
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 28 November 2024
Sec. Sleep Disorders
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1485822
This article is part of the Research TopicBeyond Rest: Exploring the Bidirectional Relationship and Intersecting Pathways of Sleep and Physical HealthView all 8 articles
Background: Pain is one of the most prevalent symptoms that disrupt daily functioning and has been increasing in prevalence. Sleep disturbances frequently occur in individuals with pain, making it difficult to initiate and maintain sleep. This study aims to examine the bidirectional correlation between pain and sleep quality/duration among middle-aged and older Chinese adults
Participants and setting: This study analyzed data from individuals aged 45 years and above who participated in both the 2018 and 2020 baseline surveys of China Health and Retirement Longitudinal Study (CHARLS).
Methods: The bidirectional association between pain and sleep disturbance was assessed using multivariate logistic regression models, adjusting for various covariates.
Results: Among individuals without pain, those with unsatisfactory sleep quality were more likely to experience future pain, with an adjusted odds ratio (OR) of 1.74 (95% CI: 1.57 - 1.92). Conversely, among individuals with satisfactory sleep quality, those with pain were more likely to develop unsatisfactory sleep quality in the future, with an adjusted OR of 1.87 (95% CI: 1.69 - 2.07). Additionally, shorter sleep duration (<6 hours) was significantly associated with pain status (OR=1.39; 95% CI: 1.28 - 1.50). The incidence of developing short sleep duration in individuals with pain was also higher (OR=1.49; 95% CI: 1.38 - 1.61).
Conclusions: This research revealed a bidirectional relationship between pain and sleep disturbance in middle-aged and older Chinese adults, where each condition exacerbated the other. Recognizing and addressing this interconnected relationship was essential for effective management of both pain and sleep quality in this population.
Pain is one of the most prevalent symptoms that disrupt daily functioning, and its prevalence is steadily increasing. In China, approximately 30% of the population experiences pain (1, 2). Similarly, international studies show that pain conditions affect about 30% of American adults (3), 19% of European adults (4), around 18% of Australian adults (5), 12% of Spaniards, and 42% of Britons (6). These prevalence rates vary depending on specific non-malignant pain conditions, with higher rates observed particularly among women and older adults (7). Among Chinese individuals aged over 65 years, it is estimated that 80-85% suffer from pain-related ailments (8).
As people age, their physical and mental states undergo changes, and with the accelerating pace of modern life, an increasing number of middle-aged and elderly individuals are encountering sleep disturbance. Sleep disturbance is commonly observed in individuals with pain, creating significant challenges in both initiating and maintaining sleep amidst painful stimuli. The prevalence of sleep disturbance among those experiencing pain is alarmingly high, with reports indicating levels ranging from 50% to 70% even in clinical cohorts with milder pain conditions (9). Additionally, research has shown that the prevalence of sleep disturbance among individuals over 60 years old in China is 47.2% (10).
Although pain is often considered the primary cause of sleep disturbance, evidence from both animal and human studies suggests a more complex relationship. A bidirectional relationship exists, where pain disrupts sleep, and sleep deprivation or disorders, in turn, exacerbate pain (11–13). Over the past decade, numerous retrospective studies have examined the association between sleep and pain, emphasizing the need for longitudinal research to better understand their interplay (9, 14). Given the current aging population in China, there is a growing need tosl focus on elderly individuals who experience pain. However, most research on pain among elderly Chinese individuals has predominantly relied on cross-sectional surveys in recent years (15), with limited investigation into the progression of pain over time. This gap in evidence can be addressed through more rigorous longitudinal data collection and advancements in analytical methodologies (16).
Therefore, the objective of this study is to investigate the bidirectional correlation between pain and sleep quality/duration in elderly individuals using data from the China Health and Retirement Longitudinal Study (CHARLS).
The data utilized in this study was derived from CHARLS, which employed a random sampling strategy to collect nationally representative, high-quality microdata from Chinese households. This is a national baseline survey, conducted every three years since 2011, encompassing a total of 450 communities (including villages) across 150 counties spanning over 28 provinces. The study included individuals aged 45 years and above who participated in both the CHARLS baseline surveys conducted in 2018 and 2020.
Participants who satisfied the following conditions were considered eligible for participation in this study: (1) comprehensive collection of demographic information, lifestyle factors, and health behavior data; (2) provision of responses regarding pain status, sleep quality, and sleep duration. Individuals were excluded if they lacked any of the relevant data mentioned above. Ultimately, 15,330 participants from the 2018 and 2020 waves of the survey were included to explore the correlation between pain and sleep quality/duration.
