- 1College of Medicine, University of Baghdad, Baghdad, Iraq
- 2Department of Community and Family Medicine, College of Medicine, University of Baghdad, Baghdad, Iraq
Background: Sexually transmitted infections are common and tend to cause a lot of public misconceptions. This study was conducted to identify knowledge gaps and negative attitudes toward sexually transmitted infections and infected individuals among undergraduate students and give recommendations accordingly for the development of more objective research-guided health campaigns and school sex education programs.
Method: A cross-sectional study was conducted between May 17, 2022 and June 2, 2022 using a self-administrated questionnaire containing 84 items related to sexually transmitted infections distributed online to Baghdad-based university students.
Result: The sample consisted of 823 respondents; 332 men and 491 women. Overall knowledge was moderate to high, with 628 individuals (76.3%) answering more than half the questions correctly. There was no difference according to gender or previous sexual experience, but knowledge increased by an average of 2.73 points (p < 0.001) when a participant knew a previously infected individual. Less than half identified systemic symptoms of STIs, and their knowledge of other HIV items was also poor. Most respondents (85.5%) agreed to the need for sex education during middle or high school and cited traditional barriers as the most critical barrier (64.8%); in comparison, those who did not agree on its need cited the sensitivity of the subject (40.3%) or religious barriers (20.2%) as more important.
Conclusion: Specific knowledge gaps exist for HIV and non-HIV sexually transmitted infections; these should be addressed during sex education, focusing on specific high-risk groups. Negative attitudes and stigmatizing behavior should be addressed as well by increasing focused STI knowledge.
Introduction
Sexually transmitted infections (STIs) are a major public health concern worldwide. They refer to the multiplication of microbes in the genital tract after transmission through sexual routes. They can present with a broad spectrum of manifestations ranging from asymptomatic infections to diseases, which can end with infertility, cancers, and even death. According to the WHO, more than one million STIs are acquired every day globally (1). In developed countries, like the USA, nearly 27 million new STIs are estimated to be transmitted annually (2), half of which are among youth aged 15–24 years. While in the UK, the highest rate of more than 142,000 diagnosed cases was recorded among the same age group in 2020 (3). The estimated incidence for four curable STIs (chlamydia, gonorrhea, syphilis, and trichomoniasis) was 60.6 per 1,000 in the Middle East/North Africa region. Although this region is classified as low risk, the estimated death of 10.4 per million was more than regions with higher incidence (4). STIs Epidemiological data (in terms of incidence and prevalence) from Iraq was scarce and incomplete; with more focus on AIDS (5) or using a syndromic approach for estimation rather than laboratory tests (6).
Despite the incomplete profile of STIs in Iraq, the recent political, socioeconomic, and cultural situation of the country suggests that there are factors that may contribute to an increased spread of STIs and cause under-reporting. These factors may include war, displacement, poverty, unemployment, and the disruption of families and communities. Furthermore, increased access to the outside world through TV, cell phones, and the Internet may lead to the development of a more open mindset toward sex in a large proportion of the young Iraqi population (5), especially in urban regions including the capital city of Baghdad. University students might be especially vulnerable, as they are part of the youth group (15–24 years) designated by the United Nations; these individuals are usually disproportionately high in terms of their STI incidence (3). In Iraq, university also characterizes a period of return to mixed-gender education after 6 years of segregation during middle and high school. A sharp increase in high-risk sexual behavior is therefore expected.
According to Becker's health belief model, people's knowledge and attitude toward a health-related problem might correlate with their future behavior (7); this, in turn, means that studies which assess these indices can be useful during the development and implementation of public health campaigns and education programs in a way that is suitable to the needs of the local environment. Many studies of this nature have been performed in countries that are culturally similar to Iraq; like Iran (8, 9), Saudi Arabia (10, 11), and Turkey (12–14), while in Iraq only few articles have been published; mainly focusing on AIDS/HIV or a specific point related to STIs rather than the subject as a whole (15–18).
This study was done to identify knowledge gaps and negative attitudes toward sexually transmitted infections and infected individuals among undergraduate students. The goal is to give recommendations for the development of more objective research-guided health campaigns and school sex education programs.
Materials and methods
Study design and sampling
A cross-sectional study was conducted from May 17, 2022, to June 2, 2022, among undergraduate college students in Iraq using a self-administrated structured questionnaire (Appendix A). The questionnaire was distributed using a web-based Google form across social media websites and applications belonging to public and private universities based in Baghdad, as listed by the Ministry of Higher Education. An explanation of the targeted sample was provided at the top of the questionnaire and on the related website posts, and private social media forums were selected during questionnaire distribution. This was done to reduce the participation of individuals not meeting the sampling criteria—although complete elimination of this bias cannot be achieved with online data collection.
College students were selected as the target sample for two reasons. First, they form a part of the youth high-risk group which tends to have a disproportionally high STI incidence (3) and because they have group-specific risk factors as university, in Iraq, is a period of return to mixed-gender education after 6 years of segregation and therefore more chances for high-risk sexual behavior to occur. Knowledge gaps and attitudes need to be assessed for this group to design targeted public health campaigns and sex education programs.
To increase the validity of our data; First, the research team did not offer any incentives to the respondents to fill out the questionnaire. Second, all questions were mandatory to reduce the number of missing values during the following data analysis steps. Finally, to ensure that no initial data analysis would occur before the end of the data collection period, we made sure that the form would close automatically after 1,000 responses were collected. This was achieved using a Google workplace application, known as “form limiter.” All this was conducted and reported according to the (CHERRIES) checklist for E-surveys (19).
