- 1School of Nursing, Philadelphia University, Amman, Jordan
- 2Department of Physiotherapy, Philadelphia University, Amman, Jordan
Background: Many studies published in other countries have identified certain perceived benefits of and barriers to physical activity among patients with coronary heart disease. Nevertheless, there is no data about the issue relating to Jordanian patients with coronary heart disease.
Objective: This study aimed to describe the prevalence of levels of physical activity, the benefits of and barriers to physical activity as perceived by Jordanian patients with coronary heart disease, and the relationship between physical activity and perceived benefits of and barriers to physical activity. In addition, it focused on examining the influence of selected sociodemographic and health characteristics on physical activity and the perceived benefits of and barriers to physical activity.
Methods: A cross-sectional design was performed on a sample of 400 patients with coronary heart disease. They were given a list of perceived benefits of and barriers to physical activity and asked to what extent they disagreed or agreed with each.
Results: Jordanian patients with coronary heart disease perceived various benefits of and barriers to physical activity. Most of these benefits were physiologically related (average mean = 5.7, SD = 0.7). The most substantial barriers to physical activity as perceived by the patients were “feeling anxiety,” “not enough time,” “lack of interest,” “bad weather,” and “feeling of being uncomfortable.” Sociodemographic and health characteristics that significantly influenced perceived barriers to physical activity were age, gender, health perception, chest pain frequency, education, job, caring responsibilities, ability to travel alone, smoking, and previous and current physical activity behavior.
Conclusion: This study demonstrates that patients with coronary heart disease have perceived physiological benefits of physical activity and have perceived motivational, physical health, and environmental barriers to physical activity, which is significant in developing intervention strategies that aim to maximize patients' participation in physical activity and overcome barriers to physical activity.
Introduction
Physical activity is essential in preventing and treating coronary heart disease (CHD) (1–3). The standard PA recommendation for patients with CHD is ≥150 min of moderate-intensity PA per week (4). Evidence suggests that PA markedly contributes to a decrease in modifiable CHD risk factors such as increased BP and overweight (5–7), which are associated with a decrease in the negative impact of CHD on physical health. Significantly, many reviews have reported a decrease in BP among patients with CHD who participated in the recommended level of PA (8–10). In addition, PA increases PA capacity and improves endothelial function, facilitating coronary blood flow through the vasodilatation mechanism (11). These physiological effects of PA have been shown to lower relapse rates, symptoms, and cardiac ischemia after cardiac events among patients with CHD (12–14). Furthermore, PA has been demonstrated to improve quality of life (QoL) and decrease anxiety and depression among patients with CHD (15, 16), even though it has been documented that the benefit from physical activity among patients with CHD is more significant than that of PA among healthy subjects without CHD (12).
Although the significant benefits of PA are well-known in the treatment of CHD, the vast majority of patients with CHD do not achieve PA following recommendations, even when they engage in a structured PA program or cardiac rehabilitation program (17). The performance of regular PA is considered one of the principal challenges in the success of the secondary prevention regimen of these patients through modifications in their lifestyle habits (17, 18). In Jordan, it was found that only 34.8% of patients with CHD performed regular walking exercises (19).
The contributing factors of low performance and adherence to PA that have been consistently reported in the literature include individual characteristics, such as motivation and self-efficacy. Perceived barriers to PA, such as time and access, and characteristics of PA behavior, such as PA type, intensity, and duration (20). In addition, the lack of PA programs and the referral of patients with CHD to these programs, as well as inaccessible PA programs, are significant reasons for low adherence to PA among patients with CHD (21, 22). Patients with CHD in Jordan do not receive structured secondary prevention or cardiac rehabilitation programs. Usually, these patients are provided with verbal or written advice about their disease and lifestyle modifications, including the performance of PA. This information is usually provided during the hospital stay or after discharge during patients' attendance at the clinic for follow-up care, which could hinder patients from performing PA and may be considered a principal barrier to performing PA. Although many studies have examined the relationships between perceived benefits of and barriers and PA participation in western societies, little information is available about how Jordanian patients with CHD perceive the benefits of and barriers to PA. In addition, how these constructs explain the patients' decision to PA is rarely examined.
The health promotion model (HPM) identifies perceived benefits of and barriers to action as influencing factors for health-promoting behavior, such as participation in PA. In this model, health-promoting behavior is the desired outcome (23, 24). The benefits of PA are defined as “a person's perceptions of positive and enjoyable outcomes of this behavior” (25). PA has perceived benefits that are incorporated into physiological, psychological, social, and body image benefits (26, 27). The motivational value of perceived benefits is based on previous personal experiences or outcomes observed by others. Perceived barriers to PA are linked to individuals' challenges when performing PA as an inconvenience, expense, difficulty, time, physical condition, or environmental barrier. The perceived barriers influence the initiation of a new PA or reduce an individual's commitment and adherence to the current PA. Systematic reviews have demonstrated an inverse relationship between the perception and number of barriers and levels of PA among patients with CHD (28).
The significant aspect of the success of programs and interventions that aim to promote PA in patients with CHD is the recognition of factors that limit participation in these programs (29). Information about the benefits of and barriers to PA perceived by Jordanian patients with CHD can inform nurses and healthcare providers, which helps develop an appropriate individualized approach based on patients' perception of PA benefits of and barriers to maximize patient participation in overcoming barriers to PA. These interventions could significantly assist patients with CHD in obtaining the beneficial effects of PA to improve their health, prevent complications, and thus decrease the mortality of CHD.
This study aimed to describe the prevalence of PA levels in patients with CHD and the benefits of and barriers to PA as perceived by Jordanian patients with CH and describe the relationship between perceived benefits of and barriers to PA and the participation of these patients in PA. Furthermore, it aimed to describe the influence of selected sociodemographic and health characteristics on perceived benefits of and barriers to PA and the participation of PA.
Methodology
First, approval from the Institutional Review Board at King Abdullah University Hospital (KAUH) and Jordan University Hospital administration to interview the patients was secured. Then, the researcher reviewed patients' files who visited the cardiac clinic between 1 July 2019 and 1 October 2019. Those who met the inclusion criteria were identified and invited to participate in the study. A structured interview technique to collect the required data was used.
The sample size was 400 patients with CHD, determined based on the prevalence of PA among CHD in the previous study by determining 40% at a 95% CI, 5% margin of error and adding 37 patients considering dropouts among participants (30). Two university hospitals in Jordan were included to recruit the participants. The inclusion criteria were patients diagnosed with angina or myocardial infarction (MI) at least 4 months before data collection, who were mentally competent, and who were aged 30–70 years. Exclusion criteria included any physical or psychological condition that affected patients' participation in the study.
