- 1Department of Psychosomatic Medicine and Psychotherapy, University Hospital Tübingen, Tübingen, Germany
- 2Department for Psychosomatic Medicine, Charité Center for Internal Medicine and Dermatology, Charité-Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin, Humboldt-Universität zu Berlin and Berlin Institute of Health, Berlin, Germany
- 3German Center for Mental Health (DZPG), Tübingen, Germany
- 4Department of Sports Medicine, University Hospital Tübingen, Tübingen, Germany
Introduction: COVID-19 affected global physical and psychological health. The purpose of this study was to explore the pandemics impact on health-related quality of life (HRQoL), mental health (anxiety, depression, and perceived stress) and eating behavior in people with severe obesity participating in a multimodal conservative behavioral weight loss (BWL) program conducted via videoconferencing. Additionally, the efficacy of the six-month BWL program in a virtual video-based setting during the pandemic was examined.
Methods: 297 participants of a face-to-face multimodal behavioral weight loss program prior to the pandemic (PrePAN, May 2014–September 2019) and 146 participants of the in terms of content same intervention in a videoconference-based setting during the pandemic (PAN, July 2020–April 2022) were questioned and compared using standardized questionnaires for HRQoL, symptoms of depressive and anxiety disorders, perceived stress, and eating behavior at baseline and at the end of treatment.
Results: Symptoms for anxiety, depression and perceived stress were similar between PrePAN and PAN at baseline. In addition, PAN tended to show lower disinhibition of eating behavior and feelings of hunger than PrePAN. During the pandemic, the BWL intervention resulted in body weight loss (67%) or stabilization (16%) in most of the participants. It also contributed by improving physical HRQoL, lower worries, and improved eating behaviors compared to baseline.
Conclusion: During the COVID-19 pandemic, baseline mental health of people with morbid obesity was not worse than before the pandemic. Additionally, the BWL intervention in the virtual video-based setting stabilized and improved physical and mental health during the COVID-19 pandemic.
1 Introduction
In December 2019, SARS-CoV-2 (Severe acute respiratory syndrome coronavirus type 2) broke out in the Chinese city of Wuhan and spread around the world within weeks. Almost three years after the coronavirus disease-19 (COVID-19) caused by SARS-CoV-2 was declared a global pandemic by the World Health Organization (WHO) (1), nearly all measures to combat the pandemic were dropped in Germany. Between these three years (March 2020 to March 2023), to contain the spread of the virus and thus combat the pandemic, various measures and decrees were enacted of the German government. All involved contact restrictions and severe adjustments to everyday life. Examples include the prohibition of public events as well as bans on the practice of team sports and closure of all sports facilities, new situations in the workplace, and even complete closures of kindergartens and schools (2). Despite the more or less dramatic measures taken by the authorities of the different countries, more than 767 million people were infected by SARS-CoV-2 and nearly seven million deaths were dated due to SARS-CoV-2 worldwide in August 2023 (3).
A global health challenge existing significantly longer than the COVID-19 pandemic is obesity, a pathological increase in body fat mass that is associated with many comorbidities and health risk (4). To prevent a further increase and reduce the current obesity prevalence, prevention and treatment strategies are of great importance. Obesity treatment is mainly achieved through conservative weight-management programs, pharmacotherapy and/or bariatric surgery. Conservative programs are generally multimodal and consist of the fields nutrition, behaviour, and physical activity (5).
Both, obesity and the COVID-19 pandemic are/were associated with stress, impaired HRQoL symptoms of depression, anxiety, and poorly modified eating behaviours (6–17). When both exposures met, severe mutual reinforcement occurred (18–22). For example, obesity was identified as a risk factor for a severe COVID-19 course (23–27) but it appeared to be known only among professionals (28). Infected people with obesity had a 39% increased likelihood of hospitalization (23, 29), increased stays at the Intensive Care Unit (25, 30), higher ventilation rates (26), and an increased mortality (24, 27, 30) as a result of COVID-19 infection. However, not only obesity represented a risk factor for a severe COVID-19 course, but the SARS-CoV-2 outbreak also appeared to be associated with an exacerbation of the obesity epidemic. In particular, an increase in weight during the COVID-19 pandemic was especially found in those individuals who were overweight (BMI 25.0–29.9 kg/m2) or obese (BMI ≥ 30.0 kg/m2) (18–21). For example, according to the German Health Update (GEDA 2021), more than one in four people living in Germany reported weight gain since the beginning of the corona pandemic (31). People with a higher BMI were more likely to gain weight than those with a BMI within the normal weight range (31). The same results were provided by other European studies and the US (18–20). Conversely, telemedicine dietary intervention during a pandemic could mitigate the negative changes in dietary habits and physical activity that lead to weight gain and thus prevent weight gain during a lockdown (32).
The COVID-19 pandemic has continued to drive technological advances in health care (33). This has enabled the care of patients over a geographical distance, known as “eHealth” or “telemedicine.” Telemedicine online weight loss interventions can be similarly effective as face-to-face BWL programs (34–38), also in older adults in rural areas (39) and as well as during the COVID-19 pandemic (40–43). Furthermore, telemedical interventions can lead to a better physical and psychological wellbeing of people suffering from obesity (44–46).
The purpose of this exploratory study was to examine the impact of the COVID-19 pandemic on mental health and eating behaviours among people with severe obesity attending an online multimodal conservative BWL program.
We hypothesised that (i) individuals with severe obesity were psychologically more distressed and had worse eating behaviour during the COVID-19 pandemic than prior to the pandemic at baseline; (ii) face-to-face BWL intervention during the COVID-19 pandemic lead to physical stabilization and improvement in eating behaviour and psychological parameters.
2 Materials and methods
2.1 Study design and participants
For this explorative study participants of the VIADUKT program, a multimodal BWL treatment at the University Hospital in Tübingen, Germany, were investigated. The study was approved by the Ethics Committee of the University Hospital Tübingen, Germany with the number 391/2019BO2.
German speaking adults living with obesity were recruited via the multidisciplinary obesity service of the University Hospital in Tübingen and through local general practitioners or specialists. Furthermore, leaflets were distributed among practitioners in and around Tübingen, and the website of the University Hospital was used for recruitment.
To uncover differences in baseline characterization of participants prior to and during the COVID-19 pandemic (i), the baseline characteristics of two groups within VIADUKT were investigated. Group 1, named “PrePAN,” consists of 297 subjects who participated in the VIADUKT program prior to the COVID-19 pandemic (from May 2014 until September 2019, face-to-face), being characterized previously (47). Group 2, “PAN” includes 146 subjects which participated in the program during the COVID-19 pandemic (from July 2020 until April 2022, virtual, video-based). To create a clear distinction between the pandemic period and the pre-pandemic period, participants from courses that started prior to the COVID-19 pandemic but were completed during the pandemic were excluded from the analyses.
To test the effectiveness of the BWL program during the COVID-19 pandemic (ii), all participants of PAN were analysed regarding subjectively measured body weight, body height, HRQoL, anxiety, depression, distress, and eating behaviour between pre- (T0, two weeks prior to the intervention) and posttreatment (T1, one week before the intervention ended). Due to less stringent lockdown policies in the summer months of 2020 and 2021, single units may have been conducted face-to-face and not online. As we did not find any differences between courses with at least 80% online sessions and online-only courses, all these online courses were included in this analysis. Furthermore, a subgroup analysis was performed according to the attitude towards bariatric surgery since this is an important factor for conservative treatment success (47). This attitude was recorded in the questionnaire at the beginning of the intervention. Participants who considering bariatric surgery at T0 were assigned to PANPOS (n = 90). Those who excluded bariatric surgery at T0 were named PANNEG (n = 53). Participants with an uncertain attitude (PANUncert, n = 3) were not included in subgroup analyses.
Due to the heterogeneous conditions between online and face-to-face courses (online courses during COVID-19 pandemic, face-to-face courses before COVID-19 pandemic), no direct comparisons were made between PrePAN and PAN.
2.2 Treatment (VIADUKT)
“VIADUKT” is a multimodal conventional BWL program for patients with predominantly severe obesity (grade III, mean BMI = 42.7 kg/m2). The program includes theory sessions as well as practical exercise sessions conducted by a multidisciplinary team consisting of nutritional, psychological and sports medicine specialists. The theory sessions focus on nutritional education and behavioural therapy to promote lifestyle change. Specifically, participants are trained on motivational enhancement, flexible but controlled eating behaviours, basics of physical activity, stress management techniques, and strategies for permanent weight loss. The program meets the requirements of the German guideline for the clinical treatment of obesity (48).
The intervention takes place at two-week intervals over a period of six months. Due to the COVID-19 pandemic, the group sessions originally held face-to-face at the hospital were moved to a synchronous virtual, video-based privacy-compliant online platform. Prior to the pandemic, twelve participants attended ten 75-min educational group sessions and twenty 45-min guided exercise sessions. As a result of the pandemic-related shift to video-based training, these ten educational theory sessions were reduced to 60 min per session but not including not more than six participants. Additional, material and homework were provided one week ahead of each theory online class via e-mail. Practical sessions were transformed to ten 60-min sessions. If participants attended at least 80% of the group sessions and physical activity meetings, the program was considered complete, otherwise a dropout was declared.
