- 1Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 2Nanjing University of Chinese Medicine, Nanjing, China
Introduction: Insomnia during pregnancy presents significant medical care challenges and heightens the risk of adverse outcomes for both pregnant women and fetuses. This study undertook a meta-analysis to assess the global prevalence of insomnia during pregnancy, examining both the overall prevalence and regional variations.
Method: The aim of this study was to perform a meta-analysis of articles indexed in PubMed, Embase, and Web of Science from the inception of these databases up to February 29, 2024. The study systematically reviewed the global prevalence of gestational insomnia and explored potential moderating factors, encompassing research type, publication date, regional influences, maternal age, pregnancy status, depressive symptoms, and anxiety symptoms.
Result: Forty-four studies, encompassing a total of 47,399,513 participants, were included in the analysis. The overall prevalence of insomnia symptoms during pregnancy was 43.9%. Regional factors and depression emerged as the main factors affecting insomnia, with Europe (53.6%) surpassing North America (41.0%), followed by South America (50.6%) and Asia (40.7%). High depression rates (56.2%) correlated with increased insomnia prevalence compared to low depression rates (39.8%). The type of research and publication date showed no significant impact on the prevalence of insomnia symptoms.
Conclusion: The meta-analysis results indicated that the prevalence of insomnia symptoms was higher during pregnancy, especially among pregnant women who were in a highly depressed state or located in the European region.
Systematic review registration: PROSPERO, identifier CRD42018104460.
Highlight
● Reassess the global prevalence of insomnia during pregnancy.
● The regional differences in insomnia disease were discussed.
● The possible reasons for the difference in prevalence were analyzed.
Introduction
Insomnia is a common clinical disorder characterized by difficulty falling asleep or maintaining sleep, often accompanied by symptoms such as irritability or fatigue when awake. It often occurs at least three times a week and lasted for a duration of at least three months, and can’t be attributed to other diseases or substances (1).
Research indicates that the incidence rate of insomnia in adults typically ranges from 6% to 10%, whereas among pregnant women it is notably higher at 38.2% (2, 3). Insomnia during pregnancy can be attributed to a varied of factors, such as physical discomfort, hormonal fluctuations, fetal growth (4), and emotional distress. Research has shown that insomnia during pregnancy (5) not only leads to a decline in quality of life, but also is a potential cause of premature delivery, cesarean section, prolonged delivery, pregnancy induced hypertension, pregnancy induced diabetes, and postpartum depression. Lu conducted a comprehensive review of sleep disorders and their association with adverse maternal and infant outcomes. The results revealed that sleep disorders, including insomnia, were associated with an increased risk of adverse pregnancy outcomes such as preeclampsia (OR=2.80, 95% CI 2.38-3.30), hypertension during pregnancy (OR=1.74, 95% CI 1.54-1.97), diabetes during pregnancy (OR=1.59, 95% CI 1.45-1.76), cesarean section (OR=1.47, 95% CI 1.31-1.64), and premature delivery (OR=1.38, 95% CI 1.26-1.51) (6); Additionally, a study demonstrated that insomnia was associated with an increased risk of perinatal suicide (OR=4.76, 95% CI 1.83-12.34) (7). Therefore, insomnia poses a significant threat to maternal and fetal health throughout pregnancy.
In the 2020 review on the prevalence of insomnia, the authors conducted subgroup analysis on variables including maternal age, gestational age, depressive symptoms, and gestational period (8). The review found that maternal age, gestational age, and anxiety significantly impact the prevalence of insomnia. Due to the limited number of articles included, the authors did not compare regional prevalence rates. As is well known, insomnia during pregnancy is a sleep disorder caused by various confounding factors. Regional studies are important for the prevention of women’s health. In China, a cross-sectional study on insomnia in Chinese pregnant women showed that 24.3% of the pregnant women suffered from insomnia, and found that maternal age, attained education, occupation, monthly household income, insurance coverage, relationship with the mother-in-law, gestational age, and anxiety symptoms were independently risk factors for insomnia (9). A Canadian study found that good social attention and partnership can reduce the incidence of prenatal depression and thus reduce the risk of insomnia during pregnancy (10). Similarly, several studies of pregnancy insomnia in the United States have found that degree of social concern is related to differences in the risk of pregnancy insomnia (11, 12). What’s more, different countries and regions may also have significant differences in the prevalence of insomnia during pregnancy due to diet, social life pressure, cultural background, and national women’s policies.
Based on this, we conducted a comprehensive database search and compare the prevalence of insomnia during pregnancy in different countries by region. These results will provide some reference evidence for the formulation of prevention and health policies in high prevalence areas, thereby increasing social attention to women’s health.
Methods
A systematic review and meta-analysis were conducted on articles related to insomnia symptoms during pregnancy. Both systematic reviews and meta-analyses were reported in accordance with the PRISMA Declaration Guidelines (13). This review has been registered in the PROSPERO database (registration number: CRD42018104460). The PRISMA checklist could be found in Supplementary Material 1. The PICOS method was used in formulating research questions (14).
Search strategy
A full-text search was conducted on the PubMed, Embase, and Web of Science databases, with a time limit for papers published until February 29, 2024, including articles that reported insomnia rates during pregnancy through self-report or questionnaire surveys. The search algorithm was based on terms such as ‘pregnancy’ and ‘insomnia’. Specific search strategies were in Supplementary Material 2.
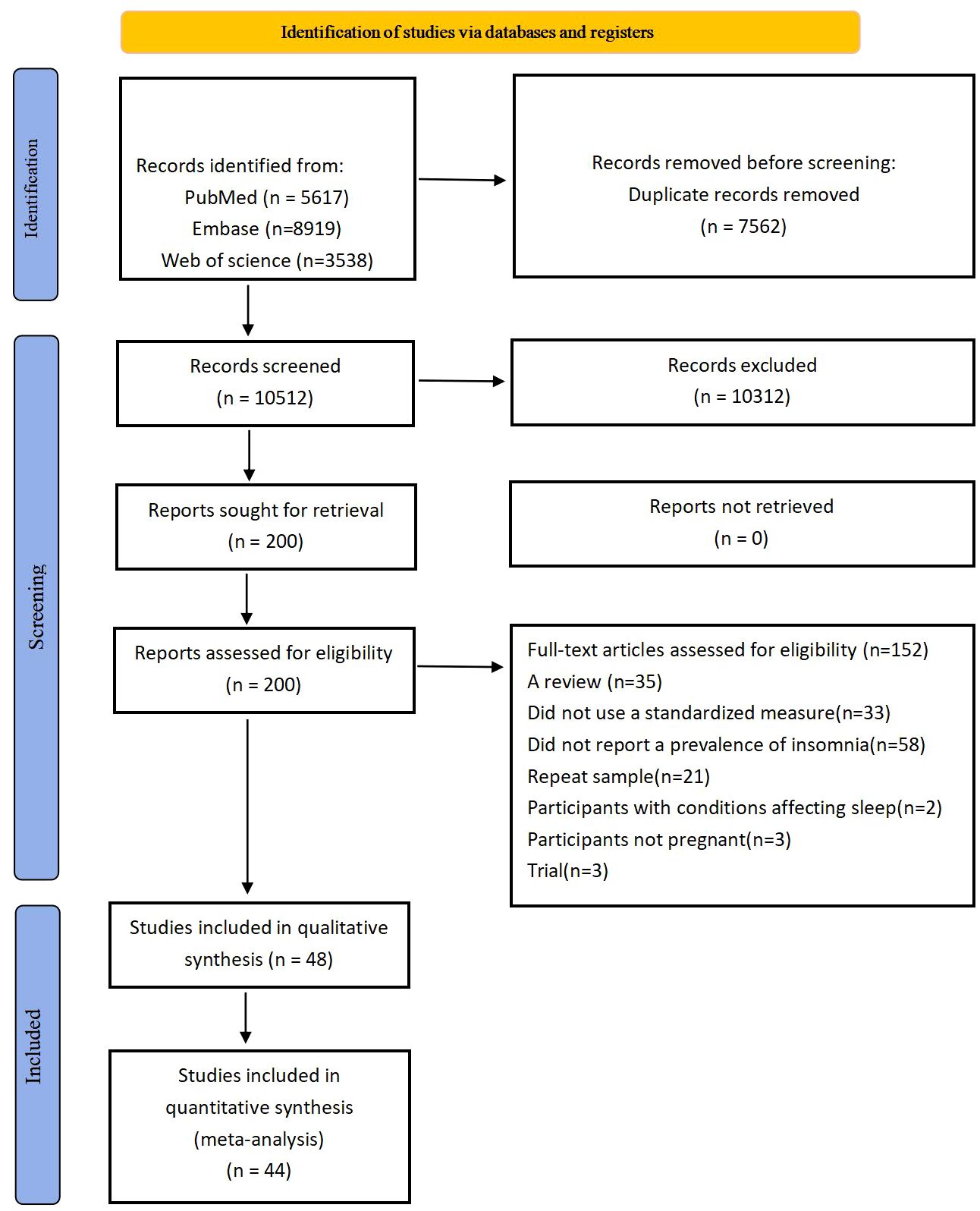
The selected titles and relevant abstracts of the articles were reviewed. Each article was categorized as ‘yes’, ‘no’, or ‘possible’, with articles marked as ‘no’ being excluded from the analysis. The entire articles with titles or abstracts marked as ‘yes’ or ‘possible’ were thoroughly reviewed to determine if they met the inclusion criteria. Please refer to Figure 1 for a detailed flowchart outlining the detection program for the study.