In the first stage, participants who did not report any pain symptoms at the 2018 baseline were selected to examine the relationship between sleep quality/duration and the subsequent development of pain, resulting in a total of 10,801 eligible individuals. In the second stage, a subset of 8,262 participants with good baseline sleep quality was identified to investigate the relationship between pain and subsequent sleep quality/duration. The research received ethical approval from the Biomedical Ethics Committee at Peking University, with the fieldwork protocol also approved (Approval number: IRB00001052-11015). A detailed flowchart of the study design is presented in Figure 1
The definitions and manifestations of pain are diverse, and in this study. In this study, the pain issues addressed in the CHARLES questionnaire were precisely defined and utilized as the focus of research (17–19). According to the questionnaire, participants were inquired about their pain-related discomfort level: “ Are you often troubled with anybody pains? None? A little? Somewhat? Quite a bit? Very?” For this question, the term “pain” in this context encompasses the sensation experienced throughout various regions of the body.
The diagnosis of sleep disturbance in this study was based on the CHARLES questionnaire, with a focus on the sleep-related issues encompassed within the questionnaire serving as the research subject matter. The evaluation of the duration and quality of sleep was based on question: “My sleep was restless.” and “During the past month, how many hours of actual sleep did you get at night?” The available choices for indicating one’s self-reported sleep quality encompassed rarely or none of the time (< 1day), some or a little of the time (1–2days), occasionally or a moderate amount of the time (3–4days), and most or all of the time (5–7days). The quality of sleep was categorized as either ‘satisfactory’ (occurring rarely or not at all, less than 1 day per week) or ‘unsatisfactory’ (occurring at least once a week). In accordance with previous research, nighttime duration of sleep was divided into three categories: insufficient (<6h), medium (6-9h), and sufficient (>9h).
The covariates analyzed in this research were categorized into demographic factors, data related to lifestyle variables and health behavior-related information. Demographic data include age, gender, educational level, marital status and residential regions. Lifestyle variables and health behavior-related information include labor force status, social interaction, alcohol consumption, smoking status, accident condition, and chronic disease history.
Age groups were categorized as follows: 45-64 years and 65 years or older. Educational level was categorized into four categories: Uncompleted primary education, primary education, secondary education and higher education. The marital status was categorized into two categories: other and married. Residential regions were categorized into rural and urban. The labor force status was classified into two categories: agricultural employment and non-agricultural employment or unemployment.
The social interaction was classified as either absent or occurring more than once a month. Regarding the consumption of alcohol, the term “drinking” was used to describe individuals who consumed beer, wine, or liquor at least once a month. Those who did not meet these criteria were categorized as “no drinking”. The term “smoking” was defined as engaging in the current or past behavior of using tobacco products. On the other hand, the term “no smoking” referred to individuals who did not engage in any form of tobacco use. Accident condition was classified into no accidents and previous accidents history (such as vehicular collision, accidental injury, history of falls or fractures). Chronic diseases were categorized as either having no or one concurrent chronic disease, or as having multiple comorbidities. Multimorbidity referred to the presence of two or more chronic diseases concurrently within an individual.
Categorical variables were represented by frequencies and percentages, while continuous variables with a normal distribution were represented by means and medians. The Chi-square tests were utilized to compare the baseline characteristics. Binary logistic regression models were employed to analyze the association between baseline sleep quality/duration and subsequent pain status. Additionally, the study developed binary logistic regression models to determine whether baseline pain status could predict poor sleep quality. For sleep duration, multinomial regression models were employed to relationship the association between baseline pain and duration of sleep status. The findings were reported as odds ratios (ORs) accompanied by 95% confidence intervals (CIs). Statistical analysis was performed using SPSS software, and a significance P level of less than 0.05 was used to determine statistical significance.
The baseline characteristics of individuals without pain are summarized in Table 1. A total of 10,801 participants were included in this stage of the study, with 5,713 (52.89%) reporting good sleep quality and 5088 (47.11%) reporting poor sleep quality. Individuals with satisfactory sleep quality were more likely to be men, have higher education levels, be married, lived in rural, engage in non-agricultural activities or be unemployed, be current or former smokers or drinkers, have no history of accidents, and be free from multimorbidity.
During the follow-up period, 770 (13.5%) participants with satisfactory sleep quality at baseline developed pain symptoms, compared to 1,124 (22.1%) participants with unsatisfactory sleep quality, who showed a significantly higher prevalence of future pain symptoms (P < 0.001).
The baseline characteristics of individuals with satisfactory sleep quality are detailed in Table 1. In this stage, 8,262 participants were included, of whom 5,088 (61.58%) were pain-free, and 3174 (38.42%) reported experiencing pain. Factors associated with a higher likelihood of developing pain included advanced age, being female, lower educational attainment, unmarried status, residing in urban areas, working in agriculture, limited social interactions, non-smoking or non-drinking habits, history of accidents, and the presence of multiple health conditions.
During the follow-up period, 3192 (62.7%) individuals without pain continued to experience poor sleep quality, whereas the prevalence of poor sleep quality was significantly higher among those with pain (2444 participants, 77.0%). Individuals with pain were found to have a significantly increased risk of developing future unsatisfactory sleep quality compared to those without pain (P < 0.001).