To be included in the final sample, respondents had to fulfill 2 criteria; be enrolled as an undergraduate in a Baghdad-based university during the academic year of 2021/2022 (assigned as criteria 1) and be enrolled in a discipline not related to medicine or medical technology (assigned as criteria 2). This was judged as a necessary step, as previous studies have demonstrated an obvious difference between non-medical and medical college students (11, 18, 20).
Data collection tool
The questionnaire was developed after a literature review (9, 12, 21). Culture-specific items were then added, including polygamy (described as a man having more than one wife as it is legal in Iraq) and circumcision. The questionnaire was then translated into Arabic and pretested on a small sample of 25 medical students and was subjected to expert review by the department of dermatology at Baghdad Teaching Hospital. Candidiasis was initially included as an item similar to a study from Kampala, Uganda (21). It was removed later as a review revealed that candidiasis is connected to sexual activity itself rather than high-risk behavior or sexual transmission (22, 23).
The questionnaire (Appendix A) was divided into demographics, knowledge, attitudes, and practices. Each section is further divided into blocks with items related to a single topic; for example, within the knowledge section, there were blocks pertaining to diseases, symptoms, transmission, outcomes, sources of information, risk, and protective factors.
In total, there were 84 items related to sexually transmitted infections. Most were presented as Yes/No questions. Knowledge-related items were each assigned 1 point for a total of 60 points from which respondents' overall knowledge could be extrapolated; with those who answered >50% of questions correctly, regarded as having good knowledge. Items related to attitudes and practices, on the other hand, had no similar scoring. This was due to their innate heterogeneity compared to knowledge-related items, it was therefore judged to be more beneficial and representative to discuss each item or block of items separately instead of calculating an overall score.
Measurements and analysis plan
Statistical Package for the Social Sciences (SPSS) version 24 was used to perform both descriptive measurements (means and proportions) and statistical analysis with an independent-samples T-test to assess the effect of gender, knowing someone with an STI, and previous sexual experience on the overall knowledge score. A Chi-square test was also performed to assess the effect of the three factors on each item. Spearman's correlation coefficient was also used to assess the congruency of knowledge self-evaluation with the measured knowledge score. D'Agostino-Pearson-Omnibus test was performed using an Excel statistics plugin as it could not be performed on SPSS.
Ethical approval and informed consent
A written description of the study's purpose was provided at the top of the questionnaire with information regarding the purpose of the study, the targeted population, and the attainment of study participants' full anonymity during the process of data collection, manuscript writing, and publication. Also, individuals were told on two instances (at the top of the questionnaire and again near the submit button) that by submitting their answers they consent to the usage of the provided information for research which might also include sharing of research data to a data repository to increase transparency. Initial ethical approval was obtained from University of Baghdad/College of Medicine followed by approval from the research committee of the National Center for Training and Human Development belonging to the Ministry of Health and Environment with decision number 8 on May 15, 2022 prior to data collection.
Results
Overview
A total of 1,000 responses were collected; 83 individuals did not meet Criteria 1 (not enrolled as undergraduates in a Baghdad-based college) and were therefore excluded from the final sample selection. A further 94 who met Criteria 1 were also excluded because they did not meet Criteria 2 (not enrolled in a medical or a medical technology-related field), providing 823 as the final sample size with a valid response rate of 82.3%.
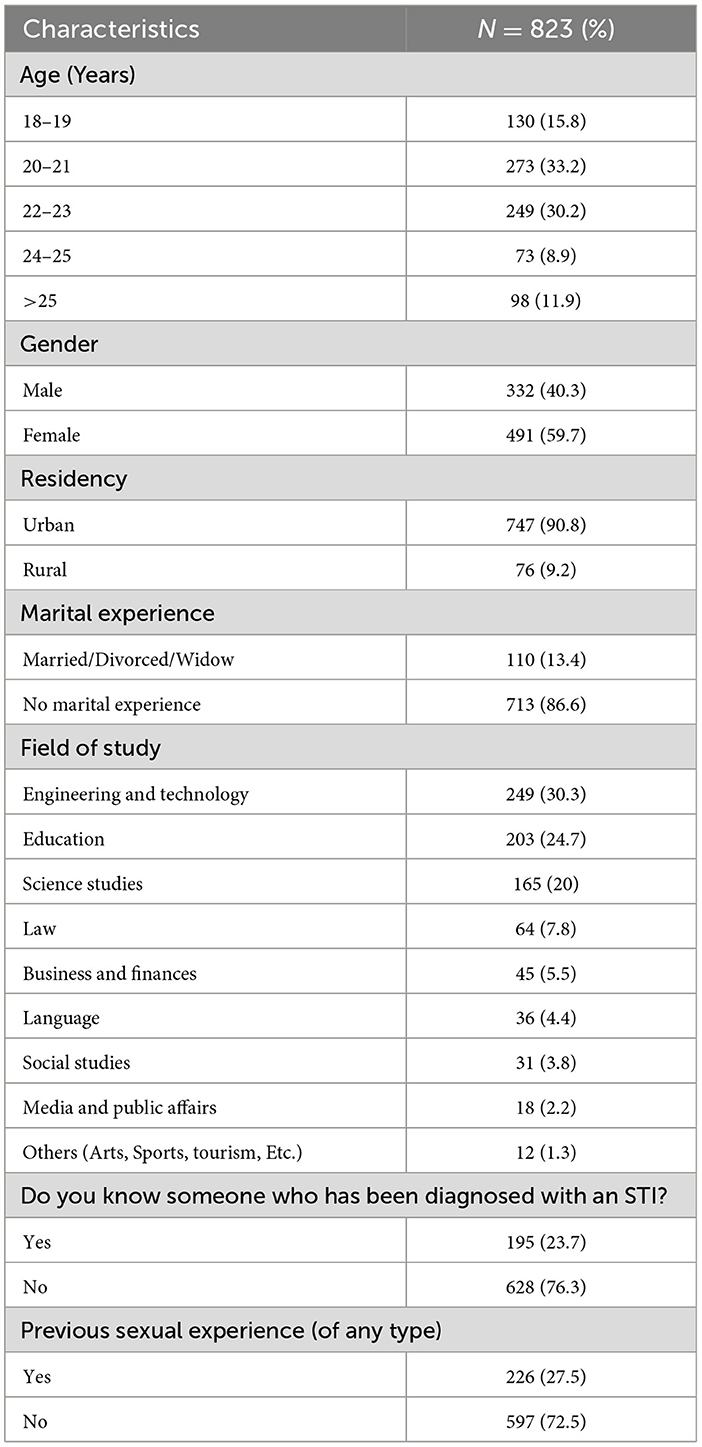
687 (83.4%) of respondents were equal to or below the age of 24 years and are therefore part of the 15–24 youth group (Table 1). The number of individuals with previous sexual experience is 226 (27.5%), more than twice that of individuals with marital experience (110, 13.4%). The number of individuals with previous sexual but no marital experience is 150 (18.2% of the study sample).
