- 1Department of Clinical and Experimental Medicine, University of Pisa, Pisa, Italy
- 2Department of Psychiatry, University of Campania “Luigi Vanvitelli”, Naples, Italy
- 3Department of Neuroscience, Mental Health and Sense Organs, University of Roma “La Sapienza”, Rome, Italy
- 4Department of Brain and Behavioral Sciences, University of Pavia, Pavia, Italy
- 5Department of Biomedical and Dental Sciences and Morphofunctional Imaging, University of Messina, Messina, Italy
- 6Department of Clinical and Experimental Sciences, University of Brescia, Brescia, Italy
Background: Recent literature has highlighted that catatonia may be more prevalent among psychiatric patients than previously thought, beginning from autism spectrum disorders (ASD), for which it has been suggested to represent a severe late consequence, but also among individuals with mood disorders and borderline personality disorder (BPD). Interestingly, one critical point shared by these conditions is the increased risk of suicidality. The aim of this study was to evaluate how the presence and the prevalence of catatonic symptoms may shape and correlate with suicidal risk in a sample of individuals with major depressive disorder (MDD) or BPD.
Methods: We recruited two clinical samples of subjects (BPD and MDD) and a control group without a diagnosis according to DSM-5 (CTL). Subjects were assessed with the catatonia spectrum (CS) and the MOODS-SR for evaluating suicidality.
Results: In the total sample, suicidality score was significantly and positively correlated with all CS domains and CS total score. Correlation and regression analyses highlighted specific patterns of association among Catatonia spectrum domains and suicidality in the MDD and BPD group and in the total sample.
Conclusion: In both disorders, higher catatonic traits are linked to higher suicidal tendencies, confirming the high risk of suicide for this population. However, different patterns of association between catatonic symptoms and suicidality were highlighted in the two disorders.
1. Introduction
The term “catatonia” was firstly introduced by Kahlbaum in 1874 (1) referring to a composite picture of behavioral and motor disturbances (such as negativism, mutism and automatisms) along with cognitive, affective and neurovegetative manifestations. Interestingly, Kahlbaum observed a high frequency of acute alterations of mood in catatonic subjects, of both polarities, underlined the similarity with manic-depressive psychosis (1). Today, the DSM-5-TR recognizes catatonia as a neuropsychiatric condition included in the chapter “Spectrum of Schizophrenia and Other Psychotic Disorders,” and characterized by the occurrence of three or more of 12 symptoms (stupor, catalepsy, waxy flexibility, negativism, fixed posture, mannerisms, stereotypes, agitation, presence of grimacing, echolalia, and echopraxia) (2). The DSM-5-TR features three main categories of catatonia: “catatonia associated with another mental disorder,” “catatonic disorder due to another medical condition,” and “catatonia without specification.” Even though the current categorization of catatonia still follows Bleuler conceptualization (3), over the years many authors argued that it should be recognized as a separate syndrome (4–6). Noticeably, catatonic symptoms may occur with a multitude of medical and organic brain conditions (7). Recent literature also highlighted that catatonia may be more prevalent among psychiatric patients than previously thought, in particular among younger patients (8, 9), patients with autism spectrum disorder (ASD) (10–14) and individuals with mood disorders rather than with non-affective disorders like schizophrenia (15); in particular, catatonic signs have been reported to be associated with mood disorders in 13% to 31% cases (16–18). One of the most recent studies reported also increased levels of catatonic symptoms in a sample of borderline personality disorder (BPD) patients, even higher that those found in patients with major depression disorder (MDD) (19). Interestingly, one of the most critical points shared by mood disorders and BPD is the increased risk of suicidality. On the other hand, the literature also reported a higher suicidal risk linked to catatonia, especially when of psychiatric origin (20, 21).
MDD with chronic course and recurrent episodes is a major affective disorder with a chronic course characterized by recurrent depressive episodes (2) known to be associated with a high risk for suicidality (22, 23). Catatonic symptoms have already been described in depressive state (24, 25) and in other mood disorders, especially with mixed states. In this framework two studies, reported a history of an index episode with mixed features in 61% and 73% catatonic patients, respectively (26, 27). Interestingly, patients with mixed states also typically show greater suicidal behavior and are at higher risk of suicide (28).
Another disorder with a well-known association with higher levels of self-injurious and suicidal behaviors is BPD (29, 30). BPD is characterized by a pervasive pattern of instability in different areas, in particular regarding emotional regulation, interpersonal relationships, self-image, and control of impulses (31). BPD is therefore an extremely relevant disorder associated with severe functional impairment and high rates of suicide, affecting almost 20% and 10% of psychiatric in- and out-patients, respectively (29, 30). Despite seeming quite different, the recent literature increasingly reported significant overlaps between BPD and ASD. For instance, although being characteristics of BPD, strong relationships and superficial friendships, as well as the propensity to acting out instead of verbalizing emotions, are also prevalent in ASD (32). In a similar way, while essential characteristics of ASD, impairments in verbal and nonverbal communication, social functioning, incorrect assumptions about intentions, and emotional outbursts are also frequently documented in BPD subjects (33–40). Other traits shared by BPD and ASD are a high proportion of self-harming behaviors (32), pervasive patterns of emotional dysregulation (41, 42) and difficulties in the Theory of Mind (43). On the other hand, to date, the pathophysiology of BPD is still relatively unexplored, and its correlation with ASD is based mainly on the shared clinical and psychological features. However, evidences from some researches may suggest that ASD and BDP may share similar neurobiological alteration such as an atypical functionality of the hypothalamus-pituitary-adrenal (HPA) axis that has been widely reported in both disorders (44–46) and an alteration of the endocannabinoid and oxytocin system, which are important for the emotional regulation and social interaction (47, 48).
In this framework, it is interesting to acknowledge that catatonic symptoms and autistic traits have been found to be particularly prevalent on the BPD population (19, 49, 50). Moreover, previous studies already reported how in both BPD and catatonia a higher prevalence of autistic traits would be associated with a greater severity of the manifestations and an increased suicidal risk (51–53).
Even if scientific literature reports overlapping features between mood disorders and BPD, in terms of mood deregulation, affective instability, impulsivity, suicidal ideation and behaviors (54, 55), they remain very distinct and different clinical conditions, not only from a psychopathological point of view, but also in terms of illness course, gender prevalence and heritability features.
In this framework the aim of this study was to evaluate how the presence and the prevalence of catatonic symptoms may shape and correlate with suicidal risk in a sample of individuals with MDD or BPD.
2. Materials and methods
A consecutive sample of subjects with a clinical diagnosis of MDD, BPD or catatonia were recruited in six Italian University Departments of Psychiatry, coordinated by the University of Pisa: University of Campania “Luigi Vanvitelli,” University of Pavia, University of Messina, La Sapienza University of Rome, University of Catania, and University of Brescia. Exclusion criteria for all groups were: age under 18 years, language or intellectual impairment affecting the possibility to fulfill the assessments, mental disability, poor cooperation skills, and ongoing psychotic symptoms. The study was conducted in accordance with the Declaration of Helsinki. The Ethics Committee of the Azienda Ospedaliero-Universitaria of Pisa approved all recruitment and assessment procedures. Written informed consent was obtained from all participants after they received a complete description of the study and had the opportunity to ask questions. Subjects were not paid for their participation according to Italian legislation.
The Structured Clinical Interview for DSM-5, Research Version (SCID-5-RV) (56) was used to confirm the diagnosis of BPD and MDD, as well as the absence of mental disorders among HC subjects. All subjects were assessed with the following self-report instruments: the catatonia Spectrum (CS) and the mood spectrum self-report (MOODS-SR). The questionnaires were compiled autonomously by all the subjects.
2.1. The catatonia spectrum
The CS is a self-assessment questionnaire that investigates nuclear, subthreshold, atypical and partial manifestations of catatonia across the lifespan, developed and validated at University of Pisa (19). It consists of 74 items divided into 8 domains investigating the main criteria of the catatonia diagnosis: (1) psychomotor activity (stupor); (2) verbal response (mutism); (3) repetitive movements (stereotypes); (4) artificial expressions and actions (mannerisms); (5) oppositivity or poor response to stimuli (negativism); (6) response to instructions given from outside (automatic obedience); (7) automatisms; (8) impulsivity. For each item there is a dichotomous answer “yes” and “no.”
The CS showed great validity and reliability, excellent internal consistency and test–retest reliability and a significant and positive convergent validity with alternative dimensional measures of catatonia (19).
2.2. The MOODS-SR
The MOODS-SR is a questionnaire tailored to evaluate the presence of a broad range of mood symptoms and temperamental traits during lifetime. It consists of 160 items and is divided in 7 domains. For each item there is a dichotomous answer “yes” and “no.” For the Italian version the Cronbach’s alphas of the instrument ranged between 0.72 and 0.92. The MOODS-SR was employed in previous studies for evaluating suicidality (suicidal ideation and behaviors) (51, 57), as measured by items 102 to 107 of the instrument.