Among individuals without pain, those with unsatisfactory sleep quality at baseline were found to have a higher risk of developing pain, with a crude odds ratio (OR) of 1.82 (95% CI, 1.65–2.01). This association persisted after adjusting for covariates, with adjusted ORs of 1.74 (95% CI, 1.57–1.92), 1.73 (95% CI, 1.56–1.91), 1.72 (95% CI, 1.55–1.91), and 1.64 (95% CI, 1.48–1.82) across models 1, 2, 3, and the fully adjusted model 4, respectively (Table 2).
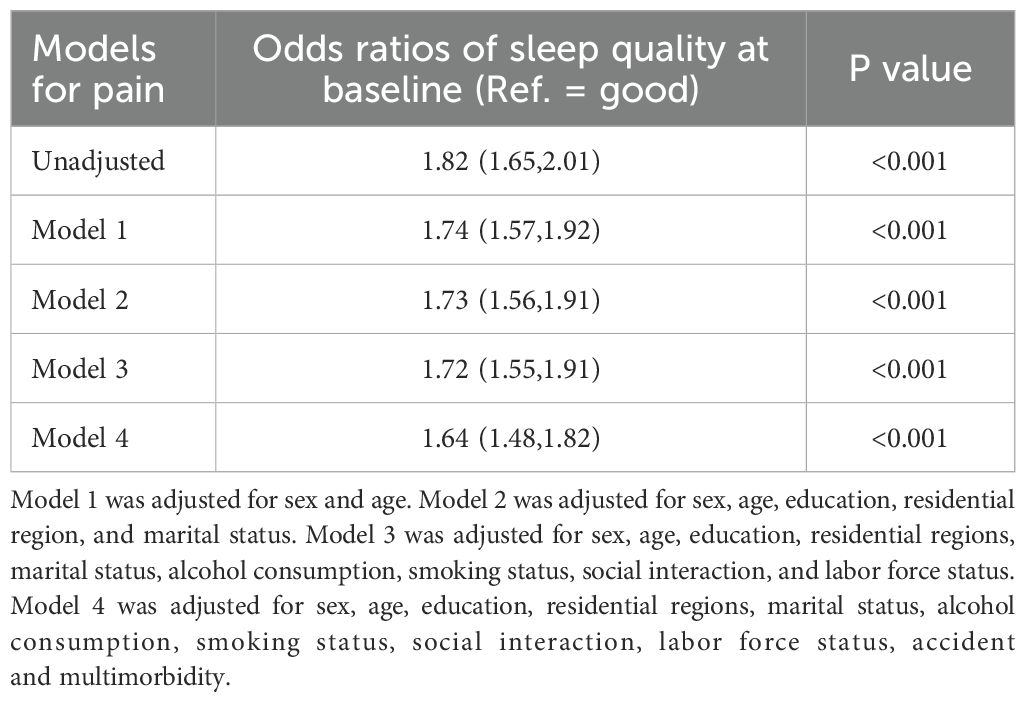
Table 2. Longitudinal association between sleep quality at baseline and risk of pain status (N = 10801).
Among individuals with satisfactory sleep quality at baseline, those with pain were found to be at an increased risk of developing future unsatisfactory sleep quality, with a crude OR of 1.99 (95% CI, 1.80–2.20). This association remained significant after adjusting for covariates, with adjusted ORs of 1.87 (95% CI, 1.69–2.07), 1.91 (95% CI, 1.72–2.11), 1.91 (95% CI, 1.72–2.11), and 1.81 (95% CI, 1.63–2.01) in models 1, 2, 3, and the fully adjusted model 4, respectively (Table 3).
Using individuals with a sleep duration of 6–9 hours per night as the reference group, it was found that shorter sleep duration was associated with an increased risk of developing pain. This effect persisted even after adjusting for covariates (OR = 1.39; 95% CI, 1.28–1.50). However, no statistically significant difference in future pain status was observed between individuals with sleep durations of 6–9 hours and those with sleep durations exceeding 9 hours (Table 4).
