- 1School of Mental Health and Psychological Science, Anhui Medical University, Hefei, China
- 2School of Health Management, Anhui Medical University, Hefei, China
Background: Medical students are confronted with a complex stress environment, encompassing academic challenges, residency training, and future workplace pressures. Therefore, the exploration of effective psychological capital intervention strategies is crucial for enhancing their mental health and promoting career development.
Objective: The aim of this study was to evaluate the efficacy of group cognitive-behavioral therapy (GCBT) and dialectical behavior therapy (DBT) in boosting the psychological capital of medical students and to compare the advantages and disadvantages of these two therapies.
Method: A randomized controlled trial was conducted, recruiting 56 second-year medical students, who were randomly assigned into three groups: GCBT intervention group, DBT intervention group, and control group. The intervention period lasted for 6 weeks, during which the GCBT and DBT groups received respective interventions, while the control group did not receive any intervention.
Results: Regardless of whether GCBT or DBT was used as an intervention, the psychological capital levels of the intervention group students showed significant improvement (mean ± SD, p < 0.05), with effect sizes ranging from 0.324 to 0.667. Further follow-up studies revealed that this improvement remained stable within 1 month post-intervention (mean ± SD, p < 0.05).
Conclusion: Both group cognitive-behavioral therapy (GCBT) and dialectical behavior therapy (DBT) have been proven to be effective psychological intervention methods, capable of significantly enhancing the psychological capital of medical students. However, there are certain differences in their effects, providing diverse intervention options to cater to the varied psychological needs of medical students.
1 Introduction
During their training and academic years, as well as in their future careers, medical students must deal with a variety of stressors. These include, but are not limited to, the demands of rigorous coursework and exams, the need to develop operational skills and adjust to clinical settings, the difficulties of high-intensity work in the workplace, patient responsibility, and professional competition (Puthran et al., 2016; Gan and Yuen, 2019; Chen et al., 2022; Xu et al., 2023; Gao et al., 2022). Among medical students, this set of pressures can quickly lead to anxiety, despair, and other negative emotions, which can then develop into mental health issues. Given this, a thorough investigation and analysis of medical students’ mental health status is essential for identifying the causes and coping strategies of their psychological stress as well as for creating successful intervention plans that support their mental well-being and professional advancement.
Positive psychological traits, including optimism, hope, self-efficacy, and mental resilience, are all included in psychological capital (PsyCap), one measure of mental health. PsyCap has been demonstrated to improve subjective well-being, which in turn lowers stress and negative emotions, and it has a substantial effect on a person’s mental health and academic achievement (Yu et al., 2022). Improving psychological capital, particularly for students, can aid in stress relief, anxiety reduction, and depression reduction, supporting the improvement of mental health (Prasath et al., 2022; Wu et al., 2019). Considering the three unique pressures that medical students encounter—study, internship training, and employment—enhancing psychological capital is thought to be a successful approach to enhancing mental health.
Even while the value of psychological capital in medical education is becoming more well recognized, little research has been done on the subject, especially when it comes to comparative studies assessing how various psychological therapies affect psychological capital development. Currently, two popular psychological therapies for improving mental health in various populations are dialectical behavior therapy (DBT) and group cognitive behavioral therapy (GCBT; Zhou, 2021; Yang, 2016; Zhang, 2022; Öst, 2008; Linehan, 1987; Linehan, 1993; Eisner et al., 2017; Saito et al., 2020). Research on the relative efficacy of these two treatments in boosting the psychological capital of medical students is still lacking, though. Comparative studies in medical student populations are especially crucial because of the variations in the mechanisms underlying these interventions.
This study compared the efficacy of GCBT and DBT as interventions for improving the psychological capital of medical students. In particular, we looked into whether these two programs’ effectiveness in raising medical students’ psychological capital differed significantly. After the 6-week intervention, the DBT group was projected to have considerably higher psychological capital enhancement than the GCBT group, supporting our hypothesis that DBT may be superior to GCBT in this regard. In addition to addressing the research gap in the field, this study intends to establish a scientific foundation for the use of successful psychological interventions in medical education in order to support medical students’ psychological well-being and professional flexibility. It does this by methodically contrasting these two interventions.
2 Research materials and methods
2.1 Participants
This study, which recruited sophomore undergraduate students, was carried out at a medical university between September and December 2023. Professional psychometricians were present to oversee the entire process and guarantee the uniformity, precision, and comprehensiveness of data collection. The questionnaires were distributed collectively by class at the appointed time, and students willingly participated in completing them. Based on the collection of 1,100 questionnaires, the study participants were chosen from a group of students with low psychological capital scores (the low-score group is defined as people scoring below the mean minus the standard deviation Yuan et al., 2022). It was necessary for each participant to have either normal or corrected vision. Those having a history of drug or alcohol addiction, neurological or psychiatric conditions, or those who had already received cognitive behavioral therapy (CBT) were eliminated in order to preserve the sample’s homogeneity.
Based on a statistical efficacy of 80%, a significance level of 0.05, an effect size of 0.5, and a 10–20% attrition rate, as determined by the G*Power 3.1 software, a minimum sample size of 42 people was advised. Ultimately, 65 qualified students—32 men and 33 women—were chosen to take part in the research. To ensure fairness and randomization of assignment, each participant was assigned at random to either the intervention or control groups using a computer-generated table of random numbers. An additional 18 participants were allocated to the control group, and 38 people in the intervention group were further randomized to the GCBT and DBT groups. Only the data from 56 individuals who finished the intervention were kept in the final analysis; the data from 9 participants who dropped out because of course conflicts were excluded.