2.3 Outcomes
For PrePAN, the outcomes are reported in details elsewhere (47). Except of body weight assessment, measurements for the PrePAN and the PAN sample were identical. Body weight of the PrePAN individuals was assessed at site, using a calibrated scale, wearing only light clothes and no shoes. Body height and body weight of the PAN-individuals was self-reported. The participants used their own body scales at home. Although subjectively measured body weight is never as accurate as objectively measured body weight, especially in people living with obesity (49), there are also studies showing that self-reported body weight is precise, even in people living with obesity (50) and especially for people living with obesity who participate a weight loss program (51).
Body weight change in kilograms over the six-month intervention period was calculated for PAN. As reported before, all body weight and height values are self-reported by the participants. The BMI of the participants was calculated from the information of height and subjectively measured body weight.
Validated questionnaires were used for HRQoL (SF-12), anxiety (GAD-7), depression (PHQ-9), distress (PSQ20), and eating behaviour (TFEQ) at T0 and T1. The applied questionnaires are described in detail below. For the subgroup analyses, the participant’s attitudes towards bariatric surgery were assessed with an open question called “What is your attitude towards bariatric surgery?.” The answers were categorized into: “Yes, bariatric surgery is an option for me” (PANPOS), “No, bariatric surgery is not an option for me” (PANNEG), “I am not sure” (PANUncert). The results are presented for the total PAN group and for the two subgroups PANPOS versus PANNEG, but not for the PANUncert.
The Short Form Health-Survey 12 (SF-12) is used to assess HRQoL, consisting of 12 items of mental and physical component summaries. The average score is 50 (SD = 10) for each. Higher scores represent better health status, whereas lower scores represent poorer referred to the general U.S. population (52).
For screening generalized anxiety disorder, the Generalized Anxiety Disorder Scale (GAD-7) is used. Patients rate the 7 items of GAD-7 with the options “not at all,” “on some days,” “on more than half of the days” and “almost every day.” Scores range between 0–21 and were categorized into minimal (0–4), mild (5-9), moderate (10-14) or severe (15-21) anxiety (53).
The occurrence and severity of depressive disorder is assessed using the 9-item Patient Health Questionnaire (PHQ-9). Possible answer options are “not at all,” “several days,” “more than half of the days” or “nearly every day.” The calculated score is categorized into none to minimal (0–4), mild (5-9), moderate (10-14), moderately severe (15-19) or severe (20-27) levels of depression (54).
Perceived stress is measured by the German version of the Perceived Stress Questionnaire-20 (PSQ20). It consists of 20 items, which are divided into four subscales and represent the distress-determining constructs “worry,” “tension,” “pleasure,” and “demands.” In addition, a sum score is calculated. All statements are to be answered on a 4-point-Likert-scale ranging from “almost never,” “sometimes,” “frequently” to “most of the time.” The result is a scale rank between 0 and 100 with high values on a subscale meant to be a high expression of the respective construct (55).
The German version of the Three-Factor Eating Questionnaire (TFEQ), which contains 51 items of 3 subscales “Cognitive Restraint,” “Disinhibition,” and “Feelings of Hunger,” efforts on eating behaviour. High scores at the subscales represent high expressions of the constructs (56).
These questionnaires have been used and validated in patients with obesity [HRQoL (57, 58), anxiety and depression (59, 60), perceived stress (55, 61) and eating behaviour (62–64)].
Additionally, at the end of the intervention the participants completed an evaluation questionnaire that captured participant satisfaction with the program in 10 questions regarding personal benefits, importance and usefulness of the sessions, adequacy of the exercise level, motivation to implement more exercise into daily life, whether participants felt prepared for the time after the program and optimism to maintain or further reduce the weight. Participants responded to the questions using a 5-point Likert scale from “strongly disagree” (1),” disagree” (2), “neither agree nor disagree” (3), “agree” (4) to “strongly agree” (5). Additionally, participants were asked if they would recommend the program to family and friends.
2.4 Statistical analysis
Statistical analysis was performed using IBM SPSS Statisics for Windows software, version 28.0 (65). Data are reported as mean (standard deviation, SD), confidence interval (CI) along with median with 25th and 75th percentiles (interquartile range, IQR). Frequencies are expressed as percentages (%). Normal distribution was tested using Kolmogorov–Smirnov tests, and equality of variances between groups was tested using Levene’s tests.
To explore the first hypothesis (i), differences in baseline-characterization between the two groups of the total sample (PrePAN and PAN) were detected with metric data and simultaneous normal distribution using the t-test. Non-normally distributed data were determined with the Mann–Whitney U test. For nominal data, the χ2-test or, if the expected frequencies of the cells were too low, the Fisher–Freeman–Halton’s exact test was used. In addition, to detect possible differences due to unequal group sizes, cases of PrePAN were matched with cases of PAN according to age, sex, BMI, and attitude toward bariatric surgery (hereafter referred to as PrePANMatch and PANMatch).
To test for the second hypothesis (ii), differences in self-reported body weight, HRQoL, anxiety, depression, perceived stress, and eating behaviors between beginning of the intervention (T0) and the end (T1) for the whole PAN group (PANNEG, PANPOS and PANUncert) were analysed using the Wilcoxon signed-rank test. To analyse subgroup (PANNEG vs. PANPOS) and time (T0 vs. T1) interactions in body weight, BMI, and psychometrics, a 2×2 ANOVA was performed with main effects for time as a within-subjects variable and subgroup as a between-subjects variable. Body weight reductions of ≥5% of baseline weight are considered clinically significant body weight reductions (5, 66). Body weight reductions up to 4.9% of baseline weight are considered low, from 5.0%–9.9% are considered moderate, and >10% are considered high body weight reductions (47). Weight gain <2 kg are considered weight stabilization (20, 67). Two-tailed tests are used throughout the outcome calculation.
To control for α-error, p-values of psychological outcomes were adjusted for the false discovery rate (FDR) in multiple testing (68). FDR values <0.001 were considered statistically highly significant. FDR values between 0.001 and 0.05 were considered statistically significant. FDR values between 0.05 and 0.1 were assessed as a trend. For age, baseline body weight, and baseline BMI, as well as for demographics at baseline and for the body weight change, p-values were reported because they were not affected by multiple testing. p-values <0.001 were considered statistically significant. p-values between 0.001 and 0.05 were considered a trend. Effect sizes for the χ2 -test and Mann–Whitney U test are defined as follows: r-(φ-) of 0.1 = low effect, 0.3 = medium effect, 0.5 = high effect (69).
2.5 Missing data imputation
Missing Data were replaced by the predictive mean-matching method after using Little’s test to determine whether missing data were random (70).
For the per protocol population, participants were only included if body weight (kg) was provided at T0 and T1 of intervention, and if they were not classified as dropout (≥80% exposure). After excluding the participants with missing data at T0 (n = 8) and/or the non-completer (n = 13), the per protocol population consisted of 132 participants,
The intention-to-treat population consisted of 146 participants for the body weight change and 138 for the psychological parameters (due to n = 8 for missing questionnaire data at T0). Age, sex, and self-reported body weight at baseline were chosen as predictors for the body weight change. For the psychological parameters, age and sex served as predictors. To fill in gaps in the assessment of HRQoL, depressive and anxiety disorders, stress, and eating behaviours, multiple imputation with five iterations was performed both for single missing values (at intervention beginning and end) and for completely missing questionnaires (at the end of intervention only) (71, 72). Cases with complete missing questionnaires and/or single-item at the end imputations were included in the intention-to-treat (ITT) population. The data were analysed for the per protocol population and for the full-data analysis. Since no differences between the approaches were found, the results of the full-data analysis are presented.
The percentage of missing data for complete questionnaires ranged from 5% to 30% [T0 HRQoL = 6.2% (n = 10), T1 HRQoL = 30.1% (n = 44), T0 anxiety = 7.5% (n = 11), T1 anxiety = 30.1% (n = 44), T0 depression = 7.5% (n = 11), T1 depression = 30.1% (n = 44), T0 eating behaviour = 5.5% (n = 8), T1 eating behaviour = 30.1% (n = 44), T0 stress = 5.5% (n = 8), T1 stress = 30.1% (n = 44)].
2.6 Further analyses
Minimal clinically important differences (MCIDs) were reported when possible. For anxiety and depression, MCIDs were set to a value of four points (53, 72). For HRQoL, a score of three points was assumed to be the minimum clinically relevant change (71). Furthermore, scores for generalized anxiety disorder and for depressive disorder as well as for eating behaviours were divided into subgroups according to the manuals (depression: 0–4 minimal, 5–9 mild, 10–14 moderate, 15–21 severe depression; anxiety: 0–4 minimal, 5–9 mild, 10–14 moderate, 15–21 severe anxiety; TFEQ subscale 1: 0–3 very low, 4–6 low, 7–9 moderate, 10–13 high, 14–21 very high Cognitive Restraint; TFEQ subscale 2: 0–3 very low, 4–5 low, 6–8 moderate, 9–11 high, 11–16 very high Disinhibition; TFEQ subscale 3: 0–2 very low, 3–4 low, 5–6 moderate, 7–9 high, 10–14 very high Feelings of hunger). The percentages of participants who attained MCIDs or achieved a change in class on TFEQ (improvement or worsening) or remained the same in their class are reported.
