameters and complications; and (4) the study was a published RCT or non-RCT trial.
Exclusion Criteria
We excluded studies as follows: (1) those without a control group; (2) studies with no available full-text version; (3) studies with no available outcome data; and (4) studies of revision PKP.
Selection Criteria
Two reviewers independently screened the titles and abstracts according to the eligibility criteria. The full text of the studies that potentially met the inclusion criteria were subsequently read, and the literature was reviewed to determine suitability of final inclusion. Disagreement was resolved by consulting with a third reviewer.
Quality Assessment
The methodological quality of the RCTs was evaluated using a modification of the generic evaluation tool described in the Cochrane handbook for systematic reviews of interventions (8). The methodological quality of non-RCTs was assessed by the methodological index for non-randomized studies (MINORS) (9).
Data Extraction
The data were extracted from the included articles by two independent reviewers. When there was incomplete data, the corresponding author of study was contacted for details. The following information was extracted: the first author's name, publication year, intervening measures, follow-up term, pain assessment, function assessment, BMD, bone metabolism parameters, and complications. Other relevant parameters were also extracted from the individual studies. If trials reported incomplete data, authors were contacted for further information.
Data Analysis and Statistical Methods
RevMan 5.1 (The Cochrane Collaboration, Oxford, United Kingdom) was used to analyze the pooled data. The P-values and I2-values from the standard chi-square test were used to estimate the level of heterogeneity. When I2 > 50%, P < 0.1 was considered to indicate significant heterogeneity, and a random-effects model was used for the data analysis. When I2 < 50%, P > 0.1 was considered to indicate non-significant heterogeneity. A fixed-effects model was used for the data analysis when non-significant heterogeneity was found. Subgroup analysis was performed when significant heterogeneity was found to investigate the sources of heterogeneity. The mean differences (MDs) and 95% confidence intervals (CIs) were determined for continuous variables. The dichotomous data are expressed as the risk differences (RDs) and 95% CIs.
Results
Search Results
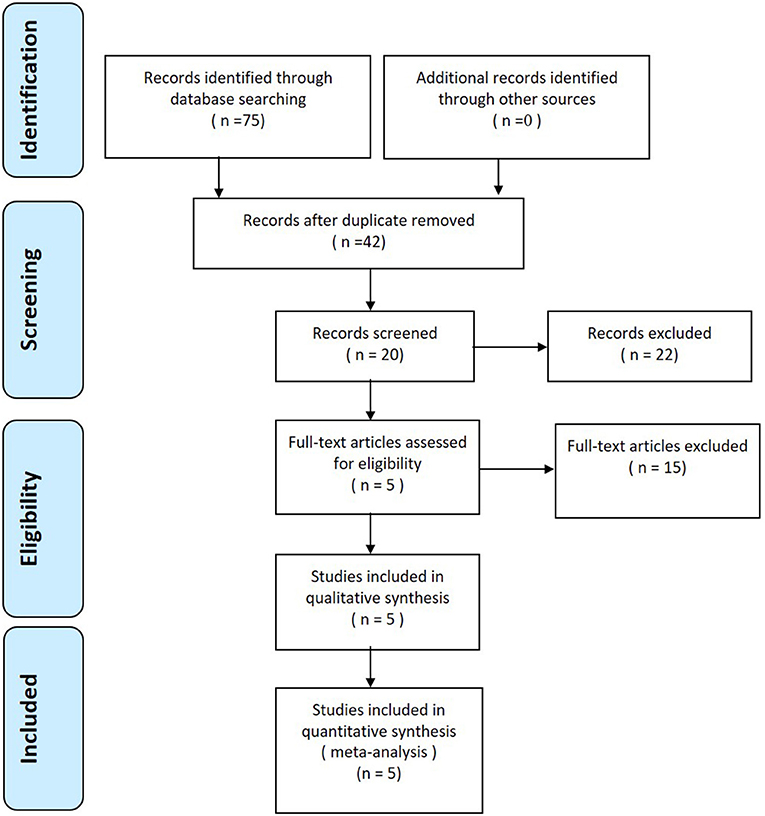
A total of 75 studies were identified as potentially relevant. After a thorough screening of the titles and abstracts, 70 reports were excluded according to the eligibility criteria. No additional studies were identified after the references were reviewed. Finally, three RCTs (10–12) and 2 non-RCTs (13, 14) met the inclusion criteria for data extraction and meta-analysis. The search process is shown in Figure 1.