Research selection
The P-population was Women with pregnancy, the I-study has no intervention, the C-compare with and without sleep problem, the O-outcome is insomnia, and S-study included Randomized controlled studies, cohort studies, cross-sectional studies, case-control studies. The study included data on the prevalence of insomnia among pregnant women, or reported the number of individuals with insomnia. Research methods involved self-reporting, questionnaire surveys, and the measurement of epidemiological data.
Exclusion criteria: The sample consisted solely of pregnant women with sleep disorders. Studies that used non-standardized measurement methods, such as evaluating insomnia with a single question, were not included. Furthermore, studies that were case reports, systematic reviews, or used data from previous studies were also excluded.
The first and second authors (FR and WH) independently reviewed these studies and conducted a full-text review based on inclusion and exclusion criteria to further exclude studies that were not qualified. Any differences were be resolved by the senior author (ZS).
Data extraction
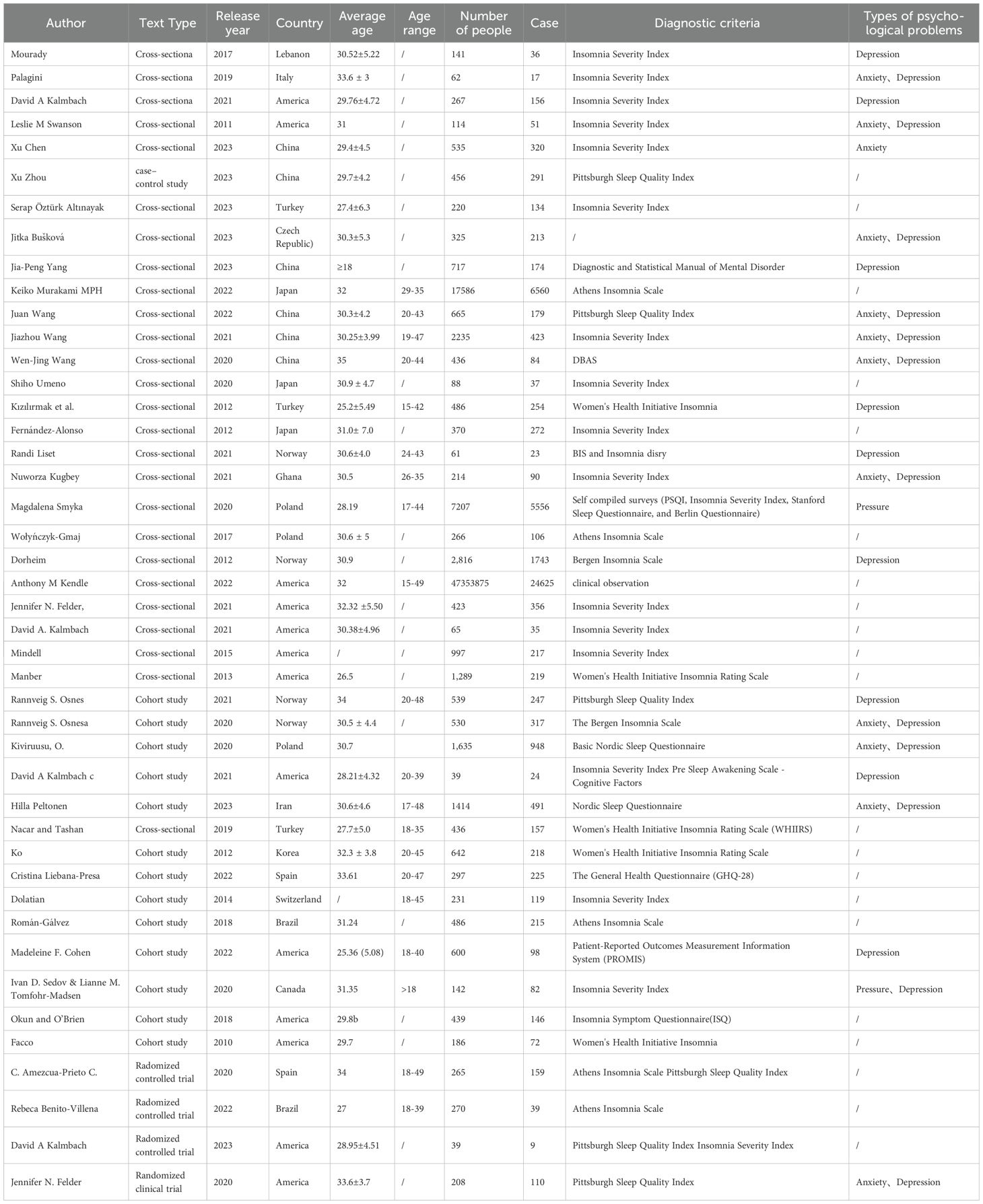
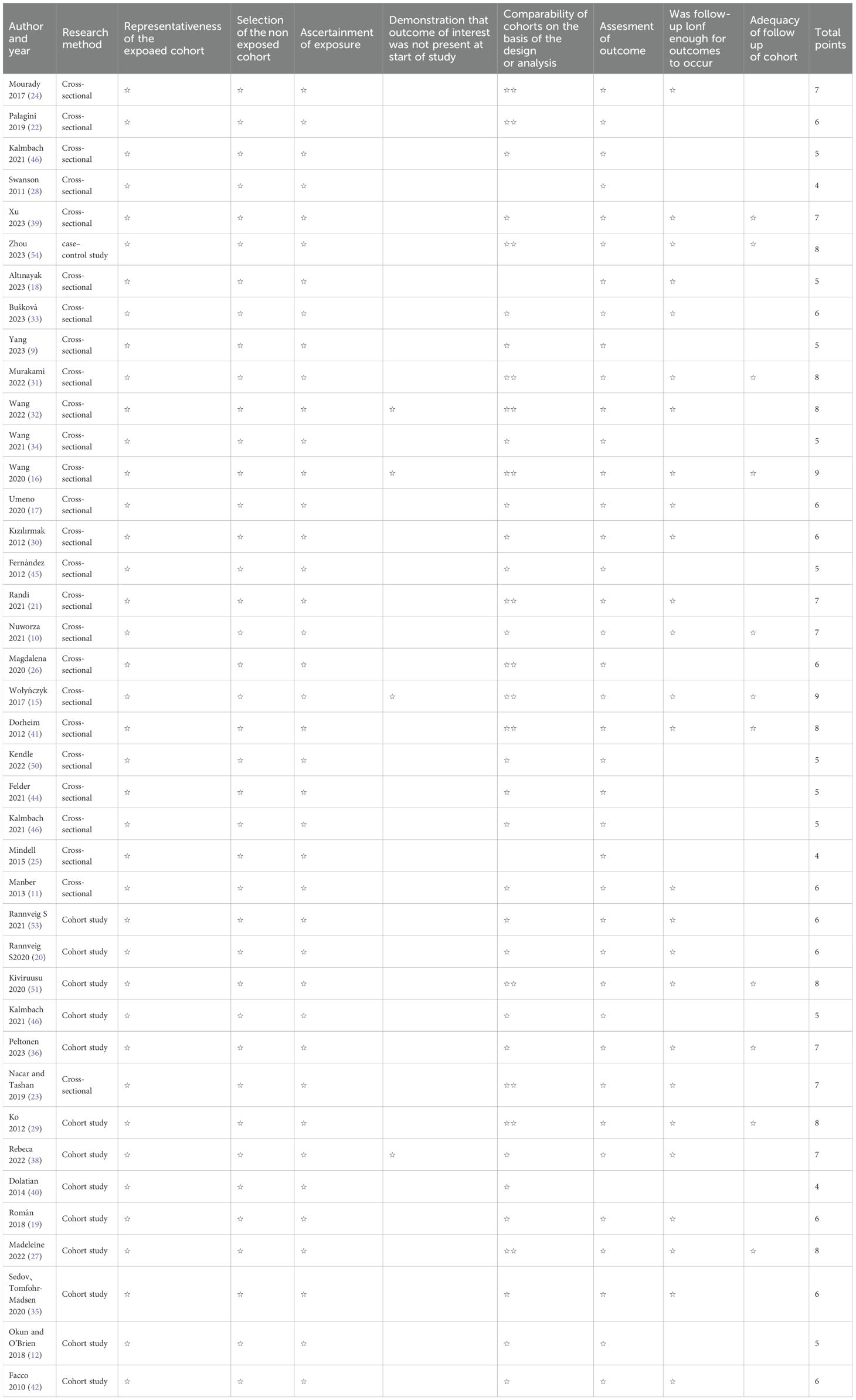
The first (FR) and second (WH) authors independently extracted data to confirm accuracy. The third author (ZS) confirmed the accuracy of the included data. The studies selected for review are recorded using standardized tables to describe the important variables of each study. The estimated prevalence of insomnia was obtained by extracting data on the number of cases, total sample size, or percentage of samples identified as having insomnia symptoms, as well as the study type, region, maternal age (year), gestational age (week), and percentage of anxiety or depression cases (see Table 1).