2.3. Statistical analysis
ANOVA and chi-square analyses were performed in order to compare among group mean MOODS suicidality scores and the presence of at least one positive answer to MOODS suicidality items. Pearson’s correlation coefficient was used for evaluating the pattern of correlations among the scores reported on psychometric instruments within the BPD, MDD and CTL subjects. Subsequently, in order to evaluate which CS domains were statistically predictive of suicidality score in the sample, linear regression analyses were performed with suicidality score as the dependent variable and CS total and domain scores as independent variables. Moreover, logistic regression analyses were performed with the presence of a positive answer to at least one suicidality item of MOODS suicidal ideation and MOODS suicidal behavior as the dependent variables and CS total and domain scores as independent variables. All statistical analyses were conducted using Statistical Package for the Social Sciences (SPSS) version 26.0.
3. Results
The sample was composed of 147 MDD subjects, 105 subjects with BPD and 156 CTL. Sociodemographic data of the sample are reported elsewhere (58).
Considering the presence of positive answers to at least one MOODS suicidality item and one MOODS suicidal thoughts item, the CTL group reported a percentage significantly lower (17.9%; 17.3%) compared to the BPD (76.4%; 76.4%) and the MDD domain (65.3%; 63.9%), while no significant differences were reported in the two pathological groups. On the other hand, when evaluating the presence of at least one positive answer to MOODS suicidal behavior items, the CTL group reported a significantly lower percentage (3.2%) compared to the MDD group (37.4%), and both groups showed a significantly lower percentage compared to the BPD group (60.4%) (see Table 1).
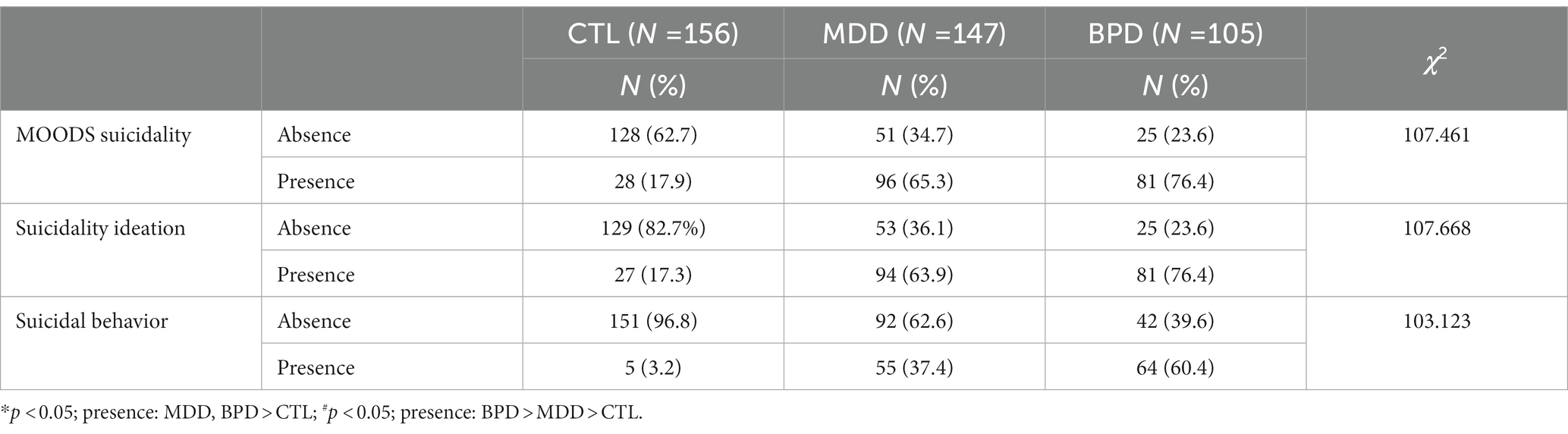
Table 1. Presence or absence of a positive answer to at least one item of MOODS suicidality, suicidal ideation and behavior, sorted by diagnosis.
In the total sample, as well as in the MDD group, the total suicidality score, the suicidal ideation and the suicidal behaviors scores, were significantly and positively correlated with all CS domains and CS total score (see Tables 2 3). In the BPD group, the suicidality total score and suicidal ideation score were significantly and positively correlated with CS total score and all CS domains except for artificial expressions, while suicidal behavior score was significantly and positively correlated with CS total score and all CS domains except for artificial expressions and repetitive movements (Table 4). Finally, in the CTL group, the total suicidality score and the suicidal ideation were significantly and positively correlated with all CS domains and CS total score, while suicidal behaviors scores, were significantly and positively correlated with CS total score and all CS domains except for verbal response, artificial expressions and repetitive movements (Table 5).
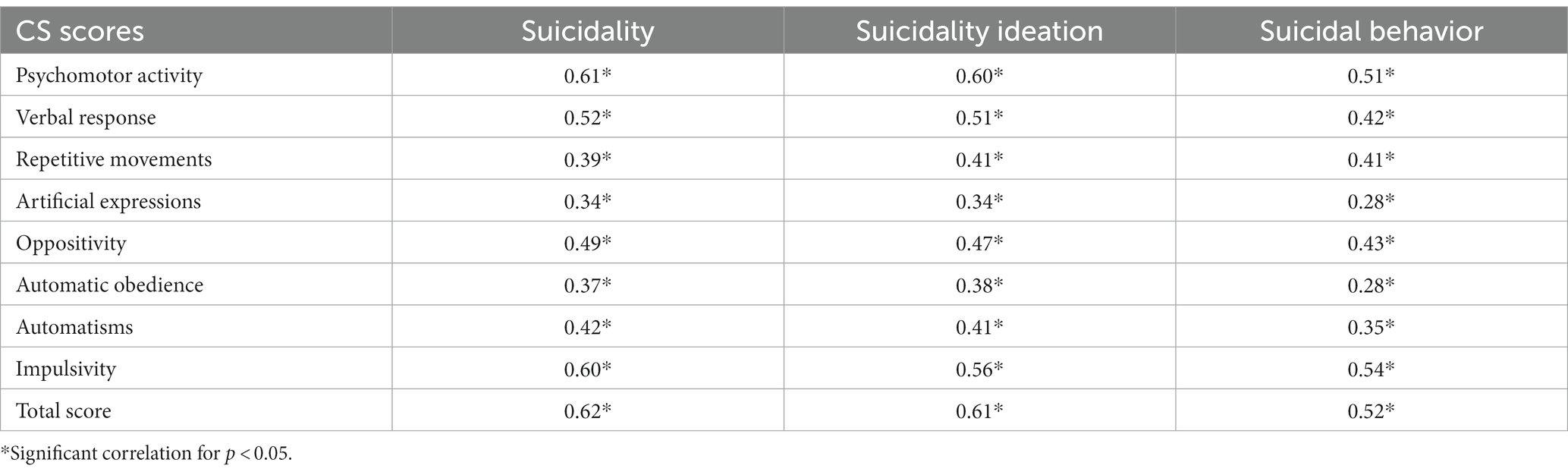
Table 2. Pearson’s correlations coefficients (r) among MOODS suicidality score and CS scores in the total sample.
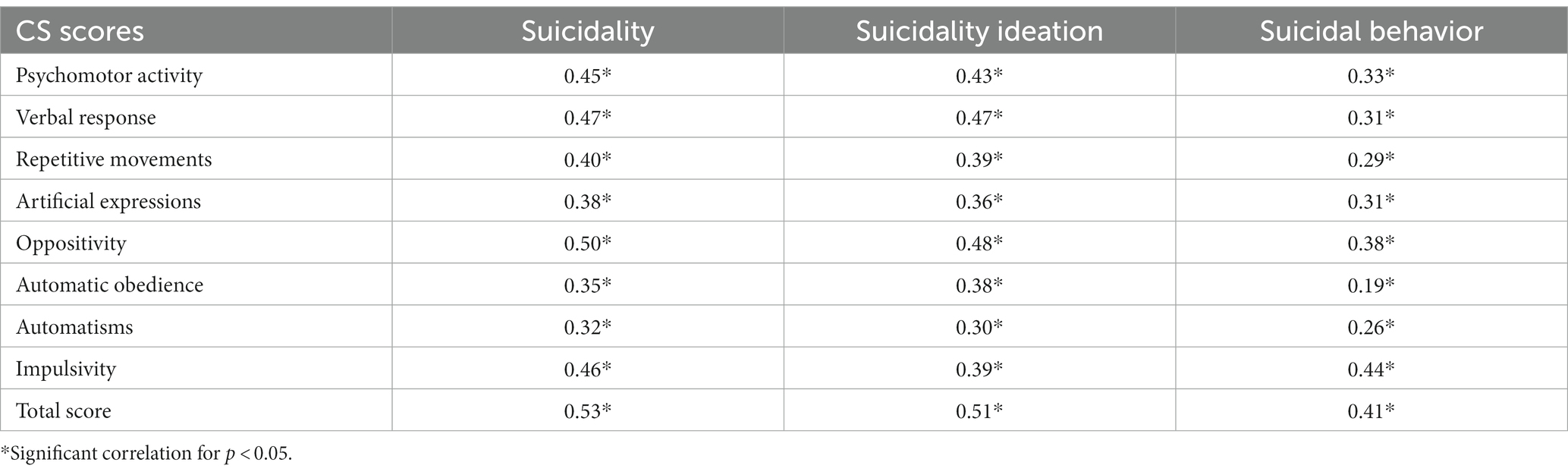
Table 3. Pearson’s correlations coefficients (r) among MOOD suicidality score and CS scores in the MDD group.
