- 1Department of Kinesiology, Iowa State University, Ames, IA, United States
- 2Department of Health and Human Development, University of Pittsburgh, Pittsburgh, PA, United States
Introduction: Physical activity (PA) is associated with better perceived health among individuals with chronic conditions. However, PA’s relationship with perceived health in people with long COVID is unclear and may be modified by long COVID symptom burden.
Methods: Participants with self-reported long COVID (N = 379) responded to an online survey cross-sectionally assessing PA levels, perceived physical and mental health, and intensity of CDC-defined long COVID symptoms on a 0–100 scale. Linear regression analyses assessed the associations between PA and perceived physical and mental health, after accounting for sociodemographic, health behavior, and long COVID intensity variables, with post-hoc analyses comparing health across PA levels.
Results: Increasing levels of PA were associated with increases in perceived physical health (β = 0.27, p < 0.001) and mental health (β = 0.19, p < 0.001) after accounting for sociodemographic and health behavior variables. PA remained significantly associated with perceived physical health (β = 0.15, p < 0.001) but not perceived mental health (β = 0.09, p = 0.067) after the adding long COVID intensity to the model. Insufficiently active and active groups reported significant better physical and mental health than the inactive group (ps < 0.05), while the highly active group did not significantly differ from any other group on perceived physical or mental health (ps > 0.05). Inactive individuals reported significantly greater long COVID symptom burden compared to each other PA level (ps < 0.05).
Conclusion: Higher levels of PA may be associated with better physical health among individuals with long COVID, even after accounting for symptom intensity. However, long COVID symptom intensity may confound the relationship between PA and mental health among individuals with long COVID.
Introduction
Long COVID, also called post-acute sequalae of COVID-19 (PASC), describes the experience of long-term symptoms following COVID-19 infection (Davis et al., 2023) Up to 20% of those infected with COVID-19 develop long COVID, and estimates suggest that over 65 million individuals are affected worldwide (Davis et al., 2023). Long COVID has been associated with significantly worse physical and mental health compared to the general population without long COVID (Ganesh et al., 2021; Sirotiak et al., 2023, 2024a, 2024b). Symptoms of long COVID are wide-ranging and heterogenous, complicating research and treatment efforts (Aiyegbusi et al., 2021). Long COVID is frequently diagnosed by a process of exclusion, in which other potential causes of symptoms are ruled out prior to diagnosis (Koc et al., 2022; Davis et al., 2023; Srikanth et al., 2023). Treatment options for long COVID are limited given the unclear nature of the condition and heterogenous symptom presentation (Koc et al., 2022; Davis et al., 2023). Somatic syndromes, such as fibromyalgia, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), and irritable bowel syndrome, describe collections of physiological symptoms that cannot be attributed to a clear organic cause (Barsky and Borus, 1999; Salari et al., 2022; Savin et al., 2023; Ursini et al., 2023). Active management strategies such as exercise and psychotherapy are common treatment strategies for these conditions, which have emerged as common comorbidities of long COVID (Henningsen, 2018; Salari et al., 2022; Savin et al., 2023; Ursini et al., 2023). Given the unclear cause of long COVID and lack of medical treatment options available, identifying self-management strategies may be particularly important to those living with long COVID.
Physical activity (PA) is one treatment strategy in the context of somatic syndromes, including long COVID, with unclear results (Twisk and Maes, 2009; Johannesson et al., 2015; Vink and Vink-Niese, 2018; Larun et al., 2019; White and Etherington, 2021). Long COVID groups undergoing exercise intervention have reported improved dyspnea, anxiety, kinesiophobia (fear of PA), muscle strength, walking capacity, quality of life, and perceived fatigue (Fugazzaro et al., 2022; Araújo et al., 2023). However, in a cross-sectional retrospective study investigating the relationship between long COVID symptoms and PA, 75% of the sample noted that PA worsened their symptoms, while just 1% reported improved symptoms following PA (Wright et al., 2022). Particularly among individuals who were physically active prior to COVID-19, a lack of ability to return to prior athletic abilities has been related to depression, suicidal thoughts, and desperation regarding a return to PA (Humphreys et al., 2021; Shelley et al., 2021). While 84% of individuals with long COVID reported meeting the PA guidelines prior to long COVID, only 8% met them at present (Wright et al., 2022).
Most studies concerning PA and long COVID have specifically considered the impact of PA on long COVID symptoms, rather than identifying the associations between PA and perceived health status (Humphreys et al., 2021; Shelley et al., 2021; Wright et al., 2022). While long COVID symptom status may be a useful consideration in tracking condition progression, perceived health may provide better information regarding the impact to the lived experience and functional abilities of each individual affected. Health perception, defined as an individual’s beliefs regarding their health status, describes to what degree an individual feels they can function in physical, mental, and social domains (Kaleta et al., 2009). By considering an individual’s quality of life and functional abilities, rather than just their physiological status or symptoms, the recent consideration of perceived health in medical research has been heralded as a meaningful and impactful change to health-related measurement in a variety of populations (Broderick et al., 2013). Therefore, the purpose of this study is to investigate the association of PA and symptom intensity with perceived physical and mental health among individuals with long COVID.
Method
A total of 379 adults in the United States (US) with self-reported long COVID responded to an online survey inquiring about sociodemographic characteristics, health status, psychological traits, and experiences during the COVID-19 pandemic. Participants were asked the number of times they had experienced COVID-19, either confirmed by a lab test (PCR, antigen, or other) or assumed by a healthcare provider or themselves. Individuals endorsing at least one infection were then asked whether they experienced long-term symptoms following COVID-19 infection. Participants endorsing currently experiencing long-term symptoms following COVID-19 infection were considered to have long COVID. Participants were not required to report symptoms for a specific duration of time due to the variation in the duration labeled long-term symptoms of COVID-19; instead, long COVID status was self-reported. Inclusion criteria included being over the age of 18 and US-dwelling. Participants were recruited through mass email to students, staff, faculty, and alumni at a large university, as well as posts on long COVID-specific social media sites. The study was approved by the Iowa State University Institutional Review Board and participants indicated consent prior to entering the survey.
Measures
Participant characteristics
Respondents reported age, gender identity, racial and ethnic groups, highest level of education, and annual income.
Long COVID symptom intensity
Participants endorsed long COVID symptoms currently experienced from a list of long COVID symptoms offered by the CDC (Center for Disease Control and Prevention, 2022). Participants were presented with a 0–100 scale and asked to rate the intensity of each endorsed symptom, with higher scores associated with greater severity of that symptom. Symptoms were grouped as defined by the CDC (Center for Disease Control and Prevention, 2022) into five categories: (1) general symptoms: exhaustion, tiredness, or fatigue; fever; symptoms that worsen after physical or mental effort; (2) cardiorespiratory symptoms: difficulty breathing or shortness of breath; cough; chest pain or tightness; fast heart rate or heart palpitations; (3) neurological symptoms: difficulty thinking, concentrating, or brain fog; pins-and-needles feeling (nerve pain); headache; lightheadedness or dizziness; sleep problems; changes in smell or taste; depression; anxiety; (4) digestive symptoms: abdominal or stomach pain; diarrhea; and (5) other symptoms: joint or muscle pain; rash; changes in menstrual cycle. Overall intensity ratings represented the combined symptom intensity, with the intensity of individual symptoms reported summed. Each subcategory of symptoms was also assigned an average intensity rating of endorsed symptoms within each symptom category.