3 Results
3.1 Group characteristics
A total of 443 participants with predominantly (65%) grade III obesity who participated in the VIADUKT program since May 2014 until April 2022 were included. Most participants (77%) were women with a mean age of 42.2 years (SD = 12.4) and a mean BMI of 42.7 kg/m2 (SD = 5.4). In the following, the participants of the total sample are divided into two groups, PrePAN and PAN.
The PrePAN group has been described in detail elsewhere (47). In short, prior to the COVID-19 pandemic, 297 probands participated in the face-to-face VIADUKT program (PrePAN). Almost all (92%) participants completed the intervention. The drop-out rate was 8%. The group consisted predominantly of women (76%) and two third of the patients had grade III obesity (65%). 38% had a negative attitude towards bariatric surgery (PrePANNEG), whereas 37% had a positive (PrePANPOS). 10% were undecided (PrePANUncert) and 15% did not provide any information on their attitude.
The PAN group consists of 146 subjects who participated in the VIADUKT program in a virtual, video-based setting during the COVID-19 pandemic, from July 2020 until April 2022. Out of these, 12 subjects attended less than 80% of the meetings, so the dropout rate was 8%. The majority (80%) of the participants were women and had obesity grade III (63%). More than half (62%) of the participants declared to not desire bariatric surgery (PANNEG), whereas 53 (36%) participants wanted to receive bariatric surgery (PANPOS). Only three (2%) participants were undecided (PANUncert).
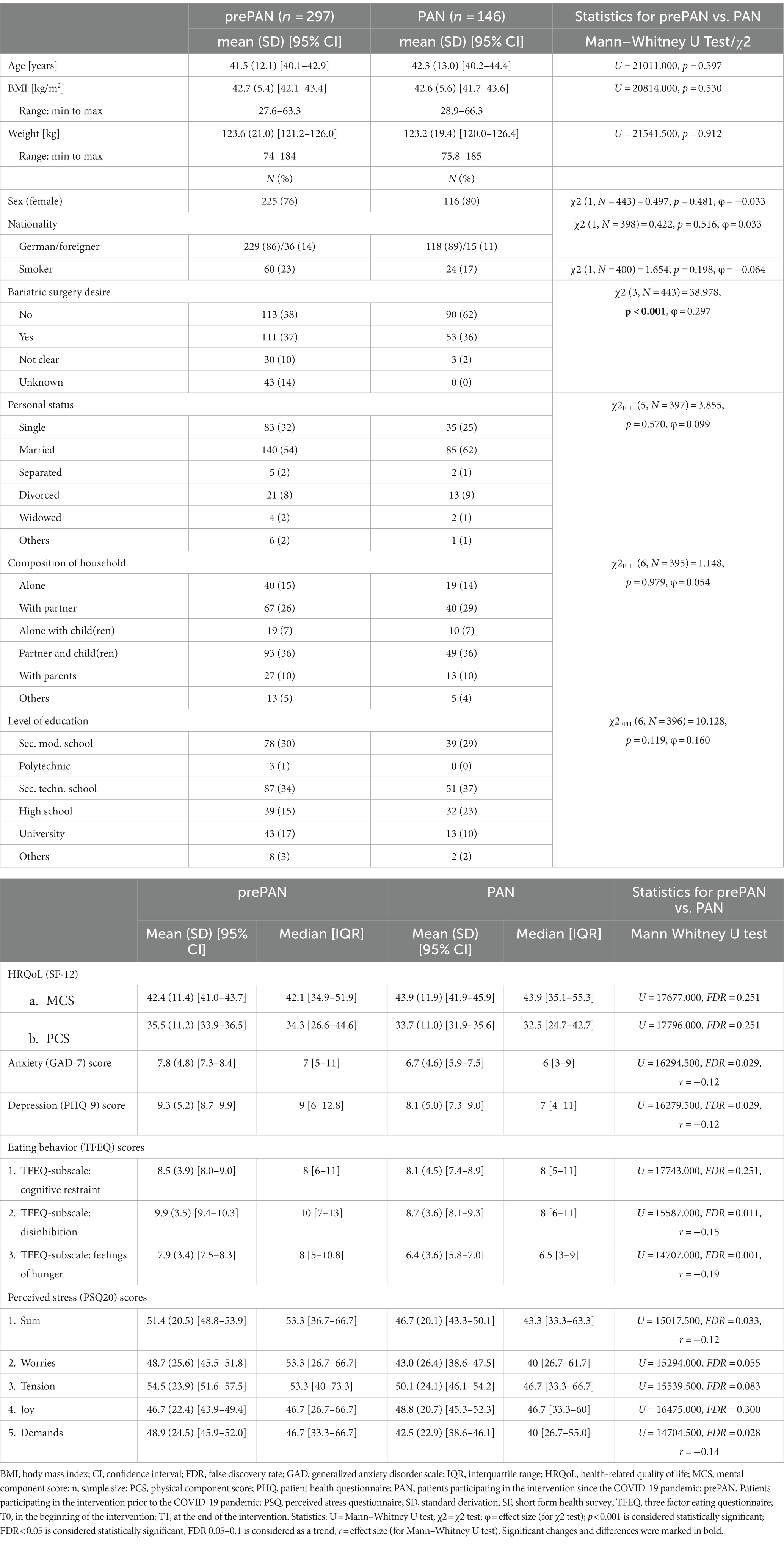
3.2 People with severe obesity were psychologically not more distressed or had worse eating behaviour during the COVID-19 pandemic than prior to the pandemic at baseline
PrePAN and PAN did not differ significantly from each other with respect to age, initial weight, and BMI as well as in sociodemographic data (p > 0.05). Furthermore, there was no significant difference in HRQoL (FDR >0.1). In contrast, PAN showed significantly lower scores for anxiety and depression, as well as stress, disinhibition of eating behaviour and feelings of hunger (FDR <0.05). A detailed overview of the baseline characteristics for PrePAN and PAN is presented in Table 1. Since the PrePAN group was almost twice as large as the PAN group, matched population analyses were also performed. Detailed baseline characterization for the two sample groups matched by age, sex, initial BMI, and attitude towards bariatric surgery are shown in Supplementary material S1. PrePANMatch and PANMatch did not differ significantly in sociodemographic data (p > 0.05). In contrast to the full population analysis (PrePAN versus PAN), there were no differences in HRQoL, anxiety, depression, and perceived stress between PrePANMatch and PANMatch (FDR >0.1). However, in line with PrePAN and PAN, in the matched population PANMatch participants tended to have lower scores in the subscales Disinhibition and Feelings of Hunger of the TFEQ.