Meta-analysis was conducted using the comprehensive software STATA 16.0. A random effects model was chosen for analysis based on the level of heterogeneity, typically with I2>50%. The I2 index was used to assess heterogeneity between point estimates, indicating the proportion of variation between point estimates attributed to heterogeneity. Traditionally, I2 values below 25% suggest low heterogeneity, while values between 25% and 50% suggest moderate heterogeneity, and values above 50% suggest high heterogeneity. Subgroup comparison was then employed to further investigate the sources of heterogeneity.
Quality evaluation
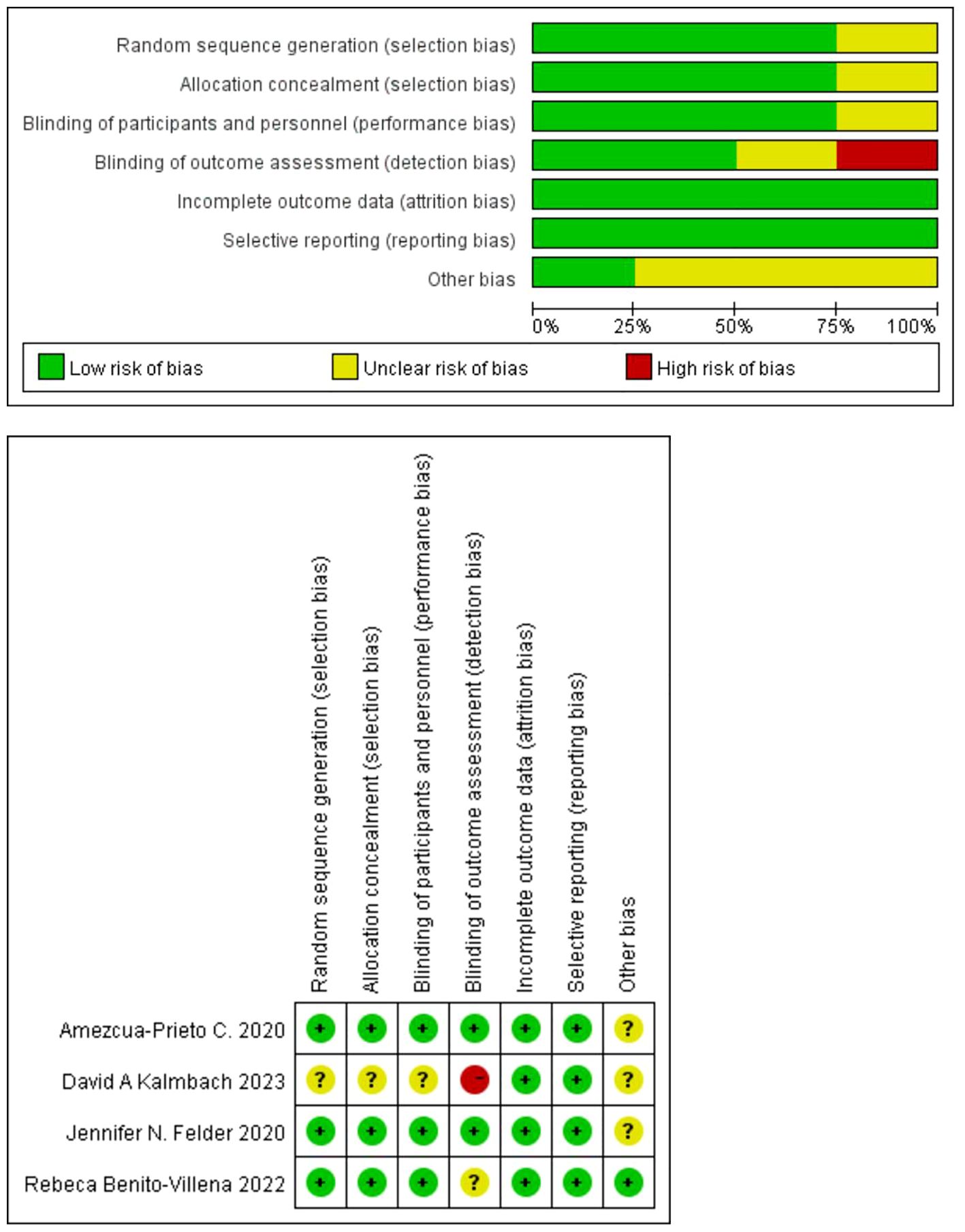
The Newcastle-Ottawa Scale (NOS) was used to evaluate the quality of the included observational studies, and it was generally considered that 1-3 was classified as low quality, 4-6 as medium quality, and 7-9 as high quality. Randomized controlled trials were evaluated using the Cochrane risk bias assessment tool.
Results
Figure 1 illustrated the flowchart of the search and selection process. Initially, a search yielded 18,074 records, of which 10,312 were filtered based on title and abstract after removing duplicates. Following a full text review of the remaining 200 studies, 152 studies were excluded due to unclear sleep outcomes. The meta-analysis included 44 studies (9–12, 15–54), involving a total of 47,399,513 participants in the analysis. The literature included 26 cross-sectional studies (9–11, 15–18, 21–26, 28, 30–34, 39, 41, 44, 45, 47, 49, 50), 13 cohort studies (12, 19, 20, 27, 29, 35, 36, 40, 42, 46, 51–53), 4 randomized controlled studies (37, 38, 43, 48), and 1 case-control study (54).
