
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 31 March 2025
Sec. Psychology for Clinical Settings
Volume 16 - 2025 | https://doi.org/10.3389/fpsyg.2025.1510383
 Maria Valentina Cavarretta1,2,3,4*
Maria Valentina Cavarretta1,2,3,4* Hugues Pellerin3
Hugues Pellerin3 Ema Maurel4
Ema Maurel4 Salvatore Maria Anzalone2
Salvatore Maria Anzalone2 Isis Truck2
Isis Truck2 David Cohen3,5
David Cohen3,5 Sonia Ingoglia1
Sonia Ingoglia1Introduction: The COVID-19 pandemic has worsened global mental health, thereby burdening mental health services and raising burnout risk among professionals. Online therapy may be an optimal solution to reduce burnout risk, ensuring flexibility for psychotherapists and the continuity of care for patients. This study investigates the link between burnout and online therapy, focusing on environmental sensitivity and exploring tailored solutions to reduce burnout while maintaining healthcare performance.
Method: Participants were 95 French psychotherapists (89% females), aged from 24 to 59 years (M = 37.13, SD = 7.75). Participants were administered the Maslach Burnout Inventory, the Highly Sensitive Person Scale, and a questionnaire assessing their professional activity.
Results: Digital psychotherapists reported lower levels of burnout compared to traditional psychotherapists who did not use online therapy. Specifically, they had lower depersonalization scores (mean difference of 0.37 points, p = 0.038) and tent to have lower scores in emotional exhaustion (mean difference of 0.44 points, p = 0.07). This association was more pronounced for those with high environmental sensitivity.
Discussion: Online therapy ensures greater workplace flexibility, serving as a protective factor in reducing psychotherapists’ burnout. Integrating digital health into public mental health services can enhance care delivery and support the wellbeing of professionals, especially those with high environmental sensitivity. Essential guidelines for online therapy use are needed to maximize benefits and ensure its effective implementation.
Interruptions in mental health services worldwide during the COVID-19 pandemic and the subsequent surge in the demand for psychological support have exacerbated the risk of burnout among mental health professionals, with negative outcomes for entire healthcare organizations (Clemente-Suárez et al., 2021; Cohen et al., 2024; Gruber et al., 2021; Joshi and Sharma, 2020; Kane et al., 2022; Kupcova et al., 2023).
Most recent literature focuses on the psychological distress of healthcare professionals who were at the frontline during the pandemic (Leo et al., 2021; Ulfa et al., 2022). As a result, the wellbeing of “second-line” operators has often been overlooked (Billings et al., 2021). Some studies have reported prolonged and chronic workplace stress and high levels of burnout among mental health workers compared to other healthcare professionals (Franzoi et al., 2021), and burnout is particularly common in helping professions (Maslach et al., 2001). However, unlike other healthcare occupations (e.g., doctors or nurses), research on burnout among psychotherapists is significantly less prevalent (Schaufeli et al., 2009; Woo et al., 2020; Van Hoy and Rzeszutek, 2022).
Among psychotherapists, occupational burnout, characterized by emotional exhaustion, depersonalization, and reduced personal accomplishment, negatively affects the clinical process and patient outcomes, potentially resulting in partial or complete therapy failure (Vivolo et al., 2024). Research indicates that unmanaged burnout among clinicians can contribute to reduced empathy and diminished clinical effectiveness in psychotherapy and, in some cases, even lead to unethical conduct (Anagnostopoulos et al., 2012; Simionato et al., 2019). This is unfortunate as clinical work with patients and the continuous interaction with individuals experiencing physical and social suffering require a high degree of emotional and relational investment (Holmqvist and Jeanneau, 2006). This investment can lead to emotional exhaustion in therapists, expressed as decreased energy, stress, fatigue, and irritability, potentially culminating in withdrawal. It can also manifest as depersonalization, expressed as detachment from others, cynicism, and disengagement. Burnout may hinder a professional’s ability to establish a therapeutic alliance with patients (Zarzycka et al., 2022). As the therapeutic alliance is the cornerstone of the clinical method, personal fulfillment related to clinical work may decline (Stubbe, 2018).
Several studies have highlighted the significant role of intrapersonal variables as predictors of individual burnout (Mills and Huebner, 1998; Rzeszutek and Schier, 2014; Lee et al., 2016; George-Levi et al., 2020; Smout et al., 2021).
Some individuals appear to be more at risk of burnout due to their sensitivity to environmental influences, while others show greater resilience to stress (Golonka and Gulla, 2021; Rossi et al., 2023). Individuals with heightened environmental sensitivity, due to deeper perception and processing of stimuli, are better at recognizing details of their environment and are more strongly influenced by what happens around them (Belsky, 2013). Consequently, they have the potential to be more deeply affected by stressful experiences (Pluess, 2015; Pluess et al., 2023).
The theoretical concept of environmental sensitivity has important implications for intervention strategies in various settings, including workplaces (Lionetti et al., 2024; Nocentini et al., 2018). People differ significantly in their response to interventions, and some benefit more than others; part of this variability may stem from individual differences in environmental sensitivity (also known as “vantage sensitivity”) (Pluess, 2017; Pluess and Belsky, 2013).
Although there are numerous studies on the personality-burnout association, this issue remains understudied in the specific occupation of psychotherapists (Van Hoy and Rzeszutek, 2022). Several studies have revealed significant associations between high workload in the public sector and increased burnout levels (Ibrahim et al., 2022; Rupert and Dorociak, 2019; Rupert et al., 2009). This evidence is often explained by the lack of control over the work environment among psychotherapists (Kim, 2017). For these reasons, it is necessary to implement personalized burnout prevention interventions aimed at Mental Health Professionals (Johnson et al., 2018; Kotera et al., 2021; Santillan-Ramos et al., 2024).
In this sense, teletherapy, in the form of video conferencing for clinical practice, may be an optimal solution to address burnout, promoting therapists’ wellbeing while simultaneously meeting patients’ bio-psycho-social treatment needs (Bhaskar et al., 2020; Patel et al., 2018; Saladino et al., 2020; Tajan et al., 2023). Teletherapy has been defined as the provision of mental health care at a distance through technology (Shore, 2015; Wibberly, 2024).
Teletherapy aligns with the goals of U.S. healthcare reform to increase “effective, cost-efficient, and patient-centered practices” (Backhaus et al., 2012).
Remote therapy can support psychotherapists by improving their working conditions (Feijt et al., 2020; Kane et al., 2022). Online consultations may help alleviate clinicians’ stress by providing them with more free time while maintaining the quality of care provided to clients (Al-Mahrouqi et al., 2022; Harris et al., 2023).
Reduced commuting time for psychotherapists increases efficiency and enables the immediate provision of care across different clinical settings and geographic regions (Chevillard et al., 2018).
Telepsychiatry improves flexibility for professionals who can deliver care from home, even when living or traveling out of state or abroad (Gardner et al., 2020). Additional advantages of telepsychiatry include reduced travel costs, increased educational opportunities, earlier interventions, bundled services, better care coordination, and access to patients in non-medical settings such as schools, childcare facilities, prisons, and homes (Simpson and Reid, 2014).
Furthermore, the support of digital resources ensures consistent, equitable, and uninterrupted access to mental health services, particularly in underserved rural areas (Poletti et al., 2021; Sampaio et al., 2021; Tohme et al., 2021). This innovative strategy optimizes clinical workflows with timely patient engagement (Mitchell et al., 2021; Stefan et al., 2021).
Recent reviews of empirical data indicate that patients and clinicians using online therapy via video conferencing generally develop a good therapeutic alliance (Békés and Aafjes-van Doorn, 2020; Simpson and Reid, 2014), and online sessions do not differ in effectiveness from in-person sessions (Backhaus et al., 2012; Fernandez et al., 2021; Shklarski et al., 2021; Simpson, 2009).
In conclusion, the pandemic has accelerated innovations, including the adoption of new laws and regulations to promote the integration of online therapy into clinical practice (Bhaskar et al., 2020). Given the benefits and positive data on online therapy, many companies and healthcare organizations, as well as individual professionals, use this approach to support the profound and complex work of psychotherapy and as a sustainable practice to ensure continuity of care (Conrad, 2024; Jurcik et al., 2020; Peng et al., 2020).
This exploratory study aims to explore burnout among psychotherapists whether they use or not online therapy, to evaluate potential risk and protective factors associated with burnout including environmental sensitivity. To do so, we first examined the association of burnout with age, gender, and some characteristics of their professional activity (years of clinical experience, sector of professional practice, and therapeutic approach). Second, we explored the association of burnout with using online therapy. Third, we examined the association between burnout and environmental sensitivity. Finally, we tested the possible moderating effect of environmental sensitivity in the relationship between the use of online therapy and burnout.