Perceived physical and mental health
Perceived physical and mental health were measured with the Patient Reported Outcomes Measurement Information System (PROMIS) Global Health, version 1.2 (National Institutes of Health, 2019). Two subscale scores can be calculated from the full scale, resulting in physical and mental health subscales. Each subscale consisted of four items. Physical health questions included a question about general physical health, ability to carry out activities of daily living, average pain, and average fatigue. Mental health questions included a question about quality of life, general mental health including mood and thinking ability, satisfaction with social activities and relationships, and emotional problems. Raw scores for each subscale were converted to T-scores, with a mean of 50 and a standard deviation of 10, as indicated by established values for the US adult population (Northwestern University, 2023). Higher scores indicate better perceived physical and mental health. Internal consistency within the current sample was as follows: physical health α = 0.59 (α = 0.69 among individuals with no missingness); mental health α = 0.67 (α = 0.75 among individuals with no missingness). This scale has been utilized in similar chronic illness populations (Merriwether et al., 2016; Pak et al., 2021).
Physical activity level
Moderate (e.g., brisk walking) or vigorous (e.g., running) aerobic PA level was measured by inquiring about the number of minutes in an average week each participant engages in moderate or vigorous aerobic PA. Participants selected from four provided options: 0 min; 1 to <150 min; 150 to <300 min; and ≥ 300 min per week. Responses fit into established categories based on the 2018 Physical Activity Guidelines for Americans (0 min = inactive; 1 to <150 min = insufficiently active; 150 to <300 min = active; ≥300 min = highly active) (U.S. Department of Health and Human Services, 2018).
Alcohol consumption
Alcohol intake was measured, which was then converted into four categories of alcohol consumption: never, former, moderate, and excessive. Moderate alcohol consumption was considered to be 14 drinks or less per week for men, or 7 drinks or less per week for women (U.S. Department of Agriculture and U.S. Department of Health and Human Services, 2020). Excessive alcohol consumption was considered to more than 14 drinks per week for men or more than 7 drinks per week for women.
Smoking status
Participants reported whether they currently smoke cigarettes, chew tobacco, vape, or use e-cigarettes. Responses were coded dichotomously: “yes” or “no.”
Sleep quality
Sleep quality was assessed with the Patient-Reported Outcome Measurement Information System (PROMIS) Sleep Disturbance Short Form 4a (PROMIS Health Organization, 2021). Respondents rate 4 items, two of which are reverse coded, on a 5-point Likert scale. Scores range from 4 to 20, with higher scores indicating greater sleep disturbance. Raw scores were translated into established T-scores for each participant, as recommended (PROMIS Health Organization, 2021). Internal consistency in the current sample was α = 0.62 (α = 0.69 among individuals with no missingness). The PROMIS sleep measures have been utilized in similar chronic condition populations (Burgess et al., 2019; Chimenti et al., 2021).
Statistical analyses
Statistical analyses were conducted in SPSS, version 27 (IBM Corp, 2020). There were no imputations performed on any scale. Sociodemographic variables (age, gender identity, racial and ethnic group, education, and income) that have been associated with long COVID were included in the regression analyses as covariates (Perlis et al., 2022; Jacobs et al., 2023). Alcohol use, smoking status, and sleep disturbance were also included as covariates due to their association with long COVID (Wickham et al., 2020; Paul and Fancourt, 2022; Subramanian et al., 2022). Gender identity, racial group, and ethnic group were dichotomized (male/female, white/non-white, not Hispanic or Latino/Hispanic or Latino) to reduce categories with a low number of participants.
Multivariable linear regression models were used to assess the association between PA level and perceived physical and mental health. Model 1 consisted of current PA level, while Model 2 added sociodemographic characteristics (age, gender identity, racial and ethnic group, education, and income). Model 3 added health behaviors (alcohol use, smoking status, sleep disturbance). Post-hoc comparison tests with Bonferroni adjustment assessed differences in perceived health among PA levels after accounting for sociodemographic and health behavior variables. Model 4 considered intensity of long COVID symptoms. A linear regression model with Bonferroni-adjusted post-hoc comparisons assessed differences in average intensity ratings for CDC-defined groupings of symptoms by PA level. Individuals with missing variables in the model were removed from that analysis. A significant level of p < 0.05 was utilized for each analysis.
Results
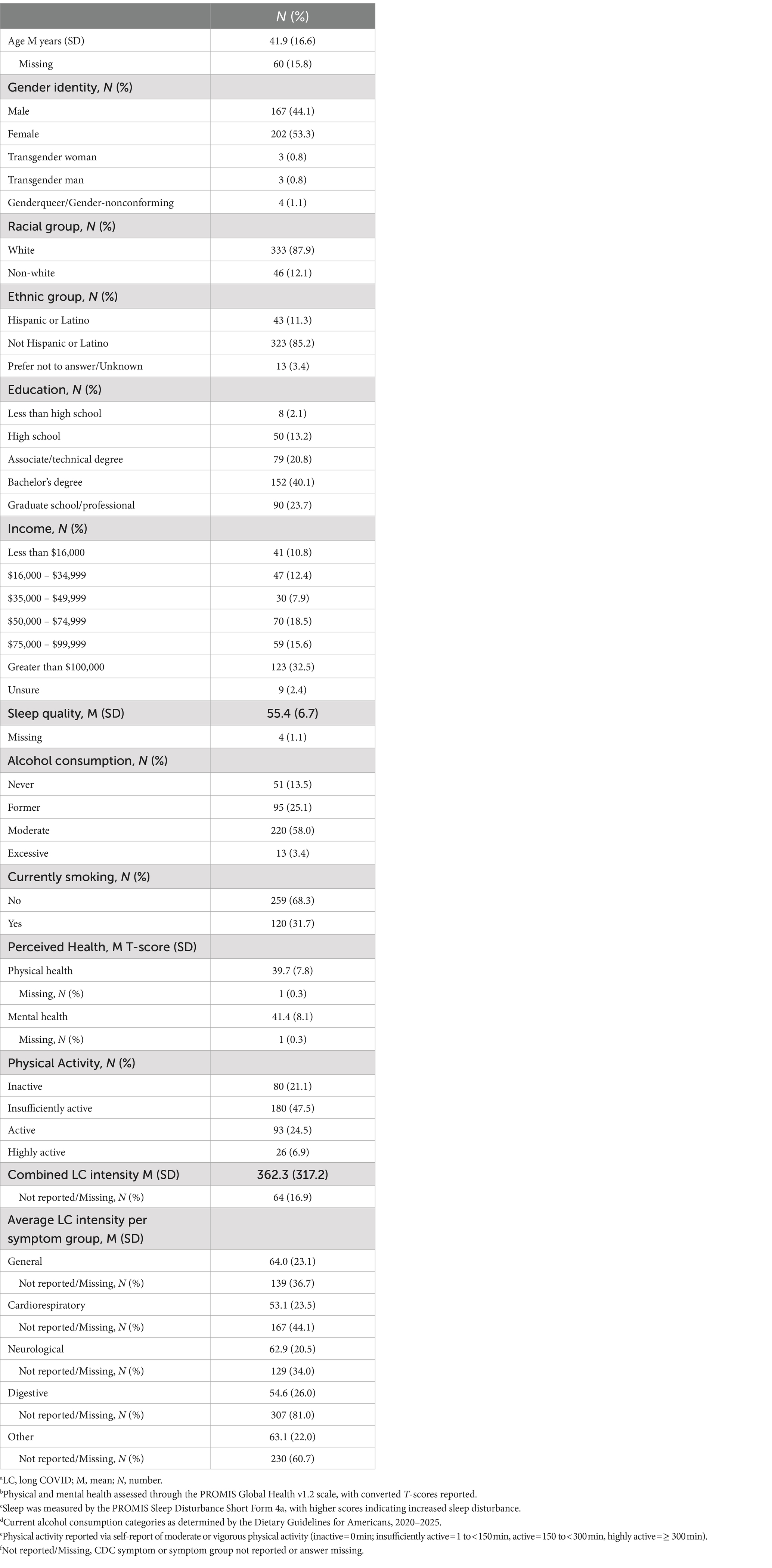
Participants were an average 41.9 (SD = 16.6) years old, and most identified as female (53.3%), white (87.9%) and not Hispanic or Latino (85.2%). Most of the sample had received at least a bachelor’s degree (63.8%). More than half participants noted moderate alcohol intake (58.0%) and no smoking (68.3%). The sample reported half a standard deviation greater sleep disturbance than the U.S. general population (T = 55.4), and perceived physical and mental health one standard deviation worse than the U.S. general population (Ts = 39.7, 41.4, respectively) (PROMIS Health Organization, 2021; Northwestern University, 2023). Around half (47.5%) of the participants reported being insufficiently active. Detailed sociodemographic characteristics can be viewed in Table 1.