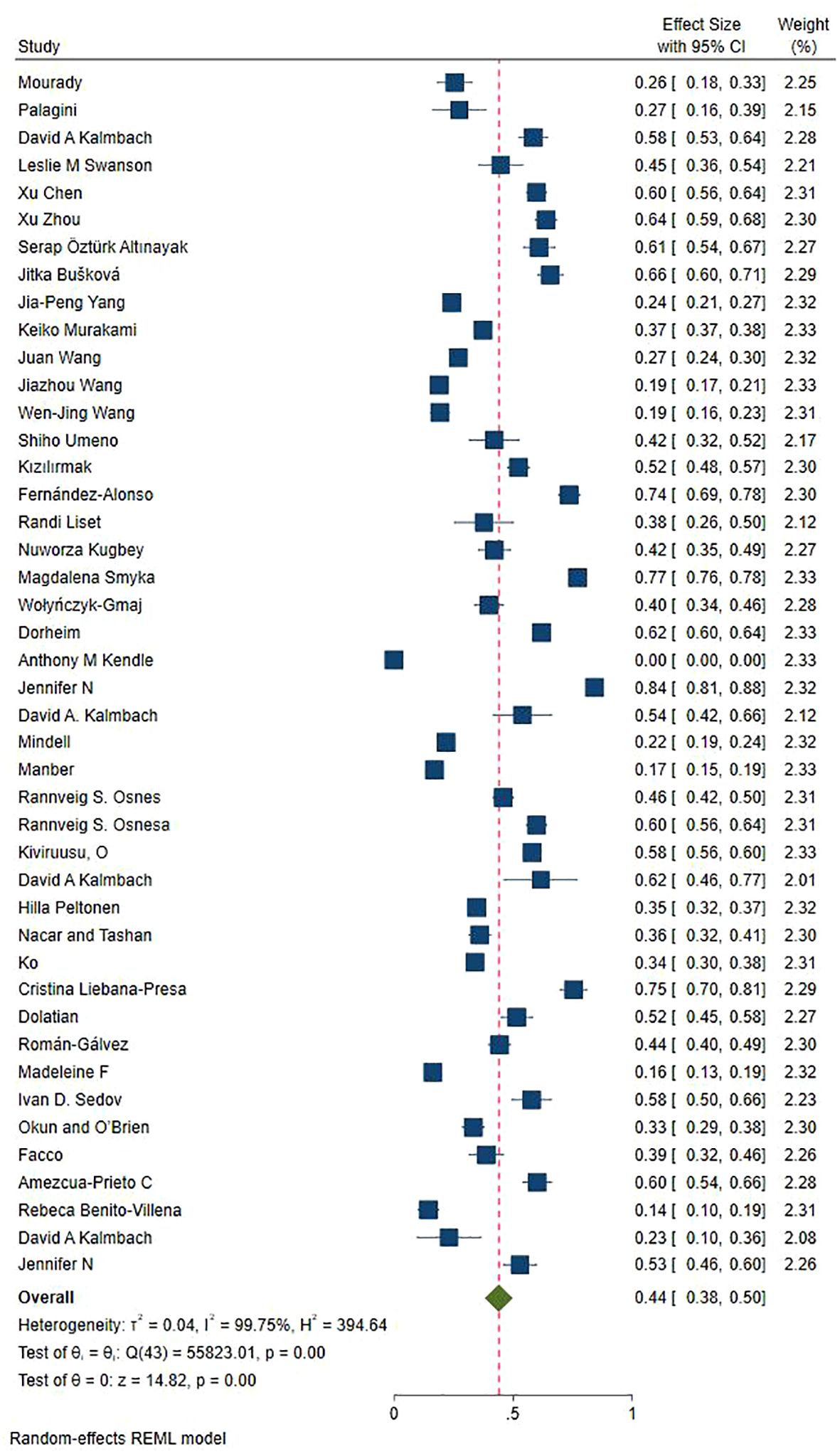
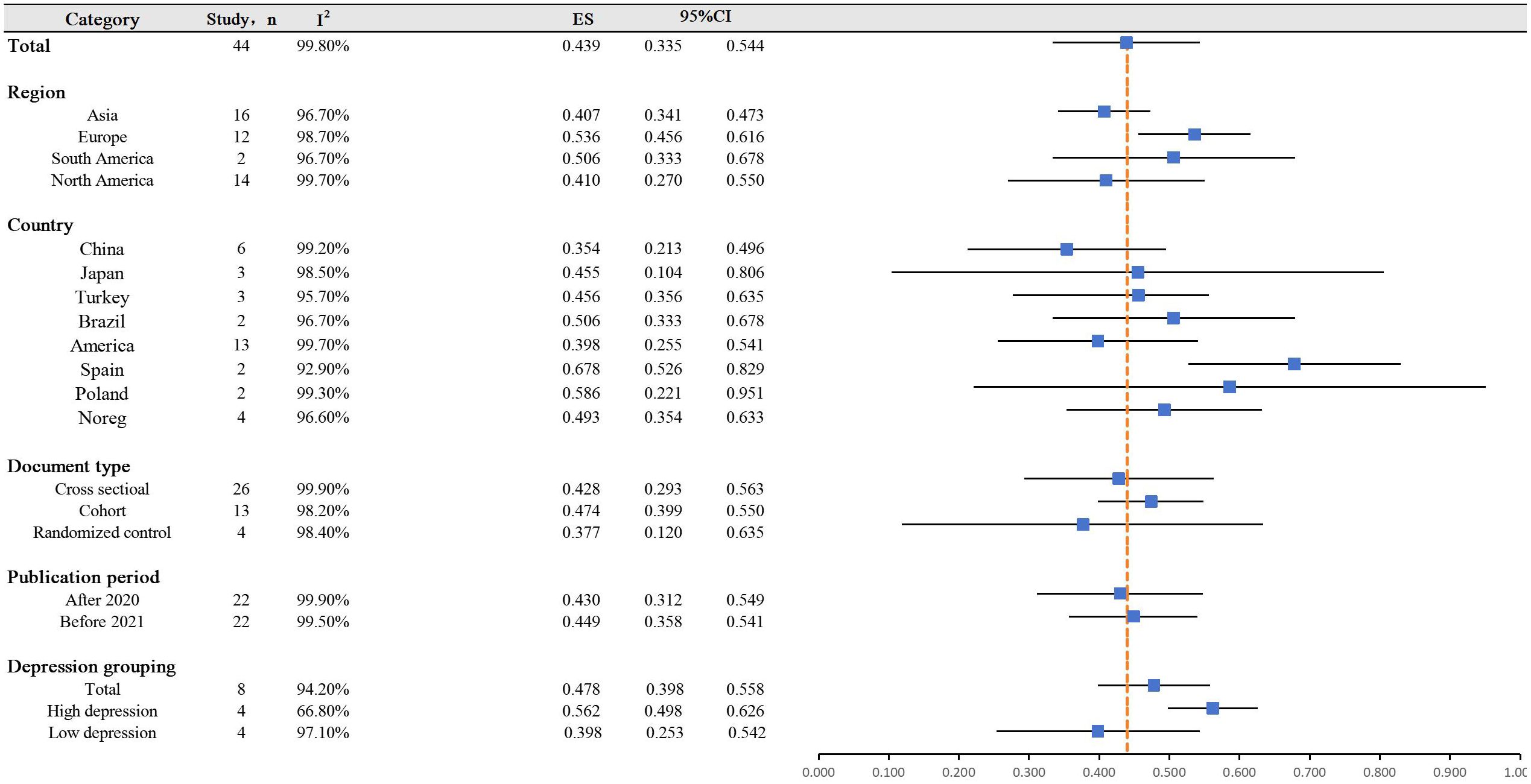
Figures 2 and 3 displayed a summary of insomnia prevalence rates and subgroup forest plots, indicating an estimated range of 1% -77.1% for the prevalence of insomnia among 44 study patients. The overall prevalence rate was 43.9% (33.5% - 54.4%). On this basis, multiple subgroup analyses were conducted.
Subgroup analysis based on region and country
Based on regional grouping results, the prevalence of insomnia in Asia was the lowest (9, 16–18, 23, 24, 29–34, 36, 39, 45, 54), with a specific value of 40.7% (34.1% - 47.3%); Pregnant women in Europe exhibited a high insomnia rate of 53.6% (45.6% - 61.6%) (10, 15, 20–22, 26, 37, 40, 41, 51–53); The prevalence rates in North and South America were 41.0% and 50.6%, respectively (11, 12, 19, 25, 27, 28, 35, 38, 42–44, 46–50). Further analysis of the prevalence of insomnia by the country revealed that Spain has the highest insomnia rate of 67.8% (52.6% - 82.9%, I2 = 92.9%) (37, 52), while China has the lowest pregnancy insomnia rate of 35.4% (21.3% -49.6%, I2 = 99.2%) (9, 16, 32, 34, 39, 54).
Subgroup analysis based on study design
According to the analysis of article categories, it was found that the prevalence of insomnia in randomized controlled studies was the lowest at 37.7% (12% - 63.5%) (37, 38, 43, 48).The prevalence of insomnia was relatively similar between cross-sectional studies (9–11, 15–18, 21–26, 28, 30–34, 39, 41, 44, 45, 47, 49, 50) and cohort studies (12, 19, 20, 27, 29, 35, 36, 40, 42, 46, 51–53), at 42.8% and 47.4%, respectively. Based on the analysis of publication years, there was no significant difference in the prevalence of insomnia.
Subgroup analysis based on psychological depression participants
Based on classification analysis, it was discovered that in studies with a high prevalence of depression, the occurrence of gestational insomnia rose by 56.2% (49.8% - 62.6%). This indicates that depression is a contributing factor to the elevated rates of insomnia.
Quality evaluation
The overall quality of the included literature was deemed high, with 24 studies in Table 2 offering moderate evidence and 2 studies presenting low-level evidence. Only one article in the randomized controlled study indicated low quality, as shown in Figure 4. The high quality of the papers contributes to the reliability of the analysis results.