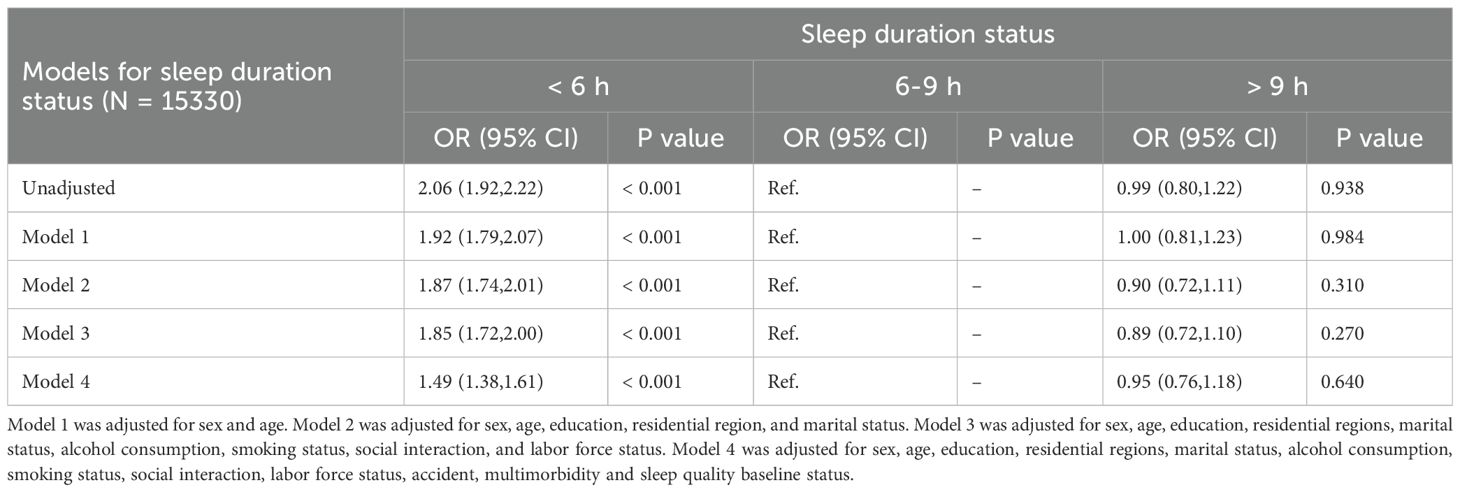
Table 4. Longitudinal association between sleep duration status at baseline and pain status (N = 15330).
The impact of baseline pain status on nighttime sleep duration is presented in Table 5. Individuals without pain served as the reference group. The analysis revealed a significantly higher incidence of short sleep duration (< 6 hours) in individuals with pain. After adjusting for covariates, this association remained significant (OR = 1.49; 95% CI, 1.38–1.61) (Table 5).
Pain is a complex neurological response that leads to unpleasant sensations (20) and is widely recognized as one of the most common and disabling symptoms in medicine (21–23). Chronic somatic pain can progressively result in physical disability, depression, and sleep disturbance (20, 24, 25). This study identified a significant bidirectional association between sleep and pain, supported by a large sample size of longitudinal follow-up data. The findings remained consistent even after adjusting for baseline variables. These adjustments further reinforced our ability to reveal the intricate relationship between sleep disturbance and pain status.
Epidemiological studies had established that poor sleep was associated with a heightened susceptibility to experiencing pain (26). Persistent sleep disturbance and pain are believed to have a reciprocal relationship, where sleep disturbance heighten an individual’s susceptibility to pain (27). Consistent with our findings, there is a bidirectional correlation between the duration, frequency, and quality of sleep disturbance and the severity and location of pain (28). For instance, VINSTRUP et al. conducted a prospective cohort study involving 1,955 medical staff and observed a significant association between poor sleep quality and the incidence of back pain (29). Furthermore, studies have indicated a negative correlation between pain sites and sleep quality.
An increase in pain reports is often observed with a reduction in sleep duration (30, 31). In a study involving 1,773 adolescents, AUVINEN et al. identified insufficient sleep duration or poor sleep quality as independent risk factors for back pain (32). The duration and frequency of sleep disturbance show a significant association with somatic pain, with stronger effects observed in cases of prolonged duration and higher frequency of sleep disturbance (33). Sleep disturbance led to heightened sensitivity to pain and impact the brain’s ability to perceive pain thresholds and inhibit pain. Shortened sleep duration results in central sensitization of nociception and a decrease in pain regulation, thereby increasing the risk of pain. Additionally, prolonged wakefulness acts as a primary driver of hyperalgesia, significantly amplifying pain perception (34, 35). There is compelling evidence that sleep disruptions negatively affect the body’s natural pain inhibition mechanisms, leading to an escalation in spontaneous pain, particularly among women (36).
Preoperative insomnia had been demonstrated as a reliable predictor of postoperative pain, and addressing sleep disturbance can effectively mitigate postoperative pain (37). A meta-analysis also revealed that sleep disruptions prior to surgery adversely affect the onset and intensity of persistent pain among individuals recovering from surgery (38). Research conducted on healthy individuals revealed a positive correlation between sleep restriction and a higher occurrence of newly emerging spontaneous pain (39).