The study was carried out on a sample of 95 psychotherapists, (89% females), ranged in age from 24 to 59 years (M = 37.13, SD = 7.75). The inclusion criteria for participants were as follows: (a) Working in mental health care during and after the COVID-19 outbreak; (b) providing informed consent.
The sample included psychotherapists who conducted online therapy (57%) and others who did not practice online therapy (43%). Among digital psychotherapists, 51% had been conducting online therapy for 1–4 years, and 4% for 5–8 years. Most participants were psychologists (84%), with an equal distribution of child psychiatrists, neuropsychologists, and psychomotor therapists among the other participants.
The majority of participants practiced their profession in metropolitan France (70.1%). The rest were a minority, distributed as 1% in Belgium, 2% in overseas France. Information was not available for 27% of the participants, that have chosen not to respond.
One third (33%) of psychotherapists had an integrative approach, which included transactional analysis, cognitive-behavioral therapy, psychoanalysis, and body therapies, 22% had a psychodynamic approach, which included psychoanalysis, group analysis and family therapy, 16% employed a cognitive-behavioral approach alone, 29% did not specified their approach.
The majority of participants worked in the private sector (59%), had an average of 8.8 years of clinical experience (SD = 6.60) (Table 1).
The study was conducted from February to June 2024. A questionnaire, developed using the Google® Forms platform, was disseminated to potential participants via a link. This link to the survey was sent directly to psychotherapists working in mental health services, psychiatric hospitals and psychological medical centers in France. It was also sent to professionals registered on Doctolib.fr, a French digital health platform facilitating online psychological appointment booking and teleconsultations between patients and healthcare providers. Additionally, an announcement containing instructions and the survey link was also disseminated through social media professional networks. Prior to participation, all respondents were presented with an online informed consent form. The survey was anonymous, and participants were assured of the confidentiality of their responses. Informed consent was obtained electronically from all participants before they could access the survey questions.
The study protocol and informed consent procedures were approved by the Ethics Committee of the University of Palermo (Ref 3145/2022, November 11th, 2022) prior to the commencement of data collection. The study was conducted in adherence to the Helsinki Declaration.
We collected participants’ age and gender, information on professional experience, including the country and sector of professional practice (public or private), the years of clinical experience, the clinical practice modality (use or non-use of online therapy), years of experience with providing online therapy and the psychotherapeutic approach.
To measure participants’ levels of professional burnout, we used The French version of the Maslach Burnout Inventory - Human Service Survey (MBI-HSS; Lheureux et al., 2017). It is a 22-item questionnaire designed to assess burnout in individuals working in healthcare and social services. The MBI-HSS comprises three subscales: Emotional Exhaustion (EE, 9 items, e.g., “Working with people all day is really a strain for me”) which measures feelings of being emotionally overextended by one’s work; Depersonalization (DP, 5 items, e.g., “I do not really care what happens to some patients”) which assesses unfeeling and impersonal responses to care and Personal Accomplishment (PA, 8 items, e.g., “I have accomplished many worthwhile things in this job”), which evaluates feelings of competence and perceived effectiveness in the job.
Respondents indicate the frequency with which they experience specific feelings or attitudes using a 7-point Likert scale, ranging from 0 (never) to 6 (every day).
The scores for each subscale are reported separately and are not combined into a global score.
In the current study, the scale showed an acceptable internal consistency, with Cronbach’s α values of 0.88 for EE, 0.60 for DP, and 0.79 for PA.
To measure the degree of an individual’s sensitivity to environmental influences, we used the Highly Sensitive Person scale (HSP-12; Pluess et al., 2023). It is a 12-item scale and includes three subscales: Ease of Excitation (EOE, 5 items, e.g., “Do you get rattled when you have a lot to do in a short amount of time?”) which refers to being easily overwhelmed by external and internal demands; Aesthetic Sensitivity (AES, 4 items, e.g., “Do you seem to be aware of subtleties in your environment?”) which captures the response and appreciation of aesthetic stimuli and Low Sensory Threshold (LST, 3 items, e.g., “Are you bothered by intense stimuli, like loud noises or chaotic scenes?”) which reflects unpleasant arousal to external stimuli. Respondents were asked to answer using a 7-point Likert scale, ranging from 1 (Not at all) to 7 (Completely).
In the current study, the scale showed a good internal consistency, with Cronbach’s α values of 0.82 for EOE, 0.72 for AES, and 0.72 for LST.
Analyses were performed using R software version 4.2.2. A p-value <0.05 was considered significant; however, we encourage the reader to interpret them here as a continuous measure of evidence against the null hypothesis.
The distribution of quantitative variables was summarized using mean and standard deviation, and alternatively using median and Q1–Q3 quartiles depending on the shape of the distribution. The distribution of qualitative variables was described using absolute and relative frequencies.
To explore psychotherapists’ workplace stress, we looked for factors associated with the three-dimensional scores of the degree of burnout. The association between the scores and quantitative variables was tested using Pearson correlation tests. The association between the scores and binary variables was tested using Welch t-tests or, alternatively, Wilcoxon rank sum tests, depending on the validity of the tests’ assumptions. For nominal variables, a Kruskal–Wallis test was used.
Finally, we tested the hypothesis that environmental sensitivity (as measured by three dimensional scores of the HSP scale) could moderate the association between using online therapy and the degree of burnout. This was done using linear regression models of the formula “Burnout ~ use of online therapy (yes/no) + environmental sensitivity + use of online therapy * environmental sensitivity.” One model was run for each combination of burnout score and environmental sensitivity subscore. We report for each model the effect of the interaction, tested using a t-test, along with its 95% parametric confidence interval.
Regarding burnout, testimated average level of Emotional Exhaustion (EE) was 2.07 Likert points, corresponding to “once a month” (SD =1.13; 95% CI 1.85; 2.30). There was a variability, with scores ranging from 0 (“never”) to 5.11 Likert points (“a few times a week”). Half of the participants scored between 1.22 and 2.78 Likert points.
The average Depersonalization (DP) level is 0.96 Likert points, indicating occurrences of “a few times a year” (SD = 0.85; 95% CI 0.78; 1.13). The DP score ranged from 0 to a maximum of 3.60 Likert points.
Conversely, Personal Accomplishment (PA) showed higher levels, with an average of 4.62 Likert points, suggesting a frequency between “once a week” and “a few times a week” (SD = 0.80; 95% CI 4.46; 4.78; Kurt = 2.68; Skew = −1.34). Scores in this domain ranged from 1.75 to 5.88 Likert points.
Regarding environmental sensitivity, the estimated average level of Ease of Excitation (EOE) was 4.18 Likert points (SD = 1.32), with scores ranging from 0 1.20 to 7.00.
The mean Aesthetic Sensitivity (AES) level was 5.56 Likert points (SD = 0.97), with scores ranging from 2.75 to 7.00 Likert points.
Finally, the estimated average level of Low Sensory Threshold (LST) was 3.86 Likert points (SD = 1.59), with scores ranging from 1.00 to 7.00 Likert points.
Results are reported in Table 2. Significant associations between burnout and gender were found. Female psychotherapists reported significantly higher EE scores, with a difference of 0.83 points between the median scores (p = 0.026). Additionally, they showed higher PA scores, with a difference of 0.5 points between the median scores, approaching significance (p = 0.078).
With regard to age, sector of professional practice, years of clinical experience and psychotherapeutic approach, no significant associations were found.
Results are reported in Table 3. Significant associations between burnout and the use of online therapy were found. Participants who utilized online therapies showed lower scores in EE, with a mean difference of 0.44 points approaching statistical significance (p = 0.07) compared to participants who did not use online therapy. Moreover, psychotherapists who practiced online therapy exhibited significantly lower DP scores, with a mean difference of 0.37 points (p = 0.038) compared to psychotherapists who did not use online therapy.
Results are reported in Table 4. Highly significant positive correlations were found between EE and both EOE (r = 0.35, p = 0.001) and LST (r = 0.30, p = 0.003). A small negative correlation was observed between PA and EOE, approaching significance (r = −0.20, p = 0.055). Finally, a positive correlation was observed between PA and AES (r = 0.31, p = 0.002).
DP was not significantly related with environmental sensitivity dimensions.
Results are reported in Table 5 and Figures 1, 2. The analysis revealed that EOE negatively moderates the association between online therapy use and EE (Beta = −0.44, p = 0.009).