Overall knowledge
As per the Agostino-Pearson-Omnibus test (K2 = 1.367, p = 0.504), respondents' knowledge scores are normally distributed with a range from 13 to 54, a mean of 35.09 (SD = 6.65) and a median of 35 (IQR = 31–40) (Figure 1). 195 (23.7%) of respondents answered less than half the assigned questions correctly (have a score of < 31). The (B) portion of the figure also shows the relation between the measured (objective) knowledge score and knowledge self-evaluation. Spearman's coefficient (r) indicates a weak but statistically significant correlation measuring 0.325.
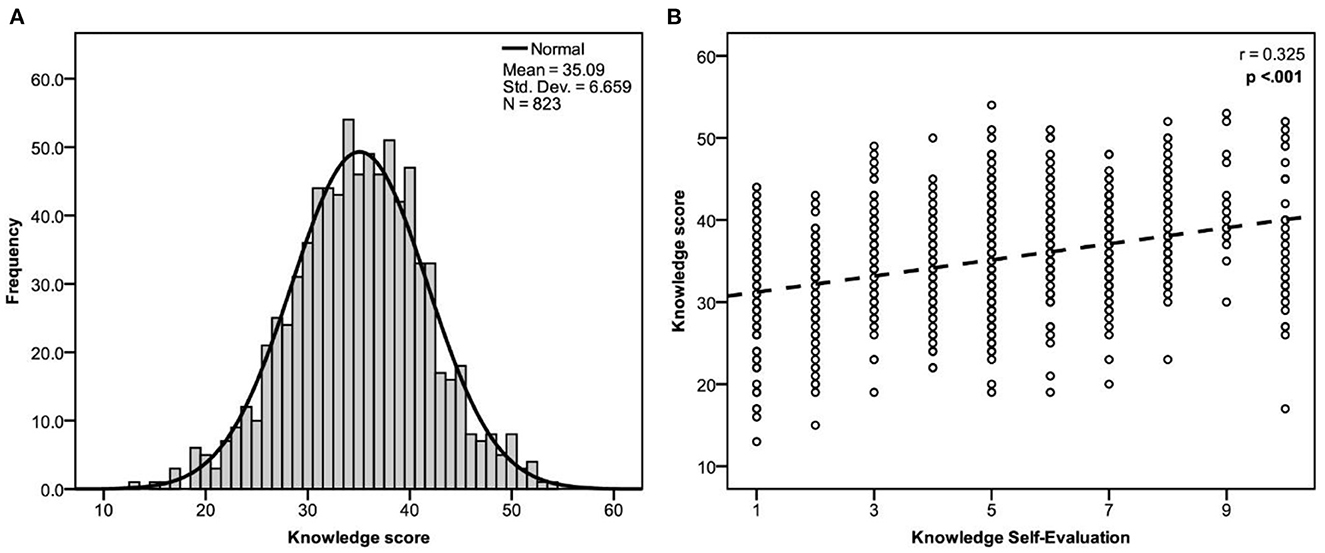
Figure 1. (A) Knowledge score distribution, (B) Correlation between measured knowledge score and knowledge self-evaluation using spearman's correlation coefficient (r) and a p-value of 0.05 as a cutoff point for significance.
Appendix B shows the effect of three factors: gender, previous sexual experience, and knowing someone who has been diagnosed with a sexually transmitted infection; out of these, the latter had the strongest effect, with a mean difference of 2.73 (P < 0.001).
Knowledge of sexually transmitted infections
In our study, the awareness that STIs can be transmitted by sexual intercourse was the most correctly answered item across all categories with a correct response rate of 98.4% (Table 2), closely followed by the awareness of HIV as an STI at 98.2%, while the lowest was the common misconception that showering before and after sex is a protective factor with only 7.9% of the study respondents having the right answer as shown in Appendix B. There were also 21 additional items with > 50% incorrect response rates, these were regarded as “common misconceptions” (Appendix Table B2). Other items exist with < 50% incorrect response rate, but they relate to topics of high public health interest and should therefore be mentioned. These include: the availability of HIV vaccination (standing at 42% incorrect response rate), the non-curability of HIV infections (32.9%), the perception that hormonal contraceptives are useful against STIs (39.2%), and that condoms cause infertility (22.2%).