Physical activity
The participants were administered the International Physical Activity Questionnaire (IPAQ), which assesses physical activity status. The instrument asks questions about the performance of 30 min of moderate-intensity activity 5 days per week (150 min per week) or a combination of walking and moderate-intensity activities amounting to a minimum of at least 600 METs-minutes/week. The IPAQ is a reliable and valid tool for assessing PA (reliability: kappa 0.67–0.73; Spearman's rho 0.67–0.81).
Benefits of and barriers to PA questionnaire
Since there are no clinical tools for the reliable evaluation of perceived benefits of and barriers to PA among patients with CHD, the researcher developed a scale consisting of two lists of perceived benefits of and barriers to PA based on the literature. The first list contains 22 items that reflect PA's physical, psychological, and social benefits. The second list contains 41 items that reflect PA's physical, psychological, social, and environmental barriers. The response for each item was on a 6-point Likert scale ranging from (1) strongly disagree to (6) strongly agree. In addition, two open-ended questions asked participants' opinions about additional benefits of and barriers to PA. Items of perceived benefits and barriers demonstrated a high level of internal consistency; Cronbach's alpha was calculated: 0.87 for perceived benefits of PA and 0.92 for perceived barriers to PA. Also, test-retest reliability for the total instrument was 0.89 for the Exercise Benefits Scale and 0.77 for the Exercise Barriers Scale.
