- 1Unit of Psychiatry, Department of Public Health and Medicinal Administration, Faculty of Health Sciences, Institute of Translational Medicine, University of Macau, Macao SAR, China
- 2Centre for Cognitive and Brain Sciences, University of Macau, Macao SAR, China
- 3Beijing Huilongguan Hospital, Peking University Huilongguan Clinical Medical School, Beijing, China
- 4School of Public Health, Southeast University, Nanjing, China
- 5School of Nursing, Hong Kong Polytechnic University, Kowloon, Hong Kong SAR, China
- 6Faculty of Health Sciences and Sports, Macao Polytechnic University, Macao SAR, China
- 7Section of Psychiatry, University of Notre Dame Australia, Fremantle, WA, Australia
- 8Division of Psychiatry, School of Medicine, University of Western Australia, Perth, WA, Australia
- 9Department of Psychiatry, The Melbourne Clinic and St Vincent's Hospital, University of Melbourne, Richmond, VIC, Australia
- 10Beijing Key Laboratory of Mental Disorders, National Clinical Research Center for Mental Disorders & National Center for Mental Disorders, Beijing Anding Hospital, Capital Medical University, Beijing, China
Objective: The coronavirus disease (COVID-19) and the public health responses were associated with a huge health burden, which could influence sleep quality. This meta-analysis and systematic review examined the prevalence of poor sleep quality in COVID-19 patients.
Methods: PubMed, Web of Science, Embase, and PsycINFO were systematically searched from their respective inception to October 27, 2022. Prevalence rates of poor sleep were analyzed using a random effects model.
Results: Totally, 24 epidemiological and 12 comparative studies with 8,146 COVID-19 patients and 5,787 healthy controls were included. The pooled prevalence of poor sleep quality based on the included studies was 65.0% (95%CI: 59.56–70.44%, I2 = 97.6%). COVID-19 patients had a higher risk of poor sleep quality compared to healthy controls (OR = 1.73, 95% CI: 1.30–2.30, p < 0.01, I2 = 78.1%) based on the 12 comparative studies. Subgroup analysis revealed that COVID-19 patients in low-income countries (p = 0.011) and in studies using a lower Pittsburgh Sleep Quality Index score cut-off (p < 0.001) were more likely to have poor sleep quality. Meta-regression analyses revealed that being female (p = 0.044), older (p < 0.001) and married (p = 0.009) were significantly correlated with a higher risk of poor sleep quality while quality score (p = 0.014) were negatively correlated with the prevalence of poor sleep quality in COVID-19 patients.
Conclusion: Poor sleep quality was found to be very common in COVID-19 patients. Considering the negative effects of poor sleep quality on daily life, sleep quality should be routinely assessed and appropriately addressed in COVID-19 patients.
1 Introduction
The huge health burden caused by the coronavirus disease (COVID-19) pandemic and the strict public health measures (e.g., social isolation) were associated with adverse physical and mental health outcomes (1, 2) including poor sleep quality (3). For instance, studies found that SARS-CoV-2 may affect negatively sleep in COVID-19 patients via a direct effect on the central nervous system (CNS) (4), or due to other COVID-19 related symptoms, such as fever, headache, dyspnea, myalgia, throat pain, cough, gastrointestinal disturbance, fatigue, anxiety and depression (5, 6), all of which could lead to poor sleep quality (7). A cohort study of hospitalized COVID-19 patients in China showed that 90.2% experienced poor sleep quality based on the Pittsburgh Sleep Quality Index (PSQI) assessment (8).
Poor sleep quality can have a negative impact on health. A study of COVID-19 patients in Turkey showed that poorer sleep quality was associated with a longer duration of hospitalization, while improving sleep quality could significantly reduce the length of hospital and intensive care unit stays (9). In addition, poor sleep quality combined with chronic retinal stimulation by electronic devices and extended or night work shifts, may worsen lung inflammation and aggravate the symptoms of COVID-19 infection (10). Furthermore, poor sleep quality can trigger oxidative stress and antioxidant imbalances and induce health-damaging pro-inflammatory states. To reduce the harmful effects of poor sleep quality on COVID-19 patients and allocate appropriate health resources, it is important to understand its pattern and associated factors (4, 11).
During the past years, prevalence studies of poor sleep quality in COVID-19 patients found wide variations, ranging from 25.5 to 88.6% (12–14), which is probably related to differences in COVID-19 severity and stages (e.g., COVID-19 onset, recovery, acute post-symptom onset), comorbidities, treatment regimens, and measures on sleep quality and cut-off values (15–19). There are various systematic reviews and meta-analyses that focused on the management of COVID-19, such as the role of methylprednisolone (20), aspirin (21), and baricitinib (22) in COVID-19 patients, but no meta-analysis on the prevalence of poor sleep quality in COVID-19 patients has been published. Therefore, we conducted this meta-analysis on the global prevalence of poor sleep quality in COVID-19 patients and its associated factors.
2 Methods
2.1 Search strategy
This meta-analysis was conducted based on the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) (23) and Meta-analysis of Observational Studies in Epidemiology (MOOSE) recommendations (24). The protocol was registered in the International Platform of Registered Systematic Review and Meta-analysis Protocols (INPLASY), with the registration number of INPLASY202320121. Three researchers (ZG, YY-W, and JX-L) independently retrieved relevant literature in PubMed, Web of Science, Embase, and PsycINFO databases from their inception until October 27, 2022, with the following search terms: (SARS-CoV-2 [MeSH] OR SARS Coronavirus 2 OR Coronavirus 2, SARS OR Coronavirus Disease 2019 Virus OR 2019 Novel Coronavirus OR 2019 Novel Coronaviruses OR Coronavirus, 2019 Novel OR Novel Coronavirus, 2019 OR SARS-CoV-2 Virus OR SARS CoV 2 Virus OR SARS-CoV-2 Viruses OR Virus, SARS-CoV-2 OR 2019-nCoV OR COVID-19 Virus OR COVID 19 Virus OR COVID-19 Viruses OR Virus, COVID-19 OR COVID19 Virus OR COVID19 Viruses OR Virus, COVID19 OR Viruses, COVID19 OR 2019 novel coronavirus infection OR COVID19 OR coronavirus disease 2019 OR coronavirus disease-19 OR 2019-nCoV disease OR 2019 novel coronavirus disease OR 2019-nCoV infection OR COVID-19 patients OR COVID-19 patient OR COVID-19 survivor) AND (Sleep Quality [MeSH] OR Qualities, Sleep OR Quality, Sleep OR Sleep Qualities OR quality of sleep OR sleeping quality OR Pittsburgh sleep quality index OR PSQI).
2.2 Study selection
The same researchers independently screened the titles and abstracts of all relevant publications, and then read the full texts to determine eligibility. Any disagreement was resolved by consensus among the three researchers or by discussion with a senior researcher (YT-X). Supplementary Figure S1 shows the detailed process of the literature search. The inclusion criteria for this study were based on the PICOS acronym (25): Participants (P): COVID-19 patients based on positive Coronavirus RT-PCR (reverse transcription-polymerase chain reaction) of nasopharyngeal and oropharyngeal swabs or a history of COVID-19 infection. Following previous research (26, 27), the COVID-19 patients in this study included the period of COVID-19 infection, symptom onset, recovery, and the onset of post-acute COVID-19 symptoms. Interventions (I): not applicable; Comparisons (C): healthy controls in comparative studies, or not applicable to epidemiological surveys; Outcome (O): the prevalence of poor sleep quality or available data could yield the prevalence of poor sleep quality in COVID-19 patients. Sleep quality in COVID-19 patients was assessed using any standardized scales such as the PSQI (7, 28); Study design (S): epidemiological and comparative studies (only the baseline data of cohort study were extracted). Exclusion criteria were as follows: (1) published in non-English language; (2) studies that only used individual items rather than the full version of a standardized scales on sleep quality; (3) patients with sleep-related disorders (as recommended in a previous meta-analysis) (29). If a dataset was used in multiple papers, only the paper with the complete information was included in this meta-analysis.
