
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 08 January 2024
Sec. Public Mental Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1268799
This article is part of the Research Topic Community Series in Mental Illness, Culture, and Society: Dealing with the COVID-19 Pandemic, volume VIII View all 63 articles
 Liangjia Wei1†
Liangjia Wei1† Jiao Qin1†
Jiao Qin1† Zhifeng Lin1†
Zhifeng Lin1† Xinju Huang1
Xinju Huang1 Jinfeng He1
Jinfeng He1 Dee Yu2
Dee Yu2 Fei Zhang1
Fei Zhang1 Sisi Li1
Sisi Li1 Ping Cen3
Ping Cen3 Mu Li1
Mu Li1 Tong Luo1
Tong Luo1 Rongjing Zhang1
Rongjing Zhang1 Shanmei Zhong1
Shanmei Zhong1 Cai Qin1
Cai Qin1 Zeyu Li1
Zeyu Li1 Yuan Yang1
Yuan Yang1 Huiqi Pan1
Huiqi Pan1 Mengdi Zhao1
Mengdi Zhao1 Xiaoqiong Wu1
Xiaoqiong Wu1 Junjun Jiang1,4
Junjun Jiang1,4 Hao Liang1,4
Hao Liang1,4 Li Ye1,4*
Li Ye1,4* Bingyu Liang1,4*
Bingyu Liang1,4*Background: The burden of depression symptoms has increased among individuals infected with SARS-CoV-2 during COVID-19 pandemic. However, the prevalence and associated factors of depressive symptoms among individuals infected with SARS-CoV-2 remain uncertain after optimizing the COVID-19 response in China.
Methods: An online cross-sectional survey was conducted among the public from January 6 to 30, 2023, using a convenience sampling method. Sociodemographic and COVID-19 pandemic-related factors were collected. The depression symptoms were assessed using the Patient Health Questionnaire-9 (PHQ-9). Logistic regression analysis was performed to explore the associated factors with depressive symptoms.
Results: A total of 2,726 participants completed the survey. The prevalence of depression symptoms was 35.3%. About 58% of the participants reported experiencing insufficient drug supply. More than 40% of participants reported that they had missed healthcare appointments or delayed treatment. One-third of participants responded experiencing a shortage of healthcare staff and a long waiting time during medical treatment. Logistic regression analysis revealed several factors that were associated with depression symptoms, including sleep difficulties (OR, 2.84; 95% CI, 2.34–3.44), chronic diseases (OR, 2.15; 95% CI, 1.64–2.82), inpatient treatment for COVID-19 (OR, 3.24; 95% CI, 2.19–4.77), with COVID-19 symptoms more than 13 days (OR, 1.30, 95% CI 1.04–1.63), re-infection with SARS-CoV-2 (OR, 1.52; 95% CI, 1.07–2.15), and the increased in demand for healthcare services (OR, 1.32; 95% CI, 1.08–1.61).
Conclusion: This study reveals a moderate prevalence of depression symptoms among individuals infected with SARS-CoV-2. The findings underscore the importance of continued focus on depressive symptoms among vulnerable individuals, including those with sleeping difficulties, chronic diseases, and inpatient treatment for COVID-19. It is necessary to provide mental health services and psychological interventions for these vulnerable groups during the COVID-19 epidemic.
Accumulating evidence showed that a high prevalence of mental health issues due to the COVID-19 pandemic (1–5). Depressive symptoms are prevalent in the public during the COVID-19 pandemic. Previous studies indicated that the COVID-19 pandemic has caused high levels of depressive symptoms, with a pooled prevalence ranging from 23% to 43% (6–8). It has been reported that COVID-19-related challenges disproportionately impact the experience of depressive symptoms among various populations. Previous studies suggested that healthcare workers (9), individuals with chronic diseases (10), students (11), and pregnant women (12) were more susceptible to depression symptoms. Furthermore, several risk factors, such as sociodemographic characteristics (e.g., younger age, female gender, lower income) and pandemic-related factors (e.g., COVID-19 exposure factors, shortage of resources, less social contact), were associated with depressive symptoms during the pandemic (13–19).
However, it is crucial to note that these findings display heterogeneity, attributable to differences in target populations, sampling methods, disease prevalence in local, policy stringency, and cultural context.
Notably, there is an elevated risk of developing incident depression symptoms among the SARS-CoV-2 infected people (13, 20). For instance, a study conducted in South Sinai, Egypt, revealed that the prevalence of depression symptoms among SARS-CoV-2 patients was 46.3% (21). This research found that patients who experienced hospitalization were more likely to exhibit symptoms of depression (21). Furthermore, a systematic review and meta-analysis revealed that individuals infected with SARS-CoV-2 were more susceptible to developing depressive symptoms, with a pooled prevalence of 41.7%, while the general population reported a prevalence of 31.5% during the COVID-19 outbreak (22). This underscores the importance of paying attention to the mental health issues among the infected population during the pandemic. Several factors, including social isolation, psychological stress, chronic illness, and the severity of COVID-19, are acknowledged as potential contributory risk factors for developing depressive symptoms after SARS-CoV-2 infection (23).
On December 7, 2022, China implemented 10 new optimization measures in response to COVID-19. These measures notably reduced mobility restrictions on the population and adjusted the isolation methods for infected individuals, particularly those with asymptomatic or mild cases. Studies have shown that 80% to 90% of the public in China was infected with SARS-CoV-2 between December 2022 to January 2023 (24, 25). Certain factors may contribute to an increased risk of depression symptoms among individuals infected with SARS-CoV-2 after optimizing the COVID-19 response in China. For instance, people intentionally keep a social distance for fear of infecting SARS-CoV-2, leading to feelings of isolation and anxiety. Moreover, temporary job losses, alterations in working hours, and decreased salaries may cause a high prevalence of depression symptoms during the COVID-19 epidemic. As the epidemic continues, access to healthcare has become increasingly challenging, exacerbating anxiety and stress among the population. Taken together, these factors may be associated with an increased risk of depressive symptoms among infected individuals (13, 20, 26).
However, it is worth noting that there is limited reported evidence on the prevalence of depression symptoms and its associated factors among infected individuals after the optimization of the COVID-19 response in China. Therefore, we used an online survey to investigate the prevalence of depression symptoms and correlates among individuals who self-reported being infected with SARS-CoV-2. Furthermore, we also examined the access to healthcare services after the optimization of the COVID-19 response in China. This study aims to identify potential factors associated with depression symptoms after optimization the COVID-19 response in China. It may provide valuable insights for healthcare professionals to implement interventions aimed at improving mental health among individuals infected with SARS-CoV-2.
A cross-sectional survey was conducted among the public in China from January 6 to 30, 2023, using a convenience sampling method.
The inclusion criteria for participants were (1) age ≥18 years and (2) the absence of a diagnosed mental disorder. The exclusion criteria were (1) age under 18 years and (2) a pre-existing mental disorder.
Several studies have estimated the prevalence of depressive symptoms among individuals infected with SARS-CoV-2, using a score of PHQ-9 ≥10. The prevalence of depressive symptoms ranges from 31.6% to 52%, using a score of PHQ-9≥10 (27–29). Therefore, we chose a prevalence of 30% for calculating the sample size. A sample size of n = 2,065 was calculated by using PASS software version 15. Taking into account a rate of loss to follow-up of 10%, therefore, the sample size was at least 2,272.
A total of 2,791 completed the survey. Eighteen people were excluded from the survey as they refused to complete the questionnaire. Additionally, 47 participants were excluded due to their invalid responses. The final sample size included in the analysis was 2,726 (Figure 1).