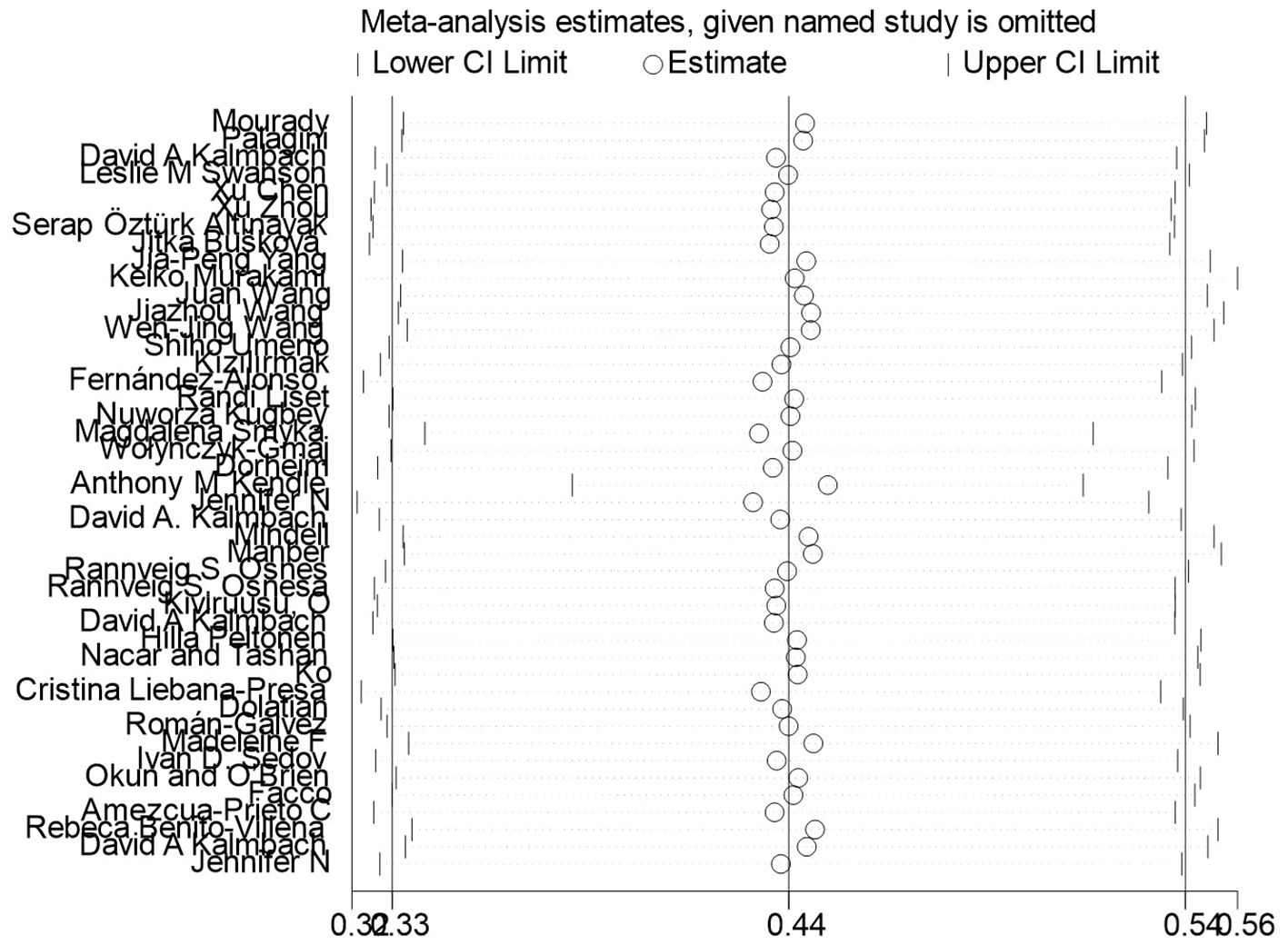
Sensitivity analysis
After deleting each study item by item (Figure 5), the overall estimates remained stable, indicating that the studies did not significantly affect the overall combined prevalence estimate.
Discussion
An in-depth analysis was conducted on the various factors influencing insomnia during pregnancy, indicating that sleep quality can be significantly impacted by pregnancy. As the pregnancy advances, there is a noticeable decline in sleep quality, with late pregnancy being the most disruptive period (53). Studies have indicated a strong correlation between subjective sleep scores and the severity of depressive symptoms (55). Moreover, pregnancy represents a physiological state characterized by continuous hormonal, physical, and behavioral changes that may significantly alter both sleep quality and duration (56).
The study found that the total prevalence of insomnia during pregnancy was 44.0%, significantly higher than the general population. This highlights the importance of addressing insomnia as a significant health issue during pregnancy. Subgroup analysis by region revealed the highest prevalence in Europe and the lowest in Asia. Further analysis was then conducted at the country level.
Among European countries, Spain, Poland, and Norway exhibited a higher risk of insomnia compared to the overall level of insomnia in this analysis. This finding is in line with previous European studies that have shown a relatively high prevalence of insomnia in the European population (57, 58). Pregnancy events will further exacerbate the burden of female insomnia. A self-reported survey conducted by David O’Regan on individuals with insomnia in Europe identified lifestyle factors and high levels of life stress as the primary causes of insomnia (59). Numerous articles on insomnia have also highlighted the impact of lifestyle factors such as diet, exercise, smoking, and sleep habits on the development of insomnia (60). Additionally, a study on diet and insomnia revealed a positive association between dietary glycemic load and insomnia risk (OR: 1.10; 95% CI, 1.01, 1.20) (61). Spain, Poland, and Norway, being developed countries, often experience higher life burdens and pressures due to the pursuit of a high quality of life. Meanwhile, the preference for sugary foods among Europeans may contribute to the increased risk of insomnia (62–64).
In the Asian subgroup analysis, Japan, a developed country, exhibited a higher prevalence of insomnia during pregnancy, in line with expectations. The study revealed that, apart from economic pressures, the societal focus on women played a significant role in causing insomnia. Notably, China has specific support measures for pregnant women, including reduced working hours, dietary adjustments, and tailored psychological counseling, effectively alleviating psychological stress (65, 66). Moreover, within the Chinese cultural context, pregnant women receive extensive care from family members, contributing to a low insomnia rate (65). These findings offer valuable insights for designing women’s health initiatives. Conversely, the status of women in Japan is comparatively lower, hindering access to social support and contributing to the high prevalence of insomnia among pregnant women (67).
North America mainly includes the United States and Canada. In this analysis, only the United States was considered, revealing a lower insomnia rate compared to the overall level. Throughout the past century, the United States has dedicated efforts to safeguarding women’s power and status. Additionally, being the most developed country globally, the United States boasts top-tier economic and medical advancements. These factors, including a robust system and favorable economic and medical conditions, play a vital role in ensuring a safe pregnancy and reducing the risk of insomnia in pregnant women (68–70).
A correlation between insomnia and depression has been observed. In recent years, the detection rate of pregnancy complications in clinical practice has been on the rise (71), attributed to changes in the living environment, maternal neuroendocrine function, and abnormal fetal development. Studies both domestically and internationally have reported a prevalence rate of depression symptoms during pregnancy among women with pregnancy complications ranging from 29.4% to 39%, significantly surpassing that of healthy pregnant women (72, 73).
Through data analysis, it was found that individuals with high levels of depression were at a higher risk of insomnia, and depression was positively correlated with an increase in sleep latency. A study found differences in the consistency of local activity in the auxiliary motor area and insula between patients with insomnia and those without. Patients with insomnia and severe depression exhibited differences in the intensity of spontaneous activity in the middle frontal gyrus and paracentral lobules compared to those without insomnia. Previous studies have shown that the potential neurobiological mechanisms of depression and insomnia symptoms may have included: (1) abnormalities in monoamine neurotransmitters, especially changes in 5-HT concentration, which were closely related to sleep awakening and depression, such as shortened REM latency in patients with depression; (2) Overexpression of biological clock genes and stress response genes; (3) Dysfunction of the hypothalamic pituitary adrenal axis (HPA) and abnormal release of cortisol (74). According to data, there was a close relationship between insomnia during pregnancy and depression at both the symptom and disease levels. Some women’s insomnia symptoms were relatively stable in the early stages of pregnancy, but temporarily increased in the late stages of pregnancy. This is closely associated with significant physiological and psychological changes, and pregnancy can be characterized as a period of heightened biological and situational stress (75), which may activate latent vulnerabilities and magnify them. Hence, many pregnant women might experience a worsening of insomnia symptoms in the later stages of pregnancy. For instance, around 70% of individuals with depression experience symptoms of insomnia, and the prevalence of depression among pregnant women with insomnia is 3-4 times higher than in those without insomnia (76). This bidirectional and cumulative relationship necessitates greater clinical attention, as gestational insomnia and depression both pose risk factors for adverse pregnancy outcomes.