2.3 Data extraction and quality assessment
The same researchers independently extracted relevant information from the included studies and recorded them using an Excel data collection spreadsheet. The following information was extracted: study characteristics [e.g., title, journal, first author, publication year, study site by country, survey time, study design, assessment method, day zero (26), sampling method, cut-off value of standard scales on sleep quality, study quality score, and comorbidities associated with sleep quality], characteristics of COVID-19 patients [e.g., number of COVID-19 patients, number with poor sleep quality, total scores of standard scales on sleep quality, mean age (year), proportion of males, proportion of married status, proportion of smoking patients, average days of hospitalization, proportion of ICU admission, prevalence of anxiety and depression, and component scores of standard scales on sleep quality (i.e., subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleep medications, daytime dysfunction in the PSQI)] and characteristics of healthy controls [e.g., number of healthy controls, number of poor sleep quality, total scores of standard scales on sleep quality, mean age (year), and proportion of males].
For epidemiological studies, study quality was assessed using an eight-item assessment instrument with a scale of 0–8 (30), with scores of 0–3, 4–6, and 7–8 were considered “low quality”, “moderate quality”, and “high quality,” respectively (31). Study quality of comparative studies was assessed using the Newcastle-Ottawa Scale (NOS) (32). The NOS included eight items in three categories. In addition to the maximum of 2 stars for comparability, the remaining items could be rated up to 1 star, with a full score of 9 stars. Therefore, the NOS total score in this study ranges from 1 to 9 points, with a higher score indicating higher quality. Details of the study quality assessment tools are shown in Supplementary Table S1.
2.4 Statistical analysis
All data analyses were performed using R software (version 4.2.21) with the “meta” package (33). The random-effects model was used to estimate the pooled prevalence of poor sleep quality with the corresponding 95% confidence intervals (95% CIs). The I2 statistic was used to assess the heterogeneity of the study, with I2 greater than 50% indicating high heterogeneity (34). Subgroup analyses were performed based on the following categorical variables if there were at least 3 studies in each subgroup (35): cut-off values of standard scales on sleep quality, income levels by country (i.e., High income, vs. upper middle income, vs. lower middle income) according to the World Bank standard,2 assessment method (e.g., online survey vs. face-to-face interview), day zero (e.g., symptom onset vs. hospital discharge vs. hospital admission of COVID-19 patients), study design, gender, and sampling method. If there were at least 10 studies (36), meta-regression analyses were performed for the following continuous variable: sample size, mean age (year), proportion of males, proportion of married status, proportion of smoking patients, average days of hospitalization, proportion of ICU admission, quality score, and the prevalence of anxiety and depression. Funnel plot and Egger’s test were used to examine the publication bias. Sensitivity analysis examined the consistency of preliminary results by excluding studies one by one. Significant level was set at p < 0.05 (two-tailed).
3 Results
3.1 Search results and study characteristics
A total of 4,238 relevant publications were initially searched and finally, 36 studies met the study entry criteria and were included in this meta-analysis, of which there were 24 epidemiological and 12 comparative studies (Supplementary Figure S1). After reading the titles and abstracts initially, 293 articles were screened for eligibility by reading the full text, of which, 256 articles were excluded. The reasons for exclusion are outlined in Supplementary Table S2.
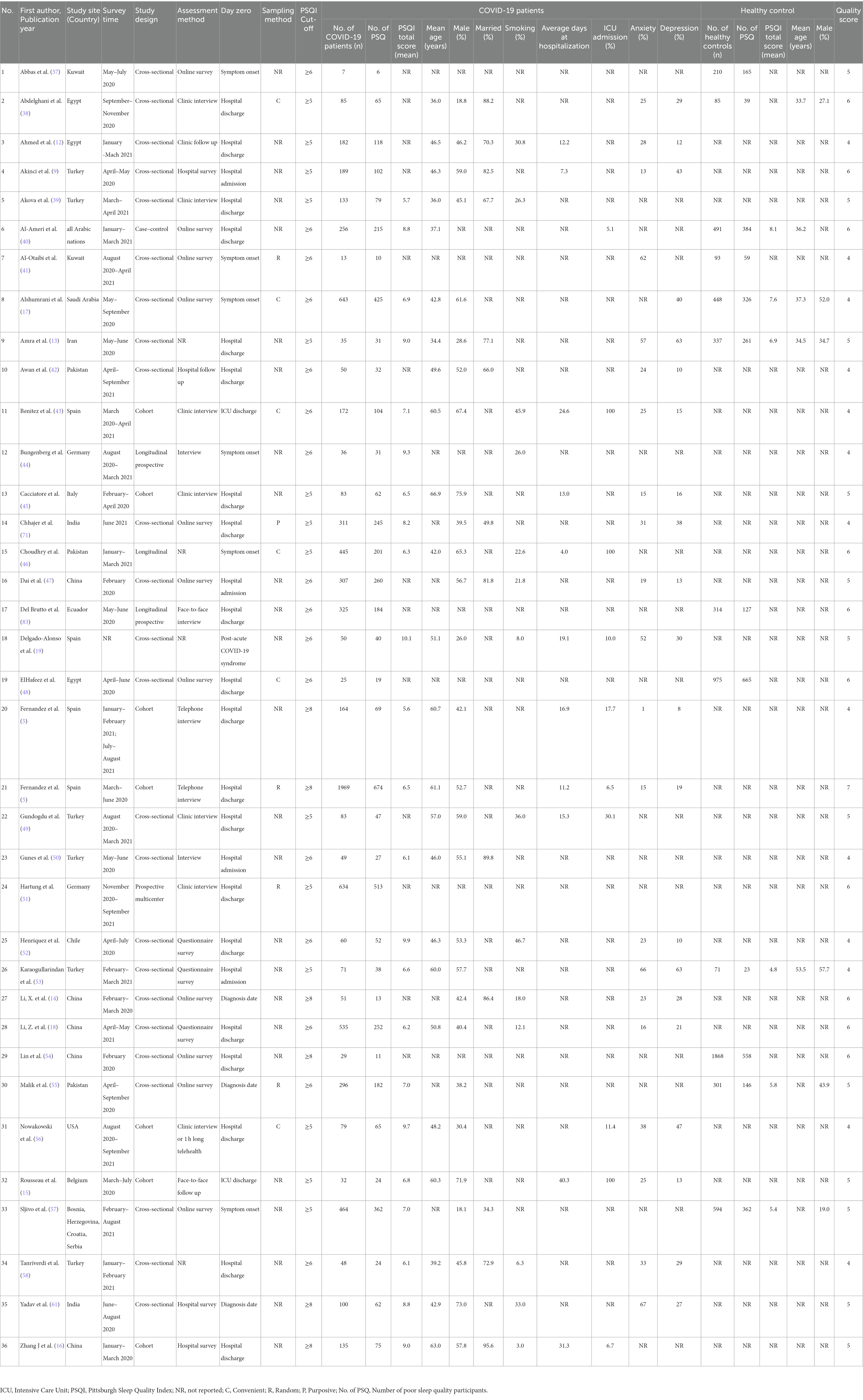
A total of 8,146 COVID-19 patients and 5,787 healthy controls were included in this study and their basic characteristics are shown in Table 1. The age range of the participants were between 18 and 99 years. The most number of studies were conducted in Turkey (6 studies, 16.7%), followed by China (5 studies, 13.9%) and Spain (4 studies, 11.1%). Most of the included studies were cross-sectional (26 studies, 72.2%), followed by cohort studies (6 studies, 19.4%). All studies used the PSQI as the measure on sleep quality; 16 studies used the PSQI cut-off values of ≥6 (44.4%), while 14 studies used the cut-off values of ≥5 (38.9%) and 6 studies used the cut-off values of ≥8 (16.7%). Twenty-one studies reported comorbid anxiety and depression, respectively. The study quality assessment scores of 24 epidemiological studies ranged from 4 to 7, of which only 1 study was rated as “high quality,” and the remaining 23 studies (95.8%) were rated as “moderate quality.” In addition, quality assessment scores of the 12 comparative studies ranged from 4 to 6, with a mean score of 5.1 (SD: 0.8) (Supplementary Table S1).