The study used a convenience sampling method to enroll participants who were both available and willing to participate. Importantly, we hypothesized that depression symptoms among participants would decrease gradually over time after the initial implementation of the relaxed policy. Consequently, data was collected during the early period of optimizing the COVID-19 response in China, which coincided with the peak of SARS-CoV-2 infections characterized by a significant surge in the number of cases. We employed the “Questionnaire Star,” a platform based on WeChat, to administer the questionnaires (30). Participants were invited to complete the questionnaire by scanning the QR code. Moreover, to ensure the quality of data, quality control questions were included in the questionnaire.
The study was approved by the Medical Ethics Committee of Guangxi Medical University (20220206). All participants were provided with online informed consent. The survey was anonymous and did not collect any personally identifiable information. Nevertheless, participants were informed that they had the right to withdraw at any point during the survey.
A structured questionnaire was composed of three sections: sociodemographic information, pandemic-related variables, and an assessment of depressive states.
Self-reported sociodemographic data were collected for gender, age, ethnicity, education, monthly income, marital status, occupation, current residence area, residency status, home-to-healthcare facility commute time, and the history of chronic disease/smoking/drinking alcohol.
This section addresses the behaviors or characteristics related to the pandemic after the optimization of the COVID-19 response in China and contains the following questions: the interruption of physical exercise (“Yes,” “No”); sleep difficulties (“Yes,” “No”); Change in utilization of healthcare services (“Same as before,” “More than before,” “less than before”); Change in healthcare costs (“the same as before,” “more than before,” “less than before”); the barriers in accessing health services are summarized in Figure 3A; Reasons for delayed or canceled medical attention are summarized in Figure 3B; COVID-19 vaccination status (“Completed zero dose,” “Completed one dose,” “Completed two doses,” “Completed three doses,” “Completed four doses”); High consumption of COVID-19-related news (“Yes,” “No”); perception of COVID-19 (“Very serious infectious disease,” “Common infectious disease,” “I don't know”); Re-infected with SARS-CoV-2 (“Yes,” “No”); Inpatient treatment for COVID-19 (“Yes,” “No”); length of COVID-19 symptom (“1 to 6 days,” “7 to 12 days,” “more than 13 days”); the self-reported COVID-19 symptoms are summarized in Figure 1. The reasons for inpatient treatment for COVID-19 are summarized in Figure 2.
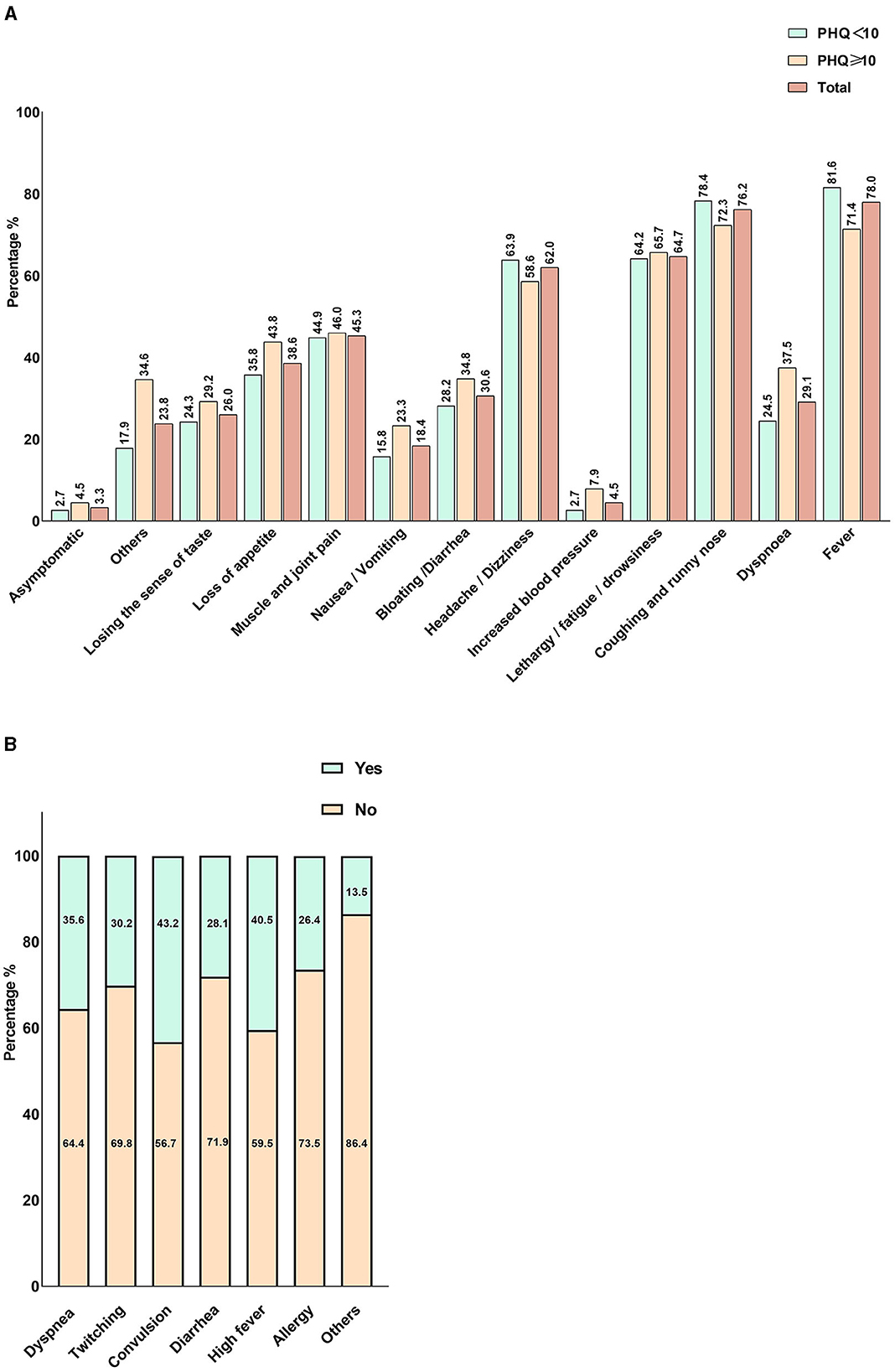
Figure 2. Self-reported COVID-19 Symptoms among participants and main symptoms for inpatient treatment. (A) The self-reported COVID-19 symptoms among participants. (B) The main symptoms for inpatient treatment. In the legend, “Yes” indicates the presence of the symptom, and “No” represents the absence of the symptom.
The Patient Health Questionnaire-9 (PHQ-9) was used to estimate the prevalence of depression symptoms. It has been reported that the PHQ-9 scale has good reliability with Cronbach's alpha of 0.91 (31). A comprehensive meta-analysis demonstrated that a cut-off score of 10 for PHQ-9 maximized both sensitivity and specificity (32). The sensitivity and specificity of PHQ-9 were both 0.85 at thresholds of 10 (33). Moreover, PHQ-9≥10 is widely employed for estimating the prevalence of depression symptoms and has been published in high-impact journals (34, 35). Hence, the scores of PHQ-9 ≥10 were used to define the symptoms of depression in this study. Participants were divided into two groups: those with PHQ-9 scores ≥10 were classified as having depressive symptoms, while those with scores below 10 were considered as not having depressive symptoms.
