
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 09 May 2024
Sec. Psychological Therapy and Psychosomatics
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1381105
 Jonathan Nowak1,2*†
Jonathan Nowak1,2*† Christoph Nikendei1,2†
Christoph Nikendei1,2† Ivo Rollmann1
Ivo Rollmann1 Maximilian Orth1
Maximilian Orth1 Hans-Christoph Friederich1,2
Hans-Christoph Friederich1,2 David Kindermann1,2
David Kindermann1,2Background: Adverse childhood experiences were previously identified as relevant risk factors for the development of anxiety disorders. Furthermore, anxiety disorders were shown to be associated with impairments of personality functioning. The objective of this study was to investigate adverse and protective childhood experiences as well as personality functioning, as defined by the Operationalized Psychodynamic Diagnosis system, as potential predictors for the speed of recovery during psychotherapy for patients with anxiety disorders.
Methods: The sample consisted of n = 312 completed psychotherapies. The speed of recovery, defined as symptom abatement over time, was calculated using a two-stage hierarchical linear model. The effects of adverse and protective childhood experiences as well as personality functioning on the speed of recovery during psychotherapy were then examined using a structural equation model.
Results: The presence of adverse childhood experiences predicted a lower speed of recovery during psychotherapy. In addition, a higher number of adverse childhood experiences was associated with greater impairments in the abilities of perception and regulation as dimensions of personality functioning. A higher number of protective childhood experiences was associated with fewer impairments in the communication and attachment dimensions. Impairments in personality functioning in patients with anxiety disorders did not predict the speed of recovery during psychotherapy.
Conclusions: Among patients with anxiety disorders, adverse childhood experiences lead to a lower speed of recovery during psychotherapy. Therefore, childhood adversity should be routinely assessed before and thoroughly addressed during psychotherapy in patients with anxiety disorders.
Anxiety disorders are among the most common mental disorders in the general population worldwide, with an estimated 12-month prevalence of approximately 11.6% (1). Previous studies have consistently found strong associations between anxiety disorders and adverse childhood experiences (ACEs). ACEs are defined as „abuse and household dysfunction during childhood” (2) and include emotional, physical and sexual abuse, physical and emotional neglect, household exposure to substance abuse, mental illness, domestic violence, parental separation or divorce, and criminal behavior (3). In a recent epidemiological study, 30% of anxiety disorder cases in North America and more than 25% of anxiety disorder cases in Europe were attributable to ACEs (4). Risk associations for the development of anxiety disorders have consistently been found for various types of adverse and traumatic childhood experiences, including sexual abuse, physical abuse, emotional abuse, and neglect (5–9). Furthermore, ACEs were previously identified as being associated with greater clinical complexity in patients with psychiatric disorders, e.g. more comorbidities, higher than typical intensity or duration of interventions, and poorer outcomes of treatment (10–12). Recent research has also begun investigating the role of protective childhood experiences (PCEs) and their interaction with ACEs (13–15). Findings regarding PCEs in anxiety disorders include moderating effects of PCEs on ACEs that influence the development of anxiety symptoms during adolescence (16) and are associated with a lower risk for later adolescent anxiety (17).
In addition to their connection with adverse and protective childhood experiences, anxiety symptoms and disorders have previously been found to be closely associated with personality traits, such as high neuroticism, low extraversion, and personality disorders (18). In particular, Cluster C personality disorders, namely avoidant personality disorder, dependent personality disorder, and obsessive-compulsive personality disorder, were shown to be associated with anxiety symptoms (18, 19). More recent studies examining the relationship between personality characteristics and anxiety symptoms focused on the concept of personality functioning in terms of the dimensional, alternative model for personality disorders according to DSM-5 (e.g. 20). With respect to this, Doering et al. (2018) demonstrated that anxiety disorders are associated with significant impairments of personality functioning, which were, in turn, shown to be significantly increased by comorbid personality disorders (21). Another prominent approach of assessing personality functioning on a dimensional level is the Operationalized Psychodynamic Diagnosis System, Version 2 (OPD-2), which is a multiaxial diagnostic and classification system developed on the basis of psychodynamic concepts (22–25). According to the OPD-system, personality functioning is operationalized as consisting of four dimensions, namely the basic mental abilities of perception/cognition, regulation, communication, and attachment (24, 25). In a recent cross-sectional study examining personality functioning, according to the OPD-system, in different anxiety disorders, it was illustrated that anxiety disorders differ with regard to impairments of specific dimensions of personality functioning (26). Furthermore, longitudinal studies in patients with anxiety and mood disorders also indicated changes in personality functioning during the course of psychotherapy (27–29). It is assumed that improvement in personality functioning may be associated with improvement of symptoms during psychotherapy (27, 30). However, it remains unclear how impairments in personality functioning at the onset of psychotherapy may predict treatment outcome in anxiety disorders.
Aside from the findings that both ACEs and personality functioning are each associated with treatment outcome in psychotherapy, ACEs have repeatedly been linked to personality functioning (23, 31–35). For example, it was found that the interaction between ACE and personality functioning predicts psychopathology, including anxiety symptoms (36). Assessing a heterogeneous sample of psychotherapy patients, Kindermann et al. (2023) recently showed that ACEs were directly associated with a lower speed of recovery during psychotherapy. Furthermore, ACEs were demonstrated to have indirect effects on the speed of recovery by being associated with impairments in the communication dimension of personality functioning, which, in turn, was associated with a slower improvement of symptoms (37).
As far as we are aware, no specific studies have been conducted analyzing possible predictive effects of childhood experiences on the speed of recovery during psychotherapy of patients with anxiety disorders. Furthermore, with respect to the previous study by Kindermann et al. (37), it remains unclear whether impairments in specific dimensions of personality functioning might also be predictive of the speed of recovery in patients with anxiety disorders. With this in mind, evaluating ACEs and impairments in specific dimensions of personality functioning before starting psychotherapy could be a relevant component of treatment planning. Based on previous studies, our hypotheses were the following: (a) Adverse and protective childhood experiences in patients with anxiety disorders predict the speed of recovery during psychotherapy, defined as symptom abatement (according to Hopkins Symptom Checklist, SCL-K11) over time; (b) Adverse and protective childhood experiences show differential associations with individual dimensions of personality functioning in patients with anxiety disorders; (c) Impairments in individual dimensions of personality functioning predict the speed of recovery during psychotherapy in patients with anxiety disorders.
This study is a retrospective study of routinely assessed longitudinal data during outpatient psychodynamic psychotherapy within the Heidelberg Institute of Psychotherapy, Heidelberg, Germany.
The present study is based on the data of a routine survey of psychotherapy sessions at the Heidelberg Institute of Psychotherapy, Heidelberg, Germany, in the period between January 2013 and July 2021 (38). At the end of the survey period, some treatments had already been completed, as far as documented in the institute, while others were still ongoing. This study is based on NCompleted = 648 completed psychotherapies from NTotal = 1646 psychotherapies that took place between January 2013 and July 2021. Among all completed psychotherapeutic treatments, NAnxiety = 312 psychotherapies were treatments of patients who had been diagnosed with at least one anxiety disorder. Patients were included after providing written informed consent.
Therapists underwent a postgraduate training program in psychodynamic therapy at the Heidelberg Institute of Psychotherapy. NTherapist = 172 therapists participated in this study. Therapists had at least 1.5 years of clinical experience and either a degree in psychology (M.Sc. or Ph.D.) or were medical residents (MD). Each therapist treated M = 9.4 patients (SD = 5.4). Every fourth session was supervised by an experienced psychodynamic psychotherapist with at least 5 years of clinical experience.
The present study applied both patient-related and therapist-related criteria for a psychotherapeutic treatment to be included: Patients (I) had to be proficient in German or English, (II) must have had at least one diagnostic session with their psychotherapist, and (III) had to have been diagnosed with at least one anxiety disorder (i.e. agoraphobia, social phobia, specific phobia, panic disorder, generalized anxiety disorder). Furthermore, therapists (IV) had to indicate that psychotherapy had been completed. We based the study on completed psychotherapeutic treatments, as it is unclear to what extent a patient’s symptoms can still improve while psychotherapy has not yet concluded.