3.2 Pooled prevalence of poor sleep quality, PSQI global and component score in COVID-19 patients
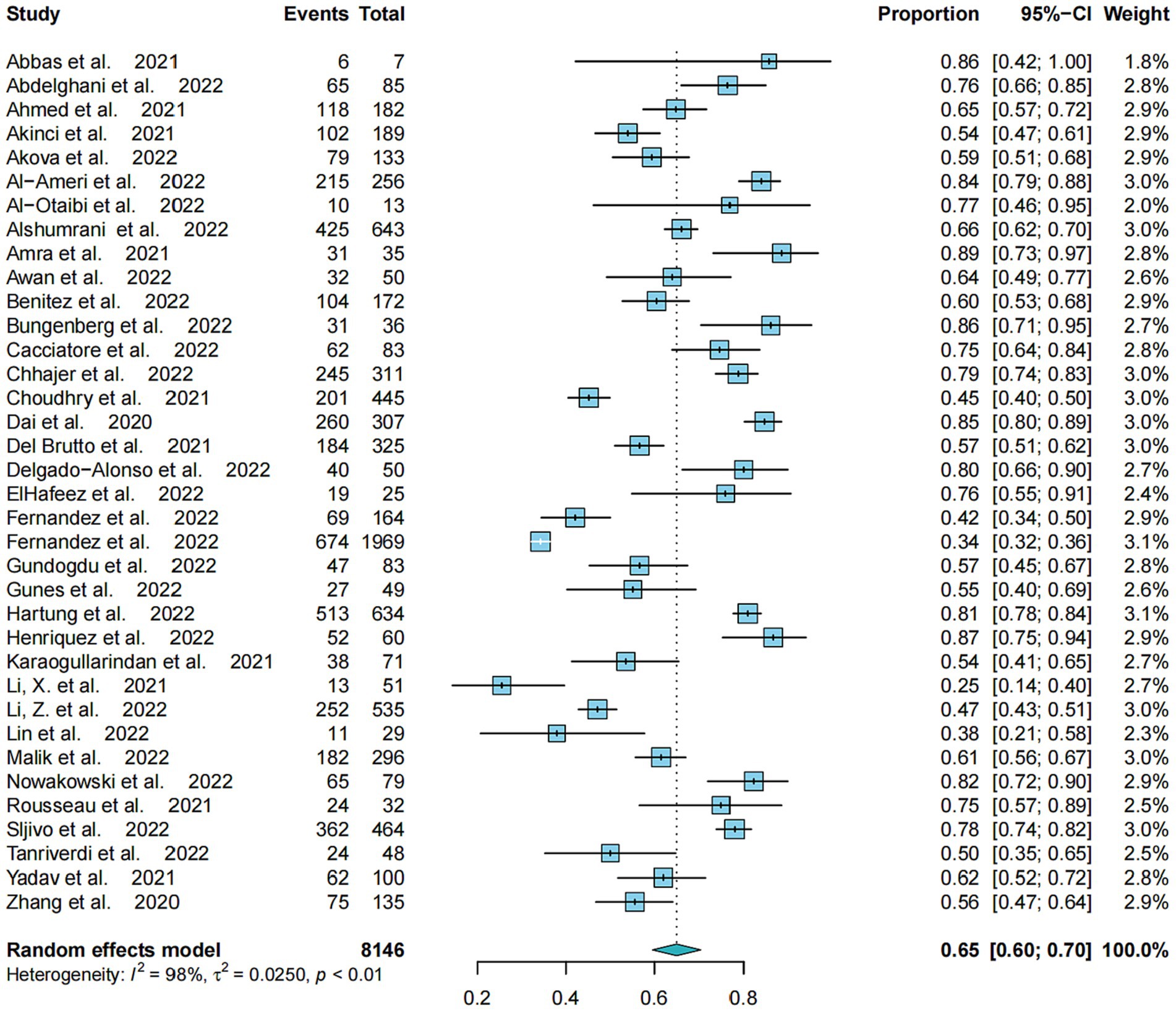
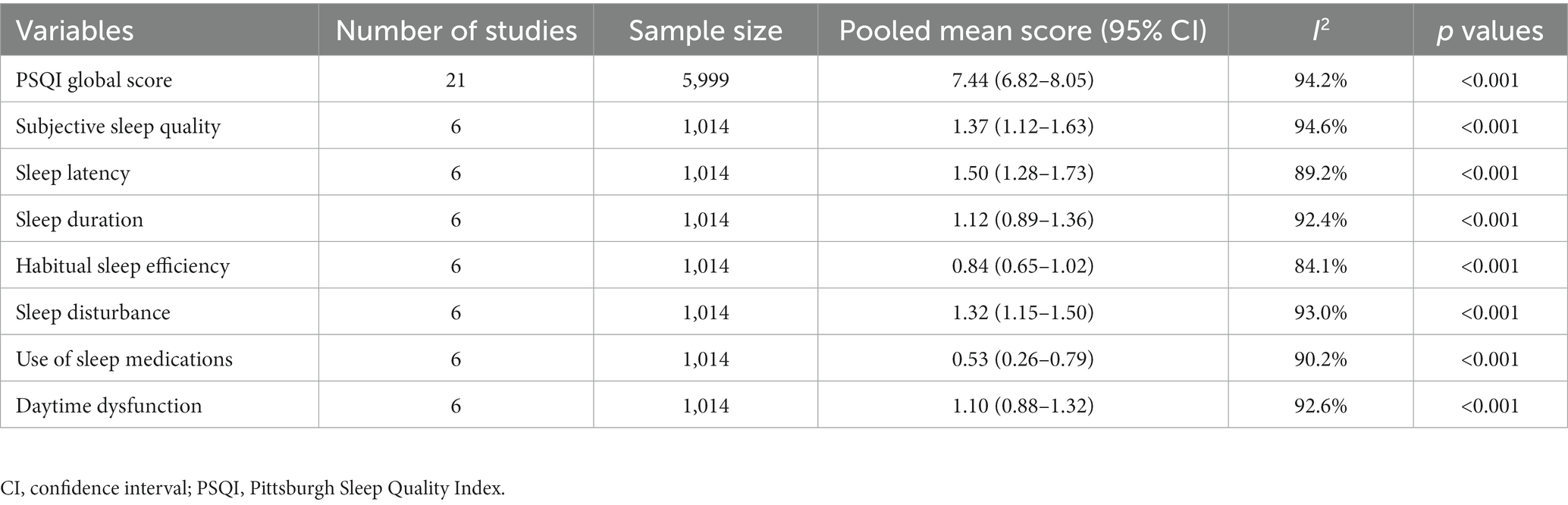
The pooled prevalence of poor sleep quality based on all 36 studies was 65.0% (95%CI: 59.56–70.44%, I2 = 97.6%) (Figure 1). Table 2 shows that a total of 21 studies with 5,999 COVID-19 patients reported on the total PSQI score, with a pooled total PSQI score of 7.44 (95% CI: 6.82–8.05, I2 = 94.2%). In addition, 6 studies with 1,014 COVID-19 patients reported on the sleep component scores in seven domains, with pooled data ranging from 0.53 (95% CI: 0.26–0.79, I2 = 90.2%) for “use of sleep medications” to 1.50 (95% CI: 1.28–1.73, I2 = 89.2%) for “sleep latency.”