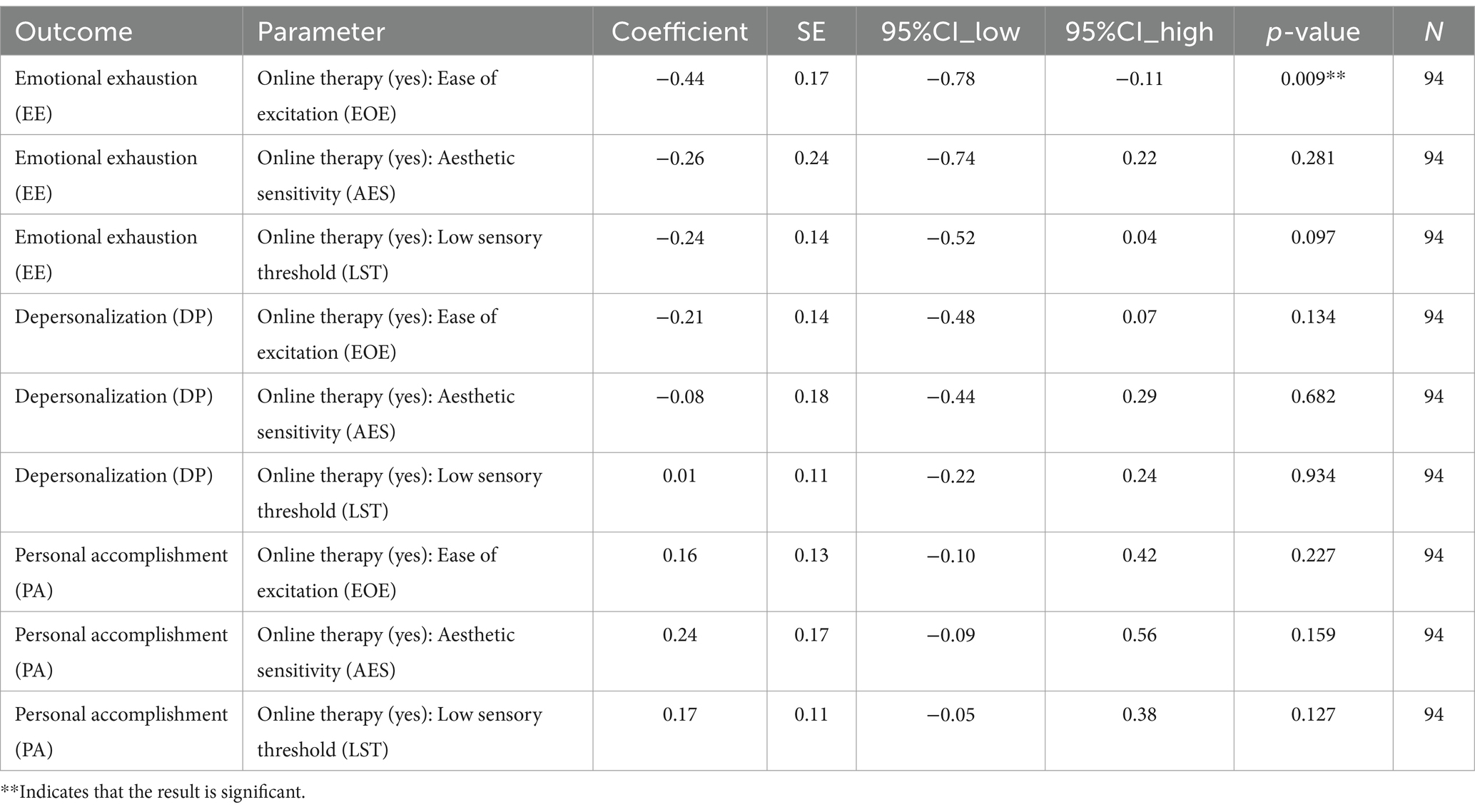
Table 5. Analysis of environmental sensitivity scores dimensions as moderators of the association between online therapy use and burnout scores.
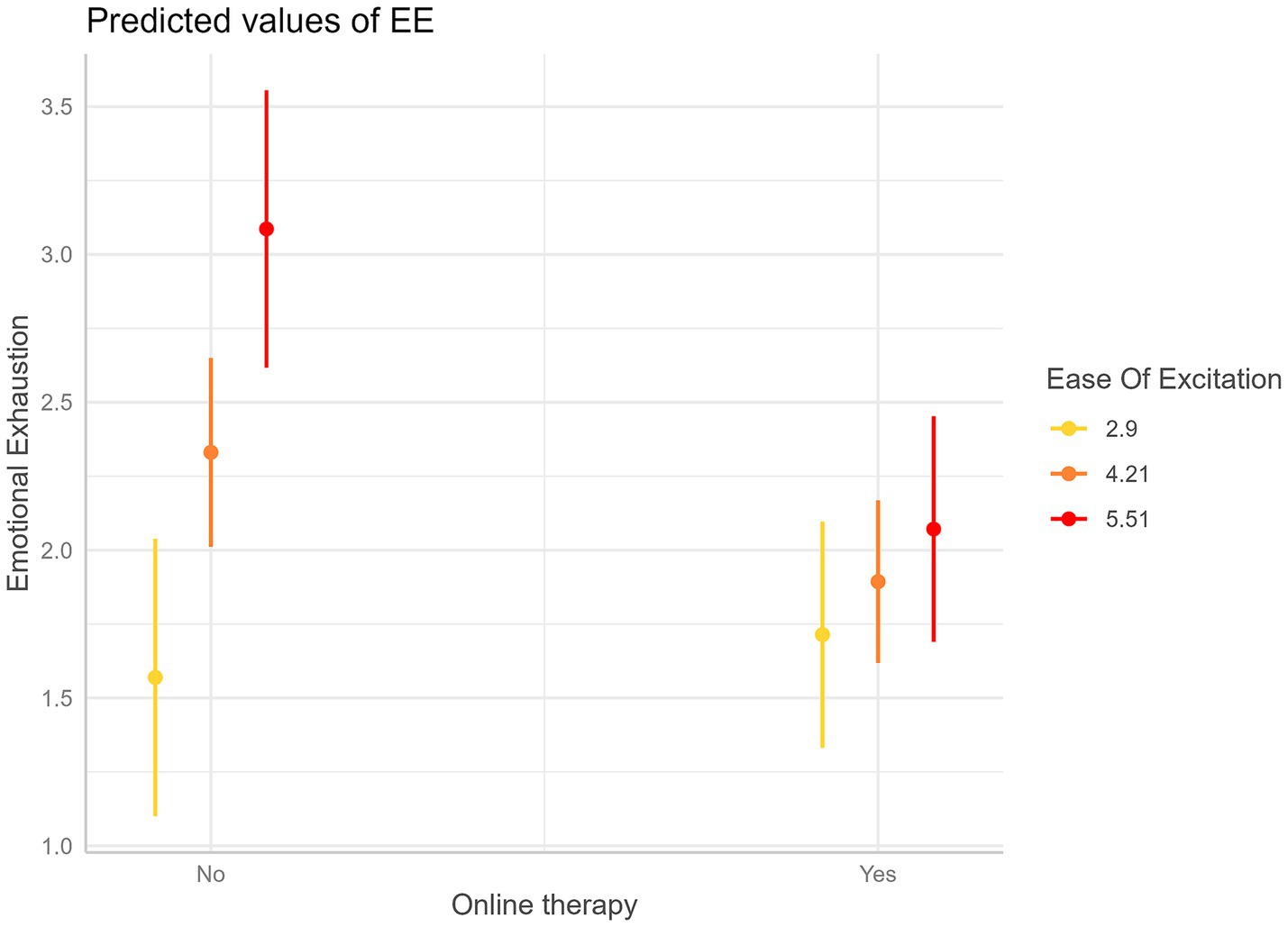
Figure 1. Interaction plot—Predicted values of Emotional Exhaustion (EE) as a function of online therapy use (Yes/No) at three values of Ease of Excitation (EOE), represented in colors. Error bars are 95% confidence intervals. This graph shows that a higher degree of EOE is associated with a higher reduction of EE for psychotherapists conducting online therapies compared to those who are not.