Insomnia during pregnancy is not inherently harmful, but it can contribute to an elevated risk of various health complications for women, such as stillbirth, miscarriage, perinatal depression, and other adverse outcomes. As a result, it is essential to focus on non-pharmacological methods for preventing and managing insomnia during pregnancy. Psychological and social factors play a significant role in the varying prevalence of insomnia during pregnancy, with psychological factors often being linked to some social factors. Pan Chen and Eric S Kim suggest that enhancing overall well-being can be an effective way to alleviate negative psychological symptoms (77, 78). Therefore, enhancing the focus on women during pregnancy is crucial for safeguarding their health (79). China, with its historical cultural background, has shown a greater emphasis on women’s health compared to other developed countries. Drawing from China’s approach, strategies such as reducing the work intensity of pregnant women, promoting increased attention from family members and social groups, providing regular psychological counseling, and encouraging appropriate exercise like relaxation training and mindfulness can help alleviate psychological issues during pregnancy and improve sleep quality to some extent (80).
Limitations
In this meta-analysis, significant heterogeneity was found, which may be attributed to population characteristics, study design, evaluation of insomnia and measurement of outcomes, as well as clinical stages of pregnancy. Secondly, insomnia mainly came from subjective reports or questionnaire surveys, and differences in diagnosis may have a certain impact on the results. Due to the fact that the summary result of single arm rate is a descriptive result and not a difference comparison result, the statistical significance of publication bias is not strong. We strictly followed the inclusion and exclusion criteria to manually screen relevant articles, without any restrictions on the language or year of the study, thus minimizing the possibility of omitting any research related to the topic; We also conducted a stratified analysis based on geographical location, publication time, literature type, and degree of depression. Therefore, compared to other small-scale studies, our research results may have more reference value and robustness. Finally, due to the limited data on insomnia across various gestational periods, a subgroup analysis based on these different periods has not yet been conducted. Further studies are anticipated to provide additional verification in the future.
Conclusion
The prevalence of insomnia during pregnancy, reaching as high as 44%, has been displaying an upward trend year by year. Urgent attention must be directed toward women’s health issues. Insomnia during pregnancy not only elevates the risk of adverse pregnancy outcomes for women but also significantly affects fetal development and postpartum well-being. As widely acknowledged, insomnia during pregnancy stems from various complex factors, with regional disparities emerging as a central aspect warranting special attention. We aim to undertake further regional research in the future to enhance clinical evidence for developing regional policies aimed at safeguarding women’s health.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Author contributions
CY: Writing – review & editing, Writing – original draft. RF: Writing – review & editing, Writing – original draft. HW: Writing – review & editing, Writing – original draft. YJ: Writing – review & editing, Writing – original draft. SZ: Writing – review & editing, Writing – original draft. XJ: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Administration of Traditional Chinese Medicine, National Famous Traditional Chinese Medicine Expert Inheritance Studio Construction Project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1427255/full#supplementary-material
References
1. Louis JM, Koch MA, Reddy UM, Silver RM, Parker CB, Facco FL, et al. Predictors of sleep-disordered breathing in pregnancy. Am J Obstet Gynecol. (2018) 218:521.e1–.e12. doi: 10.1016/j.ajog.2018.01.031
2. Krystal AD, Ashbrook LH, Prather AA. What is insomnia? Jama. (2021) 326:2444. doi: 10.1001/jama.2021.19283
4. Chaudhry SK, Susser LC. Considerations in treating insomnia during pregnancy: A literature review. Psychosomatics. (2018) 59:341–8. doi: 10.1016/j.psym.2018.03.009
5. Okun ML, Mancuso RA, Hobel CJ, Schetter CD, Coussons-Read M. Poor sleep quality increases symptoms of depression and anxiety in postpartum women. J Behav Med. (2018) 41:703–10. doi: 10.1007/s10865-018-9950-7
6. Lu Q, Zhang X, Wang Y, Li J, Xu Y, Song X, et al. Sleep disturbances during pregnancy and adverse maternal and fetal outcomes: A systematic review and meta-analysis. Sleep Med Rev. (2021) 58:101436. doi: 10.1016/j.smrv.2021.101436
7. Palagini L, Cipriani E, Miniati M, Bramante A, Gemignani A, Geoffroy PA, et al. Insomnia, poor sleep quality and perinatal suicidal risk: A systematic review and meta-analysis. J Sleep Res. (2024) 33:e14000. doi: 10.1111/jsr.14000
8. Sedov ID, Anderson NJ, Dhillon AK, Tomfohr-Madsen LM. Insomnia symptoms during pregnancy: A meta-analysis. J Sleep Res. (2021) 30:e13207. doi: 10.1111/jsr.13207
9. Yang JP, Lin RJ, Sun K, Gao LL. Incidence and correlates of insomnia and its impact on health-related quality of life among Chinese pregnant women: a cross-sectional study. J Reprod Infant Psychol. (2023) 41:391–402. doi: 10.1080/02646838.2021.2020228
10. Kugbey N, Ayanore M, Doegah P, Chirwa M, Bartels SA, Davison CM, et al. Prevalence and correlates of prenatal depression, anxiety and suicidal behaviours in the Volta region of Ghana. Int J Environ Res Public Health. (2021) 18(11):5857. doi: 10.3390/ijerph18115857
11. Manber R, Steidtmann D, Chambers AS, Ganger W, Horwitz S, Connelly CD. Factors associated with clinically significant insomnia among pregnant low-income Latinas. J Women's Health (2002). (2013) 22:694–701. doi: 10.1089/jwh.2012.4039
12. Okun ML, O'Brien LM. Concurrent insomnia and habitual snoring are associated with adverse pregnancy outcomes. Sleep Med. (2018) 46:12–9. doi: 10.1016/j.sleep.2018.03.004
13. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clinical Res ed). (2021) 372:n71. doi: 10.1136/bmj.n71
14. Morgan RL, Whaley P, Thayer KA, Schünemann HJ. Identifying the PECO: A framework for formulating good questions to explore the association of environmental and other exposures with health outcomes. Environ Int. (2018) 121:1027–31. doi: 10.1016/j.envint.2018.07.015
15. Wołyńczyk-Gmaj D, Różańska-Walędziak A, Ziemka S, Ufnal M, Brzezicka A, Gmaj B, et al. Insomnia in pregnancy is associated with depressive symptoms and eating at night. J Clin Sleep Med: JCSM: Off Publ Am Acad Sleep Med. (2017) 13:1171–6. doi: 10.5664/jcsm.6764
16. Wang WJ, Hou CL, Jiang YP, Han FZ, Wang XY, Wang SB, et al. Prevalence and associated risk factors of insomnia among pregnant women in China. Compr Psychiatry. (2020) 98:152168. doi: 10.1016/j.comppsych.2020.152168
17. Umeno S, Kato C, Nagaura Y, Kondo H, Eto H. Characteristics of sleep/wake problems and delivery outcomes among pregnant Japanese women without gestational complications. BMC Pregnancy Childbirth. (2020) 20:179. doi: 10.1186/s12884-020-02868-1
18. Altınayak S, Rüzgar Ş, Koç E. The relationship between sleep problems and sexual dysfunction among pregnant women in Turkey. Sleep Breathing Schlaf Atmung. (2024) 28:459–65. doi: 10.1007/s11325-023-02896-z
19. Román-Gálvez RM, Amezcua-Prieto C, Salcedo-Bellido I, Martínez-Galiano JM, Khan KS, Bueno-Cavanillas A. Factors associated with insomnia in pregnancy: A prospective Cohort Study. Eur J Obstet Gynecol Reprod Biol. (2018) 221:70–5. doi: 10.1016/j.ejogrb.2017.12.007