3.3 Odds ratio for poor sleep quality between COVID-19 patients and healthy controls
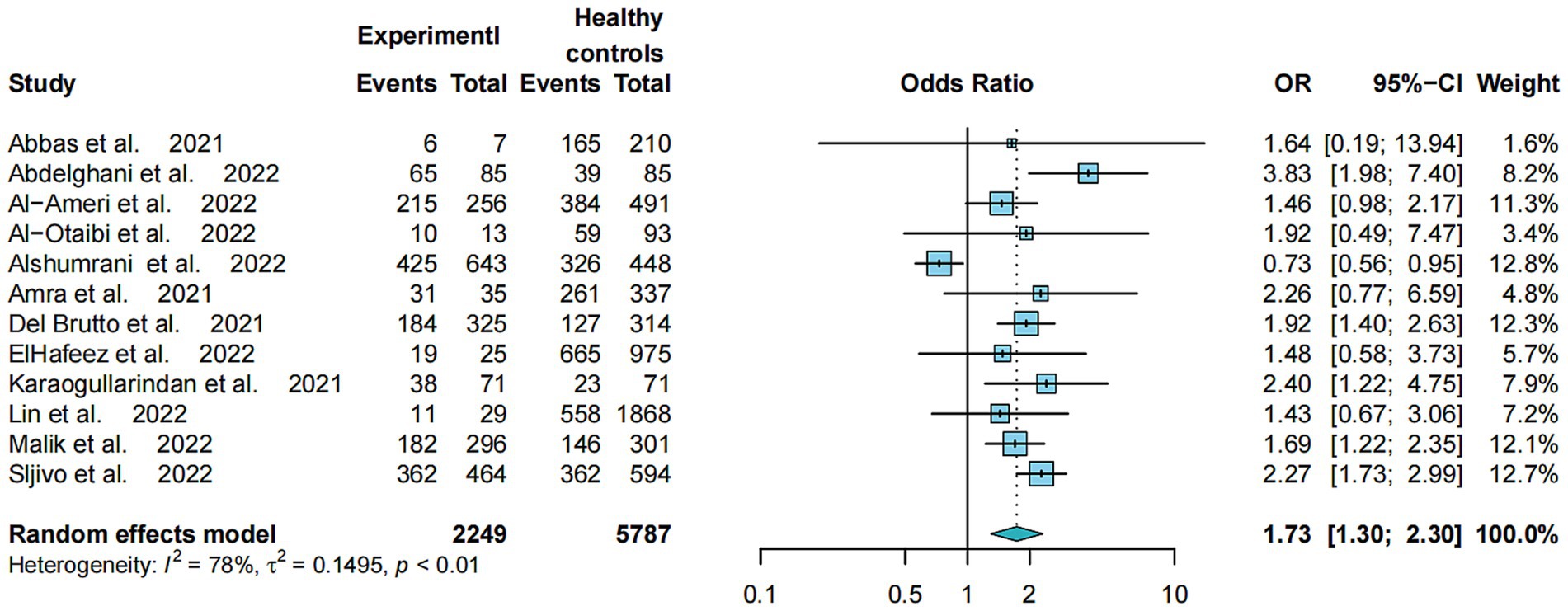
The Odds Ratio (OR) of the 12 comparative studies on the prevalence of poor sleep quality between COVID-19 patients and healthy controls is shown in Figure 2. Specifically, COVID-19 patients had a higher risk of poor sleep quality compared to healthy controls (OR = 1.73, 95% CI: 1.30–2.30, p < 0.01, I2 = 78.1%). Moreover, COVID-19 patients had significantly higher PSQI total scores than healthy controls, with a large effect size (SMD = 0.31, 95%CI: 0.07–0.55, p < 0.0001, I2 = 92%) (Supplementary Figure S3).
3.4 Subgroup and meta-regression analyses
The results of subgroup analysis showed that the cut-offs of PSQI (p < 0.001) and countries by income (p = 0.011) were significantly associated with the prevalence of poor sleep quality in COVID-19 patients. COVID-19 patients in lower middle-income countries were more likely to have poor sleep quality than those in upper middle income and high-income countries (64.9% vs. 60.1% vs. 55.8%). Meta-regression analyses of 24 epidemiological studies revealed that mean age (β = 1.0000, z = 42.6046, p < 0.001) and married status (β = 0.0016, z = 2.6261, p = 0.009) were positively correlated with the prevalence of poor sleep quality in COVID-19 patients, while proportion of males (β = −0.0003, z = −2.0108, p = 0.044) and quality score (β = −0.0873, z = −2.4469, p = 0.014) were negatively correlated with the prevalence of poor sleep quality in COVID-19 patients (Table 3).
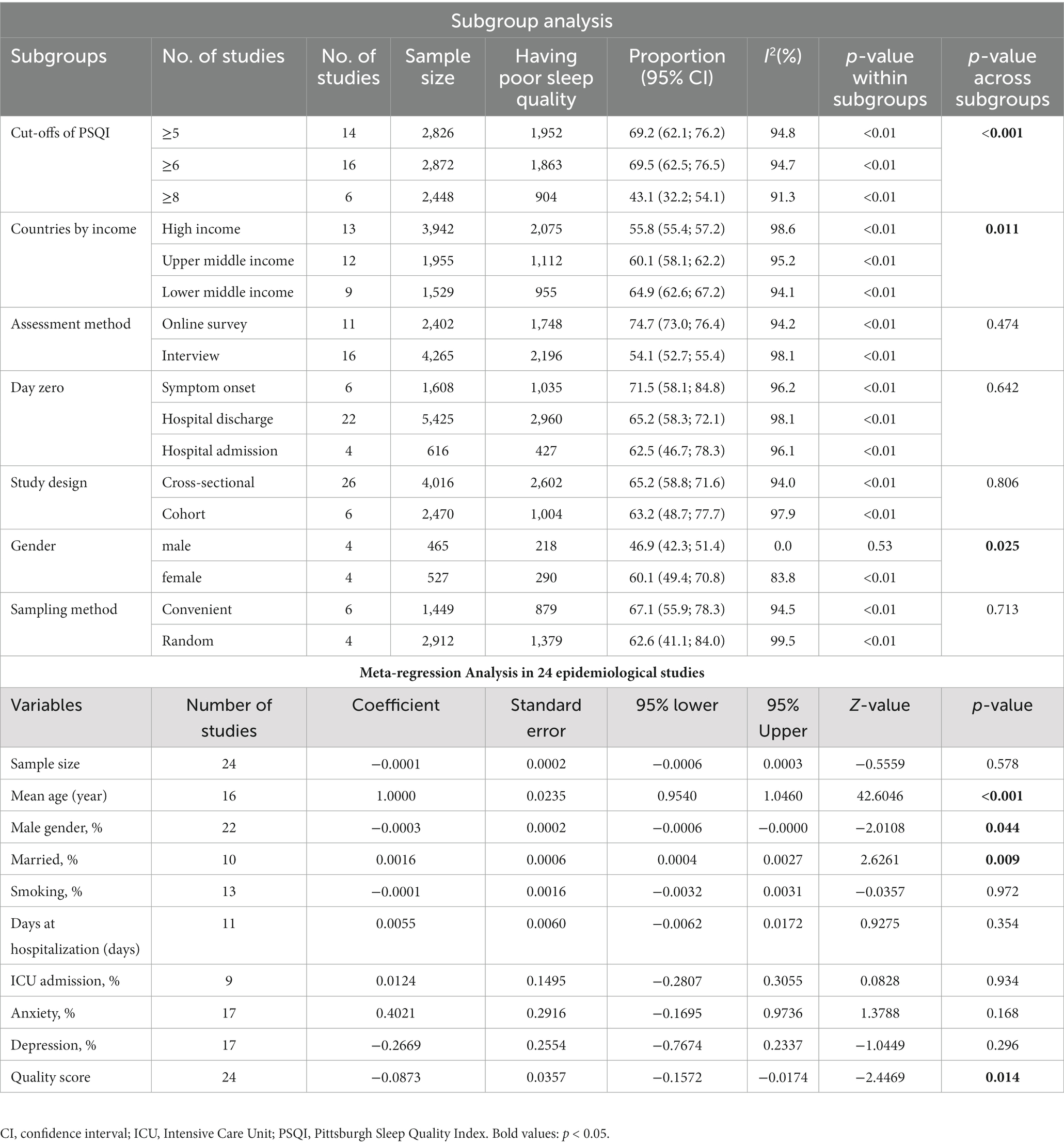
Table 3. Subgroup and meta-regression analyses of prevalence of poor sleep quality in COVID-19 patients.
3.5 Publication bias and sensitivity analyses
As shown in Supplementary Figures S2A,B, no publication bias was found in funnel plots. The Egger tests of the 36 studies (t = 1.41, p = 0.168) and the 12 comparative studies (t = 0.77, p = 0.457) also did not find any publication bias. Moreover, Supplementary Figures S4, S5 display the sensitivity analyses for the prevalence of poor sleep quality in the 36 studies and also the odds ratio in the 12 comparative studies, respectively. No outlying studies were found that could significantly alter the primary results.