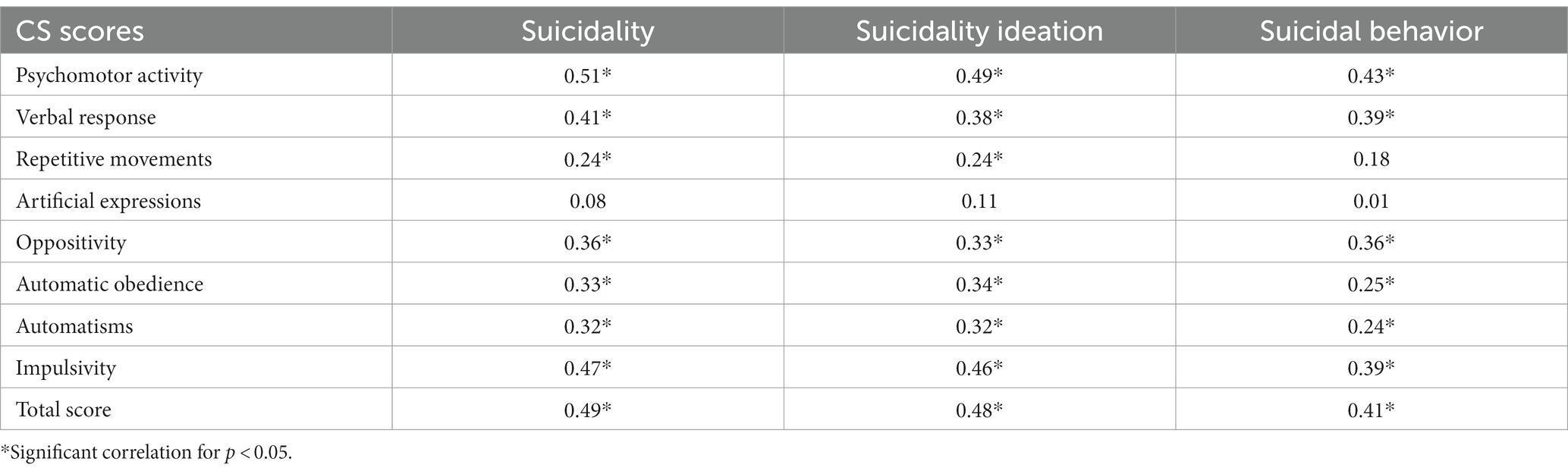
Table 4. Pearson’s correlations coefficients (r) among MOOD suicidality score and CS scores in the BPD group.
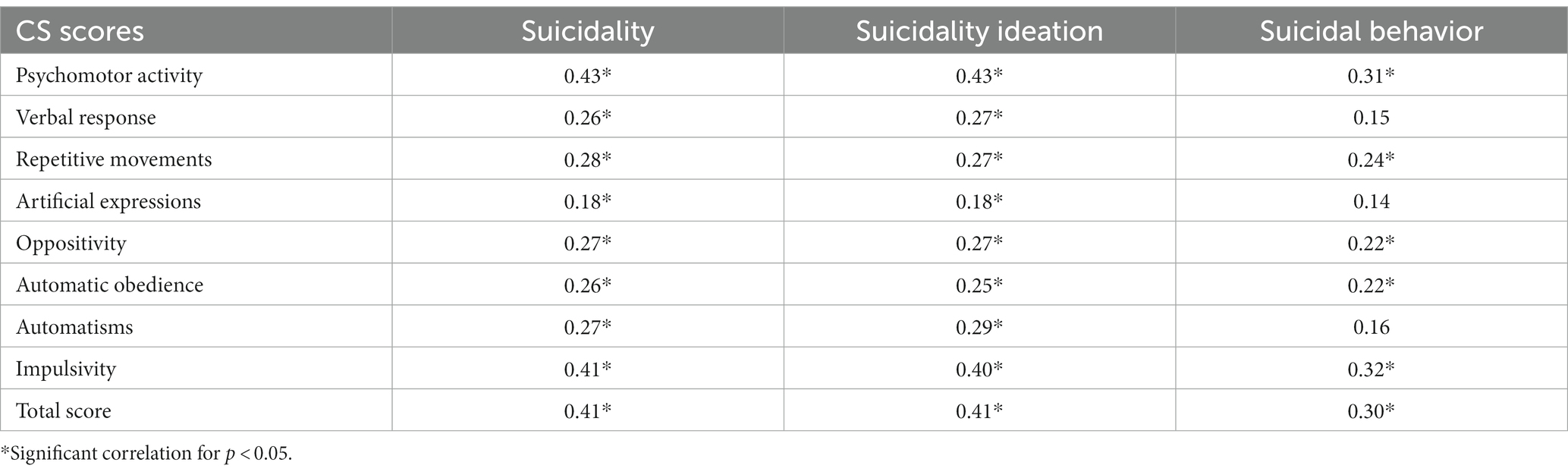
Table 5. Pearson’s correlations coefficients (r) among MOOD suicidality score and CS scores in the CTL group.
The regression line showed that for every positive item of the CS the suicidality score increases of 0.08 in the total sample (Figure 1), and of 0.08 and 0.07 in the BPD and MDD groups, respectively (Figures 2 3). Finally, results from linear regression analysis showed that CS total score was a significant predictor of a higher suicidality score, as well as CS psychomotor activity (beta = 0.35; t = 5.57; p < 0.001), verbal response (beta = 0.11; t = 1. 99; p = 0.047) and Impulsivity (beta = 0.38; t = 6.32; p < 0.001) domain scores, while automatism was a negative predictor (beta = −0.14; t = −2.35; p = 0.02) (Table 6); meanwhile results from logistic regression analysis reported that the CS total score and CS psychomotor activity, verbal response and impulsivity (Table 7) domain scores were significant positive predictors of the presence of at least one positive response in the items evaluating the presence of suicidal thoughts whereas only psychomotor activity and impulsivity domain scores were significant positive predictors of the presence of at least one positive response in the items evaluating the suicidal behaviors (Table 8).
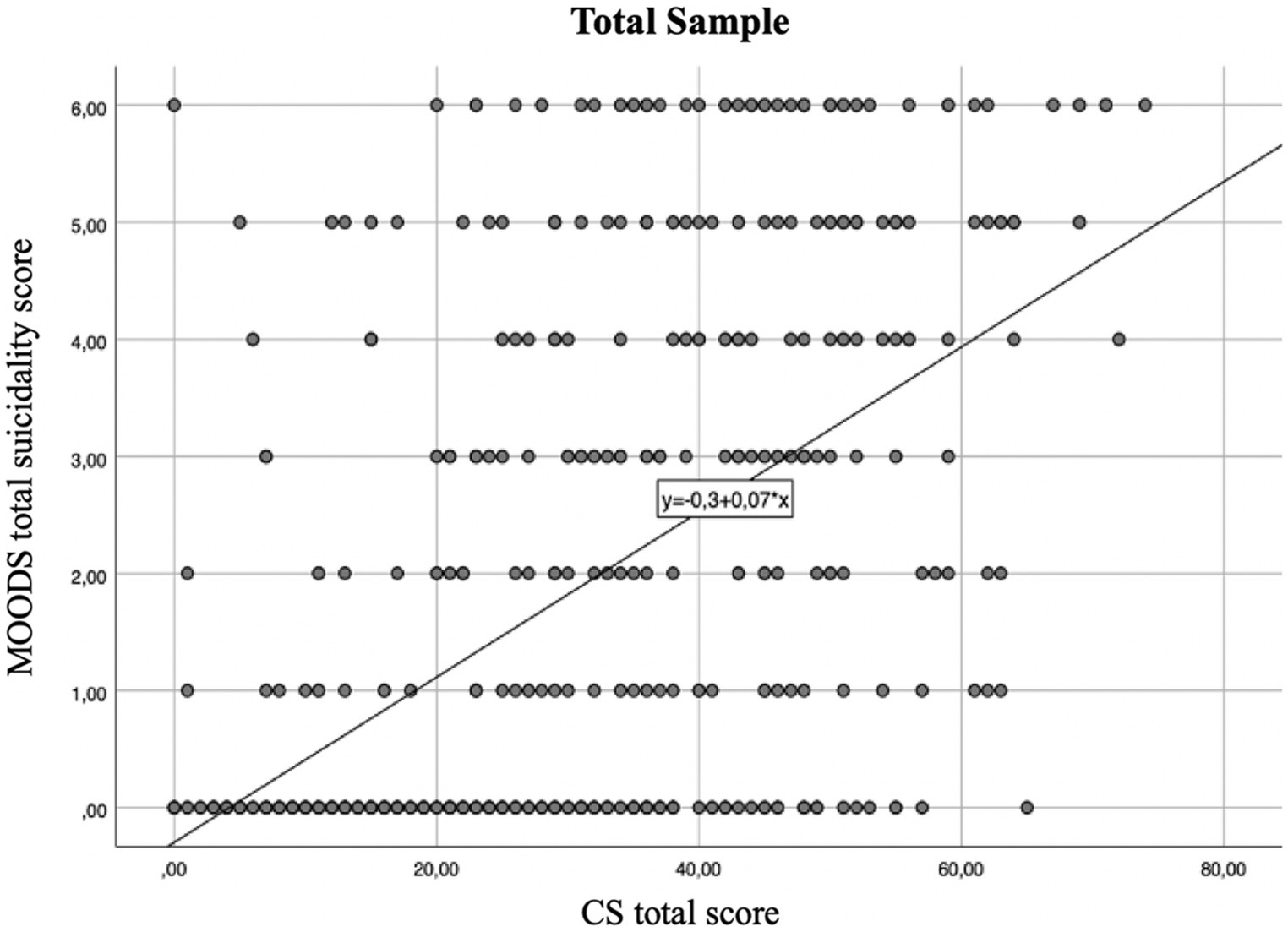
Figure 1. Regression line between suicidality score and catatonia spectrum (CS) total score in the total sample linear R2 = 0.408.