The Chinese version and the original PHQ-9 scale are consistent, comprising nine items. It covers the following areas: (1) “No interest or pleasure in doing things,” (2) “feeling depressed, downhearted, or hopeless,” (3) “feeling tired or having no energy,” (4) “feeling bad/frustration/failure about myself, or the sense that you let your family down,” (5) “Thoughts of dying or hurting yourself in some way,” (6) “difficulty sleeping or sleeping too much,” (7) “poor appetite or overeating,” (8) “difficulty concentrating,” and (9) “slow movement/speech or irritability or fidgeting.” The total score is calculated by summing the scores for each question, which range from 0 to 27. The reliability of this study was 0.92 (36, 37).
All data were imported into Microsoft Excel 2019 for collation. Data were statistically analyzed using SPSS version 25.0 (IBM, Armonk, NY, United States). Descriptive information including the sociodemographic and pandemic-related predictor variables were provided as percentages. Participants were categorized into two groups: those who reported SARS-CoV-2 infection were categorized as the SARS-CoV-2 infected group, while others were considered as the non-SARS-CoV-2 infected group. The chi-square test was employed to explore the differences of these two groups. For multivariate analysis, binary logistic regression was used to examine the associated factors with symptoms of depression among all participants.
Then, we compared differences between participants with and without depressive symptoms among individuals with the SARS-CoV-2 infection using the chi-square test. Variables with a p < 0.05 in analyses were included in multivariate analyses. Subsequently, for multivariate analysis, binary logistic regression was performed to explore the factors associated with depressive symptoms after assessing multicollinearity. Variables with variance inflation factors (VIF) >5 or tolerances <0.1 were excluded from the multivariate analysis. For multivariate analysis using the backward conditional method, P < 0.05 was used as the cutoff for entering the model. In addition, percentages were used to describe self-reported COVID-19 symptoms and symptoms for hospitalization. Barriers to healthcare access and reasons for delayed or canceled medical appointments were also described as percentages. Bar charts were employed for visualization.
Table 1 presents the Sociodemographic of participants. A total of 2,726 participants completed the survey, with 2,332 participants who self-reported being infected with SARS-CoV-2 (a positive SARS-CoV-2 test or clinical symptom-diagnosed) and 394 participants were not infected with SARS-CoV-2. The age ranges from 18 to 81 years (M = 29.5 years, SD = 11.1). More than half of the participants were female (62.5%) and single (60.6%). A total 63.4% of the participants belonged to the Han ethnicity, and 61.3% of the participants had a college or undergraduate education. The majority of participants (72.9%) reported a commute time of <30 min from their homes to healthcare facilities. Only 13.7% of the participants reported that they had a history of chronic disease. Additionally, the prevalence of depression symptoms among participants infected with SARS-CoV-2 was 33.3%. Additional details are provided in Table 1. Furthermore, participants who self-reported being infected with SARS-CoV-2 had a 2-fold higher risk of depression symptoms compared to non-infected individuals (Supplementary Table 1).
Table 2 shows the differences in the distribution of sociodemographic and epidemic-related factors between depressed and non-depressed individuals infected with SARS-CoV-2. There were significant differences in sociodemographic and COVID-19-related factors, such as age, education, occupation, current residence area, the home-to-healthcare facility commute time, history of chronic illness, smoking, drinking, sleep difficulties, change in healthcare services, change in healthcare costs, vaccines, attitudes toward COVID-19, re-infected with SARS-CoV-2, duration of COVID-19 symptoms, inpatient treatment for COVID-19.
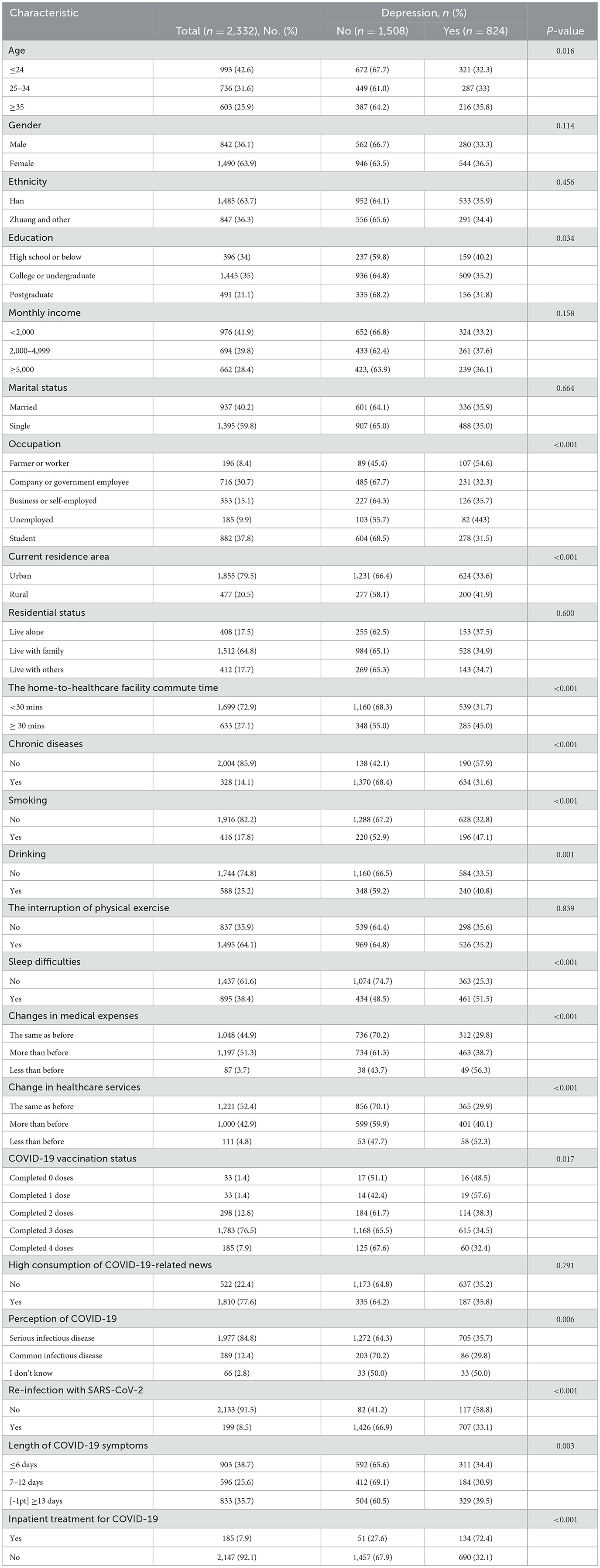
Table 2. Associated factors with depression among participants with Self-reported SARS-CoV-2 infection after optimizing the COVID-19 response in China.
Table 3 presents the associated factors related to depression symptoms. Binary logistic regression analysis revealed that several factors were associated with an increased risk of depression symptoms. These factors included sleep difficulties (OR, 2.84; 95% CI, 2.34–3.44), chronic diseases (OR, 2.15; 95% CI, 1.64–2.82), inpatient treatment for COVID-19 (OR, 3.24; 95% CI, 2.19–4.77), COVID-19 symptoms more than 13 days (OR, 1.30; 95% CI, 1.04–1.63), re-infection with SARS-CoV-2 (OR, 1.52; 95% CI, 1.07–2.15), and the increase in demand for healthcare services (OR, 1.32; 95% CI, 1.08–1.61).