4 Discussion
This is the first meta-analysis of the pooled prevalence of poor sleep quality in COVID-19 patients. The results showed that 65.0% (95%CI: 59.56–70.44%) of COVID-19 patients had poor sleep quality, which was around two times higher than that in healthy controls (OR = 1.73, 95%CI: 1.30–2.30). Globally, there were more than 757 million COVID-19 confirmed cases (59), which means that approximately 492 million COVID-19 patients suffered from poor sleep quality based on the prevalence rate found in this study. The COVID-19 pandemic had a profound impact on sleep quality in the population especially COVID-19 patients (11). A meta-analysis found that sleep problems were common and strongly associated with higher levels of psychological distress among health professionals, the general population, and COVID-19 patients during the COVID-19 pandemic (60). Another meta-analysis showed that sleep disturbances including poor sleep quality were higher among COVID-19 patients during lockdown periods compared with periods without lockdowns, and COVID-19 patients were the most affected subgroup (7). The high rate of sleep disturbances including poor sleep quality in COVID-19 patients may be related to several factors. First, sleep problems, including poor sleep quality, are among the main symptoms of COVID-19 infection (11). During the COVID-19 pandemic, the risk of mental health problems such as depression and anxiety increased, which had a negative impact on sleep quality of COVID-19 patients (27, 61). Second, those infected with COVID-19 are more likely to experience physical health problems (1, 2), such as fever, headache, dyspnea, myalgia, throat pain, cough, gastrointestinal disturbance, and other COVID-19 related symptoms (5, 6), which can affect immunological response and compromise sleep quality by altering related circadian rhythms (62). Moreover, many COVID-19 patients may suffer from impaired lung function and various sleep-related problems, such as obstructive sleep apnea, which affected sleep quality (63, 64). Third, usually COVID-19 patients are placed in long-term isolation treatment and tend to overuse their electronic devices during isolation causing chronic retinal irritation, which may lead to disturbance in sleep and circadian rhythm, and eventually poor sleep quality (65, 66). In addition, the strict lockdown measures can influence normal rhythms of the sleep–wake cycle among COVID-19 patients by reducing social activities and supports, increasing time spent in bed and delaying bedtimes (67, 68). As a result, depression, anxiety and insomnia are more likely to occur, thereby lowering their sleep quality (69, 70).
Subgroup analyses revealed that the prevalence of poor sleep quality in COVID-19 patients was higher in studies using PSQI cut-off value of 6 (69.5, 95% CI: 62.5–76.2%) compared to those using other PSQI cut-off values (e.g., cut-off of 8: 43.1, 95% CI: 32.2–54.1%), which is unsurprising given that a more stringent criterion for poor sleep quality would be associated with a lower prevalence rate. Poor sleep quality in COVID-19 patients in lower income countries (64.9, 95% CI: 62.6–67.2%) was more common than in higher income countries (e.g., upper middle income: 60.1, 95% CI: 58.1–62.2%; high income: 55.8, 95% CI: 55.4–57.2%), which could be explained by the fact that COVID-19 patients in low-income countries have less access to adequate and high-quality medical services compared to high-income countries (71). COVID-19 patients in high-income countries with advanced health system and greater resources tend to receive better care (72, 73) and have a lower mortality rate, which may also result in a lower risk of mental health problems such as anxiety, depression and insomnia among COVID-19 patients (72, 74, 75). In addition, both subgroup and meta-regression analyses revealed that women had a higher risk of poor sleep quality than men. This is consistent with previous findings that women are more likely to experience sleep problems than men such as poorer sleep quality, longer sleep latency periods, and more frequent use of sedative and hypnotic drugs (76). In addition, some studies found that women had more severe sleep difficulties than men during the COVID-19 pandemic due to shorter sleep duration and longer sleep latency (77, 78). This might be related to the finding that women are more susceptible than men to stress-related conditions (79, 80). A study conducted in Mexico found that the COVID-19 pandemic had different influences on women and men; for example, females reported more severe psychological distress, stress, and poorer sleep quality than males, probably related to the gender differences in response to stress, sensitivity to life events, and domestic and childcare responsibilities (81, 82).
Meta-regression analysis found more common poor sleep quality in older COVID-19 patients, which is consistent with previous research (83). There could be several reasons for this finding, first, older COVID-19 patients may have less outdoor activities and physical exercise, and spend more time in bed, leading to an increased risk of physical and psychological problems (84–86). Second, severe infection and morbidity rate are more common in older COVID-19 patients (87). Third, the likelihood of poor sleep quality and reduced sleep duration also increase with age. Meta-regression analysis also found that married COVID-19 patients had a higher risk of poor sleep quality. Compared to their unmarried counterparts, married COVID-19 patients may experience greater psychological pressure due to the fear of transmitting the virus to their family members, particularly children. Finally, higher quality studies were associated with a lower prevalence of poor sleep quality in COVID-19 patients. Stricter study design and more reliable measures were usually adopted in higher quality studies, which could reduce the likelihood of false positive rate and result in a lower prevalence of poor sleep quality.
The strengths of this meta-analysis included the large number of studies across different countries, inclusion of both epidemiological and comparative studies, and the use of sophisticated analyses such as subgroup, meta-regression, and sensitivity analyses. Additionally, all studies had used the PSQI to measure sleep quality, which would reduce the heterogeneity caused by different tools. However, several limitations of this study should be considered. First, due to the limited data, some factors related to sleep quality of COVID-19 patients could not be examined such as patients’ physical comorbidities, illness severity and treatment of COVID-19 patients. Second, due to differences in demographic data, COVID-19 related variables, sampling method and scale cutoff values between studies, heterogeneity could not be avoided in meta-analyses of epidemiological studies (88–91), even though subgroup analyses and meta-regression analyses were performed (92, 93). Finally, only published articles in English were included in this meta-analysis, which may bias the results of this study to an uncertain extent.
In conclusion, poor sleep quality was found to be very common in COVID-19 patients, especially in low-income countries, females, older adults and married patients. Considering the negative effects of poor sleep quality on daily life, sleep quality of COVID-19 patients should be assessed regularly, and effective treatments should be provided.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
ZG: Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Resources, Software, Writing – original draft. Y-YW: Data curation, Writing – review & editing. J-XL: Data curation, Writing – review & editing. X-HL: Data curation, Writing – review & editing. ZS: Data curation, Writing – review & editing. TC: Data curation, Writing – review & editing. K-IL: Data curation, Writing – review & editing. GU: Data curation, Writing – review & editing. CN: Data curation, Writing – review & editing. QZ: Writing – review & editing, Methodology. Y-TX: Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study was supported by the National Science and Technology Major Project for investigational new drug (2018ZX09201-014), the Beijing Hospitals Authority Clinical Medicine Development of special funding support (XMLX202128), and the University of Macau (MYRG2019-00066-FHS; MYRG2022-00187-FHS).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1272812/full#supplementary-material
Footnotes
References
1. Lee, JH, Lee, D, Hyun, S, Hong, JS, Kim, CH, Kim, W, et al. Online mental health assessments of COVID-19 patients in South Korea. Front Psych. (2021) 12:8. doi: 10.3389/fpsyt.2021.685445
