- 1School of Health Preservation and Rehabilitation, Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 2Department of Rehabilitation, The Third Hospital of Mianyang, Sichuan Mental Health Center, Mianyang, China
- 3Department of rehabilitation, Mianyang Hospital of Traditional Chinese Medicine, Mianyang, China
- 4Mental Health Center, West China Hospital, West China School of Medicine, Sichuan University, Chengdu, China
Background: Depression is a mental health disorder characterized by affective, somatic, and cognitive symptoms. Attention bias modification (ABM) has been widely used to treat depression. However, the results seem inconsistent. We conducted a systematic review and meta-analysis to investigate the efficacy of ABM for depression and to explore the optimal protocol of ABM.
Methods: Seven databases were systematically searched from their inceptions to 5 October 2022 to include randomized controlled trials (RCTs) of ABM for depression. Two independent reviewers selected the eligible articles, extracted data, and evaluated the risk of bias using version 2 of the Cochrane risk-of-bias tool (ROB 2.0) for randomized trials. The primary outcome was the evaluation of depressive symptoms using widely accepted and validated scales. The secondary outcomes included rumination and attentional control. Meta-analysis was conducted by using RevMan (version 5.4) and Stata (version 12.0). Subgroup analyses and meta-regressions were performed to identify the source of heterogeneity. The certainty of the evidence was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE).
Results: A total of 19 trials involving 20 datasets (1,262 participants) were included. The overall risk of bias in one study was rated as low risk of bias, three studies were considered as high, and the remaining studies were some concerns. Compared with attention control training (ACT), ABM had a greater effect in the improvement of depression (SMD = −0.48, 95% CI −0.80 to −0.17, I2 = 82%) and rumination (MD = −3.46, 95% CI −6.06 to −0.87, I2 = 0%). No significant differences were observed in the attentional control outcome between ABM and ACT (MD = 3.07, 95% CI −0.52 to 6.65, I2 = 0%). Subgroup analysis demonstrated that adults exhibited a greater decrease in depression scores than adolescents. ABM using the dot-probe task, training target stimulus presented by face, and training directions by left–right were associated with better antidepressant effects. ABM training delivered in the laboratory tended to yield a better effect than those conducted at home. Sensitivity analysis indicated that the results were robust. The certainty of the evidence for all outcomes was low or very low, and publication bias may exist.
Conclusion: Due to high heterogeneity and limited studies, not enough current evidence supported that ABM could be an effective intervention to relieve depressive symptoms. More rigorous RCTs are required to verify the benefits and to explore the optimal protocol of ABM training for depression.
Systematic Review Registration: [PROSPERO], identifier [No. CRD42021279163].
1. Introduction
Depression is a common mental disorder characterized by a persistent low mood and anhedonia, with an approximately 16% lifetime prevalence (1) and is affecting nearly 350 million individuals (2). Since the outbreak of the COVID-19 pandemic in 2019, 52 million new major depressive disorder cases had been diagnosed globally, with an increase of 27.6% (3). In the United States, the absence days from work due to depression were estimated to be 27.2 workdays per patient with depression a year (4), which brought a significant financial burden to patients, families, and society (5). According to the cognitive theory of depression, the acquisition and processing of information are considered to be significant contributors to the occurrence and development of depression (6). Individuals with depression are unable to process all sensory information equally, and they selectively tend to focus on negative emotional information (7, 8). Negative attentional bias and deficits in cognitive control may interfere with emotion regulation and mood state. The increased activation of subcortical emotion processing regions and a weakening of top-down cognitive control may be responsible for negative cognitive biases (9). At present, attention bias modification (ABM) for depressive individuals has attracted increasing attention.
As a type of cognitive bias modification, ABM utilizes computer-based attention training to directly modify aberrant attentional bias in patients with depression (10). ABM aims at increasing the process of neutral or positive stimulation to reduce negative attentional bias, thus regulating emotional function (11, 12). ABM relies on the automatic cognitive processing of altering motivation, rather than solely changing the content of individual behaviors (13–15). In recent years, several paradigms of ABM have been devised and applied, which include the dot-probe task (DPT), the spatial cueing task (SCT), and the free viewing task (FVT) (16). Clinical studies showed that ABM was able to reduce depressive symptoms in situations when negative attentional bias was successfully modified (17, 18). Therefore, ABM programs could be a promising treatment for depressive symptoms. In addition, considerable evidence indicated that ABM had a positive effect on other psychiatric disorders such as anxiety disorders (10, 19), social phobia (20), and obsessive–compulsive disorders (21, 22).
Previous meta-analyses (23–25) concluded that ABM was not effective for patients with depression. However, Yang et al. (17) found that ABM had a significant effect to decrease BDI scores when compared with the placebo condition. Woolridge et al. (26) discovered that ABM might be an optimal treatment to relieve depressive symptoms. Furthermore, the optimal protocols of ABM (e.g., task types, target stimulus, stimulus directions, and training settings) for depression remain unknown. As more relevant trials have been conducted in recent years, we performed this systematic review (SR) and meta-analysis to update the evidence on the effect of ABM on depression and to explore the optimal protocols of ABM.
2. Methods
The protocol of this SR and meta-analysis has been registered on the International Prospective Register of Systematic Reviews (PROSPERO).1 We conducted this SR and meta-analysis according to A Measurement Tool to Assess Systematic Reviews 2 (AMSTAR 2) (27) and reported conforming to the preferred reporting items for systematic reviews and meta-analyses (PRISMA 2020) statement criteria (28) (Supplementary Appendix 1).
2.1. Search strategy
Two reviewers independently (HSX and XYG) searched PubMed, Embase, the Cochrane Library, Chinese National Knowledge Infrastructure (CNKI), Wanfang Database, Chinese Biomedical Literature Database (CBM), and China Science and Technology Journal Database (VIP) from their inceptions to 5 October 2022. Search terms used depression, attention bias modification, and randomized controlled trial. The full search strategies for all databases are shown in Supplementary Appendix 2. We manually searched the reference lists of all identified articles, gray literature, and relevant registration websites2 for possible eligible studies. In addition, we consulted the relevant experts for potential studies.
2.2. Inclusion criteria
Studies were included if they fulfilled all the inclusion criteria: (1) Patients diagnosed with depression based on the Diagnostic and Statistical Manual of Mental Disorders (DSM) (29), International Classification of Diseases (ICD) (30), Chinese Classification and Diagnosis of Mental Diseases (CCMD), or validated scales (24, 31). There were no restrictions on race, gender, or age. (2) Intervention included ABM alone, or ABM plus conventional treatment (CT). CT contained medication and psychological intervention. There were no limitations on task types, stimulus types, and training directions of ABM. (3) Participants in the control group received attention control training (ACT) alone, ACT plus CT, or CT alone. (4) The primary outcome was depressive symptoms evaluated with widely accepted and validated scales. Secondary outcomes included rumination and attentional control. (5) RCTs that investigated the effect of ABM on patients with depression were included.
2.3. Exclusion criteria
Studies were excluded if they met any of the following criteria: (1) studies using interpretation bias modification; (2) cross-over RCTs, review articles, and conference abstracts; (3) overlapping publications; (4) the full texts were not available through various approaches.
2.4. Study selection
Endnote X9 was used to manage the retrieved records. After removing duplicates, two independent reviewers (H-sX and X-bL) screened the titles and abstracts to identify the potential studies. Then, the rest records were scrutinized in full text. Any inconsistency was resolved through consultation with the third reviewer (JL). If multiple publications reported data from the same trial, we included the article with the most complete or latest data.
2.5. Data collection and extraction
Two independent reviewers (H-sX and X-yG) extracted data from included studies with a standard extraction form. The following data were extracted: (1) study information: first author, publication year, and country; (2) participant characteristics: diagnostic criteria, sample size, and age; (3) details of interventions: types, paradigms, stimulus types, stimulus directions, sessions, and total trials of per session; (4) comparators: types of intervention, frequency, and duration; (5) primary outcome and secondary outcomes; (6) information related to the risk of bias. With regards to missing data, corresponding authors were contacted via email for missing or incomplete data. For multi-arm RCTs, we extracted the eligible comparisons or the comparison with an inferior effect size. If the data was displayed in the graph, the GetData Graph Digitizer 2.26 was used to extract the data. After cross-checking, disagreements were settled through consultation with an experienced reviewer (Y-xL).
2.6. Risk-of-bias assessment
Two researchers (JF and D-lZ) separately evaluated the risk of bias using version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2.0). There are five domains in RoB 2.0: randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported results. Each domain is rated as “low risk of bias,” “some concerns,” or “high risk of bias.” In case of disagreements, a third investigator (JL) was involved.
2.7. Certainty of The evidence
The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system was used to assess the certainty of the evidence of each outcome (32). Each outcome was evaluated from the following five aspects: limitations, inconsistency, indirectness, imprecision, and publication bias. The certainty of the evidence was categorized as “high,” “moderate,” “low,” or “very low.” (33).
2.8. Statistical analysis
Data synthesis was conducted using RevMan (version 5.4) and Stata (version 12.0). Among the included studies, different measurement tools were used to evaluate the symptoms of depression, and the standardized mean difference (SMD) was calculated (34–36). The ability of attention control among the included studies was evaluated using an attention control scale (ACS), and the ruminative symptoms were assessed with a ruminative response scale (RRS); thus, weighted mean difference (WMD) was used to synthesize these results. The uncertainty was expressed with 95% confidence intervals (CIs). The statistical heterogeneity across the included studies was assessed by the Chi-squared test and I2 statistic. The fixed-effect model was performed when p > 0.1 or I2 values < 50%. Otherwise, the random-effect model was used. Forest plots were used to display the pooled estimates, and a value of p < 0.05 was regarded as statistically significant. If the pooled data could not be synthesized, we conducted the descriptive analysis.