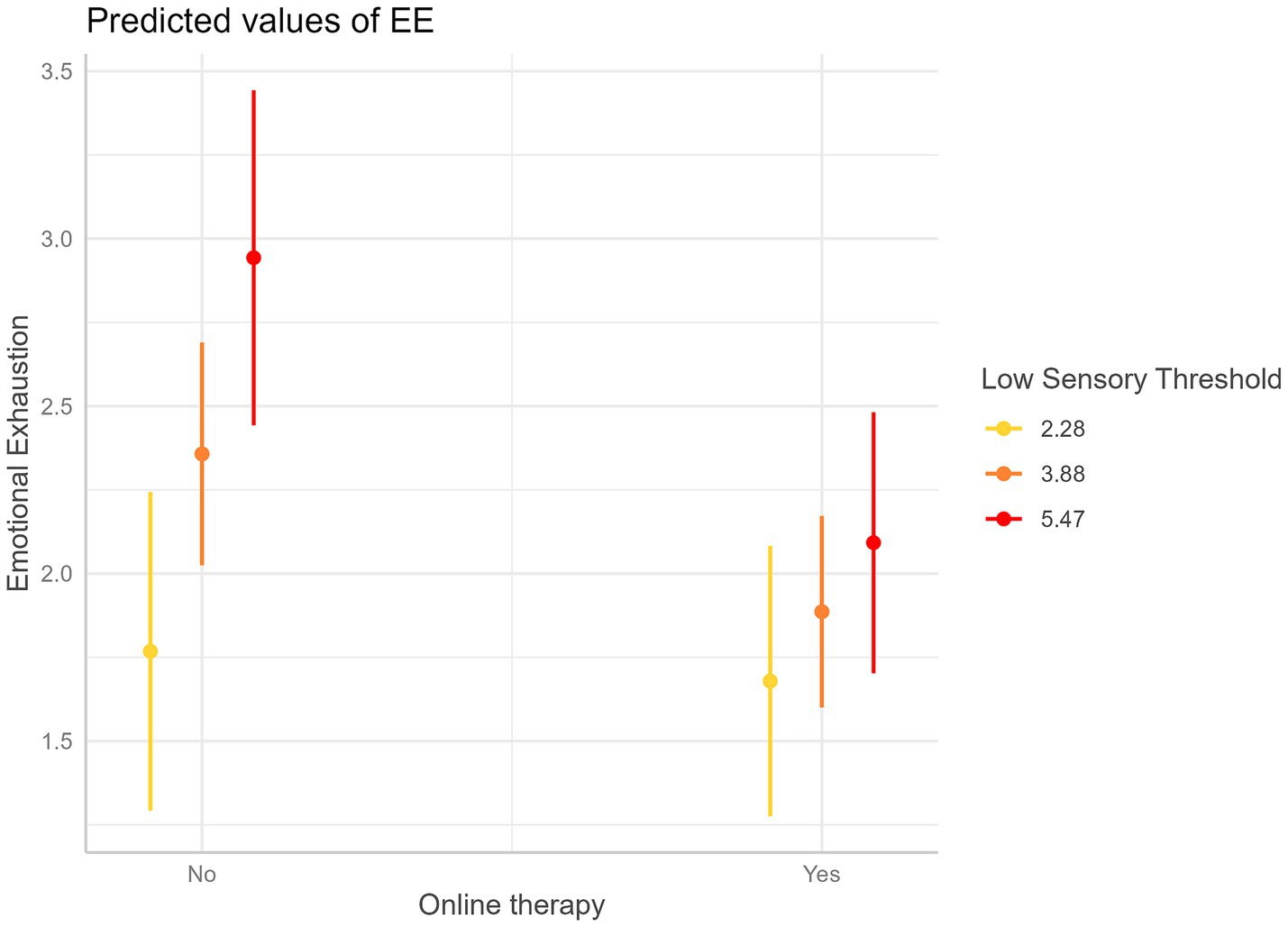
Figure 2. Interaction plot—Predicted values of Emotional Exhaustion (EE) as a function of online therapy use (Yes/No) at three values of Low Sensory Threshold (LST), represented in colors. Error bars are 95% confidence intervals. This graph shows that a higher degree of LST is associated with a higher reduction of EE for psychotherapists conducting online therapies compared to those who are not.
For example, for an EOE of 2.90 points Likert, online therapy use does not show a significant association with EE. However, for an EOE of 4.21 points Likert, a significant negative association begins to appear with a decrease in EE of 0.44 Likert points (p = 0.042) for psychotherapists who use online therapy compared to psychotherapists who do not use it. The negative association becomes more pronounced at higher levels of EOE. Finally, for an EOE of 5.51 points, the negative association becomes highly significant with an average decrease in EE of 1.01 Likert points (p = 0.001) when the psychotherapists use teleconferences compared to when they do not use them.
The analyses revealed also that the association between online therapy use and EE tended to decrease with LST (Beta = −0.24, p = 0.097), although this relationship approached but did not reach statistical significance.
For example, at lower levels of LST (2.28 Likert points), online therapy use does not show a significant association with EE. However, as LST increases, a negative association begins to emerge. Specifically, at an LST of 3.88 Likert points, a significant reduction in EE of 0.47 Likert points is observed (p = 0.036) when psychotherapists conduct teleconsultations compared to those who do not. This negative association becomes more pronounced at higher levels of LST. For instance, at an LST of 5.47 Likert points, psychotherapists conducting online therapy experience a substantial decrease in EE, with an average reduction of 0.85 Likert points (p = 0.009), compared to psychotherapists who do not conduct online therapy.
The objective of this study was to investigate workplace stress in a sample of psychotherapists: we compared the burnout of those who use online therapy with those who do not and we focused on the association with individual sensitivity to environmental influences. Subsequently, we evaluated the link between use of online therapy, environmental sensitivity and burnout.
The results showed moderate levels of Emotional Exhaustion among psychotherapists. This outcome aligns with previous research regarding individual experiences of stress accompanied by a decline in emotional and physical resources experienced by psychologists in their work with patients (Kercher et al., 2024; Probst et al., 2020).
The analysis conducted so far has shown low levels of Depersonalization among the survey participants. This finding suggests that most psychotherapists have maintained empathy and connection with their clients.
It was also found that the experience of the pandemic and the current crisis affecting the mental health sector did not impact feelings of professional efficacy and productivity at work: participants exhibited high levels in the dimension of Professional Accomplishment.
Comparing psychotherapists who practice online therapy and those who do not. It revealed significant results for Emotional Exhaustion and Depersonalization.
Regarding Emotional Exhaustion, it is known that exercising sensitivity, the effort to attune with the patient, and the co-construction of a relationship between partners are necessary to effectively conduct psychotherapeutic treatment. A profound and continuous emotional effort is therefore required of the clinician (Békés et al., 2021; Fernández-Álvarez and Fernández-Álvarez, 2021). The online methodology appears to have had a protective role for the psychotherapist: professionals who did not use it were found to be more emotionally exhausted, increasing the risk of poor outcomes in face-to-face work with the patient (Patel et al., 2018).
Even more advantageous was the use of online therapy for the other dimension of burnout: Depersonalization (the phenomenon of detachment and a cynical attitude of the worker towards their occupation). Participants practicing online consultations demonstrated significantly lower Depersonalization scores compared to those practicing traditional consultations. This result appears to be of some importance: professionals who lose enthusiasm and passion for their occupation with using traditional therapies could expose the treatment to the risk of poor therapeutic outcomes (Singh et al., 2020).
Although it may seem counterintuitive, traditional psychotherapists may feel like an external observers of patients’ mental processes during face-to-face clinical work. “Depersonalized” psychotherapists may experience sensations of coldness, irritation, and negativity in the concrete relationship with patients. This could limit the quality of their performance; for example, they may provide evasive responses to patients’ requests for help, underestimate their problems, and fail to recognize or deny their psychological needs. The therapist’s detachment from the patient, combined with emotional numbness or loss of reactivity, could thus cause discomfort for both partners of the dyad (Yang and Hayes, 2020).
The paradox of depersonalization might, therefore, be conceptualized as a form of coping strategy, a protective mechanism against personally experiencing patients’ lived experiences and excessive identification with them.
In contrast, the digital setting promotes engagement in a deep “disembodied” relationship with the patient. The screen would not constitute a concrete barrier separating therapist and patient; rather, it would function as a metaphorical boundary that regulates distance, stimulates emotional sharing, and facilitates the management of transference-countertransference movements. A “disciplined subjectivity,” balanced between approaching and withdrawing, would favor the therapist’s emotional resonance, mirroring, and their shared experience or participation in the other’s lived experiences, which are essential elements for finding the patients (Zavattini, 2014).
In contrast to various technological tools that can be employed in remote clinical practice, such as text messages, emails, and telephone calls (Zhou et al., 2020), videoconferencing allows the clinician to deeply attend to the patient’s non-verbal cues within a secure environment.
Simpson et al. (2021) discussed the “democratizing effect” in remote treatment. Both therapists and patients share their personal environments, creating a shift in the power balance. In the online setting, the parity between client and therapist would be greater compared to the traditional setting, as both are situated in independent spaces, communicating through their respective technological tools, over which they have individual control (Mitchell, 2020; Norwood et al., 2018). Consequently, patients might feel less threatened by the therapist, their psychological defenses could lower, and patient empowerment would increase, as they would not perceive themselves as submitting to the therapists’ will (e.g., in terms of attending their building, being seated in their room, according to their wishes) (Simpson et al., 2021).