To evaluate the clarity and understandability of the perceived benefits of and barriers to PA, the researcher interviewed ten patients with CHD in the cardiac clinics of both hospitals before starting data collection using structured interviews. The patients were six males and four females. In total, seven patients were diagnosed with MI, and three patients with angina. Results showed that all participants reported that all items were clear, understandable, and at the level of the patient's comprehension.
Statistical analysis
Descriptive statistical analysis was used to describe the sample. The Pearson correlation was used to describe the relationship between the benefits of and barriers to PA and the continuously measured sociodemographic and health characteristics. The same test was used to describe the relationship between individual and health characteristics, and PA was measured continuously. In addition, the t-test, chi-square test, and Fisher's exact test were used to examine differences in perceived benefits of and barriers to PA and individual and health characteristics concerning PA behavior that was measured on a continuous and dichotomous level. A one-way analysis of variance was used to compare the means of two or more independent groups.
Results
Demographic and health characteristics of the study
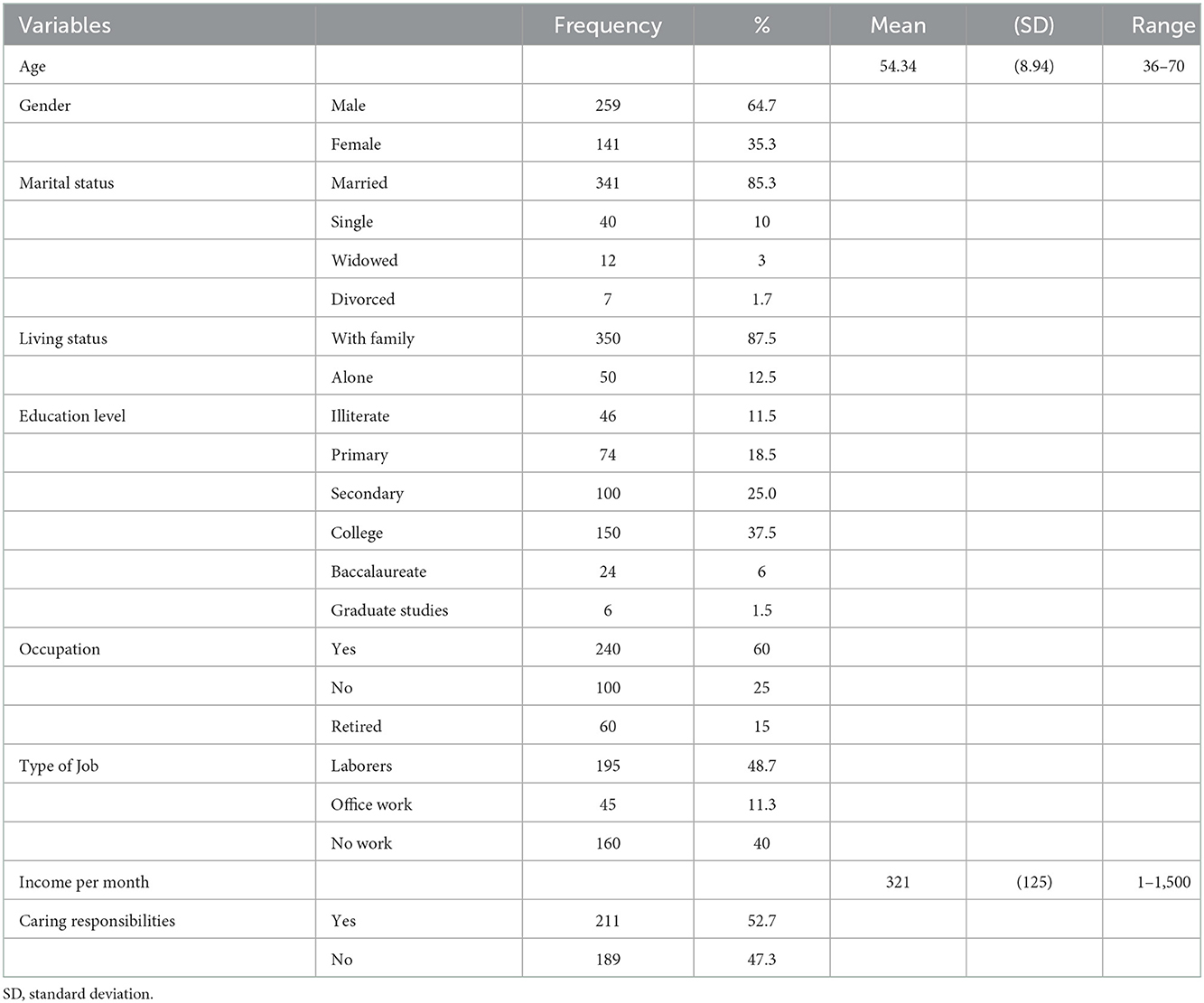
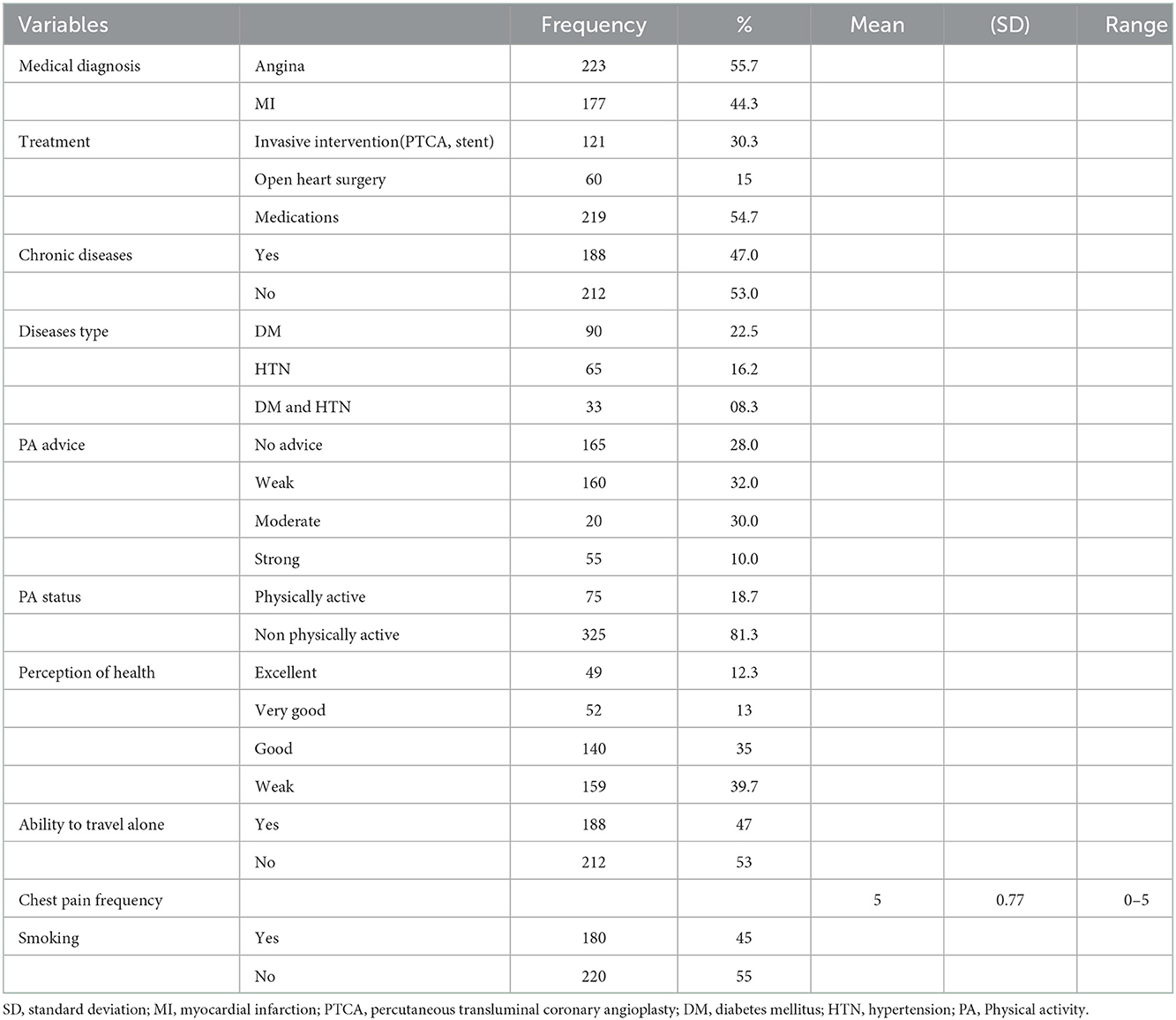
The participants were 400 patients with CHD between 36 and 70 years old, with two-thirds being male. There were no significant differences between the two groups (Tables 1,2).
Physical activity prevalence
According to the International Physical Activity Questionnaire (IPAQ), 24% of the patients are classified as physically active. According to IPAQ, participants were recognized as physically active when they met the PA guidelines of 30 min of moderate-intensity activity 5 days/week (150 min/week) or engaged in a combination of walking and moderate-intensity activities for a minimum of at least 600 METs-min/week.