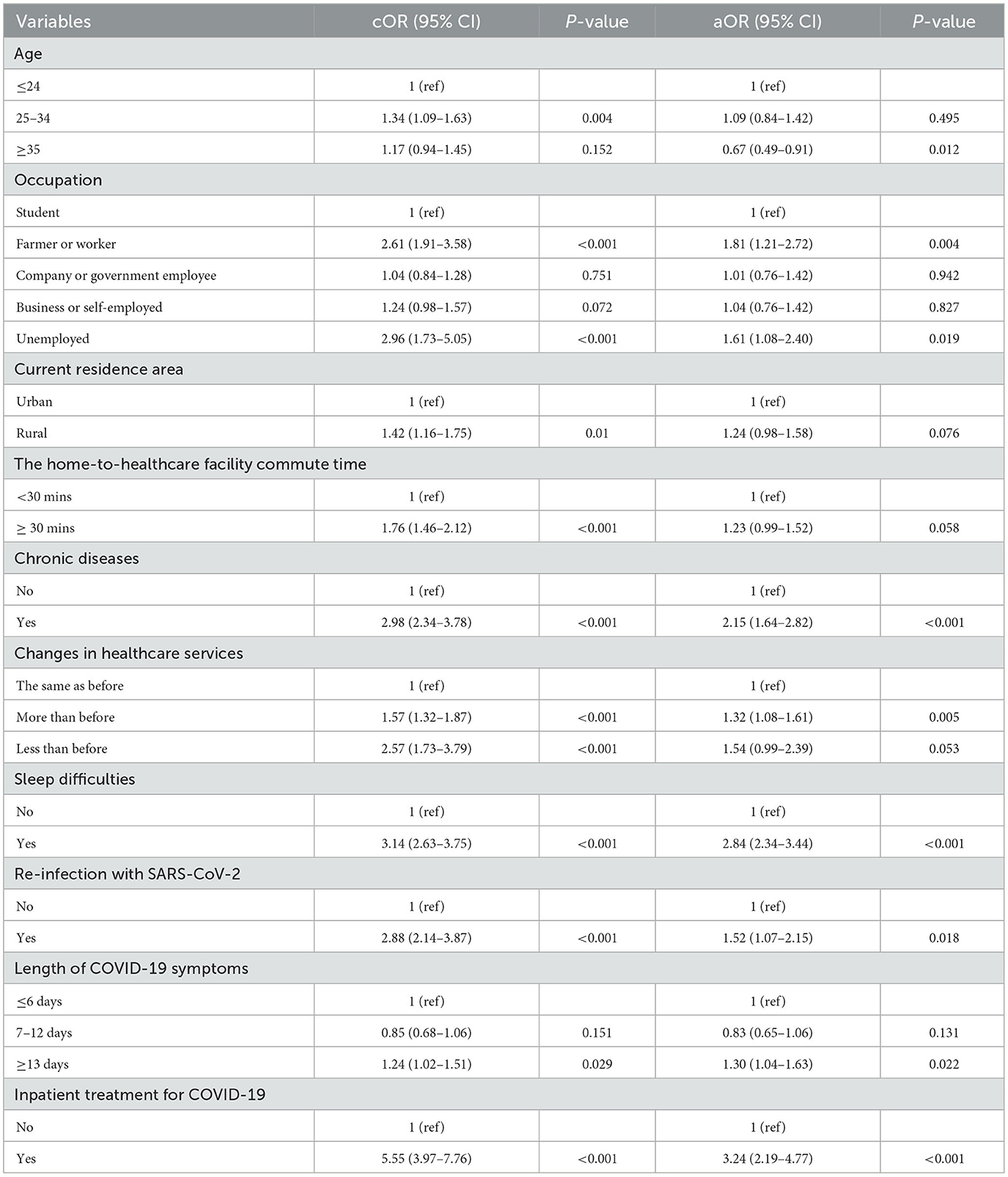
Table 3. Correlates of depression symptoms among participants with Self-reported SARS-CoV-2 infection after optimizing the COVID-19 response in China.
Figure 2 provides a summary of the self-reported COVID-19 symptoms among participants. The most common symptom was cough/runny nose (72.3%) among infected individuals (Figure 1A), followed by fever (71.4%), fatigue/drowsiness (65.7%), and headache/dizziness (58.6%). Regarding the reasons for inpatient treatment (Figure 1B), convulsions and high fever are the most common symptoms for inpatients, reported by more than 40% of those affected, followed by dyspnea (35.6%) and twitching (30.2%).
Figure 3A illustrates barriers to accessing healthcare services among participants with depressive symptoms. More than half of the participants (58.0%) reported experiencing a shortage of medication supply. Additionally, over one-third of participants reported longer waiting times for doctors (36.7%) and a shortage of medical staff (32.5%) compared to the past. Furthermore, 27.4% stated that they were required to provide a negative SARS-CoV-2 nucleic acid test result to access hospital services.
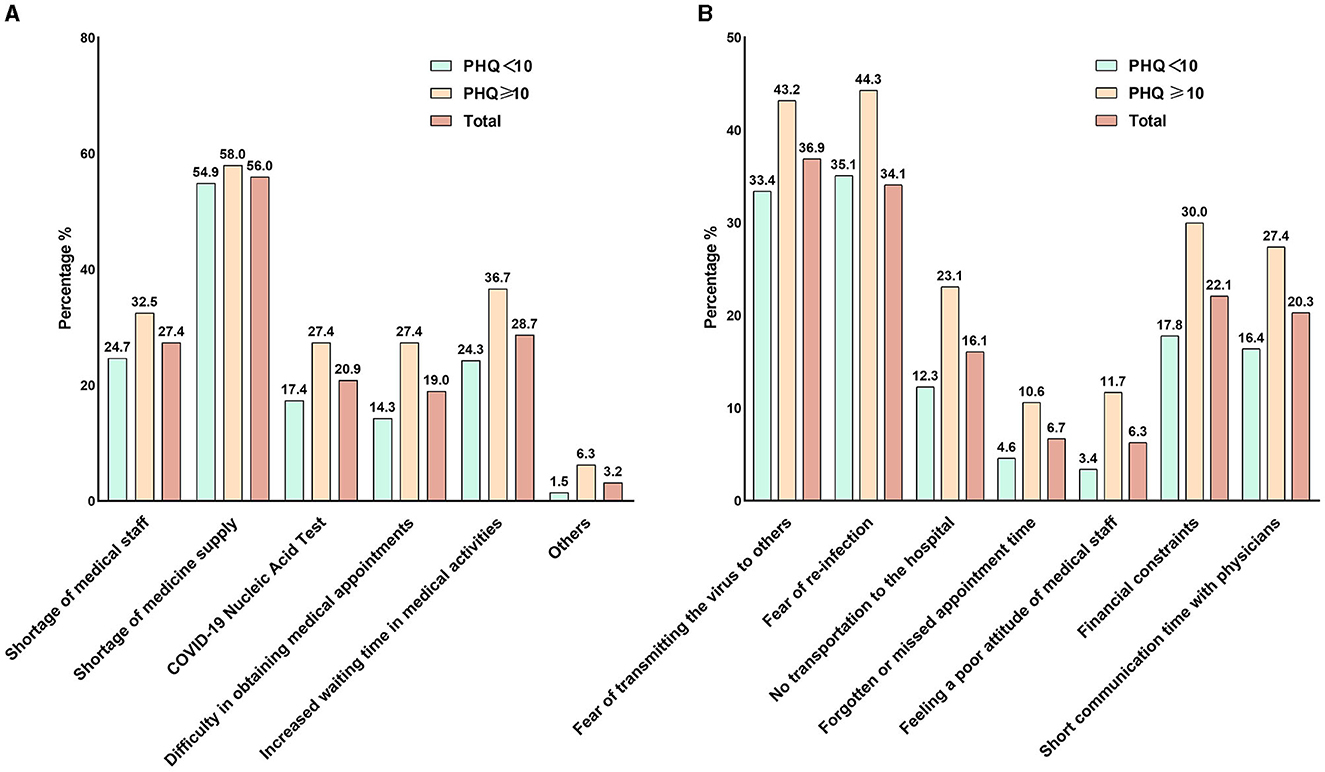
Figure 3. Barriers to accessing healthcare services and reasons for delayed or canceled medical appointments after optimizing the COVID-19 response in China. (A) Barriers to accessing healthcare services. (B) The reasons for delaying or canceling medical appointments.