Table 2. Knowledge about sexually transmitted infections among non-medical undergraduates in Baghdad, Iraq.
Attitudes toward sexually transmitted infections
82.6% of respondents agreed that sex education should be taught in middle or high school (Table 3). For these individuals, “traditional barriers” was selected as the most important barrier against the implementation of such programs (64.77%), followed by the sensitivity of the subject (24.57%) and religious barriers (10.65%) (Appendix C). This distribution was different for individuals who were against teaching sex education. On average, individuals who agreed to sex education scored 2.3 points higher on the knowledge scale (P < 0.001).
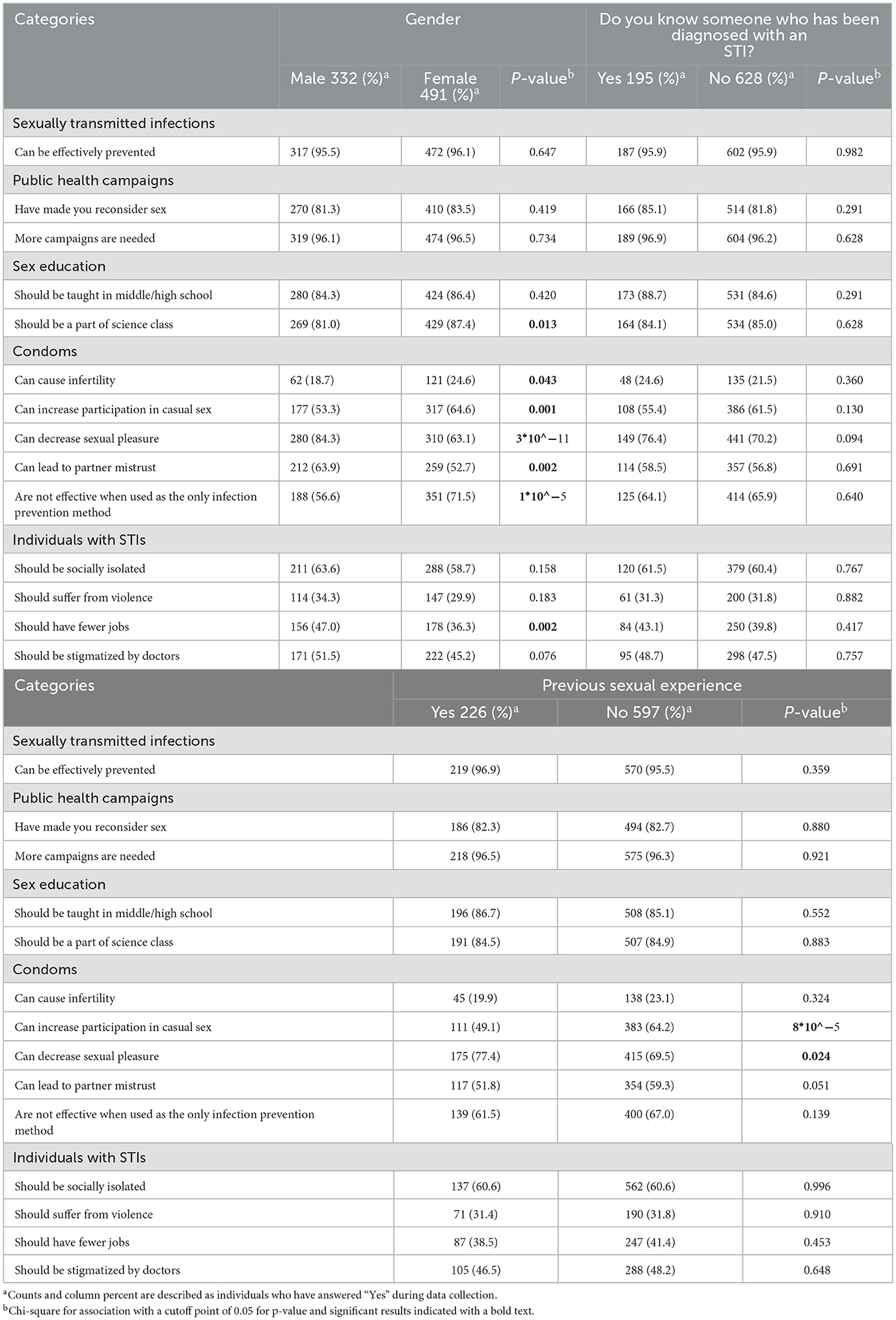
Table 3. Attitudes toward sexually transmitted infections, their prevention, and infected individuals among non-medical undergraduates in Baghdad, Iraq.
Practices related to sexually transmitted infections
Individuals who had a previous sexual experience were 2 years older on average and more likely to be men (41.3% of men had some sort of sexual experience compared to 18.1% of women) and as demonstrated in Appendix D, they were also more likely to know someone who has been diagnosed with an STI compared to those without sexual experience. Other practices related to suspicion or after a diagnosis with an STI are summarized in Table 4.