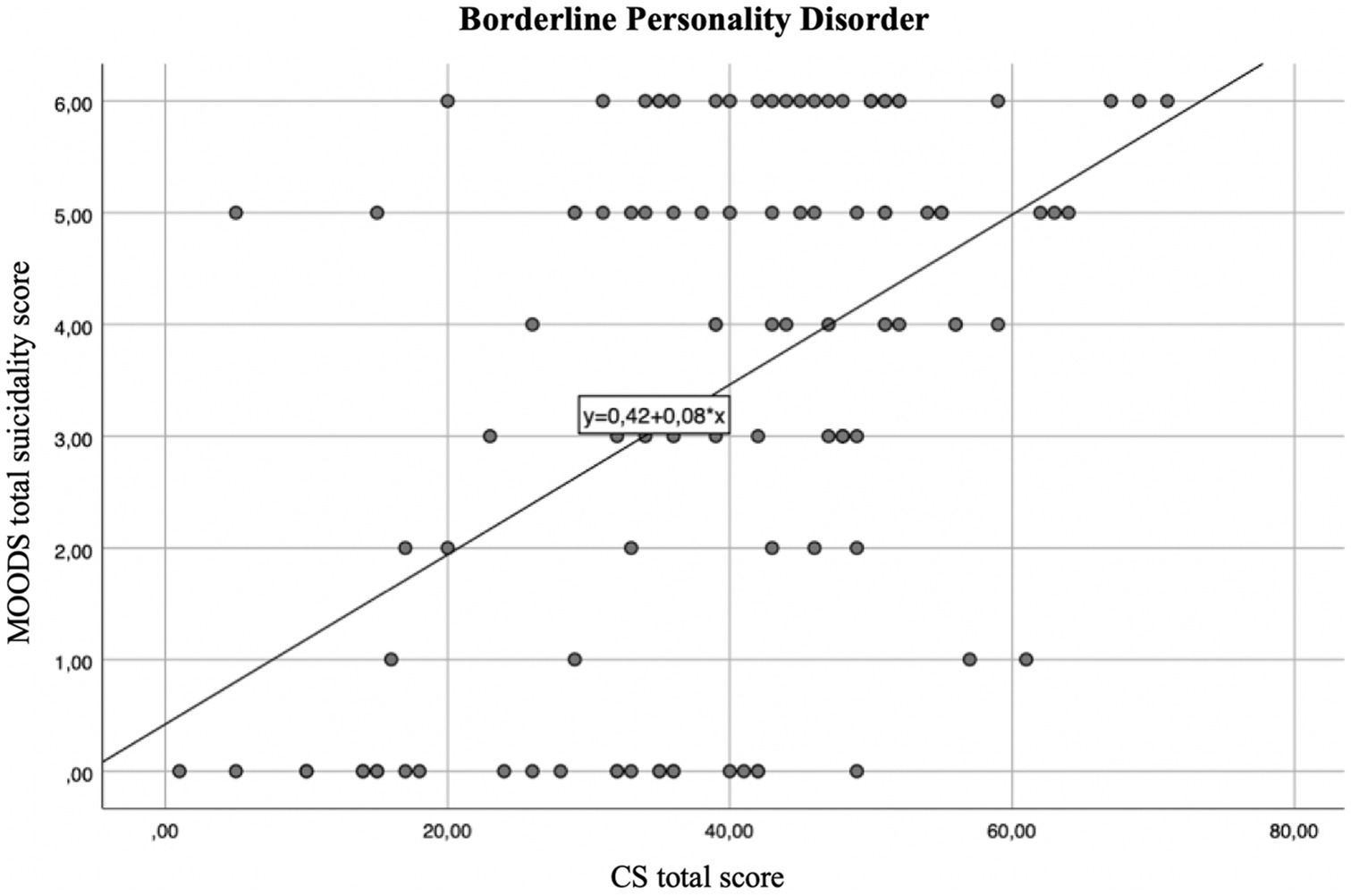
Figure 2. Regression line between suicidality score and CS total score in the BPD group linear R2 = 0.241.
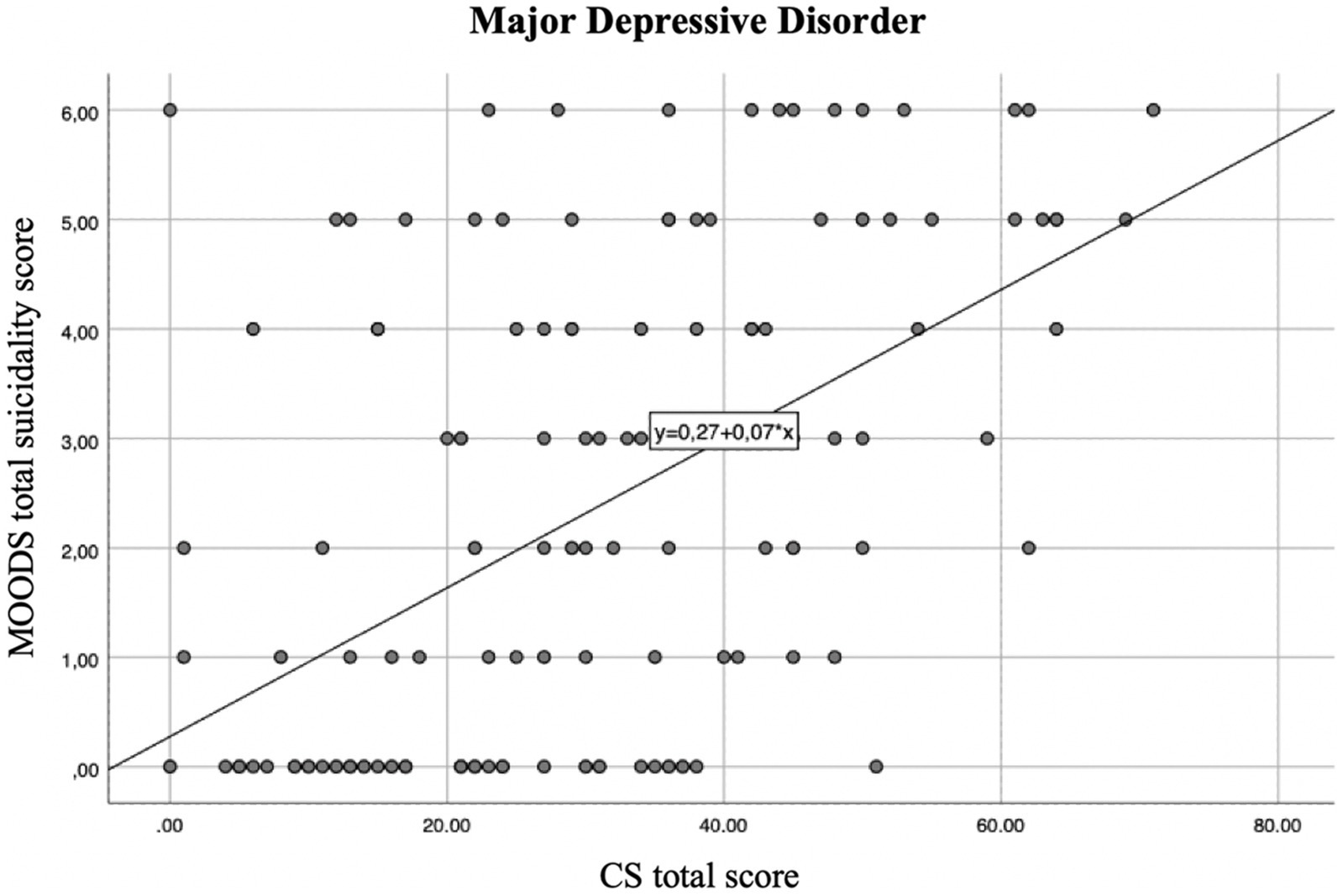
Figure 3. Regression line between suicidality score and CS total score in the MDD group linear R2 = 0.281.