2. Tjendra, Y, Al Mana, AF, Espejo, AP, Akgun, Y, Millan, NC, Gomez-Fernandez, C, et al. Predicting disease severity and outcome in COVID-19 patients. Arch Pathol Lab Med. (2020) 144:1465–74. doi: 10.5858/arpa.2020-0471-SA
3. Caroppo, E, Mazza, M, Sannella, A, Marano, G, Avallone, C, Claro, AE, et al. Will nothing be the same again?: Changes in lifestyle during COVID-19 pandemic and consequences on mental health. Int J Environ Res Public Health. (2021) 18:8433. doi: 10.3390/ijerph18168433
4. Kumar, N, and Gupta, R. Disrupted sleep during a pandemic. Sleep Med Clin. (2022) 17:41–52. doi: 10.1016/j.jsmc.2021.10.006
5. Fernández-de-las-Peñas, C, de-la-Llave-Rincón, AI, Ortega-Santiago, R, Ambite-Quesada, S, Gómez-Mayordomo, V, Cuadrado, ML, et al. Prevalence and risk factors of musculoskeletal pain symptoms as long-term post-COVID sequelae in hospitalized COVID-19 survivors: A multicenter study. Pain. (2022) 163:E989–e996. doi: 10.1097/j.pain.0000000000002564
6. Tanriverdi, A, Savci, S, Kahraman, BO, and Ozpelit, E. Extrapulmonary features of post-COVID-19 patients: muscle function, physical activity, mood, and sleep quality. Ir J Med Sci. (2022) 191:969–75. doi: 10.1007/s11845-021-02667-3
7. Jiang, ZY, Zhu, PP, Wang, LY, Hu, Y, Pang, MF, Ma, SS, et al. Psychological distress and sleep quality of COVID-19 patients in Wuhan, a lockdown city as the epicenter of COVID-19. J Psychiatr Res. (2021) 136:595–602. doi: 10.1016/j.jpsychires.2020.10.034
8. Zhang, L, Li, TT, Chen, LK, Wu, F, Xia, WG, Huang, M, et al. Association of sleep quality before and after SARS-COV-2 infection with clinical outcomes in hospitalized patients with Covid-19 in China. EXCLI J. (2021) 20:894–906. doi: 10.17179/excli2021-3451
9. Akinci, T, and Basar, HM. Relationship between sleep quality and the psychological status of patients hospitalised with COVID-19. Sleep Med. (2021) 80:167–70. doi: 10.1016/j.sleep.2021.01.034
10. De Mello, MT, Silva, A, Guerreiro, RD, da-Silva, FR, Esteves, AM, Poyares, D, et al. Sleep and COVID-19: considerations about immunity, pathophysiology, and treatment. Sleep Sci. (2020) 13:199–209. doi: 10.5935/1984-0063.20200062
11. Bhat, S, and Chokroverty, S. Sleep disorders and COVID-19. Sleep Med. (2022) 91:253–61. doi: 10.1016/j.sleep.2021.07.021
12. Ahmed, GK, Khedr, EM, Hamad, DA, Meshref, TS, Hashem, MM, and Aly, MM. Long term impact of Covid-19 infection on sleep and mental health: a cross-sectional study. Psychiatry Res. (2021) 305:114243. doi: 10.1016/j.psychres.2021.114243
13. Amra, B, Salmasi, M, Soltaninejad, F, Sami, R, Nickpour, M, Mansourian, M, et al. Healthcare workers' sleep and mood disturbances during COVID-19 outbreak in an Iranian referral center. Sleep Breath. (2021) 25:2197–204. doi: 10.1007/s11325-021-02312-4
14. Li, X, Cai, Q, Jia, Z, Liu, L, Zhou, Y, Zhang, B, et al. The correlation between mental health status, sleep quality, and inflammatory markers, virus negative conversion time among patients confirmed with 2019-nCoV during the COVID-19 outbreak in China An observational study. Medicine (United States). (2021) 100:e26520. doi: 10.1097/MD.0000000000026520
15. Rousseau, AF, Minguet, P, Colson, C, Kellens, I, Chaabane, S, Delanaye, P, et al. Post-intensive care syndrome after a critical COVID-19: Cohort study from a Belgian follow-up clinic. Ann Intensive Care. (2021) 11:118. doi: 10.1186/s13613-021-00910-9
16. Zhang, J, Xu, D, Xie, B, Zhang, Y, Huang, H, Liu, H, et al. Poor-sleep is associated with slow recovery from lymphopenia and an increased need for ICU care in hospitalized patients with COVID-19: A retrospective cohort study. Brain Behav Immun. (2020) 88:50–8. doi: 10.1016/j.bbi.2020.05.075
17. Alshumrani, R, Qanash, S, Aldobyany, A, Alhejaili, F, Alqassas, I, Shabrawishi, M, et al. Sleep quality and mental health in coronavirus disease 2019 patients and general population during the pandemic. Ann Thoracic Med. (2022) 17:21–7. doi: 10.4103/atm.atm_191_21
18. Li, Z, He, J, Wang, Y, Bai, M, Zhang, Y, Chen, H, et al. A cross-sectional study on the mental health of patients with COVID-19 1 year after discharge in Huanggang, China. Eur Arch Psych Clin Neurosci. (2022) 273:301–10. doi: 10.1007/s00406-022-01484-8
19. Delgado-Alonso, C, Valles-Salgado, M, Delgado-Alvarez, A, Yus, M, Gomez-Ruiz, N, Jorquera, M, et al. Cognitive dysfunction associated with COVID-19: A comprehensive neuropsychological study. J Psychiatr Res. (2022) 150:40–6. doi: 10.1016/j.jpsychires.2022.03.033
20. Thakur, M, Datusalia, AK, and Kumar, A. Use of steroids in COVID-19 patients: A meta-analysis. Eur J Pharmacol. (2022) 914:174579. doi: 10.1016/j.ejphar.2021.174579
21. Srivastava, R, and Kumar, A. Use of aspirin in reduction of mortality of COVID-19 patients: A meta-analysis. Int J Clin Pract. (2021) 75:7. doi: 10.1111/ijcp.14515
22. Thakur, M, Babu, A, Khatik, GL, Datusalia, AK, Khatri, R, and Kumar, A. Role of baricitinib in COVID-19 patients: A systematic review and meta-analysis. World J Meta-Anal. (2023) 11:125–33. doi: 10.13105/wjma.v11.i4.125
23. Moher, D, Liberati, A, Tetzlaff, J, Altman, DG, and Grp, P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:6. doi: 10.1371/journal.pmed.1000097
24. Stroup, DF, Berlin, JA, Morton, SC, Olkin, I, Williamson, GD, Rennie, D, et al. Meta-analysis of observational studies in epidemiology - A proposal for reporting. J Am Med Assoc. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
25. Scarpelli, S, Zagaria, A, Ratti, PL, Albano, A, Fazio, V, Musetti, A, et al. Subjective sleep alterations in healthy subjects worldwide during COVID-19 pandemic: A systematic review, meta-analysis and meta- regression. Sleep Med. (2022) 100:89–102. doi: 10.1016/j.sleep.2022.07.012
26. Alkodaymi, MS, Omrani, OA, Fawzy, NA, Abou Shaar, B, Almamlouk, R, Riaz, M, et al. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: a systematic review and meta-analysis. Clin Microbiol Infect. (2022) 28:657–66. doi: 10.1016/j.cmi.2022.01.014
27. Deng, JW, Zhou, FW, Hou, WT, Silver, Z, Wong, CY, Chang, O, et al. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci. (2021) 1486:90–111. doi: 10.1111/nyas.14506
28. Zhou, YF, Yang, Y, Shi, TY, Song, YZ, Zhou, YN, Zhang, ZB, et al. Prevalence and demographic correlates of poor sleep quality among frontline health professionals in Liaoning Province, China during the COVID-19 outbreak. Front Psych. (2020) 11:6. doi: 10.3389/fpsyt.2020.00520
29. Sedov, ID, Cameron, EE, Madigan, S, and Tomfohr-Madsen, LM. Sleep quality during pregnancy: A meta-analysis. Sleep Med Rev. (2018) 38:168–76. doi: 10.1016/j.smrv.2017.06.005
30. Boyle, MH. Guidelines for evaluating prevalence studies. Evid Based Mental Health. (1998) 1:37–9. doi: 10.1136/ebmh.1.2.37
31. Dong, M, Lu, L, Zhang, L, Zhang, QG, Ungvari, GS, Ng, CH, et al. Prevalence of suicide attempts in bipolar disorder: a systematic review and meta-analysis of observational studies. Epidemiol Psychiatr Sci. (2020) 29:9. doi: 10.1017/S2045796019000593
32. Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
33. Institute of Medical Biometry and Statistics. R packages. (2023). Available at: http://www.imbi.uni-freiburg.de/lehre/lehrbuecher/meta-analysis-with-r/r-packages (Accessed February 22, 2023).
34. Higgins, JPT, Thompson, SG, Deeks, JJ, and Altman, DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
35. Vaseghi, N, Sharifisooraki, J, Khodadadi, H, Nami, S, Safari, F, Ahangarkani, F, et al. Global prevalence and subgroup analyses of coronavirus disease (COVID-19) associated Candida auris infections (CACa): A systematic review and meta-analysis. Mycoses. (2022) 65:683–703. doi: 10.1111/myc.13471
36. Akiyama, S, Hamdeh, S, Micic, D, and Sakuraba, A. Prevalence and clinical outcomes of COVID-19 in patients with autoimmune diseases: a systematic review and meta-analysis. Ann Rheum Dis. (2021) 80:384–91. doi: 10.1136/annrheumdis-2020-218946
37. Abbas, A, Al-Otaibi, T, Gheith, OA, Nagib, AM, Farid, MM, and Walaa, M. Sleep quality among healthcare workers during the covid-19 pandemic and its impact on medical errors: Kuwait experience. Turkish Thoracic Journal. (2021) 22:142–8.
38. Abdelghani, M, Alsadik, M, Abdelmoaty, A, Atwa, S, Said, A, and Hassan, M. Sleep disturbances following recovery from COVID-19: a comparative cross-sectional study in Egypt. Eastern Mediterranean Health Journal. (2022) 28:14–22.
39. Akova, I, and Gedikli, MA. Fatigue and Sleep Quality Levels of Post-COVID-19 Healthcare Workers and Affecting Factors. International Journal of Academic Medicine and Pharmacy. (2022) 4:65–9.