The correlation between sleep and pain is bidirectional: pain hinders sleep quality, while insufficient sleep or sleep disturbance exacerbate pain perception. The potential link between sleep disturbance and pain may be attributed to oxidative stress. Oxidative stress can be triggered in the brain experiencing sleep deprivation (35), and the various biomarkers indicative of oxidative stress and redox status exhibit significant circadian rhythms (40). A previous study indicated that sleep deprivation could exert a significant influence on pressure pain thresholds and plasma oxidative stress markers among healthy adult residents (41). Staying awake at night can elevate oxidative stress levels, while sleep acts as a protective measure against its harmful effects. Moreover, specific brain structures are responsible for encoding both pain and sleep. The nucleus accumbens (NAc) receives sensorimotor and sleep-related inputs (42–44), and subsequently transmits signals to multiple brain regions involved in the processing of pain perception and sleep, suggesting a bidirectional relationship between insufficient sleep and altered pain perception (45). The presence of sleep problems is also associated with the severity of pain, and sleep issues have been found to predict worsening pain over time, with this effect being more pronounced in women compared to men and potentially mediated by fatigue (46).
In the Chinese population aged between middle age and elderly, a significant association between body pain and falls had been documented (8), aligning with our study’s findings of a history of accidental trauma. A bidirectional relationship exists between sleep quality and pain intensity with age, where pain experienced during the day significantly impacts sleep quality at night, and insufficient or poor sleep quality at night results in heightened pain levels the following day (47). The prevalence of pain symptoms tends to increase with advancing age, although not universally among older adults. Pain in the elderly is often associated with the onset of chronic conditions, as the incidence of chronic diseases rises with age, potentially exacerbating pain. This study suggested that sleep quality moderated the relationship between the number of chronic diseases and the extent of pain experienced. Patients with chronic diseases often face challenges such as reduced sleep quality and difficulty initiating sleep.
At baseline, women, agricultural workers, unmarried individuals, patients with a history of trauma, and those with multiple chronic diseases exhibited a higher likelihood of experiencing sleep disturbance and pain. Research has indicated that females are more susceptible to pain due to factors such as reduced muscle mass and lower bone density compared to males, increased engagement in daily household chores, heightened sensitivity to pain stimuli, greater willingness to report pain symptoms, and poorer response to analgesics (48, 49). Additionally, the interplay between physiological and psychosocial mechanisms may factors could potentially play a role in explaining differences in how males and females perceive pain (50). Other studies had also reported an inverse relationship between education level/manual labor intensity and pain experience. Individuals with lower educational attainment or those engaged in agricultural manual labor tend to exhibit higher rates of pain, possibly due to frequent outdoor physical exertion (51, 52).
Firstly, the concept of pain encompasses a broad spectrum of experiences, encompassing both chronic and episodic pain, as well as physical and psychological discomfort. No division was made into types of pain in this study. Sleep disturbance was identified on CHARLS questionnaires, not by polysomnography. The reliance on self-reported data for pain and sleep may result in certain deviations. However, previous studies have demonstrated that self-reported multiple illnesses exhibit good specificity in large-scale population baseline studies (41). Future research should aim to conduct more comprehensive investigations from various perspectives to measure sleep and pain accurately. Secondly, due to missing data for some quality-of-life scores, correlational analyses were not feasible, limiting our ability to fully understand how other factors interact with sleep and pain. Additionally, despite the longitudinal analysis conducted in this study to further elucidate the association between sleep quality, duration, and pain, there is an urgent requirement for a more extensive comprehension of the underlying mechanisms linking sleep and pain intensity to optimize pain management interventions. Therefore, additional studies should be undertaken to thoroughly analyze and clarify the causal pathways connecting sleep and pain intensity. Finally, as the sample is drawn from the Chinese population, it might be worth mentioning any potential differences that might arise in different ethnic or geographical populations.