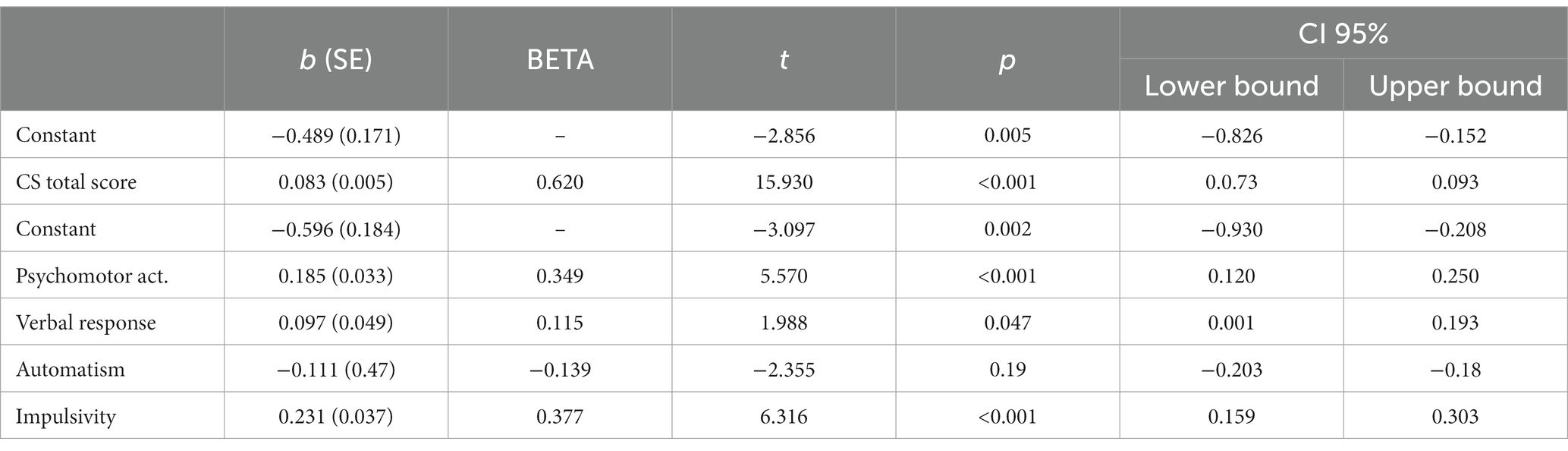
Table 6. Linear regression analysis with MOODS suicidality score as a dependent variable and CS domains as independent variables in the total sample.
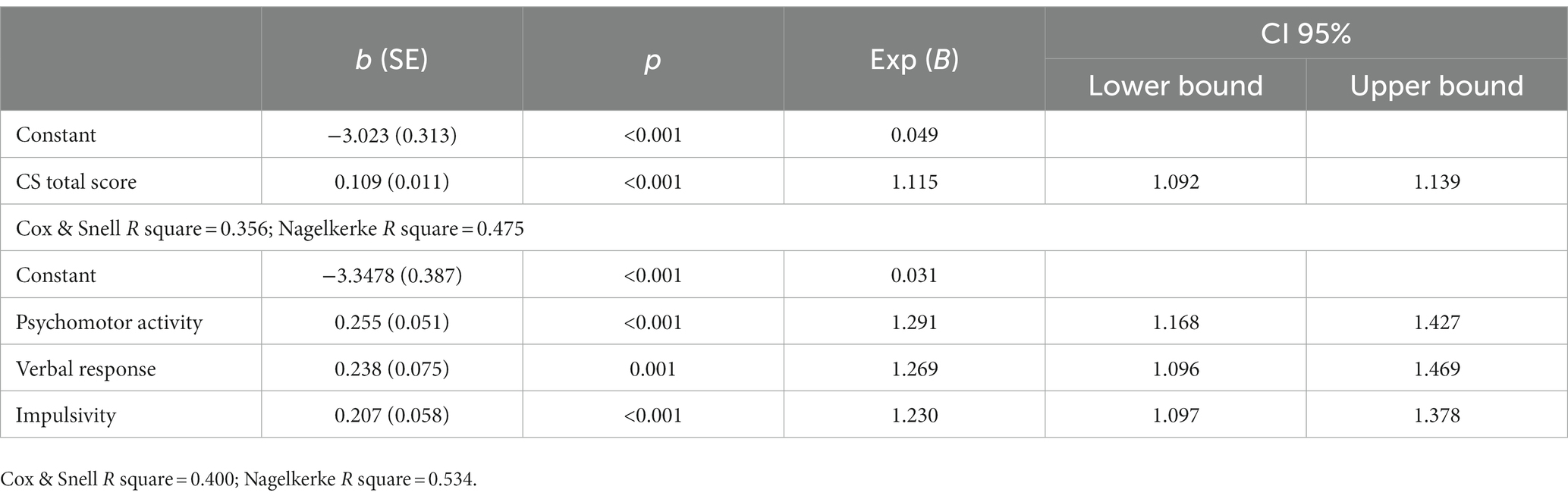
Table 7. Logistic regression analysis with the presence of at least one positive MOOD Suicidal ideation item as a dependent variable and CS domains as independent variables in the total sample.
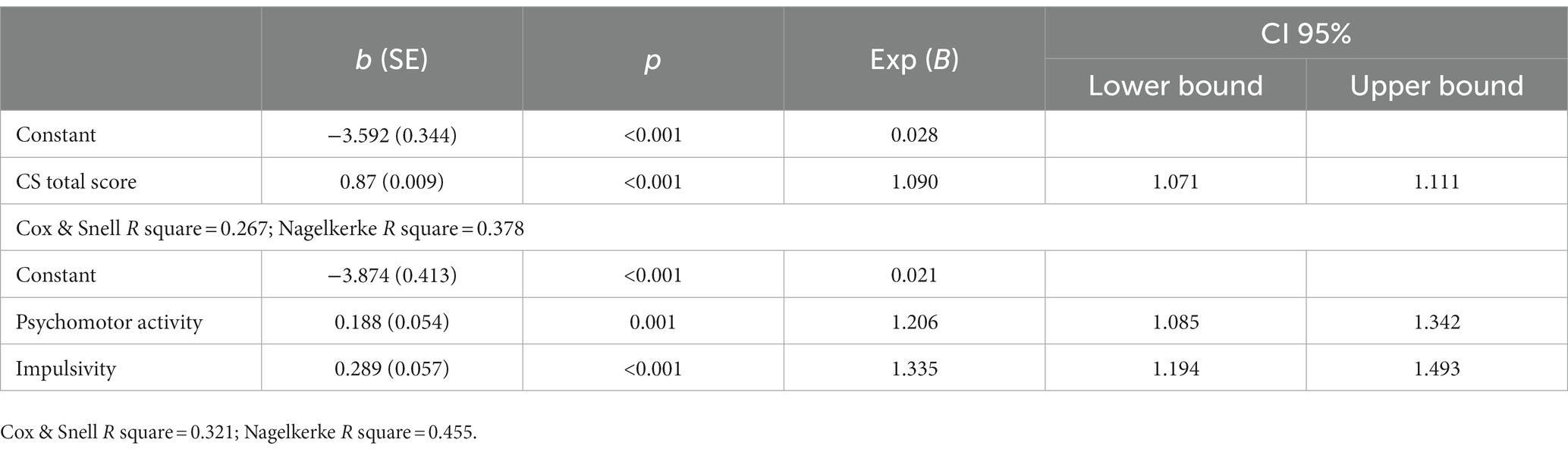
Table 8. Logistic regression analysis with the presence of at least one positive MOOD Suicidal behavior item as a dependent variable and CS domains as independent variables in the total sample.
4. Discussion
The aim of this study was to evaluate the presence and the prevalence of catatonic symptoms and how they may shape and correlate with suicidal risk in a sample of individuals with MDD or BPD, investigating also if they could represent statistically predictive factors of suicidality. Embracing the modern definition of the catatonic clinical picture, brought by the DSM-5-TR, which seems to be receptive of a less strictly categorical conceptualization and open to an expansion of its boundaries towards a dimensional approach, the Catatonia Spectrum model aims to evaluate the presence and correlates of catatonic sub-threshold and full-threshold symptoms in different clinical conditions (59). The “catatonic spectrum” comprehends a wide range of manifestations with various degrees of severity, consistent with the conceptualization of catatonia as a trans-nosographic specifier, potentially associated with every mental disorder (58).
As expected, we found that both clinical groups showed greater suicidality scores than controls. Noticeably, BPD patients showed increased suicidal behaviors than MDD ones, supporting the strong link between BPD and risk of suicidal attempts (60, 61).
In addition, we found strong correlation between the presence of catatonic symptoms, as evaluated by the CS, and suicidality, as measured by the MOODS suicidality items, in the total sample and in all groups. Increasing evidence is stressing a higher prevalence of catatonic manifestations in several mental disorders: in particular, about 10% of patients with severe acute psychiatric illness are reported to exhibit motor signs (including mutism, negativism, rigidity, stereotypy, etc.) that are identified as catatonia (62), and most of the cases involve individuals with depressive or bipolar disorders (2). In particular, a recent study reported high levels of catatonic manifestations in the patients affected by BPD (19), a severe mental disorder strongly correlated with suicidal behaviors (63, 64). Both disorders, as well as catatonia of psychiatric origin, are well known for the increased risk of suicidality, and our results seem to be in line with these evidences (20, 21).
It should be noted that previous studies also highlighted in both BPD and MDD populations a significant prevalence of autistic traits, even though they may differ in terms of quality and/or quantity, among individuals with mood disorders and BPD (49, 52, 65, 66), which also seem to increase the suicidal risk in both the categories of subjects (51).