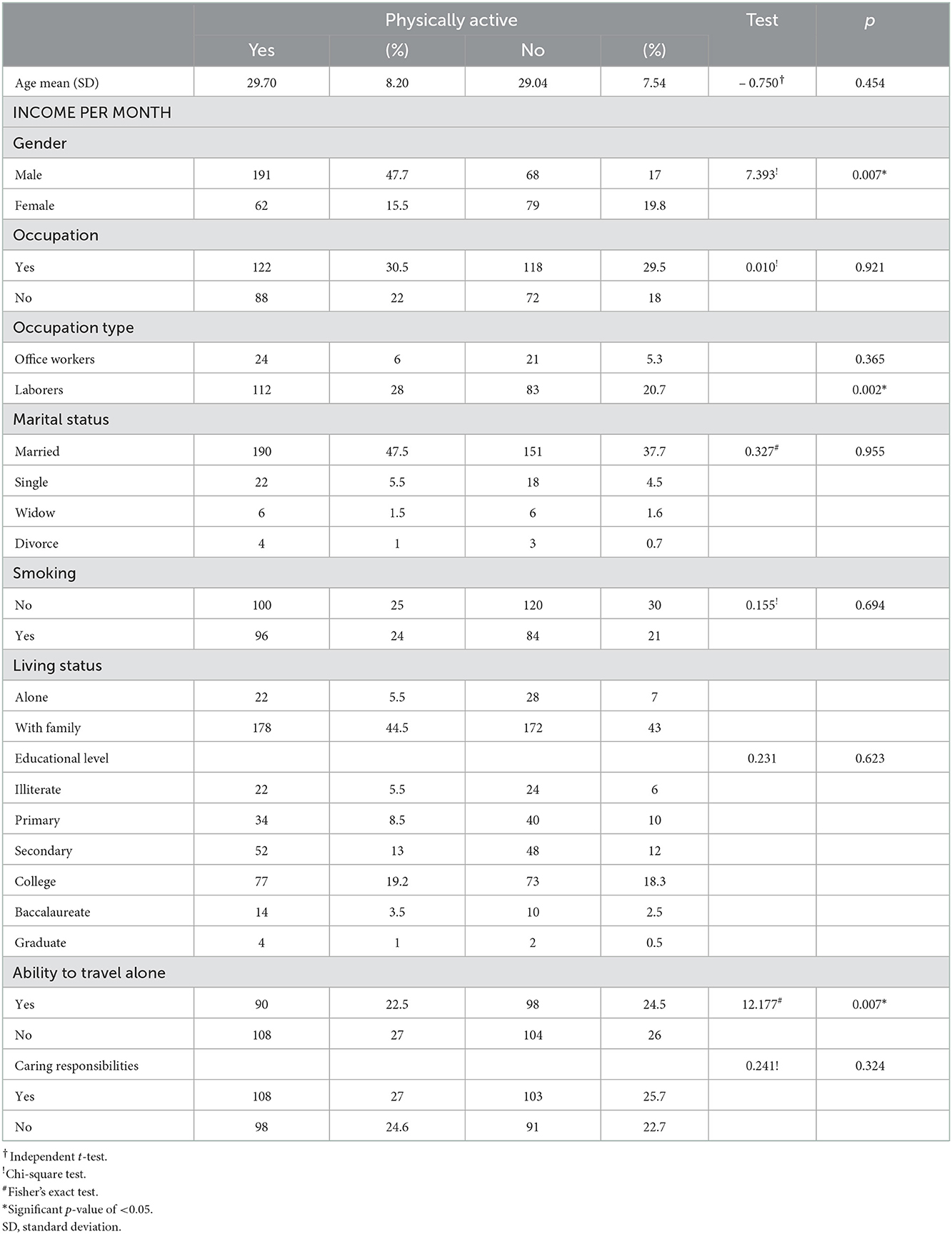
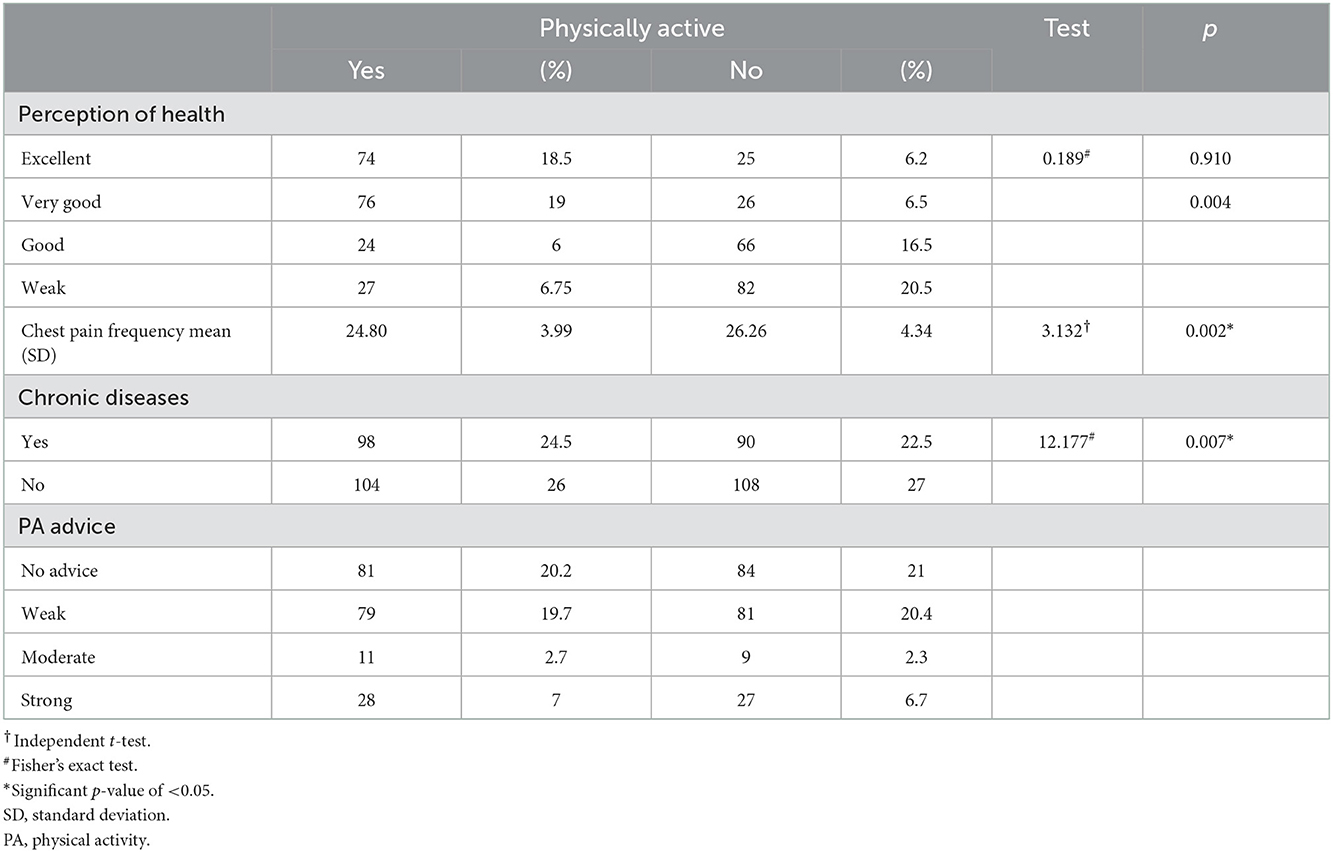
The influence of patient's characteristics on PA status
It was found that male respondents and laborers were significantly more engaged in PA than females and office workers. Also, there was a statistically significant difference between physically active and non-physically active participants regarding physical activity advice, chest pain frequency, and perception of health. Patients with weak PA advice perceive their health as poor and have more chest pain frequency. They also have low PA levels. However, other factors such as marital status and smoking showed no statistically significant relationship with PA engagement (Tables 3, 4).
The association between PA status and perceived benefits of and barriers to PA
There was a significant difference between physically active and non-physically active participants regarding PA's psychological and social benefits. Physically active patients perceive these benefits more than non-physically active patients. However, no significant difference between the two groups of patients was detected as regards the physical benefits of PA, such as “preventing overweight,” “decreasing the risk of coronary artery disease,” and “decreasing triglycerides.” Improving knowledge about the physiological benefits of PA is an essential element that should be included in the PA programs provided to patients with CHD.
While regarding perceived barriers items about performing PA, physically active and non-physically active participants were significantly different regarding most of the perceived barriers to PA. Physically active patients exhibited fewer physical, psychological, social, and environmental barriers to the perception of PA than non-physically active participants.