In addition, we investigated the reasons for delaying or canceling medical appointments for participants with depression symptoms. As shown in Figure 3B, 43.2% of the participants reported that they fear of causing SARS-CoV-2 infections to others after SARS-CoV-2 infection. Meanwhile, 44.3% expressed concerns that a hospital visit might increase the risk of re-infection with SARS-CoV-2. Approximately one-third of the participants reported financial difficulties in seeking medical care. A total 27.4% of the participants reported that the communication time with the doctor was insufficient to meet their needs.
We investigated the prevalence of depression symptoms and their correlates among individuals with SARS-CoV-2 infection after optimizing the COVID-19 response in China. We found that the prevalence of depression symptoms was 35.3%. Moreover, participants with sleep difficulties, chronic illnesses, inpatient treatment for COVID-19, symptoms duration for more than 13 days, re-infection with SARS-CoV-2 and the increased demand for healthcare services were associated with depressive symptoms. Additionally, the findings also revealed certain barriers that participants faced in accessing health care services. Thus, it is necessary for health professionals to implement targeted psychological interventions for high-risk populations.
Little evidence on how COVID-19 optimization policies influence depression symptoms among those infected in China. We found that the prevalence of depression symptoms was 35.3% which was similar to the study conducted in Pokhara (38) and China (25). The potential for temporary unemployment, reduced salary, and strained medical resources during the early stages of implementing the COVID-19 optimization policy may exacerbate psychological distress among the public. Besides, the physical distress caused by SARS-CoV-2 may bring significant emotional and psychological. That's why the COVID-19 pandemic continues to put a substantial burden on mental health. Nevertheless, it is noteworthy that certain studies have reported a higher prevalence of depression symptoms than the present study (39, 40). A study conducted in Shanghai showed that the prevalence of depression symptoms was 82% among infected individuals before the optimization of the COVID-19 response in China (28). The low prevalence of depression symptoms in this study may be attributed to the following reasons: First of all, increased awareness of COVID-19 illness (e.g., mitigated the risk of disease progression) and the adaptation to the pandemic, thereby might reduce the fear of COVID-19. Secondly, the optimal policies decreased the mobility restrictions (24), thereby effectively alleviating loneliness in the public. Moreover, those with asymptomatic or mild symptoms were permitted to self-isolate at home rather than being subjected to compulsory isolation (41), potentially easing their anxiety and worries. This low prevalence of depressive symptoms suggests the COVID-19 optimal policy in China has effectively reduced the negative impact of COVID-19 on mental health in the public. Nonetheless, mental health problems among SARS-CoV-2 infected individuals still warrant attention (24, 41).
Specifically, our study revealed that individuals aged 35 and above had a lower risk of developing depression symptoms during the pandemic compared with the 18–24 age group. Our findings align with prior research that has emphasized age-related disparities in the prevalence of depression symptoms (10, 18, 42). A study conducted at the Shahroud University of Medical Sciences in northeastern Iran revealed a substantial increase in depression scores among students after COVID-19 outbreak (43). In this study, a significant proportion of participants in the 18–24 age groups were students, who may face potential ongoing challenges, including prolonged distance learning, school closures, and exam delays. Therefore, it is advisable to pay attention to the mental health of individuals aged 18–24. Educational institutions should implement targeted mental health interventions to restore the mental health (44).
In line with previous studies, sleep difficulties were associated with depression symptoms during COVID-19 (10, 45). Almost all of the participants in this study reported experiencing COVID-19 symptoms (such as fever, cough, dyspnea, and fatigue). The severity of COVID-19 may cause difficulty falling asleep, subsequently increasing the risk of depressive symptoms. Furthermore, our study found a high proportion of participants experiencing sleep difficulties who expressed heightened concerns about the epidemic-related information and perceived COVID-19 as a severe disease (Supplementary Table 2). Thus, we hypothesized that their excessive apprehension negatively affected their sleep quality, potentially contributing to the persistence or worsening of depressive symptoms. Therefore, it is essential for individuals with sleep difficulties to seek mental health services or treatment to better cope with the challenges associated with sleep problems.
Furthermore, our findings are consistent with previous research suggesting an increased risk of depression symptoms with chronic disease (46, 47). Our study revealed that individuals with chronic diseases exhibited a high consumption of COVID-19-related news (Supplementary Table 2). Studies conducted in both China (48) and Japan (49) consistently indicated that patients with chronic diseases are at a higher risk of developing severe COVID-19, suggesting that the severity of the illness may worsen mental health. Additionally, previous reports consistently indicated that individuals with comorbidities such as diabetes (50), heart failure (51), chronic dialysis patients (52), HIV infection (53), chronic lung disease (54), chronic kidney diseases (55) and malignancies (56) experience significantly high mortality when infected with SARS-CoV-2. Therefore, an increased risk of depressive symptoms among SARS-CoV-2 infected individuals with chronic disease may be attributed to the fear of underlying health risks and the elevated mortality associated with COVID-19. To effectively address these challenges, it is crucial to develop personalized strategies and provide mental health services for patients with chronic disease when they are infected with SARS-CoV-2.
The disruptions in healthcare utilization during the pandemic had a substantial impact on the symptoms of depression among patients with chronic diseases (57, 58). We found that approximately half of the respondents with depression symptoms reported shortages of medications. Furthermore, a large number of infected individuals avoided seeking medical services from hospitals because they fear of causing SARS-CoV-2 infections to others. Further analysis revealed that these individuals experienced a decreased healthcare service utilization (Supplementary Table 3), indicating that they indeed encountered difficulties in seeking medical care. These findings underscore the challenges regarding to healthcare services among patients with chronic diseases. Therefore, it is necessary to provide timely and uninterrupted access to medical care for individuals with chronic diseases during the pandemic.
In this study, 7.9% of participants were hospitalized due to severe symptoms. Surprisingly, we found that inpatient treatment for COVID-19 increased the risk of depression symptoms. This is supported by previous studies that high incidences of depression symptoms were reported among patients hospitalized with COVID-19 (59–62). A possible explanation may be the fear of the high mortality of COVID-19 (63), which might significantly contribute to an increased risk of developing depressive symptoms. Furthermore, research indicated that individuals who have been hospitalized with COVID-19 are at a high risk of experiencing post-COVID-19 syndrome (64–67), potentially reflecting poor prognosis which may cause worry and stress among inpatients. Therefore, timely communication with patients about their health status and progress of treatment is necessary to alleviate their fear of uncertainty. Also, health professionals should provide effective psychological support and treatment to reduce mental burdens in patients hospitalized with COVID-19.
This study has several limitations. Firstly, we could not confirm the causal relationship due to the limitation of a cross-sectional design. Future studies with longitudinal designs would be necessary. Secondly, the self-reported data might introduce recall bias, which may affect the reliability of the findings. Thirdly, it is important to acknowledge that the findings may be limited in generalizability due to the small sample size. Moreover, it is crucial to acknowledge that we did not collect data to assess other psychological factors such as anxiety, trauma, and stress. This is an important limitation of this study, as these mental health issues may also play significant roles in mental health among participants. Lastly, the use of PHQ-9 scales may overestimate the prevalence of depressive symptoms (68), as the clinical diagnosis is typically required for accurate determination.