Moreover, in the past decades, particular attention has been dedicated to the relationship between catatonia and ASD (58), thanks to the many shared clinical features shared by the two disorders, many authors have indicated that catatonia may slowly develop over the course of ASD (67), supporting the hypothesis of the presence of a psychopathological continuum starting from a neuroatypical vulnerability, and progressing and culminating in the manifestations of the catatonic spectrum, trespassing affective and personality disorders (62, 68). Interestingly, the presence of a positive correlation between suicidality score and most of the CS domains also in the CTL group support the hypothesis of a connection between catatonic traits and suicidality even in a subthreshold context of non full-blown psychopathologies.
Our findings also highlighted the possible presence of a specific pattern of features that seems to be predictive of suicidality. Considering the correlation analysis, in the MDD group all CS domains and the total score were significantly and positively correlated with suicidality scores, suicidal ideation and suicidal behavior, globally supporting the strong link between catatonic spectrum and suicidality (20, 21). Similarly, in the BPD group significant correlations were reported between suicidality total score, suicidal ideation, suicidal behavior and all CS domains, with the exception of CS artificial expressions domain and, only for suicidal behavior, of CS repetitive movement domain.
However, results from the regression analysis revealed that, besides the CS total score, specific catatonic symptoms seem to be statistically predictive of suicidality in the sample. In particular when considering the CS mean score as the dependent variable, the predictive factor for suicidality were the CS psychomotor activity, verbal response and impulsivity were identified as positive predictors, while automatism as a negative predictor. Similarly, CS psychomotor activity, verbal response and impulsivity domains emerged as positive predictors of suicidal ideation, while only CS psychomotor activity, and impulsivity were highlighted as significant predictors of suicidal behavior.
The domains psychomotor activity (stupor) and impulsivity represent the two most severe and extreme clinical presentation of catatonia. Noticeably, one of the factors which was already hypothesized to be at the basis of catatonic episodes is the feeling urged towards two opposite actions at the same time: an ambi-tendence. Clinically, catatonia is not just petrifying paralysis, but a complex condition in which psychomotor activity is reduced, excessive or abnormal, in a so-called psychomotor alternation. Following the theory proposed by Fink (69) for which catatonia is often linked to and can be driven by fear (70), and that the signs of catatonia may be adaptations to persistent fear, similar to a tonic immobilization, the manifestation of stupor and impulsivity could easily be compared to the animal behavior in front of danger where the freeze reaction is the catatonic extreme form of total psychomotor block and the flight one would correspond to agitation and impulsive behaviors (71). In this view, the two extreme and opposite manifestations are the main indicators of the gravity of the catatonic manifestation, explaining also the raised suicidal risk and the specific link with suicidal behavior. This assumption in also supported by the fact that the sedation derived from the benzodiazepines can afford relief to for the fear that occupies the mind of the catatonic patient (69).
Suicidality total score and suicidal ideation was instead found to be associated also with the CS verbal response domain. The presence of deficits in the verbal and non-verbal communication has often been reported to be linked to suicidality, especially in ASD patients, where they could lead to a higher risk of isolation and depressive symptoms (57, 72, 73). This correlation is also in line with previous studies that highlighted how a greater awareness of the self-difficulties in communicating with others can lead to a greater distress (74, 75).
On the other side, the artificial expressions domain portrays the clinical symptom of catatonic mannerism. Noticeably, this dimension seemed to negative predict suicidality scores according to our results. Although the available literature lacks to report a hypothetic link between mannerism and suicidality or its protective effect, we can assume that mannerism manifestations are partially similar to camouflaging, featuring exaggerated, abnormal expression of common gestures and behaviors (76). Despite previous research highlighted instead a possible positive link between camouflaging behavior and suicidality (77), the recent literature has also focused on camouflaging as a strategy adopted to cope with social environment, in order to reach a greater integration between verbal and nonverbal behaviors, a greater reciprocity in conversations or relationships, and minimizing responses toward sensory over stimulations (74, 78, 79). In this view, camouflaging and mannerism, for some individuals might result in a better adjustment (75, 80).
This study should be considered in light of some obvious limitations. Firstly, the cross-sectional design of the study prevented us to evaluate possible temporal relationships between the considered variables. Moreover, we recognize that the optimal way to investigate suicidal ideation and behaviors should be via clinical evaluation, and that the use of self-report instruments may have led to over- or underestimations of symptoms by the subjects, and to consequent biases in our results. Thirdly, this study does not report the clinical characteristics nor other component of MOODS-SR (such as energy, cognition and rhythmicity) for they are analyzed elsewhere. Furthermore, the presence of substance misuse was not investigated, nor the use pharmacological therapies whose current use or withdrawal could have cause catatonic manifestations. Additionally, no blinding procedures were used for the study and this possibly could have implied a bias in the interpretation of the results. Finally, the relatively small sample size limits the extensibility of the present work. Further study in wider sample and with a longitudinal design are needed for clarifying the relationship between catatonic spectrum and suicidality in different clinical conditions.
5. Conclusion
In the context of the above limitations, results from this study seem to globally highlight that higher catatonic manifestations are linked to higher suicidal tendencies, confirming the high risk of suicide for patients falling under the umbrella of the “catatonic spectrum,” conceptualized as a wider range of manifestations with various degrees of severity. Further studies should address the presence of specific patterns of catatonic symptoms and traits in different mental disorders, such as affective and personality ones, and how they might affect psychopathological trajectories and clinical outcomes.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of the Azienda Ospedaliero-Universitaria of Pisa. The patients/participants provided their written informed consent to participate in this study.
Author contributions
LD conceived the work. LD, BN, CB, DG, FB, GA, SB, GM, ML, IB, NB, MG, GD, MN, AR, MMu, MP, PP, AV, CC, IC, BC, and MMa collected the data processed in the study. GM did statistical analysis. BN and LD drafted the manuscript and revised the work. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors thank the participants for their continued support and participation in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington: American Psychiatric Association (2022).
3. Fink, M. Catatonia: a syndrome appears, disappears, and is rediscovered. Can J Psychiatry. (2009) 54:437–45. doi: 10.1177/070674370905400704
4. Pfuhlmann, B, and Stöber, G. The different conceptions of catatonia: historical overview and critical discussion. Eur Arch Psychiatry Clin Neurosci. (2001) 251:I4–7. doi: 10.1007/pl00014199
5. Ungvari, GS, Leung, SK, Ng, FS, Cheung, HK, and Leung, T. Schizophrenia with prominent catatonic features ('catatonic schizophrenia'): I. Demographic and clinical correlates in the chronic phase. Prog Neuropsychopharmacol Biol Psychiatry. (2005) 29:27–38. doi: 10.1016/j.pnpbp.2004.08.007
6. Taylor, MA, and Fink, M. Catatonia in psychiatric classification: a home of its own. Am J Psychiatry. (2003) 160:1233–41. doi: 10.1176/appi.ajp.160.7.1233
7. Nath, S, Bhoi, R, Mishra, B, and Padhy, S. Does recurrent catatonia manifest in a similar fashion in all the episodes of mood disorder? A case series with literature review. Gen Psychiatry. (2021) 34:e100494. doi: 10.1136/gpsych-2021-100494
8. Dhossche, DM, and Withane, N. Electroconvulsive therapy for catatonia in children and adolescents. Child Adolesc Psychiatr Clin N Am. (2019) 28:111–20. doi: 10.1016/j.chc.2018.07.007
9. Ghaziuddin, N, Dhossche, D, and Marcotte, K. Retrospective chart review of catatonia in child and adolescent psychiatric patients. Acta Psychiatr Scand. (2012) 125:33–8. doi: 10.1111/j.1600-0447.2011.01778.x
10. Billstedt, E, Gillberg, C, and Gillberg, C. Autism after adolescence: population-based 13-to 22-year follow-up study of 120 individuals with autism diagnosed in childhood. J Autism Dev Disord. (2005) 35:351–60. doi: 10.1007/s10803-005-3302-5
11. Dell’Osso, L, Amatori, G, Gesi, C, and Carmassi, C. A case of catatonia in the aftermath of the COVID-19 pandemic: does autism spectrum matter? Ann Gen Psychiatry. (2021) 20:54–4. doi: 10.1186/s12991-021-00377-9
12. Dell’Osso, L, Toschi, D, Amatori, G, and Gesi, C. Rethinking catatonia: new insights from the autism spectrum. CNS Neurol Disord Drug Targets. (2022) 22:462–5. doi: 10.2174/1871527321666220406105844
13. Rambault, A, Benchaïba, S, Tobie, D, Roberti, H, Claire, R, and Malvy, J. Catatonie et trouble du spectre de l’autisme [Catatonia and autism spectrum disorder]. Soins Pediatr Pueric. (2020) 41:44–6. doi: 10.1016/j.spp.2020.02.010
14. Shrivastava, SVK, Poulsen, R, Mavrides, N, and Coffey, BJ. Catatonia in a 12-year-old child. J Child Adolesc Psychopharmacol. (2021) 31:144–6. doi: 10.1089/cap.2021.29197.bjc
16. Caroff, SN, Mann, SC, Francis, A, and Fricchione, GL. Catatonia: from psychopathology to neurobiology. Washington, DC: American Psychiatric Pub (2007).