3.3 Effectiveness of the intervention during the COVID-19 pandemic
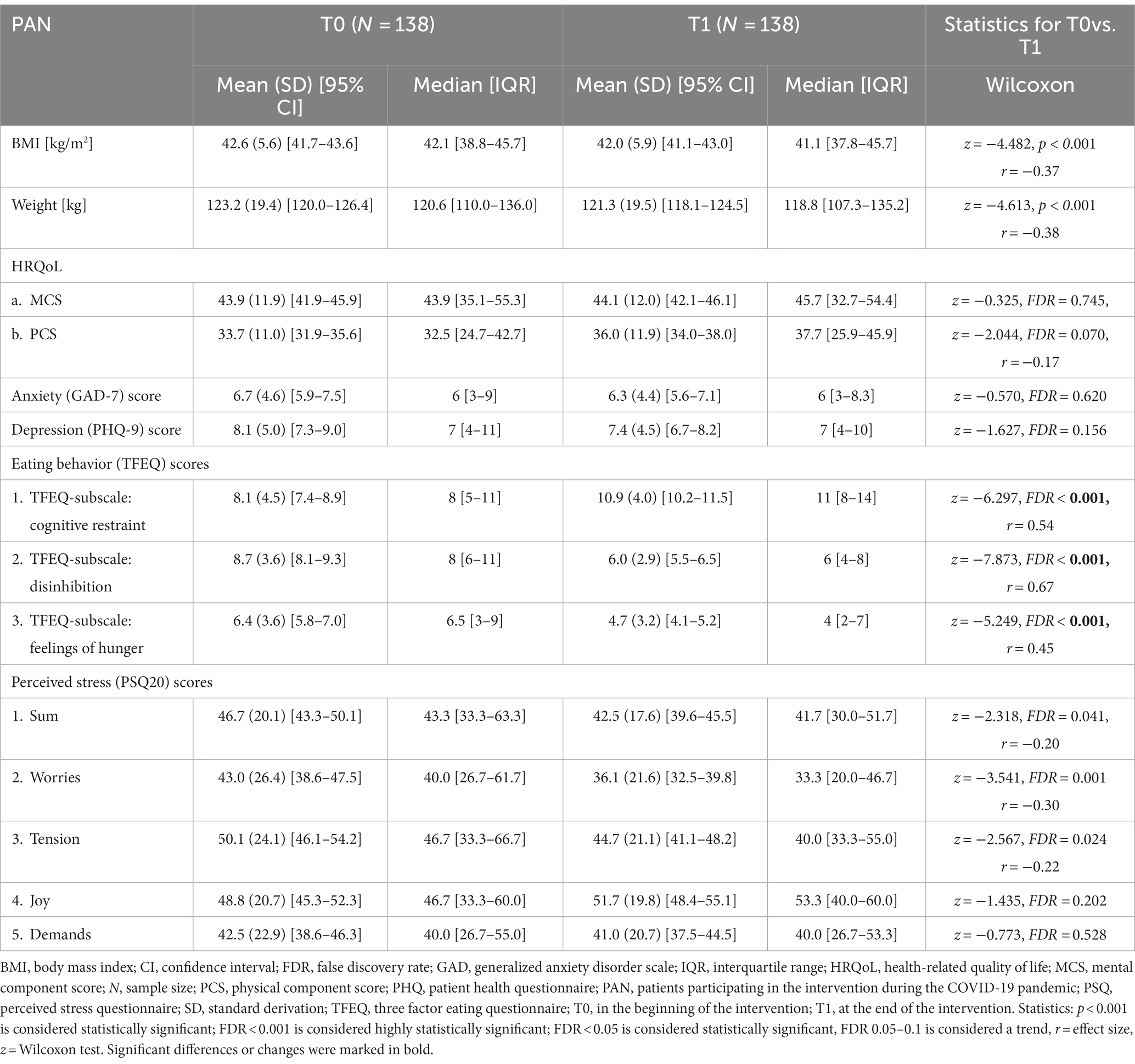
3.3.1 Patients’ physical situation and health related quality of life was stabilized in most participants
A detailed overview of the body weight change data is presented in Supplementary material S2. In the per protocol population the mean percentage reduction of subjectively measured body weight for PAN was 1.5%. This equates to a mean body weight change of −1.9 kg (SD = 5.5), ranging from −25.3 kg to +11.9 kg (z = −4.148, p < 0.001, n = 132, r = −0.36). Since the treatment efficacy differs in people with positive versus negative attitude towards bariatric surgery at the beginning of the treatment (47), the results are also reported for these subgroups. PANNEG refers to the group with a negative attitude towards bariatric surgery and PANPOS to the group with a positive attitude. Mean percentage reduction of subjectively measured body weight was 2.3% for PANNEG and 0.04% for PANPOS, equating to a mean body weight change of −2.8 kg (SD = 4.7) and −0.1 kg (SD = 6.3), respectively (F(1,129) = 7.852, p = 0.006, partial η2 = 0.1). In the intention-to-treat population the mean percentage reduction of subjectively measured body weight was 1.5%, which equates to a mean body weight change of −1.9 kg (SD = 5.2; z = −4.613, p < 0.001, n = 146, r = −0.38). In comparison, the mean percentage reduction of subjectively measured body weight was 2.2% for the PANNEG (n = 90) and 0.2% for the PANPOS (n = 53), equating to a mean body weight change of −2.7 kg (SD = 4.5) and −0.3 kg (SD = 6.1), respectively (F(1,143) = 7.496, p = 0.007, partial η2 = 0.1).
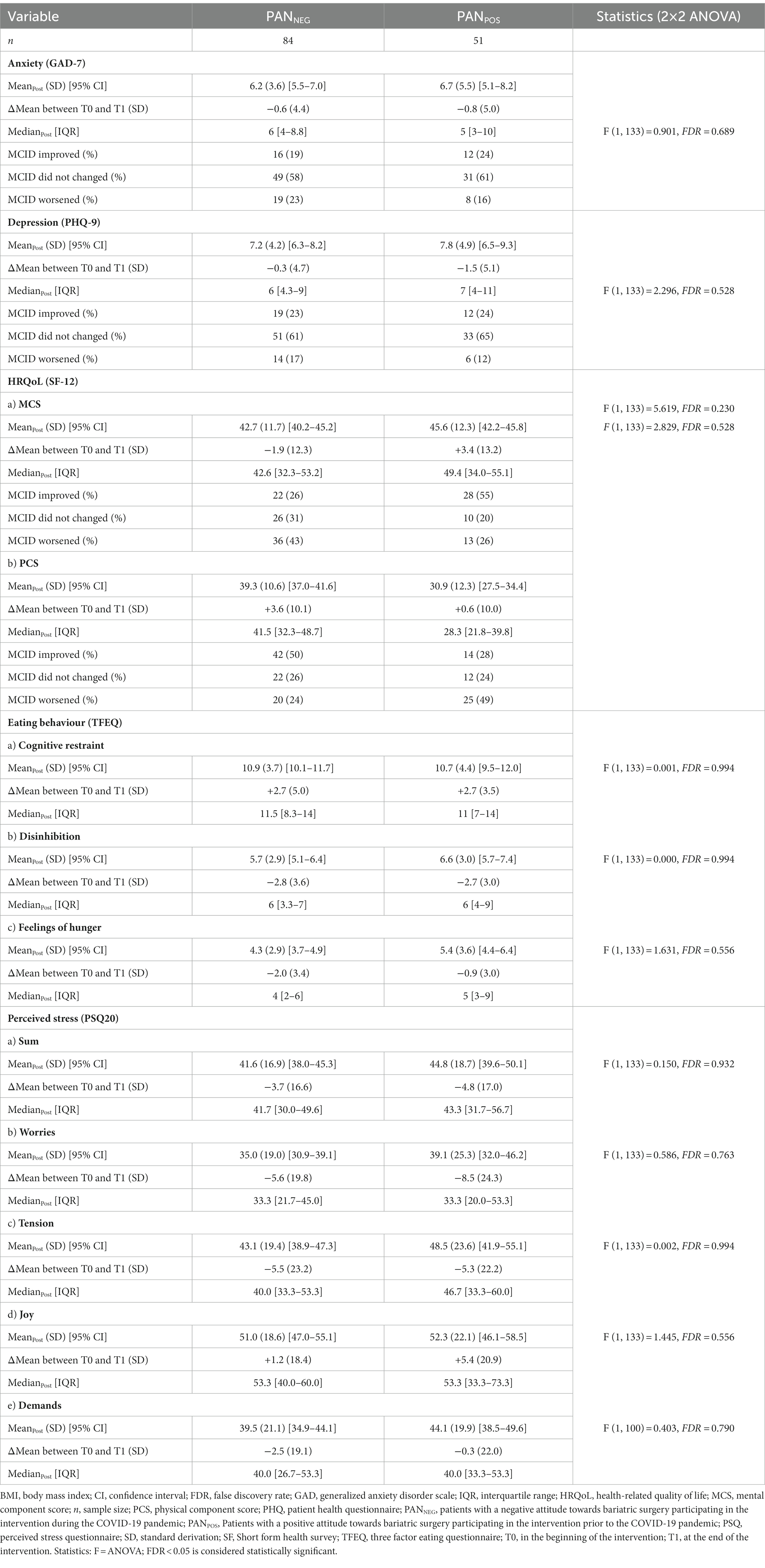
In line, the physical component summary of the HRQoL questionnaire (SF-12) tended to be improved (Table 2) whereas the mental component summary remained stable. For PANPOS, the mental component summary improved over the course of time, while PANNEG showed significant improvements for the physical component summary (Table 3).
Categorized according to MCIDs of the PAN group, the physical score improved in 41%, worsened in 34% and remained stable in 25% of the patients; the mental score improved in 37%, worsened in 36% and remained stable in 27% of the participants.
3.3.2 Stress perception and eating behaviour improved while depression and anxiety symptoms remained stable
The sum score for perceived stress improved significantly during the intervention period (Table 2). Additionally, the subscale “worries” and “tension” improved significantly from pre- to post-treatment. PANNEG showed significant improvements for “worries” subscale, and they tended to show improved scores for subscale “tension” (Table 3). In contrast, PANPOS tended to show lower scores for the subscale “worries.”
Anxiety and depression symptoms did not differ from T0 to T1, neither for the whole PAN, nor for the subgroups PANNEG and PANPOS (Tables 2, 3). For the whole PAN, the MCIDs for anxiety improved in 20%, worsened in 20% and remained stable in 60% of the patients. For depression, the MCIDs improved in 23%, worsened in 15% and remained stable in 63% of the patients.
For the whole PAN, all subscales of the eating behaviour questionnaire (TFEQ) improved significantly from baseline to the end of the intervention (Figure 1). More than half (58%) of the participants showed an improvement for “Cognitive restraint,” 16% worsened and 26% remained stable. “Disinhibition” improved in 55% of the patients, worsened in 6% and remained stable in 40%. Regarding “Feelings of hunger” from pre-to post-treatment, more than half of the patients (54%) improved, while 20% worsened and 26% remained similar. In line were the results for the two subgroups PANNEG and PANPOS: except for Feelings of Hunger for PANPOS all three subscales improved from pre-to post-treatment. Eating behavior did not differ significantly between PANNEG and PANPOS from pre-to post-treatment (FDR >0.1, Table 3).