The study protocol was developed according to the Helsinki II declaration (39). Prior to recruitment of patients and therapists, the study was approved by the independent Ethics Committee of the Medical Faculty of the University of Heidelberg (S-195/2014). Written informed consent was obtained from all study participants.
All patients seeking psychotherapy underwent the following procedure (see Figure 1): First, a clinical intake interview was conducted to assess indication for psychodynamic psychotherapy (38). During the interview, patients were invited to participate in the study. They were then informed about the study and asked for written informed consent. After this, patients had to answer the sociodemographic and psychometric questionnaires and a standardized diagnostic interview (SCID-I and SCID-II: 40, German version: 41) took place with a trained graduate student (at least B.Sc. in psychology). Patients were then referred to a therapist of the Heidelberg Institute of Psychotherapy involved in the study.
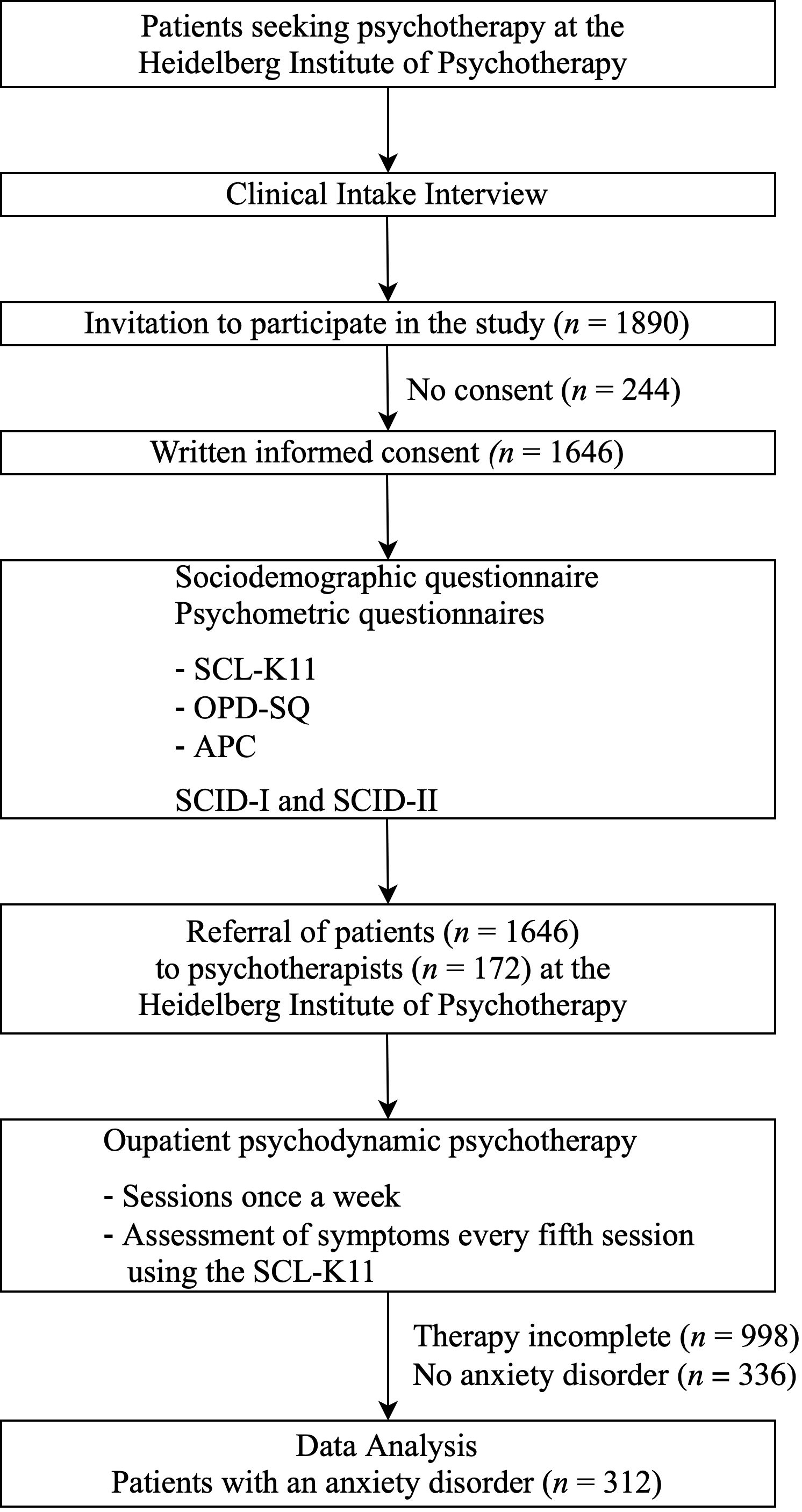
Figure 1 Procedure. The present study was based on data collected between January 2013 and July 2021. At the end of the survey period, some treatments had already been completed, while others were still ongoing. Data analysis was based on completed psychotherapeutic treatments. SCL-K11 = Short Version of the Hopkins Symptom Checklist; OPD-SQ = Operationalised Psychodynamic Diagnosis Structure Questionnaire; APC = Questionnaire for the Assessment of Adverse and Protective Childhood Experiences; SCID = Structured Clinical Interview.
Treatment was conducted in the form of outpatient psychodynamic psychotherapy. Psychotherapy sessions took place once a week with a length of 50 minutes. The German public health care system fully covers psychotherapy fees, but patients must apply for a quota of sessions in predefined steps (12, 24, 60 and 100 sessions). Before applying for psychotherapy sessions, patients are required to take up to seven preparatory and diagnostic sessions. The number of conducted therapy sessions was agreed individually between therapist and patient according to severity and psychotherapeutic focus of the treatment. We included therapies of all lengths to increase external validity. After every fifth session, patients were asked to answer the German 11-item short version of the Hopkins Symptom Checklist (SCL-K11; 42, German Short Version: 43) stated below. On average, patients had M = 57.7 (SD = 29.7, Min = 4, Max = 120) psychotherapy sessions and participated in M = 6.34 (SD = 6.2) repeated assessments for the SCL-K11.
The SCL-K11 assesses the patients experienced symptom severity, including anxiety symptoms (42, German Short Version: 43). Patients are asked to rate the severity of their psychological and somatic symptoms on a five-point-Likert scale from 1 (not at all) to 5 (all the time). The SCL-K11 is reported to have excellent psychometric properties for the 11-item short version (43). Within our total patient sample, internal consistency was high, with a range of Cronbach’s α of.87 -.95 at all measurement occasions.
In the present study, the Operationalised Psychodynamic Diagnosis, second edition (OPD-2) system was used to assess personality functioning (32). The OPD-2 consists of five axes: Axis I= experience of illness and prerequisites for treatment; Axis II= interpersonal relations; Axis III= conflict; Axis IV= structure; Axis V= mental disorders according to ICD-10 (25, 44). Axis IV is also described as Levels of Structural Integration Axis (LSIA) (32). From a conceptual perspective, the LSIA exhibits great overlap with the Levels of Personality Functioning Scale (LPFS), according to DSM-5 (25). The OPD-SQ is a self-assessment questionnaire that addresses the basic dimensions of personality structure (Axis IV of OPD), which can also be referred to as personality functioning: perception/cognition, regulation, communication, and attachment (25, 32). It consists of 95 items and comprises eight subscales, with two subscales for each of the aforementioned four dimensions. The subscales are measured by a five-point-Likert scale from ‘0 = Not true at all’ to ‘4 = is completely true’. Higher scores represent greater impairments in personality functioning. Patients answered the OPD-SQ after the clinical intake interview. Within our total patient sample, internal consistency was high for the subscales of perception/cognition of the self (α = .89) and objects (α = .85); regulation of the self (α = .85) and relationships (α = .85); communication with the internal (α = .78) and external (α = .74) world; and attachment to internal (α = .81) and external (α = .77) objects.