2.9. Subgroup analysis and meta-regressions
Subgroup analyses were conducted according to age, task types, training target stimuli, training directions, and training settings, whereas meta-regressions were performed based on BDI scores at baseline, publication year, gender, number of training sessions, and number of training trials per session.
2.10. Sensitivity analysis
The sensitivity analysis was conducted by eliminating studies with a high risk of bias to verify the robustness of the results.
2.11. Publication bias
The funnel plot was used to assess possible publication bias when ≥10 studies were included in the analysis.
3. Result
3.1. Selection and inclusion of studies
A total of 2,560 articles were identified. After removing 513 duplicates, 2,004 articles did not conform with the eligible criteria and were excluded. Among the remaining 43 records, 24 studies were excluded after reviewing the full text. Then, we included 20 datasets from 19 reports. The diagram of the screening process is shown in Figure 1. The list of excluded records with reasons is provided in Supplementary Appendix 3.
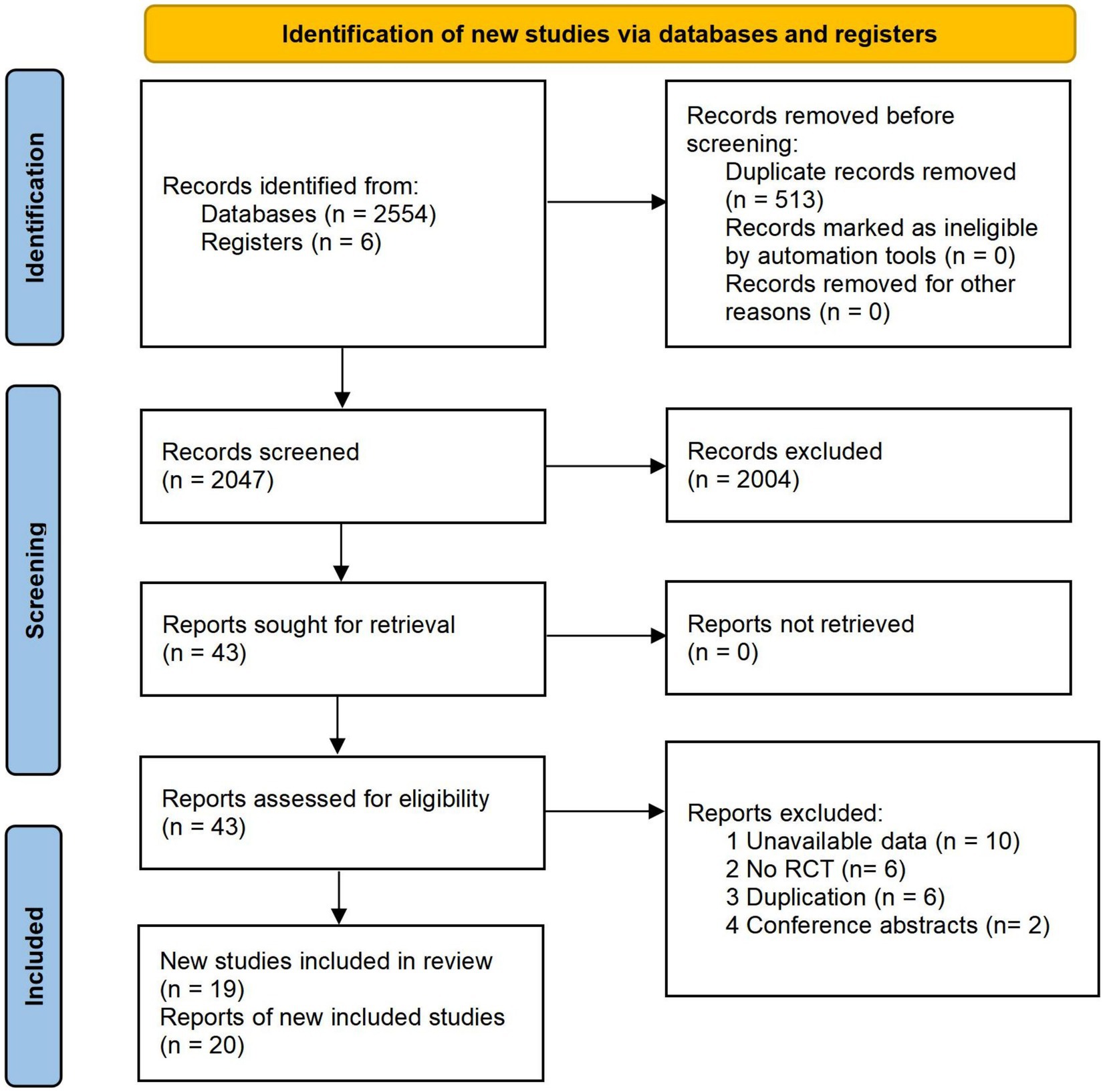
Figure 1. Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow chart of literature searching and screening.
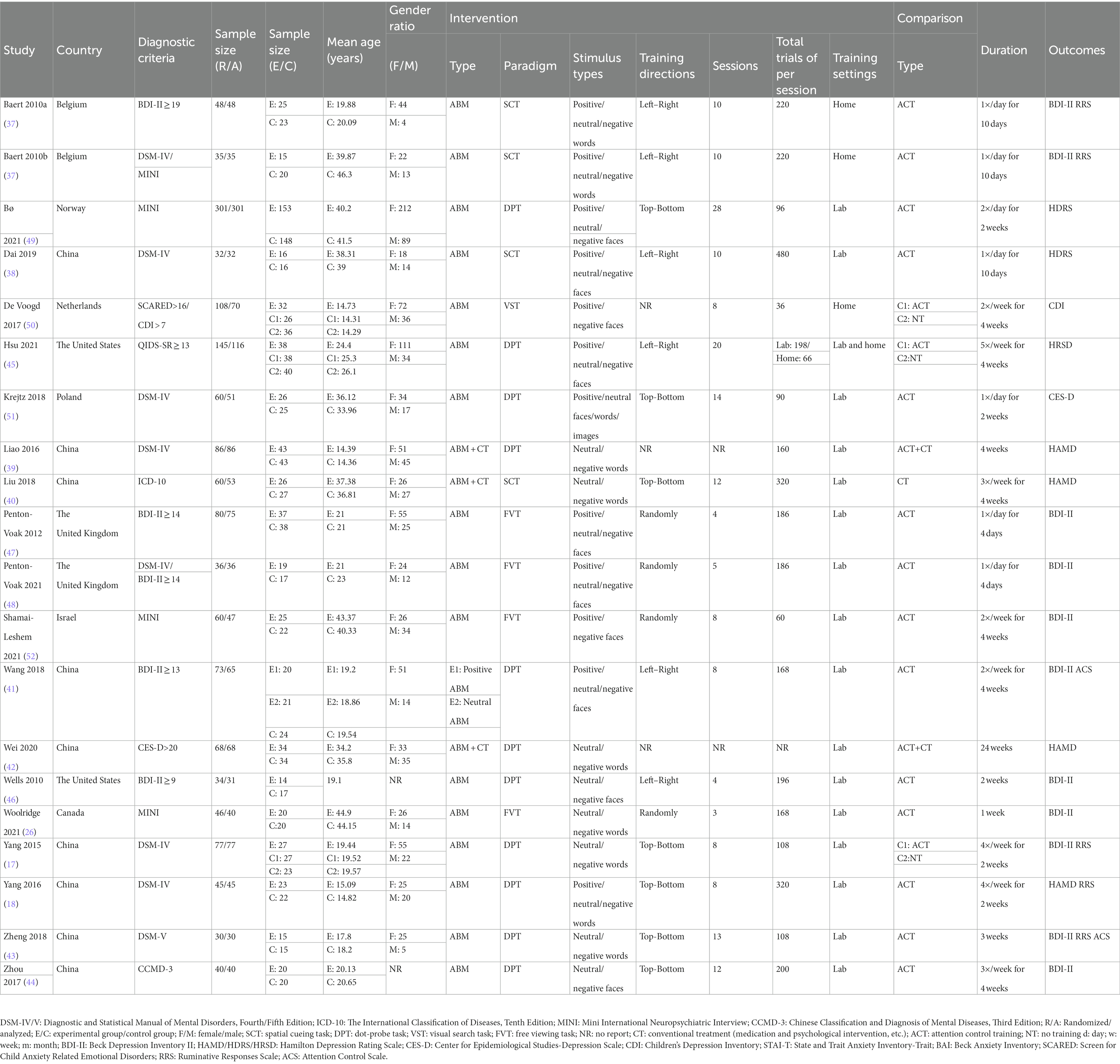
3.2. Characteristics of included studies
The characteristics of the included trials are shown in Table 1. A total of 19 trials involving 20 datasets with 1,262 patients with depression were included, wherein Baert et al. (37) observed the effect of ABM for patients with depression diagnosed by DSM-IV criteria and BDI-II scales separately; therefore, we extracted these two datasets, respectively. Among included studies, nine studies were performed in China (17, 18, 39, 43, 44, 48, 49, 51, 52), two were in Belgium (37), two were in the United States (41, 50), two were in the United Kingdom (45, 46), and one in Norway (38), Netherlands (40), Poland (42), Israel (47), and Canada (26). The sample size of these studies varied from 30 to 301. The age of the included patients ranged from 14 to 45. Sixteen studies involved adults (17, 26, 37–39, 41, 42, 44–50, 52), and four studies included adolescents (18, 40, 43, 51). Among included studies, four studies were three-arm trials (17, 40, 41, 48), and the rest studies were two-arm trials. As for comparison, 17 studies compared ABM with ACT (17, 18, 26, 37–42, 45–48, 50–52), two studies compared ABM plus CT versus ACT plus CT (43, 49), and only one study compared ABM plus CT versus CT (44). The number of training sessions ranged from 1 to 28, and the duration of training was between 1 and 4 weeks.