A linear regression model demonstrated that PA level was significantly positively associated with perceived physical health (Model 1; β = 0.35, t(281) = 6.20, p < 0.001). PA level remained significantly associated with perceived physical health after accounting for sociodemographic variables (Model 2; β = 0.32, t(281) = 5.80, p < 0.001) and health behaviors (Model 3; β = 0.27, t(281) = 5.34, p < 0.001). The total intensity of CDC-defined long COVID symptoms significantly contributed to the model (Model 4; β = −0.48, t(281) = −9.85, p < 0.001). However, the association between PA level and perceived physical health remained significant after accounting for long COVID intensity (Model 4; β = 0.15, t(281) = 3.44, p < 0.001). In the sensitivity analysis, the interaction of PA and long COVID intensity on perceived physical health was not significant (β = −0.11, t(281) = −1.06, p = 0.292). Detailed results can be viewed in Table 2.
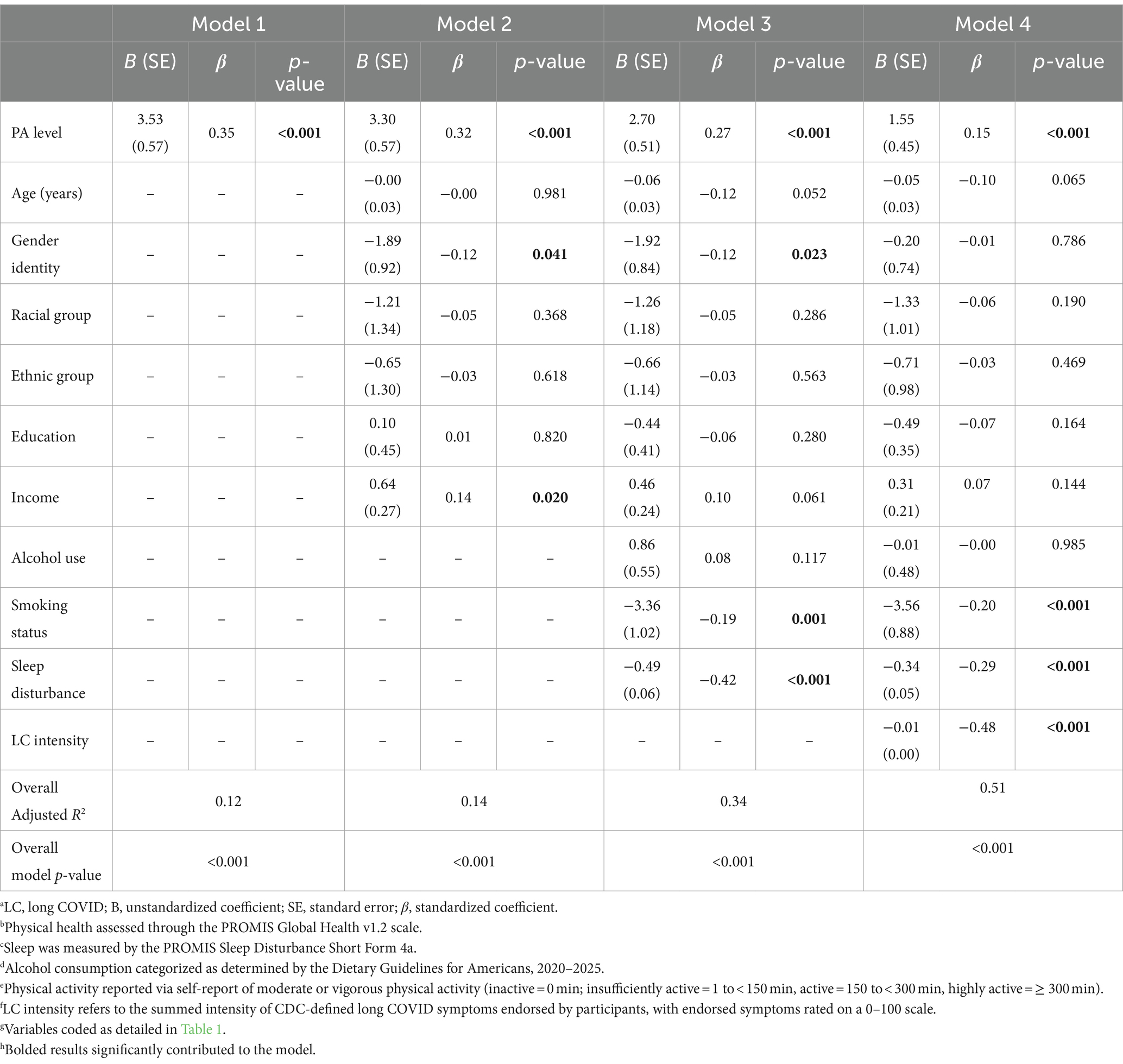
Table 2. Multivariable linear regression of PA level and long COVID symptom intensity on physical health.
A linear regression model demonstrated that PA level was significantly associated with perceived mental health (Model 1; β = 0.28, t(281) = 4.94, p < 0.001). PA level continued to remain significantly associated with perceived mental health after accounting for sociodemographic variables (Model 2; β = 0.25, t(281) = 4.58, p < 0.001) and health behaviors (Model 3; β = 0.19, t(281) = 3.77, p < 0.001). The total intensity of CDC-defined long COVID symptoms significantly contributed to the model (Model 4; β = −0.45, t(281) = −8.74, p < 0.001). The association between PA level and perceived mental health was no longer significant after accounting for long COVID intensity (Model 4; β = 0.09, t(281) = 1.84, p = 0.067). In the sensitivity analysis, the interaction of PA and long COVID intensity on perceived mental health was not significant (β = −0.10, t(281) = −0.90, p = 0.369). Detailed regression results can be found in Table 3.

Table 3. Multivariable linear regression of PA level and long COVID symptom intensity on mental health.
Post-hoc comparison tests with Bonferroni adjustment (Model 3) were utilized to determine estimated marginal means of perceived physical health T-score by PA level, M(SE): inactive: 36.1 (0.9); insufficiently active: 39.7 (0.5); active: 42.8 (0.8); highly active: 41.1 (1.8). The comparison tests with Bonferonni adjustment demonstrated that the inactive group reported significantly worse perceived physical health than the insufficiently active (p = 0.002) and active (p < 0.001) groups. The insufficiently active group had significantly worse perceived physical health than the active group (p = 0.013). The highly active group did not significantly differ from any of the other PA levels (ps > 0.05), in part due to small sample size. Post-hoc comparison tests with Bonferroni adjustment (Model 3) were utilized to determine estimated marginal means of perceived mental health T-score by PA level, M(SE): inactive: 38.1 (0.9); insufficiently active: 41.6 (0.6); active: 43.0 (0.9); highly active: 42.0 (1.9). The comparison tests with Bonferonni adjustment showed the inactive group had significantly worse perceived mental health than the insufficiently active (p = 0.009) and active (p < 0.001) groups. The highly active group did not significantly differ in their mental health from any other activity group (p > 0.05). Figure 1 demonstrates these relationships among PA levels.