This study revealed a moderate prevalence of depressive symptoms among individuals infected with SARS-CoV-2 after optimizing the COVID-19 response in China. It is necessary to provide mental health services and psychological interventions for the at-risk groups, including individuals with sleep difficulties, chronic diseases, inpatient treatment for COVID-19, long COVID-19 symptoms duration, and re-infection with SARS-CoV-2. Furthermore, health policymakers should formulate policies and interventions for responding to the mental health challenges for the future pandemics similar to SARS-CoV-2.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The study was approved by the Medical Ethics Committee of Guangxi Medical University (20220206). All participants were provided with online informed consent. The studies were conducted in accordance with the local legislation and institutional requirements.
LW: Writing—original draft. JQ: Writing—original draft. ZLin: Investigation, Visualization, Writing— original draft. XH: Investigation, Supervision, Writing—review & editing. JH: Investigation, Methodology, Writing—review & editing. DY: Project administration, Writing—review & editing. FZ: Software, Writing— review & editing. SL: Supervision, Writing—review & editing. PC: Writing—review & editing. ML: Project administration, Writing—review & editing. TL: Data curation, Writing—review & editing. RZ: Writing—review & editing. SZ: Writing—review & editing. CQ: Writing—review & editing. ZLi: Writing—review & editing. YY: Investigation, Writing—review & editing. HP: Writing—review & editing. MZ: Writing—review & editing. XW: Writing—review & editing. JJ: Supervision, Writing—review & editing. HL: Funding acquisition, Writing—review & editing. LY: Funding acquisition, Supervision, Writing— review & editing. BL: Funding acquisition, Supervision, Writing—review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Guangxi Scientific and Technological Talent Project (Grant number 2022AC20031), the National Key R&D Program of China (Grant number 2022YFC2305001), and thousands of Young and Middle Age Key Teachers Training Program in Guangxi Colleges and Universities (To BL).
We are very appreciative of the participants who took the time to participate in the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1268799/full#supplementary-material
1. Fong TCT, Chang K, Ho RTH. Association between quarantine and sleep disturbance in Hong Kong adults: the mediating role of COVID-19 mental impact and distress. Front Psychiatry. (2023) 14:1127070. doi: 10.3389/fpsyt.2023.1127070
2. Mooldijk SS, Dommershuijsen LJ, de Feijter M, Luik AI. Trajectories of depression and anxiety during the COVID-19 pandemic in a population-based sample of middle-aged and older adults. J Psychiatr Res. (2022) 149:274–80. doi: 10.1016/j.jpsychires.2022.03.002
3. Motrico E, Dominguez-Salas S, Rodriguez-Dominguez C, Gomez-Gomez I, Rodriguez-Munoz MF, Gomez-Baya D. The impact of the COVID-19 pandemic on perinatal depression and anxiety: a large cross-sectional study in Spain. Psicothema. (2022) 34:200–8. doi: 10.7334/psicothema2021.380
4. Benke C, Autenrieth LK, Asselmann E, Pane-Farre CA. Stay-at-home orders due to the COVID-19 pandemic are associated with elevated depression and anxiety in younger, but not older adults: results from a nationwide community sample of adults from Germany. Psychol Med. (2020) 2:1–2. doi: 10.1017/S0033291720003438
5. Liao YH, Fan BF, Zhang HM, Guo L, Lee Y, Wang WX, et al. The impact of COVID-19 on subthreshold depressive symptoms: a longitudinal study. Epidemiol Psychiatr Sci. (2021) 30:e20. doi: 10.1017/S2045796021000044
6. Yuan K, Zheng YB, Wang YJ, Sun YK, Gong YM, Huang YT, et al. A systematic review and meta-analysis on prevalence of and risk factors associated with depression, anxiety and insomnia in infectious diseases, including COVID-19: a call to action. Mol Psychiatry. (2022) 27:3214–22. doi: 10.1038/s41380-022-01638-z
7. Li W, Zhao Z, Chen D, Peng Y, Lu Z. Prevalence and associated factors of depression and anxiety symptoms among college students: a systematic review and meta-analysis. J Child Psychol Psychiatry. (2022) 63:1222–30. doi: 10.1111/jcpp.13606
8. Huang G, Chu H, Chen R, Liu D, Banda KJ, O'Brien AP, et al. Prevalence of depression, anxiety, and stress among first responders for medical emergencies during COVID-19 pandemic: a meta-analysis. J Glob Health. (2022) 12:05028. doi: 10.7189/jogh.12.05028
9. Yassin A, Al-Mistarehi AH, Soudah O, Karasneh R, Al-Azzam S, Qarqash AA, et al. Trends of prevalence estimates and risk factors of depressive symptoms among healthcare workers over one year of the COVID-19 pandemic. Clin Pract Epidemiol Ment Health. (2022) 18:e174501792206160. doi: 10.2174/17450179-v18-e2206160
10. Liao DD, Dong M, Ding KR, Hou CL, Tan WY, Ke YF, et al. Prevalence and patterns of major depressive disorder and subthreshold depressive symptoms in south China. J Affect Disord. (2023) 329:131–40. doi: 10.1016/j.jad.2023.02.069
11. Huang J, Liu X. Anxiety, depression, and their comorbidity among Chinese college students during the COVID-19 lockdown in the post-epidemic era: an online cross-sectional survey. BMC Psychiatry. (2023) 23:923. doi: 10.1186/s12888-023-05442-z
12. Zhang Y, Ma ZF. Psychological responses and lifestyle changes among pregnant women with respect to the early stages of COVID-19 pandemic. Int J Soc Psychiatry. (2021) 67:344–50. doi: 10.1177/0020764020952116
13. Shi L, Lu ZA, Que JY, Huang XL, Liu L, Ran MS, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in china during the coronavirus disease 2019 pandemic. JAMA Netw Open. (2020) 3:e2014053. doi: 10.1001/jamanetworkopen.2020.14053
14. Witteveen AB, Young SY, Cuijpers P, Ayuso-Mateos JL, Barbui C, Bertolini F, et al. COVID-19 and common mental health symptoms in the early phase of the pandemic: an umbrella review of the evidence. PLoS Med. (2023) 20:e1004206. doi: 10.1371/journal.pmed.1004206
15. Talham CJ, Williams F. Household food insecurity during the COVID-19 pandemic is associated with anxiety and depression among US- and foreign-born adults: findings from a nationwide survey. J Affect Disord. (2023) 336:126–32. doi: 10.1016/j.jad.2023.05.081
16. Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. (2021) 8:141–9. doi: 10.1016/S2215-0366(20)30482-X
17. Garre-Olmo J, Turro-Garriga O, Marti-Lluch R, Zacarias-Pons L, Alves-Cabratosa L, Serrano-Sarbosa D, et al. Changes in lifestyle resulting from confinement due to COVID-19 and depressive symptomatology: a cross-sectional a population-based study. Compr Psychiatry. (2021) 104:152214. doi: 10.1016/j.comppsych.2020.152214