Risk of Bias Assessment
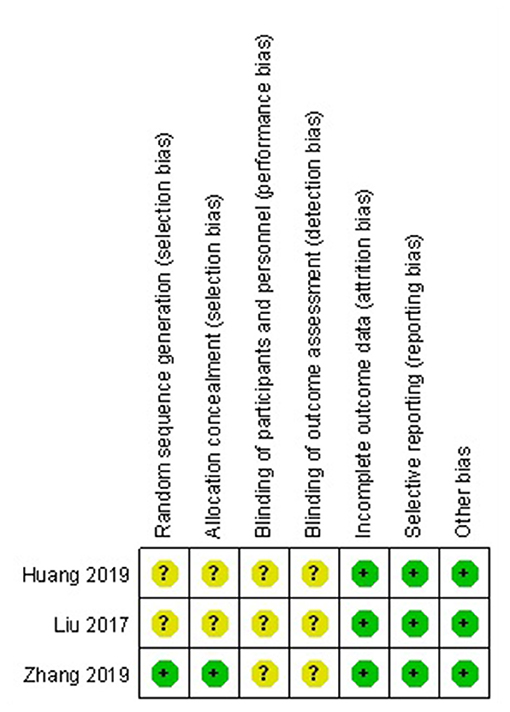
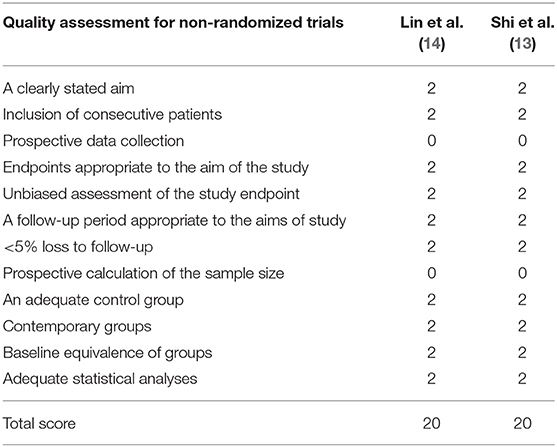
The methodological quality of RCTs was assessed according to the Cochrane handbook for systematic reviews of interventions (Figure 2). The inclusion and exclusion criteria were clearly stated in all RCTs. One RCT that was included reported adequate methodology for randomization, concealment of allocation and intent-to-treatment analysis. In addition, blinding was not described in all of the included RCTs. Unclear bias was not reported due to incomplete outcome data or selective outcomes. The MINORS score of the non-RCTs was 20. The methodological quality assessment of the non-RCTs is presented in Table 1.
Study Characteristics
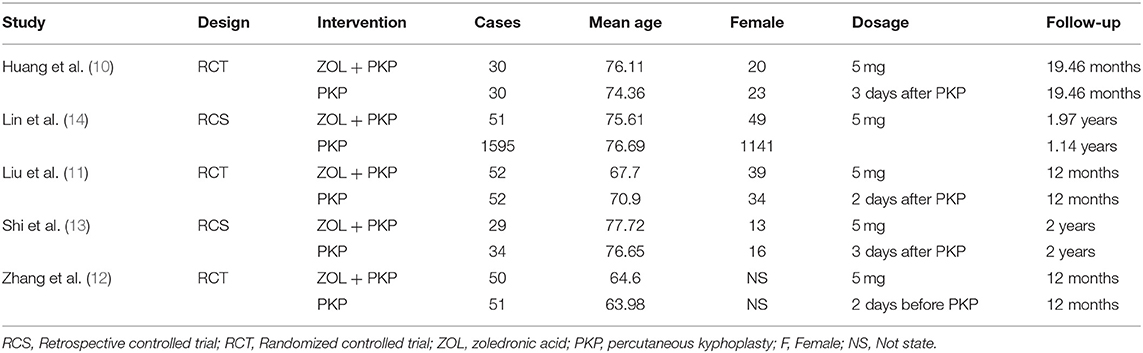
Demographic characteristics and other details of the included studies are presented in Table 2. In each study, the baseline characteristics of the two groups were similar. Zoledronic acid was used in all included studies.
