
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 18 January 2024
Sec. Digital Public Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1294183
This article is part of the Research Topic Internet of Things (IoT) and Public Health: An Artificial Intelligence Perspective View all 9 articles
A correction has been applied to this article in:
Addendum: Validation of the digital health literacy assessment among the university students in China
 Limei Nie1,2,3
Limei Nie1,2,3 Jiajia Zhao1,2,3
Jiajia Zhao1,2,3 Lutong Pan1,2,3
Lutong Pan1,2,3 Mingli Pang1,2,3
Mingli Pang1,2,3 Jieru Wang1,2,3
Jieru Wang1,2,3 Yue Zhou4
Yue Zhou4 Rui Chen1,2,3
Rui Chen1,2,3 Hui Liu1,2,3
Hui Liu1,2,3 Xixing Xu1,2,3
Xixing Xu1,2,3 Baochen Su1,2,3
Baochen Su1,2,3 Fanlei Kong1,2,3*
Fanlei Kong1,2,3*Purpose: With the development of the internet, digital health literacy (DHL) has become increasingly important for managing health. Consequently, various digital health literacy scales have been created for different groups. The purpose of this study was to verify the reliability and validity of the simplified Chinese version of the Digital Health Literacy Assessment (DHLA) scale among university students in China.
Method: Snowball sampling was used to recruit the participants via an online platform (Wenjuan.com), and finally 304 university students were included in the survey. Demographic information and the status of DHL were collected through the online questionnaire. Cronbach’s alpha and split-half reliability were used to test the internal consistency of the scale, while the structural validity was verified by exploratory factor analysis and confirmatory factor analysis. Additionally, the convergence of the scale was tested by composite reliability (CR) and average variance extracted (AVE).
Result: Two dimensions were generated from 10 entries in the scale, named Self-rated Digital Health Literacy and Trust Degree of Online Health Information, respectively. The Cronbach’s alpha and split-half reliability of the total scale were 0.912 and 0.828, while the Cronbach’s alpha of the two dimensions were 0.913 and 0.830, respectively. The structural validity-related indexes of the scale met the standards (RMSEA = 0.079, GFI = 0.943, AGFI = 0.902, CFI = 0.971). In each dimension, the CR and AVE also reached critical values (CR > 0.7 and AVE > 0.5).
Conclusion: The scale had high reliability and validity, indicating the simplified Chinese DHLA scale could be used to evaluate the DHL of university students in China.
The rapid development of information technology has made the internet an accessible resource for people to obtain health information (1). The size of China’s internet users is 1.067 billion and the internet penetration rate has reached 75.6% in 2023 (2), of which, the internet usage rate of university students has reached nearly 100% (3). University students use online health information to address or solve health problems and communicate about their health issues online (4), yet health misinformation is rife on social media (5). As a vulnerable group, university students may lack knowledge and skills for seeking and evaluating health information from the internet (6), which makes the research on the improvement of digital health literacy (DHL) among university students more and more important.
In 2006, Norman and Skinner first defined electronic health literacy (eHL) as the ability to read, use computers, search for information, understand health information, and put it into context (7). With the innovative development of digital technology, interactivity on the Web has become more and more important, the concept of DHL was then introduced in 2021 (8), where DHL refers to the skills to search, select, evaluate, and apply online health information and healthcare-related digital applications (9, 10). Compared to eHL’s focus solely on the ability to read and send information online, DHL further includes the skills of writing and communicating health-related messages online; that is how DHL differs from eHL and emphasizes people’s interactivity with the internet (10, 11).
With the digitization of health care and the wide availability of Web-based applications, DHL is an essential skill to be mastered in the digital age, which is an important determinant of health (12) and has a profound impact on an individual’s health (13). Existing research has shown that DHL could alleviate anxiety related to both physical health and the usage of digital technology among older adults (14). Additionally, DHL was also found to be related to the health status of patients with cancer (15) and cardiovascular disease (16). Moreover, DHL could enhance patient autonomy and improve the doctor–patient relationship by ensuring that patients use online health information correctly (17, 18). Digital technologies could increase the transparency of health information, yet could also hinder access to health information due to low DHL (19). Therefore, it is crucial to use scales to assess the DHL of the population promptly and implement intervention measures for people with low literacy levels.