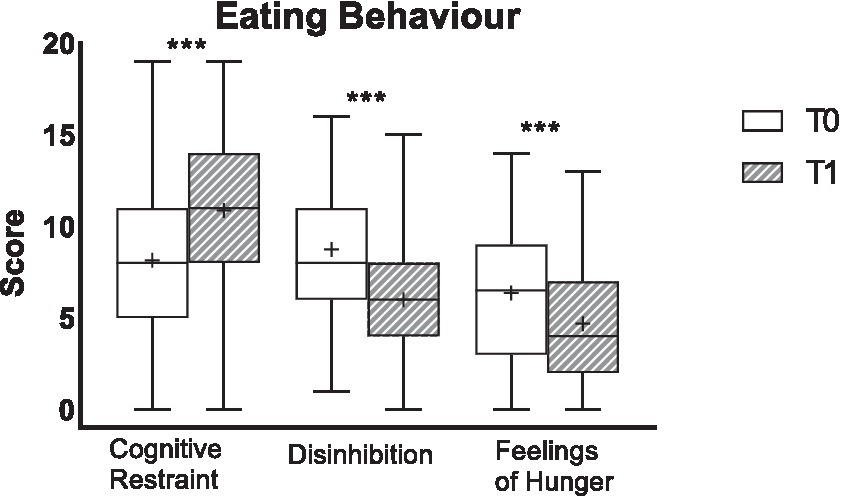
Figure 1. Eating behaviour of the total study population for pre- (T0) and post-intervention (T1). Scores for eating behaviour are presented. The data are shown as box-whiskers [median with upper and lower quartiles, whose difference describes the interquartile range (IQR) and minimum and maximum (=whiskers)]. Mean is depicted as “+.” Increases from T0 to T1 for cognitive restraint as well as decreases from T0 to T1 for disinhibition and feelings of hunger represent an improvement. ***Significant differences between T0 and T1 (FDR < 0.001).
3.3.3 Participants benefit personally from the intervention
In general, the evaluation questionnaire at the end of the intervention showed a high satisfaction of the participants with the program. Almost all participants (90%) would recommend the intervention to family and friends. The results are shown in Supplementary material S3. Participants with worsening MCIDs did not show lower levels of satisfaction with the program than participants who showed improvement or had stable MCIDs. Detailed information is presented in the Supplementary material S4.
4 Discussion
This study investigated the impact of the COVID-19 pandemic on psychological parameters and eating behavior in people with predominantly grade III obesity who sought help from a multimodal conservative weight loss program during the pandemic. Contrary to our hypothesis (i), people with severe obesity who enrolled in a multimodal BWL program did neither show increased anxiety and depression symptoms nor higher perceived stress than prior to the pandemic. These findings are partially consistent with previous research. Studies recorded an increase in anxiety and depressive symptomatology and stress experience during the COVID-19 pandemic, in contrast to the present work (6, 15). However, this research related to the initial period of the pandemic, concomitant with the first lockdown. In the “Mannheim Corona Study,” which examined the impact of the COVID-19 pandemic on the German population over a sixteen-week period beginning in March 2020, symptoms of anxiety and depression were most pronounced shortly after the quarantine order. Over time, these symptoms decreased slightly. This may be due to a habituation effect (73) or, as trauma researchers have shown, to the fact that many people experience a phase of resilience or recovery after negative events (74). Studies that also focused on later time points in the pandemic like this (started in July 2020 up to April 2022) research showed similar results to the present (75, 76).
People living with obesity are highly affected by weight stigma and discrimination, which are associated with psychological distress (77): in the workplace, schools and colleges, in health care settings, and even in private settings (78–80). Strict contact restrictions and curfews were mandated to combat the COVID-19 pandemic, which may have led to a reduction in discrimination and stigmatization of people living with obesity (81, 82) and thus may have contributed to trending lower expressions of anxiety and depression symptomatology and stress experience. Furthermore, the certainty of experiencing food without an external evaluation may have led to these lower scores compared to before. Another possibility for the trend toward lower stress levels during the COVID-19 pandemic compared with before may be less experienced time stress since pandemic onset. The introduction and expansion of home office in various work sectors (83, 84) allowed for more flexible work schedules and decimated commutes and travel for many employees (85). In addition, many business trips were cancelled. Meetings with people in other places and countries were instead held online via videoconferencing, resulting in significantly reduced times spent in cars, buses, trains or planes (86).
Compared to PrePAN, PAN exhibited lower perceived hunger levels as well as lower disturbance of eating behavior at baseline. One reason for this may be a decreased opportunity for casual purchases, social eating situations, or restaurant visits. Some research suggests that as BMI increases, experienced feelings of hunger and the disturbance of eating behavior increases, while cognitive control decreases (8, 87, 88). Because many activities occurred within the home due to COVID-19 constraints and significantly less time was spent on the go (89), spontaneous purchases due to external factors such as the sight or smell of food may have decreased. Research shows that higher cognitive restraint scores are associated with lower BMI, lower energy intake, and lower appetite ratings (62) and leads to higher weight loss in weight reduction interventions (90). Nevertheless, it is also possible that although cognitive restraint may lead to lower BMI and greater weight loss during weight loss interventions, rigid cognitive restraint may also lead to the development of disordered eating behaviors (62, 91) and can therefore also have a negative impact.
As hypothesised (ii), BWL intervention during the COVID-19 pandemic led to stabilization and improvement in eating behaviour and physical and psychological parameters. At the end of the intervention, body weight reduction was observed in two-thirds of the subjects and body weight stabilization in 16% of the participants. There was an improvement or stabilization with respect to anxiety and depression symptoms in 86% and 80% of the patients, respectively. Consistent with our hypothesis, perceived stress (worry and demands) tended to decrease over the course of the intervention. However, PAN was significantly higher in stress experience both before and after the intervention than the sample of healthy adults studied by Fliege et al. (61).
Furthermore, PAN showed improvements in physical, but not psychological HRQoL at the end of the intervention. This is also documented in the existing literature: clinical BWL programs showed successful improvements in physical HRQoL (92–94). Improvements in HRQoL were shown independent of weight loss in various weight loss programs (9, 94). Interestingly, participants who showed a worsening of psychological parameters during treatment, rated the BWL program as positive as those with improvement or stabilization. This suggests that the participants’ benefit extends beyond the reduction of psychological symptoms.
Patients in medical and psychotherapeutic treatments during the pandemic were especially grateful that therapeutic treatment could take place despite the pandemic (95). This may have been the same for the patients in this study. The program may have prevented the development of even worse psychological outcomes in these patients.
PAN showed more beneficial eating behavior after the intervention when compared to baseline. Previous studies showed that eating behavior change positively during weight loss interventions, but that the disturbance of eating behavior and experienced feelings of hunger are not directly associated with body weight change (47, 96, 97). This is supported by the present results.
The presented study has strengths and limitations. A clear strength of the study is the low dropout rate of 8%, whereby the large sample provides meaningful results for further theoretical assumptions and practical implementations. Only validated questionnaires were used to assess participants’ anxiety and depression symptoms, stress experience, HRQoL, and eating behavior, which is another clear strength of the work. Missing values were replaced using the predictive mean matching method to calculate values for the ITT population. During the COVID-19 pandemic body weight was subjectively reported with data appearing realistic. One study showed that self-reported body weight is underestimated in people with obesity (49) whereas other studies report that body weight is also accurately reported in people with overweight and obesity (50), especially in those participating in a weight loss program (51). The data of this study could not be compared to a control group. Theoretically, a comparison with the PrePAN group would have been possible but we decided, that this comparison was not acceptable because two variables would have been mixed at the same time, being the life condition (pre-pandemic versus pandemic) and mode of delivery of the BWL intervention (face-to-face versus online). The differences between PrePAN and PAN regarding anxiety and depression symptomatology as well as stress experience disappeared after comparing age-, gender-, BMI-, and surgery-attitude-matched subjects between the two groups. The reason could be due to the only minor differences in the total sample, which were lost after matching the sample groups due to the reduced sample size.
5 Conclusion
People with severe obesity attending a virtual, video-based multimodal BWL intervention program during COVID-19 were similar burdened with regard to HRQoL and symptoms for anxiety and depression, stress, when compared to pre-pandemic times. A multidisciplinary conservative weight loss intervention in a virtual setting during the uncertain times of the pandemic helped to stabilize and improve the physiological and psychological burdens of people with severe obesity. Although, digitization due to the COVID-19 pandemic has rapidly advanced the progress of technology in healthcare, digital options in the field of obesity treatment should be further expanded and evaluated to maximize the effectiveness of these interventions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of the University Hospital Tübingen, Germany. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JS: Formal analysis, Methodology, Visualization, Writing – original draft. KB: Formal analysis, Methodology, Writing – review & editing. SS: Methodology, Writing – review & editing. BK: Methodology, Writing – review & editing. RE: Methodology, Writing – review & editing. AS: Supervision, Writing – review & editing. AN: Resources, Writing – review & editing. SZ: Resources, Writing – review & editing. IM: Conceptualization, Formal analysis, Methodology, Resources, Supervision, Visualization, Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The authors acknowledge support by the Deutsche Forschungsgemeinschaft and the Open Access Publishing Fund of Tübingen University.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
SZ was an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1330278/full#supplementary-material
Abbreviations
BMI, body mass index; BWL, behavioral weight loss; COVID-19, coronavirus disease-19; GAD-7, generalized anxiety disorder scale; HRQoL, health-related quality of life; MCID, minimal clinically important difference; PAN, people participating in the intervention during the pandemic; PHQ-9, patient health questionnaire-9; PSQ-20, perceived stress questionnaire-20; PrePAN, people participating in the intervention prior to the pandemic; SF-12, short form health-survey 12; TFEQ, three factor eating questionnaire; WHO, World Health Organization.