The APC (45) is a self-assessment questionnaire assessing protective childhood experiences (PCE) and adverse childhood experiences (ACE). The questionnaire consists of 59 items (including 17 items for PCE and 40 items for ACE); patients are asked how often they had a specific childhood experience on a five-point-Likert scale from ‘0 = Never’ to ‘4 = Very Often’. The ACE scale comprises questions regarding emotional neglect and abuse, physical neglect and abuse, sexual abuse, traumatic experiences, separation experiences, dysfunctional family situation and missing or dysfunctional peer-group experiences, for example: “In my childhood and youth I was unwanted, I was rejected or made to feel that I was better off not being born” (Item 11). The PCE scale addresses experiences of feeling protected and secure in the family, of respectful interaction and mutual support within the family, of being able to rely on caregivers, of being comforted when feeling sad, and of being accepted and loved for who one was, for example: “In my childhood and youth, I was comforted when I was sad” (Item 23). The APC demonstrates high convergent validity with significant correlations to the childhood trauma questionnaire (CTQ) (45). In addition, Ehrenthal et al. (2020) found a significant negative correlation between PCE, measured by the APC, and the CTQ sum score (45). For this study, the PCE scale (Cronbach’s α = .95) and the ACE scale (Cronbach’s α = .93) were both used (45). We measured the childhood experiences directly after the initial interview.
For our power analysis, we used the R package ‘semtools’ (Version 5.6) (46). Model A assumes every possible effect and will always fit perfectly (47). Therefore, the power analysis was based on Model B, which only assumed indirect effects of childhood experiences on the speed of recovery. Thus, model B had df = 2. Following Kline’s (47) recommendation, we calculated the required sample size for a poor fit test (H0: RMSEA =0.1, HA: RMSEA = 0.01). With our sample size of NAnxiety=312 patients, we achieved a power of.66.
Missing data analysis and imputation was done within the R environment (48) using the package ‘mice’ (Version 3.16) (49). Our subsample of anxiety patients with completed psychotherapies had 13.2% missing data, which resulted in the need of a missing at random assumption and the need of multiple imputation (50). For our imputation model, we included all sociodemographic and psychometric data available and excluded variables with an influx above 0.50 (50). For imputation, we used predictive mean matching. Sum scores were imputed using passive imputation. On average, a variable was predicted with 28.7 predictors (50). The imputation results were checked for plausibility using density, box-and-whisker, and scatter plots (50). For more information, we refer to our online repository, in which the complete analysis is uploaded: https://doi.org/10.11588/data/AJKTKU.
The sample description was done using Microsoft Excel 2019. All further analyses were conducted using R, Version 4.3.1 (48). Calculations were done with the subsample of anxiety patients which completed their psychotherapy. However, for calculation of internal consistencies, we used the total sample of 1646 psychotherapies, also including therapies that treated depression, eating disorders etc., to achieve a more precise estimation of internal consistencies. Imputation was done after calculation of the speed of recovery because imputation of longitudinal data is not robust (50, 51). For more information, we refer to our online repository, in which the complete analysis and results are uploaded: https://doi.org/10.11588/data/AJKTKU.
All calculations of the speed of recovery were done using the R package ‘nlme’ (Version 3.1-162) (52) and ‘r2mlm’ (Version 0.3.3) (53) using Restricted Maximum Likelihood estimation. Because the symptom severity of patients was right-skewed, we logarithmised symptom severity. Scatterplots of logarithmic symptom severity against therapy hours then showed only a linear relationship. Therefore, we compared two hierarchical linear models to calculate the speed of recovery. We used a null model, which assumed no decrease in symptom severity, and a linear model with random intercept and random slopes with time as the only predictor. Model fit was checked by testing the residuals for normal distribution and heteroscedasticity (54, 55). Model comparison was done using R², MAE, RMSE, and a likelihood ratio test based on the Akaike Information Criterion and Bayesian Information Criterion. Adopting the linear hierarchical model, we extracted the individual slope parameters of the patients. As symptom severity decreases during therapy, we inverted the slope parameter to facilitate interpretation. Thus, a higher value represents a higher speed of recovery.
All calculations for the structural equation models were conducted with the R packages ‘lavaan’ (Version 0.6-15) (56) and ‘semtools’ (Version 0.5-6) (46) using Maximum Likelihood estimation and their default settings. All tested models were recursive and thus identified (47). Skewness was between -1 and 1 for all variables and excess kurtosis between -4 and 4. Thus, our variables could be considered sufficiently normally distributed (47). We computed our models on each imputed dataset and pooled the results using Rubin’s Rule (50). We first calculated Model A, which assumes effects between all variables. To account for sociodemographic and routinely assessed clinical data, we included age, gender, education (operationalized via the highest educational attainment), and the number of ICD-10 diagnoses in addition to adverse and protective childhood experiences, the four dimensions of personality functioning, and the speed of recovery. In Model B, we removed non- significant paths stemming from Model A if there was a theoretical rationale supported by preliminary studies (47). Both models were checked for global fit using the χ²-Test, the global fit indices SRMR, CFI, the RMSEA, and the 90% confidence interval of the RMSEA. Local fit of both models was assessed using the differences between the observed and calculated correlation matrix. According to Kline (47), a good local fit can be assumed if no difference is greater than 0.1. The models were then compared using a χ²-Test. Finally, we calculated the power post-hoc for our Model B.
We report how we determined our sample size, all data exclusions, all manipulations, and all measures in the study, and we follow the Journal Article Reporting Standards (JARS; 57, 58). The analysis code is available at https://doi.org/10.11588/data/AJKTKU. The datasets used and analyzed during the present study cannot be shared due to restrictions by the Ethics Committee of the University of Heidelberg. However, data can be requested from the author J. Nowak (jonathan.nowak@med.uni-heidelberg.de) upon reasonable request and with permission of the Ethics Committee of the University of Heidelberg. Data were analysed using R, Version 4.3.1 (48), all packages are stated above. This study’s design and analysis were not pre-registered.
All results are available at https://doi.org/10.11588/data/AJKTKU.
Between January 2013 and July 2021, a total of 1890 psychotherapies were conducted at the Heidelberg Institute of Psychotherapy. Written informed consent was given for 1646 psychotherapies. This corresponds to a participation rate of 87.1%. Overall, 648 patients completed their psychotherapy, of whom 312 patients were diagnosed with at least one anxiety disorder (see Table 1). As demonstrated in Table 1, the subsample of patients with anxiety disorders is slightly younger, has a higher proportion of female patients, and, on average, has one more ICD-10 diagnosis than the patients from the total sample of completed psychotherapies. Furthermore, it appears that the anxiety subsample has a minimally higher proportion of comorbid depression, substance use disorders, posttraumatic stress disorder (PTSD), and eating disorders. Moreover, there is a higher comorbidity of personality disorders in the assessed anxiety patients. Of all patients with anxiety disorders, 32.4% were found to have social phobia, 26.9% specific phobia, 26.0% panic disorder, 25.7% agoraphobia, 16.0% generalized anxiety disorder, 9.9% unspecified anxiety disorder, and 1.28% hypochondriasis.
Table 2 shows the mean decrease in symptom severity per measurement time point. At the beginning of therapy, a sharp drop in symptom severity was identified. As therapy progressed, symptom abatement decreased.
Due to missing values, the null model used 287 patients with a total of 3014 measurements and estimated the intercept at 0.65 (SE = 0.02, df = 2727, t = 38.02, p <.001). The standard deviation of the intercept and residual were 0.28 and 0.23, respectively. The intercept explained 59.69% of all variance. Diagnostic plots revealed heteroscedasticity and non-normally distributed residuals. Thus, not all effects have been captured in the model (55). RMSE and MAE of the null model were 0.22 and 0.17 respectively.
The results for the linear model can be seen in Table 3. There is a significant linear slope of psychotherapy sessions on logarithmized symptom severity. This means that symptom severity decreases exponentially with the number of therapy sessions. The slope varies between each patient with a standard deviation of 0.02; this variation explains about 6.77% of the total variance. In total, the linear model explains about 74.81% of the variance, 15.12% more than the null model. Residuals are not normally distributed and exhibit heteroskedasticity. Therefore, not all effects are captured in this model either (55). RMSE and MAE of the linear model were 0.19 and 0.14 respectively. The log-likelihood ratio test showed a significant difference between the two models (dfnull = 3, dflinear = 6, Likelihood ratio = 484.68, p <.001). Therefore, we accepted the linear model.
Table 4 shows the differences between the means and standard deviations of the original data with missing values and the average mean and standard deviation of the 20 imputed data sets. Table 4 also depicts the standard error, calculated using Rubin’s rule (50). Across all variables that were included in the model, the average mean and standard deviation of the imputed data sets are the same as those of the original data. Patients with missing values, on average, most likely do not differ from patients without missing values.