Outcomes of the Meta-Analysis
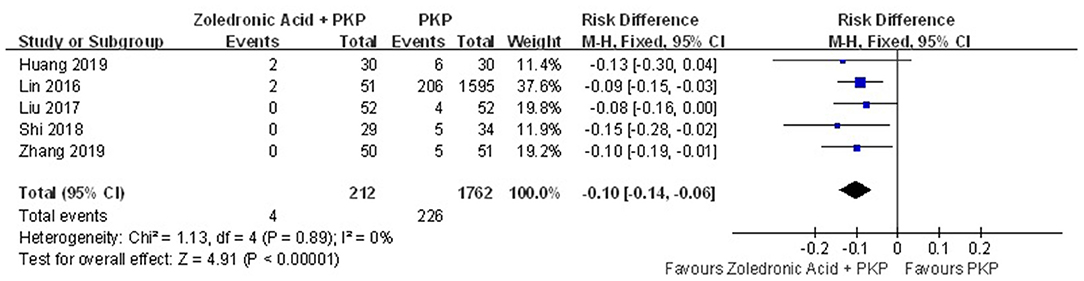
Additional Vertebral Body Fractures
Additional vertebral body fractures were assessed in five studies. The pooled results demonstrated that zoledronic acid combined with PKP was related to a significant decrease in the occurrence of additional vertebral body fractures compared with PKP alone (RD = −0.10; 95% CI, −0.14, −0.06; P < 0.00001), with no heterogeneity (n.s., I2 = 0%) (Figure 3).
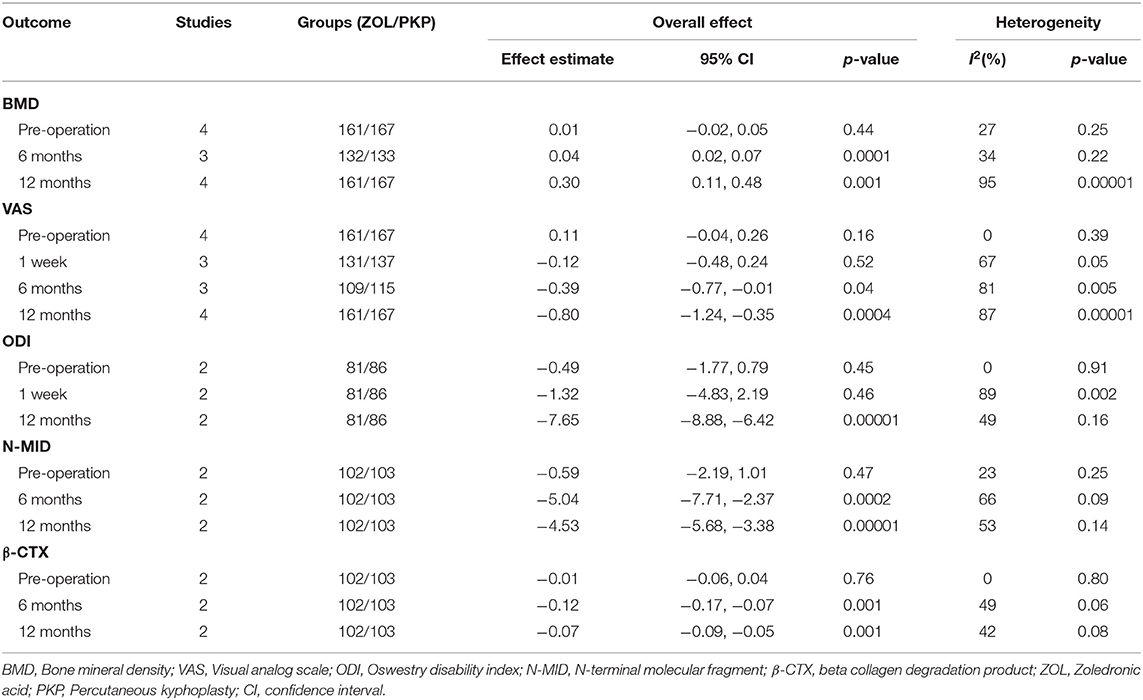
Pre-operative and Post-operative Bone Mineral Density
Pre-operative and post-operative BMD were reported in four studies. For pre-operative BMD, there was no significant difference between the two groups (MD = 0.01; 95% CI, −0.02, 0.05; P = 0.44), with no heterogeneity (n.s., I2 = 27%) (Table 3). The pooled results demonstrated that compared with PKP alone, zoledronic acid combined with PKP significantly improved BMD at the 6- and 12-month follow-ups (Table 3).