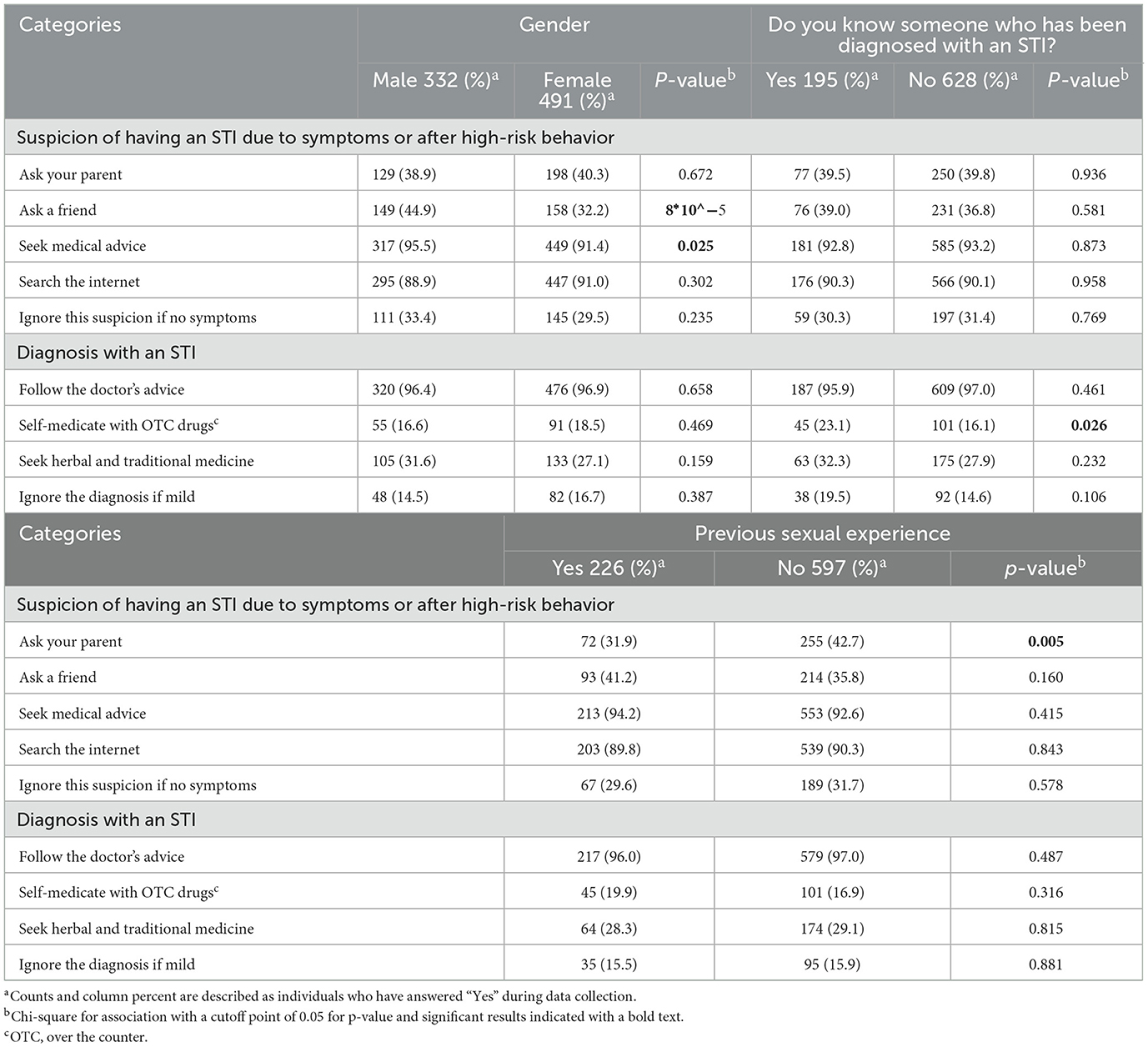
Table 4. Practices upon suspicion or diagnosis with a sexually transmitted infection among non-medical undergraduates in Baghdad, Iraq.
Discussion
The current study revealed that overall knowledge was moderate to high, with around three-quarters of respondents answering more than half the questions correctly; this is higher than the overall knowledge reported in other studies from Kufa in south Iraq (18), Iran (9), and Saudi Arabia (11) and comparable to results from Malaysia (20, 24). In this study, knowledge about STIs was not affected by gender. This is similar to several studies (9, 20, 24, 25), but differs from two studies in which women had higher knowledge (11, 18). Knowing someone who has been infected with an STI was more critical to increase knowledge than having a previous sexual experience. This is a concerning finding, as knowledge is acquired after someone else has already been affected. It also shows that people who might be thinking about having a sexual relationship might not have access to better sources of information, making school-based sex education programs and targeted public health campaigns more essential.
Internet was the most common source of information, as with most studies (9, 10, 20). However, this was not the case in one Turkish study from 2014 in which written media like books, magazines, and newspapers took first place (13). Studies on the credibility of Arab health-related websites show that only a minority of the websites are credible and certified by the Health on the Net (HON) foundation (26, 27). Social media is probably more problematic but less investigated. This dependence on online information may stem from the void created by a lack of sufficient information from other sources which were less cited (9, 10, 13). Furthermore, almost all the respondents think that more public health campaigns are needed and more than 80% think that sex education should be taught in middle or high school. This propensity to know more about STIs must be met with credible sources under the supervision of Iraqi health and education authorities.
HIV was the most commonly recognized STI (98.2%). The same finding was obtained from other research (8, 10, 12–14, 20, 24). A study conducted on Iraqi females published in 2008 showed that only half the respondents had heard about HIV/AIDS and 88.5% recognized sex as a transmission route (17). Another study conducted on high school students in Erbil, north of Iraq, in 2015 showed a higher level of recognition for HIV sexual transmission (94.3%) (16). It should be noted that both of these studies did not mention systemic manifestations commonly associated with AIDS (frequent diarrhea, frequent cough, and frequent sore throat). In our study, less than half the respondents recognized these as symptoms of STIs. As for other HIV items, only 58% of respondents correctly identified the unavailability of a vaccine, and 67.1% correctly identified HIV as a non-curable infection. The vaccine misconception was less prominent in two other studies from Iraq focusing on knowledge of HIV in a sample of Erbil high school students and university students from two governorates (15, 16), in the latter those from Diyala were more likely to believe in the vaccine misconception. All of this indicates that although more people now recognize HIV as an STI, there are still gaps in knowledge that might lead to lower risk perception and delayed care-seeking.