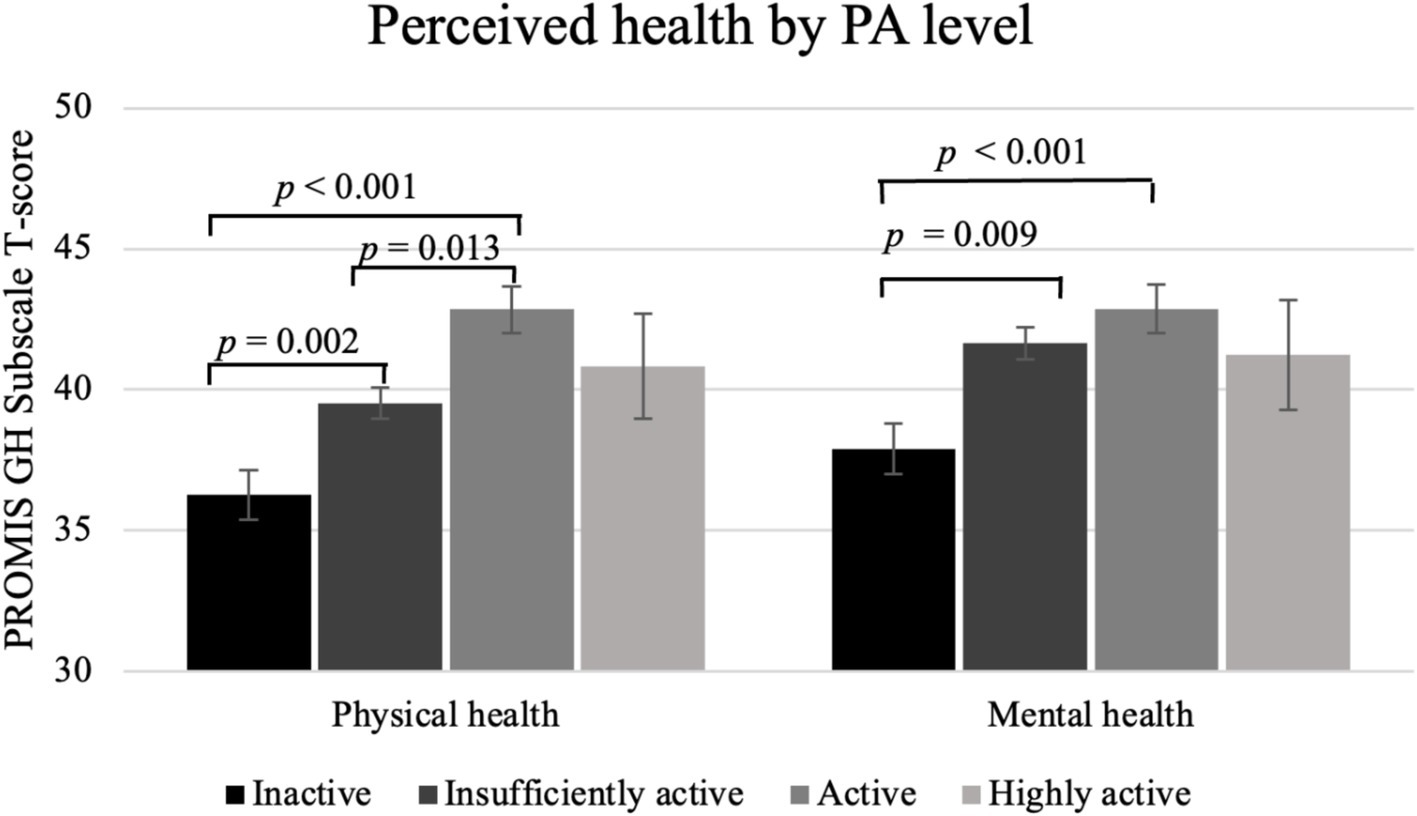
Figure 1. Perceived physical and mental health by PA level among individuals with long COVID. Physical health assessed through the PROMIS Global Health v1.2 scale. Physical activity reported via self-report of moderate or vigorous physical activity (inactive = 0 min; insufficiently active = 1 to <150 min, active = 150 to <300 min, highly active = ≥300 min). Estimated marginal means shown, adjusted for age, gender identity, racial and ethnic group, education, income, alcohol consumption, current smoking status, and sleep disturbance. Standard error bars shown.
Combined symptom intensity, considering all CDC-defined long COVID symptoms, was significantly higher among inactive individuals. The inactive group reported significantly greater combined long COVID intensity compared to the insufficiently active (p < 0.001), active (p < 0.001), and highly active (p = 0.006) groups following Bonferroni adjustment. However, no other comparisons among PA levels were significant (ps > 0.05). Overall intensity ratings by PA level can be viewed in Figure 2. The average intensity within each CDC-defined symptom category generally showed the highest intensity rating across symptom categories among the inactive group, except for the digestive symptom category, which had the highest intensity rating among the highly active group. However, the only significant comparison among symptom groups by PA level was significantly greater general long COVID intensity among the active group compared to the inactive group (p = 0.005). Average intensity symptom ratings by symptom group and PA level can be viewed in Figure 2b.