However, few studies have focused on the assessment tools of DHL currently (20). The tools for assessing DHL include the Digital Health Literacy Assessment (DHLA) (21), Digital Health Literacy Instrument (DHLI) (10), Digital Health Technology Literacy Assessment Questionnaire (DHTL-AQ) (22), and Digital Health Literacy Assessment Scale for Community-dwelling older adults (23). The traditional Chinese version of the DHLA was developed by Peggy Liu based on the eHealth Literacy Scale (eHEALS), which has 10 items (three dimensions) and good reliability and validity in Taiwan Province, China. Moreover, a strong correlation between the total score of the DHLA and DHLI also indicated that the DHLA could be used to measure DHL (21). To date, no research has ever tested the validation of the DHLA among the population in mainland China; considering the vulnerability of university students and their frequent use of the internet, this study chose them as the target population. Thus, the purpose of this study was to verify the reliability and validity of the simplified Chinese DHLA among university students in mainland China.
This study utilized a cross-sectional correlational design using a self-assessment questionnaire. Snowball sampling was used to recruit the participants. An online questionnaire was created from an online platform (Wenjuan.com) and distributed to university students in China through WeChat to collect the data. The survey began on 8 September 2022 and ended on 17 September 2022. Ultimately, a total of 304 participants from nine Chinese provinces were selected and interviewed. However, 22 participants were excluded as they answered their questionnaires incorrectly or incompletely, including those with incomplete answers (five questionnaires), took less than 3 min to complete the questionnaire (11 questionnaires), or their age was under 10 years (six questionnaires). Ultimately, a total of 282 participants were finally included in the data analysis.
Based on the traditional Chinese version of the DHLA, the simplified Chinese version of the DHLA was created and used to assess the DHL of university students in China. The original scale had 10 questions and was divided into three dimensions, with each question being answered using a 5-point Likert scale. The first to sixth questions belonged to the first dimension and were entitled Self-rated digital health literacy, with response styles ranging from 1 (very bad) to 5 (very good). The seventh to ninth questions belonged to the second dimension and were named as the Trust degree of online health information. The tenth question belonged to the third dimension and was named as the Trust degree of online traditional Chinese medicine health information. The options for the seventh to tenth question ranged from 1 (very unconvinced) to 5 (very convinced).
Besides the DHLA, the questionnaire also included: (1) sociodemographic characteristics of the participants: sex, age, educational level, and residential area; and (2) eHEALS.
Descriptive analyses, Chi-square test, and ANOVA were conducted to explore the characteristics and distribution differences between male and female university students. A p-value <0.01 denotes statistical significance. The critical indicators of the quality of a measuring instrument are reliability and validity (24). Depending on the type of questionnaire, some validity tests are mandatory to apply (such as the internal consistency reliability, construct validity, or construct convergent validity) (25). In this study, internal consistency reliability, construct validity, convergent validity, and criterion validity were chosen to verify the quality of the DHLA. All analyses were performed using the Statistical Package for Social Sciences (SPSS, IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. IBM Corp., Armonk, NY, United States).
The study used the Kolmogorov–Smirnov (KS) test which is a well-known non-parametric goodness-of-fit test to check whether the scale scores conformed to the normal distribution (26). Floor or ceiling effects are considered to be present if more than 15% of respondents achieved the lowest or highest score, respectively (27). The items of the scale were judged comprehensively according to the screening criteria of item analysis: item–scale correlation ≥0.4 and Cronbach’s α does not increase if the item deleted. (28).
The reliability of the DHLA was tested using Cronbach’s alpha and split-half reliability. The Cronbach’s alpha α >0.8 (29) and split-half reliability >0.85 (30) indicated good internal consistency of the scale in this study. The Spearman–Brown formula was then used to analyze the split-half reliability to compare with Cronbach’s alpha. When the Cronbach’s alpha α >0.8 and the value of split-half reliability >0.85, the scale was prove to have good reliability. (31).