Perceived benefits of and barriers to PA
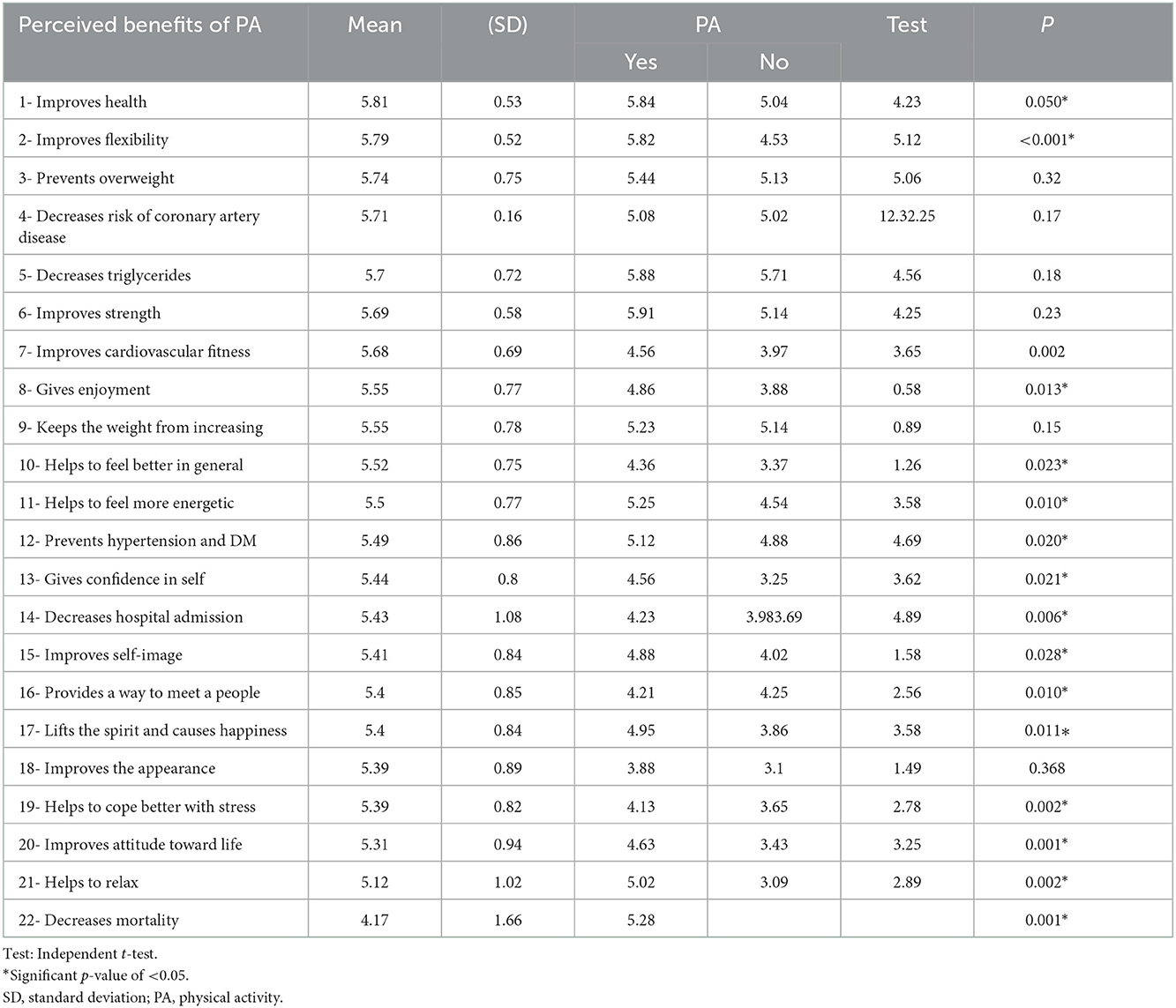
Most of the benefits perceived by patients with CHD were physiological benefits, such as “improves health” (M = 5.81, SD = 0.53) “improves body muscle's flexibility” (M = 5.79, SD = 0.52), “improves strength” (M = 5.69, SD = 0.58), “prevents overweight” (M = 5.74, SD = 0.75), “decreases risk of CHD” (M = 5.71, SD = 0.16), “decreases triglycerides” (M = 5.70, SD = 0.72), and “improves cardiovascular fitness” (M = 5.68, SD = 0.69) (Table 5).
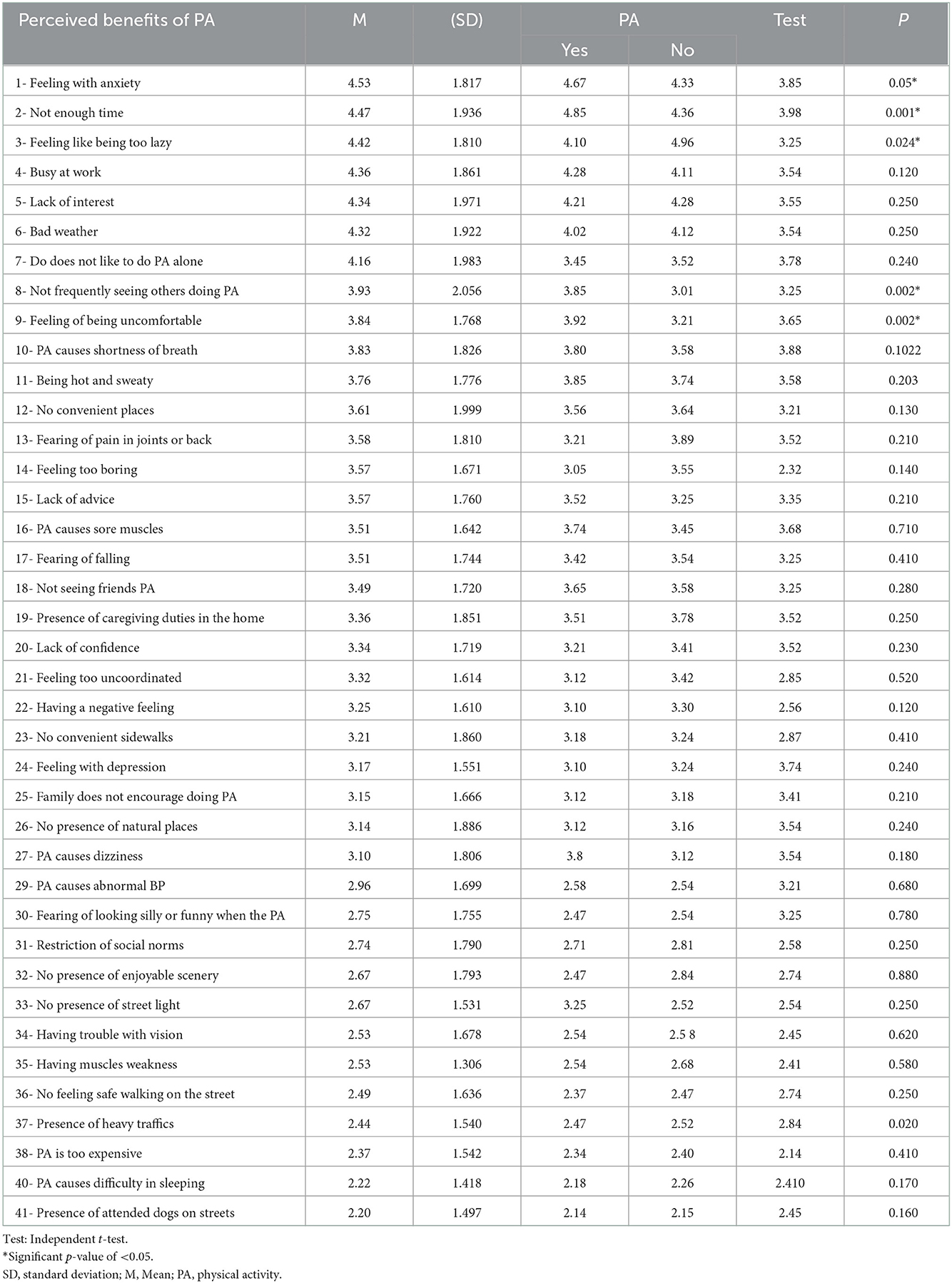
The biggest barriers to PA as perceived by the patients were as follows: “feeling with anxiety” (M = 4.53, SD = 1.81), “not enough time” (M = 4.47, SD = 1.93), “feeling of being too lazy” (M = 4.42, SD = 1.81), “busy at work” (M = 4.36, SD = 1.86), “lack of interest” (M = 4.34, SD = 1.97), “bad weather” (M = 4.32, SD = 1.92), “don't like to do PA alone” (M = 4.16, SD = 1.98), “not frequently seeing others perform PA” (M = 3.93, SD = 2.05), “feeling of being uncomfortable” (M = 3.84, SD = 1.76), and “PA causes shortness of breath” (M = 3.83, SD = 1.82) (Table 6).