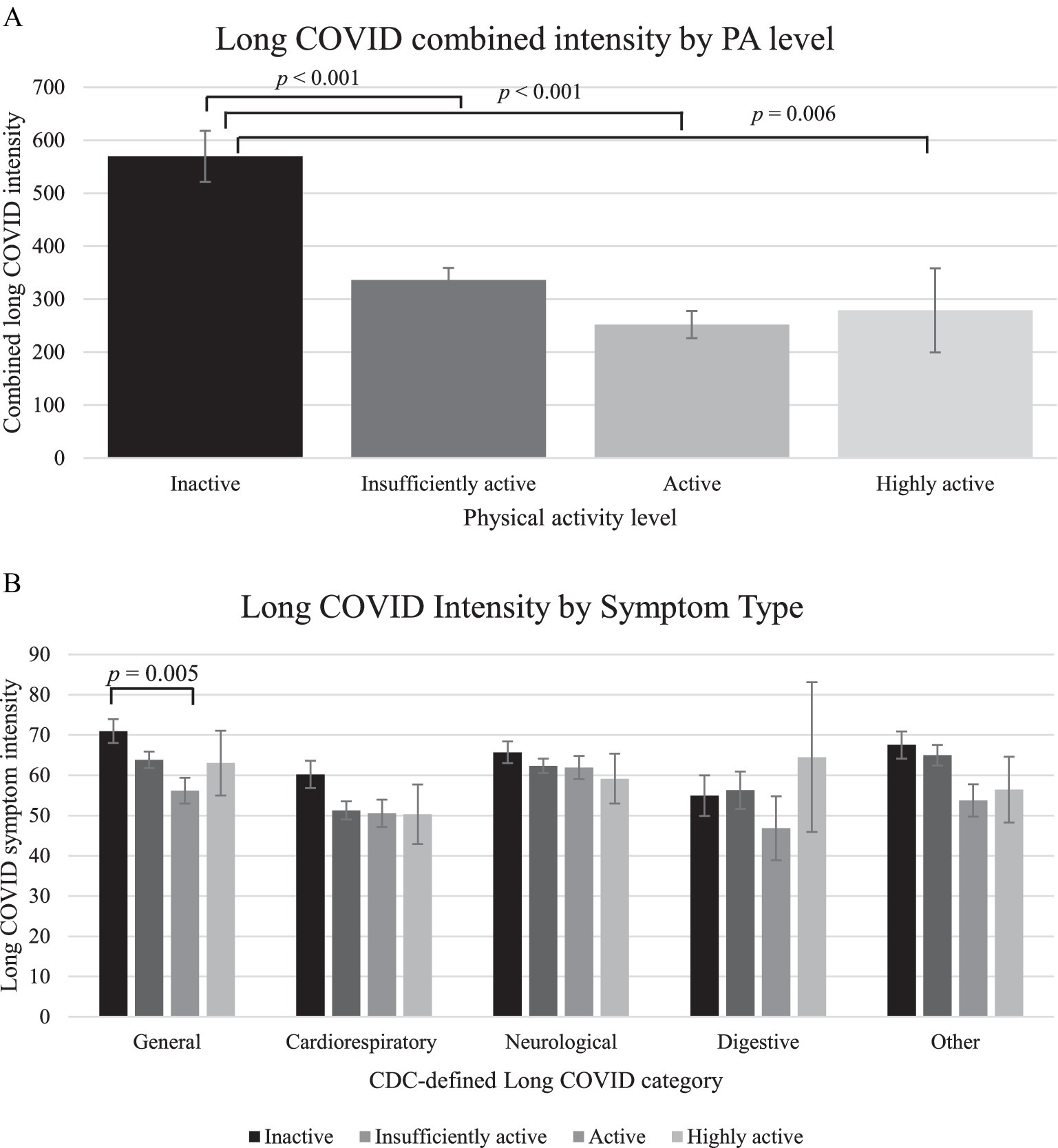
Figure 2. (a) Long COVID combined intensity by PA level. (b) Long COVID intensity in each CDC-defined symptom group by PA level. Mean intensity shown. Physical activity reported via self-report of moderate or vigorous physical activity (inactive = 0 min; insufficiently active = 1 to <150 min, active = 150 to <300 min, highly active = ≥ 300 min). Long COVID symptom groups are as defined by the CDC. All comparisons not noted as significant had p-values >0.05 following Bonferroni adjustment. Standard error bars shown.
Discussion
The significant association between PA level and perceived physical health among individuals with long COVID fits with literature noting improvements in physical health with increasing PA levels among both control and long COVID samples (Anderson and Durstine, 2019; Fugazzaro et al., 2022; Araújo et al., 2023). Similar to the PA and perceived physical health association, PA was significantly associated with perceived mental health among the sample, fitting with PA intervention studies in the context of long COVID (Araújo et al., 2023). Long COVID intensity was significantly associated with both perceived physical and mental health after accounting for sociodemographic and health behaviors, including PA level. PA level continued to be significantly associated with perceived physical health after accounting for long COVID intensity, further supporting the idea that PA appears to be uniquely associated with physical health in long COVID beyond sociodemographic, illness severity, and health behavior factors (Humphreys et al., 2021; Wright et al., 2022; Colas et al., 2023).
Increasing PA levels were generally associated with increasing levels of perceived health, fitting with literature noting better physical and mental health ratings among individuals with long COVID engaging in more PA (Vélez-Santamaría et al., 2023). Comparisons involving the inactive category particularly stood out, with insufficiently active and active groups reporting significantly greater perceived physical and mental health scores than inactive individuals. These results suggest that any amount of PA within the comfort zone and ability level of individuals with long COVID may provide physical and mental health benefits, although prospective data are required. The consistent increases in perceived physical and mental health with increasing PA level fits with established literature in both healthy and clinical samples demonstrating that even a small volume of PA can have measurable health benefits (Blair et al., 1992; Huber et al., 2020; Centers for Disease Control and Prevention, 2023b).
Although the insufficiently active and active groups reported better perceived physical and mental health than inactive individuals, comparisons of other PA levels with the highly active group were not significant in both perceived physical and mental health analyses, conflicting with findings in the general population showing that each increased activity level is associated with better perceived health (Tyson et al., 2010). It is unclear why there was a tapering of perceived health observed among the highly active group, but there are several possible explanations. Post-exertional malaise, or worsened symptoms following physical, mental, or emotional exertion, can affect both physical and mental health and it has been noted following PA among individuals with long COVID (Stussman et al., 2020; Humphreys et al., 2021; Vernon et al., 2023; Appelman et al., 2024). It is possible that high levels of PA, while providing some perceivable health benefits, may also be associated with post-exertional malaise, attenuating perceived health. However, post-exertional malaise is often noted following even low intensity and duration of exertion among individuals affected (Centers for Disease Control and Prevention, 2023a), and it is unclear whether or why individuals reporting high levels of activity may be particularly prone in this sample. Symptomatic responses to PA were also not assessed in our sample, complicating the consideration of response to exercise and post-exertional malaise among PA groups.
Regarding the lack of significant perceived mental health comparisons among the highly active group, individuals who were physically active before COVID-19, such as living an active lifestyle or being a competitive athlete, have reported significant losses of identity associated with long COVID development and loss of abilities (Humphreys et al., 2021; Shelley et al., 2021; Wurz et al., 2022). It is possible that individuals who were physically active before COVID-19 may continue to attempt high levels of PA, becoming frustrated when their physical ability limitations become apparent (Humphreys et al., 2021; Shelley et al., 2021; Wurz et al., 2022), leading to the lack of improved perceived mental health noted among highly active individuals with long COVID. Observational studies among long COVID samples have reported conflicting associations between PA and mental health, with some participants reporting improved mental health and cognitive functioning with PA, while others report that their symptoms worsen (Humphreys et al., 2021; Shelley et al., 2021; Wright et al., 2022). Illness perception, coping mechanisms, and previous mental health status may each affect how an individual understands and manages their condition, affecting their mental health, thus offering other explanations for the results that were not accounted for in the regression analyses (Turner and Kelly, 2000; Petrie et al., 2008; Algorani and Gupta, 2023). The relatively low number of individuals with long COVID reporting being highly active (N = 26; 6.9%) compared to the other PA level groups is another important consideration. The highly active group reported greater variation in perceived health compared to the other PA levels, with over double the standard error of the second most variable PA level in both the physical health (SE = 1.83), and mental health (SE = 1.96) models. Therefore, it appears that individuals reporting both relatively low and high ratings of perceived health (physical health range: T = 26.7–54.1; mental health range: T = 28.4–62.5) may have been included in this PA level group, creating a wide distribution of perceived health scores within the highly active group and contributing to the lack of significant comparisons observed.
Long COVID severity is another important consideration in understanding perceived health. Individuals with severe ME/CFS are often bedbound for extensive periods of time, limiting most PA including activities of daily living (Chang et al., 2021; Montoya et al., 2021). Long COVID appears to follow a similar course, with severely affected individuals limited in most aspects of daily life (Brodin et al., 2022; Davis et al., 2023). Severely ill individuals with ME/CFS have noted significant health burden (Chang et al., 2021; Ziauddeen et al., 2022), including fatigue, pain interference, and pain behavior. Given the strong associations between ME/CFS and long COVID (Komaroff and Lipkin, 2023), it seems plausible that long COVID severity may be driving the association noted between PA levels and perceived physical and mental health (i.e., people with severe symptoms may be more likely to be inactive and have worse perceived health). Following the addition of combined long COVID severity to the model, however, current PA level remained significantly associated with perceived physical health (p < 0.001), but not perceived mental health (p = 0.067). The few significant differences among PA groups in average severity by CDC-defined symptom category further suggest that PA appears to be uniquely associated with perceived physical health, suggesting that PA promotion, even to levels below the current PA guidelines, may be helpful in enhancing physical health in the context of long COVID.