The Kaiser-Meyer-Olkin (KMO) measure and Bartlett’s test were used to test the suitability of the data for the exploratory factor analysis (EFA). This study used a KMO of ≥0.8 and a significant Bartlett’s test p < 0.05 as empirical evidence of a sufficiently large sample size for factor analysis (32, 33).
Since the DHLA is a multiple factor scale, a confirmatory factor analysis (CFA) was then conducted to investigate its construct validity by factor structure model (34). CFA is an old and mature method of confirming the number of factors in a scale to test how well the data fits the proposed model (35). A χ2/df < 3.00, root mean square error of approximation (RMSEA) < 0.08, goodness-of-fit index (GFI) > 0.900, adjusted goodness of fit index (AGFI) > 0.900, and comparative fit index (CFI) > 0.900 indicated a reasonable fit (36).
Convergent validity is the illustration of substantial and significant correlation between different scales designed to assess a common construct, which is a subset of construct validity and regarded as a core component of the validity in a test (37). To test the correlation between factors of the DHLA, the average variance extracted (AVE) and composite reliability (CR) were used to evaluate the convergent validity of the scale. The AVE > 0.5 and CR > 0.7 indicated the convergent validity of the scale is acceptable (38).
Criterion validity can reflect the degree of agreement between a measured score and an external criterion. Finding the relevant, valid, objective, uncontaminated, and practical criterion and measuring the criterion accurately is the basis of the test (39). This study chose eHEALS which is the most commonly used method to assess DHL and assess whether individuals can utilize e-healthcare resources actively (40), and the correlation method was used to estimate the criterion validity. The larger the correlation coefficient r, the higher the correlation degree between the score and criterion, and the scale can better measure or predict the content of the study.
All the participants provided informed consent for inclusion in the study. This study was approved by the Shandong University Institutional Ethics Committee (task no. LL20220425).
Table 1 shows the demographic characteristics of the participants. The majority of them (97.5%) were 19 years old or older, with 203 (72.0%) being female and 79 (28.0%) male. In addition, 67% (189) of the students were living in cities, and almost half (53.2%) of the participants were pursuing undergraduate programs. There were no statistically significant differences (P>0.05) between the male and female university students in age, residential area, and educational level.
The total score on the scale ranges from 10 to 50 points. Through exploratory analysis, the Kolmogorov–Smirnov test was significant (p < 0.05), indicating that the scores were not normally distributed. In this study, 13 (4.6%) subjects scored the highest score and 0 subjects scored the lowest (both under 15%) indicating that the DHLA had no significant floor or ceiling effect. Table 2 shows the item analysis of the scale. Cronbach’s α remained hardly increased when any one of the items was deleted from the calculation except for item 10. Meanwhile, the item–total correlation coefficients were high, with individual item values ranging from 0.585 to 0.843 (p < 0.01 for each one of the correlations).
The results of the reliability tests for the total and two-dimensional scores of the DHLA are displayed in Table 2. In this study, the α of all the 10 items was 0.912, and the split-half reliability was 0.828, both of which were higher than the standard value of 0.8. Additionally, the α for each dimension was above 0.8.
In this study, KMO = 0.906, and Bartlett’s test significance level was p < 0.01. The exploratory factor analysis of the 10 items of the DHLA showed that it was suitable for factor analysis. The principal component analysis method was used to extract common factors with an eigenvalue >1 by the maximum variance method. Considered together with the result of the steep slope map test, it was more appropriate to retain the two factors, which was different from the results of the original scale with three factors in Taiwan on the factor classification. After analyzing various dimensionality reduction methods, most of the data results showed that factor 2 (network information trust) and factor 3 (folk information trust) of the original scale should be combined as one factor (named “network health information trust”) according to the database used in this study. Ultimately, there were two dimensions in the whole scale, with the first to sixth questions entitled “Self-rated Digital Health Literacy” (shorted for SRDHL), and the seventh to tenth questions entitled “Trust Degree of Online Health Information” (shorted for TDOHI). The dimensionality factor loading ranged from 0.621 to 0.884. To further verify the scale structure validity, AMOS software was used for two-factor structure validation analysis. According to the correction index, a total of two covariant relations between errors were added and the modified model fitting indexes all reached the reference standard, which indicated that the model was well-fitted. Multiple criteria in the CFA analysis showed a good fit to the two-factor structural model: RMSEA = 0.079, GFI = 0.943, AGFI = 0.902, and CFI = 0.971 (as shown in Figure 1).