3.3. Risk of bias In studies
The plot of the risk of bias (RoB 2.0) for each included study is presented in Figure 2, and the proportions of individual studies are presented in Figure 3.
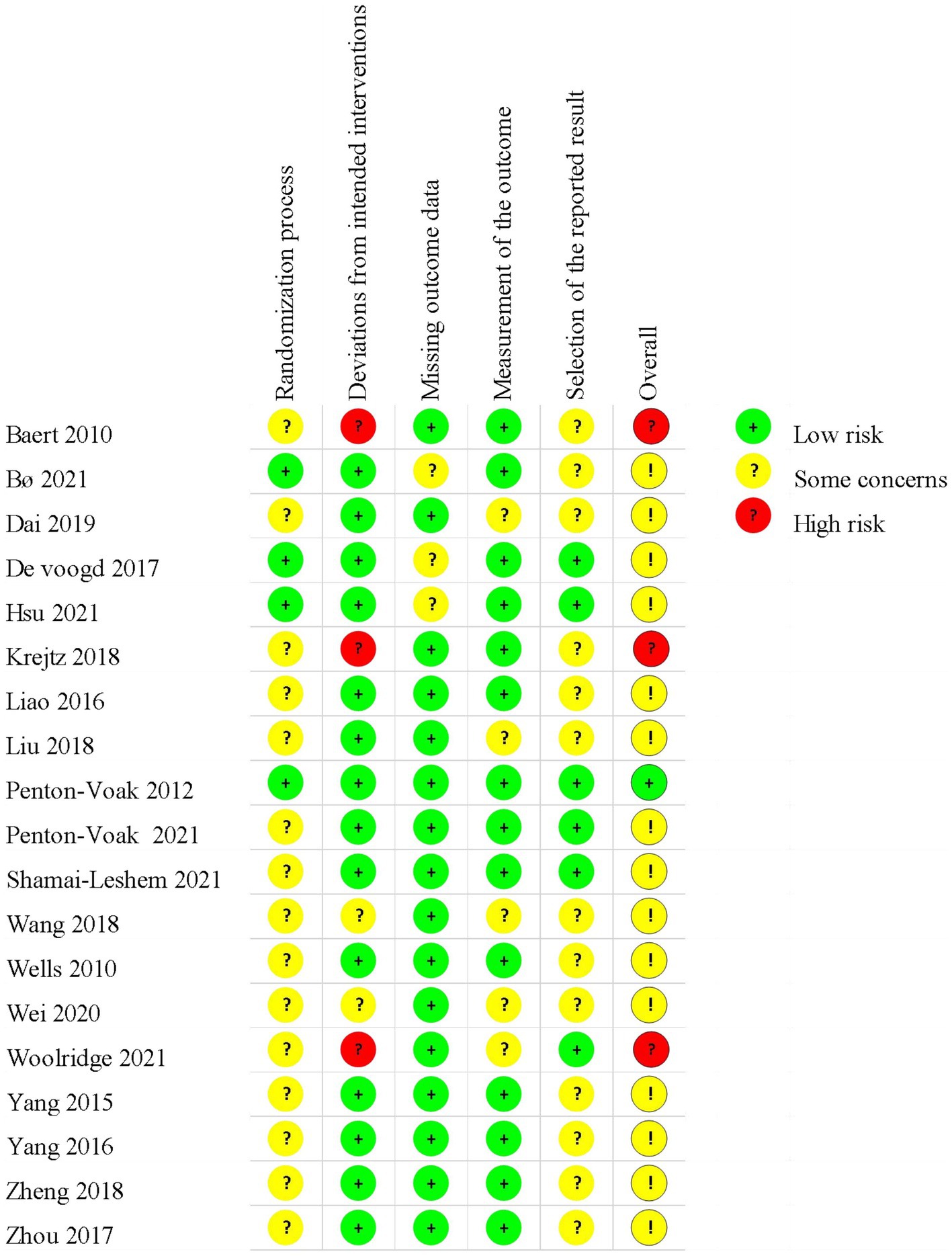
Figure 2. Results of risk-of-bias (RoB 2.0) assessment. The plot of RoB 2.0 for each included study.
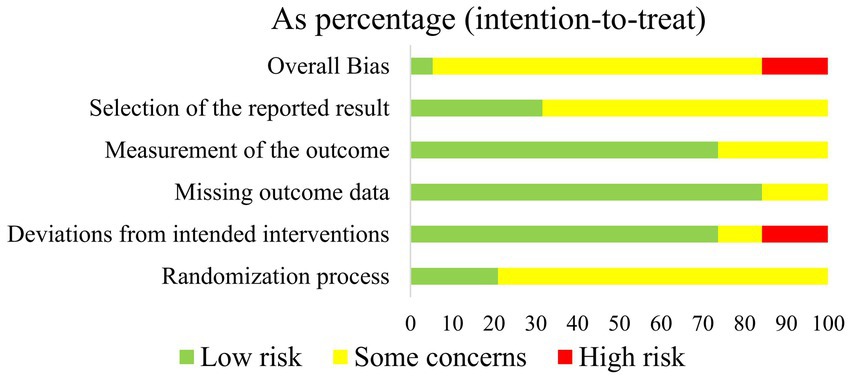
Figure 3. Results of risk-of-bias (RoB 2.0) assessment. Proportions of individual study for each domain.
In the randomization process, all included studies showed no statistically significant difference between groups at baseline. Four studies (38, 40, 41, 45) were judged as low risk, while the rest 15 studies were assessed as having some concerns due to no details of randomization or allocation concealment.
Considering the deviation from intended interventions, 14 trials (17, 18, 38–43, 45–47, 50–52) performed appropriate analysis on all randomly assigned participants, which were judged as low risk of bias. Two studies (48, 49) did not report blinding, which was considered as some concerns. The remaining three trials (26, 37, 44) were regarded as high risk due to no blinding in outcome assessors and inappropriate analysis.
As for the missing outcome, 13 studies (17, 18, 26, 37–42, 44, 45, 47, 51) reported the number of drop-outs or lost to follow-up. Among these studies, three studies (38, 40, 41) did not report the details of drop-outs, which were rated as some concerns.
With regard to the measurement of outcomes, six studies (26, 37, 39, 44, 48, 49) were assessed as some concerns due to the lack of a blinding method of outcome assessors. The remaining 13 studies were a low risk of bias.
For the selection of the reported results, six trials (26, 40, 41, 45–47) provided protocol information and reported most of the expected outcomes comprehensively, which were considered as low risk. The rest trials did not provide protocol information, which was assessed as some concerns.
In summary, the overall risk of bias in one trial was considered as low risk, three trials were considered as high risk, and the remaining were considered as some concerns.
3.4. Results of the meta-analysis
3.4.1. Primary outcome (depression)
3.4.1.1. ABM versus ACT
A total of 16 trials (17, 18, 26, 37–42, 45–48, 50–52) involving 17 datasets reported depressive symptoms. The results demonstrated that ABM was superior to ACT in reducing depressive symptoms (SMD = −0.48, 95% CI −0.80 to −0.17, I2 = 82%; Figure 4A). By exploring heterogeneity, we found the risk of bias in Baert et al. (37), Krejtz et al. (42), and Woolridge et al. (26) were high, while the risk-of-bias assessment in other studies was identified as low risk or some concerns. After removing these datasets (26, 37, 42) with a high risk of bias, sensitivity analysis showed that the overall effects did not change (SMD = −0.35, 95% CI −0.61 to −0.10, I2 = 66%; Figure 4B).