Model A assumes effects between all variables and therefore has perfect global and local fit to the data. As in the previous study by Kindermann et al. (37), protective childhood experiences had no significant effect on the speed of recovery. Therefore, we removed this path for Model B. Furthermore, age, gender, and education also had no significant effect on the speed of recovery. As there have been previous studies also showing that sociodemographic variables, like age and gender, have no effect on psychotherapy outcome (e.g. 21, 59, 60), we decided to remove those paths for Model B. Although the number of diagnoses had no significant effect on the speed of recovery, there was no theoretical rationale to remove this variable; therefore, we decided to keep this path in the model.
Global Fit. Model B showed mixed global fit indices. The χ²-Test was not significant (χ² = 0.827, df = 4, p = .935) and the model could therefore be tentatively accepted. The CFI and TLI were 1.000 and 1.033, respectively. The RMSEA was.000 (90% CI = [.000;.022]). Since the upper interval of the RMSEA is lower than 0.05, the not-close-fit test and the poor-fit test are significant (47). Therefore, the model fits better than a not-close fitting model. The Likelihood ratio test showed no significant difference to Model A (F = 0.207, df1 = 4, df2 = 542.433, p = 0.935).
Local Fit. The parameter estimates are shown in Table 5. The direct effect of ACEs on the dimensions of perception and regulation within personality functioning were found to be significant. For PCEs, the direct effects on the dimensions of attachment and communication were found to be significant. No direct effects of dimensions of personality functioning on the speed of recovery were significant. A visualization of these paths and their significance can be seen in Figure 2. Age and the number of diagnoses both had direct effects on all four dimensions of personality functioning. Gender only had a direct effect on the dimension of attachment; education had no direct effect on any dimension of personality functioning. A comparison of the observed and calculated correlations from Model B showed that no correlation is severely underestimated, as can be seen in Table 6. Thus, Model B has a good local fit and can be accepted (47).
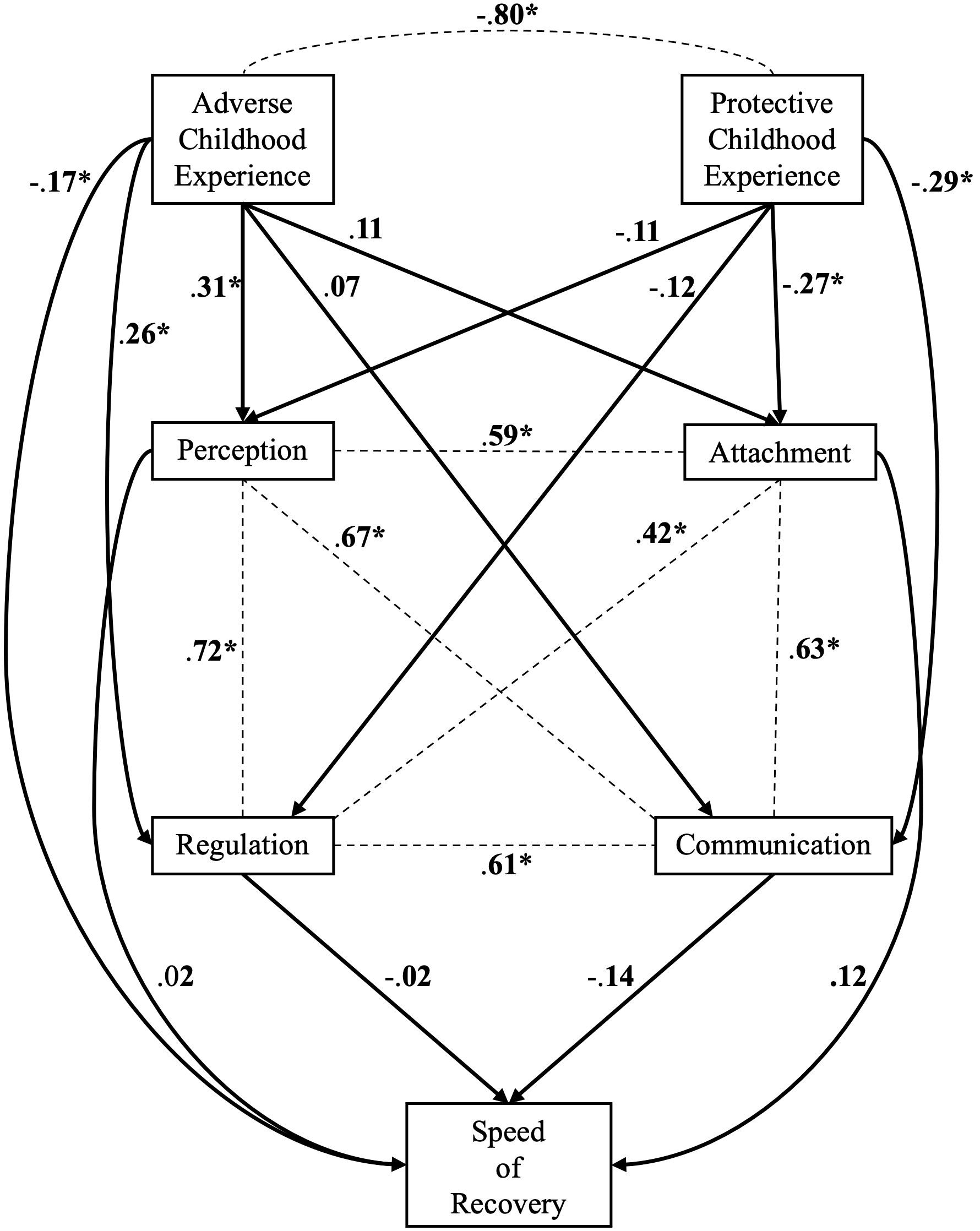
Figure 2 Model B. To achieve readability we omitted all disturbances, variances and all paths connected to the covariates; we only visualized the path corresponding to our hypotheses. The omitted path can be seen in Table 5. Dotted Lines represent correlations and arrows represent direct effects. Standardized values are shown. * p <.05.
For our post-hoc power analysis, we calculated the power of the poor-fit test assuming H0 = .10 and HA = .01 with df = 4 and n = 312 using the ‘semtools’ package (46). We obtained a power of .77.
According to Kline (47), R² equals 1- Disturbance (= error + unknown causes) for endogenous variables. Accordingly, we obtained a R² of 1 - 0.964 = .036 for the speed of recovery. Therefore, our model explains 3.6% of variance of speed of recovery for patients with anxiety disorders.
The present study examined adverse and protective childhood experiences as well as personality functioning as potential predictors for the speed of recovery in psychotherapy of patients with anxiety disorders. A higher number of ACEs was found to predict a lower speed of recovery during psychotherapy in terms of a direct effect. The effect of ACEs on the speed of recovery was still present after controlling for age, gender, education, and number of diagnoses. Furthermore, a higher number of ACEs was associated with greater impairments in the abilities of perception and regulation as dimensions of personality functioning. However, none of the dimensions in personality functioning showed significant associations with the speed of recovery in psychotherapy. Therefore, concerning the variables included in our model, ACEs seem to have direct but no indirect effects on the speed of recovery in anxiety disorders. On the other hand, a higher number of PCEs was associated with fewer impairments in the abilities of communication and attachment as dimensions of personality functioning, but had no direct effect on the speed of recovery during psychotherapy.