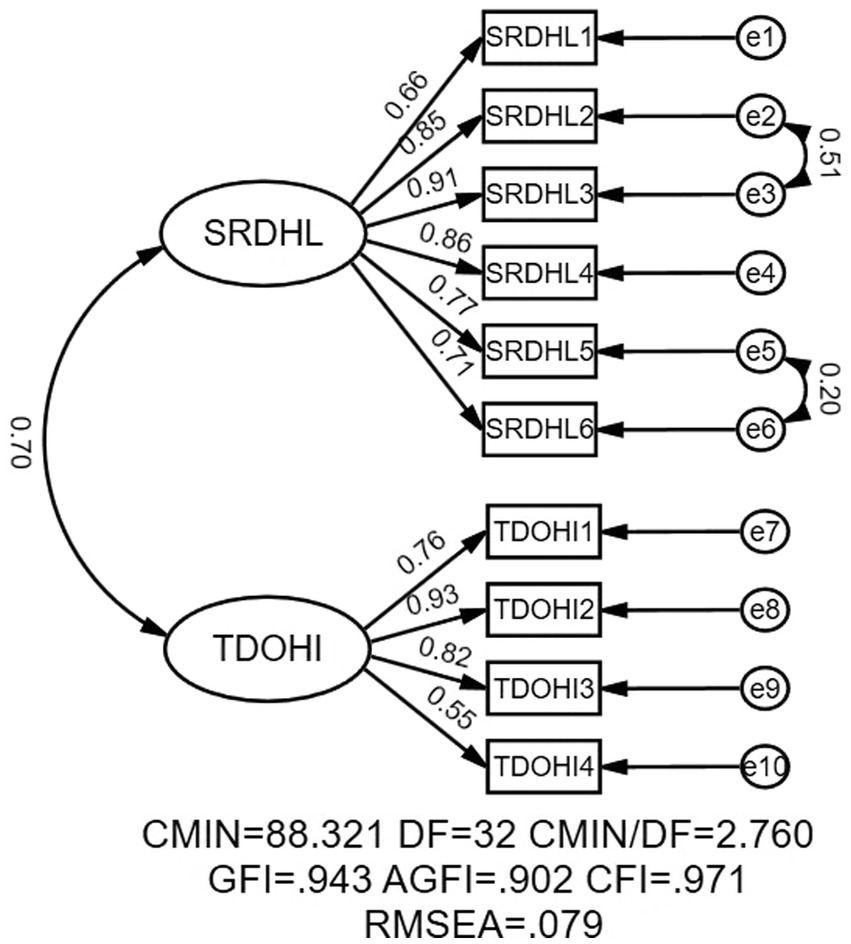
Figure 1. The measurement model. SRDHL, Self-rated Digital Health Literacy; TDOHI, Trust Degree of Online Health Information.
Table 3 shows that the CR and AVE values were conducted to examine the convergent validity of SRDHL and TDOHI. Both dimensions met the standard AVE > 0.50 and CR > 0.70. The Chinese version of the DHLA further proved the convergence efficiency. The values of standardized factor load were also obtained. Factor loading of each item in the scale was greater than 0.5 (Table 4).
To verify the criterion validity of the DHLA, its correlation with the eHEALS was examined because eHEALS is also a commonly used method to assess DHL at present. The findings revealed a statistically significant positive correlation between the two scales (r = 0.720, p < 0.01; Table 5).