Although PA level continued to be associated with perceived physical health after accounting for long COVID intensity, long COVID intensity was a stronger predictor of perceived health. Long COVID intensity had an absolute standardized coefficient more than three times greater than that of PA in predicting perceived physical health (β = −0.48 and 0.15, respectively), and an absolute standardized coefficient more than four times greater than that of PA in predicting mental health (β = −0.45 and 0.09, respectively). This result seems to fit with literature noting that perceived severity of illness is negatively associated with perceived health in clinical contexts (Lackner et al., 2014; Kim et al., 2015). Therefore, while PA level appears to be positively associated with perceived physical and mental health, the intensity of long COVID symptoms experienced appears to be a more impactful predictor. Increasing PA levels, particularly from inactive to at least some PA may be a useful long COVID management technique, however, our results indicate that targeting long COVID intensity, and ensuring that PA does not worsen symptoms, must be considered as well. Strategies previously suggested in the context of other somatic syndromes include treating the most disruptive symptoms first and identifying treatment strategies that target multiple symptoms for maximum benefit (Centers for Disease Control and Prevention, 2021).
This study had limitations. First, the survey offered a cross-sectional assessment of long COVID and PA, as well as perceived physical and mental health, and causation and direction of association cannot be inferred. The survey relied on participant self-report for diagnosis of COVID-19, though it has been reported that some who report prior COVID-19 infection do not have COVID-19 antibodies (Matta et al., 2022). PA status was also self-reported, and muscle strengthening PA was not assessed. Moderate and vigorous intensity PA were not individually assessed, and the PA level assignment of individuals may vary from the 2018 Physical Activity Guidelines for Americans, which doubles vigorous minutes in the determination of moderate-to-vigorous PA level (U.S. Department of Health and Human Services, 2018). In addition, limited medical history was obtained, and it is unclear how unmeasured physical comorbidities might have affected the results. The inclusion and exclusion criteria, as well as the recruitment strategies utilized in the study may have affected those who participated in the study, limiting generalizations and conclusions that can be drawn from the data. Although this study consisted of largely of individuals with white and not Hispanic or Latino identities, as well as those with high educational attainment and higher annual income, individuals with not white and Hispanic or Latino identities, as well as individuals with lower educational attainment and lower annual income have been suggested to be more likely to develop long COVID and be more severely affected (Wong and Weitzer, 2021; Jacobs et al., 2023; Tanne, 2023). No official definition of long COVID was utilized, with all participants endorsing current long-term symptoms following COVID-19 being considered to have long COVID. However, the prevalence of long COVID in our overall sample was 8.8%, which is smaller than the estimated 10–20% for individuals with COVID-19 infection developing long COVID in the general population (The Lancet, 2023). Therefore, our sample is likely more conservative in identifying those with long COVID. Not all CDC-defined long COVID symptom categories were noted by each individual reporting long COVID, leaving smaller sample sizes in several symptom categories. Finally, while participants were asked about long COVID intensity, frequency and duration of long COVID symptoms were not probed though these factors may also affect perceived long COVID severity.
Conclusion
PA level was significantly positively associated with both perceived physical and mental health among individuals with long COVID. PA remained associated with perceived physical health even after accounting for the intensity of long COVID symptoms. Individuals reporting insufficiently active or active PA levels each reported significantly better perceived physical and mental health than individuals who reporting inactive PA levels, suggesting that even modest amounts of PA may be associated with significantly better perceived health among individuals with long COVID. However, long COVID symptom intensity appears to be a stronger predictor of perceived physical and mental health than PA, emphasizing the importance of targeting disruptive symptoms in addressing long COVID. This study was cross-sectional, and future PA intervention studies and dose–response studies may be helpful in further elucidating the relationship between PA level and perceived health among individuals with long COVID. In addition, future studies could assess the impact of changing PA level on specific physical and mental health outcomes, such as functional ability level, pain, or clinical depression and anxiety.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Iowa State University Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because participants noted consent when clicking to the next screen of a survey. As the survey was anonymous and personally identifying information was not shared, the Iowa State University Institutional Review Board approved this protocol for obtaining participant consent.
Author contributions
ZS: Conceptualization, Formal analysis, Methodology, Writing – original draft. DL: Methodology, Writing – review & editing. AB: Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors note that this project was part of a master’s thesis project, with the entire thesis available at https://www.proquest.com/docview/3065858829?sourcetype=Dissertations%20&%20Theses.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aiyegbusi, O. L., Hughes, S. E., Turner, G., Rivera, S. C., McMullan, C., Chandan, J. S., et al. (2021). Symptoms, complications and management of long COVID: a review. J. R. Soc. Med. 114, 428–442. doi: 10.1177/01410768211032850
Algorani, E. B., and Gupta, V. (2023). Coping mechanisms. Westerly 63:102. doi: 10.2307/j.ctvp7d4ft.13
Anderson, E., and Durstine, J. L. (2019). Physical activity, exercise, and chronic diseases: a brief review. Sports Med. Health Sci. 1, 3–10. doi: 10.1016/J.SMHS.2019.08.006
Appelman, B., Charlton, B. T., Goulding, R. P., Kerkhoff, T. J., Breedveld, E. A., Noort, W., et al. (2024). Muscle abnormalities worsen after post-exertional malaise in long COVID. Nat. Commun. 15, 1–15. doi: 10.1038/s41467-023-44432-3
Araújo, B. T. S., Barros, A. E. V. R., Nunes, D. T. X., Remígio de Aguiar, M. I., Mastroianni, V. W., de Souza, J. A. F., et al. (2023). Effects of continuous aerobic training associated with resistance training on maximal and submaximal exercise tolerance, fatigue, and quality of life of patients post-COVID-19. Physiother. Res. Int. 28:e1972. doi: 10.1002/PRI.1972
Barsky, A. J., and Borus, J. F. (1999). Functional somatic syndromes. Ann. Intern. Med. 130, 910–921. doi: 10.7326/0003-4819-130-11-199906010-00016
Blair, S. N., Kohl, H. W., Gordon, N. F., and Paffenbarger, R. S. (1992). How much physical activity is good for health? Annu. Rev. Public Health 13, 99–126. doi: 10.1146/annurev.pu.13.050192.000531
Broderick, J. E., DeWitt, E. M., Rothrock, N., Crane, P. K., and Forrest, C. B. (2013). Advances in patient-reported outcomes: the NIH PROMIS® measures. EGEMS 1:12. doi: 10.13063/2327-9214.1015
Brodin, P., Casari, G., Townsend, L., O’Farrelly, C., Tancevski, I., Löffler-Ragg, J., et al. (2022). Studying severe long COVID to understand post-infectious disorders beyond COVID-19. Nat. Med. 28, 879–882. doi: 10.1038/s41591-022-01766-7
Burgess, H. J., Burns, J. W., Buvanendran, A., Gupta, R., Chont, M., Kennedy, M., et al. (2019). Associations between sleep disturbance and chronic pain intensity and function. Clin. J. Pain 35, 569–576. doi: 10.1097/ajp.0000000000000711
Center for Disease Control and Prevention (2022). Long COVID or Post-COVID Conditions. Available at: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html.
Centers for Disease Control and Prevention. (2021). Treating the Most disruptive symptoms first and preventing worsening of symptoms. Available at: https://www.cdc.gov/me-cfs/healthcare-providers/clinical-care-patients-mecfs/treating-most-disruptive-symptoms.html.