Our main result was the finding that ACEs are a predictor of a lower speed of recovery during psychotherapy in patients with anxiety disorders. There are few previous studies that have examined predictors of treatment outcome across different anxiety disorders. In 2016, Jakubovski & Bloch were able to identify comorbid depression and a low socioeconomic status as the most important predictors of poor therapy outcome across different anxiety disorders (61). In contrast, an association between a good treatment outcome on the one hand and positive treatment expectancy and high self-efficacy expectancy on the other hand could be demonstrated (61). In a 2012 study, Wolitzky-Taylor et al. (2012) analyzed non-specific predictors of treatment outcome for different anxiety disorders in comparison of cognitive behavioral therapy (CBT) to acceptance and commitment therapy (ACT) (62). It was shown that higher baseline neuroticism was associated with a poorer outcome across the two different treatment conditions; ethnicity, age, gender, and baseline severity of anxiety disorder were not predictive of treatment outcome (62). In the present study, we found a direct effect of ACEs on the speed of recovery during psychotherapy in patients with anxiety disorders, which persisted after controlling for age, gender, education, and number of diagnoses. In previous studies, the effects of ACEs on treatment outcome have been studied primarily in relation to depressive disorders, wherein a higher number of ACEs was associated with a higher symptom severity and complexity, as well as with a poorer treatment outcome in patients with depressive disorder, assuming a dose-response relationship of experienced ACEs (12, 31, 63, 64). A similar relationship between ACEs and treatment outcome has been reported for borderline personality disorder (65), substance abuse disorders (66) as well as for a heterogenous sample of psychiatric outpatients (10). Previous studies explained the association between ACEs and poorer treatment outcome in different ways: On the one hand, ACEs are assumed to lead to a higher psychopathological symptom severity and to a greater number of comorbidities, which in turn could be associated with a worse therapy outcome (67, 68). On the other hand, previous studies indicated that individuals with ACEs exhibit a high risk of developing insecure attachment, which may lead to disturbances in therapeutic alliance in psychotherapeutic treatment, ultimately resulting in poorer outcome (68–73). Overall, our finding that a history of ACEs may lead to a lower speed of recovery in psychotherapy is consistent with the results of previous studies on other mental disorders.
In our study, childhood experiences were assessed retrospectively, namely once before the beginning of psychotherapy. However, with regard to childhood experiences, some studies found evidence that the recollection of these memories might change during psychotherapy (74). In a recent study, Ernst et al. (2023) assessed self-reported childhood adversity before and after 7-8 weeks of inpatient psychotherapy (75). After treatment, patients were shown to report some kinds of abuse and neglect as more severe (75). Furthermore, these changes in the recollection were found to be related to a reduction of depressive symptoms, indicating that a new evaluation of past events might be connected to symptom improvement (75). However, other studies investigating the stability of self-reported childhood adversity over time found no significant changes (76, 77). In their 2018 study, Frampton et al. (2018) examined the effects of depression on the recollection of ACEs and found that changes in depressive symptoms did not correspond with changes in the recollection of ACEs (77). Frampton et al. (2018) concluded that ACE measurements seem to be reliable and stable over time, regardless of depression status (77). Overall, there are heterogeneous findings regarding the stability of self-reported ACEs over time and their possible impact on the course of treatment. Therefore, in order to further investigate how potential changes in recollection might affect recovery during psychotherapy and to what extent psychopathology or other factors might influence the recollection of childhood adversity, future research should assess the recollection of childhood experiences pre- and post-treatment with regard to different diagnostic entities.
With regard to the relationship between specific personality characteristics and anxiety disorders, previous studies have mainly focused on personality disorder traits (78). Epidemiological studies have demonstrated a high comorbidity with personality disorders of Cluster C in anxiety patients, with the avoidant personality disorder occurring most frequently, followed by the obsessive-compulsive, and the dependent personality disorder (19). In a 2014 study, Skodol et al. found that a variety of personality disorders predicted the persistence of anxiety disorders over 3 years (79). Therefore, personality psychopathology seems to be not only a risk factor but also a maintaining factor for anxiety disorders. Skodol et al. concluded their study with the recommendation that personality psychopathology should be assessed and addressed in psychotherapeutic treatment for all patients with anxiety disorders (79). In their 2018 study, Doering et al. (2018) investigated personality functioning in patients with generalized anxiety disorder, panic disorder, and phobia. Significant impairments of personality functioning were found in all three patient groups compared to a control group (21). However, they found no differences in personality functioning between patients with different anxiety disorders. In a recent cross-sectional study, Nowak et al. (2023) examined personality functioning according to OPD in anxiety disorders, comparing patients with generalized anxiety disorder, panic disorder and phobic disorders with non-anxiety patients (26). It was discovered that anxiety patients showed greater impairments in the overall mean as well as in most dimensions of personality functioning compared to patients without anxiety disorder. More specifically, in comparison to other anxiety disorders, patients with phobic disorders showed significantly greater impairments in the ability to communicate with the external world as one dimension of personality functioning (26). Furthermore, evidence was found that patients with generalized anxiety disorder have greater impairments in the ability of self-regulation than patients with other anxiety disorders (26). In summary, our results underscore the findings from previous studies that anxiety disorders are associated with impairments in personality functioning.
The present study provided further evidence that specific impairments in personality functioning in patients with anxiety disorders seem to be associated with ACEs. However, we found no direct effects of personality functioning on the speed of recovery during psychotherapy. Our findings are partially consistent with the recent study by Kerber et al. (2023), in which ACEs and personality functioning were examined as predictors of anxiety symptoms, depressiveness, and somatization (36). In this cross-sectional study, while it was shown that ACEs were positively associated with psychopathology, an association between ACEs and impairments of personality functioning was also found. Furthermore, in a recent study, Dagnino et al. (2020) investigated the relationship between ACEs, personality functioning, and depressive symptomatology and found that personality functioning mediated the relationship between ACEs and depressive symptoms; thus, this finding also implies indirect effects of ACEs on depressive symptoms via personality functioning (31). However, most of the previous studies did not clearly differentiate which individual dimensions of personality functioning may have an effect on symptom severity or on the speed of recovery in psychotherapy. Kindermann et al. (2023) recently found that ACEs had direct as well as indirect effects on the speed of recovery by being associated with impairments in the communication dimension of personality functioning, which in turn was associated with a lower speed of recovery (37). In contrast, the present study found direct, but no indirect, effects of ACEs on the speed of recovery in patients with anxiety disorders. Therefore, while our hypotheses (a) and (b) were confirmed, hypothesis (c) could not be confirmed. A possible explanation for this finding could be that the effect of personality functioning on the speed of recovery during psychotherapy is rather small and emerges as non-significant due to the relatively small group size of the present study. This assumption may be underscored by the previous study by Kindermann et al. (2023), in which the effect sizes of personality functioning on the speed of recovery were also found to be small (37). Furthermore, recent studies assumed that, in particular, changes in personality functioning during psychotherapy may be predictive of treatment outcome (27, 30). This notion could indicate that, although the present study found that the pre-treatment assessed personality functioning was not predictive for the speed of recovery, changes in personality functioning during psychotherapy may be predictive. Therefore, the improvement of personality functioning in anxiety patients should remain an important target of psychotherapy.
In previous studies, ACEs were mainly related to a higher risk of developing mental illness, higher symptom burden, and poorer treatment outcome (10–12). However, childhood adversity was found to be not necessarily associated with psychosocial distress (80). With regard to traumatic experiences, it was shown that stressful life events may also lead to positive psychological changes, which can be referred to as posttraumatic growth (PTG; 81). The concept of PTG refers to subjectively experienced positive changes, such as an increased appreciation for one’s life, increased experience of closeness in relationships, or an increased recognition of personal strengths in the aftermath of traumatic events (81). Previous studies were able to identify PTG in individuals having experienced sexual abuse (82) or neglect (83) in their childhood. In a 2021 study, Tranter et al. (2021) investigated the association between ACEs and PTG and identified emotional resilience as a mediating factor, which could represent an important target in psychotherapeutic treatment of individuals that have experienced childhood adversity (84). Furthermore, Tranter et al. (2021) concluded that psychotherapeutic interventions could focus on enhancing the awareness of potential positive changes after childhood adversity to encourage the patients to recognize possible gains from their childhood experiences (84). However, it still remains unclear which other variables may influence whether ACEs result in psychological distress or psychological growth.
Overall, the results of the present study emphasized the important role that childhood adversity plays in the course of psychotherapy for patients with anxiety disorders. Consequently, ACEs should be routinely assessed before starting psychotherapy and thoroughly addressed during psychotherapy in patients with anxiety disorders. Further research is needed to specify the complex relationships between childhood experiences, individual dimensions of personality functioning, and their possible effect on the course and outcome of psychotherapy in anxiety disorders.