Thus, in virtual reality, conceptualized as a “transitional space” (Jesser et al., 2022), something unique could occur: not only greater openness from the patient but also an empathic and “synchronous” understanding by the therapist (Boldrini et al., 2020). Indeed, it is not physical proximity that is decisive for feeling close and connected, but rather the realization of a “true encounter” (Manguel, 2019).
Research on strategies to combat burnout suggests the need for therapists to disengage from their occupation at the end of work (O’Connor et al., 2018). In this sense, digital mental health ensures greater workplace flexibility for the psychotherapist compared to standard therapy (James et al., 2022). The possibility of working from any location and at any time can mitigate clinical stress, improving the balance between professional and personal life (Olwill et al., 2021).
Moreover, the ease of organizing online meetings with the patient favors continuity in treatment (Yellowlees et al., 2020). The difficult work of building the therapeutic alliance is thus facilitated through continuous online care (Stefana et al., 2024).
These results suggest that the practice of teletherapy may serve as a protective factor in reducing psychotherapists’ burnout, facilitating the development of clinical reasoning and promoting the profound engagement with the patient.
Understanding the interaction between burnout and the practice of online therapy is crucial to support the wellbeing of clinicians and thus ensure quality and effective care for patients.
In this study, psychotherapists with high levels of Ease of Excitation and Low Sensory Threshold were both strongly and negatively affected by potentially stressful experiences, with an associated increase in Emotional Exhaustion. While less sensitive individuals tend to be more robust and resilient when facing adversity, highly sensitive individuals are more reactive to adverse experiences and tend to adopt less adaptive coping strategies (Belsky and Pluess, 2009).
However, the findings also proposed a more nuanced picture, suggesting that certain aspects of environmental sensitivity may be beneficial for personal accomplishment. Psychotherapists with heightened Aesthetic Sensitivity may experience a greater sense of mastery over situations, self-determination and self-efficacy in their work, possibly due with their ability to process environmental influences in a deep and detailed manner (Redfearn et al., 2020; Sun et al., 2023).
These results highlight the complex relationship between individual personality and occupational wellbeing. Differences in the degree of psychotherapist burnout could be related to the complex and distinctive set of characteristics and psychological processes that define the personality (Van Hoy and Rzeszutek, 2022). High environmental sensitivity has emerged as a significant factor associated with psychotherapist burnout, functioning as both a potential risk factor and a possible protective factor.
The moderation models revealed the specific utility of the online methodology, particularly for psychotherapists with higher environmental sensitivity. For these individuals, the use of remote consultations was associated with lower emotional exhaustion compared to the other respondents who do not practice online consultations.
In line with vantage sensitivity framework, more sensitive psychotherapists would be more reactive to the positive effect of teletherapy compared to less sensitive psychotherapists (De Villiers et al., 2018).
Significant results were found in the dimensions Ease of Excitation and Low Sensory Threshold of Environmental Sensitivity.
Regarding Ease of Excitation, online therapy use showed a stronger association with lower Emotional Exhaustion of psychotherapists who are more reactive to external stimuli compared to less excitable psychotherapists who do not use online therapy.
Highly reactive psychotherapists would feel overwhelmed in highly stimulating work environments. Public health services, particularly psychiatric hospitals and mental health centers, exemplify such environments, exposing professionals to intense demands (Giusti et al., 2020; Luo et al., 2020). Psychotherapists working in these settings are required to respond quickly and appropriately to patient needs, often managing delicate situations in hectic conditions (Mittal et al., 2023). In such chaotic environments, clinicians prone to excitation would experience discomfort, stress and fatigue. The online setting reduces exposure to excessive stimulation (Stoll et al., 2020).
Regarding Low Sensory Threshold, psychotherapists with heightened sensibility to stimuli seemed to benefit from online practice in terms of reducing Emotional Exhaustion compared to those who do not conduct online therapy. Their heightened sensitivity to low-intensity stimuli can make them particularly susceptible to environmental changes.
In this regard as well, teleconsultations with patients would benefit clinicians working in public health settings, which are subject to frequent and often unpredictable environmental variations. Teletherapy thus constitutes a controlled alternative where sensory input can be minimized and the expression of practitioners’ clinical skills can be facilitated, helping them to buffer the stressors of traditional face-to-face settings (Batastini et al., 2021; Rutkowska et al., 2023).
This study presents several limitations.
The complexity of the survey and the time required to complete the questionnaires reduced the number of participants. Although the survey included various professionals working in the field of mental health, the majority of participants were psychologists. Furthermore, the study was conducted during a period when most respondents were directly involved with patients, which may have limited survey participation. These limitations make it difficult to generalize the results.
The cross-sectional nature of the study and the lack of longitudinal follow-up do not allow for inferences about causal relationships between variables and the long-term consequences of the psychological outcomes observed. These limitations preclude solid conclusions.
Finally, qualitative studies could explore in depth the individual experiences of psychotherapists adopting digital methodologies to thoroughly understand the effects of different digital spaces on the psychotherapeutic process and expand research on the possibilities and limitations of virtual encounters for psychological maturation. Further research is needed to carefully investigate the “complex mixture of proximity and distance, presence and absence, reality and fantasy” (Roesler, 2017) that characterizes exchanges in the digital setting, creating new forms of relationships that differ significantly from traditional face-to-face interactions.
This study provides a snapshot of the benefits of online therapy practice in reducing workplace stress among psychotherapists, with significant implications for the future healthcare policies and the clinical method in psychotherapy.
Teletherapy is particularly useful for enhancing the wellbeing of psychotherapists with high environmental sensitivity, which can be measured with a brief questionnaire. In this way, strategic ad hoc choices, based on individual differences, could be implemented in different clinical settings. One solution involves the targeted use of online therapy by more sensitive clinicians in particularly stimulating contexts, including psychiatric hospitals and mental health services. The virtual dimension of the online setting, isolated and detached from the concreteness of the physical environment, would reduce exposure to intense stimuli and allow for greater control over the therapeutic setting.
Digital tools can represent interesting, useful, and effective resources to integrate into the clinical method in psychotherapy. Online consultation does not replace conventional treatment but serves as a valuable complement to psychological practice. Therefore, mental health organizations should invest in digital health by providing resources to support the tele-psychotherapy. Most clinicians have little education in the online practice (Doan et al., 2021; Perle et al., 2024). It would be useful to promote training programs, guidelines and best practices to effectively use digital platforms and transition patient care to an online format. Technological development in the field of mental health predicts future trends that include “smart” mobile devices, cloud computing, virtual worlds and realities, electronic games, in addition to conventional psychotherapy tools. Greater knowledge of these tools and their main differences is necessary to adapt them to the specific purposes of the clinician.
It is beneficial to support a more efficient “connected” healthcare system by strengthening care and replicating successful practices, also in preparation for possible future emergencies.
In conclusion, the development of socially advantageous psychotherapy strategies continues to represent a global challenge in this post-COVID period. This study leverages advances in digital health to propose personalized healthcare solutions aimed at promoting the wellbeing of psychotherapists, providing adequate responses to the bio-psycho-social treatment needs of patients and enhancing the quality of care in different clinical settings.
The raw data supporting the conclusions of this article will be made available upon request by the authors, without undue reservation.
The studies involving humans were approved by Ethics Committee of University of Palermo (Ref 3145/2022, November 11th, 2022). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
MC: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft. HP: Data curation, Formal analysis, Methodology, Writing – original draft. EM: Investigation, Writing – original draft. SA: Resources, Supervision, Writing – review & editing. IT: Resources, Supervision, Writing – review & editing. DC: Resources, Supervision, Writing – review & editing. SI: Conceptualization, Methodology, Supervision, Writing – review & editing.