References
1. WHO. Rolling updates on coronavirus disease (COVID-19) (2020) Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
2. Steinmetz, H, Batzdorfer, V, and Bosnjak, M. The ZPID lockdown measures dataset. ZPID Science Information Online. (2020) 20. doi: 10.23668/psycharchives.6679
3. World Health Organization. WHO coronavirus (COVID-19) dashboard (2022). Available at: https://covid19.who.int/
4. WHO. Obesity—preventing and managing the global epidemic: report on a WHO consultation. Geneva: World Health Organization (2000). 266 p.
5. The German Obesity Society e.V.; the German diabetes society; the German nutrition society e.V.; the German Society of Nutritional Medicine e.V. Interdisciplinary S3 guideline prevention and therapy of obesity. Adipositas—Ursachen, Folgeerkrankungen, Therapie (2014) 08:179–221
6. Bäuerle, A, Teufel, M, Musche, V, Weismüller, B, Kohler, H, Hetkamp, M, et al. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J Public Health (Oxf). (2020) 42:672–8. doi: 10.1093/pubmed/fdaa106
7. Bemanian, M, Mæland, S, Blomhoff, R, Rabben, ÅK, Arnesen, EK, Skogen, JC, et al. Emotional eating in relation to worries and psychological distress amid the COVID-19 pandemic: a population-based survey on adults in Norway. Int J Environ Res Public Health. (2020) 18:18. doi: 10.3390/ijerph18010130
8. Ernst, B, Wilms, B, Thurnheer, M, and Schultes, B. Eating behaviour in treatment-seeking obese subjects—influence of sex and BMI classes. Appetite. (2015) 95:96–100. doi: 10.1016/j.appet.2015.06.019
9. Fontaine, KR, and Barofsky, I. Obesity and health-related quality of life. Obes Rev. (2001) 2:173–82. doi: 10.1046/j.1467-789x.2001.00032.x
10. Gariepy, G, Wang, J, Lesage, AD, and Schmitz, N. The longitudinal association from obesity to depression: results from the 12-year National Population Health Survey. Obesity (Silver Spring). (2010) 18:1033–8. doi: 10.1038/oby.2009.333
11. Luppino, FS, Wit, LM, Bouvy, PF, Stijnen, T, Cuijpers, P, Penninx, BWJH, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. (2010) 67:220–9. doi: 10.1001/archgenpsychiatry.2010.2
12. Moore, CJ, and Cunningham, SA. Social position, psychological stress, and obesity: a systematic review. J Acad Nutr Diet. (2012) 112:518–26. doi: 10.1016/j.jand.2011.12.001
13. Mühlhans, B, Horbach, T, and Zwaan, M. Psychiatric disorders in bariatric surgery candidates: a review of the literature and results of a German prebariatric surgery sample. Gen Hosp Psychiatry. (2009) 31:414–21. doi: 10.1016/j.genhosppsych.2009.05.004
14. Peters, E, Hübner, J, and Katalinic, A. Stress, Copingstrategien und gesundheitsbezogene Lebensqualität während der Corona-Pandemie im April 2020 in Deutschland. [stress, coping strategies and health-related quality of life during the corona pandemic in April 2020 in Germany]. Dtsch Med Wochenschr. (2021) 146:e11–20. doi: 10.1055/a-1275-3792
15. Petzold, MB, Bendau, A, Plag, J, Pyrkosch, L, Mascarell Maricic, L, Betzler, F, et al. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav. (2020) 10:e01745. doi: 10.1002/brb3.1745
16. Vázquez Velázquez, V, Pizarro, J, Sánchez Román, S, Arcila Martínez, D, Soto Fuentes, V, and Velázquez, JH. Eating behavior during COVID-19 pandemic: comparison between people with obesity, overweight and normal weight. Obes Facts. (2021) 14:1–154. doi: 10.1159/000515911
17. Eicher, S, Pryss, R, Baumeister, H, Hövener, C, Knoll, N, and Cohrdes, C. Quality of life during the COVID-19 pandemic—results of the CORONA HEALTH app study. J Health Monit. (2021) 6:2–21. doi: 10.25646/8867
18. Flanagan, EW, Beyl, RA, Fearnbach, SN, Altazan, AD, Martin, CK, and Redman, LM. The impact of COVID-19 stay-at-home orders on health behaviors in adults. Obesity (Silver Spring). (2021) 29:438–45. doi: 10.1002/oby.23066
19. Kriaucioniene, V, Bagdonaviciene, L, Rodríguez-Pérez, C, and Petkeviciene, J. Associations between changes in health Behaviours and body weight during the COVID-19 quarantine in Lithuania: the Lithuanian COVIDiet study. Nutrients. (2020) 12:12. doi: 10.3390/nu12103119
20. Seal, A, Schaffner, A, Phelan, S, Brunner-Gaydos, H, Tseng, M, Keadle, S, et al. COVID-19 pandemic and stay-at-home mandates promote weight gain in US adults. Obesity (Silver Spring). (2022) 30:240–8. doi: 10.1002/oby.23293
21. Khubchandani, J, Price, JH, Sharma, S, Wiblishauser, MJ, and Webb, FJ. COVID-19 pandemic and weight gain in American adults: a nationwide population-based study. Diabetes Metab Syndr. (2022) 16:102392. doi: 10.1016/j.dsx.2022.102392
22. Almandoz, JP, Xie, L, Schellinger, JN, Mathew, MS, Gazda, C, Ofori, A, et al. Impact of COVID-19 stay-at-home orders on weight-related behaviours among patients with obesity. Clin Obes. (2020) 10:e12386. doi: 10.1111/cob.12386
23. Hamer, M, Gale, CR, Kivimäki, M, and Batty, GD. Overweight, obesity, and risk of hospitalization for COVID-19: a community-based cohort study of adults in the United Kingdom. Proc Natl Acad Sci U S A. (2020) 117:21011–3. doi: 10.1073/pnas.2011086117
24. Singh, R, Rathore, SS, Khan, H, Karale, S, Chawla, Y, Iqbal, K, et al. Association of Obesity with COVID-19 severity and mortality: an updated systemic review, Meta-analysis, and Meta-regression. Front Endocrinol. (2022) 13:780872. doi: 10.3389/fendo.2022.780872
25. Battisti, S, Pedone, C, Napoli, N, Russo, E, Agnoletti, V, Nigra, SG, et al. Computed tomography highlights increased visceral adiposity associated with critical illness in COVID-19. Diabetes Care. (2020) 43:e129–30. doi: 10.2337/dc20-1333
26. Huang, Y, Lu, Y, Huang, Y-M, Wang, M, Ling, W, Sui, Y, et al. Obesity in patients with COVID-19: a systematic review and meta-analysis. Metab Clin Exp. (2020) 113:154378. doi: 10.1016/j.metabol.2020.154378
27. Poly, TN, Islam, MM, Yang, HC, Lin, MC, Jian, W-S, Hsu, M-H, et al. Obesity and mortality among patients diagnosed with COVID-19: a systematic review and Meta-analysis. Front Med. (2021) 8:620044. doi: 10.3389/fmed.2021.620044
28. Schäffeler, N, Lohmiller, J, Mack, I, Archid, R, Zipfel, S, and Stengel, A. Patients with super obesity do not perceive themselves as being at higher risk for a more severe course of COVID-19 infection. Front Psych. (2021) 12:798662. doi: 10.3389/fpsyt.2021.798662
29. Petrilli, CM, Jones, SA, Yang, J, Rajagopalan, H, O'Donnell, L, Chernyak, Y, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in new York City: prospective cohort study. BMJ (Clinical research ed). (2020) 369:m1966. doi: 10.1136/bmj.m1966
30. Paravidino, VB, Leite, TH, Mediano, MF, Sichieri, R, Silva, AE, Cravo, V, et al. Association between obesity and COVID-19 mortality and length of stay in intensive care unit patients in Brazil: a retrospective cohort study. Sci Rep. (2022) 12:13737. doi: 10.1038/s41598-022-17197-w
31. Schienkiewitz, A, Damerow, S, Richter, A, and Mensink, GB. How has body weight changed since the beginning of the COVID-19 pandemic? J Health Monit. (2022) 7:54–61. doi: 10.25646/10670
32. Policarpo, S, Machado, MV, and Cortez-Pinto, H. Telemedicine as a tool for dietary intervention in NAFLD-HIV patients during the COVID-19 lockdown: a randomized controlled trial. Clini Nut ESPEN. (2021) 43:329–34. doi: 10.1016/j.clnesp.2021.03.031
33. Wang, Q, Su, M, Zhang, M, and Li, R. Integrating digital technologies and public health to fight Covid-19 pandemic: key technologies, applications, challenges and outlook of digital healthcare. Int J Environ Res Public Health. (2021) 18:18. doi: 10.3390/ijerph18116053