The present study was an exploratory study designed to collect first data on the relationship between ACEs, personality functioning, and the speed of recovery during psychotherapy in patients with anxiety disorders. Several limitations of the presented study should be addressed, with some related to the exploratory approach of the study. First of all, it must be pointed out that we assessed childhood experiences and dimensions of personality functioning simultaneously. Although theoretical considerations and the results of previous studies may lead to the conclusion that childhood experiences could influence the dimensions of personality functioning, the simultaneous assessment of both variables ultimately does not allow any statement on causality. One could possibly argue that impairments in specific dimensions of personality functioning may lead to distorted childhood memories, which in turn lead to a lower speed of recovery in psychotherapy. Another limitation is the fact that the present study only assessed childhood experiences pre-treatment; however, previous studies could demonstrate that the recollection of adverse childhood experiences can change during psychotherapy and can therefore be considered as not being perfectly stable over time (75). Furthermore, a major limitation is the fact that the present study only assessed personality functioning pre-treatment and did not assess changes in personality functioning during therapy, which in turn could interact with the speed of recovery. Future studies should therefore also investigate changes in the recollection of childhood memories and/or changes in personality functioning in parallel with the speed of recovery during psychotherapy. The patients’ heterogeneity with regard to the different anxiety disorders (i.e. panic disorder, generalized anxiety disorder, phobic disorders) may be a further limitation of our results, as individual and diagnosis-specific aspects of personality functioning and the speed of recovery were not addressed accordingly. Thus, it cannot be excluded that the relationship between ACEs, PCEs, and personality functioning differs across diagnostic entities.
The presence of ACEs had a direct effect on the speed of recovery during psychodynamic treatment of patients with anxiety disorders. Moreover, ACEs and PCEs were shown to be associated with specific dimensions of personality functioning. Therefore, evaluating childhood experiences before starting psychotherapy could be a relevant component for treatment planning. Future studies should focus particularly on the complex relationship between childhood experiences, personality functioning, and treatment outcome in different mental disorders.
The data that support the findings of this study were collected at the outpatient training clinic for psychodynamic therapy at the University Hospital Heidelberg, Germany (https://www.klinikum.uni-heidelberg.de/zentrum-fuer-psychosoziale-medizin-zpm/hip/heidelberger-institut-fuer-psychotherapie-hip). Data can be supplied by the author J. Nowak (jonathan.nowak@med.uni-heidelberg.de) upon reasonable request and after permission has been granted by the Ethics Committee of the University of Heidelberg. The analysis code of our data analysis is publicly available at: https://doi.org/10.11588/data/AJKTKU.
The studies involving humans were approved by Ethics Committee of the Medical Faculty of the Heidelberg University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
JN: Methodology, Writing – review & editing, Writing – original draft, Conceptualization. CN: Methodology, Writing – review & editing, Writing – original draft, Supervision, Project administration, Conceptualization. IR: Writing – review & editing, Writing – original draft, Visualization, Software, Methodology, Formal analysis, Conceptualization. MO: Writing – review & editing, Software, Formal analysis, Data curation. HF: Writing – review & editing, Supervision. DK: Writing – review & editing, Writing – original draft, Supervision, Methodology, Conceptualization.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Open Access funding enabled and organized by “Projekt DEAL”. For the publication fee we acknowledge financial support by Deutsche Forschungsgemeinschaft within the funding programme “Open Access Publikationskosten” as well as by Heidelberg University.
We thank Molly Sutcliffe for English language editing. The manuscript has been uploaded as a preprint on “Research Square”, DOI: https://doi.org/10.21203/rs.3.rs-3698147/v1.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Baxter AJ, Scott KM, Vos T, Whiteford HA. Global prevalence of anxiety disorders: a systematic review and meta-regression. psychol Med. (2013) 43:897–910. doi: 10.1017/S003329171200147X
2. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. (1998) 14:245–58. doi: 10.1016/S0749-3797(98)00017-8
3. Dong M, Anda RF, Felitti VJ, Dube SR, Williamson DF, Thompson TJ, et al. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse neglect. (2004) 28:771–84. doi: 10.1016/j.chiabu.2004.01.008
4. Bellis MA, Hughes K, Ford K, Rodriguez GR, Sethi D, Passmore J. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet Public Health. (2019) 4:e517–e28. doi: 10.1016/S2468-2667(19)30145-8
5. Carr MJ, Steeg S, Mok PL, Pedersen CB, Antonsen S, Kapur N, et al. Adverse childhood experiences and risk of subsequently engaging in self-harm and violence towards other People—“Dual Harm”. Int J Environ Res Public Health. (2020) 17:9409. doi: 10.3390/ijerph17249409
6. Gardner M, Thomas H, Erskine H. The association between five forms of child maltreatment and depressive and anxiety disorders: A systematic review and meta-analysis. Child Abuse neglect. (2019) 96:104082. doi: 10.1016/j.chiabu.2019.104082
7. Kisely S, Abajobir AA, Mills R, Strathearn L, Clavarino A, Najman JM. Child maltreatment and mental health problems in adulthood: birth cohort study. Br J Psychiatry. (2018) 213:698–703. doi: 10.1192/bjp.2018.207
8. Li M, D'Arcy C, Meng X. Maltreatment in childhood substantially increases the risk of adult depression and anxiety in prospective cohort studies: systematic review, meta-analysis, and proportional attributable fractions. psychol Med. (2016) 46:717–30. doi: 10.1017/S0033291715002743
9. Lindert J, von Ehrenstein OS, Grashow R, Gal G, Braehler E, Weisskopf MG. Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: systematic review and meta-analysis. Int J Public Health. (2014) 59:359–72. doi: 10.1007/s00038-013-0519-5
10. Maunder RG, Wiesenfeld L, Lawson A, Hunter JJ. The relationship between childhood adversity and other aspects of clinical complexity in psychiatric outpatients. J interpersonal violence. (2021) 36:9060–76. doi: 10.1177/0886260519865968
11. Maunder RG, Wiesenfeld L, Rawkins S, Park J. Development of the C4 inventory: a measure of common characteristics that complicate care in outpatient psychiatry. J Comorbidity. (2016) 6:56–64. doi: 10.15256/joc.2016.6.66
12. Schilling C, Weidner K, Schellong J, Joraschky P, Pöhlmann K. Patterns of childhood abuse and neglect as predictors of treatment outcome in inpatient psychotherapy: a typological approach. Psychopathology. (2015) 48:91–100. doi: 10.1159/000368121
13. Bethell C, Jones J, Gombojav N, Linkenbach J, Sege R. Positive childhood experiences and adult mental and relational health in a statewide sample: Associations across adverse childhood experiences levels. JAMA pediatrics. (2019) 173:e193007. doi: 10.1001/jamapediatrics.2019.3007
14. Crandall A, Miller JR, Cheung A, Novilla LK, Glade R, Novilla MLB, et al. ACEs and counter-ACEs: How positive and negative childhood experiences influence adult health. Child Abuse neglect. (2019) 96:104089. doi: 10.1016/j.chiabu.2019.104089
15. Narayan AJ, Lieberman AF, Masten AS. Intergenerational transmission and prevention of adverse childhood experiences (ACEs). Clin Psychol Rev. (2021) 85:101997. doi: 10.1016/j.cpr.2021.101997
16. Qu G, Ma S, Liu H, Han T, Zhang H, Ding X, et al. Positive childhood experiences can moderate the impact of adverse childhood experiences on adolescent depression and anxiety: Results from a cross-sectional survey. Child Abuse Neglect. (2022) 125:105511. doi: 10.1016/j.chiabu.2022.105511
17. Wang D, Jiang Q, Yang Z, Choi J-K. The longitudinal influences of adverse childhood experiences and positive childhood experiences at family, school, and neighborhood on adolescent depression and anxiety. J Affect Disord. (2021) 292:542–51. doi: 10.1016/j.jad.2021.05.108
18. Brandes M, Bienvenu OJ. Personality and anxiety disorders. Curr Psychiatry Rep. (2006) 8:263–9. doi: 10.1007/s11920-006-0061-8
19. Friborg O, Martinussen M, Kaiser S, Øvergård KT, Rosenvinge JH. Comorbidity of personality disorders in anxiety disorders: A meta-analysis of 30 years of research. J Affect Disord. (2013) 145:143–55. doi: 10.1016/j.jad.2012.07.004
20. Gruber M, Doering S, Blüml V. Personality functioning in anxiety disorders. Curr Opin Psychiatry. (2020) 33:62–9. doi: 10.1097/YCO.0000000000000556
21. Doering S, Blüml V, Parth K, Feichtinger K, Gruber M, Aigner M, et al.Personality functioning in anxiety disorders. BMC Psychiatry. (2018) 18:1–9. doi: 10.1186/s12888-018-1870-0
22. Hörz S, Clarkin JF, Stern BL, Caligor E. The Structured Interview of Personality Organization (STIPO): An instrument to assess severity and change of personality pathology. In: Psychodynamic psychotherapy research: Evidence-based practice and practice-based evidence. Humana Totowa, NJ (2012). p. 571–92.