The influence of sociodemographic and health characteristics on perceived benefits of PA among Jordanian patients with CHD
Job type significantly influenced the perceived benefits of “decreasing triglycerides” and “giving enjoyment.” Laborer workers perceived this PA benefits more than office workers. Physically active participants perceived all physiological benefits more than non-physically active participants.
The influence of sociodemographic and health characteristics on perceived barriers to PA
This study demonstrated the importance of sociodemographic and health characteristics of patients with CHD in influencing their perception of barriers to PA, including (1) health perception, (2) chest pain, (3) the ability to travel alone, (4) education, (5) age, (6) gender, (7) caring responsibilities, (8) job status, (9) current PA behavior, (10) smoking, and (1) PA advice. Health perception had a significant negative relationship with the barriers “feeling with anxiety” and “PA causes shortness of breath”. Patients with poor health were more likely to perceive “feeling with anxiety” and “PA causes shortness of breath” as solid barriers to PA. Chest pain frequency had a significant positive relationship with “feeling uncomfortable” barriers and “PA causes shortness of breath.” Participants who reported more chest pain frequency were more likely to perceive “feeling uncomfortable” and “PA causes shortness of breath” as solid barriers to PA. Age is negatively related to “busy at work” and “not enough time” barriers. Young participants were more likely to perceive “busy at work” and “not enough time” as solid barriers to PA. No significant relationships with other barriers were found.
Females, illiterate, patients who could not travel alone, smokers, and non-regular physically active perceived “feeling uncomfortable” and “not enough time” as barriers to PA more than their counterparts. Illiterates and individuals who are unable to travel alone perceived “feeling anxiety” as a barrier to PA more than educated individuals who were able to travel alone. Illiterate and non-regular physically active perceived “PA causes shortness of breath” as a barrier to PA more than educated and regular physically active. Individuals who had caring responsibilities perceived being busy at work as a barrier to PA more than those who were not employed and did not have caring responsibilities. Office workers perceived bad weather as a barrier to PA more than laborers workers. PA advice had a significant negative relationship with barriers such as “not enough time,” “feeling of being uncomfortable,” “lack of advice,” and “feeling too boring.”
Discussion
Although physical activity is widely reported as a principal factor in improving health, it is viewed as a significant challenge for patients with CHD worldwide. This study found that patients were mainly physically inactive (76%). Perceived benefits of and barriers to PA are vital elements influencing PA participation in this study. The physically active patients perceive more benefits of and fewer barriers to PA than non-physically participants. However, no study documented the perceived benefits of and barriers to PA in Jordan among patients with CHD.
All participants in this study reported substantial perceived benefits of PA that were mainly physiological benefits rather than psychosocial benefits, which may be related to the influence of media components that focus on the physiological benefits of PA. Therefore, patients may have more information about the physiological benefits of PA than the psychological benefits of PA. However, physically active patients perceived the physiological and psychosocial benefits of PA more than those who were not regularly physically active. In addition, it may be related that most participants (76%) were not regularly physically active to experience PA's physiological and psychosocial benefits. The role of healthcare providers in reinforcing the knowledge about the impact of physical and psychosocial benefits of PA is a crucial step to be considered in PA programs.
A predominance of perceived psychosocial barriers to PA was observed were “anxiety,” “lack of interest,” “feeling of being too lazy,” “do not like to do PA alone,” and “not frequently seeing others doing PA.” These barriers were also identified in Myers and Roth's studies (26). Anxiety reflects that patients may feel anxious about fear from fatigue or other symptoms when they do PA because they have CHD. “Feeling of being too lazy” reflects that patients have low motivation and negative feelings that inhibit them from PA.
Not enough time was reported in the present study. As such, the need for positive reinforcement and reassurance from healthcare providers who advocate physical activity in CHD is considered necessary to overcome this barrier. The time barrier reflects that individuals are busy at work, which is also perceived as a barrier to PA. It reflects no motivation to do PA because time barriers and busyness at work excuse more than the cause of not participating in PA, which is congruent with the findings of other studies, which showed that time was the most significant barrier perceived by cardiac patients. It is the most prevalent self-reported reason for dropout from supervised clinical and community PA programs (31, 32). Motivation to do PA is predominately prescribed as a barrier to doing PA among adult people (32). The barriers of “lack of interest,” “do not like to do PA alone,” and “not frequently seeing others doing PA” reflect the importance of social support in motivating patients to use PA. It was demonstrated that social support was significantly associated with physical activity behavior (33–35). The physical barriers PA perceived were “feeling of being uncomfortable” and “shortness of breath”. This finding is congruent with the literature, which showed that physical problems were one of the most significant barriers to PA (36–38). Physical barriers that are frequently reported in the literature include fatigue (36), being uncomfortable (37, 38), lacking energy, and shortness of breath (38). After CHD, patients may feel too weak for PA and fear that PA will lead to cardiac events. This feeling may decrease their self-efficacy with PA. Decreased self-efficacy may increase the perception of physical barriers. On the contrary, regular PA could improve self-efficacy to perform PA; thus, the barrier of low self-efficacy may be diminished (39). The result that could be noticed in this study is that the participants who are not physically active perceive a lack of confidence as a barrier to PA more than the physically active participants. The environmental concern of bad weather was strongly perceived as a significant barrier to PA. This finding is congruent with other findings (18). Since some patients have no unique places or closed centers to perform PA as alternatives to brisk outdoor walking, bad weather may be an essential concern. In addition, bad weather seems to reflect no attention and excuses more than barriers to PA.