The author(s) declare that financial support was received for the research and/or publication of this article. Funding support for the conduct of this research was provided by University of Palermo, University of Paris 8, and CY Cergy Paris University.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Al-Mahrouqi, T., Al-Alawi, K., Al-Alawi, M., Al Balushi, N., Al Ghailani, A., Al Sabti, H., et al. (2022). A promising future for tele-mental health in Oman: a qualitative exploration of clients and therapists’ experiences. SAGE Open Med. 10:20503121221086372. doi: 10.1177/20503121221086372
Anagnostopoulos, F., Liolios, E., Persefonis, G., Slater, J., Kafetsios, K., and Niakas, D. (2012). Physician burnout and patient satisfaction with consultation in primary health care settings: evidence of relationships from a one-with-many design. J. Clin. Psychol. Med. Settings 19, 401–410. doi: 10.1007/s10880-011-9278-8
Backhaus, A., Agha, Z., Maglione, M. L., Repp, A., Ross, B., Zuest, D., et al. (2012). Videoconferencing psychotherapy: a systematic review. Psychol. Serv. 9, 111–131. doi: 10.1037/a0027924
Batastini, A. B., Paprzycki, P., Jones, A. C. T., and MacLean, N. (2021). Are videoconferenced mental and behavioral health services just as good as in-person? A meta-analysis of a fast-growing practice. Clin. Psychol. Rev. 83:101944. doi: 10.1016/j.cpr.2020.101944
Békés, V., and Aafjes-van Doorn, K. (2020). Psychotherapists’ attitudes toward online therapy during the COVID-19 pandemic. J. Psychother. Integr. 30, 238–247. doi: 10.1037/int0000214
Békés, V., Aafjes-van Doorn, K., Luo, X., Prout, T. A., and Hoffman, L. (2021). Psychotherapists’ challenges with online therapy during COVID-19: concerns about connectedness predict therapists’ negative view of online therapy and its perceived efficacy over time. Front. Psychol. 12:705699. doi: 10.3389/fpsyg.2021.705699
Belsky, J. (2013). Differential susceptibility to environmental influences. Int. J. Child Care Educ. Policy 7, 15–31. doi: 10.1007/2288-6729-7-2-15
Belsky, J., and Pluess, M. (2009). Beyond diathesis stress: differential susceptibility to environmental influences. Psychol. Bull. 135, 885–908. doi: 10.1037/a0017376
Bhaskar, S., Bradley, S., Chattu, V. K., Adisesh, A., Nurtazina, A., Kyrykbayeva, S., et al. (2020). Telemedicine across the globe-position paper from the COVID-19 pandemic health system resilience PROGRAM (REPROGRAM) international consortium (part 1). Front. Public Health 8:556720. doi: 10.3389/fpubh.2020.556720
Billings, J., Biggs, C., Ching, B. C. F., Gkofa, V., Singleton, D., Bloomfield, M., et al. (2021). Experiences of mental health professionals supporting front-line health and social care workers during COVID-19: qualitative study. BJPsych Open 7:e70. doi: 10.1192/bjo.2021.29
Boldrini, T., Schiano Lomoriello, A., Del Corno, F., Lingiardi, V., and Salcuni, S. (2020). Psychotherapy during COVID-19: how the clinical practice of Italian psychotherapists changed during the pandemic. Front. Psychol. 11:591170. doi: 10.3389/fpsyg.2020.591170
Chevillard, G., Lucas-Gabrielli, V., and Mousques, J. (2018). « Déserts médicaux » en France: État des lieux et perspectives de recherches: L’Espace géographique, Tome 47, 362–380. doi: 10.3917/eg.474.0362
Clemente-Suárez, V. J., Martínez-González, M. B., Benitez-Agudelo, J. C., Navarro-Jiménez, E., Beltran-Velasco, A. I., Ruisoto, P., et al. (2021). The impact of the COVID-19 pandemic on mental disorders. A critical review. Int. J. Environ. Res. Public Health 18:10041. doi: 10.3390/ijerph181910041
Cohen, D. (2020). Appréhender le COVID-19 au fil de l’eau en tant que psychiatre d’enfant et d’adolescent. L'Encéphale 46, S99–S106. doi: 10.1016/j.encep.2020.05.005
Cohen, D. (2024). Editorial: Insights in adolescent and young adult psychiatry: 2023. Front. Psychiatry 15. doi: 10.3389/fpsyt.2024.1446846
Conrad, J. A. (2024). Digitization and its discontents: the promise and limitations of digital mental health interventions. J. Contemp. Psychother. 54, 209–215. doi: 10.1007/s10879-024-09620-2
De Villiers, B., Lionetti, F., and Pluess, M. (2018). Vantage sensitivity: a framework for individual differences in response to psychological intervention. Soc. Psychiatry Psychiatr. Epidemiol. 53, 545–554. doi: 10.1007/s00127-017-1471-0
Doan, B. T., Yang, Y. B., Romanchych, E., Grewal, S., Monga, S., Pignatiello, T., et al. (2021). From pandemic to progression: an educational framework for the implementation of virtual mental healthcare for children and youth as a response to COVID-19. J. Contemp. Psychother. 51, 1–7. doi: 10.1007/s10879-020-09478-0
Feijt, M., de Kort, Y., Bongers, I., Bierbooms, J., Westerink, J., and Jsselsteijn, W. (2020). Mental health care Goes online: practitioners’ experiences of providing mental health care during the COVID-19 pandemic. Cyberpsychol. Behav. Soc. Netw. 23, 860–864. doi: 10.1089/cyber.2020.0370
Fernandez, E., Woldgabreal, Y., Day, A., Pham, T., Gleich, B., and Aboujaoude, E. (2021). Live psychotherapy by video versus in-person: a meta-analysis of efficacy and its relationship to types and targets of treatment. Clin. Psychol. Psychother. 28, 1535–1549. doi: 10.1002/cpp.2594
Fernández-Álvarez, J., and Fernández-Álvarez, H. (2021). Videoconferencing psychotherapy during the pandemic: exceptional times with enduring effects? Front. Psychol. 12:589536. doi: 10.3389/fpsyg.2021.589536
Franzoi, I. G., Granieri, A., Sauta, M. D., Agnesone, M., Gonella, M., Cavallo, R., et al. (2021). Anxiety, post-traumatic stress, and burnout in health professionals during the COVID-19 pandemic: comparing mental health professionals and other healthcare workers. Healthcare 9:635. doi: 10.3390/healthcare9060635
Gardner, J. S., Plaven, B. E., Yellowlees, P., and Shore, J. H. (2020). Remote Telepsychiatry workforce: a solution to Psychiatry’s workforce issues. Curr. Psychiatry Rep. 22:8. doi: 10.1007/s11920-020-1128-7
George-Levi, S., Schmidt-Barad, T., Natan, I., and Margalit, M. (2020). Sense of coherence and burnout among school psychologists: the moderating role of loneliness. Curr. Psychol. 41, 2390–2397. doi: 10.1007/s12144-020-00766-5
Giusti, E. M., Pedroli, E., D’Aniello, G. E., Stramba Badiale, C., Pietrabissa, G., Manna, C., et al. (2020). The psychological impact of the COVID-19 outbreak on health professionals: a cross-sectional study. Front. Psychol. 11:1684. doi: 10.3389/fpsyg.2020.01684
Golonka, K., and Gulla, B. (2021). Individual differences and susceptibility to burnout syndrome: sensory processing sensitivity and its relation to exhaustion and disengagement. Front. Psychol. 12:751350. doi: 10.3389/fpsyg.2021.751350
Gruber, J., Prinstein, M. J., Clark, L. A., Rottenberg, J., Abramowitz, J. S., Albano, A. M., et al. (2021). Mental health and clinical psychological science in the time of COVID-19: challenges, opportunities, and a call to action. Am. Psychol. 76, 409–426. doi: 10.1037/amp0000707
Harris, B. A., Aajmain, S., Scharff, A., and Boswell, J. F. (2023). Outcome trajectories in a county mental health clinic before and after telemental health: a retrospective COVID-19 cohort study. Front. Psychol. 14:1095217. doi: 10.3389/fpsyg.2023.1095217
Holmqvist, R., and Jeanneau, M. (2006). Burnout and psychiatric staff’s feelings towards patients. Psychiatry Res. 145, 207–213. doi: 10.1016/j.psychres.2004.08.012
Ibrahim, F., Samsudin, E. Z., Chen, X. W., and Toha, H. R. (2022). The prevalence and work-related factors of burnout among public health workforce during the COVID-19 pandemic. J. Occup. Environ. Med. 64, e20–e27. doi: 10.1097/JOM.0000000000002428
James, G., Schröder, T., and De Boos, D. (2022). Changing to remote psychological therapy during COVID-19: psychological therapists’ experience of the working alliance, therapeutic boundaries and work involvement. Psychol. Psychother. Theory Res. Pract. 95, 970–989. doi: 10.1111/papt.12413