40. Al-Ameri, LT, Hameed, EK, and Maroof, BS. Sleep quality in COVID-19 recovered patients. Sleep Science. (2022) 15:168–71.
41. Al-Otaibi, T, Abbas, A, Nagib, AM, Gheith, OA, Nair, P, Farid, MM, et al. COVID-somnia: anxiety, insomnia, and poor sleep among second-line healthcare workers during COVID-19 pandemic. EGYPTIAN JOURNAL OF BRONCHOLOGY. (2022) 16
42. Awan, I, Balouch, AH, Juseja, AK, Lakho, MA, and Shaikh, A. Long Term Impact of COVID-19 Infection on Sleep and Mental Health. Pakistan Journal of Medical and Health Sciences. (2022) 16:102–4.
43. Benitez, ID, Moncusi-Moix, A, Vaca, R, Gort-Paniello, C, Minguez, O, Santisteve, S, et al. Sleep and Circadian Health of Critical COVID-19 Survivors 3 Months After Hospital Discharge. Critical care medicine. (2022) 50:945–54.
44. Bungenberg, J, Humkamp, K, Hohenfeld, C, Rust, MI, Ermis, U, Dreher, M, et al. Long COVID-19: Objectifying most self-reported neurological symptoms. Annals of Clinical and Translational Neurology. (2022) 9:141–54.
45. Cacciatore, M, Raggi, A, Pilotto, A, Cristillo, V, Guastafierro, E, Toppo, C, et al. Neurological and Mental Health Symptoms Associated with Post-COVID-19 Disability in a Sample of Patients Discharged from a COVID-19 Ward: A Secondary Analysis. International Journal of Environmental Research and Public Health. (2022) 19:4242.
46. Choudhry, AA, Shahzeen, F, Choudhry, SA, Batool, N, Murtaza, F, Dilip, A, et al. Impact of COVID-19 Infection on Quality of Sleep. Cureus. (2021) 13:e18182
47. Dai, LL, Wang, X, Jiang, TC, Li, PF, Wang, Y, Wu, SJ, et al. Anxiety and depressive symptoms among COVID-19 patients in Jianghan Fangcang Shelter Hospital in Wuhan, China. PLoS ONE. (2020) 15:e0238416.
48. ElHafeez, SA, Meira e Cruz, M, Gouda, S, Nofal, M, Fayed, A, Ghazy, RM, et al. Sleep quality and anxiety among Egyptian population during covid-19 pandemic. Sleep. Science. (2022) 15:8–16.
49. Gundogdu, N, and Tanriverdi, M. Sleep Quality of Patients with COVID-19 after Hospital Discharge. Progress in Nutrition. (2022) 24:e2022059
50. Gunes, A, and Sensoy, B. Sleepiness, Insomnia, and Sleep Quality of Hospitalized Patients with Coronavirus Disease-2019: Sleep Scale Evaluation. Journal of Turkish Sleep Medicine. (2022) 9:11–5.
51. Hartung, TJ, Neumann, C, Bahmer, T, Chaplinskaya-Sobol, I, Endres, M, Geritz, J, et al. Fatigue and cognitive impairment after COVID-19: A prospective multicentre study. EClinicalMedicine. (2022) 53:101651
52. Henriquez-Beltran, M, Labarca, G, Cigarroa, I, Enos, D, Lastra, J, Nova-Lamperti, E, et al. Sleep health and the circadian rest-activity pattern four months after COVID-19. Jornal Brasileiro de Pneumologia. (2022) 48:e20210398
53. Karaogullarindan, A, Erkan, SO, Tuhanioglu, B, Kuran, G, and Gorgulu, O. Sleep quality in patients over 65 years of age in the covid-19 pandemic. Turk Geriatri Dergisi. (2021) 24:381–90.
54. Lin, Y, Liu, S, Li, S, Zuo, H, and Zhang, B. Relationships between the changes in sleep patterns and sleep quality among Chinese people during the 2019 coronavirus disease outbreak. Sleep Medicine. (2022) 91:154–60.
55. Malik, M, Atiq, A, Tahir, MJ, Akhtar, FK, Malik, MI, Hassan, W, et al. Comparison of sleep quality among COVID-19 patients and non-COVID-19 population in Pakistan: A cross sectional study during the COVID-19 pandemic. Annals of Medicine and Surgery. (2022) 78:103894
56. Nowakowski, S, Kokonda, M, Sultana, R, Duong, BB, Nagy, SE, Zaidan, MF, et al. Association between Sleep Quality and Mental Health among Patients at a Post-COVID-19 Recovery Clinic. Brain Sciences. (2022) 12:586.
57. Sljivo, A, Juginovic, A, Ivanovic, K, Quraishi, I, Mulac, A, Kovacevic, Z, et al. Sleep quality and patterns of young West Balkan adults during the third wave of COVID-19 pandemic: A cross-sectional study. BMJ Open. (2022) 12:e060381
58. Tanriverdi, A, Savci, S, Kahraman, BO, and Ozpelit, E. Extrapulmonary features of post-COVID-19 patients: muscle function, physical activity, mood, and sleep quality. Irish Journal of Medical Science. (2022) 191:969–75.
59. World Health Organization. (2023). Coronavirus disease (COVID-2019) situation reports. Available at: https://www.who.int (Accessed March 1, 2023).
60. Alimoradi, Z, Broström, A, Tsang, HWH, Griffiths, MD, Haghayegh, S, Ohayon, MM, et al. Sleep problems during COVID-19 pandemic and its' association to psychological distress: A systematic review and meta-analysis. EClinicalMedicine. (2021) 36:100916. doi: 10.1016/j.eclinm.2021.100916
61. Yadav, R, Yadav, P, Kumar, SS, and Kumar, R. Assessment of depression, anxiety, and sleep disturbance in COVID-19 patients at Tertiary Care Centre of North India. J Neurosci Rural Pract. (2021) 12:316–22. doi: 10.1055/s-0040-1722811
62. Silva, E, Ono, BVS, and Souza, JC. Sleep and immunity in times of COVID-19. Rev Assoc Med Bras. (2020) 66:143–7. doi: 10.1590/1806-9282.66.s2.143
63. Voncken, SFJ, Feron, TMH, Laven, S, Karaca, U, Beerhorst, K, Klarenbeek, P, et al. Impact of obstructive sleep apnea on clinical outcomes in patients hospitalized with COVID-19. Sleep Breath. (2022) 26:1399–407. doi: 10.1007/s11325-021-02476-z
64. Beltramo, G, Cottenet, J, Mariet, AS, Georges, M, Piroth, L, Tubert-Bitter, P, et al. Chronic respiratory diseases are predictors of severe outcome in COVID-19 hospitalised patients: a nationwide study. Eur Resp J. (2021) 58:2004474. doi: 10.1183/13993003.04474-2020
65. Ma, J, Hua, TT, Zeng, K, Zhong, BL, Wang, G, and Liu, XB. Influence of social isolation caused by coronavirus disease 2019 (COVID-19) on the psychological characteristics of hospitalized schizophrenia patients: a case-control study. Transl Psychiatry. (2020) 10:5. doi: 10.1038/s41398-020-01098-5
66. Zhen, R, Li, L, Li, GQ, and Zhou, X. Social Isolation, loneliness, and mobile phone dependence among adolescents during the COVID-19 pandemic: roles of parent-child communication patterns. Int J Mental Health Addict. (2021) 21:1931–45. doi: 10.1007/s11469-021-00700-1
67. Barateau, L, Chenini, S, Rassu, AL, Denis, C, Lorber, Q, Dhalluin, C, et al. Changes in sleep pattern during the COVID-19 lockdown in patients with narcolepsy, idiopathic hypersomnia, and restless legs syndrome. Neurology. (2022) 99:E1475–e1485. doi: 10.1212/WNL.0000000000200907
68. Sun, NN, Wei, LQ, Wang, HY, Wang, XR, Gao, MX, Hu, XJ, et al. Qualitative study of the psychological experience of COVID-19 patients during hospitalization. J Affect Disord. (2021) 278:15–22. doi: 10.1016/j.jad.2020.08.040
69. Gordon, JM, Magbee, T, and Yoder, LH. The experiences of critical care nurses caring for patients with COVID-19 during the 2020 pandemic: A qualitative study. Appl Nurs Res. (2021) 59:151418. doi: 10.1016/j.apnr.2021.151418