The bidirectional correlation between poor sleep quality or insufficient sleep duration and pain in middle-aged and older Chinese adults was well established. We recommend focusing on sleep disturbance and pain in middle-aged and elderly patients while enhancing public awareness of sleep health and pain management. From a clinical perspective, this potential long-term bidirectional association emphasize the importance of evidence-based interventions targeting sleep and pain issues in older adults.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving humans were approved by Biomedical Ethics Committee at Peking University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
DY: Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. MY: Methodology, Writing – original draft, Writing – review & editing, Data curation, Formal analysis. QL: Formal analysis, Methodology, Writing – original draft, Writing – review & editing. HL: Data curation, Formal analysis, Writing – original draft. LK: Data curation, Formal analysis, Writing – original draft. QC: Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor JQ declared a shared parent affiliation with the authors DY and QL at the time of review.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Yongjun Z, Tingjie Z, Xiaoqiu Y, Zhiying F, Feng Q, Guangke X, et al. A survey of chronic pain in China. Libyan J Med. (2020) 15:1730550. doi: 10.1080/19932820.2020.1730550
2. Zis P, Daskalaki A, Bountouni I, Sykioti P, Varrassi G, Paladini A. Depression and chronic pain in the elderly: links and management challenges. Clin Interv Aging. (2017) 12:709–20. doi: 10.2147/cia.S113576
3. Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an internet-based survey. J Pain. (2010) 11:1230–9. doi: 10.1016/j.jpain.2010.07.002
4. Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. (2006) 10:287–333. doi: 10.1016/j.ejpain.2005.06.009
5. Blyth FM, March LM, Brnabic AJ, Jorm LR, Williamson M, Cousins MJ. Chronic pain in Australia: a prevalence study. Pain. (2001) 89:127–34. doi: 10.1016/s0304-3959(00)00355-9
6. Sharon H, Greener H, Hochberg U, Brill S. The prevalence of chronic pain in the adult population in Israel: an internet-based survey. Pain Res Manage. (2022) 2022:3903720. doi: 10.1155/2022/3903720
7. Lee KA. The need for longitudinal research on chronic pain and sleep disturbance. Sleep Med Rev. (2016) 26:108–10. doi: 10.1016/j.smrv.2015.10.006
8. Li W, Gamber M, Han J, Sun W, Yu T. The association between pain and fall among middle-aged and older chinese. Pain Manag Nurs. (2021) 22:343–8. doi: 10.1016/j.pmn.2020.10.004
9. Menefee LA, Cohen MJ, Anderson WR, Doghramji K, Frank ED, Lee H. Sleep disturbance and nonmalignant chronic pain: a comprehensive review of the literature. Pain Med. (2000) 1:156–72. doi: 10.1046/j.1526-4637.2000.00022.x
10. Liu Y, Dong YH, Li XY, Mao XQ, Liu L. Meta-analysis of the prevalence of sleep disorder among Chinese elderly aged 60 years and over. Modern Prev Med. (2014) 41:1442–5,9.
11. Saconi B, Polomano RC, Compton PC, McPhillips MV, Kuna ST, Sawyer AM. The influence of sleep disturbances and sleep disorders on pain outcomes among veterans: A systematic scoping review. Sleep Med Rev. (2021) 56. doi: 10.1016/j.smrv.2020.101411
12. Finan PH, Goodin BR, Smith MT. The association of sleep and pain: an update and a path forward. J Pain. (2013) 14:1539–52. doi: 10.1016/j.jpain.2013.08.007
13. Andersen ML, Araujo P, Frange C, Tufik S. Sleep disturbance and pain: A tale of two common problems. Chest. (2018) 154:1249–59. doi: 10.1016/j.chest.2018.07.019
14. Smith MT, Haythornthwaite JA. How do sleep disturbance and chronic pain inter-relate? Insights from the longitudinal and cognitive-behavioral clinical trials literature. Sleep Med Rev. (2004) 8:119–32. doi: 10.1016/s1087-0792(03)00044-3
15. Yu T, Ma J, Jiang Y, Li J, Gen Y, Wen Y, et al. Assessing pain among chinese elderly-chinese health and retirement longitudinal study. Iran J Public Health. (2018) 47:553–60.
16. Whibley D, AlKandari N, Kristensen K, Barnish M, Rzewuska M, Druce KL, et al. Sleep and pain: A systematic review of studies of mediation. Clin J Pain. (2019) 35:544–58. doi: 10.1097/ajp.0000000000000697
17. Chen J, Yan L, Chu J, Wang X, Xu Z. Pain characteristics and progression to sarcopenia in chinese middle-aged and older adults: A 4-year longitudinal study. J Gerontol A Biol Sci Med Sci. (2024) 79. doi: 10.1093/gerona/glae080