In terms of non-HIV STIs, trichomoniasis and chlamydia have the highest incidence among all STIs both globally and in the Middle East/North Africa region (1, 4). Yet, they were the least recognized in this study and many other studies (8, 10, 13, 24). Men were more likely to recognize gonorrhea as an STI similar to another study conducted in Iran (9) since gonorrhea is more symptomatic in men (28). In contrast, women were more likely to recognize the presence of HPV vaccines, presumably because cervical cancer in women is given more public health attention than HPV outcomes in men. This gender difference was also found in other studies (29–31). Half the respondents did not recognize pregnancy and childbirth as modes of transmission, and an even higher portion did not recognize breastfeeding as such. These are important topics that should be focused on in future educational campaigns as they relate to a significant risk to the baby from severe forms of non-HIV sexually transmitted infections including chronic hepatitis B, gonococcal conjunctivitis, and HSV, along with HIV transmission (28).
An interesting trend is noted regarding gender differences in the recognition of preventive methods; men were more likely to recognize condoms as a protective method, even when used alone, and unprotected sex as a risk factor, making men favor protection over monogamy. Women, on the other hand, were more likely to recognize polygamy (which is permissible in the Muslim world) as a risk factor, and having a single partner as a protective factor, which indicates a propensity for monogamy as a preventive method. This notion was not found in a study from Iran (9) where females were more likely to cite condom non-use as a risk factor.
Although there was relatively high support for school sex education programs, individuals who did not support such measures reported sensitivity and religious barriers more frequently. This means that future programs need to be modified and modulated in a generally acceptable way to traverse these two barriers. Still, the most cited barrier overall was traditional barriers, exemplified by tribalism which constitutes a part of legal pluralism in Iraq (32). This is unlikely to be solved just by adjusting the content of sex education programs and might need a wider governmental approach outside the scope of sexual health education. The notion that higher overall knowledge correlated with higher acceptance of sex education programs points out that it might also be possible to increase acceptance by improving knowledge from other sources like the media, the internet, or by community-based public health campaigns, and not only by addressing the aforementioned barriers.
Despite the moderately good level of knowledge, attitudes toward infected individuals were still negative, especially social stigmatization. People in favor of the social isolation of infected individuals were more likely to recognize sharing food and swimming pools as possible transmission routes for STIs (Appendix C). Women were more empathetic in terms of institutional stigmatization. This might be explained by women having a more compassionate nature than men (33) or due to socio-demographic differences between the two genders locally (34).
A significant portion of respondents, especially men and individuals with previous sexual experience, had the attitude that condoms decrease sexual pleasure. While women and those without sexual experience were more likely to think that condoms can increase participation in casual sex. These concerns should be addressed in future educational programs if an attempt is to be made to encourage condom usage. A previous study done in north Iraq also showed that an increased individual's risk perception was associated with more condom use, which may indicate that increasing overall knowledge about STIs might also increase condom use (35).
College students were more likely to have sex as they got older. This can be explained by increased independence from parents and is supported by the lower likelihood of asking parents for advice when suspecting being infected. This means that if sex education was to be implemented in college, implementing it in early grades would be more beneficial. Women were less likely to have had sex, similar to another study (14), and less likely to ask friends for advice upon suspicion of having an STI, largely because females are more stigmatized in terms of sexual activity and even more in the context of STIs (36). This stigma may also delay or prevent test seeking (37). People who know someone with an STI are more likely to self-medicate with over-the-counter drugs on suspicion of having an STI. This might be explained by studies done on self-medication behavior in Iraq and the Middle East, in which family and friends were prominent sources for self-medication advice (38, 39).
Limitations
The main shortcoming of this study is that the sample was convenient and not random. This is due to the lack of an official body to facilitate the random allocation of university students. In addition, the heterogeneity of STIs, especially in terms of their transmission routes, might call for separate studies for each individual disease. Finally, although an explanation of the targeted sample was provided at the top of the questionnaire and on the related website posts, and the questionnaire was distributed to private social media forums, belonging to Baghdad-based universities, to decrease the participation of individuals who don't meet the sample criteria, online data collection methodically leads to an inability to verify the integrity of participants' answers or sample selection.
Conclusion and recommendations
Despite the good level of recognition for HIV and gonorrhea as sexually transmitted infections, certain knowledge gaps still persist for both HIV (recognizing systemic symptoms usually associated with AIDS, unavailability of a vaccine, and non-curability of HIV infections) and non-HIV infections (recognizing chlamydia and trichomoniasis as STIs and vertical transmission). Most students showed openness toward public health campaigns and school sex education, but negative attitudes were still found toward condom usage and STI-infected individuals with certain gender variations. All the aforementioned points should be addressed in any future sex education program or public health campaign. Such interventions should be started early before sexual debut and modified according to the needs of each demographic group.
Data availability statement
The original contributions presented in the study are publicly available. This data can be found here: https://data.mendeley.com/datasets/2dmhrmt7n8/3.