18. O'Connor RC, Wetherall K, Cleare S, McClelland H, Melson AJ, Niedzwiedz CL, et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry. (2021) 218:326–33. doi: 10.1192/bjp.2020.212
19. Zurcher SJ, Kerksieck P, Adamus C, Burr CM, Lehmann AI, Huber FK, et al. Prevalence of mental health problems during virus epidemics in the general public, health care workers and survivors: a rapid review of the evidence. Front Pub Health. (2020) 8:560389. doi: 10.3389/fpubh.2020.560389
20. Xie Y, Xu E, Al-Aly Z. Risks of mental health outcomes in people with covid-19: cohort study. BMJ. (2022) 376:e068993. doi: 10.1136/bmj-2021-068993
21. Gad BK, Arafa MA, Attia AF, Farahat AH, Abdou MS. Depression, anxiety, and stress among COVID-19 patients in South Sinai, Egypt: prevalence and associated predictors. Sci Rep. (2023) 13:19193. doi: 10.1038/s41598-023-45775-z
22. Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. (2021) 281:91–8. doi: 10.1016/j.jad.2020.11.117
23. Mazza MG, Palladini M, Poletti S, Benedetti F. Post-COVID-19 depressive symptoms: epidemiology, pathophysiology, and pharmacological treatment. CNS Drugs. (2022) 36:681–702. doi: 10.1007/s40263-022-00931-3
24. Zhang F, Yang Y, Liang N, Liang H, Chen Y, Lin Z, et al. Transmission network and phylogenetic analysis reveal older male-centered transmission of CRF01_AE and CRF07_BC in Guangxi, China. Emerg Microbes Infect. (2023) 12:2147023. doi: 10.1080/22221751.2022.2147023
25. Xiao J, Liu L, Peng Y, Wen Y, Lv X, Liang L, et al. Anxiety, depression, and insomnia among nurses during the full liberalization of COVID-19: a multicenter cross-sectional analysis of the high-income region in China. Front Pub Health. (2023) 11:1179755. doi: 10.3389/fpubh.2023.1179755
26. Salanti G, Peter N, Tonia T, Holloway A, White IR, Darwish L, et al. The impact of the COVID-19 pandemic and associated control measures on the mental health of the general population: a systematic review and dose-response meta-analysis. Ann Intern Med. (2022) 175:1560–71. doi: 10.7326/M22-1507
27. Zhang J, Lu H, Zeng H, Zhang S, Du Q, Jiang T, et al. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav Immun. (2020) 87:49–50. doi: 10.1016/j.bbi.2020.04.031
28. Hall BJ Li G, Chen W, Shelley D, Tang W. Prevalence of depression, anxiety, and suicidal ideation during the Shanghai 2022 Lockdown: a cross-sectional study. J Affect Disord. (2023) 330:283–90. doi: 10.1016/j.jad.2023.02.121
29. Perlis RH, Ognyanova K, Santillana M, Baum MA, Lazer D, Druckman J, et al. Association of acute symptoms of COVID-19 and symptoms of depression in adults. JAMA Netw Open. (2021) 4:e213223. doi: 10.1001/jamanetworkopen.2021.3223
30. Wu W, Zhang Y, Wang P, Zhang L, Wang G, Lei G, et al. Psychological stress of medical staffs during outbreak of COVID-19 and adjustment strategy. J Med Virol. (2020) 92:1962–70. doi: 10.1002/jmv.25914
31. Lee Y, Hyun Y, You M, Lee H, Han JO, Seo S. The effect of resource loss on depression and peritraumatic distress during the early period of the COVID-19: considering the pandemic-situational and social context. BMC Pub Health. (2023) 23:760. doi: 10.1186/s12889-023-15628-5
32. Levis B, Benedetti A, Thombs BD. Accuracy of patient health questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. (2019) 365:l1476. doi: 10.1136/bmj.l1476
33. Negeri ZF, Levis B, Sun Y, He C, Krishnan A, Wu Y, et al. Accuracy of the patient health questionnaire-9 for screening to detect major depression: updated systematic review and individual participant data meta-analysis. BMJ. (2021) 375:n2183. doi: 10.1136/bmj.n2183
34. Clark DM, Canvin L, Green J, Layard R, Pilling S, Janecka M. Transparency about the outcomes of mental health services (IAPT approach): an analysis of public data. Lancet. (2018) 391:679–86. doi: 10.1016/S0140-6736(17)32133-5
35. Rouquette A, Descarpentry A, Dione F, Falissard B, Legleye S, Vuillermoz C, et al. Comparison of depression and anxiety following self-reported COVID-19-like symptoms vs SARS-CoV-2 seropositivity in France. JAMA Network Open. (2023) 6:e2312892. doi: 10.1001/jamanetworkopen.2023.12892
36. Guo B, Kaylor-Hughes C, Garland A, Nixon N, Sweeney T, Simpson S, et al. Factor structure and longitudinal measurement invariance of PHQ-9 for specialist mental health care patients with persistent major depressive disorder: exploratory structural equation modelling. J Affect Disord. (2017) 219:1–8. doi: 10.1016/j.jad.2017.05.020
37. Wu Y, Levis B, Riehm KE, Saadat N, Levis AW, Azar M, et al. Equivalency of the diagnostic accuracy of the PHQ-8 and PHQ-9: a systematic review and individual participant data meta-analysis. Psychol Med. (2020) 50:1368–80.
38. Paudel S, Khanal SP, Gautam S, Chalise A, Koirala TN, Marahatta SB. Anxiety and depression among people with type 2 diabetes visiting diabetes clinics of Pokhara Metropolitan, Nepal: a cross-sectional study. BMJ Open. (2023) 13:e064490. doi: 10.1136/bmjopen-2022-064490
39. Ettman CK, Fan AY, Subramanian M, Adam GP, Badillo Goicoechea E, Abdalla SM, et al. Prevalence of depressive symptoms in U. S adults during the COVID-19 pandemic: a systematic review. SSM Popul Health. (2023) 21:101348. doi: 10.1016/j.ssmph.2023.101348
40. Zhang Y, Luo M, Ouyang J, Chen Y, Xia H, Yang F, et al. The influence of changes in the Chinese COVID-19 prevention and control policies on mental health of medical staff: a network analysis. J Affect Disord. (2023) 335:10–7. doi: 10.1016/j.jad.2023.05.013
41. Chen H, Zhang K. “Nationwide fever” vs “Nationwide fear” after optimizing the COVID-19 response in China. Asian J Psychiatr. (2023) 82:103499. doi: 10.1016/j.ajp.2023.103499
42. Kreski NT, Keyes KM, Parks MJ, Patrick ME. Depressive and anxious symptoms among young adults in the COVID-19 pandemic: Results from monitoring the future. Depress Anxiety. (2022) 39:536–47. doi: 10.1002/da.23273
43. Mirhosseini S, Grimwood S, Dadgari A, Basirinezhad MH, Montazeri R, Ebrahimi H. One-year changes in the prevalence and positive psychological correlates of depressive symptoms during the COVID-19 pandemic among medical science students in northeast of Iran. Health Sci Rep. (2022) 5:e490. doi: 10.1002/hsr2.490
44. Goularte JF, Serafim SD, Colombo R, Hogg B, Caldieraro MA, Rosa AR. COVID-19 and mental health in Brazil: psychiatric symptoms in the general population. J Psychiatr Res. (2021) 132:32–7. doi: 10.1016/j.jpsychires.2020.09.021
45. Goldstein AN, Walker MP. The role of sleep in emotional brain function. Annu Rev Clin Psychol. (2014) 10:679–708. doi: 10.1146/annurev-clinpsy-032813-153716