Centers for Disease Control and Prevention (2023a). Diagnosis and treatment of Myalgic encephalomyelitis/chronic fatigue syndrome | programs | Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Available at: https://www.cdc.gov/me-cfs/programs/evidence-review.html.
Centers for Disease Control and Prevention (2023b). How much physical activity do older adults need? United States: Centers for Disease Control and Prevention.
Chang, C. J., Hung, L. Y., Kogelnik, A. M., Kaufman, D., Aiyar, R. S., Chu, A. M., et al. (2021). A comprehensive examination of severely ill ME/CFS patients. Healthcare 9:1290. doi: 10.3390/HEALTHCARE9101290
Chimenti, R. L., Rakel, B. A., Dailey, D. L., Vance, C. G. T., Zimmerman, M. B., Geasland, K. M., et al. (2021). Test–retest reliability and responsiveness of PROMIS sleep short forms within an RCT in women with fibromyalgia. Front. Pain Res. 2:682072. doi: 10.3389/fpain.2021.682072
Colas, C., Le Berre, Y., Fanget, M., Savall, A., Killian, M., Goujon, I., et al. (2023). Physical activity in long COVID: a comparative study of exercise rehabilitation benefits in patients with long COVID, coronary artery disease and fibromyalgia. Int. J. Environ. Res. Public Health 20:6513. doi: 10.3390/IJERPH20156513
Davis, H. E., McCorkell, L., Vogel, J. M., and Topol, E. J. (2023). Long COVID: major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 21, 133–146. doi: 10.1038/s41579-022-00846-2
Fugazzaro, S., Contri, A., Esseroukh, O., Kaleci, S., Croci, S., Massari, M., et al. (2022). Rehabilitation interventions for post-acute COVID-19 syndrome: a systematic review. Int. J. Environ. Res. Public Health 19:5185. doi: 10.3390/ijerph19095185
Ganesh, R., Ghosh, A. K., Nyman, M. A., Croghan, I. T., Grach, S. L., Anstine, C. V., et al. (2021). PROMIS scales for assessment of persistent post-COVID symptoms: a cross sectional study. J. Prim. Care Community Health 12:21501327211030413. doi: 10.1177/21501327211030413
Henningsen, P. (2018). Management of somatic symptom disorder. Dialogues Clin. Neurosci. 20, 23–31. doi: 10.31887/DCNS.2018.20.1/PHENNINGSEN
Huber, A., Höfer, S., Saner, H., and Oldridge, N. (2020). A little is better than none: the biggest gain of physical activity in patients with ischemic heart disease. Wien. Klin. Wochenschr. 132, 726–735. doi: 10.1007/S00508-020-01767-X
Humphreys, H., Kilby, L., Kudiersky, N., and Copeland, R. (2021). Long COVID and the role of physical activity: a qualitative study. BMJ Open 11:e047632. doi: 10.1136/BMJOPEN-2020-047632
IBM Corp. (2020). SPSS Statistics for Windows. Available at: https://www.ibm.com/support/pages/how-cite-ibm-spss-statistics-or-earlier-versions-spss.
Jacobs, M. M., Evans, E., and Ellis, C. (2023). Racial, ethnic, and sex disparities in the incidence and cognitive symptomology of long COVID-19. J. Natl. Med. Assoc. 115, 233–243. doi: 10.1016/J.JNMA.2023.01.016
Johannesson, E., Ringström, G., Abrahamsson, H., and Sadik, R. (2015). Intervention to increase physical activity in irritable bowel syndrome shows long-term positive effects. World J. Gastroenterol. 21, 600–608. doi: 10.3748/WJG.V21.I2.600
Kaleta, D., Polańska, K., Dziankowska-Zaborszczyk, E., Hanke, W., and Drygas, W. (2009). Factors influencing self-perception of health status. Cent. Eur. J. Public Health 17, 122–127. doi: 10.21101/cejph.b0017
Kim, S. H., Wolde-Tsadik, G., and Reuben, D. B. (2015). Predictors of perceived health in hospitalized older persons: a cross-sectional and longitudinal study. J. Am. Geriatr. Soc. 45, 420–426. doi: 10.1111/J.1532-5415.1997.TB05165.X
Koc, H. C., Xiao, J., Liu, W., Li, Y., and Chen, G. (2022). Long COVID and its management. Int. J. Biol. Sci. 18, 4768–4780. doi: 10.7150/IJBS.75056
Komaroff, A. L., and Lipkin, W. I. (2023). ME/CFS and long COVID share similar symptoms and biological abnormalities: road map to the literature. Front. Med. 10:1187163. doi: 10.3389/fmed.2023.1187163
Lackner, J. M., Gudleski, G. D., Thakur, E. R., Stewart, T. J., Iacobucci, G. J., and Spiegel, B. M. (2014). The impact of physical complaints, social environment, and psychological functioning on IBS patients’ health perceptions: looking beyond GI symptom severity. Am. J. Gastroenterol. 109, 224–233. doi: 10.1038/AJG.2013.410
Larun, L., Brurberg, K. G., Odgaard-Jensen, J., and Price, J. R. (2019). Exercise therapy for chronic fatigue syndrome. Cochrane Database Syst. Rev. 2021:CD003200. doi: 10.1002/14651858.CD003200.pub7
Matta, J., Wiernik, E., Robineau, O., Carrat, F., Touvier, M., Severi, G., et al. (2022). Association of Self-reported COVID-19 infection and SARS-CoV-2 serology test results with persistent physical symptoms among French adults during the COVID-19 pandemic. JAMA Intern. Med. 182, 19–25. doi: 10.1001/JAMAINTERNMED.2021.6454
Merriwether, E. N., Rakel, B. A., Zimmerman, M. B., Dailey, D. L., Vance, C. G. T., Darghosian, L., et al. (2016). Reliability and construct validity of the patient-reported outcomes measurement information system (PROMIS) instruments in women with fibromyalgia. Pain Med. 18, 1485–1495. doi: 10.1093/pm/pnw187
Montoya, J. G., Dowell, T. G., Mooney, A. E., Dimmock, M. E., and Chu, L. (2021). Caring for the patient with severe or very severe Myalgic encephalomyelitis/chronic fatigue syndrome. Healthcare 9:1331. doi: 10.3390/HEALTHCARE9101331
National Institutes of Health (2019). PROMIS: Clinical Outcomes Assessment. Available at: https://commonfund.nih.gov/promis/index.
Northwestern University (2023). PROMIS reference populations. Evanston, IL: Northwestern University.
Pak, S. S., Miller, M. J., and Cheuy, V. A. (2021). Use of the PROMIS-10 global health in patients with chronic low back pain in outpatient physical therapy: a retrospective cohort study. J. Patient Rep. Outcomes 5:81. doi: 10.1186/s41687-021-00360-8
Paul, E., and Fancourt, D. (2022). Health behaviours the month prior to COVID-19 infection and the development of self-reported long COVID and specific long COVID symptoms: a longitudinal analysis of 1581 UK adults. BMC Public Health 22, 1–14. doi: 10.1186/S12889-022-14123-7/TABLES/6
Perlis, R. H., Santillana, M., Ognyanova, K., Safarpour, A., Lunz Trujillo, K., Simonson, M. D., et al. (2022). Prevalence and correlates of long COVID symptoms among US adults. JAMA Netw. Open 5:e2238804. doi: 10.1001/JAMANETWORKOPEN.2022.38804
Petrie, K. J., Broadbent, E., and Kydd, R. (2008). Illness perceptions in mental health: issues and potential applications. J. Ment. Health 17, 559–564. doi: 10.1080/09638230802523047
PROMIS Health Organization. (2021). Sleep disturbance. A brief guide to the PROMIS® sleep disturbance instruments. Available at: https://www.assessmentcenter.net/ac_scoringserviceU.