Ethics statement
The studies involving human participants were reviewed and approved by the Research Committee of the National Center for Training and Human Development belonging to the Ministry of Health and Environment. The patients/participants provided their written informed consent to participate in this study.
Author contributions
JA-D and AA-S led the conception of the research idea. GA-G, AA-S, and JA-D designed the data collection tool and participated in data collection. FL reviewed the study design and reviewed the manuscript for intellectual content. JA-D applied for and provided ethical approvals for the implementation of the study. GA-G led the data analysis. AA-S and GA-G interpreted the data. All authors drafted the manuscript, attain full responsibility for the accuracy, integrity of the work, and have approved the final version of the manuscript.
Acknowledgments
The authors are grateful to Razan Al-yousif from the Department of Dermatology at Baghdad Teaching Hospital for their expert review during the development of the research questionnaire. We would also like to thank Hussaam Haider Akram, a medical student from Al-Kindy Medical College, for their help during data collection.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1017300/full#supplementary-material
References
1. World Health Organization. Sexually Transmitted Infections (STIs). World Health Organization. (2021). Available online at: https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(STIs) (accessed January 29, 2023).
2. Weinstock HS, Kreisel KM, Spicknall IH, Chesson HW, Miller WC. STI prevalence, incidence, and costs in the United States: new estimates, new approach. Sex Transm Dis. (2021) 48:207–207. doi: 10.1097/OLQ.0000000000001368
3. UK Health Security Agency. Sexually transmitted infections (STIs): Annual Data Tables. Updated March 1. (2022). Available online at: https://www.gov.uk/government/statistics/sexually-transmitted-infections-stis-annual-data-tables (accessed July 23, 2022).
4. Kenyon C, Buyze J, Colebunders R. Classification of incidence and prevalence of certain sexually transmitted infections by world regions. Int J Infect Dis. (2014) 18:73–80. doi: 10.1016/j.ijid.2013.09.014
5. Ministry of health. Country Progress Report. UNAIDS. (2012). p. 4–6. Available online at: https://www.unAIDS.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries (accessed January 29, 2023).
6. Al Jumaily H. Prevalence of sexually transmitted Diseases (STDs) in Iraq for the years (1999–2001) based on syndromic approach. IRAQI J Community Med. (2022) 24:105–8.
7. Becker MH. The Health Belief Model and Sick Role Behavior. Health Educ Monogr. (1974) 2:409–19. doi: 10.1177/109019817400200407
8. Vakilian K. Investigating the knowledge of sexually transmitted diseases in university students of Iran. Open Public Health J. (2021) 14:277–81. doi: 10.2174/1874944502114010277
9. Karamouzian M, Shahesmaeili A, Khajehkazemi R, Hooshyar SH, Fallahi H, Haghdoost AA, et al. Awareness of and Knowledge About STIs Among Nonmedical Students in Iran. Int Perspect Sex Reprod Health. (2017) 43:21–8. doi: 10.1363/43e3217
10. El-Tholoth H, Alqahtani F, Aljabri A, Alfaryan K, Alharbi F, Alhowaimil A, et al. Knowledge and attitude about sexually transmitted diseases among youth in Saudi Arabia. Urol Ann. (2018) 10:198–202. doi: 10.4103/UA.UA_14_17
11. Albanghali MA, Othman BA. A cross-sectional study on the knowledge of sexually transmitted diseases among young adults living in Albaha, Saudi Arabia. Int J Environ Res Public Health. (2020) 17:1872. doi: 10.3390/ijerph17061872
12. Kaptanoglu AF, Süer K, Diktaş H, Hinçal E. Knowledge, attitudes and behaviour towards sexually transmitted diseases in turkish cypriot adolescents. Cent Eur J Public Health. (2013) 21:54–8. doi: 10.21101/cejph.a3808
13. Ekşi Z, Kömürcü N. Knowledge level of university students about sexually transmitted diseases. Procedia Soc Behav Sci. (2014) 122:465–72. doi: 10.1016/j.sbspro.2014.01.1374
14. Saraçoglu GV, Erdem I, Dogan S, Tokuç B. Gençlik Cinsel Sagligi: Türkiye'deki Bir Üniversitede Ögrenciler Arasinda Cinsel Bilgi, Tutumlar ve Davranişlar. Nöro Psikiyatr Arşivi. (2014) 51:222–8. doi: 10.4274/npa.y6768
15. Naif HM, Hwaid AH, Hasan A-RSH, Khalifa RM, Humadi AT. Knowledge and awareness about HIV and AIDS among Iraqi College Students. Open AIDS J. (2019) 13:17–24. doi: 10.2174/1874613601913010017
16. Othman SM. Knowledge about HIV/AIDS among high school students in Erbil City/Iraq. Glob J Health Sci. (2014) 7:16–23. doi: 10.5539/gjhs.v7n1p16
17. Siziya S, Muula AS, Rudatsikira E, HIV, and AIDS-related knowledge among women in Iraq. BMC Res Notes. (2008) 1:123. doi: 10.1186/1756-0500-1-123
18. Hasan SM, Khudair FW. Knowledge and attitudes of undergraduate university students about sexual transmitted diseases at university of Kufa. Int J Sci Res Publ. (2019) 9:893–901. doi: 10.29322/IJSRP.9.08.2019.p92122
19. Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet e-surveys (CHERRIES). J Med Internet Res. (2004) 6:e34. doi: 10.2196/jmir.6.3.e34
20. Soleymani S, Abdul Rahman H, Lekhraj R, Mohd Zulkefli NA, Matinnia N. A cross-sectional study to explore postgraduate students' understanding of and beliefs about sexual and reproductive health in a public university, Malaysia. Reprod Health. (2015) 12:77. doi: 10.1186/s12978-015-0070-3
21. Sekirime WK, Tamale J, Lule JC, Wabwire-Mangen F. Knowledge, attitude and practice about sexually transmitted diseases among university students in Kampala. Afr Health Sci. (2001) 1:16–22.