20. Osnes RS, Eberhard-Gran M, Follestad T, Kallestad H, Morken G, Roaldset JO. Mid-pregnancy insomnia is associated with concurrent and postpartum maternal anxiety and obsessive-compulsive symptoms: A prospective cohort study. J Affect Disord. (2020) 266:319–26. doi: 10.1016/j.jad.2020.01.140
21. Liset R, Grønli J, Henriksen RE, Henriksen TEG, Nilsen RM, Pallesen S. Sleep, evening light exposure and perceived stress in healthy nulliparous women in the third trimester of pregnancy. PloS One. (2021) 16:e0252285. doi: 10.1371/journal.pone.0252285
22. Palagini L, Cipollone G, Masci I, Novi M, Caruso D, Kalmbach DA, et al. Stress-related sleep reactivity is associated with insomnia, psychopathology and suicidality in pregnant women: preliminary results. Sleep Med. (2019) 56:145–50. doi: 10.1016/j.sleep.2019.01.009
23. Nacar G, Taşhan ST. Relationship between sleep characteristics and depressive symptoms in last trimester of pregnancy. Afr Health Sci. (2019) 19:2934–44. doi: 10.4314/ahs.v19i4.14
24. Mourady D, Richa S, Karam R, Papazian T, Hajj Moussa F, El Osta N, et al. Associations between quality of life, physical activity, worry, depression and insomnia: A cross-sectional designed study in healthy pregnant women. PloS One. (2017) 12:e0178181. doi: 10.1371/journal.pone.0178181
25. Mindell JA, Cook RA, Nikolovski J. Sleep patterns and sleep disturbances across pregnancy. Sleep Med. (2015) 16:483–8. doi: 10.1016/j.sleep.2014.12.006
26. Smyka M, Kosińska-Kaczyńska K, Sochacki-Wójcicka N, Zgliczyńska M, Wielgoś M. Sleep problems in pregnancy-A cross-sectional study in over 7000 pregnant women in Poland. Int J Environ Res Public Health. (2020) 17(15):5306. doi: 10.3390/ijerph17155306
27. Cohen MF, Corwin EJ, Johnson DA, Amore AD, Brown AL, Barbee NR, et al. Discrimination is associated with poor sleep quality in pregnant Black American women. Sleep Med. (2022) 100:39–48. doi: 10.1016/j.sleep.2022.07.015
28. Swanson LM, Pickett SM, Flynn H, Armitage R. Relationships among depression, anxiety, and insomnia symptoms in perinatal women seeking mental health treatment. J Women's Health (2002). (2011) 20:553–8. doi: 10.1089/jwh.2010.2371
29. Ko H, Shin J, Kim MY, Kim YH, Lee J, Kil KC, et al. Sleep disturbances in Korean pregnant and postpartum women. J Psychosom Obstet Gynaecol. (2012) 33:85–90. doi: 10.3109/0167482X.2012.658465
30. Kızılırmak A, Timur S, Kartal B. Insomnia in pregnancy and factors related to insomnia. Sci World J. (2012) 2012:197093. doi: 10.1100/2012/197093
31. Murakami K, Ishikuro M, Obara T, Ueno F, Noda A, Onuma T, et al. Social isolation and insomnia among pregnant women in Japan: The Tohoku Medical Megabank Project Birth and Three-Generation Cohort Study. Sleep Health. (2022) 8:714–20. doi: 10.1016/j.sleh.2022.08.007
32. Wang J, Huang Y, Li Y, Wu L, Cao D, Cao F. Sleep-related attentional bias: Development and validation of a Chinese version of the brief sleep-associated monitoring index in pregnant women. J Psychosom Res. (2022) 163:111052. doi: 10.1016/j.jpsychores.2022.111052
33. Bušková J, Miletínová E, Králová R, Dvořáková T, Tefr Faridová A, Heřman H, et al. Parasomnias in pregnancy. Brain Sci. (2023) 13(2):357. doi: 10.3390/brainsci13020357
34. Wang J, Zhou Y, Qian W, Zhou Y, Han R, Liu Z. Maternal insomnia during the COVID-19 pandemic: associations with depression and anxiety. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:1477–85. doi: 10.1007/s00127-021-02072-2
35. Sedov ID, Tomfohr-Madsen LM. Trajectories of insomnia symptoms and associations with mood and anxiety from early pregnancy to the postpartum. Behav Sleep Med. (2021) 19:395–406. doi: 10.1080/15402002.2020.1771339
36. Peltonen H, Paavonen EJ, Saarenpää-Heikkilä O, Vahlberg T, Paunio T, Polo-Kantola P. Sleep disturbances and depressive and anxiety symptoms during pregnancy: associations with delivery and newborn health. Arch Gynecol Obstet. (2023) 307:715–28. doi: 10.1007/s00404-022-06560-x
37. Amezcua-Prieto C, Naveiro-Fuentes M, Arco-Jiménez N, Olmedo-Requena R, Barrios-Rodríguez R, Vico-Zúñiga I, et al. Walking in pregnancy and prevention of insomnia in third trimester using pedometers: study protocol of Walking_Preg project (WPP). A randomized Controlled trial. BMC Pregnancy Childbirth. (2020) 20:521. doi: 10.1186/s12884-020-03225-y
38. Benito-Villena R, Guerrero-Martínez I, Naveiro-Fuentes M, Cano-Ibánez N, Femia-Marzo P, Gallo-Vallejo JL, et al. Walking promotion in pregnancy and its effects on insomnia: results of walking_Preg project (WPP) clinical trial. Int J Environ Res Public Health. (2022) 19(16):10012. doi: 10.3390/ijerph191610012
39. Chen X, Liu Y, Liu M, Min F, Tong J, Wei W, et al. Prevalence and associated factors of insomnia symptoms among pregnant women in the third trimester in a moderately developing region of China. BMC Public Health. (2023) 23:2319. doi: 10.1186/s12889-023-17269-0
40. Dolatian M, Mehraban Z, Sadeghniat K. The effect of impaired sleep on preterm labour. West Indian Med J. (2014) 63:62–7. doi: 10.7727/wimj.2012.305
41. Dørheim SK, Bjorvatn B, Eberhard-Gran M. Insomnia and depressive symptoms in late pregnancy: a population-based study. Behav Sleep Med. (2012) 10:152–66. doi: 10.1080/15402002.2012.660588
42. Facco FL, Kramer J, Ho KH, Zee PC, Grobman WA. Sleep disturbances in pregnancy. Obstet Gynecol. (2010) 115:77–83. doi: 10.1097/AOG.0b013e3181c4f8ec
43. Felder JN, Epel ES, Neuhaus J, Krystal AD, Prather AA. Efficacy of digital cognitive behavioral therapy for the treatment of insomnia symptoms among pregnant women: A randomized clinical trial. JAMA Psychiatry. (2020) 77:484–92. doi: 10.1001/jamapsychiatry.2019.4491
44. Felder JN, Hartman AR, Epel ES, Prather AA. Pregnant patient perceptions of provider detection and treatment of insomnia. Behav Sleep Med. (2020) 18:787–96. doi: 10.1080/15402002.2019.1688153
45. Fernández-Alonso AM, Trabalón-Pastor M, Chedraui P, Pérez-López FR. Factors related to insomnia and sleepiness in the late third trimester of pregnancy. Arch Gynecol Obstet. (2012) 286:55–61. doi: 10.1007/s00404-012-2248-z
46. Kalmbach DA, Ahmedani BK, Gelaye B, Cheng P, Drake CL. Nocturnal cognitive hyperarousal, perinatal-focused rumination, and insomnia are associated with suicidal ideation in perinatal women with mild to moderate depression. Sleep Med. (2021) 81:439–42. doi: 10.1016/j.sleep.2021.03.004
47. Kalmbach DA, Cheng P, Ong JC, Ciesla JA, Kingsberg SA, Sangha R, et al. Depression and suicidal ideation in pregnancy: exploring relationships with insomnia, short sleep, and nocturnal rumination. Sleep Med. (2020) 65:62–73. doi: 10.1016/j.sleep.2019.07.010
48. Kalmbach DA, Cheng P, Reffi AN, Seymour GM, Ruprich MK, Bazan LF, et al. Racial disparities in treatment engagement and outcomes in digital cognitive behavioral therapy for insomnia among pregnant women. Sleep Health. (2023) 9:18–25. doi: 10.1016/j.sleh.2022.10.010
49. Kalmbach DA, Roth T, Cheng P, Ong JC, Rosenbaum E, Drake CL. Mindfulness and nocturnal rumination are independently associated with symptoms of insomnia and depression during pregnancy. Sleep Health. (2020) 6:185–91. doi: 10.1016/j.sleh.2019.11.011
50. Kendle AM, Salemi JL, Jackson CL, Buysse DJ, Louis JM. Insomnia during pregnancy and severe maternal morbidity in the United States: nationally representative data from 2006 to 2017. Sleep. (2022) 45(10):zsac175. doi: 10.1093/sleep/zsac175
51. Kiviruusu O, Pietikäinen JT, Kylliäinen A, Pölkki P, Saarenpää-Heikkilä O, Marttunen M, et al. Trajectories of mothers' and fathers' depressive symptoms from pregnancy to 24 months postpartum. J Affect Disord. (2020) 260:629–37. doi: 10.1016/j.jad.2019.09.038
52. Liebana-Presa C, Martínez-Fernández MC, García-Fernández R, Martín-Vázquez C, Fernández-Martínez E, Hidalgo-Lopezosa P. Self perceived health and stress in the pregnancy during the COVID-19 pandemic. Front Psychiatry. (2023) 14:1166882. doi: 10.3389/fpsyt.2023.1166882