Conclusion
This study demonstrated that most patients with CHD (74%) are non-physically active. The challenge of participation in PA was linked to perceived benefits and barriers to PA. The patients in this study perceived various physiological and psychosocial benefits of PA. Also, Jordanian patients with CHD perceived different physical and psychosocial barriers to PA. In addition, it was found that the sociodemographic and health characteristics of the patients with CHD influenced their participation in PA and their perception of PA benefits and barriers to PA. The factors such as age, gender, health perception, chest pain frequency, education, job, PA advice, caring responsibilities, ability to travel alone, smoking, and current PA behavior were considered. It seems that different groups with samples perceived different barriers to PA. The findings of this study suggest that it may be valuable to replicate this study using a more significant and heterogeneous randomly selected sample to increase the generalization of the findings. The findings also suggest investigating barriers to PA as perceived by different groups of people (young, old, female, and educated people) to identify their specific perceived barriers to PA and investigate selected interventions that are appropriate to decrease barriers to PA among patients with CHD. Also, the findings of this study indicate the need for an influential role for nurses and other health team members who provide care to patients with CHD in Jordanian hospitals and clinics. This role should consider the benefits of and barriers to PA and the influence of sociodemographic and health characteristics on perceived barriers to PA in their interventions to motivate the patients to participate in regular PA.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board at King Abdullah University Hospital (KAUH) and Jordan University Hospital Administration. The patients/participants provided their written informed consent to participate in this study.
Author contributions
EA planned the research, carried out the data collection, analyzed the data, and wrote the manuscript. FB reviewed the paper for publication. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Shiroma EJ, Lee IM. Physical activity and cardiovascular health: lessons learned from epidemiological studies across age, gender, and race/ethnicity. Circulation. (2010) 122:743–52. doi: 10.1161/CIRCULATIONAHA.109.914721
2. British Association for Cardiovascular Prevention and Rehabilitation. BACPR Standards and Core Components for Cardiovascular Disease Prevention and Rehabilitation 2012. 2nd ed. UKBACPR (2012). Available online at: www.bacpr.com/resources/46C_BACPR_Standards_and_Core_Components_2012.pdf.GoogleScholar (accessed September 10, 2022).
3. Amidei CB, Trevisan C, Dotto M, Ferroni E, Noale M, Maggi S, et al. Association of physical activity trajectories with major cardiovascular diseases in elderly people. Heart. (2022) 108:360–6. doi: 10.1136/heartjnl-2021-320013
4. World Health Organization. Global Action Plan on Physical Activity 2018-2030: More Active People for a Healthier World. World Health Organization (2019).
5. Börjesson M, Onerup A, Lundqvist S, Dahlöf B. Physical activity and exercise lower blood pressure in individuals with hypertension: narrative review of 27 RCTs. Br J Sports Med. (2016) 50:356–61. doi: 10.1136/bjsports-2015-095786
6. Tian D, Meng J. Exercise for prevention and relief of cardiovascular disease: prognoses, mechanisms, and approaches. Oxid Med Cell Longev. (2019) 2019:3756750. doi: 10.1155/2019/3756750
7. Franklin B, Bonzheim K, Warren J, Haapaniemi S, Byl N, Gordon N. Effects of a contemporary, exercise-based rehabilitation and cardiovascular risk-reduction program on coronary patients with abnormal baseline risk factors. Chest. (2002) 122:338–43. doi: 10.1378/chest.122.1.338
8. Clark AM, Haykowsky M, Kryworuchko J, MacClure T, Scott J, DesMeules M, et al. meta-analysis of randomized control trials of home-based secondary prevention programs for coronary artery disease. Eur J Cardiovasc Prev Rehabil. (2010) 17:261–70. doi: 10.1097/HJR.0b013e32833090ef
9. Fagard RH, Cornelissen VA. Effect of exercise on blood pressure control in hypertensive patients. Eur J Prev Cardiol. (2007) 14:12–7. doi: 10.1097/HJR.0b013e3280128bbb
10. Nystoriak MA, Bhatnagar A. Cardiovascular effects and benefits of exercise. Front Cardiovasc Med. (2018) 5:135. doi: 10.3389/fcvm.2018.00135
11. Walther C, Gielen S, Hambrecht R. The effect of exercise training on endothelial function in cardiovascular disease in humans. Exerc Sport Sci Rev. (2004) 32:129–34. doi: 10.1097/00003677-200410000-00002
12. Jeong SW, Kim SH, Kang SH, Kim HJ, Yoon CH, Youn TJ, et al. Mortality reduction with physical activity in patients with and without cardiovascular disease. Eur Heart J. (2019) 40:3547–55. doi: 10.1093/eurheartj/ehz564
13. Winzer EB, Woitek F, Linke A. Physical activity in the prevention and treatment of coronary artery disease. J Am Heart Assoc. (2018) 7:e007725. doi: 10.1161/JAHA.117.007725
14. Thompson PD, Buchner D, Piña IL, Balady GJ, Williams MA, Marcus BH, et al. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: a statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity). Circulation. (2003) 107:3109–16. doi: 10.1161/01.CIR.0000075572.40158.77
15. Arrigo I, Brunner-LaRocca H, Lefkovits M, Pfisterer M, Hoffmann A. Comparative outcome one year after formal cardiac rehabilitation: the effects of a randomized intervention to improve exercise adherence. Eur J Prev Cardiol. (2008) 15:306–11. doi: 10.1097/HJR.0b013e3282f40e01
16. Won MH. Mediating effect of physical activity in the relationship between depressive symptoms and health-related quality of life in patients with coronary artery disease: the 2016 nationwide community health survey in Korea. Kor J Adult Nurs. (2019) 31:691–700. doi: 10.7475/kjan.2019.31.6.691