17. Fink, M, and Taylor, MA. Catatonia: a clinician's guide to diagnosis and treatment. Cambridge, UK: Cambridge University Press (2006).
18. Barnes, MP, Saunders, M, Walls, TJ, Saunders, I, and Kirk, CA. The syndrome of Karl Ludwig Kahlbaum. J Neurol Neurosurg Psychiatry. (1986) 49:991–6. doi: 10.1136/jnnp.49.9.991
19. Dell’Osso, L, Amatori, G, Cappelli, A, Cremone, IM, Massimetti, G, Gravina, D, et al. Catatonia spectrum: validation of a questionnaire investigating catatonia spectrum. Front Psychiatry. (2022) 13:913286. doi: 10.3389/fpsyt.2022.913286
20. Yanagawa, Y, Ohshita, T, Takemoto, M, Matsumoto, N, Sakamoto, T, and Okada, Y. A case of catatonia associated with the ingestion of hydroxyzine. No To Shinkei. (2005) 57:45–9.
21. Godfroid, IO. Violence, desire and death. Reflections on 3 taboos in psychiatry. Encephale. (2001) 27:22–7.
22. Ribeiro, JD, Huang, X, Fox, KR, and Franklin, JC. Depression and hopelessness as risk factors for suicide ideation, attempts and death: meta-analysis of longitudinal studies. Br J Psychiatry. (2018) 212:279–86. doi: 10.1192/bjp.2018.27
23. Cavanagh, JT, Carson, AJ, Sharpe, M, and Lawrie, SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. (2003) 33:395–405. doi: 10.1017/s0033291702006943
24. Starkstein, SE, Petracca, G, Teson, A, Chemerinski, E, Merello, M, Migliorelli, R, et al. Catatonia in depression: prevalence, clinical correlates, and validation of a scale. J Neurol Neurosurg Psychiatry. (1996) 60:326–32. doi: 10.1136/jnnp.60.3.326
25. Bolgov, MI, and Barkhatova, AN. Struktura katatonii pri depressiyakh i depressivno-bredovykh sostoyaniyakh [the structure of catatonia in depression and depressive-delusional conditions]. Zh Nevrol Psikhiatr Im S S Korsakova. (2022) 122:78–83. doi: 10.17116/jnevro202212206278
26. Medda, P, Toni, C, Luchini, F, Giorgi Mariani, M, Mauri, M, and Perugi, G. Catatonia in 26 patients with bipolar disorder: clinical features and response to electroconvulsive therapy. Bipolar Disord. (2015) 17:892–901. doi: 10.1111/bdi.12348
27. Krüger, S, Cooke, RG, Spegg, CC, and Bräunig, P. Relevance of the catatonic syndrome to the mixed manic episode. J Affect Disord. (2003) 74:279–85. doi: 10.1016/s0165-0327(02)00088-5
28. Swann, AC, Lafer, B, Perugi, G, Frye, MA, Bauer, M, Bahk, WM, et al. Bipolar mixed states: an international society for bipolar disorders task force report of symptom structure, course of illness, and diagnosis. Am J Psychiatry. (2013) 170:31–42. doi: 10.1176/appi.ajp.2012.12030301
29. Korzekwa, MI, Dell, PF, Links, PS, Thabane, L, and Webb, SP. Estimating the prevalence of borderline personality disorder in psychiatric outpatients using a two-phase procedure. Compr Psychiatry. (2008) 49:380–6. doi: 10.1016/j.comppsych.2008.01.007
30. Leichsenring, F, Leibing, E, Kruse, J, New, AS, and Leweke, F. Borderline personality disorder. Lancet. (2011) 377:74–84. doi: 10.1016/S0140-6736(10)61422-5
31. Lieb, K, Zanarini, MC, Schmahl, C, Linehan, MM, and Bohus, M. Borderline personality disorder. Lancet. (2004) 364:453–61. doi: 10.1016/S0140-6736(04)16770-6
32. Moseley, RL, Gregory, NJ, Smith, P, Allison, C, and Baron-Cohen, S. Links between self-injury and suicidality in autism. Mol Autism. (2020) 11:14. doi: 10.1186/s13229-020-0319-8
33. Carpita, B, Muti, D, Cremone, IM, Fagiolini, A, and Dell’Osso, L. Eating disorders and autism spectrum: links and risks. CNS Spectr. (2022) 27:272–80. doi: 10.1017/S1092852920002011
34. Dell’Osso, L, Cremone, IM, Carpita, B, Fagiolini, A, Massimetti, G, Bossini, L, et al. Correlates of autistic traits among patients with borderline personality disorder. Compr Psychiatry. (2018) 83:7–11. doi: 10.1016/j.comppsych.2018.01.002
35. Dell’Osso, L, Muti, D, Carpita, B, Cremone, IM, Bui, E, Gesi, C, et al. The adult autism subthreshold spectrum (AdAS) model: a neurodevelopmental approach to mental disorders. J Psychopathol. (2018) 24:118–24.
36. Dinsdale, N, and Crespi, BJ. The borderline empathy paradox: evidence and conceptual models for empathic enhancements in borderline personality disorder. J Personal Disord. (2013) 9:172–95. doi: 10.1521/pedi.2013.27.2.172
37. Jeung, H, and Herpertz, SC. Impairments of interpersonal functioning: empathy and intimacy in borderline personality disorder. Psychopathology. (2014) 47:220–34. doi: 10.1159/000357191
38. Suzuki, T, Miyaki, K, Eguchi, H, and Tsutsumi, A. Distribution of autistic traits and their association with sociodemographic characteristics in Japanese workers. Autism. (2018) 22:907–14. doi: 10.1177/1362361317716605
39. Sansone, RA, and Sansone, LA. Personality pathology and its influence on eating disorders. Innov Clin Neurosci. (2011) 8:14–8.
40. Sloan, E, Hall, K, Moulding, R, Bryce, S, Mildred, H, and Staiger, PK. Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: a systematic review. Clin Psychol Rev. (2017) 57:141–63. doi: 10.1016/j.cpr.2017.09.002
41. Barnow, S, Limberg, A, Stopsack, M, Spitzer, C, Grabe, HJ, Freyberger, HJ, et al. Dissociation and emotion regulation in borderline personality disorder. Psychol Med. (2012) 42:783–94. doi: 10.1017/S0033291711001917
42. Carmassi, C, Conti, L, Gravina, D, Nardi, B, and Dell’Osso, L. Emotional dysregulation as trans-nosographic psychopathological dimension in adulthood: a systematic review. Front Psychiatry. (2022) 13:900277. doi: 10.3389/fpsyt.2022.900277
43. Vegni, N, D'Ardia, C, and Torregiani, G. Empathy, mentalization, and theory of mind in borderline personality disorder: possible overlap with autism spectrum disorders. Front Psychol. (2021) 12:626353. doi: 10.3389/fpsyg.2021.626353
44. Makris, G, Agorastos, A, Chrousos, GP, and Pervanidou, P. Stress system activation in children and adolescents with autism spectrum disorder. Front Neurosci. (2022) 15:756628. doi: 10.3389/fnins.2021.756628
45. Drews, E, Fertuck, EA, Koenig, J, Kaess, M, and Arntz, A. Hypothalamic-pituitary-adrenal axis functioning in borderline personality disorder: a meta-analysis. Neurosci Biobehav Rev. (2019) 96:316–34. doi: 10.1016/j.neubiorev.2018.11.008
46. Rinne, T, de Kloet, ER, Wouters, L, Goekoop, JG, DeRijk, RH, and van den Brink, W. Hyperresponsiveness of hypothalamic-pituitary-adrenal axis to combined dexamethasone/corticotropin-releasing hormone challenge in female borderline personality disorder subjects with a history of sustained childhood abuse. Biol Psychiatry. (2002) 52:1102–12. doi: 10.1016/s0006-3223(02)01395-1
47. LeGris, J, van der Meer, L, and Maltby, N. Borderline personality disorder and autism spectrum disorder: similarities and differences in neurocognitive functioning. J Autism Dev Disord. (2019) 49:3939–55. doi: 10.1007/s10803-019-04087-w
48. Lugnegård, T, Hallerbäck, MU, and Gillberg, C. Personality disorders and autism spectrum disorders: what are the connections? Compr Psychiatry. (2012) 53:333–40. doi: 10.1016/j.comppsych.2011.05.014
49. Dudas, RB, Lovejoy, C, Cassidy, S, Allison, C, Smith, P, and Baron-Cohen, S. The overlap between autistic spectrum conditions and borderline personality disorder. PLoS One. (2017) 12:e0184447. doi: 10.1371/journal.pone.0184447
50. Nanchen, K, Brodführer, A, Heinrichs, M, Philipsen, A, van Elst, LT, and Matthies, S. Autistic traits in patients with borderline personality disorder. Z Psychiatr Psychol Psychother. (2016) 64:247–55. doi: 10.1024/1661-4747/a000286
51. Dell’Osso, L, Cremone, IM, Amatori, G, Cappelli, A, Cuomo, A, Barlati, S, et al. Investigating the relationship between autistic traits, ruminative thinking, and suicidality in a clinical sample of subjects with bipolar disorder and borderline personality disorder. Brain Sci. (2021) 11:621. doi: 10.3390/brainsci11050621.