One-way ANOVA between male and female students on the total score and the scores of both two dimensions of the DHLA were also conducted. The scores for female students were lower than those for male students on both the total score (37.2 ± 6.7 vs. 38.5 ± 7.5) and the scores of each of the two dimensions (23.6 ± 4.1 vs. 24.0 ± 4.7 for SRDHL, 13.6 ± 3.3 vs. 14.5 ± 3.4 for TDOHI). The dimension with the largest difference in scores was the total score. Moreover, there were no significant differences between male and female students in both the total and individual scores for the two dimensions (Table 6).
To the utmost of the knowledge of the authors, there was no standardized assessment to measure DHL which included interactive skills (41). This study investigated the validation of the simplified Chinese version of the DHLA which consists of 10 items from two dimensions among the university students in terms of Cronbach’s alpha, split-half reliability, structural validity, convergent validity, and criterion validity. The results showed that it was applicable for evaluating the DHL of the university students in mainland China, with good internal consistency and acceptable model fit. This study may provide a useful tool for assessing DHL and further conducting interventions for the target individuals or groups in the future.
The DHLA had a good internal consistency reliability, which was consistent with the original study (21). The value of Cronbach’s alpha in this study was 0.912, which was higher than the original study’s 0.87. In detail, the values of Cronbach’s alpha of the two dimensions (items 1–6, items 7–10) were 0.913 and 0.830, respectively, while the split-half reliability of the scale was 0.828.
The results of the KMO and Bartlett’s tests showed that the DHLA was suitable for factor analysis. However, the attribution of DHLA factors in the simplified Chinese version was inconsistent with the expected original version of the DHLA scale. Through the EFA, this study found that it was reasonable to retain two factors, which was different from the original scale with three factors. Moreover, the CFA results showed that the scale structure validity of the two dimensions and the degree of model fitting were acceptable. CFA used in this study could disprove the models or hypotheses effectively yet the results may also indicate potential adjustments that should be studied further in future analyses (42). All the fit indexes in the CFA were within the acceptable range which showed that the internal structure of the scale was relatively stable among the university students. It may be related to the difference in the meaning of “folk prescriptions” in the context of Taiwan Province and mainland China (43).
Compared to the original study, this study added convergence validity that could test the degree of correlation between items that belonged to the same variable (44). The standardized factor loadings of each item was more than 0.5. The CR of the two dimensions of the DHLA were both more than 0.70 and the AVE were both more than 0.50, indicating that the items belonging to different dimensions were highly correlated and each dimension could evaluate the content of interest. The correlation coefficient of criterion validity (r) was 0.720 (p < 0.01) indicating that the DHLA could measure DHL accurately.
The results of this study also showed that the average DHLA score of male students was higher than that of female students, but there was no statistically significant correlation between DHLA score and sex. Previous studies have shown inconclusive evidence regarding whether sex was statistically significantly correlated with DHL (45–47).
The study had some limitations. Firstly, due to the COVID-19 pandemic, the survey was conducted online using snowball sampling, which may increase the possibility of sampling bias and selection bias. Students who had no access to the internet or missed the survey period could not participate in the data collection. Secondly, this study collected information among the university students who generally had higher education levels and had more exposure to the internet, which may have an impact on the results of the DHLA. Future studies should include more age groups and education levels to eliminate this limitation. Thirdly, due to the geographical constraints and cultural differences, whether the DHLA scale could be extended to other countries and regions remains to be verified.
This study is the first to use the simplified Chinese DHLA to evaluate DHL among Chinese university students, while the high reliability and validity of the scale indicated it was acceptable as a new measurement tool to assess an individual’s DHL. Future research should attempt to examine the acceptability of this instrument in other regions and among different populations to obtain wider applications.
Under reasonable requirements, the data and material of this study can be obtained from the corresponding author.