17. Guiraud T, Granger R, Gremeaux V, Bousquet M, Richard L, Soukarie L, et al. Accelerometer as a tool to assess sedentarity and adherence to physical activity recommendations after cardiac rehabilitation program. Ann Phys Rehabil Med. (2012) 55:312–21. doi: 10.1016/j.rehab.2012.05.002
18. Kotseva K, Wood D, De Backer G, De Bacquer D, Pyorala K, Keil U, et al. Cardiovascular prevention guidelines in daily practice: a comparison of EUROASPIRE I, II and III surveys in eight European countries. Lancet. (2009) 373:929–40. doi: 10.1016/S0140-6736(09)60330-5
19. Mosleh SM, Darawad M. Patients' adherence to healthy behavior in coronary heart disease: risk factor management among Jordanian patients. J Cardiovasc Nurs. (2015) 30:471–8. doi: 10.1097/JCN.0000000000000189
20. Sherwood NE, Jeffery RW. The behavioral determinants of exercise: implications for physical activity interventions. Annu Rev Nutr. (2000) 20:21–44. doi: 10.1146/annurev.nutr.20.1.21
21. Thomas RJ, King M, Lui K, Oldridge N, Piña IL, Spertus J, et al. AACVPR/ACC/AHA 2007 performance measures on cardiac rehabilitation for referral to and delivery of cardiac rehabilitation/secondary prevention services: endorsed by the American college of chest physicians. American college of sports medicine, American physical therapy association, Canadian association of cardiac rehabilitation, European association for cardiovascular prevention and rehabilitation, inter-American heart foundation, national association of clinical nurse specialists, preventive. J Am Coll Cardiol. (2007) 50:1400–33. doi: 10.1016/j.jacc.2007.04.033
22. Wenger NK. Current status of cardiac rehabilitation. J Am Coll Cardiol. (2008) 51:1619–31. doi: 10.1016/j.jacc.2008.01.030
24. Lusk SL, Ronis DL, Hogan MM. Test of the health promotion model as a causal model of construction workers' use of hearing protection. Res Nurs Health. (1997) 20:183–94. doi: 10.1002/(SICI)1098-240X(199706)20:3<183::AID-NUR2>3.0.CO;2-E
25. McEwen M, Nies MA. Community/Public Health Nursing - E-Book: Promoting the Health of Populations. 5th ed. Saunders, an imprint of Elsevier Inc. (2013). Available onine at: https://books.google.com.eg/books?isbn_0323293883 (accessed September 10, 2022).
26. Myers RS, Roth DL. Perceived benefits of and barriers to exercise and stage of exercise adoption in young adults. Health Psychol. (1997) 16:277. doi: 10.1037/0278-6133.16.3.277
27. De Bourdeaudhuij I, Sallis J. Relative contribution of psychosocial variables to the explanation of physical activity in three population-based adult samples. Prev Med. (2002) 34:279–88. doi: 10.1006/pmed.2001.0979
28. Evenson KR, Fleury J. Barriers to outpatient cardiac rehabilitation participation and adherence. J Cardiopulm Rehabil Prev. (2000) 20:241–6. doi: 10.1097/00008483-200007000-00005
29. Salmon J, Owen N, Crawford D, Bauman A, Sallis JF. Physical activity and sedentary behavior: a population-based study of barriers, enjoyment, and preference. Health Psychol. (2003) 22:178. doi: 10.1037/0278-6133.22.2.178
30. Sharma SK, Mudgal SK, Thakur K, Gaur R. How to calculate sample size for observational and experimental nursing research studies. Natl J Physiol Pharm Pharmacol. (2020) 10:1–8. doi: 10.5455/njppp.2020.10.0930717102019
31. Kelly S, Martin S, Kuhn I, Cowan A, Brayne C, Lafortune L. Barriers and facilitators to the uptake and maintenance of healthy behaviours by people at mid-life: a rapid systematic review. PLoS ONE. (2016) 11:e0145074. doi: 10.1371/journal.pone.0145074
32. Fraser MJ, Leslie SJ, Gorely T, Foster E, Walters R. Barriers and facilitators to participating in cardiac rehabilitation and physical activity: a cross-sectional survey. World J Cardiol. (2022) 14:83. doi: 10.4330/wjc.v14.i2.83
33. Teleki S, Zsidó AN, Lénárd L, Komócsi A, Kiss EC, Tiringer I. Role of received social support in the physical activity of coronary heart patients: The Health Action Process Approach. Appl Psychol Health WellBeing. (2022) 14:44–63. doi: 10.1111/aphw.12290
34. Chair SY, Wong KB, Tang JY, Wang Q, Cheng HY. Social support as a predictor of diet and exercise self-efficacy in patients with coronary artery disease. Contemp Nurse. (2015) 51:188–99. doi: 10.1080/10376178.2016.1171726
35. Aggarwal B, Liao M, Mosca L. Predictors of physical activity at 1-year in a randomized controlled trial of family members of patients with cardiovascular disease. J Cardiovasc Nurs. (2010) 25:444. doi: 10.1093/med/9780199238439.003.0006
36. Stewart R, Held C, Brown R, Vedin O, Hagstrom E, Lonn E, et al. Physical activity in patients with stable coronary heart disease: an international perspective. Eur Heart J. (2013) 34:3286–93. doi: 10.1093/eurheartj/eht258
37. LaPier TK, Wintz G, Holmes W, Cartmell E, Hartl S, Kostoff N, et al. Analysis of activities of daily living performance in patients recovering from coronary artery bypass surgery. Phys Occup Ther Geriatr. (2008) 27:16–35. doi: 10.1080/02703180802206215
38. Gray E, Dasanayake S, Sangelaji B, Hale L, Skinner M. Factors influencing physical activity engagement following coronary artery bypass graft surgery: a mixed methods systematic review. Heart & Lung. (2021) 50:589–98. doi: 10.1016/j.hrtlng.2021.04.006
Keywords: physical activity, perceived benefits, perceived barriers, coronary heart disease, prevalence
Citation: Alsaleh E and Baniyasin F (2023) Prevalence of physical activity levels and perceived benefits of and barriers to physical activity among Jordanian patients with coronary heart disease: A cross-sectional study. Front. Public Health 10:1041428. doi: 10.3389/fpubh.2022.1041428
Received: 10 September 2022; Accepted: 28 November 2022;
Published: 04 January 2023.
Edited by:
Yihui Du, University Medical Center Groningen, NetherlandsReviewed by:
Sandheep Sugathan, Quest International University Perak, MalaysiaXiaomin Song, BeiGene, China
Copyright © 2023 Alsaleh and Baniyasin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eman Alsaleh,  ealsaleh@philadelphia.edu.jo
ealsaleh@philadelphia.edu.jo
 Eman Alsaleh
Eman Alsaleh