18. Qiu Y, Li H, Yang Z, Liu Q, Wang K, Li R, et al. The prevalence and economic burden of pain on middle-aged and elderly Chinese people: results from the China health and retirement longitudinal study. BMC Health Serv Res. (2020) 20:600. doi: 10.1186/s12913-020-05461-6
19. Zhu X, Zhang X, Ding L, Tang Y, Xu A, Yang F, et al. Associations of pain and sarcopenia with successful aging among older people in China: evidence from CHARLS. J Nutr Health Aging. (2023) 27:196–201. doi: 10.1007/s12603-023-1892-2
20. Estévez-López F, Maestre-Cascales C, Russell D, Álvarez-Gallardo IC, Rodriguez-Ayllon M, Hughes CM, et al. Effectiveness of exercise on fatigue and sleep quality in fibromyalgia: A systematic review and meta-analysis of randomized trials. Arch Phys Med Rehabil. (2021) 102:752–61. doi: 10.1016/j.apmr.2020.06.019
21. Vitiello MV, Zhu W, Von Korff M, Wellman R, Morin CM, Yeung K, et al. Long-term improvements in sleep, pain, depression, and fatigue in older adults with comorbid osteoarthritis pain and insomnia. Sleep. (2022) 45. doi: 10.1093/sleep/zsab231
22. Miettinen T, Sverloff J, Lappalainen O-P, Linton SJ, Sipilä K, Kalso E. Sleep problems in pain patients entering tertiary pain care: the role of pain-related anxiety, medication use, self-reported diseases, and sleep disorders. Pain. (2022) 163:e812–e20. doi: 10.1097/j.pain.0000000000002497
23. Błaszczyk B, Martynowicz H, Więckiewicz M, Straburzyński M, Antolak M, Budrewicz S, et al. Prevalence of headaches and their relationship with obstructive sleep apnea (OSA) - Systematic review and meta-analysis. Sleep Med Rev. (2024) 73:101889. doi: 10.1016/j.smrv.2023.101889
24. Andreucci A, Groenewald CB, Rathleff MS, Palermo TM. The role of sleep in the transition from acute to chronic musculoskeletal pain in youth-A narrative review. Children (Basel). (2021) 8. doi: 10.3390/children8030241
25. Yamada K, Kubota Y, Shimizu Y, Cui R, Mori Y, Okuno Y, et al. Sleep shortage is associated with postherpetic neuralgia development through hyperesthesia and acute pain intensity: A community-based prospective cohort study. Pain Pract. (2019) 19:476–83. doi: 10.1111/papr.12766
26. Seweryn P, Orzeszek SM, Waliszewska-Prosół M, Jenča A, Osiewicz M, Paradowska-Stolarz A, et al. Relationship between pain severity, satisfaction with life and the quality of sleep in Polish adults with temporomandibular disorders. Dent Med Probl. (2023) 60:609–17. doi: 10.17219/dmp/171894
27. Chang JR, Cheung YK, Sharma S, Li SX, Tao RR, Lee JLC, et al. Comparative effectiveness of non-pharmacological interventions on sleep in individuals with chronic musculoskeletal pain: A systematic review with network meta-analysis. Sleep Med Rev. (2024) 73:101867. doi: 10.1016/j.smrv.2023.101867
28. Griffin SC, Ravyts SG, Bourchtein E, Ulmer CS, Leggett MK, Dzierzewski JM, et al. Sleep disturbance and pain in U.S. adults over 50: evidence for reciprocal, longitudinal effects. Sleep Med. (2021) 86:32–9. doi: 10.1016/j.sleep.2021.08.006
29. Vinstrup J, Jakobsen MD, Andersen LL. Poor sleep is a risk factor for low-back pain among healthcare workers: prospective cohort study. Int J Environ Res Public Health. (2020) 17. doi: 10.3390/ijerph17030996
30. Chen W, Wang JP, Wang ZM, Hu PC, Chen Y. Association between sleep duration and chest pain in US adults: A cross-sectional study. Front Public Health. (2022) 10:952075. doi: 10.3389/fpubh.2022.952075
31. Katsifaraki M, Nilsen KB, Christensen JO, Wærsted M, Knardahl S, Bjorvatn B, et al. Sleep duration mediates abdominal and lower-extremity pain after night work in nurses. Int Arch Occup Environ Health. (2019) 92:415–22. doi: 10.1007/s00420-018-1373-9
32. Auvinen JP, Tammelin TH, Taimela SP, Zitting PJ, Järvelin MR, Taanila AM, et al. Is insufficient quantity and quality of sleep a risk factor for neck, shoulder and low back pain? A longitudinal study among adolescents. Eur Spine journal: Off Publ Eur Spine Society Eur Spinal Deformity Society Eur Section Cervical Spine Res Society. (2010) 19:641–9. doi: 10.1007/s00586-009-1215-2
33. Yabe Y, Hagiwara Y, Sekiguchi T, Sugawara Y, Tsuchiya M, Yoshida S, et al. Association between sleep disturbance and low back pain: A 3-year longitudinal study after the great east Japan earthquake. Spine (Phila Pa 1976). (2022) 47:361–8. doi: 10.1097/brs.0000000000004234
34. Guo M, Wu Y, Zheng D, Chen L, Xiong B, Wu J, et al. Preoperative acute sleep deprivation causes postoperative pain hypersensitivity and abnormal cerebral function. Neurosci Bull. (2022) 38:1491–507. doi: 10.1007/s12264-022-00955-1