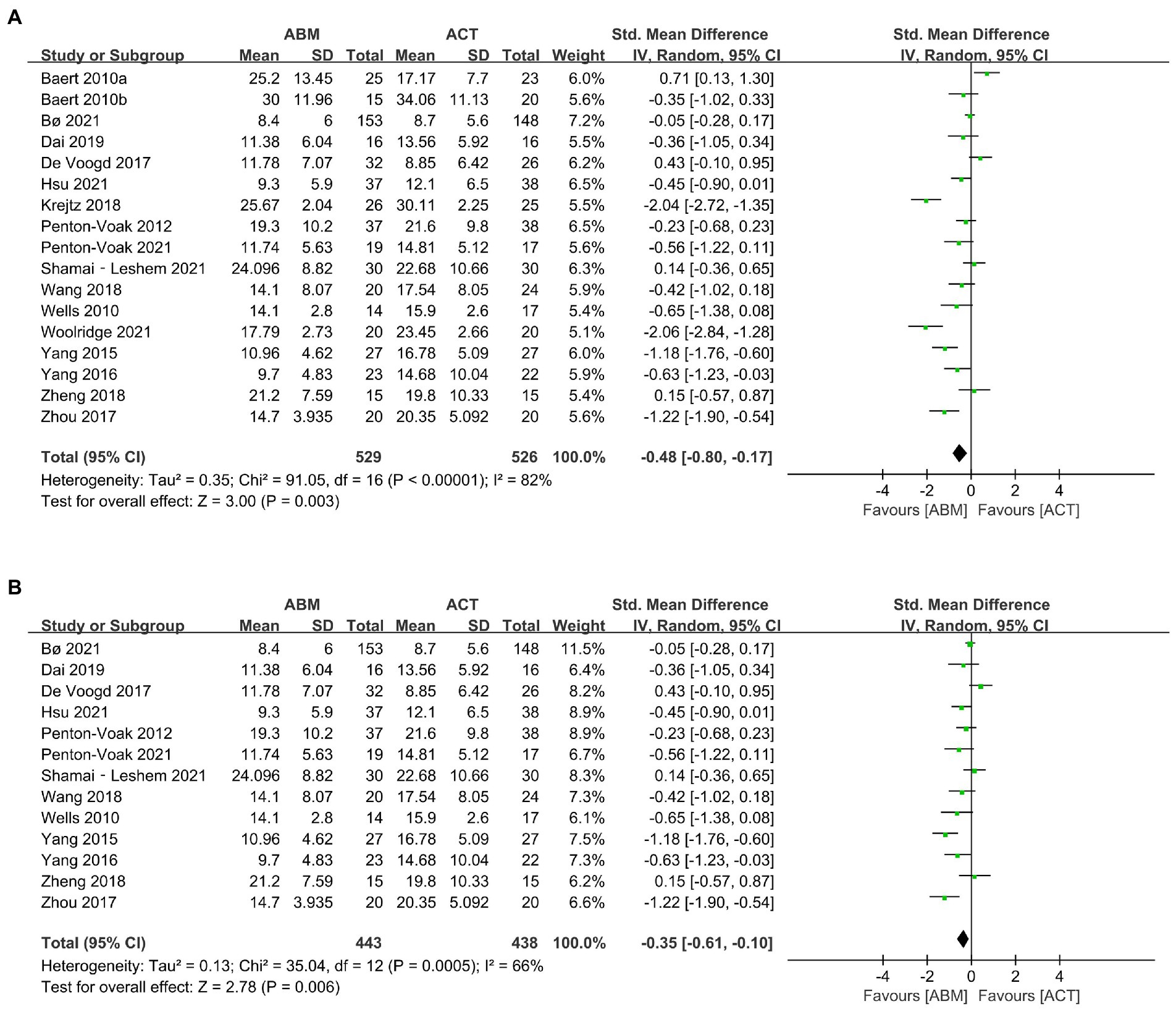
Figure 4. (A) Forest plot of depression outcome in comparison with attention bias modification (ABM) versus attention control training (ACT). (B) Forest plot of depression outcome in comparison with ABM versus ACT after removing high risk-of-bias studies.
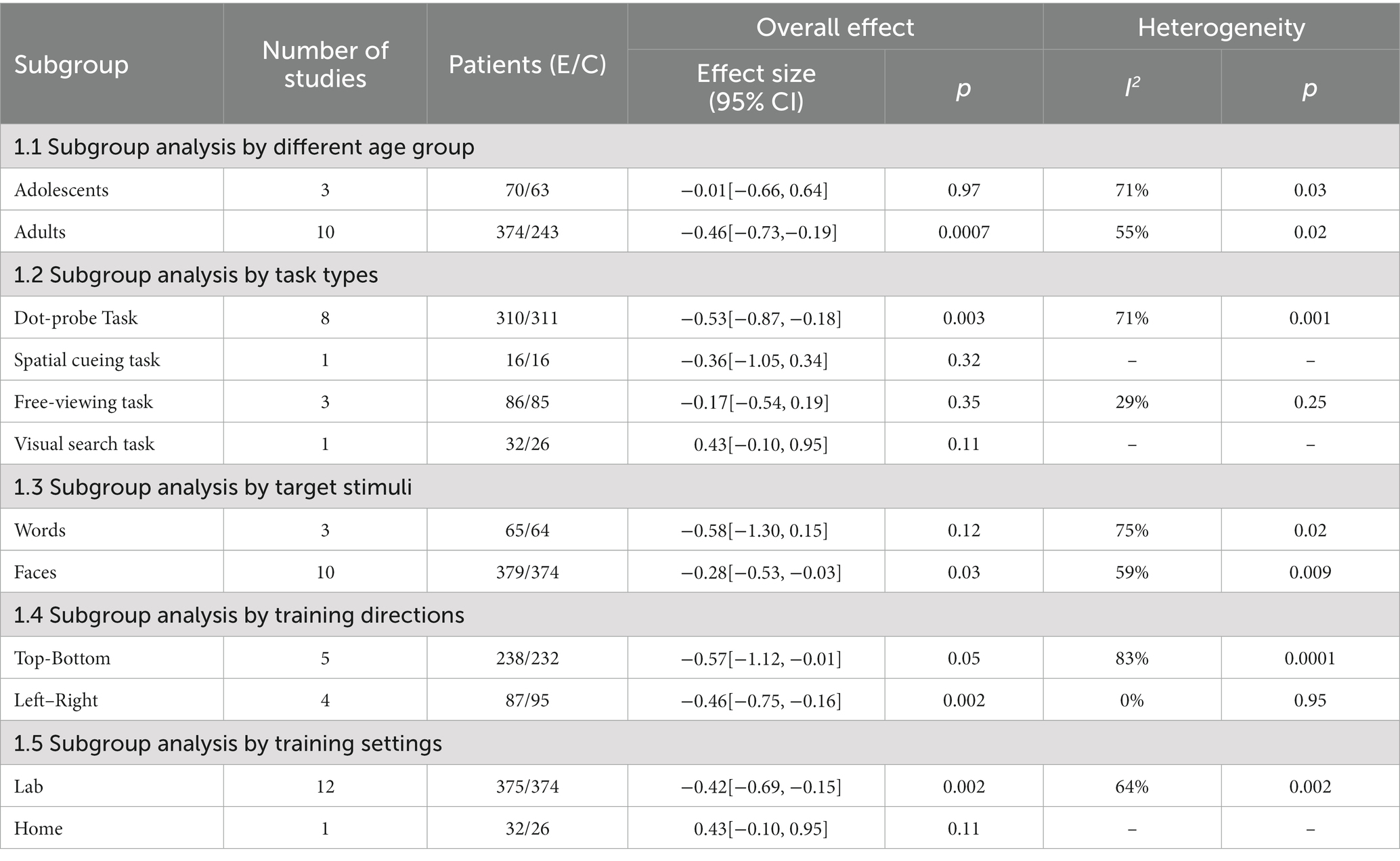
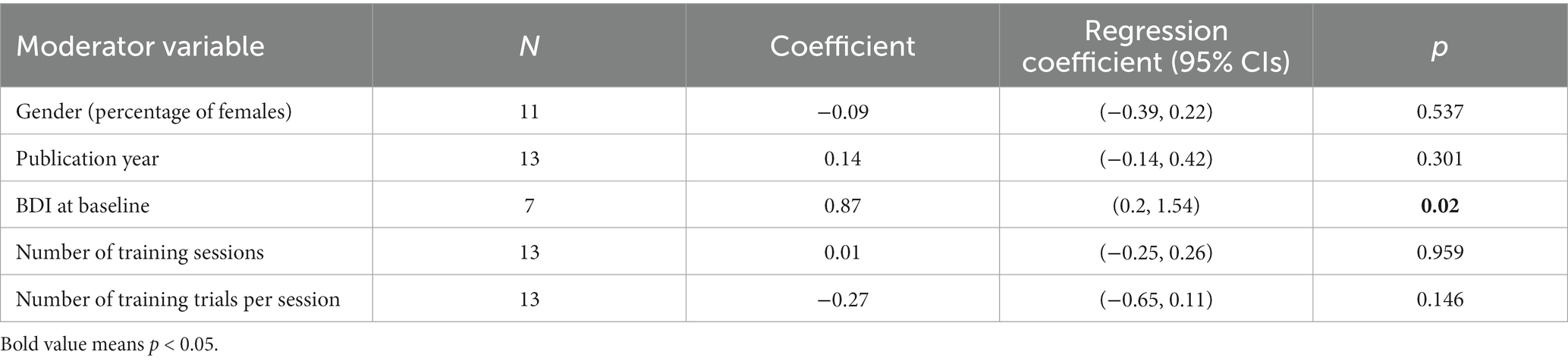
3.4.1.1.1. Subgroup and meta-regression analysis
As depicted in Table 2, the subgroup analysis showed that adults had greater improvement in depression than adolescents. Regarding types of task, ABM using dot-probe task was more effective to relieve depressive symptoms than the ACT, while ABM with spatial cueing, visual search, or free viewing task had no effect. As for the training target stimuli, ABM using face stimulus had a significantly larger effect than those using word stimulus. Concerning training directions, ABM with left–right training alleviated more depressive symptoms than the ACT, while those presented by top-bottom training did not. In addition, the training delivered in the laboratory tended to yield a better effect than those conducted at home.
We performed meta-regression in accordance with gender (percentage of females; range 43.3–83.3%), publication year (range 2010–2021), BDI at baseline (range 17.1–29.94 scores), number of training sessions (range 4–28 sessions), and number of training trials per session (range 36–480 trials). The results indicated that BDI at baseline was a moderator of the ABM, lower BDI at baseline benefited more from ABM (Table 3).