34. Levine, DM, Savarimuthu, S, Squires, A, Nicholson, J, and Jay, M. Technology-assisted weight loss interventions in primary care: a systematic review. J Gen Intern Med. (2015) 30:107–17. doi: 10.1007/s11606-014-2987-6
35. Raaijmakers, LC, Pouwels, S, Berghuis, KA, and Nienhuijs, SW. Technology-based interventions in the treatment of overweight and obesity: a systematic review. Appetite. (2015) 95:138–51. doi: 10.1016/j.appet.2015.07.008
36. Ufholz, K, and Bhargava, D. A review of telemedicine interventions for weight loss. Curr Cardiovasc Risk Rep. (2021) 15:17. doi: 10.1007/s12170-021-00680-w
37. Weinstein, PK . A review of weight loss programs delivered via the internet. J Cardiovasc Nurs. (2006) 21:251–8. doi: 10.1097/00005082-200607000-00003
38. Baer, HJ, Rozenblum, R, La Cruz, BA, Orav, EJ, Wien, M, Nolido, NV, et al. Effect of an online weight management program integrated with population health management on weight change: a randomized clinical trial. JAMA. (2020) 324:1737–46. doi: 10.1001/jama.2020.18977
39. Batsis, JA, Petersen, CL, Clark, MM, Cook, SB, Kotz, D, Gooding, TL, et al. Feasibility and acceptability of a technology-based, rural weight management intervention in older adults with obesity. BMC Geriatr. (2021) 21:44. doi: 10.1186/s12877-020-01978-x
40. Zaman, A, Sloggett, KJ, Caldwell, AE, Catenacci, VA, Cornier, M-A, Grau, L, et al. The effects of the COVID-19 pandemic on weight loss in participants in a behavioral weight-loss intervention. Obesity (Silver Spring). (2022) 30:1015–26. doi: 10.1002/oby.23399
41. Bailly, S, Fabre, O, Legrand, R, Pantagis, L, Mendelson, M, Terrail, R, et al. The impact of the COVID-19 lockdown on weight loss and body composition in subjects with overweight and obesity participating in a Nationwide weight-loss program: impact of a remote consultation follow-up-the CO-RNPC study. Nutrients. (2021) 13:13. doi: 10.3390/nu13072152
42. Santagiuliana, F, Cosentino, C, Pala, L, Frizza, F, Nannoni, A, Mannucci, E, et al. Online group lifestyle modification programs for obesity during the COVID-19 pandemic: the EDucation ONline (EDON) retrospective study. Nutr Metab Cardiovasc Dis. (2022) 32:1317–8. doi: 10.1016/j.numecd.2022.02.009
43. Tchang, BG, Morrison, C, Kim, JT, Ahmed, F, Chan, KM, Alonso, LC, et al. Weight loss outcomes with telemedicine during COVID-19. Front Endocrinol. (2022) 13:793290. doi: 10.3389/fendo.2022.793290
44. Mueller, J, Richards, R, Jones, RA, Whittle, F, Woolston, J, Stubbings, M, et al. Supporting weight management during COVID-19: a randomized controlled trial of a web-based, ACT-based, Guided Self-Help Intervention. Obesity Facts. (2022) 15:550–9. doi: 10.1159/000524031
45. Ozturk, B, and Duruturk, N. Effect of telerehabilitation applied during COVID-19 isolation period on physical fitness and quality of life in overweight and obese individuals. Int J Obes. (2022) 46:95–9. doi: 10.1038/s41366-021-00965-5
46. Yin, W, Liu, Y, Hu, H, Sun, J, Liu, Y, and Wang, Z. Telemedicine management of type 2 diabetes mellitus in obese and overweight young and middle-aged patients during COVID-19 outbreak: a single-center, prospective, randomized control study. PLoS One. (2022) 17:e0275251. doi: 10.1371/journal.pone.0275251
47. Bauer, K, Schild, S, Sauer, H, Teufel, M, Stengel, A, Giel, KE, et al. Attitude matters! How attitude towards bariatric surgery influences the effects of Behavioural weight loss treatment. Obes Facts. (2021) 14:531–42. doi: 10.1159/000517850
48. Wirth, A, Wabitsch, M, and Hauner, H. The prevention and treatment of obesity. Dtsch Arztebl Int. (2014) 111:705–13. doi: 10.3238/arztebl.2014.0705
49. Lin, CJ, DeRoo, LA, Jacobs, SR, and Sandler, DP. Accuracy and reliability of self-reported weight and height in the sister study. Public Health Nutr. (2012) 15:989–99. doi: 10.1017/S1368980011003193
50. Stunkard, AJ, and Albaum, JM. The accuracy of self-reported weights. Am J Clin Nutr. (1981) 34:1593–9. doi: 10.1093/ajcn/34.8.1593
51. Rossouw, K, Senekal, M, and Stander, I. The accuracy of self-reported weight by overweight and obese women in an outpatient setting. Public Health Nutr. (2001) 4:19–26. doi: 10.1079/phn200051
52. Ware, JE, Keller, SD, and Kosinski, M. SF-12: How to score the SF-12 physical and mental health summary scales. Health Institute, New England Medical Center. (1995).
53. Spitzer, RL, Kroenke, K, Williams, JB, and Löwe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
54. Kroenke, K, Spitzer, RL, and Williams, JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
55. Fliege, H, Rose, M, Arck, P, Levenstein, S, and Klapp, BF. Validation of the perceived stress questionnaire (PSQ) in a German sample. Diagnostica. (2001) 47:142–52. doi: 10.1026//0012-1924.47.3.142
56. Pudel, V, and Westenhoefer, J. Fragebogen zum Essverhalten (FEV). Handanweisung. Goettingen u.a: Hogrefe (1989).
57. Wee, CC, Davis, RB, and Hamel, MB. Comparing the SF-12 and SF-36 health status questionnaires in patients with and without obesity. Health Qual Life Outcomes. (2008) 6:11. doi: 10.1186/1477-7525-6-11
58. Batsis, JA, Lopez-Jimenez, F, Collazo-Clavell, ML, Clark, MM, Somers, VK, and Sarr, MG. Quality of life after bariatric surgery: a population-based cohort study. Am J Med. (2009) 122:1055.e1–1055.e10. doi: 10.1016/j.amjmed.2009.05.024
59. Alizai, PH, Akkerman, MK, Kaemmer, D, Ulmer, F, Klink, CD, Ernst, S, et al. Presurgical assessment of bariatric patients with the patient health questionnaire (PHQ)—a screening of the prevalence of psychosocial comorbidity. Health Qual Life Outcomes. (2015) 13:1–7. doi: 10.1186/s12955-015-0278-5
60. Wild, B, Hünnemeyer, K, Sauer, H, Hain, B, Mack, I, Schellberg, D, et al. A 1-year videoconferencing-based psychoeducational group intervention following bariatric surgery: results of a randomized controlled study. Surg Obes Relat Dis. (2015) 11:1349–60. doi: 10.1016/j.soard.2015.05.018
61. Fliege, H, Rose, M, Arck, P, Walter, OB, Kocalevent, R-D, Weber, C, et al. The perceived stress questionnaire (PSQ) reconsidered: validation and reference values from different clinical and healthy adult samples. Psychosom Med. (2005) 67:78–88. doi: 10.1097/01.psy.0000151491.80178.78
62. Bryant, EJ, Rehman, J, Pepper, LB, and Walters, ER. Obesity and eating disturbance: the role of TFEQ restraint and disinhibition. Curr Obes Rep. (2019) 8:363–72. doi: 10.1007/s13679-019-00365-x
63. Löffler, A, Luck, T, Then, FS, Sikorski, C, Kovacs, P, Böttcher, Y, et al. Eating behaviour in the general population: an analysis of the factor structure of the German version of the three-factor-eating-questionnaire (TFEQ) and its association with the body mass index. PLoS One. (2015) 10:e0133977. doi: 10.1371/journal.pone.0133977
64. Mack, I, Ölschläger, S, Sauer, H, Feilitzsch, M, Weimer, K, Junne, F, et al. Does laparoscopic sleeve gastrectomy improve depression, stress and eating behaviour? A 4-year follow-up study. Obes Surg. (2016) 26:2967–73. doi: 10.1007/s11695-016-2219-8
66. Jensen, MD, Ryan, DH, Apovian, CM, Ard, JD, Comuzzie, AG, Donato, KA, et al. 2013 AHA/ACC/TOS guideline for the Management of Overweight and Obesity in adults. Circulation. (2014) 129:S102–38. doi: 10.1161/01.cir.0000437739.71477.ee
67. Fine, JT, Colditz, GA, Coakley, EH, Moseley, G, Manson, JE, Willett, WC, et al. A prospective study of weight change and health-related quality of life in women. JAMA. (1999) 282:2136–42. doi: 10.1001/jama.282.22.2136
68. Benjamini, Y, and Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Royal Stat Soc. (1995) 57:289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x