23. Kernberg OF, Caligor E. A psychoanalytic theory of personality disorders. In Lenzenweger M. F., Clarkin J. F. (Eds.) Major theories of personality disorders. (2005) 2:114–5. New York, London: The Guilford Press.
24. Force OT. Operationalized psychodynamic diagnosis OPD-2: Manual of diagnosis and treatment planning. Göttingen, Germany: Hogrefe Publishing (2008).
25. Zimmermann J, Ehrenthal JC, Cierpka M, Schauenburg H, Doering S, Benecke C. Assessing the level of structural integration using operationalized psychodynamic diagnosis (OPD): Implications for DSM–5. J Pers assessment. (2012) 94:522–32. doi: 10.1080/00223891.2012.700664
26. Nowak J, Nikendei C, Rollmann I, Orth M, Friederich H-C, Kindermann D. Characterization of different types of anxiety disorders in relation to structural integration of personality and adverse and protective childhood experiences in psychotherapy outpatients – a cross-sectional study. BMC Psychiatry. (2023) 23:501. doi: 10.1186/s12888-023-04988-2
27. Lindfors O, Knekt P, Lehtonen J, Virtala E, Maljanen T, Härkänen T. Effectiveness of psychoanalysis and long-term psychodynamic psychotherapy on personality and social functioning 10 years after start of treatment. Psychiatry Res. (2019) 272:774–83. doi: 10.1016/j.psychres.2018.12.082
28. Beutel M, Krakau L, Kaufhold J, Bahrke U, Grabhorn A, Hautzinger M, et al. Recovery from chronic depression and structural change: 5-year outcomes after psychoanalytic and cognitive-behavioural long-term treatments (LAC depression study). Clin Psychol Psychother. (2023) 30:188–201. doi: 10.1002/cpp.2793
29. Huber D, Zimmermann J, Klug G. Change in personality functioning during psychotherapy for depression predicts long-term outcome. Psychoanal Psychol. (2017) 34:434. doi: 10.1037/pap0000129
30. Falkenström F, Grant J, Broberg J, Sandell R. Self-analysis and post-termination improvement after psychoanalysis and long-term psychotherapy. J Am Psychoanal Assoc. (2007) 55:629–74. doi: 10.1177/00030651070550020401
31. Dagnino P, Ugarte MJ, Morales F, González S, Saralegui D, Ehrenthal JC. Risk factors for adult depression: Adverse childhood experiences and personality functioning. Front Psychol. (2020) 3224. doi: 10.3389/fpsyg.2020.594698
32. Ehrenthal, Dinger U, Horsch L, Komo-Lang M, Klinkerfuss M, Grande T, et al. The OPD Structure Questionnaire (OPD-SQ): first results on reliability and validity. Psychotherapie Psychosomatik Medizinische Psychologie. (2012) 62:25–32. doi: 10.1055/s-0031-1295481
33. Hovens JG, Giltay EJ, van Hemert AM, Penninx BW. Childhood maltreatment and the course of depressive and anxiety disorders: the contribution of personality characteristics. Depression anxiety. (2016) 33:27–34. doi: 10.1002/da.2016.33.issue-1
34. Rogosch FA, Cicchetti D. Child maltreatment and emergent personality organization: Perspectives from the five-factor model. J Abnormal Child Psychol. (2004) 32:123–45. doi: 10.1023/B:JACP.0000019766.47625.40
35. Spinhoven P, Elzinga BM, Van Hemert AM, de Rooij M, Penninx BW. Childhood maltreatment, maladaptive personality types and level and course of psychological distress: A six-year longitudinal study. J Affect Disord. (2016) 191:100–8. doi: 10.1016/j.jad.2015.11.036
36. Kerber A, Gewehr E, Zimmermann J, Sachser C, M. Fegert J, Knaevelsrud C, et al. Adverse childhood experiences and personality functioning interact substantially in predicting depression, anxiety, and somatization. Pers Ment Health. (2023) 17(3):246–58. doi: 10.1002/pmh.1578
37. Kindermann D, Rollmann I, Orth M, Friederich H-C, Nikendei C. Direct and indirect effects of adverse and protective childhood experiences on symptom improvement in psychotherapy. Psychother Res. (2023), 1–16. doi: 10.1080/10503307.2023.2254917
38. Schauenburg H, Dinger U, Kriebel A, Huber J, Friederich H-C, Herzog W, et al. Zur Entwicklung tiefenpsychologischer Ausbildungsinstitute. Das Beispiel des Heidelberger Instituts für Psychotherapie. Psychotherapeut. (2019) 64:46–54. doi: 10.1007/s00278-018-0320-2
39. Williams JR. The Declaration of Helsinki and public health. Bull World Health Organization. (2008) 86:650–2. doi: 10.2471/BLT.00.000000
40. First MB, Gibbon M. The structured clinical interview for DSM-IV axis I disorders (SCID-I) and the structured clinical interview for DSM-IV axis II disorders (SCID-II). In Hilsenroth M. J., Segal D. L. (Eds.), Comprehensive handbook of psychological assessment. John Wiley & Sons, Inc. (2004) 2:134–43.
41. Wittchen H, Zaudig M, Fydrich T. SKID-I und SKID-II. Strukturiertes klinisches interview für DSM-IV. (1997).
42. Derogatis LR, Cleary PA. Confirmation of the dimensional structure of the SCL-90: A study in construct validation. J Clin Psychol. (1977) 33:981–9. doi: 10.1002/(ISSN)1097-4679
43. Lutz W, Tholen S, Schürch E, Berking M. Reliabilität von Kurzformen gängiger psychometrischer Instrumente zur Evaluation des therapeutischen Fortschritts in Psychotherapie und Psychiatrie. Diagnostica. (2006) 52:11–25. doi: 10.1026/0012-1924.52.1.11
44. Cierpka M, Grande T, Rudolf G, Von Der Tann M, Stasch M. The operationalized psychodynamic diagnostics system: clinical relevance, reliability and validity. Psychopathology. (2007) 40:209–20. doi: 10.1159/000101363
45. Ehrenthal, Schauenburg H, Wagner FE, Dinger U, Volz M. [Development and evaluation of the questionnaire for the assessment of adverse and protective childhood experiences (APC)]. Psychiatr Prax. (2020) 47:207–13. doi: 10.1055/a-1123-1615
46. Jorgensen TD, Pornprasertmanit S, Schoemann AM, Rosseel Y. semTools: Usefull tools for structural equation modeling. R package version 0.5-6. (2022). 5–6. Available at: https://CRAN.R-project.org/package=semTools
47. Kline RB. Principles and practice of structural equation modeling. 4th ed. New York, London: The Guilford Press (2016).
48. R Core Team. A language and environment for statistical computing. R Foundation for Statistical Computing (2020). Available at: https://www.R-project.org/
49. van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Software. (2011) 45:1–67. doi: 10.18637/jss.v045.i03
50. Van Buuren SG-O. Mice: Multivariate imputation by chained equations in R. J Stat Software. (2011) 45(3):1–67. doi: 10.18637/jss.v045.i03
51. Daniels MJ, Hogan JW. Missing data in longitudinal studies: Strategies for Bayesian modeling and sensitivity analysis. New York: CRC press (2008). doi: 10.1201/9781420011180
52. José P, Douglas B, R Core Team. nlme: Linear and Nonlinear Mixed Effects Models. R package version 3 (2022). Available online at: https://CRAN.R-project.org/package=nlme.
53. Shaw M, Rights JD, Sterba SK, Flake JK. r2mlm: An R package calculating R-squared measures for multilevel models. Behav Res. (2023) 55:1942–64. doi: 10.3758/s13428-022-01841-4
54. Wasserman L. All of statistics : a concise course in statistical inference. New York; Berlin; Heidelberg: Springer (2007).