Pre-operative and Post-operative Visual Analog Scale
The pre-operative and post-operative VAS scores were documented in four studies. For the pre-operative and post-operative 1-week VAS scores, there were no significant differences between the two groups (Table 3). The pooled results demonstrated that compared with PKP alone, zoledronic acid combined with PKP significantly decreased the VAS score at the 6- and 12-month follow-ups (Table 3).
Pre-operative and Post-operative Oswestry Disability Index
The pre-operative and post-operative ODI scores were provided in two trials. For the pre-operative and post-operative 1-week ODI scores, there were no significant differences between the two groups (Table 3). The pooled results demonstrated that compared with PKP alone, zoledronic acid combined with PKP significantly improved the ODI score at the 12-month follow-up (Table 3).
Pre-operative and Post-operative N-Terminal Molecular Fragment
The pre-operative and post-operative N-MID values were available in two studies. For the pre-operative N-MID values, there was no significant difference between the two groups (Table 3). The pooled results demonstrated that compared with PKP alone, zoledronic acid combined with PKP significantly improved N-MID at the 6- and 12-month follow-ups (Table 3).
Pre-operative and Post-operative Beta Collagen Degradation Product (β-CTX)
Two articles reported the pre-operative and post-operative β-CTX values. For the pre-operative β-CTX values, there was no significant difference between the two groups (Table 3). The pooled results demonstrated that compared with PKP alone, zoledronic acid combined with PKP significantly improved β-CTX at the 6- and 12-month follow-ups (Table 3).
Discussion
Our meta-analysis included five studies. The purpose of our meta-analysis was to evaluate the efficacy and safety of zoledronic acid combined with PKP in the treatment of OVCFs. In this analysis of studies, we found that compared with PKP alone, zoledronic acid combined with PKP decreased the incidence of additional vertebral body fractures, relieved low back pain, increased BMD and improved quality of life. To our knowledge, the present study is the first quantitative meta-analysis to evaluate the efficacy and safety of zoledronic acid combined with PKP in the treatment of OVCFs.
BPs have been confirmed to prevent bone loss and increase bone quality and density by inhibiting osteoclast-mediated bone resorption (4, 15). Zoledronic acid is administered by annual intravenous infusions (16). Therefore, zoledronic acid is the most commonly used and powerful BP in clinical practice (6). N-MID and β-CTX, which are bone metabolism markers, have been widely used in the diagnosis of osteoporosis, the monitoring of the effects of anti-bone resorption therapy and the prediction of osteoporotic fracture risk (17, 18). The pooled results suggest that zoledronic acid significantly decreases the post-operative levels of N-MID and β-CTX BMD at 6 and 12 months. Zoledronic acid can effectively decrease bone absorption.
During PKP, a balloon is percutaneously inflated in the fractured vertebral body to restore the height and kyphosis angle of the fractured vertebra. Then, bone cement is injected into the fractured vertebral body to maintain vertebral strength and stiffness (19). However, several studies have shown that vertebral augmentation (the injection of bone cement) leads to increased mechanical pressure on vertebrae adjacent to the region of PKP and may cause an additional vertebral body fracture (20–22). On the other hand, Rho et al. found that the major risk factors for new adjacent OVCFs include the progression of osteoporosis after the PKP procedure (23). The administration of BPs as anti-osteoporotic drugs has been confirmed to effectively prevent bone loss and increase bone quality and density. Several studies have verified that BPs decrease the risk of vertebral and non-vertebral fractures (5, 24). The present meta-analysis revealed that zoledronic acid not only significantly improved post-operative BMD at 6 and 12 months but also decreased the incidence of additional vertebral body fractures. The administration of zoledronic acid is beneficial for OVCFs treated with PKP.