70. Little, RJ, and Rubin, DB. Statistical analysis with missing data. Hoboken, NJ, USA: Wiley (2020). 449 p.
71. Lubetkin, EI, and Gold, MR. Areas of decrement in health-related quality of life (HRQL): comparing the SF-12, EQ-5D, and HUI 3. Qual Life Res Int J Qual Life Asp Treat Care Rehab. (2003) 12:1059–67. doi: 10.1023/a:1026183317288
72. Toussaint, A, Hüsing, P, Gumz, A, Wingenfeld, K, Härter, M, Schramm, E, et al. Sensitivity to change and minimal clinically important difference of the 7-item generalized anxiety disorder questionnaire (GAD-7). J Affect Disord. (2020) 265:395–401. doi: 10.1016/j.jad.2020.01.032
73. Mata, J, Wenz, A, Rettig, T, Reifenscheid, M, Möhring, K, Krieger, U, et al. Health behaviors and mental health during the COVID-19 pandemic: a longitudinal population-based survey in Germany. Soc Sci Med. (2021) 287:114333. doi: 10.1016/j.socscimed.2021.114333
74. Chen, S, and Bonanno, GA. Psychological adjustment during the global outbreak of COVID-19: a resilience perspective. Psychol Trauma Theory Res Pract Policy. (2020) 12:S51–4. doi: 10.1037/tra0000685
75. Mahmud, S, Mohsin, M, Dewan, MN, and Muyeed, A. The global prevalence of depression, anxiety, stress, and insomnia among general population during COVID-19 pandemic: a systematic review and Meta-analysis. Trends Psychol. (2022) 31:143–70. doi: 10.1007/s43076-021-00116-9
76. Robinson, E, Sutin, AR, Daly, M, and Jones, A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J Affect Disord. (2022) 296:567–76. doi: 10.1016/j.jad.2021.09.098
77. O'Brien, KS, Latner, JD, Puhl, RM, Vartanian, LR, Giles, C, Griva, K, et al. The relationship between weight stigma and eating behavior is explained by weight bias internalization and psychological distress. Appetite. (2016) 102:70–6. doi: 10.1016/j.appet.2016.02.032
78. Puhl, RM, and Brownell, KD. Confronting and coping with weight stigma: an investigation of overweight and obese adults. Obesity (Silver Spring). (2006) 14:1802–15. doi: 10.1038/oby.2006.208
79. Puhl, RM, and Heuer, CA. The stigma of obesity: a review and update. Obesity (silver spring). (2009) 17:941–64. doi: 10.1038/oby.2008.636
80. Puhl, RM, and Lessard, LM. Weight stigma in youth: prevalence, consequences, and considerations for clinical practice. Curr Obes Rep. (2020) 9:402–11. doi: 10.1007/s13679-020-00408-8
81. Brown, A, Flint, SW, Kalea, AZ, O'Kane, M, Williams, S, and Batterham, RL. Negative impact of the first COVID-19 lockdown upon health-related behaviours and psychological wellbeing in people living with severe and complex obesity in the UK. EClinicalMedicine. (2021) 34:100796. doi: 10.1016/j.eclinm.2021.100796
82. Fung, XC, Siu, AM, Potenza, MN, O'Brien, KS, Latner, JD, Chen, C-Y, et al. Problematic use of internet-related activities and perceived weight stigma in schoolchildren: a longitudinal study across different epidemic periods of COVID-19 in China. Front Psych. (2021) 12:675839. doi: 10.3389/fpsyt.2021.675839
83. Schröder, C, Entringer, TM, Goebel, J, Grabka, MM, Graeber, D, Kroh, M, et al. Covid-19 is not affecting all working people equally In: Working Paper. Berlin: Deutsches Institut für Wirtschaftsforschung (DIW) (2020)
84. Möhring, K, Naumann, E, Reifenscheid, M, Weiland, A, Blom, AG, Wenz, A, et al. Die Mannheimer Corona-Studie: Schwerpunktbericht zur Nutzung und Akzeptanz von Homeoffice in Deutschland während des Corona-Lockdowns. Mannheim: Universitätsbibliothek Mannheim (2020) Online-Ressource.
85. Huang, Z, Loo, BP, and Axhausen, KW. Travel behaviour changes under work-from-home (WFH) arrangements during COVID-19. Travel Behav Soc. (2023) 30:202–11. doi: 10.1016/j.tbs.2022.09.006
86. Statistisches Bundesamt, Wissenschaftszentrum Berlinf ür Sozialforschung, Bundesinstitut für Bevölkerungsforschung. Datenreport 2021. Ein Sozialbericht für die Bundesrepublik Deutschland.: Auswirkungen der Coronapandemie. Auszug aus dem Datenreport 2021 (2021).
87. Davison, KM . The relationships among psychiatric medications, eating behaviors, and weight. Eat Behav. (2013) 14:187–91. doi: 10.1016/j.eatbeh.2013.01.001
88. Thomas, EA, Bechtell, JL, Vestal, BE, Johnson, SL, Bessesen, DH, Tregellas, JR, et al. Eating-related behaviors and appetite during energy imbalance in obese-prone and obese-resistant individuals. Appetite. (2013) 65:96–102. doi: 10.1016/j.appet.2013.01.015
89. Statistisches Bundesamt, Wissenschaftszentrum Berlin für Sozialforschung, Bundesinstitut für Bevölkerungsforschung. Datenreport 2021. Ein Sozialbericht für die Bundesrepublik Deutschland: Auswirkungen der Coronapandemie. Auszug aus dem Datenreport 2021 (2021).
90. Papini, NM, Foster, RN, Lopez, NV, Ptomey, LT, Herrmann, SD, and Donnelly, JE. Examination of three-factor eating questionnaire subscale scores on weight loss and weight loss maintenance in a clinical intervention. BMC Psychol. (2022) 10:101. doi: 10.1186/s40359-022-00806-8
91. Tuschl, RJ . From dietary restraint to binge eating: some theoretical considerations. Appetite. (1990) 14:105–9. doi: 10.1016/0195-6663(90)90004-r
92. Blissmer, B, Riebe, D, Dye, G, Ruggiero, L, Greene, G, and Caldwell, M. Health-related quality of life following a clinical weight loss intervention among overweight and obese adults: intervention and 24 month follow-up effects. Health Qual Life Outcomes. (2006) 4:43. doi: 10.1186/1477-7525-4-43
93. Bond, DS, Unick, JL, Jakicic, JM, Vithiananthan, S, Trautvetter, J, O'Leary, KC, et al. Physical activity and quality of life in severely obese individuals seeking bariatric surgery or lifestyle intervention. Health Qual Life Outcomes. (2012) 10:86. doi: 10.1186/1477-7525-10-86
94. Harding, C, Seal, A, and Mills, N. Evaluation of a lifestyle and weight management program within rural general practice. J Prim Care Community Health. (2022) 13:21501319221084166. doi: 10.1177/21501319221084166
95. Erschens, R, Adam, SH, Weisshap, C, Giel, KE, Wallis, H, Herrmann-Werner, A, et al. The role of face masks within in-patient psychotherapy: results of a survey among inpatients and healthcare professionals. Front Neurosci. (2022) 16:1030397. doi: 10.3389/fnins.2022.1030397
96. Freund, AM, and Hennecke, M. Changing eating behaviour vs. losing weight: the role of goal focus for weight loss in overweight women. Psychol Health. (2012) 27:25–42. doi: 10.1080/08870446.2011.570867
Keywords: Behavioral weight loss, COVID-19, morbid obesity, psychological effects, videoconference-based intervention
Citation: Schraml J, Bauer K, Schild S, Klos B, Erschens R, Stengel A, Nieß A, Zipfel S and Mack I (2024) Conventional weight loss therapy in morbid obesity during COVID-19 pandemic: degree of burdens at baseline and treatment efficacy. Front. Psychiatry. 15:1330278. doi: 10.3389/fpsyt.2024.1330278
Edited by:
Paolo Meneguzzo, University of Padua, ItalyReviewed by:
Edoardo Mocini, Sapienza University of Rome, ItalyPatrizia Todisco, Casa di Cura Villa Margherita, Italy
Copyright © 2024 Schraml, Bauer, Schild, Klos, Erschens, Stengel, Nieß, Zipfel and Mack. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Isabelle Mack, aXNhYmVsbGUubWFja0B1bmktdHVlYmluZ2VuLmRl
 Jessica Schraml
Jessica Schraml Kerstin Bauer1
Kerstin Bauer1 Bea Klos
Bea Klos Rebecca Erschens
Rebecca Erschens Andreas Stengel
Andreas Stengel Andreas Nieß
Andreas Nieß Stephan Zipfel
Stephan Zipfel Isabelle Mack
Isabelle Mack