53. Osnes RS, Eberhard-Gran M, Follestad T, Kallestad H, Morken G, Roaldset JO. Mid-pregnancy insomnia and its association with perinatal depressive symptoms: A prospective cohort study. Behav Sleep Med. (2021) 19:285–302. doi: 10.1080/15402002.2020.1743705
54. Zhou X, Hong X, Huang K, Ding X, Yu H, Zhao J, et al. Poor sleep quality in early pregnancy increases the risk of developing gestational diabetes mellitus: a propensity score matching analysis. Sleep Breathing Schlaf Atmung. (2023) 27:1557–65. doi: 10.1007/s11325-022-02748-2
55. Bjornsdottir E, Lindberg E, Benediktsdottir B, Gislason T, Garcia Larsen V, Franklin K, et al. Are symptoms of insomnia related to respiratory symptoms? Cross-sectional results from 10 European countries and Australia. BMJ Open. (2020) 10:e032511. doi: 10.1136/bmjopen-2019-032511
56. Schmidhuber J, Traill WB. The changing structure of diets in the European Union in relation to healthy eating guidelines. Public Health Nutr. (2006) 9:584–95. doi: 10.1079/PHN2005844
57. Palagini L, Manni R, Liguori C, De Gennaro L, Gemignani A, Fanfulla F, et al. Evaluation and management of insomnia in the clinical practice in Italy: a 2023 update from the Insomnia Expert Consensus Group. J Neurol. (2024) 271:1668–79. doi: 10.1007/s00415-023-12112-3
58. Bjornsdottir E, Thorarinsdottir EH, Lindberg E, Benediktsdottir B, Franklin K, Jarvis D, et al. Association between physical activity over a 10-year period and current insomnia symptoms, sleep duration and daytime sleepiness: a European population-based study. BMJ Open. (2024) 14:e067197. doi: 10.1136/bmjopen-2022-067197
59. O'Regan D, Garcia-Borreguero D, Gloggner F, Wild I, Leontiou C, Ferini-Strambi L. Mapping the insomnia patient journey in Europe and Canada. Front Public Health. (2023) 11:1233201. doi: 10.3389/fpubh.2023.1233201
60. Höglund P, Hakelind C, Nordin M, Nordin S. Risk factors for insomnia and burnout: A longitudinal population-based cohort study. Stress Health: J Int Soc Invest Stress. (2023) 39:798–812. doi: 10.1002/smi.3218
61. Arab A, Karimi E, Garaulet M, Scheer F. Dietary patterns and insomnia symptoms: A systematic review and meta-analysis. Sleep Med Rev. (2024) 75:101936. doi: 10.1016/j.smrv.2024.101936
62. Poličnik R, Hristov H, Lavriša Ž, Farkaš J, Smole Možina S, Koroušić Seljak B, et al. Dietary intake of adolescents and alignment with recommendations for healthy and sustainable diets: results of the SI.Menu study. Nutrients. (2024) 16(12):1912. doi: 10.3390/nu16121912
63. Sonestedt E, Lukic M. Beverages - a scoping review for Nordic Nutrition Recommendations 2023. Food Nutr Res. (2024) 68. doi: 10.29219/fnr.v68.10458
64. Yusta-Boyo MJ, González EG, García-Solano M, Rollán Gordo A, Peña-Rey I, Rodríguez-Artalejo F. Reduction of sugar, salt and fat content in foods over the period 2016-2021 in Spain: the National Food Reformulation Plan. Eur J Clin Nutr. (2024) 78:149–54. doi: 10.1038/s41430-023-01357-w
65. Zheng G, Lyu X, Pan L, Chen A. The role conflict-burnout-depression link among Chinese female health care and social service providers: the moderating effect of marriage and motherhood. BMC Public Health. (2022) 22:230. doi: 10.1186/s12889-022-12641-y
66. Yan HWM. Hotspots and Prospects of fertility Support Policy Research in China: A Visual econometric Analysis based on CNKI Database Literature (2013-2023). Jianghan Acad. (2024) 2024:46–57. doi: 10.16388/j.cnki.cn42-1843/c.2024.04.005
67. Sakurai K, Kawakami N, Yamaoka K, Ishikawa H, Hashimoto H. The impact of subjective and objective social status on psychological distress among men and women in Japan. Soc Sci Med (1982). (2010) 70:1832–9. doi: 10.1016/j.socscimed.2010.01.019
68. Davis KC, Fortino BR, O'Shea NG. Potential consequences of the Dobbs v. Jackson Women's Health Organization decision. Psychol Addictive Behav: J Soc Psychol Addictive Behav. (2024) 38:161–6. doi: 10.1037/adb0000986
69. Ickovics JR, Lewis JB, Cunningham SD, Thomas J, Magriples U. Transforming prenatal care: Multidisciplinary team science improves a broad range of maternal-child outcomes. Am Psychol. (2019) 74:343–55. doi: 10.1037/amp0000435
70. Pirkle JRA. Protecting and advancing women's health and rights post-roe era through policy. Health Educ Behav: Off Publ Soc Public Health Educ. (2023) 50:538–42. doi: 10.1177/10901981231164578
71. Wu D, Chen S, Zhong X, Zhang J, Zhao G, Jiang L. Prevalence and factors associated with antenatal depressive symptoms across trimesters: a study of 110,584 pregnant women covered by a mobile app-based screening programme in Shenzhen, China. BMC Pregnancy Childbirth. (2024) 24:480. doi: 10.1186/s12884-024-06680-z
72. Vargas I, Perlis ML. Insomnia and depression: clinical associations and possible mechanistic links. Curr Opin Psychol. (2020) 34:95–9. doi: 10.1016/j.copsyc.2019.11.004
73. Zhang Jihui LY, Jiyang P. Research progress and existing problems on the relationship between insomnia and depression from 2008 to 2013. Chin J Ment Health. (2015) 2015:29.
74. Grigoriadis S, Graves L, Peer M, Mamisashvili L, Tomlinson G, Vigod SN, et al. Maternal anxiety during pregnancy and the association with adverse perinatal outcomes: systematic review and meta-analysis. J Clin Psychiatry. (2018) 79(5):17r12011. doi: 10.4088/JCP.17r12011
75. Wan EY, Moyer CA, Harlow SD, Fan Z, Jie Y, Yang H. Postpartum depression and traditional postpartum care in China: role of zuoyuezi. Int J Gynaecol Obstet: Off Organ Int Fed Gynaecol Obstet. (2009) 104:209–13. doi: 10.1016/j.ijgo.2008.10.016
76. Dunkel Schetter C, Rahal D, Ponting C, Julian M, Ramos I, Hobel CJ, et al. Anxiety in pregnancy and length of gestation: Findings from the healthy babies before birth study. Health Psychol: Off J Division Health Psychol Am psychol Assoc. (2022) 41:894–903. doi: 10.1037/hea0001210
77. Chen P, Sun HL, Zhang L, Feng Y, Sha S, Su Z, et al. Inter-relationships of depression and insomnia symptoms with life satisfaction in stroke and stroke-free older adults: Findings from the Health and Retirement Study based on network analysis and propensity score matching. J Affect Disord. (2024) 356:568–76. doi: 10.1016/j.jad.2024.04.036
78. Kim ES, Wilkinson R, Case BW, Cowden RG, Okuzono SS, VanderWeele TJ. Connected communities: Perceived neighborhood social cohesion during adolescence and subsequent health and well-being in young adulthood-An outcome-wide longitudinal approach. J Community Psychol. (2024) 52:774–91. doi: 10.1002/jcop.23130
79. Li Q, Kanduma E, Ramiro I, Xu DR, Cuco RMM, Chaquisse E, et al. Spatial access to continuous maternal and perinatal health care services in low-resource settings: cross-sectional study. JMIR Public Health Surveil. (2024) 10:e49367. doi: 10.2196/49367
Keywords: insomnia, depression, geographic location, prevalence during pregnancy, global
Citation: Yang C, Fu R, Wang H, Jiang Y, Zhang S and Ji X (2024) Evaluating the global prevalence of insomnia during pregnancy through standardized questionnaires and diagnostic criteria: a systematic review and meta-analysis. Front. Psychiatry 15:1427255. doi: 10.3389/fpsyt.2024.1427255
Received: 03 May 2024; Accepted: 25 July 2024;
Published: 13 August 2024.
Edited by:
Frank Quansah, University of Education, GhanaReviewed by:
Yi-Jun Ge, Anhui Medical University, ChinaGloria Angeletti, Sapienza University of Rome, Italy
Copyright © 2024 Yang, Fu, Wang, Jiang, Zhang and Ji. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shipeng Zhang, MTM0MzEwODc1MEBxcS5jb20=; Xiaoli Ji, aml4aWFvbGkxMDMwQHFxLmNvbQ==
†These authors share first authorship
 Chengcheng Yang1†
Chengcheng Yang1† Rui Fu
Rui Fu Yanjie Jiang
Yanjie Jiang Shipeng Zhang
Shipeng Zhang