70. González-Hijón, J, Kähler, AK, Frans, EM, Valdimarsdóttir, UA, Sullivan, PF, Fang, F, et al. Unravelling the link between sleep and mental health during the COVID-19 pandemic. Stress Health. (2023) 39:828–40. doi: 10.1002/smi.3223
71. Chhajer, R, and Shukla, SD. Sleep quality of Covid-19 recovered patients in India. Neurosci Insights. (2022) 17:263310552211091. doi: 10.1177/26331055221109174
72. Shapiro, GK, Gottfredson, N, Leask, J, Wiley, K, Ganter-Restrepo, FE, Jones, SP, et al. COVID-19 and missed or delayed vaccination in 26 middle- and high-income countries: An observational survey. Vaccine. (2022) 40:945–52. doi: 10.1016/j.vaccine.2021.12.041
73. Kaadan, MI, Abdulkarim, J, Chaar, M, Zayegh, O, and Keblawi, MA. Determinants of COVID-19 vaccine acceptance in the Arab world: a cross-sectional study. Glob Health Res Policy. (2021) 6:7. doi: 10.1186/s41256-021-00202-6
74. Cai, R, Novosad, P, Tandel, V, Asher, S, and Malani, A. Representative estimates of COVID-19 infection fatality rates from four locations in India: cross-sectional study. BMJ Open. (2021) 11:e050920. doi: 10.1136/bmjopen-2021-050920
75. Tyler, CM, McKee, GB, Alzueta, E, Perrin, PB, Kingsley, K, Baker, FC, et al. A study of older adults' mental health across 33 countries during the COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18:15. doi: 10.3390/ijerph18105090
76. Middelkoop, HAM, SmildevandenDoel, DA, Neven, AK, Kamphuisen, HA, and Springer, CP. Subjective sleep characteristics of 1,485 males and females aged 50-93: Effects of sex and age, and factors related to self-evaluated quality of sleep. J Gerontol ABiol Sci Med Sci. (1996) 51:M108–15. doi: 10.1093/gerona/51A.3.M108
77. Qiu, JY, Shen, B, Zhao, M, Wang, Z, Xie, B, and Xu, YF. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiat. (2020) 33:3. doi: 10.1136/gpsych-2020-100213
78. Losada-Baltar, A, Jiménez-Gonzalo, L, Gallego-Alberto, L, Pedroso-Chaparro, MD, Fernandes-Pires, J, and Márquez-González, M. "We Are Staying at Home." Association of self-perceptions of aging, personal and family resources, and loneliness with psychological distress during the lock-down period of COVID-19. J Gerontol Ser B Psychol Sci Soc Sci. (2021) 76:E10–e16. doi: 10.1093/geronb/gbaa048
79. Li, SH, and Graham, BM. Why are women so vulnerable to anxiety, trauma-related and stress-related disorders? The potential role of sex hormones. Lancet Psychiatry. (2017) 4:73–82. doi: 10.1016/S2215-0366(16)30358-3
80. Hohagen, F, Rink, K, Kappler, C, Schramm, E, Riemann, D, Weyerer, S, et al. Prevalence and treatment of insomnia in general-practice-a longitudinal-study. Eur Arch Psych Clin Neurosci. (1993) 242:329–36. doi: 10.1007/BF02190245
81. Cellini, N, Conte, F, De Rosa, O, Giganti, F, Malloggi, S, Reyt, M, et al. Changes in sleep timing and subjective sleep quality during the COVID-19 lockdown in Italy and Belgium: age, gender and working status as modulating factors. Sleep Med. (2021) 77:112–9. doi: 10.1016/j.sleep.2020.11.027
82. Vuelvas-Olmos, CR, Sanchez-Vidana, DI, and Cortes-Alvarez, NY. Gender-based analysis of the association between mental health, sleep quality, aggression, and physical activity among university students during the COVID-19 outbreak. Psychol Rep. (2022) 126:2212–36. doi: 10.1177/00332941221086209
83. Del Brutto, OH, Mera, RM, Costa, AF, Recalde, BY, and Castillo, PR. Sleep quality deterioration in middle-aged and older adults living in a rural Ecuadorian village severely struck by the SARS-CoV-2 pandemic. A population-based longitudinal prospective study. Sleep. (2021) 44:10.1093/sleep/zsab041:6.
84. Dayaramani, C, De Leon, J, and Reiss, AB. Cardiovascular disease complicating COVID-19 in the elderly. Medicina-Lithuania. (2021) 57:22. doi: 10.3390/medicina57080833
85. Dai, LS, Xiong, F, and Li, WT. The impact of social quarantine on the living status and mental health of the elderly in the Wuhan community: one year after Wuhan COVID-19 blockade. BMC Geriatr. (2022) 22:8. doi: 10.1186/s12877-022-03560-z
86. Lee, DY, Cho, J, You, SC, Park, RW, Kim, CS, Lee, EY, et al. Risk of mortality in elderly coronavirus disease 2019 patients with mental health disorders: a nationwide retrospective study in South Korea. Am J Geriatr Psychiatr. (2020) 28:1308–16. doi: 10.1016/j.jagp.2020.09.016
87. Wang, L, He, WB, Yu, XM, Hur, DL, Bao, MW, Liu, HF, et al. Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up. J Infect. (2020) 80:639–45. doi: 10.1016/j.jinf.2020.03.019
88. Rotenstein, LS, Ramos, MA, Torre, M, Segal, JB, Peluso, MJ, Guille, C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students a systematic review and meta-analysis. J Am Med Assoc. (2016) 316:2214–36. doi: 10.1001/jama.2016.17324
89. Zeng, LN, Zong, QQ, Yang, Y, Zhang, L, Xiang, YF, Ng, CH, et al. Gender difference in the prevalence of insomnia: a meta-analysis of observational studies. Front Psych. (2020) 11:9. doi: 10.3389/fpsyt.2020.577429
90. Rao, WW, Zhu, XM, Zong, QQ, Zhang, QG, Hall, BJ, Ungvari, GS, et al. Prevalence of prenatal and postpartum depression in fathers: A comprehensive meta-analysis of observational surveys. J Affect Disord. (2020) 263:491–9. doi: 10.1016/j.jad.2019.10.030
91. Mata, DA, Ramos, MA, Bansal, N, Khan, R, Guille, C, Di Angelantonio, E, et al. Prevalence of depression and depressive symptoms among resident physicians a systematic review and meta-analysis. J Am Med Assoc. (2015) 314:2373–83. doi: 10.1001/jama.2015.15845
92. Bai, W, Liu, ZH, Jiang, YY, Zhang, QE, Rao, WW, Cheung, T, et al. Worldwide prevalence of suicidal ideation and suicide plan among people with schizophrenia: a meta-analysis and systematic review of epidemiological surveys. Transl Psychiatry. (2021) 11:10. doi: 10.1038/s41398-021-01671-6
Keywords: COVID-19, sleep quality, meta-analysis, prevalence, review
Citation: Gui Z, Wang Y-Y, Li J-X, Li X-H, Su Z, Cheung T, Lok K-I, Ungvari GS, Ng CH, Zhang Q and Xiang Y-T (2024) Prevalence of poor sleep quality in COVID-19 patients: a systematic review and meta-analysis. Front. Psychiatry. 14:1272812. doi: 10.3389/fpsyt.2023.1272812
Edited by:
Akiyoshi Shimura, Tokyo Medical University, JapanReviewed by:
Haitham Jahrami, Arabian Gulf University, BahrainAnoop Kumar, Delhi Pharmaceutical Sciences and Research University, India
Copyright © 2024 Gui, Wang, Li, Li, Su, Cheung, Lok, Ungvari, Ng, Zhang and Xiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chee H. Ng, Y25nQHVuaW1lbGIuZWR1LmF1; Qinge Zhang, enFlODFAMTI2LmNvbQ==; Yu-Tao Xiang, eHl1dGx5QGdtYWlsLmNvbQ==
†These authors have contributed equally to this work
 Zhen Gui
Zhen Gui Yue-Ying Wang2†
Yue-Ying Wang2† Zhaohui Su
Zhaohui Su Teris Cheung
Teris Cheung Ka-In Lok
Ka-In Lok Gabor S. Ungvari
Gabor S. Ungvari Chee H. Ng
Chee H. Ng Qinge Zhang
Qinge Zhang Yu-Tao Xiang
Yu-Tao Xiang