46. Xiao S, Shi L, Dong F, Zheng X, Xue Y, Zhang J, et al. The impact of chronic diseases on psychological distress among the older adults: the mediating and moderating role of activities of daily living and perceived social support. Aging Ment Health. (2022) 26:1798–804. doi: 10.1080/13607863.2021.1947965
47. Zhu K, Niu Z, Freudenheim JL, Zhang ZF, Lei L, Homish GG, et al. COVID-19 related symptoms of anxiety, depression, and PTSD among US Adults. Psychiatry Res. (2021) 301:113959. doi: 10.1016/j.psychres.2021.113959
48. Cai J, Lin K, Zhang H, Xue Q, Zhu K, Yuan G, et al. A one-year follow-up study of systematic impact of long COVID symptoms among patients post SARS-CoV-2 omicron variants infection in Shanghai, China. Emerg Microbes Infect. (2023) 12:2220578. doi: 10.1080/22221751.2023.2220578
49. Miyashita K, Hozumi H, Furuhashi K, Nakatani E, Inoue Y, Yasui H, et al. Changes in the characteristics and outcomes of COVID-19 patients from the early pandemic to the delta variant epidemic: a nationwide population-based study. Emerg Microbes Infect. (2023) 12:2155250. doi: 10.1080/22221751.2022.2155250
50. Li R, Shen M, Yang Q, Fairley CK, Chai Z, McIntyre R, et al. Global diabetes prevalence in COVID-19 patients and contribution to COVID-19- related severity and mortality: a systematic review and meta-analysis. Diabetes Care. (2023) 46:890–7. doi: 10.2337/dc22-1943
51. Ellis RJ, Moffatt CR, Aaron LT, Beaverson G, Chaw K, Curtis C, et al. Factors associated with hospitalisations and deaths of residential aged care residents with COVID-19 during the Omicron (BA. 1) wave in Queensland. Med J Aust. (2023) 218:174–9. doi: 10.5694/mja2.51813
52. Vallejos A, Baldani AEM, Gauto MA, Rueda DV, Santoro FM, Abriata G. COVID-19 among chronic dialysis patients after first year of pandemic, Argentina. Emerg Infect Dis. (2022) 28:2294–7. doi: 10.3201/eid2811.212597
53. Bertagnolio S, Thwin SS, Silva R, Nagarajan S, Jassat W, Fowler R, et al. Clinical features of, and risk factors for, severe or fatal COVID-19 among people living with HIV admitted to hospital: analysis of data from the WHO global clinical platform of COVID-19. Lancet HIV. (2022) 9:e486–e95. doi: 10.1016/S2352-3018(22)00097-2
54. Tran A, Fernando SM, Rochwerg B, Barbaro RP, Hodgson CL, Munshi L, et al. Prognostic factors associated with mortality among patients receiving venovenous extracorporeal membrane oxygenation for COVID-19: a systematic review and meta-analysis. Lancet Respir Med. (2023) 11:235–44. doi: 10.1016/S2213-2600(22)00296-X
55. Li Y, Ashcroft T, Chung A, Dighero I, Dozier M, Horne M, et al. Risk factors for poor outcomes in hospitalised COVID-19 patients: A systematic review and meta-analysis. J Glob Health. (2021) 11:10001. doi: 10.7189/jogh.11.10001
56. Matsuo K, Mandelbaum RS, Vallejo A, Klar M, Roman LD, Wright JD. Assessment of gender-specific COVID-19 case fatality risk per malignant neoplasm type. JAMA Oncol. (2023). doi: 10.1001/jamaoncol.2023.0768
57. Pouwels BDC, Simons SO, Theunissen M, Peters ML, Schoenmaekers JJ, Bekkers SC, et al. Healthcare use during COVID-19 and the effect on psychological distress in patients with chronic cardiopulmonary disorders in the Netherlands: a cross-sectional study. BMJ Open. (2021) 11:e046883. doi: 10.1136/bmjopen-2020-046883
58. Kim K, Kim H, Lee J, Cho IK, Ahn MH, Son KY, et al. Functional impairments in the mental health, depression and anxiety related to the viral epidemic, and disruption in healthcare service utilization among cancer patients in the COVID-19 pandemic era. Cancer Res Treat. (2022) 54:671–9. doi: 10.4143/crt.2021.585
59. Clift AK, Ranger TA, Patone M, Coupland CAC, Hatch R, Thomas K, et al. Neuropsychiatric ramifications of severe COVID-19 and other severe acute respiratory infections. JAMA Psychiatry. (2022) 79:690–8. doi: 10.1001/jamapsychiatry.2022.1067
60. Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. (2021) 8:416–27. doi: 10.1016/S2215-0366(21)00084-5
61. Liu CH, Stevens C, Conrad RC, Hahm HC. Evidence for elevated psychiatric distress, poor sleep, and quality of life concerns during the COVID-19 pandemic among U. S young adults with suspected and reported psychiatric diagnoses. Psychiatry Res. (2020) 292:113345. doi: 10.1016/j.psychres.2020.113345
62. Liu D, Baumeister RF, Veilleux JC, Chen C, Liu W, Yue Y, et al. Risk factors associated with mental illness in hospital discharged patients infected with COVID-19 in Wuhan, China. Psychiatry Res. (2020) 292:113297. doi: 10.1016/j.psychres.2020.113297
63. Isath A, Malik AH, Goel A, Gupta R, Shrivastav R, Bandyopadhyay D. Nationwide analysis of the outcomes and mortality of hospitalized COVID-19 patients. Curr Probl Cardiol. (2023) 48:101440. doi: 10.1016/j.cpcardiol.2022.101440
64. Zhang Y, Han Z, Dai Y, Liu Y, Wang Q, Cheng L, et al. Symptom burden among older COVID-19 survivors two years after hospital discharge. Aging Dis. (2023). doi: 10.14336/AD.2023.0304
65. Lam ICH, Wong CKH, Zhang R, Chui CSL, Lai FTT Li X, et al. Long-term post-acute sequelae of COVID-19 infection: a retrospective, multi-database cohort study in Hong Kong and the UK. EClinicalMedicine. (2023) 60:102000. doi: 10.1016/j.eclinm.2023.102000
66. Guo Y, Wang H, Xiao M, Guan X, Lei Y, Diao T, et al. Long-term outcomes of COVID-19 convalescents: an 18. 5-month longitudinal study in Wuhan. Int J Infect Dis. (2023) 127:85–92. doi: 10.1016/j.ijid.2022.12.008
67. Godoy-Gonzalez M, Navarra-Ventura G, Goma G, de Haro C, Espinal C, Fortia C, et al. Objective and subjective cognition in survivors of COVID-19 one year after ICU discharge: the role of demographic, clinical, and emotional factors. Crit Care. (2023) 27:188. doi: 10.1186/s13054-023-04478-7
Keywords: COVID-19, depressive symptoms, healthcare services, optimizing the COVID-19 response, PHQ-9 scale
Citation: Wei L, Qin J, Lin Z, Huang X, He J, Yu D, Zhang F, Li S, Cen P, Li M, Luo T, Zhang R, Zhong S, Qin C, Li Z, Yang Y, Pan H, Zhao M, Wu X, Jiang J, Liang H, Ye L and Liang B (2024) Prevalence of depressive symptoms and correlates among individuals who self-reported SARS-CoV-2 infection after optimizing the COVID-19 response in China. Front. Public Health 11:1268799. doi: 10.3389/fpubh.2023.1268799
Received: 31 July 2023; Accepted: 18 December 2023;
Published: 08 January 2024.
Edited by:
Samer El Hayek, Erada Center for Treatment and Rehab, United Arab EmiratesReviewed by:
Chuntana Reangsing, Mae Fah Luang University, ThailandCopyright © 2024 Wei, Qin, Lin, Huang, He, Yu, Zhang, Li, Cen, Li, Luo, Zhang, Zhong, Qin, Li, Yang, Pan, Zhao, Wu, Jiang, Liang, Ye and Liang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li Ye, eWVsaUBneG11LmVkdS5jbg==; Bingyu Liang, bGlhbmdiaW5neXVAZ3htdS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.