Salari, N., Khodayari, Y., Hosseinian-Far, A., Zarei, H., Rasoulpoor, S., Akbari, H., et al. (2022). Global prevalence of chronic fatigue syndrome among long COVID-19 patients: a systematic review and meta-analysis. Biopsychosoc. Med. 16, 1–12. doi: 10.1186/s13030-022-00250-5
Savin, E., Rosenn, G., Tsur, A. M., Hen, O., Ehrenberg, S., Gendelman, O., et al. (2023). The possible onset of fibromyalgia following acute COVID-19 infection. PLoS One 18:e0281593. doi: 10.1371/JOURNAL.PONE.0281593
Shelley, J., Hudson, J., Mackintosh, K. A., Saynor, Z. L., Duckers, J., Lewis, K. E., et al. (2021). “I live a kind of shadow life”: individual experiences of COVID-19 recovery and the impact on physical activity levels. Int. J. Environ. Res. Public Health 18:11417. doi: 10.3390/IJERPH182111417
Sirotiak, Z., Thomas, E. B. K., Adamowicz, J. L., and Brellenthin, A. G. (2024a). Fatigue and somatic symptom burden among U.S. adults with current, previous, or no history of long COVID. Fatigue 12, 205–216. doi: 10.1080/21641846.2024.2326406
Sirotiak, Z., Thomas, E. B. K., and Brellenthin, A. G. (2023). Stress, anxiety, and depression severity among individuals with no history, previous history, or current history of long COVID. J. Psychosom. Res. 175:111519. doi: 10.1016/J.jpsychores.2023.111519
Sirotiak, Z., Thomas, E. B. K., Wade, N. G., and Brellenthin, A. G. (2024b). Associations between forgiveness and physical and mental health in the context of long COVID. J. Psychosom. Res. 178:111612. doi: 10.1016/j.jpsychores.2024.111612
Srikanth, S., Boulos, J. R., Dover, T., Boccuto, L., and Dean, D. (2023). Identification and diagnosis of long COVID-19: a scoping review. Prog. Biophys. Mol. Biol. 182, 1–7. doi: 10.1016/J.PBIOMOLBIO.2023.04.008
Stussman, B., Williams, A., Snow, J., Gavin, A., Scott, R., Nath, A., et al. (2020). Characterization of post–exertional malaise in patients with Myalgic encephalomyelitis/chronic fatigue syndrome. Front. Neurol. 11:1025. doi: 10.3389/FNEUR.2020.01025
Subramanian, A., Nirantharakumar, K., Hughes, S., Myles, P., Williams, T., Gokhale, K. M., et al. (2022). Symptoms and risk factors for long COVID in non-hospitalized adults. Nat. Med. 28, 1706–1714. doi: 10.1038/s41591-022-01909-w
Tanne, J. H. (2023). Covid-19: US studies show racial and ethnic disparities in long covid. BMJ 380:p535. doi: 10.1136/BMJ.P535
Turner, J., and Kelly, B. (2000). Emotional dimensions of chronic disease. West. J. Med. 172, 124–128. doi: 10.1136/EWJM.172.2.124
Twisk, F. N. M., and Maes, M. (2009). A review on cognitive behavorial therapy (CBT) and graded exercise therapy (GET) in myalgic encephalomyelitis (ME) / chronic fatigue syndrome (CFS): CBT/GET is not only ineffective and not evidence-based, but also potentially harmful for many patients with ME/CFS. Neuro Endocrinol. Lett. 30, 284–299.
Tyson, P., Wilson, K., Crone, D., Brailsford, R., and Laws, K. (2010). Physical activity and mental health in a student population. J. Ment. Health 19, 492–499. doi: 10.3109/09638230902968308
U.S. Department of Agriculture and U.S. Department of Health and Human Services. (2020). Dietary guidelines for Americans, 2020-2025. Available at: https://www.dietaryguidelines.gov/.
U.S. Department of Health and Human Services (2018). Physical activity guidelines for Americans. Washington, DC: U.S. Department of Health and Human Services.
Ursini, F., Ruscitti, P., and Giacomelli, R. (2023). “Post-COVID-19 syndrome and fibromyalgia” in Autoimmunity, COVID-19, Post-COVID19 Syndrome and COVID-19 Vaccination. ed. S. Ashkenaz (Massachusetts: Academic Press), 777–782.
Vélez-Santamaría, R., Fernández-Solana, J., Méndez-López, F., Domínguez-García, M., González-Bernal, J. J., Magallón-Botaya, R., et al. (2023). Functionality, physical activity, fatigue and quality of life in patients with acute COVID-19 and long COVID infection. Sci. Rep. 13, 1–9. doi: 10.1038/s41598-023-47218-1
Vernon, S. D., Hartle, M., Sullivan, K., Bell, J., Abbaszadeh, S., Unutmaz, D., et al. (2023). Post-exertional malaise among people with long COVID compared to myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Work 74, 1179–1186. doi: 10.3233/WOR-220581
Vink, M., and Vink-Niese, A. (2018). Graded exercise therapy for myalgic encephalomyelitis/chronic fatigue syndrome is not effective and unsafe. Re-analysis of a Cochrane review. Health Psychol. Open 5:2055102918805187. doi: 10.1177/2055102918805187
White, P. D., and Etherington, J. (2021). Adverse outcomes in trials of graded exercise therapy for adult patients with chronic fatigue syndrome. J. Psychosom. Res. 147:110533. doi: 10.1016/J.JPSYCHORES.2021.110533
Wickham, S. R., Amarasekara, N. A., Bartonicek, A., and Conner, T. S. (2020). The big three health behaviors and mental health and well-being among young adults: a cross-sectional investigation of sleep, exercise, and diet. Front. Psychol. 11:579205. doi: 10.3389/fpsyg.2020.579205
Wong, T. L., and Weitzer, D. J. (2021). Long COVID and Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)—a systemic review and comparison of clinical presentation and symptomatology. Medicina 57:418. doi: 10.3390/MEDICINA57050418
Wright, J., Astill, S. L., and Sivan, M. (2022). The relationship between physical activity and long COVID: a cross-sectional study. Int. J. Environ. Res. Public Health 19:5093. doi: 10.3390/ijerph19095093
Wurz, A., Culos-Reed, S. N., Franklin, K., DeMars, J., Wrightson, J. G., and Twomey, R. (2022). “I feel like my body is broken”: exploring the experiences of people living with long COVID. Qual. Life Res. 31, 3339–3354. doi: 10.1007/s11136-022-03176-1
Keywords: long COVID, post-acute sequalae of COVID-19, physical activity, exercise, physical health, mental health
Citation: Sirotiak Z, Lee D-c and Brellenthin AG (2024) Associations between physical activity, long COVID symptom intensity, and perceived health among individuals with long COVID. Front. Psychol. 15:1498900. doi: 10.3389/fpsyg.2024.1498900
Edited by:
Pedro Forte, Higher Institute of Educational Sciences of the Douro, PortugalReviewed by:
Christiano Veneroso, Federal University of Maranhão, BrazilSoukaina Hattabi, University of Jendouba, Tunisia
Copyright © 2024 Sirotiak, Lee and Brellenthin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zoe Sirotiak, em1zaXJvQGlhc3RhdGUuZWR1
 Zoe Sirotiak
Zoe Sirotiak Duck-chul Lee2
Duck-chul Lee2 Angelique G. Brellenthin
Angelique G. Brellenthin