The studies involving humans were approved by Shandong University Institutional Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
LN: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Software, Validation, Writing – original draft. JZ: Conceptualization, Methodology, Writing – review & editing. LP: Formal analysis, Investigation, Writing – review & editing. MP: Software, Supervision, Writing – review & editing. JW: Methodology, Project administration, Resources, Software, Writing – review & editing. YZ: Software, Supervision, Writing – review & editing. RC: Resources, Validation, Visualization, Writing – review & editing. HL: Conceptualization, Data curation, Formal analysis, Writing – review & editing. XX: Conceptualization, Visualization, Writing – review & editing. BS: Conceptualization, Writing – review & editing. FK: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported and funded by the National Natural Science Foundation of China (No. 71804094) and Fundamental Research Funds for the Central Universities (No. 2022KJGL01).
The research team greatly appreciates the funding support and the research participants for their cooperation and support. The authors are grateful that Insha Yousuf Ellahie conducted the English language proofreading of the revised manuscript; Jiajia Li and Shixue Li gave many valuable suggestions on the revision of manuscript during the peer review procedure.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Bujnowska-Fedak, MM, Waligóra, J, and Mastalerz-Migas, A. The internet as a source of health information and services. Adv Exp Med Biol. (2019) 1211:1–16. doi: 10.1007/5584_2019_396
2. China Internet Network Information Center. The 51st statistical report on China's internet development. China Internet (2023) 51:23.
4. Escoffery, C, Miner, KR, Adame, DD, Butler, S, McCormick, L, and Mendell, E. Internet use for health information among college students. J Am Coll Health. (2005) 53:183–8. doi: 10.3200/jach.53.4.183-188
5. Swire-Thompson, B, and Lazer, D. Public health and online misinformation: challenges and recommendations. Annu Rev Public Health. (2020) 41:433–51. doi: 10.1146/annurev-publhealth-040119-094127
6. Stellefson, M, Hanik, B, Chaney, B, Chaney, D, Tennant, B, and Chavarria, EA. eHealth literacy among college students: a systematic review with implications for eHealth education. J Med Internet Res. (2011) 13:74. doi: 10.2196/jmir.1703
7. Norman, CD, and Skinner, HA. eHEALS: the eHealth literacy scale. J Med Internet Res. (2006) 8:74. doi: 10.2196/jmir.8.4.e27
8. Mein, E, Fuentes, B, Soto Más, F, and Muro, A. Incorporating digital health literacy into adult ESL education on the US-Mexico border. Rhetor Prof Commun Glob. (2012) 3:162–74.
9. Lee, J-A, Choi, M, Lee, SA, and Jiang, N. Effective behavioral intervention strategies using mobile health applications for chronic disease management: a systematic review. BMC Med Inform Decis Mak. (2018) 18:12. doi: 10.1186/s12911-018-0591-0
10. van der Vaart, R, and Drossaert, C. Development of the digital health literacy instrument: measuring a broad Spectrum of health 1.0 and health 2.0 skills. J Med Internet Res. (2017) 19:e27. doi: 10.2196/jmir.6709
11. Bittlingmayer, UH, Dadaczynski, K, Sahrai, D, van den Broucke, S, and Okan, O. Digital health literacy-conceptual contextualization, measurement, and promotion. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. (2020) 63:176–84. doi: 10.1007/s00103-019-03087-6
12. van Kessel, R, Wong, BLH, Clemens, T, and Brand, H. Digital health literacy as a super determinant of health: more than simply the sum of its parts. Internet Interv. (2022) 27:100500. doi: 10.1016/j.invent.2022.100500
13. Dong, Q, Liu, T, Liu, R, Yang, H, and Liu, C. Effectiveness of digital health literacy interventions in older adults: single-arm Meta-analysis. J Med Internet Res. (2023) 25:e48166. doi: 10.2196/48166
14. Williams, V. Digital health literacy and resolution of anxiety in the elderly. J South China Normal University (social science edition). (2022) 4:72-83+206.