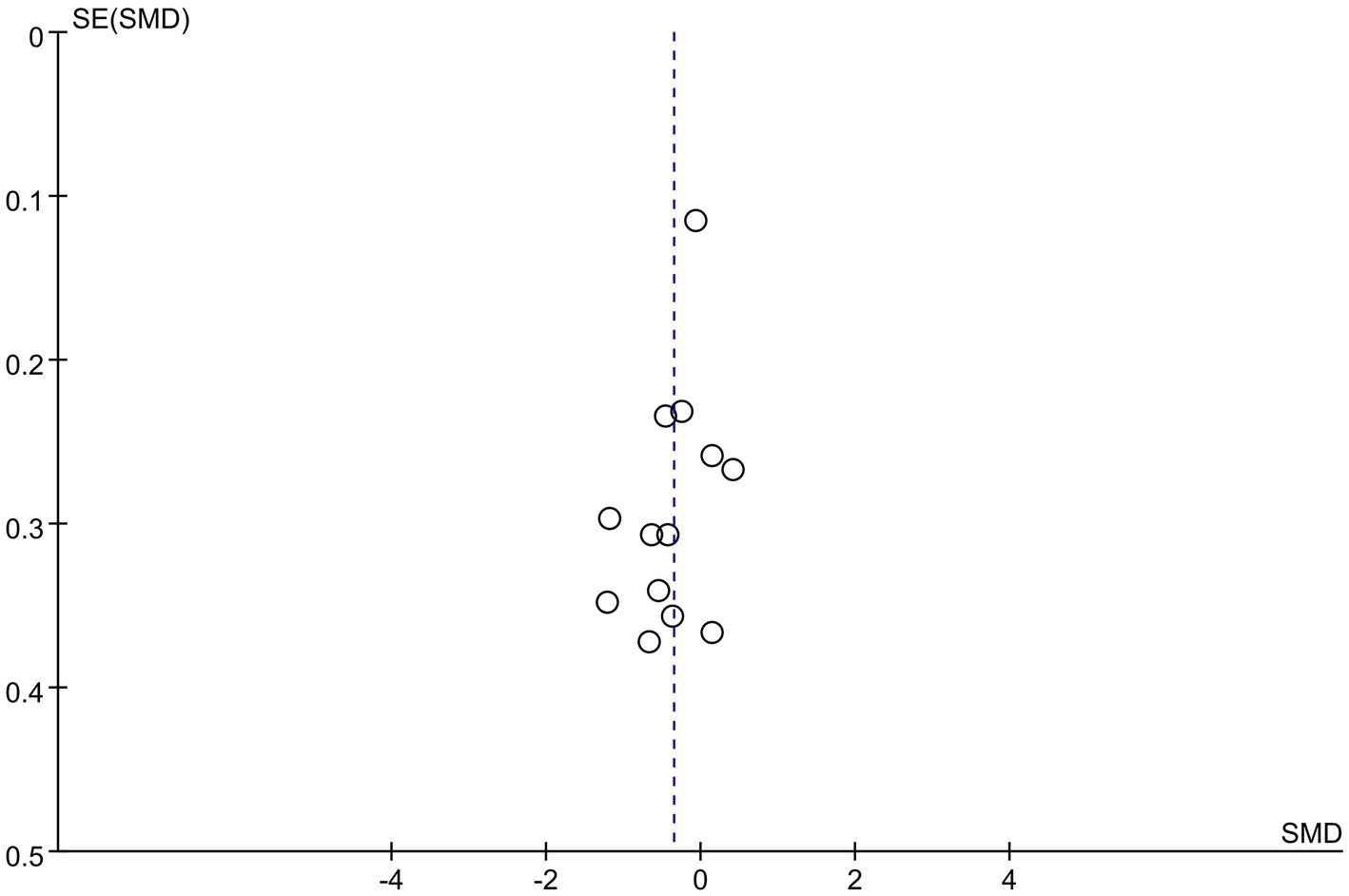
3.4.1.1.2. Publication bias
The funnel plot was asymmetry, which indicated publication bias existed (Figure 5).
3.4.1.2. ABM plus CT versus ACT plus CT
No difference was identified between ABM plus CT and ACT plus CT in alleviating depressive symptoms (SMD = −0.11, 95% CI −0.43 to 0.21), I2 = 0%) (43, 49).
3.4.1.3. ABM plus CT versus CT
Liu et al. (44) revealed that ABM plus CT had a better improvement in depressive symptoms than CT (p < 0.05).
3.4.2. Secondary outcomes
3.4.2.1. Rumination (ABM versus ACT)
Four trials (17, 18, 37, 51) involving five datasets with 212 participants compared the effects of ABM with ACT for rumination. We found ABM was superior to ACT in relieving ruminative symptoms of patients with depression (MD = −3.46, 95% CI −6.06 to −0.87, I2 = 0%; Figure 6A). According to sensitivity analysis, the results of rumination remained unchanged after excluding 2 datasets with a high risk of bias (37) (MD = −4.10, 95% CI −6.95 to −1.26, I2 = 0%; Figure 6B).
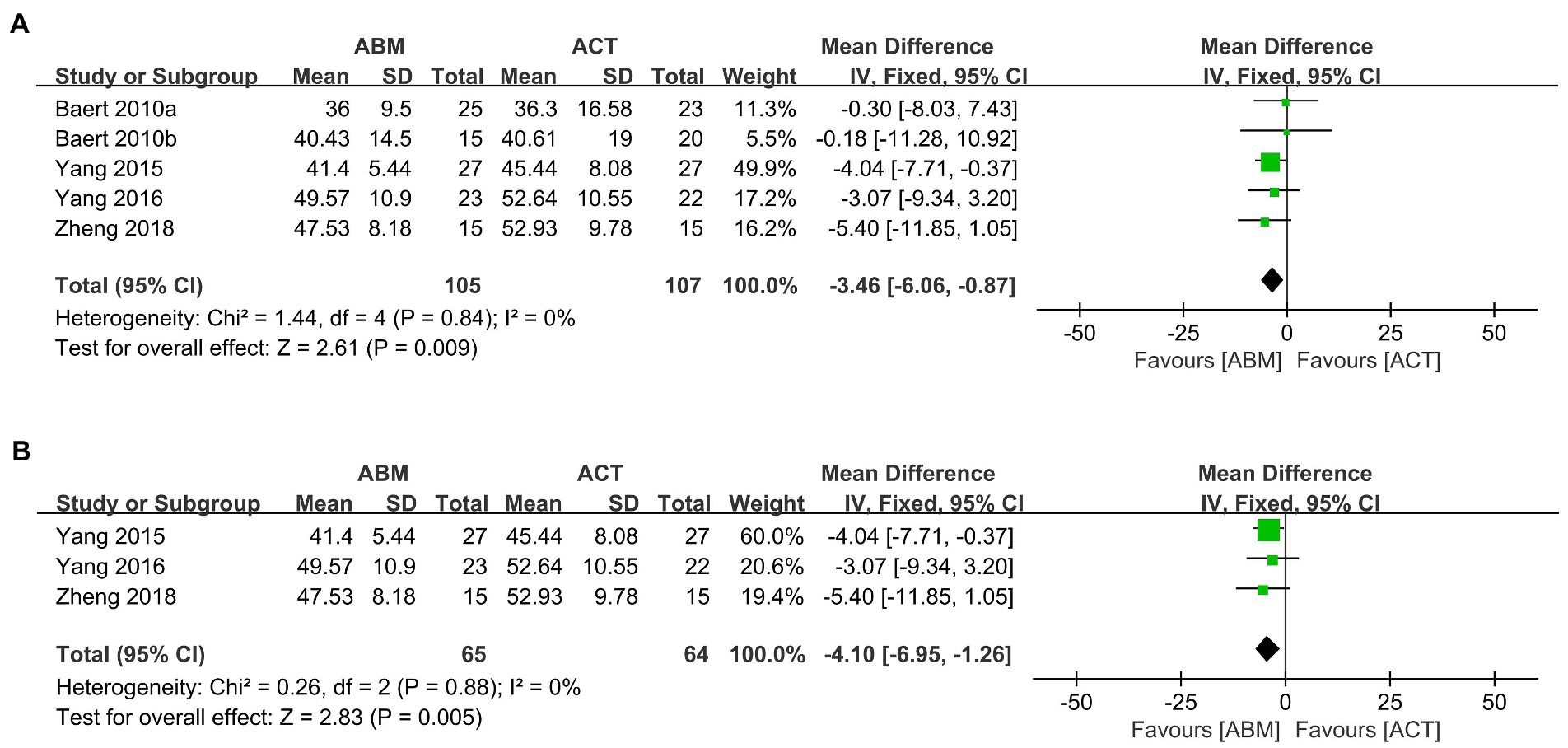
Figure 6. (A) Forest plot of rumination outcome in comparison with ABM versus ACT. (B) Forest plot of rumination outcome in comparison with ABM versus ACT after removing high risk-of-bias studies.
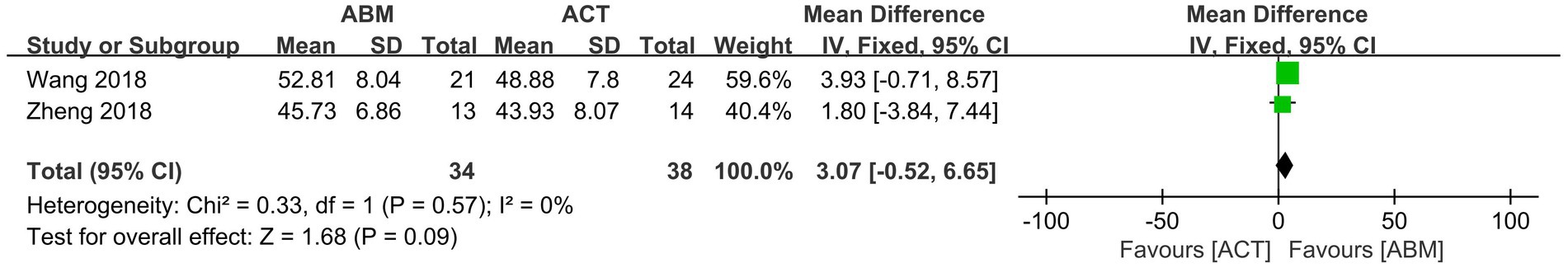
3.4.2.2. Attention control ability (ABM versus ACT)
According to two studies (48, 51), ABM did not differ from ACT in improving attention control scores (MD = 3.07, 95% CI −0.52 to 6.65), I2 = 0%; Figure 7).