Post-operative function and pain determine the overall efficacy of spinal surgery. The present meta-analysis suggests that zoledronic acid combined with PKP significantly improved the ODI score at the 12-month follow-up (MD = −7.56, P = 0.00001). The VAS score is a patient-reported score and has been used extensively in previous studies to assess patient pain following spinal surgery. The pooled data showed that BPs combined with PKP decreased the VAS score for back pain at the 6- and 12-month follow-ups. This small MD was thus quite unlikely to be the actual difference between the two groups. We should consider these factors when analyzing the present findings.
Several potential limitations should be noted. (1) Only three RCTs and 2 non-RCTs were included, and the sample size of all the studies was relatively small; (2) the suboptimal methodological quality of the included studies and insufficient outcomes may weaken our analysis; (3) we failed to perform subgroup analysis and determine the source of heterogeneity for the limited number of studies that were included.
Conclusion
Among patients with OVCFs, zoledronic acid combined with PKP was associated with a higher BMD, a better quality of life, less severe low back pain, and fewer additional vertebral body fractures than was PKP alone.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the authors of the included studies.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2021.668551/full#supplementary-material
References
1. Cauley JA, Chalhoub D, Kassem AM, Fuleihan GEH. Geographic and ethnic disparities in osteoporotic fractures. Nat Rev Endocrinol. (2014) 10:338–51. doi: 10.1038/nrendo.2014.51
2. Kung AWC. Epidemiology and diagnostic approaches to vertebral fractures in Asia. J Bone Miner Metab. (2004) 22:170–5. doi: 10.1007/s00774-003-0467-x
3. Garfin SR, Yuan HA, Reiley MA. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine. (2001) 26:1511–5. doi: 10.1097/00007632-200107150-00002
4. Russell RGG, Watts NB, Ebetino FH, Rogers MJ. Mechanisms of action of bisphosphonates: similarities and differences and their potential influence on clinical efficacy. Osteoporos Int. (2008) 19:733–59. doi: 10.1007/s00198-007-0540-8
5. Byun JH, Jang S, Lee S, Park S, Yoon HK, Yoon BH, et al. The efficacy of bisphosphonates for prevention of osteoporotic fracture: an update meta-analysis. J Bone Metab. (2017) 24:37–49. doi: 10.11005/jbm.2017.24.1.37
6. Spiegel R, Nawroth PP, Kasperk C. The effect of zoledronic acid on the fracture risk in men with osteoporosis. J Endocrinol Invest. (2014) 37:229–32. doi: 10.1007/s40618-013-0038-5
7. Seo DH, Oh SH, Yoon KW, Ko JH, Kim YJ, Lee JY. Risk factors of new adjacent compression fracture after percutaneous vertebroplasty: effectiveness of bisphosphonate in osteoporotic or osteopenic elderly patients. Korean J Neurotrauma. (2014) 10:86–91. doi: 10.13004/kjnt.2014.10.2.86
8. Handoll HH, Gillespie WJ, Gillespie LD, Madhok R. The cochrane collaboration: a leading role in producing reliable evidence to inform healthcare decisions in musculoskeletal trauma and disorders. Indian J Orthop. (2008) 42:247–51. doi: 10.4103/0019-5413.41849
9. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. (2003) 73:712–6. doi: 10.1046/j.1445-2197.2003.02748.x
10. Huang ZF, Xiao SX, Liu K, Xiong W. Effectiveness analysis of percutaneous kyphoplasty combined with zoledronic acid in treatment of primary osteoporotic vertebral compression fractures. Pain Phys. (2019) 22:63–8. doi: 10.36076/ppj/2019.22.63