22. Reed BD, Zazove P, Pierson CL, Gorenflo DW, Horrocks J. Candida transmission and sexual behaviors as risks for a repeat episode of Candida Vulvovaginitis. J Women's Heal. (2003) 12:979–89. doi: 10.1089/154099903322643901
23. Ginter G, Soyer HP, Rieger E. Vaginal yeast colonization and promiscuity. A study of 197 prostitutes. Mycoses. (2009) 35:177–80. doi: 10.1111/j.1439-0507.1992.tb00841.x
24. Mansor N, Ahmad N, Rahman HA. Determinants of knowledge on sexually transmitted infections among students in public higher education institutions in Melaka state, Malaysia. PLoS ONE. (2020) 15:e0240842. doi: 10.1371/journal.pone.0240842
25. Sham f, Yaakub S, Fawati fn, Fatinni SJ, Azamuddin AA. Knowledge, attitudes, risk behaviours and preventive practices on sexually transmitted diseases among students in a public university in Malaysia Malaysian. J Public Heal Med. (2020) 20:100–8. doi: 10.37268/mjphm/vol.20/no.3/art.610
26. Halboub E, Al-Ak'hali MS, Al-Mekhlafi HM, Alhajj MN. Quality and readability of web-based Arabic health information on COVID-19: an infodemiological study. BMC Public Health. (2021) 21:151–8. doi: 10.1186/s12889-021-10218-9
27. Weber AS, Verjee M, Rahman ZH, Ameerudeen F, Al Baz N. Typology and credibility of internet health websites originating from gulf cooperation council countries. East Mediterr Heal J. (2014) 20:804–11. doi: 10.26719/2014.20.12.804
28. Gross GE, Tyring SK. Sexually Transmitted Infections and Sexually Transmitted Diseases. 1st ed. Berlin, Heidelberg: Springer Berlin Heidelberg. (2011). p. 79.
29. Oz M, Cetinkaya N, Apaydin A, Korkmaz E, Bas S, Ozgu E, et al. Awareness and knowledge levels of turkish college students about human papilloma virus infection and vaccine acceptance. J Cancer Educ. (2018) 33:260–8. doi: 10.1007/s13187-016-1116-0
30. Cinar IO, Ozkan S, Aslan GK, Alatas E. Knowledge and behavior of university students toward human papillomavirus and vaccination. Asia Pac J Oncol Nurs. (2019) 6:300–7. doi: 10.4103/apjon.apjon_10_19
31. Kwang NB, Yee CM, Shan LP, Teik CK, Chandralega KN, Abdul Kadir AK. Knowledge perception and attitude towards human papillomavirus among pre-university students in Malaysia. Asian Pacific J Cancer Prev. (2014) 15:9117–23. doi: 10.7314/APJCP.2014.15.21.9117
33. Rueckert L, Branch B, Doan T. Are gender differences in empathy due to differences in emotional reactivity? Psychology. (2011) 2:574–8. doi: 10.4236/psych.2011.26088
34. World Bank. Labor Force, Female (% of total labour force) – Iraq. (2022). Available online at: https://data.worldbank.org/indicator/SL.TLF.TOTL.FE.ZS?locations=IQ (accessed July 22, 2022).
35. Ismael AS, Sabir Zangana JM. Knowledge attitudes and practice of condom use among males aged (15-49) Years in Erbil Governorate. Glob J Health Sci. (2012) 4:27–36. doi: 10.5539/gjhs.v4n4p27
36. Bruyn M. Facing the Challenges of HIV, AIDS, STD. Amsterdam: KIT Royal Tropical Institute. (1998).
37. Fortenberry JD, McFarlane M, Bleakley A, Bull S, Fishbein M, Grimley DM, et al. Relationships of Stigma and Shame to Gonorrhea and HIV Screening. Am J Public Health. (2002) 92:378–81. doi: 10.2105/AJPH.92.3.378
38. Khalifeh MM, Moore ND, Salameh PR. Self-medication misuse in the Middle East: a systematic literature review. Pharmacol Res Perspect. (2017) 5:e00323. doi: 10.1002/prp2.323
Keywords: sexually transmitted infections, sex education, Middle East, Iraq, Baghdad
Citation: Al-Gburi G, Al-Shakarchi A, Al-Dabagh JD and Lami F (2023) Assessing knowledge, attitudes, and practices toward sexually transmitted infections among Baghdad undergraduate students for research-guided sexual health education. Front. Public Health 11:1017300. doi: 10.3389/fpubh.2023.1017300
Received: 11 August 2022; Accepted: 30 January 2023;
Published: 16 February 2023.
Edited by:
Sudip Bhattacharya, All India Institute of Medical Sciences, Deoghar (AIIMS Deoghar), IndiaReviewed by:
Hasanain Faisal Ghazi, Al-Bayan University, IraqRiyadh K. Lafta, Al-Mustansiriya University, Iraq
Copyright © 2023 Al-Gburi, Al-Shakarchi, Al-Dabagh and Lami. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ghaith Al-Gburi,  Ghaith.ali.khaleel@gmail.com
Ghaith.ali.khaleel@gmail.com
†These authors share first authorship
 Ghaith Al-Gburi
Ghaith Al-Gburi