3.5. Certainty of the evidence
The results of the GRADE are shown in Supplementary Appendix 4. The certainty of the evidence of depression (ABM plus CT versus ACT plus CT) was graded as “moderate,” and the rest outcomes were considered as low or very low. The reasons for downgrading were mainly attributed to the risk of bias of included studies and imprecision and publication bias generated by small sample sizes.
4. Discussion
4.1. The effect of ABM on depression
Due to limited RCTs, previous meta-analyses demonstrated that ABM had no effect on relieving depressive symptoms (23, 24, 53). In the present meta-analysis, with 20 RCTs included, the synthesized data indicated that ABM might be an effective treatment for depressive disorder. Neurophysiologic studies have confirmed that ABM could modify functional brain connectivity within neural networks related to attentional control (54, 55). Specifically, Beaver’s study (56) found that ABM could reduce negative attention bias and enhance connectivity between the middle frontal gyrus and the dorsal anterior cingulate cortex (ACC). The dorsal ACC involves in attention control through connections with other frontal regions and plays an important role in the cognitive regulation of emotional information. Another study highlighted that greater activation in the lateral prefrontal cortex (PFC) and rostral ACC was observed when the direction of patients’ attention was opposite to ABM training (54). Hakamata et al. discovered that ABM enhanced the pulvinar control over the ventral frontoparietal network (vFPN) to maintain endogenous attention to behavioral targets and diminished the information exchanges between the postcentral gyrus and vFPN to inhibit the capture of exogenous attention by potential threats (57). Moreover, ABM could increase the levels of cortisol awakening responses, which were related to the development and progression of depression (58). Nevertheless, the mechanism of ABM for depression needs further exploration.
4.2. The effect of ABM on rumination
Significant reduction in rumination after ABM treatment was noted in our study. Depressive rumination is defined as a maladaptive emotion regulation strategy, which focuses one’s attention on sad mood and negative thoughts (59). The current study revealed that rumination was associated with negative attention bias and attentional control deficits with depression (60). Nolen-Hoeksema et al. (61) conducted a 3-year follow-up visit of 82 patients with depression and found individuals who engaged in rumination were more likely to develop depressive disorders. In addition, several studies concluded that ABM could decrease maladaptive ruminative processing by reducing negative attention bias, thus producing antidepressant effects (17, 62, 63). These findings suggested that ABM was able to promote resilience to the normal pattern of emotional regulation in depression by reducing rumination.
4.3. The effect of ABM on attentional control
Attentional control is a type of cognitive control schema and defined as the effortful allocation of attention toward goal-relevant information in the face of conflicting prepotent attentional demands (64). Evidence showed that patients with depression manifested hypoactivation in cortical structures of attentional control, which might be related to the impairment of cognitive performance (65). Attentional control appears to have an impact on depressive symptoms through rumination, and poor mood states can be regulated by improving attention control performance (65). Previous studies discovered that ABM might enhance attentional performance through the repetitive activation of neural circuitry with information processing and attentional control (62). However, based on limited studies, the results of our data showed that ABM was not effective to improve attentional control. Wang et al. (48) interpreted that long material presentation times may cause patients with depression to induce attentional avoidance toward negative stimuli in the later stages of attention processing. Therefore, the effect of ABM on attention control requires further investigation.
4.4. The protocol of ABM on depression
According to subgroup analysis, ABM training with the dot-probe task was more effective than ACT in reducing depression scores. It is reported that the dot probe has increasingly become an optimal type for attentional modulation (66, 67). However, Robert et al. (68) argued that the dot-probe task was not reliable in measuring reaction time, thus limiting its application in clinical practice. Future studies should identify the reliability of the dot-probe task for depression and compare the effect of different ABM tasks.
Our studies showed that ABM using training direction presented by left–right had a larger effect, while those using top-bottom training did not. Heeren et al. (69) explained that it was more ecologically relevant than processing faces presented horizontally rather than vertically. In contrast, Hakamata et al. (19) and Beard et al. (70) found that top-bottom training had a better effect than those with left–right. Different ABM protocols such as stimuli types or stimuli presentation time may be the reasons for the inconsistent findings.
Regarding training target stimuli, ABM using face stimulus was superior to those using word stimulus in our study. Similarly, Browning et al. (58) found that ABM training with face stimulus reduced the risk of depression, while ABM with word stimulus did not produce such beneficial effects. Jones et al. (71) revealed that ABM studies benefited more from using word stimulus combined with top-down training than those using face stimulus combined with left–right training.
ABM training delivered in the laboratory tended to yield a larger effect than those conducted at home, which was consistent with previous studies (23, 24, 69). Heeren et al. (69) inferred that patients who received ABM training in the standardized laboratory were less susceptible to outside interference.
Of note, ABM appeared to be beneficial for depressive adults and had no effect on adolescents. However, Hang et al. (10) concluded that younger participants could benefit more from ABM as they have a greater potential for attention control. In addition, it has been reported that the cognitive abilities of normal adults may decline in their 20s and 30s (72). Since few studies pay attention to depressive adolescents, more studies are needed to verify this finding.
In addition, the results of meta-regression also showed that BDI scores at baseline were the influencing factor of ABM, and lower BDI scores at baseline yielded a larger effect. Li et al. (73) found that severely depressive individuals exhibited deficits in executive function and attention compared to those with mild depression. A neuroimaging study showed that severe patients with depression manifested dorsolateral prefrontal cortex hypoactivity during attention control (74). This may elucidate why depressive patients with lower BDI benefit more from ABM.
As mentioned earlier, task types, target stimuli, training directions, training settings, age, and BDI scores at baseline were closely associated with the effect of ABM on depression. However, due to limited studies, the optimal protocols and potential influencing factors of ABM for patients with depression were undetermined, and more rigorously designed RCTs are needed to address these issues.
4.5. Deviations from the protocol
(1) Comparators mentioned in the protocol were sham ABM alone or sham ABM plus conventional rehabilitation or any other active intervention. In this review, participants in the control group received ACT alone, ACT plus CT, or CT alone. Sham ABM and ACT mean the same thing, while the ACT was widely used in the literature (10, 75); thus, we used ACT. (2) The age of the included patients was different. In the protocol, all patients over 18 years of age were included. Previous studies showed that ABM was also widely used for depression in adolescents (18, 40). To enlarge the applicability of this study, we did not impose age restrictions in this review. In addition, we conducted a subgroup analysis by different age groups to identify the advantages of ABM for specific age groups. (3) Different from the protocol, rumination and attentional control were added as secondary outcomes in the review. Rumination and attentional control are closely related to the occurrence and development of depression. The addition of secondary outcomes would facilitate a more broad and more comprehensive exploration of the effect of ABM on depression.
4.6. Limitations of this study
There were several potential limitations in our study. First, high heterogeneity was detected among the included studies; although the subgroup and meta-regression analyses were carried out, we still failed to find out the source of heterogeneity. Second, the risk of bias in most included studies was some concerns, and most of the evidence was low or very low certainty evidence, the findings should be taken with caution. Third, we included studies published in both Chinese and English, and publication bias might exist.