55. Döring N, Bortz J. Forschungsmethoden und Evaluation in den Sozial- und Humanwissenschaften. Berlin, Heidelberg: Springer Berlin Heidelberg (2016).
56. Rosseel Y. lavaan: an R package for structural equation modeling. J Stat Software. (2012) 48:1–36. doi: 10.18637/jss.v048.i02
57. Appelbaum M, Cooper H, Kline RB, Mayo-Wilson E, Nezu AM, Rao SM. Journal article reporting standards for quantitative research in psychology: The APA Publications and Communications Board task force report. Am Psychol. (2018) 73:3. doi: 10.1037/amp0000191
58. Association AP. Quantitative research design (JARS– Quant) (2018). Available online at: https://apastyle.apa.org/jars/quantitative.
59. Comninos A, Grenyer BFS. The influence of interpersonal factors on the speed of recovery from major depression. Psychother Res. (2007) 17:230–9. doi: 10.1080/10503300600849140
60. Kathmann N, Jacobi T, Elsner B, Reuter B. Effectiveness of individual cognitive-behavioral therapy and predictors of outcome in adult patients with obsessive-compulsive disorder. Psychother Psychosomatics. (2022) 91:123–35. doi: 10.1159/000520454
61. Jakubovski E, Bloch MH. Anxiety disorder-specific predictors of treatment outcome in the coordinated anxiety learning and management (CALM) trial. Psychiatr Quarterly. (2016) 87:445–64. doi: 10.1007/s11126-015-9399-6
62. Wolitzky-Taylor KB, Arch JJ, Rosenfield D, Craske MG. Moderators and non-specific predictors of treatment outcome for anxiety disorders: a comparison of cognitive behavioral therapy to acceptance and commitment therapy. J Consulting Clin Psychol. (2012) 80:786. doi: 10.1037/a0029418
63. Giampetruzzi E, Tan AC, LoPilato A, Kitay B, Posse PR, McDonald WM, et al. The impact of adverse childhood experiences on adult depression severity and treatment outcomes. J Affect Disord. (2023) 333:233–9. doi: 10.1016/j.jad.2023.04.071
64. Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. Am J Psychiatry. (2012) 169:141–51. doi: 10.1176/appi.ajp.2011.11020335
65. Arntz A, Stupar-Rutenfrans S, Bloo J, van Dyck R, Spinhoven P. Prediction of treatment discontinuation and recovery from borderline personality disorder: results from an RCT comparing schema therapy and transference focused psychotherapy. Behav Res Ther. (2015) 74:60–71. doi: 10.1016/j.brat.2015.09.002
66. Ford JD, Hawke J, Alessi S, Ledgerwood D, Petry N. Psychological trauma and PTSD symptoms as predictors of substance dependence treatment outcomes. Behav Res Ther. (2007) 45:2417–31. doi: 10.1016/j.brat.2007.04.001
67. Miniati M, Rucci P, Benvenuti A, Frank E, Buttenfield J, Giorgi G, et al. Clinical characteristics and treatment outcome of depression in patients with and without a history of emotional and physical abuse. J Psychiatr Res. (2010) 44:302–9. doi: 10.1016/j.jpsychires.2009.09.008
68. Vermetten E, Spiegel D. Trauma and dissociation: implications for borderline personality disorder. Curr Psychiatry Rep. (2014) 16:1–10. doi: 10.1007/s11920-013-0434-8
69. Bifulco A, Kwon J, Jacobs C, Moran PM, Bunn A, Beer N. Adult attachment style as mediator between childhood neglect/abuse and adult depression and anxiety. Soc Psychiatry Psychiatr Epidemiol. (2006) 41:796–805. doi: 10.1007/s00127-006-0101-z
70. Bifulco A, Moran P, Ball C, Bernazzani O. Adult attachment style. I: Its relationship to clinical depression. Soc Psychiatry Psychiatr Epidemiol. (2002) 37:50–9. doi: 10.1007/s127-002-8215-0
71. Cooke JE, Racine N, Plamondon A, Tough S, Madigan S. Maternal adverse childhood experiences, attachment style, and mental health: pathways of transmission to child behavior problems. Child Abuse neglect. (2019) 93:27–37. doi: 10.1016/j.chiabu.2019.04.011
72. McCarthy G, Taylor A. Avoidant/ambivalent attachment style as a mediator between abusive childhood experiences and adult relationship difficulties. J Child Psychol Psychiatry. (1999) 40:465–77. doi: 10.1017/S0021963098003734
73. Sitko K, Bentall RP, Shevlin M, Sellwood W. Associations between specific psychotic symptoms and specific childhood adversities are mediated by attachment styles: an analysis of the National Comorbidity Survey. Psychiatry Res. (2014) 217:202–9. doi: 10.1016/j.psychres.2014.03.019
74. Kremers I, Van Giezen A, van der Does A, Van Dyck R, Spinhoven P. Memory of childhood trauma before and after long-term psychological treatment of borderline personality disorder. J Behav Ther Exp Psychiatry. (2007) 38:1–10. doi: 10.1016/j.jbtep.2005.12.003
75. Ernst M, Beutel ME, Zwerenz R, Krakau L. Seeing the past in a new light: change in reports of childhood abuse and neglect before and after inpatient psychotherapy and its relevance for change in depression symptoms. Psychother Res. (2023) 33:222–34. doi: 10.1080/10503307.2022.2088313
76. Paivio SC. Stability of retrospective self-reports of child abuse and neglect before and after therapy for child abuse issues☆. Child Abuse neglect. (2001) 25:1053–68. doi: 10.1016/S0145-2134(01)00256-3
77. Frampton NM, Poole JC, Dobson KS, Pusch D. The effects of adult depression on the recollection of adverse childhood experiences. Child Abuse Neglect. (2018) 86:45–54. doi: 10.1016/j.chiabu.2018.09.006
78. Bienvenu OJ, Stein MB. Personality and anxiety disorders: a review. J Pers Disord. (2003) 17:139–51. doi: 10.1521/pedi.17.2.139.23991
79. Skodol AE, Geier T, Grant BF, Hasin DS. Personality disorders and the persistence of anxiety disorders in a nationally representative sample. Depression Anxiety. (2014) 31:721–8. doi: 10.1002/da.2014.31.issue-9
80. Schaefer LM, Howell KH, Schwartz LE, Bottomley JS, Crossnine CB. A concurrent examination of protective factors associated with resilience and posttraumatic growth following childhood victimization. Child Abuse Neglect. (2018) 85:17–27. doi: 10.1016/j.chiabu.2018.08.019
81. Tedeschi RG, Calhoun LG. " Posttraumatic growth: Conceptual foundations and empirical evidence". psychol inquiry. (2004) 15:1–18. doi: 10.1207/s15327965pli1501_01
82. Sheridan G, Carr A. Survivors’ lived experiences of posttraumatic growth after institutional childhood abuse: An interpretative phenomenological analysis. Child Abuse neglect. (2020) 103:104430. doi: 10.1016/j.chiabu.2020.104430
83. Brooks M, Graham-Kevan N, Robinson S, Lowe M. Trauma characteristics and posttraumatic growth: The mediating role of avoidance coping, intrusive thoughts, and social support. psychol Trauma: Theory Research Practice Policy. (2019) 11:232. doi: 10.1037/tra0000372
Keywords: adverse childhood experiences, protective childhood experiences, anxiety disorders, personality functioning, psychotherapy, recovery
Citation: Nowak J, Nikendei C, Rollmann I, Orth M, Friederich H-C and Kindermann D (2024) Examining childhood experiences and personality functioning as potential predictors for the speed of recovery during psychotherapy of patients with anxiety disorders. Front. Psychiatry 15:1381105. doi: 10.3389/fpsyt.2024.1381105
Received: 02 February 2024; Accepted: 16 April 2024;
Published: 09 May 2024.
Edited by:
Katrin Giel, Tübingen University Hospital, GermanyReviewed by:
Edwin de Beurs, Leiden University, NetherlandsCopyright © 2024 Nowak, Nikendei, Rollmann, Orth, Friederich and Kindermann. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jonathan Nowak, jonathan.nowak@med.uni-heidelberg.de
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.