52. Ruggieri, V. Autismo, depresión y riesgo de suicidio. Medicina. (2020) 80:12–6. doi: 10.3390/ijerph19073809
53. Dell’Osso, L, Buselli, R, Corsi, M, Baldanzi, S, Bertelloni, CA, Marino, R, et al. Do autistic traits correlate with post-traumatic stress and mood Spectrum symptoms among workers complaining of occupational stress? Int J Environ Res Public Health. (2022) 19:3809. doi: 10.3390/ijerph19073809
54. Rao, S, and Broadbear, J. Borderline personality disorder and depressive disorder. Australas Psychiatry. (2019) 27:573–7. doi: 10.1177/1039856219878643
55. Luca, M, Luca, A, and Calandra, C. Borderline personality disorder and depression: an update. Psychiatry Q. (2012) 83:281–92. doi: 10.1007/s11126-011-9198-7
56. First, MB, Williams, JBW, Karg, RS, and Spitzer, RL. Structured clinical interview for DSM-5—research version (SCID-5 for DSM-5, research version; SCID-5-RV). American Psychiatric Association: Arlington, VA (2015).
57. Dell'Osso, L, Carpita, B, Bertelloni, CA, Diadema, E, Barberi, FM, Gesi, C, et al. Subthreshold autism spectrum in bipolar disorder: prevalence and clinical correlates. Psychiatry Res. (2019) 281:112605. doi: 10.1016/j.psychres.2019.112605
58. Dell’Osso, L, Amatori, G, Massimetti, G, Nardi, B, Gravina, D, Benedetti, F, et al. Investigating the relationship between autistic traits and symptoms and Catatonia Spectrum. Eur Psychiatry. (2022) 65:e81. doi: 10.1192/j.eurpsy.2022.2334
59. Ungvari, GS, Caroff, SN, and Gerevich, J. The catatonia conundrum: evidence of psychomotor phenomena as a symptom dimension in psychotic disorders. Schizophr Bull. (2010) 36:231–8. doi: 10.1093/schbul/sbp105
60. Paris, J. Suicidality in borderline personality disorder. Medicina. (2019) 55:223. doi: 10.3390/medicina55060223
61. Oumaya, M, Friedman, S, Pham, A, Abou Abdallah, T, Guelfi, JD, and Rouillon, F. Personnalité borderline, automutilations et suicide: revue de la littérature [Borderline personality disorder, self-mutilation and suicide: literature review]. Encéphale. (2008) 34:452–8. doi: 10.1016/j.encep.2007.10.007
62. Fink, M, and Taylor, MA. The many varieties of catatonia. Eur Arch Psychiatry Clin Neurosci. (2001) 251:I8–I13. doi: 10.1007/pl00014200
63. Trull, TJ, Useda, JD, Conforti, K, and Doan, BT. Borderline personality disorder features in nonclinical young adults: 2. Two-year outcome. J Abnorm Psychol. (1997) 106:307–14. doi: 10.1037//0021-843x.106.2.307
64. Zanarini, MC, Frankenburg, FR, Hennen, J, Reich, DB, and Silk, KR. The McLean study of adult development (MSAD): overview and implications of the first six years of prospective follow-up. J Personal Disord. (2005) 19:505–23. doi: 10.1521/pedi.2005.19.5.505
65. Axelson, D, Birmaher, B, Strober, M, Gill, MK, Valeri, S, Chiappetta, L, et al. Phenomenology of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. (2006) 63:1139–48. doi: 10.1001/archpsyc.63.10.1139
66. Rydén, G, Rydén, E, and Hetta, J. Borderline personality disorder and autism spectrum disorder in females: a cross-sectional study. Clin Neuropsychiatry. (2008) 5:22–30.
67. Wing, L, and Shah, A. Catatonia in autistic spectrum disorders. Br J Psychiatry. (2000) 176:357–62. doi: 10.1192/bjp.176.4.357
68. Vaquerizo-Serrano, J, Salazar De Pablo, G, Singh, J, and Santosh, P. Catatonia in autism spectrum disorders: a systematic review and meta-analysis. Eur Psychiatry. (2021) 65:e4. doi: 10.1192/j.eurpsy.2021.2259
69. Fink, M, and Shorter, E. Does persisting fear sustain catatonia? Acta Psychiatr Scand. (2017) 136:441–4. doi: 10.1111/acps.12796
70. Shorter, E, and Fink, M. The madness of fear: a history of catatonia. Oxford, UK: Oxford University Press (2018).
71. Zingela, Z, Stroud, L, Cronje, J, Fink, M, and van Wyk, S. The psychological and subjective experience of catatonia: a qualitative study. BMC Psychol. (2022) 10:173. doi: 10.1186/s40359-022-00885-7
72. Kato, K, Mikami, K, Akama, F, Yamada, K, Maehara, M, Kimoto, K, et al. Clinical features of suicide attempts in adults with autism spectrum disorders. Gen Hosp Psychiatry. (2013) 35:50–3. doi: 10.1016/j.genhosppsych.2012.09.006
73. Shtayermman, O. Peer victimization in adolescents and young adults diagnosed with Asperger’s syndrome: a link to depressive symptomatology, anxiety symptomatology and suicidal ideation. Issues Compr Pediatr Nurs. (2007) 30:87–107. doi: 10.1080/01460860701525089
74. Dell’Osso, L, Lorenzi, P, and Carpita, B. Camouflaging: psychopathological meanings and clinical relevance in autism spectrum conditions. CNS Spectr. (2021) 26:437–9. doi: 10.1017/S1092852920001467
75. Hull, L, Mandy, W, Lai, MC, Baron-Cohen, S, Allison, C, Smith, P, et al. Development and validation of the camouflaging autistic traits questionnaire (CAT-Q). J Autism Dev Disord. (2019) 49:819–33. doi: 10.1007/s10803-018-3792-6
76. Brüne, M. Ethological remarks on mannerisms. Conceptualisation and proposal for a definition. Off. Psychopathology. (1998) 31:188–96. doi: 10.1159/000029039
77. Cassidy, SA, Gould, K, Townsend, E, Pelton, M, Robertson, AE, and Rodgers, J. Is camouflaging autistic traits associated with suicidal thoughts and behaviours? Expanding the interpersonal psychological theory of suicide in an undergraduate student sample. J Autism Dev Disord. (2020) 50:3638–48. doi: 10.1007/s10803-019-04323-3
78. Hull, L, Petrides, KV, Allison, C, Smith, P, Baron-Cohen, S, Lai, MC, et al. "Putting on my best normal": social camouflaging in adults with autism spectrum conditions. J Autism Dev Disord. (2017) 47:2519–34. doi: 10.1007/s10803-017-3166-5
79. Grant, JE, and Phillips, KA. Recognizing and treating body dysmorphic disorder. Ann Clin Psychiatry. (2005) 17:205–10. doi: 10.1080/10401230500295313
Keywords: catatonia spectrum, mood disorder, major depression disorder (MDD), borderline personality disorder (BPD), suicide, catatonic traits, catatonia, autistic-catatonic continuum
Citation: Dell’Osso L, Nardi B, Bonelli C, Gravina D, Benedetti F, Amatori G, Battaglini S, Massimetti G, Luciano M, Berardelli I, Brondino N, De Gregorio M, Deste G, Nola M, Reitano A, Muscatello MRA, Pompili M, Politi P, Vita A, Carmassi C, Cremone IM, Carpita B and Maj M (2023) Investigating suicidality across the autistic-catatonic continuum in a clinical sample of subjects with major depressive disorder and borderline personality disorder. Front. Psychiatry. 14:1124241. doi: 10.3389/fpsyt.2023.1124241
Edited by:
Soumitra Das, NorthWestern Mental Health, AustraliaReviewed by:
Giovanni Martinotti, University of Studies G. d’Annunzio Chieti and Pescara, ItalyRohan Mendonsa, Melbourne Health, Australia
Copyright © 2023 Dell’Osso, Nardi, Bonelli, Gravina, Benedetti, Amatori, Battaglini, Massimetti, Luciano, Berardelli, Brondino, De Gregorio, Deste, Nola, Reitano, Muscatello, Pompili, Politi, Vita, Carmassi, Cremone, Carpita and Maj. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Benedetta Nardi, YmVuZWRldHRhLm5hcmRpQGxpdmUuaXQ=
 Liliana Dell’Osso1
Liliana Dell’Osso1 Benedetta Nardi
Benedetta Nardi Chiara Bonelli
Chiara Bonelli Davide Gravina
Davide Gravina Giulia Amatori
Giulia Amatori Mario Luciano
Mario Luciano Isabella Berardelli
Isabella Berardelli Natascia Brondino
Natascia Brondino Giacomo Deste
Giacomo Deste Marta Nola
Marta Nola Antonino Reitano
Antonino Reitano Maria Rosaria Anna Muscatello
Maria Rosaria Anna Muscatello Maurizio Pompili
Maurizio Pompili Pierluigi Politi
Pierluigi Politi Antonio Vita
Antonio Vita Claudia Carmassi
Claudia Carmassi Ivan Mirko Cremone
Ivan Mirko Cremone Barbara Carpita
Barbara Carpita