5. Conclusion
Due to high heterogeneity and limited studies, not enough current evidence supported that ABM could be an effective intervention to relieve depressive symptoms. More rigorous RCTs are required to verify the benefits and to explore the optimal protocols of ABM training for depression.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
H-sX, Y-xL, and Q-yZ designed the protocol and drafted the manuscript. J-xH, JL, and R-jJ revised this manuscript. D-lZ, X-bL, X-yG, JZ, JF, and YZ screened the articles, extracted data, and conducted data synthesis. JL and S-cA highlighted the research question and guided the whole process of this review. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the National Key Research and Development Project of China (2019YFC1710302), the Key Project of Sichuan Province Science and Technology (2020YFS0284), the National Natural Science Foundation of China (81873354), and the Sichuan Province Science and Technology Program (2023NSFSC1824).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1098610/full#supplementary-material
Footnotes
References
1. Otte, C, Gold, SM, Penninx, BW, Pariante, CM, Etkin, A, Fava, M, et al. Major depressive disorder. Nat Rev Dis Primers. (2016) 2:16065. doi: 10.1038/nrdp.2016.65
2. Lim, GY, Tam, WW, Lu, Y, Ho, CS, Zhang, MW, and Ho, RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. (2018) 8:2861. doi: 10.1038/s41598-018-21243-x
3. COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the Covid-19 pandemic. Lancet. (2021) 398:1700–12. doi: 10.1016/s0140-6736(21)02143-7
4. Kessler, RC, Akiskal, HS, Ames, M, Birnbaum, H, Greenberg, P, Hirschfeld, RMA, et al. Prevalence and effects of mood disorders on work performance in a nationally representative sample of U.S. Workers. Am J Psychiatry. (2006) 163:1561–8. doi: 10.1176/ajp.2006.163.9.1561
5. Chisholm, D, Sweeny, K, Sheehan, P, Rasmussen, B, Smit, F, Cuijpers, P, et al. Scaling-up treatment of depression and anxiety: a global return on investment analysis. Lancet Psychiatry. (2016) 3:415–24. doi: 10.1016/s2215-0366(16)30024-4
6. Beck, AT. The evolution of the cognitive model of depression and its neurobiological correlates. Am J Psychiatry. (2008) 165:969–77. doi: 10.1176/appi.ajp.2008.08050721
7. Baek, K, Kwon, J, Chae, JH, Chung, YA, Kralik, JD, Min, JA, et al. Heightened aversion to risk and loss in depressed patients with a suicide attempt history. Sci Rep. (2017) 7:11228. doi: 10.1038/s41598-017-10541-5
8. Peckham, AD, McHugh, RK, and Otto, MW. A meta-analysis of the magnitude of biased attention in depression. Depress Anxiety. (2010) 27:1135–42. doi: 10.1002/da.20755
9. Hilland, E, Landrø, NI, Harmer, CJ, Browning, M, Maglanoc, LA, and Jonassen, R. Attentional bias modification is associated with Fmri response toward negative stimuli in individuals with residual depression: a randomized controlled trial. J Psychiatry Neurosci. (2020) 45:23–33. doi: 10.1503/jpn.180118
10. Hang, Y, Zhang, G, Wang, C, Zhang, N, and Liu, G. Attention bias modification for anxiety disorders in children and adolescents: a systematic review and meta-analysis. Psychiatry Res. (2021) 300:113896. doi: 10.1016/j.psychres.2021.113896
11. Alvares, GA, Chen, NTM, Notebaert, L, Granich, J, Mitchell, C, and Whitehouse, AJO. Brief social attention bias modification for children with autism Spectrum disorder. Autism Res. (2019) 12:527–35. doi: 10.1002/aur.2067
12. Zhang, M, Ying, J, Song, G, Fung, DS, and Smith, H. Attention and cognitive bias modification apps: review of the literature and of commercially available apps. JMIR Mhealth Uhealth. (2018) 6:e10034. doi: 10.2196/10034
13. Notebaert, L, Grafton, B, Clarke, PJ, Rudaizky, D, Chen, NT, and MacLeod, C. Emotion-in-motion, a novel approach for the modification of attentional bias: an experimental proof-of-concept study. JMIR Serious Games. (2018) 6:e10993. doi: 10.2196/10993
14. Price, RB, Wallace, M, Kuckertz, JM, Amir, N, Graur, S, Cummings, L, et al. Pooled patient-level meta-analysis of children and adults completing a computer-based anxiety intervention targeting Attentional bias. Clin Psychol Rev. (2016) 50:37–49. doi: 10.1016/j.cpr.2016.09.009
15. Zhang, MWB, and Ying, J. Incorporating participatory action research in attention bias modification interventions for addictive disorders: perspectives. Int J Environ Res Public Health. (2019) 16:822. doi: 10.3390/ijerph16050822
16. Masataka, N, Koda, H, Atsumi, T, Satoh, M, and Lipp, OV. Preferential Attentional engagement drives Attentional bias to snakes in Japanese macaques (Macaca Fuscata) and humans (homo sapiens). Sci Rep. (2018) 8:17773. doi: 10.1038/s41598-018-36108-6
17. Yang, W, Ding, Z, Dai, T, Peng, F, and Zhang, JX. Attention bias modification training in individuals with depressive symptoms: a randomized controlled trial. J Behav Ther Exp Psychiatry. (2015) 49:101–11. doi: 10.1016/j.jbtep.2014.08.005
18. Yang, W, Zhang, JX, Ding, Z, and Xiao, L. Attention bias modification treatment for adolescents with major depression: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. (2016) 55:208–18.e2. doi: 10.1016/j.jaac.2015.12.005
19. Hakamata, Y, Lissek, S, Bar-Haim, Y, Britton, JC, Fox, NA, Leibenluft, E, et al. Attention bias modification treatment: a meta-analysis toward the establishment of novel treatment for anxiety. Biol Psychiatry. (2010) 68:982–90. doi: 10.1016/j.biopsych.2010.07.021
20. De Voogd, EL, Wiers, RW, Prins, PJ, and Salemink, E. Visual search Attentional bias modification reduced social phobia in adolescents. J Behav Ther Exp Psychiatry. (2014) 45:252–9. doi: 10.1016/j.jbtep.2013.11.006
21. Rouel, M, and Smith, E. Attentional bias and its modification in contamination Ocd symptomatology. Cogn Ther Res. (2018) 42:686–98. doi: 10.1007/s10608-018-9927-4
22. Habedank, I, Lennartz, SJ, Arslan, RC, and Ertle, A. Online attention bias modification for obsessive-compulsive disorder: A randomized controlled trial. (2017). doi: 10.31234/osf.io/gxvwk
23. Mogoaşe, C, David, D, and Koster, EH. Clinical efficacy of Attentional bias modification procedures: an updated meta-analysis. J Clin Psychol. (2014) 70:1133–57. doi: 10.1002/jclp.22081
24. Fodor, LA, Georgescu, R, Cuijpers, P, Szamoskozi, Ş, David, D, Furukawa, TA, et al. Efficacy of cognitive bias modification interventions in anxiety and depressive disorders: a systematic review and network meta-analysis. Lancet Psychiatry. (2020) 7:506–14. doi: 10.1016/s2215-0366(20)30130-9
25. Cristea, IA, Kok, RN, and Cuijpers, P. Efficacy of cognitive bias modification interventions in anxiety and depression: meta-analysis. Br J Psychiatry. (2015) 206:7–16. doi: 10.1192/bjp.bp.114.146761
26. Woolridge, SM, Harrison, GW, Best, MW, and Bowie, CR. Attention bias modification in depression: a randomized trial using a novel, reward-based, eye-tracking approach. J Behav Ther Exp Psychiatry. (2021) 71:101621. doi: 10.1016/j.jbtep.2020.101621
27. Shea, BJ, Reeves, BC, Wells, G, Thuku, M, Hamel, C, Moran, J, et al. Amstar 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. (2017) 358:j4008. doi: 10.1136/bmj.j4008
28. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The Prisma 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
29. Trull, TJ, Vergés, A, Wood, PK, Jahng, S, and Sher, KJ. The structure of diagnostic and statistical manual of mental disorders (4th edition, text revision) personality disorder symptoms in a large National Sample. Pers Disord. (2012) 3:355–69. doi: 10.1037/a0027766
30. Janca, A, Ustün, TB, Early, TS, and Sartorius, N. The Icd-10 symptom checklist: a companion to the Icd-10 classification of mental and Behavioural disorders. Soc Psychiatry Psychiatr Epidemiol. (1993) 28:239–42. doi: 10.1007/bf00788743
31. Cuijpers, P, Karyotaki, E, Eckshtain, D, Ng, MY, Corteselli, KA, Noma, H, et al. Psychotherapy for depression across different age groups: a systematic review and meta-analysis. JAMA Psychiat. (2020) 77:694–702. doi: 10.1001/jamapsychiatry.2020.0164
32. Balshem, H, Helfand, M, Schünemann, HJ, Oxman, AD, Kunz, R, Brozek, J, et al. Grade guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. (2011) 64:401–6. doi: 10.1016/j.jclinepi.2010.07.015
33. Guyatt, GH, Oxman, AD, Schünemann, HJ, Tugwell, P, and Knottnerus, A. Grade guidelines: a new series of articles in the journal of clinical epidemiology. J Clin Epidemiol. (2011) 64:380–2. doi: 10.1016/j.jclinepi.2010.09.011
34. Sherifali, D, Ali, MU, Ploeg, J, Markle-Reid, M, Valaitis, R, Bartholomew, A, et al. Impact of internet-based interventions on caregiver mental health: systematic review and meta-analysis. J Med Internet Res. (2018) 20:e10668. doi: 10.2196/10668
35. Boundy, EO, Dastjerdi, R, Spiegelman, D, Fawzi, WW, Missmer, SA, Lieberman, E, et al. Kangaroo mother care and neonatal outcomes: a meta-analysis. Pediatrics. (2016) 137:e20152238. doi: 10.1542/peds.2015-2238
36. Barkas, F, Nomikos, T, Liberopoulos, E, and Panagiotakos, D. Diet and cardiovascular disease risk among individuals with familial hypercholesterolemia: systematic review and meta-analysis. Nutrients. (2020) 12:2436. doi: 10.3390/nu12082436
37. Baert, S, De Raedt, R, Schacht, R, and Koster, EH. Attentional bias training in depression: therapeutic effects depend on depression severity. J Behav Ther Exp Psychiatry. (2010) 41:265–74. doi: 10.1016/j.jbtep.2010.02.004
38. Dai, Q, Hu, L, and Feng, Z. Attentional Bias Modification Reduces Clinical Depression and enhances attention toward Happiness. J Psychiatr Res. (2019) 109:145–55. doi: 10.1016/j.jpsychires.2018.11.024
39. Liao, JJ, Zheng, YN, Huang, LM, and Wei, ZH. Effect of attention bias modification training on adolescents with depression. J. Int. Psychiatr. (2016) 43:824–7. doi: 10.13479/j.cnki.jip.2016.05.015
40. Liu, WX. The intervention of attention bias modification training on cognitive bias in depression. Master. Wuhu: Wannan Medical College (2018).
41. Wang, LJ. A study on attention bias modification of depressive symptoms in college students. Master. Shanghai: Shanghai Normal University (2018).
42. Wei, M. The application of attention bias correction training in treatment of depression. Chin For Med Res. (2020) 18:140–2. doi: 10.14033/j.cnki.cfmr.2020.19.057
43. Zheng, ZF. The effect of attention bias modification training on the treatment of major depression disorder. Master. Changsha: Hunan Normal University (2018).