15. Kemp, E, Trigg, J, Beatty, L, Christensen, C, Dhillon, HM, Maeder, A, et al. Health literacy, digital health literacy and the implementation of digital health technologies in cancer care: the need for a strategic approach. Health Promot J Austr. (2021) 32:104–14. doi: 10.1002/hpja.387
16. Dunn, P, and Conard, S. Digital health literacy in cardiovascular research. Int J Cardiol. (2018) 269:274–5. doi: 10.1016/j.ijcard.2018.07.011
17. Li, X, and Liu, Q. Social media use, eHealth literacy, disease knowledge, and preventive behaviors in the COVID-19 pandemic: cross-sectional study on Chinese netizens. J Med Internet Res. (2020) 22:e19684. doi: 10.2196/19684
18. Heiman, H, Keinki, C, and Huebner, J. EHealth literacy in patients with cancer and their usage of web-based information. J Cancer Res Clin Oncol. (2018) 144:1843–50. doi: 10.1007/s00432-018-2703-8
19. Dunn, P, and Hazzard, E. Technology approaches to digital health literacy. Int J Cardiol. (2019) 293:294–6. doi: 10.1016/j.ijcard.2019.06.039
20. Lee, J, Lee, E-H, and Chae, D. eHealth literacy instruments: systematic review of measurement properties. J Med Internet Res. (2021) 23:e30644. doi: 10.2196/30644
21. Liu, P, Yeh, L-L, Wang, J-Y, and Lee, S-T. Relationship between levels of digital health literacy based on the Taiwan digital health literacy assessment and accurate assessment of online health information: cross-sectional questionnaire study. J Med Internet Res. (2020) 22:e19767. doi: 10.2196/19767
22. Yoon, J, Lee, M, Ahn, JS, Oh, D, Shin, S-Y, Chang, YJ, et al. Development and validation of digital health technology literacy assessment questionnaire. J Med Syst. (2022) 46:13. doi: 10.1007/s10916-022-01800-8
23. Liu, SQ, Fu, JJ, Kong, DH, Zhong, Z, Gu, CY, and Luo, Y. Development and reliability and validation test of the digital health literacy assessment scale for the community-dwelling elderly. School of Nurs. (2021) 23:4169–4174.
24. Kimberlin, CL, and Winterstein, AG. Validity and reliability of measurement instruments used in research. Am J Health-Syst Pharm. (2008) 65:2276–84. doi: 10.2146/ajhp070364
25. Taherdoost, H. Validity and reliability of the research instrument; how to test the validation of a questionnaire/survey in a research. How to test the validation of a questionnaire/survey in a research (august 10, 2016). Intern J Academic Res Manag. (2016).
26. Smirnov, NV. On the estimation of the discrepancy between empirical curves of distribution for two independent samples. Bull Math Univ Moscou. (1939) 2:3–14.
27. Terwee, CB, Bot, SDM, de Boer, MR, van der Windt, DAWM, Knol, DL, Dekker, J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. (2007) 60:34–42. doi: 10.1016/j.jclinepi.2006.03.012
28. Wu, M. Practice of questionnaire statistical analysis -- SPSS operation and application. China: Chongqing University Press (2010).
29. Liu, Q, Zhou, H, Qiu, H, Huang, C, Jiang, L, Jiang, G, et al. Reliability and validity of healthy fitness measurement scale Version1.0 (HFMS V1.0) in Chinese elderly people. BMC Public Health. (2021) 21:1019. doi: 10.1186/s12889-021-11021-2
30. Cronbach, LJ. A case study of the split-half reliability coefficient. J Educ Psychol. (1946) 37:473–80. doi: 10.1037/h0054328
31. de Vet, HCW, Mokkink, LB, Mosmuller, DG, and Terwee, CB. Spearman-Brown prophecy formula and Cronbach's alpha: different faces of reliability and opportunities for new applications. J Clin Epidemiol. (2017) 85:45–9. doi: 10.1016/j.jclinepi.2017.01.013
33. HF, K. The application of electronic computers to factor analysis. Educ Psychol Meas. (1960) 20:141–51. doi: 10.1177/001316446002000116
34. Tavakol, M, and Wetzel, A. Factor analysis: a means for theory and instrument development in support of construct validity. International. J Med Educ. (2020) 11:245–7. doi: 10.5116/ijme.5f96.0f4a
35. Ho, MY, and Liang, S. The development and validation of a short form of the forbearance scale. Frontiers in. Psychol Forsch. (2021) 12:686097. doi: 10.3389/fpsyg.2021.686097