Jesser, A., Muckenhuber, J., and Lunglmayr, B. (2022). Psychodynamic Therapist’s subjective experiences with remote psychotherapy during the COVID-19-pandemic—a qualitative study with therapists practicing guided affective imagery, hypnosis and autogenous relaxation. Front. Psychol. 12:777102. doi: 10.3389/fpsyg.2021.777102
Johnson, J., Hall, L. H., Berzins, K., Baker, J., Melling, K., and Thompson, C. (2018). Mental healthcare staff well-being and burnout: a narrative review of trends, causes, implications, and recommendations for future interventions. Int. J. Ment. Health Nurs. 27, 20–32. doi: 10.1111/inm.12416
Joshi, G., and Sharma, G. (2020). Burnout: a risk factor amongst mental health professionals during COVID-19. Asian J. Psychiatr. 54:102300. doi: 10.1016/j.ajp.2020.102300
Jurcik, T., Jarvis, G. E., Zeleskov Doric, J., Krasavtseva, Y., Yaltonskaya, A., Ogiwara, K., et al. (2020). Adapting mental health services to the COVID-19 pandemic: reflections from professionals in four countries. Couns. Psychol. Q. 34:649–675. doi: 10.1080/09515070.2020.1785846
Kane, H., Baumgart, J. G., El-Hage, W., Deloyer, J., Maes, C., Lebas, M.-C., et al. (2022). Opportunities and challenges for professionals in psychiatry and mental health care using digital technologies during the COVID-19 pandemic: systematic review. JMIR Hum. Factors 9:e30359. doi: 10.2196/30359
Kane, H., Baumgart, J. G., Rusch, E., Deloyer, J., Fuenzalida, C., Kelemen, G., et al. (2022). The impact of COVID-19 on psychiatric and mental health services in Europe: suffering experienced by professionals. BMC Health Serv. Res. 22:1360. doi: 10.1186/s12913-022-08776-8
Kercher, A., Rahman, J., and Pedersen, M. (2024). The COVID-19 pandemic, psychologists’ professional quality of life and mental health. Front. Psychol. 15:1339869. doi: 10.3389/fpsyg.2024.1339869
Kim, Y. (2017). Secondary traumatic stress and burnout of north Korean refugees service providers. Psychiatry Investig. 14, 118–125. doi: 10.4306/pi.2017.14.2.118
Kotera, Y., Maxwell-Jones, R., Edwards, A., and Knutton, N. (2021). Burnout in professional psychotherapists: relationships with self-compassion, work–life balance, and telepressure. Int. J. Environ. Res. Public Health 18:5308. doi: 10.3390/ijerph18105308
Kupcova, I., Danisovic, L., Klein, M., and Harsanyi, S. (2023). Effects of the COVID-19 pandemic on mental health, anxiety, and depression. BMC Psychol. 11:108. doi: 10.1186/s40359-023-01130-5
Lee, H., Kuo, C., Chien, T., and Wang, Y. (2016). A meta-analysis of the effects of coping strategies on reducing nurse burnout. Appl. Nurs. Res. 31, 100–110. doi: 10.1016/j.apnr.2016.01.001
Leo, C. G., Sabina, S., Tumolo, M. R., Bodini, A., Ponzini, G., Sabato, E., et al. (2021). Burnout among healthcare workers in the COVID 19 era: a review of the existing literature. Front. Public Health 9:750529. doi: 10.3389/fpubh.2021.750529
Lheureux, F., Truchot, D., Borteyrou, X., and Rascle, N. (2017). The Maslach burnout inventory–human services survey (MBI-HSS): factor structure, wording effect and psychometric qualities of known problematic items. Le Travail Humain 80, 161–186. doi: 10.3917/th.802.0161
Lionetti, F., Dumpfrey, R. S. C., Richetin, J., Fasolo, M., Nocentini, A., Penolazzi, B., et al. (2024). Is environmental sensitivity a unique trait? A multi-sample study on the association between sensitivity, personality, and psychological adjustment. Personal. Individ. Differ. 217:112463. doi: 10.1016/j.paid.2023.112463
Luo, M., Guo, L., Yu, M., Jiang, W., and Wang, H. (2020). The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public – a systematic review and meta-analysis. Psychiatry Res. 291:113190. doi: 10.1016/j.psychres.2020.113190
Manguel, L. (2019). “Proximity and distance in teletherapy” in Psychoanalysis online 4. ed. J. S. Scharff (London: Routledge).
Maslach, C., Schaufeli, W. B., and Leiter, M. P. (2001). Job burnout. Annu. Rev. Psychol. 52, 397–422. doi: 10.1146/annurev.psych.52.1.397
Mills, L., and Huebner, E. (1998). A prospective study of personality characteristics, occupational stressors, and burnout among school psychology practitioners. J. Sch. Psychol. 36, 103–120. doi: 10.1016/S0022-4405(97)00053-8
Mitchell, E. (2020). “Much more than second best”: therapists’ experiences of videoconferencing psychotherapy. Eur. J. Qual. Res. Psychother. 10, 121–135.
Mitchell, L. M., Joshi, U., Patel, V., Lu, C., and Naslund, J. A. (2021). Economic evaluations of internet-based psychological interventions for anxiety disorders and depression: a systematic review. J. Affect. Disord. 284, 157–182. doi: 10.1016/j.jad.2021.01.092
Mittal, M., Morgan, A. A., Du, J., Jiang, J., Boekeloo, B., and Fish, J. N. (2023). “Each week feels like a mountain”: the impact of COVID-19 on mental health providers’ well-being and clinical work. Prof. Psychol. Res. Pract. 54, 103–113. doi: 10.1037/pro0000501
Nocentini, A., Menesini, E., and Pluess, M. (2018). The personality trait of environmental sensitivity predicts Children’s positive response to school-based Antibullying intervention. Clin. Psychol. Sci. 6, 848–859. doi: 10.1177/2167702618782194
Norwood, C., Moghaddam, N. G., Malins, S., and Sabin-Farrell, R. (2018). Working alliance and outcome effectiveness in videoconferencing psychotherapy: a systematic review and noninferiority meta-analysis. Clin. Psychol. Psychother. 25, 797–808. doi: 10.1002/cpp.2315
O’Connor, K., Muller Neff, D., and Pitman, S. (2018). Burnout in mental health professionals: a systematic review and meta-analysis of prevalence and determinants. Eur. Psychiatry 53, 74–99. doi: 10.1016/j.eurpsy.2018.06.003
Olwill, C., Mc Nally, D., and Douglas, L. (2021). Psychiatrist experience of remote consultations by telephone in an outpatient psychiatric department during the COVID-19 pandemic. Ir. J. Psychol. Med. 38, 132–139. doi: 10.1017/ipm.2020.51
Patel, R. S., Bachu, R., Adikey, A., Malik, M., and Shah, M. (2018). Factors related to physician burnout and its consequences: a review. Behav Sci 8:98. doi: 10.3390/bs8110098
Peng, D., Wang, Z., and Xu, Y. (2020). Challenges and opportunities in mental health services during the COVID-19 pandemic. General Psychiatry 33:e100275. doi: 10.1136/gpsych-2020-100275
Perle, J. G., Zheng, W., Gardner, L., and Law, K.-B. (2024). Editorial: education, training, and competency development for mental health-focused telehealth providers. Front. Psychol. 15:1443750. doi: 10.3389/fpsyg.2024.1443750
Pluess, M. (2015). Individual differences in environmental sensitivity. Child Dev. Perspect. 9, 138–143. doi: 10.1111/cdep.12120
Pluess, M. (2017). Vantage sensitivity: environmental sensitivity to positive experiences as a function of genetic differences. J. Pers. 85, 38–50. doi: 10.1111/jopy.12218
Pluess, M., and Belsky, J. (2013). Vantage sensitivity: individual differences in response to positive experiences. Psychol. Bull. 139, 901–916. doi: 10.1037/a0030196
Pluess, M., Lionetti, F., Aron, E. N., and Aron, A. (2023). People differ in their sensitivity to the environment: an integrated theory, measurement and empirical evidence. J. Res. Pers. 104:104377. doi: 10.1016/j.jrp.2023.104377
Poletti, B., Tagini, S., Brugnera, A., Parolin, L., Pievani, L., Ferrucci, R., et al. (2021). Telepsychotherapy: a leaflet for psychotherapists in the age of COVID-19. A review of the evidence. Couns. Psychol. Q. 34, 352–367. doi: 10.1080/09515070.2020.1769557
Probst, T., Humer, E., Stippl, P., and Pieh, C. (2020). Being a psychotherapist in times of the novel coronavirus disease: stress-level, job anxiety, and fear of coronavirus disease infection in more than 1,500 psychotherapists in Austria. Front. Psychol. 11:559100. doi: 10.3389/fpsyg.2020.559100
Redfearn, R. A., van Ittersum, K. W., and Stenmark, C. K. (2020). The impact of sensory processing sensitivity on stress and burnout in nurses. Int. J. Stress. Manag. 27, 370–379. doi: 10.1037/str0000158