35. Chen S, Xie Y, Liang Z, Lu Y, Wang J, Xing F, et al. A narrative review of the reciprocal relationship between sleep deprivation and chronic pain: the role of oxidative stress. J Pain Res. (2024) 17:1785–92. doi: 10.2147/jpr.S455621
36. Smith MT, Edwards RR, McCann UD, Haythornthwaite JA. The effects of sleep deprivation on pain inhibition and spontaneous pain in women. Sleep. (2007) 30:494–505. doi: 10.1093/sleep/30.4.494
37. Owens MA, Mun CJ, Hamilton KR, Hughes A, Campbell CM, Edwards RR, et al. Presurgical sleep and pain behaviors predict insomnia symptoms and pain after total knee arthroplasty: a 12-month longitudinal, observational study. Pain Med. (2023) 24:1224–33. doi: 10.1093/pm/pnad106
38. Varallo G, Giusti EM, Manna C, Castelnuovo G, Pizza F, Franceschini C, et al. Sleep disturbances and sleep disorders as risk factors for chronic postsurgical pain: A systematic review and meta-analysis. Sleep Med Rev. (2022) 63:101630. doi: 10.1016/j.smrv.2022.101630
39. Simpson NS, Scott-Sutherland J, Gautam S, Sethna N, Haack M. Chronic exposure to insufficient sleep alters processes of pain habituation and sensitization. Pain. (2018) 159:33–40. doi: 10.1097/j.pain.0000000000001053
40. Ruskovska T, Beekhof P, Velickova N, Kamcev N, Jansen E. Circadian rhythm and time-of-day-effects of (anti)oxidant biomarkers for epidemiological studies. Free Radic Res. (2021) 55:792–8. doi: 10.1080/10715762.2021.1942464
41. Chen S, Xie Y, Li Y, Fan X, Xing F, Mao Y, et al. Sleep deprivation and recovery sleep affect healthy male resident’s pain sensitivity and oxidative stress markers: The medial prefrontal cortex may play a role in sleep deprivation model. Front Mol Neurosci. (2022) 15:937468. doi: 10.3389/fnmol.2022.937468
42. Smith ML, Asada N, Malenka RC. Anterior cingulate inputs to nucleus accumbens control the social transfer of pain and analgesia. Science. (2021) 371:153–9. doi: 10.1126/science.abe3040
43. Eban-Rothschild A, Rothschild G, Giardino WJ, Jones JR, de Lecea L. VTA dopaminergic neurons regulate ethologically relevant sleep-wake behaviors. Nat Neurosci. (2016) 19:1356–66. doi: 10.1038/nn.4377
44. Wang HR, Hu SW, Zhang S, Song Y, Wang XY, Wang L, et al. KCNQ channels in the mesolimbic reward circuit regulate nociception in chronic pain in mice. Neurosci Bull. (2021) 37:597–610. doi: 10.1007/s12264-021-00668-x
45. Sun H, Li Z, Qiu Z, Shen Y, Guo Q, Hu SW, et al. A common neuronal ensemble in nucleus accumbens regulates pain-like behaviour and sleep. Nat Commun. (2023) 14:4700. doi: 10.1038/s41467-023-40450-3
46. Bonvanie IJ, Oldehinkel AJ, Rosmalen JGM, Janssens KAM. Sleep problems and pain: a longitudinal cohort study in emerging adults. Pain. (2016) 157:957–63. doi: 10.1097/j.pain.0000000000000466
47. Morelhão PK, Gobbi C, Christofaro DGD, Damato TM, Grande GD, Frange C, et al. Bidirectional association between sleep quality and low back pain in older adults: A longitudinal observational study. Arch Phys Med Rehabil. (2022) 103:1558–64. doi: 10.1016/j.apmr.2021.11.009
48. Stewart Williams J, Ng N, Peltzer K, Yawson A, Biritwum R, Maximova T, et al. Risk factors and disability associated with low back pain in older adults in low- and middle-income countries. Results from the WHO study on global AGEing and adult health (SAGE). PloS One. (2015) 10:e0127880. doi: 10.1371/journal.pone.0127880
49. Presto P, Mazzitelli M, Junell R, Griffin Z, Neugebauer V. Sex differences in pain along the neuraxis. Neuropharmacology. (2022) 210:109030. doi: 10.1016/j.neuropharm.2022.109030
50. Osborne NR, Davis KD. Sex and gender differences in pain. Int Rev Neurobiol. (2022) 164:277–307. doi: 10.1016/bs.irn.2022.06.013
51. Borenstein DG, Balagué F. Low back pain in adolescent and geriatric populations. Rheum Dis Clin North Am. (2021) 47:149–63. doi: 10.1016/j.rdc.2020.12.001
Keywords: pain, sleep quality, sleep duration, China health and retirement longitudinal study, bidirectional correlation
Citation: Yi D, Yang M, Luo Q, Li H, Kong L and Cheng Q (2024) Bidirectional relationship between pain and sleep disturbance in middle-aged and older adults: evidence from the China health and retirement longitudinal study. Front. Psychiatry 15:1485822. doi: 10.3389/fpsyt.2024.1485822
Received: 24 August 2024; Accepted: 28 October 2024;
Published: 28 November 2024.
Edited by:
Jianyu Que, Peking University Sixth Hospital, ChinaReviewed by:
Marta Waliszewska-Prosół, Wroclaw Medical University, PolandCopyright © 2024 Yi, Yang, Luo, Li, Kong and Cheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qinghao Cheng, cqh4000@163.com
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.