36. Tabachnick, BG, Fidell, LS, and Ullman, JB. Using multivariate statistics, vol. 5. Boston, MA: Pearson (2007).
37. Duckworth, AL, and Kern, ML. A Meta-analysis of the convergent validity of self-control measures. J Res Pers. (2011) 45:259–68. doi: 10.1016/j.jrp.2011.02.004
38. Fornell, C, and Larcker, DF. Structural equation models with unobservable variables and measurement error: Algebra and statistics. Los Angeles, CA: Sage Publications Sage CA (1981).
39. Educational and psychological measurement. Social Sciences Ciation Index. Thousand Oaks, CA, USA: SAGE Publications. (1941).
40. Faux-Nightingale, A, Philp, F, Chadwick, D, Singh, B, and Pandyan, A. Available tools to evaluate digital health literacy and engagement with eHealth resources: a scoping review. Heliyon. (2022) 8:e10380. doi: 10.1016/j.heliyon.2022.e10380
41. Seçkin, G, Yeatts, D, Hughes, S, Hudson, C, and Bell, V. Being an informed consumer of health information and assessment of electronic health literacy in a National Sample of internet users: validity and reliability of the e-HLS instrument. J Med Internet Res. (2016) 18:e161. doi: 10.2196/jmir.5496
42. Mueller, RO, and Hancock, GR. Factor analysis and latent structure: confirmatory factor analysis. Int Encyclopedia Soc Behav Sci. (2001) 8:3–14.
43. Jing-Xia, L. The verbal communication between Taiwan and mainland for their different cultural context. J Qiqihar Teach College. (2013).
44. Strauss, ME, and Smith, GT. Construct validity: advances in theory and methodology. Annu Rev Clin Psychol. (2009) 5:1–25. doi: 10.1146/annurev.clinpsy.032408.153639
45. Sundell, E, Wångdahl, J, and Grauman, Å. Health literacy and digital health information-seeking behavior - a cross-sectional study among highly educated swedes. BMC Public Health. (2022) 22:2278. doi: 10.1186/s12889-022-14751-z
46. Patil, U, Kostareva, U, Hadley, M, Manganello, JA, Okan, O, Dadaczynski, K, et al. Health literacy, digital health literacy, and COVID-19 pandemic attitudes and behaviors in U.S. college students: implications for interventions. Int J Environ Res Public Health. (2021) 18:301. doi: 10.3390/ijerph18063301
47. Dadaczynski, K, Okan, O, Messer, M, Leung, AYM, Rosário, R, Darlington, E, et al. Digital health literacy and web-based information-seeking behaviors of university students in Germany during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. (2021) 23:e24097. doi: 10.2196/24097
Keywords: digital health literacy assessment, reliability, validity, university students, China
Citation: Nie L, Zhao J, Pan L, Pang M, Wang J, Zhou Y, Chen R, Liu H, Xu X, Su B and Kong F (2024) Validation of the digital health literacy assessment among the university students in China. Front. Public Health. 11:1294183. doi: 10.3389/fpubh.2023.1294183
Received: 14 September 2023; Accepted: 18 December 2023;
Published: 18 January 2024.
Edited by:
Wellington Pinheiro dos Santos, Federal University of Pernambuco, BrazilReviewed by:
Mohamed Awad Abdalaziz Mousnad, International University of Africa, SudanCopyright © 2024 Nie, Zhao, Pan, Pang, Wang, Zhou, Chen, Liu, Xu, Su, Ellahie, Li, Li and Kong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fanlei Kong, a29uZ2ZhbmxlaUBzZHUuZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.