Roesler, C. (2017). Tele-analysis: the use of media technology in psychotherapy and its impact on the therapeutic relationship. J. Anal. Psychol. 62, 372–394. doi: 10.1111/1468-5922.12317
Rossi, M. F., Gualano, M. R., Magnavita, N., Moscato, U., Santoro, P. E., and Borrelli, I. (2023). Coping with burnout and the impact of the COVID-19 pandemic on workers’ mental health: a systematic review. Front. Psych. 14:1139260. doi: 10.3389/fpsyt.2023.1139260
Rupert, P., and Dorociak, K. (2019). Self-care, stress, and well-being among practicing psychologists. Prof. Psychol. Res. Pract. 50, 343–350. doi: 10.1037/pro0000251
Rupert, P., Stevanovic, P., and Hunley, H. (2009). Work-family conflict and burnout among practicing psychologists. Prof. Psychol. Res. Pract. 40, 54–61. doi: 10.1037/a0012538
Rutkowska, E., Furmańska, J., Lane, H., Marques, C. C., Martins, M. J., Sahar, N. U., et al. (2023). Determinants of psychotherapists’ attitudes to online psychotherapy. Front. Psych. 14:1196907. doi: 10.3389/fpsyt.2023.1196907
Rzeszutek, M., and Schier, K. (2014). Temperament traits, social support, and burnout symptoms in a sample of therapists. Psychotherapy 51, 574–579. doi: 10.1037/a0036020
Saladino, V., Algeri, D., and Auriemma, V. (2020). The psychological and social impact of Covid-19: new perspectives of well-being. Front. Psychol. 11:577684. doi: 10.3389/fpsyg.2020.577684
Sampaio, M., Navarro Haro, M. V., De Sousa, B., Vieira Melo, W., and Hoffman, H. G. (2021). Therapists make the switch to telepsychology to safely continue treating their patients during the COVID-19 pandemic. Virtual reality telepsychology may be next. Front. Virtual Real 1:576421. doi: 10.3389/frvir.2020.576421
Santillan-Ramos, P., Humer, E., Schaffler, Y., Pieh, C., Probst, T., Felnhofer, A., et al. (2024). Impact of the COVID-19 pandemic on the work of clinical psychologists in Austria: results of a mixed-methods study. Front. Psychol. 15:1302442. doi: 10.3389/fpsyg.2024.1302442
Schaufeli, W. B., Bakker, A. B., and Van Rhenen, W. (2009). How changes in job demands and resources predict burnout, work engagement, and sickness absenteeism. J. Organ. Behav. 30, 893–917. doi: 10.1002/job.595
Shklarski, L., Abrams, A., and Bakst, E. (2021). Will we ever again conduct in-person psychotherapy sessions? Factors associated with the decision to provide in-person therapy in the age of COVID-19. J. Contemp. Psychother. 51, 265–272. doi: 10.1007/s10879-021-09492-w
Shore, J. (2015). The evolution and history of telepsychiatry and its impact on psychiatric care: current implications for psychiatrists and psychiatric organizations. Int. Rev. Psychiatry 15, 469–475. doi: 10.3109/09540261.2015.1072086
Simionato, G., Simpson, S., and Reid, C. (2019). Burnout as an ethical issue in psychotherapy. Psychotherapy 56, 470–482. doi: 10.1037/pst0000261
Simpson, S. G., and Reid, C. L. (2014). Therapeutic alliance in videoconferencing psychotherapy: A review. The Australian Journal of Rural Health, 22, 280–299. doi: 10.1111/ajr.12149
Simpson, S., Richardson, L., Pietrabissa, G., Castelnuovo, G., and Reid, C. (2021). Videotherapy and therapeutic alliance in the age of COVID-19. Clin. Psychol. Psychother. 28, 409–421. doi: 10.1002/cpp.2521
Singh, J., Karanika-Murray, M., Baguley, T., and Hudson, J. (2020). A systematic review of job demands and resources associated with compassion fatigue in mental health professionals. Int. J. Environ. Res. Public Health 17:19. doi: 10.3390/ijerph17196987
Smout, M. F., Simpson, S. G., Stacey, F., and Reid, C. (2021). The influence of maladaptive coping modes, resilience, and job demands on emotional exhaustion in psychologists. Clin. Psychol. Psychother. 29, 260–273. doi: 10.1002/cpp.2631
Stefan, R., Mantl, G., Höfner, C., Stammer, J., Hochgerner, M., and Petersdorfer, K. (2021). Remote psychotherapy during the COVID-19 pandemic. Experiences with the transition and the therapeutic relationship. A longitudinal mixed-methods study. Front. Psychol. 12:743430. doi: 10.3389/fpsyg.2021.743430
Stefana, A., Fusar-Poli, P., Vieta, E., and Youngstrom, E. A. (2024). Patients’ perspective on the therapeutic relationship and session quality: the central role of alliance. Front. Psychol. 15:1367516. doi: 10.3389/fpsyg.2024.1367516
Stoll, J., Müller, J. A., and Trachsel, M. (2020). Ethical issues in online psychotherapy: a narrative review. Front. Psych. 10:993. doi: 10.3389/fpsyt.2019.00993
Stubbe, D. E. (2018). The therapeutic Alliance: the fundamental element of psychotherapy. Focus 16, 402–403. doi: 10.1176/appi.focus.20180022
Sun, R., Yang, H. M., Chau, C. T. J., Cheong, I. S., and Wu, A. M. S. (2023). Psychological empowerment, work addiction, and burnout among mental health professionals. Curr. Psychol. 42, 25602–25613. doi: 10.1007/s12144-022-03663-1
Tajan, N., Devès, M., and Potier, R. (2023). Tele-psychotherapy during the COVID-19 pandemic: a mini-review. Front. Psych. 14:1060961. doi: 10.3389/fpsyt.2023.1060961
Tohme, P., De Witte, N. A. J., Van Daele, T., and Abi-Habib, R. (2021). Telepsychotherapy during the COVID-19 pandemic: the experience of Lebanese mental health professionals. J. Contemp. Psychother. 51, 349–355. doi: 10.1007/s10879-021-09503-w
Ulfa, M., Azuma, M., and Steiner, A. (2022). Burnout status of healthcare workers in the world during the peak period of the COVID-19 pandemic. Front. Psychol. 13:952783. doi: 10.3389/fpsyg.2022.952783
Van Hoy, A., and Rzeszutek, M. (2022). Burnout and psychological wellbeing among psychotherapists: a systematic review. Front. Psychol. 13:928191. doi: 10.3389/fpsyg.2022.928191
Vivolo, M., Owen, J., and Fisher, P. (2024). Psychological therapists’ experiences of burnout: a qualitative systematic review and meta-synthesis. Mental Health Prevent. 33:200253. doi: 10.1016/j.mhp.2022.200253
Wibberly, K. H. (2024). Preparing mental health providers for the future: the case for moving beyond the elective telehealth course to integrating telehealth training throughout the curriculum. Front. Psychol. 14:1301569. doi: 10.3389/fpsyg.2023.1301569
Woo, T., Ho, R., Tang, A., and Tam, W. (2020). Global prevalence of burnout symptoms among nurses: a systematic review and meta-analysis. J. Psychiatr. Res. 123, 9–20. doi: 10.1016/j.jpsychires.2019.12.015
Yang, Y., and Hayes, J. A. (2020). Causes and consequences of burnout among mental health professionals: a practice-oriented review of recent empirical literature. Psychotherapy 57, 426–436. doi: 10.1037/pst0000317
Yellowlees, P., Nakagawa, K., Pakyurek, M., Hanson, A., Elder, J., and Kales, H. C. (2020). Rapid conversion of an outpatient psychiatric clinic to a 100% virtual Telepsychiatry Clinic in Response to COVID-19. Psychiatric services (Washington, D.C.), 71(7), 749–752
Zarzycka, B., Jankowski, T., and Krasiczyńska, B. (2022). Therapeutic relationship and professional burnout in psychotherapists: a structural equation model approach. Clin. Psychol. Psychother. 29, 250–259. doi: 10.1002/cpp.2629
Zavattini, G. C. (2014). Dentro o fuori la Strega? Per una “soggettività disciplinata” in psicologia clinica. Giornale Italiano di Psicologia, XXXVI, 3: 623–629. doi: 10.1421/78507
Keywords: burn-out, online therapy, telepsychology, environmental sensitivity, clinical method, quality of care, mental health strategy
Citation: Cavarretta MV, Pellerin H, Maurel E, Anzalone SM, Truck I, Cohen D and Ingoglia S (2025) The effectiveness of online therapy in promoting wellbeing and reducing burnout among psychotherapists. Front. Psychol. 16:1510383. doi: 10.3389/fpsyg.2025.1510383
Received: 12 October 2024; Accepted: 17 February 2025;
Published: 31 March 2025.
Edited by:
Evgenia Gkintoni, General University Hospital of Patras, GreeceReviewed by:
Ermanno Vitale, Kore University of Enna, ItalyCopyright © 2025 Cavarretta, Pellerin, Maurel, Anzalone, Truck, Cohen and Ingoglia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria Valentina Cavarretta, bWFyaWF2YWxlbnRpbmEuY2F2YXJyZXR0YUB1bmlwYS5pdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.