44. Zhou, Y. The effect of positive self-schema Attentional bias modification (ABM) on depressive individuals with different neuroticism levels. Master. Changchun: Northeast Normal University (2017).
45. Hsu, KJ, Shumake, J, Caffey, K, Risom, S, Labrada, J, Smits, JAJ, et al. Efficacy of attention bias modification training for depressed adults: a randomized clinical trial. Psychol Med. (2021) 52:1–9. doi: 10.1017/s0033291721000702
46. Wells, TT, and Beevers, CG. Biased attention and Dysphoria: manipulating selective attention reduces subsequent depressive symptoms. Cognit Emot. (2010) 24:719–28. doi: 10.1080/02699930802652388
47. Penton-Voak, IS, Bate, H, Lewis, G, and Munaf?, MR., Effects of emotion perception training on mood in undergraduate students: randomised controlled trial. Br J Psychiatry. (2012) 201:71–2. doi: 10.1192/bjp.bp.111.107086
48. Penton-Voak, IS, Adams, S, Button, KS, Fluharty, M, Dalili, M, Browning, M, et al. Emotional recognition training modifies neural response to emotional faces but does not improve mood in healthy volunteers with high levels of depressive symptoms. Psychol Med. (2021) 51:1211–9. doi: 10.1017/s0033291719004124
49. Bø, R, Kraft, B, Jonassen, R, Harmer, CJ, Hilland, E, Stiles, TC, et al. Symptom severity moderates the outcome of attention bias modification for depression: an exploratory study. J Psychiatr Res. (2021) 138:528–34. doi: 10.1016/j.jpsychires.2021.04.027
50. De Voogd, EL, Wiers, RW, and Salemink, E. Online visual search Attentional bias modification for adolescents with heightened anxiety and depressive symptoms: a randomized controlled trial. Behav Res Ther. (2017) 92:57–67. doi: 10.1016/j.brat.2017.02.006
51. Krejtz, I, Holas, P, Rusanowska, M, and Nezlek, JB. Positive online attentional training as a means of modifying attentional and interpretational biases among the clinically depressed: an experimental study using eye tracking. J Clin aPsychol. (2018) 74:1594–606. doi: 10.1002/jclp.22617
52. Shamai-Leshem, D, Lazarov, A, Pine, DS, and Bar-Haim, YA. Randomized controlled trial of gaze-contingent music reward therapy for major depressive disorder. Depress Anxiety. (2021) 38:134–45. doi: 10.1002/da.23089
53. Hallion, LS, and Ruscio, AM. A meta-analysis of the effect of cognitive bias modification on anxiety and depression. Psychol Bull. (2011) 137:940–58. doi: 10.1037/a0024355
54. Browning, M, Holmes, EA, Murphy, SE, Goodwin, GM, and Harmer, CJ. Lateral prefrontal cortex mediates the cognitive modification of Attentional bias. Biol Psychiatry. (2010) 67:919–25. doi: 10.1016/j.biopsych.2009.10.031
55. Browning, M, Holmes, EA, and Harmer, CJ. The modification of Attentional bias to emotional information: a review of the techniques, mechanisms, and relevance to emotional disorders. Cogn Affect Behav Neurosci. (2010) 10:8–20. doi: 10.3758/cabn.10.1.8
56. Beevers, CG, Clasen, PC, Enock, PM, and Schnyer, DM. Attention bias modification for major depressive disorder: effects on attention bias, resting state connectivity, and symptom change. J Abnorm Psychol. (2015) 124:463–75. doi: 10.1037/abn0000049
57. Hakamata, Y, Mizukami, S, Komi, S, Sato, E, Moriguchi, Y, Motomura, Y, et al. Attentional bias modification alters intrinsic functional network of Attentional control: a randomized controlled trial. J Affect Disord. (2018) 238:472–81. doi: 10.1016/j.jad.2018.06.018
58. Browning, M, Holmes, EA, Charles, M, Cowen, PJ, and Harmer, CJ. Using Attentional bias modification as a cognitive vaccine against depression. Biol Psychiatry. (2012) 72:572–9. doi: 10.1016/j.biopsych.2012.04.014
59. Olthof, M, Hasselman, F, and Lichtwarck-Aschoff, A. Complexity in psychological self-ratings: implications for research and practice. BMC Med. (2020) 18:317. doi: 10.1186/s12916-020-01727-2
60. Jelinek, L, Van Quaquebeke, N, and Moritz, S. Cognitive and metacognitive mechanisms of change in metacognitive training for depression. Sci Rep. (2017) 7:3449. doi: 10.1038/s41598-017-03626-8
61. Nolen-Hoeksema, S, Morrow, J, and Fredrickson, BL. Response styles and the duration of episodes of depressed mood. J Abnorm Psychol. (1993) 102:20–8. doi: 10.1037//0021-843x.102.1.20
62. Zeng, KB. Neutral and positive attention bias training improves depressive symptoms and the comparison of the role of redundant thought. master. Changsha: Hunan Normal University (2018).
63. Wang, ML. The long-term efficacy of attention bias modification treatment for individuals with depressive disorders:A randomized double-blind controlled trial. master. Changsha: Hunan Normal University (2020).
64. Jones, CR, Fazio, RH, and Vasey, MW. Attentional control buffers the effect of public speaking anxiety on performance. Soc Psychol Personal Sci. (2012) 3:556–61. doi: 10.1177/1948550611430166
65. Koster, EH, De Lissnyder, E, Derakshan, N, and De Raedt, R. Understanding depressive rumination from a cognitive science perspective: the impaired disengagement hypothesis. Clin Psychol Rev. (2011) 31:138–45. doi: 10.1016/j.cpr.2010.08.005
66. van Rooijen, R, Ploeger, A, and Kret, ME. The dot-probe task to measure emotional attention: a suitable measure in comparative studies? Psychon Bull Rev. (2017) 24:1686–717. doi: 10.3758/s13423-016-1224-1
67. Winer, ES, and Salem, T. Reward devaluation: dot-probe meta-analytic evidence of avoidance of positive information in depressed persons. Psychol Bull. (2016) 142:18–78. doi: 10.1037/bul0000022
68. Torrence, RD, and Troup, LJ. Event-related potentials of Attentional bias toward faces in the dot-probe task: a systematic review. Psychophysiology. (2018) 55:e13051. doi: 10.1111/psyp.13051
69. Heeren, A, Mogoașe, C, Philippot, P, and McNally, RJ. Attention bias modification for social anxiety: a systematic review and meta-analysis. Clin Psychol Rev. (2015) 40:76–90. doi: 10.1016/j.cpr.2015.06.001
70. Beard, C, Sawyer, AT, and Hofmann, SG. Efficacy of attention bias modification using threat and appetitive stimuli: a meta-analytic review. Behav Ther. (2012) 43:724–40. doi: 10.1016/j.beth.2012.01.002
71. Jones, EB, and Sharpe, L. Cognitive bias modification: a review of meta-analyses. J Affect Disord. (2017) 223:175–83. doi: 10.1016/j.jad.2017.07.034
72. Salthouse, TA. When does age-related cognitive decline begin? Neurobiol Aging. (2009) 30:507–14. doi: 10.1016/j.neurobiolaging.2008.09.023
73. Li, Y, Wang, W, Liu, T, Ren, L, Zhou, Y, Yu, C, et al. Source analysis of P3a and P3b components to investigate interaction of depression and anxiety in Attentional systems. Sci Rep. (2015) 5:17138. doi: 10.1038/srep17138
74. Heleven, E, van Dun, K, and Van Overwalle, F. The posterior cerebellum is involved in constructing social action sequences: an Fmri study. Sci Rep. (2019) 9:11110. doi: 10.1038/s41598-019-46962-7
75. Salum, GA, Petersen, CS, Jarros, RB, Toazza, R, DeSousa, D, Borba, LN, et al. Group cognitive behavioral therapy and attention bias modification for childhood anxiety disorders: a factorial randomized trial of efficacy. J Child Adolesc Psychopharmacol. (2018) 28:620–30. doi: 10.1089/cap.2018.0022
Keywords: depression, cognitive deficits, attention bias modification, systematic review, meta-analysis
Citation: Xia H-s, Li Y-x, Zhang Q-y, Zhong D-l, Liu X-b, Gou X-y, Fan J, Zhao J, Zhang Y, Ai S-c, Huang J-x, Li J and Jin R-j (2023) Attention bias modification for depression: A systematic review and meta-analysis. Front. Psychiatry. 14:1098610. doi: 10.3389/fpsyt.2023.1098610
Edited by:
Maritta Välimäki, Central South University, ChinaCopyright © 2023 Xia, Li, Zhang, Zhong, Liu, Gou, Fan, Zhao, Zhang, Ai, Huang, Li and Jin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jia-xi Huang, aHVhbmdqaWF4aTIwMTlAMTYzLmNvbQ==; Juan Li, Nzg1OTM5MDE2QHFxLmNvbQ==; Rong-jiang Jin, Y2R6eXlkeGpyakAxMjYuY29t
†These authors have contributed equally to this work and share first authorship
 Hai-sha Xia
Hai-sha Xia Yu-xi Li
Yu-xi Li Qing-yun Zhang
Qing-yun Zhang Dong-ling Zhong
Dong-ling Zhong Xiao-bo Liu
Xiao-bo Liu Xin-yun Gou
Xin-yun Gou Jin Fan
Jin Fan Jing Zhao
Jing Zhao Yue Zhang
Yue Zhang Shuang-chun Ai
Shuang-chun Ai Jia-xi Huang
Jia-xi Huang Juan Li
Juan Li Rong-jiang Jin
Rong-jiang Jin