11. Liu B, Gan F, Ge Y, Yu H. Clinical Efficacy analysis of percutaneous kyphoplasty combined with zoledronic acid in the treatment and prevention of osteoporotic vertebral compression fractures. J Invest Surg. (2018) 31:425–30. doi: 10.1080/08941939.2017.1339151
12. Zhang J, Zhang T, Xu X, Cai Q, Zhao D. Zoledronic acid combined with percutaneous kyphoplasty in the treatment of osteoporotic compression fracture in a single T12 or L1 vertebral body in postmenopausal women. Osteoporos Int. (2019) 30:1475–80. doi: 10.1007/s00198-019-04896-w
13. Shi C, Zhang M, Cheng AY, Huang ZF. Percutaneous kyphoplasty combined with zoledronic acid infusion in the treatment of osteoporotic thoracolumbar fractures in the elderly. Clin Intervent Aging. (2018) 13:853–61. doi: 10.2147/CIA.S146871
14. Lin TY, Yang SC, Tsai TT, Lai PL, Fu TS, Niu CC, et al. Correlation between zoledronic acid infusion and repeat vertebroplasty surgery in osteoporotic patients. Curr Med Res Opin. (2016) 32:921–7. doi: 10.1185/03007995.2016.1151775
15. Xue D, Li F, Chen G, Yan S, Pan Z. Do bisphosphonates affect bone healing? A meta-analysis of randomized controlled trials. J Orthop Surg Res. (2014) 9:45. doi: 10.1186/1749-799X-9-45
16. Dhillon S. Zoledronic acid (Reclast®, Aclasta®): a review in osteoporosis. Drugs. (2016) 76:1683–97. doi: 10.1007/s40265-016-0662-4
17. Vasikaran S, Eastell R, Bruyère O, Foldes AJ, Garnero P, Griesmacher A, et al. Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards. Osteoporos Int. (2011) 22:391−420. doi: 10.1007/s00198-010-1501-1
18. Schousboe JT, Paudel ML, Taylor BC, Kats AM, Virnig BA, Dowd BE, et al. Pre-fracture individual characteristics associated with high total health care costs after hip fracture. Osteoporos Int. (2017) 28:889–99. doi: 10.1007/s00198-016-3803-4
19. Chandra RV, Yoo AJ, Hirsch JA. Vertebral augmentation: update on safety, efficacy, cost effectiveness and increased survival? Pain Phys. (2013) 16:309–20. doi: 10.36076/ppj.2013/16/309
20. Berlemann U, Ferguson SJ, Nolte LP, Heini PF. Adjacent vertebral failure after vertebroplasty. A biomechanical investigation. J Bone Joint Surg Br. (2002) 84:748–52. doi: 10.1302/0301-620X.84B5.0840748
21. Polikeit A, Nolte LP, Ferguson SJ. The effect of cement augmentation on the load transfer in an osteoporotic functional spinal unit: finite-element analysis. Spine. (2003) 28:991–6. doi: 10.1097/01.BRS.0000061987.71624.17
22. Villarraga ML, Bellezza AJ, Harrigan TP, Cripton PA, Kurtz SM, Edidin AA. The biomechanical effects of kyphoplasty on treated and adjacent nontreated vertebral bodies. J Spinal Disord Tech. (2005) 18:84–91. doi: 10.1097/01.bsd.0000138694.56012.ce
23. Rho YJ, Choe WJ, Chun YI. Risk factors predicting the new symptomatic vertebral compression fractures after percutaneous vertebroplasty or kyphoplasty. Eur Spine J. (2012) 21:905–11. doi: 10.1007/s00586-011-2099-5
Keywords: zoledronic acid, osteoporosis, vertebral compression fractures, percutaneous kyphoplasty, meta-analysis
Citation: Tian P, Liu Y, Li Z-j, Xu G-j and Ma X-l (2021) Zoledronic Acid in Osteoporotic Vertebral Compression Fractures Treated With Percutaneous Kyphoplasty: A Meta-Analysis. Front. Surg. 8:668551. doi: 10.3389/fsurg.2021.668551
Received: 16 February 2021; Accepted: 23 April 2021;
Published: 21 May 2021.
Edited by:
Emmanouil Liodakis, Hannover Medical School, GermanyReviewed by:
Sebastian Decker, Hannover Medical School, GermanyXuesong Zhu, The First Affiliated Hospital of Soochow University, China
Copyright © 2021 Tian, Liu, Li, Xu and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin-long Ma, bWF4aW5sb25nODY4Njg2QDE2My5jb20=
†These authors have contributed equally to this work
 Peng Tian
Peng Tian Yue Liu2†
Yue Liu2† Xin-long Ma
Xin-long Ma