Before the intervention, each participant signed an informed permission form attesting to their voluntary involvement in the research. The experiment’s precise goal was not disclosed; instead, it was only mentioned as being connected to psychological capital in order to reduce experimental bias. Social workers with specific CBT training carried out the study under the supervision of a qualified supervisor. As an observer, a psychology graduate student was in charge of gathering information and recording the intervention procedure. With the clinical trial registration number ChiCTR2400080269 and ethical review number 84230092, the study was approved by Anhui Medical University’s Ethics Committee.
2.2 Materials
The Positive Psychological Capital Questionnaire (PPQ), created by Zhang and Zhang (2010), was used in this study. Its 26 assessment items gauge the four primary components of psychological capital—self-efficacy, optimism, hope, and resilience—which collectively constitute a person’s positive psychological state, also known as “positive psychological capital” (Luthans et al., 2006). A seven-point Likert scale, with 1 denoting “completely disagree” and 7 denoting “completely agree,” was used to grade the participants. The total score ranged from 26 to 182, with higher scores indicating larger amounts of positive psychological capital. It is important to note that in order to properly evaluate the corresponding attributes, items 8, 10, 12, 14, and 25 of the questionnaire call for a reverse scoring approach. Prior research has demonstrated the PPQ’s strong validity and reliability among college students and other youth populations (Chen et al., 2024; Wei et al., 2024). The KMO value in this study was 0.925, while the Cronbach’s alpha coefficient of the PPQ was 0.918.
2.3 Methods
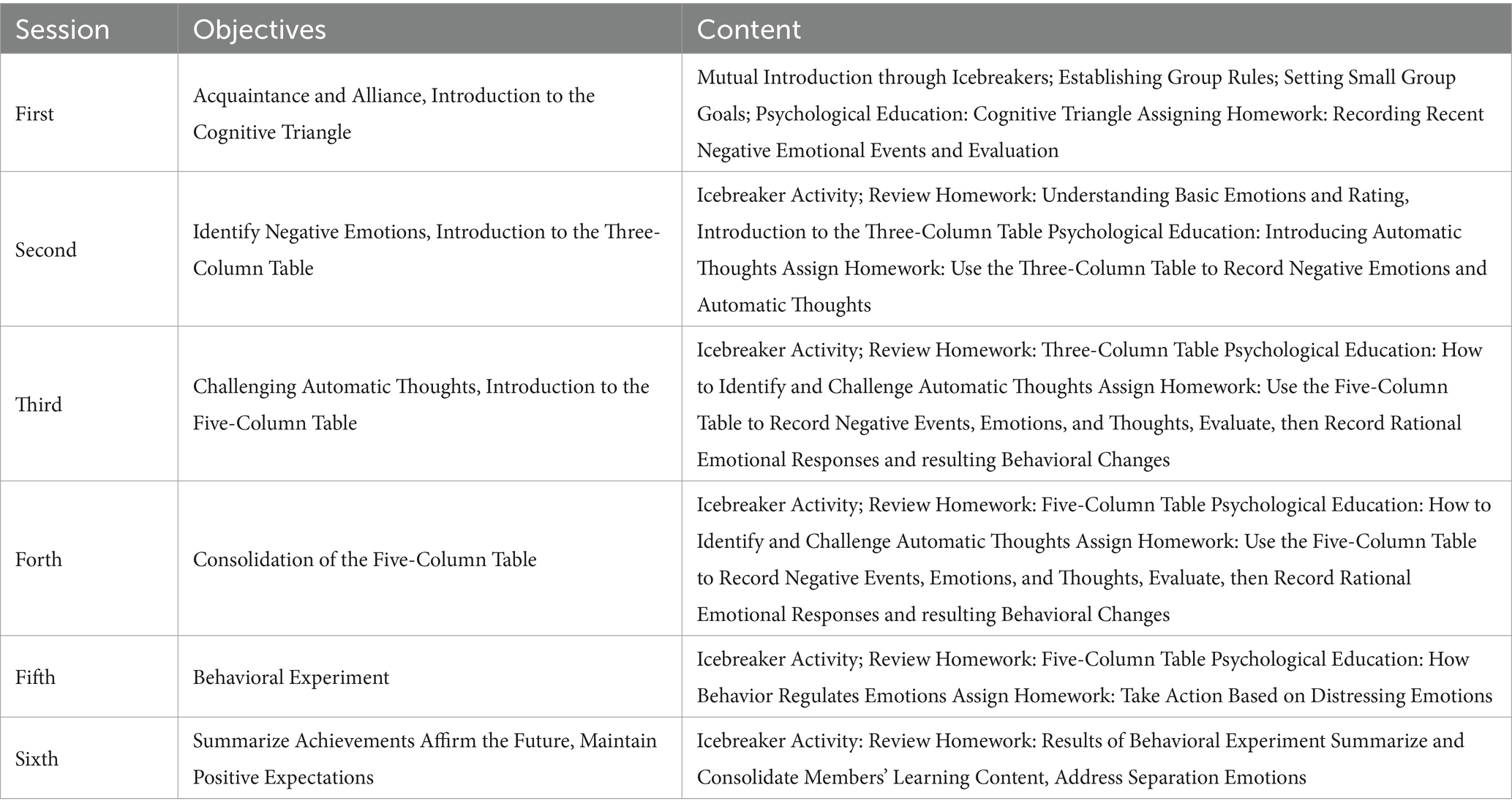
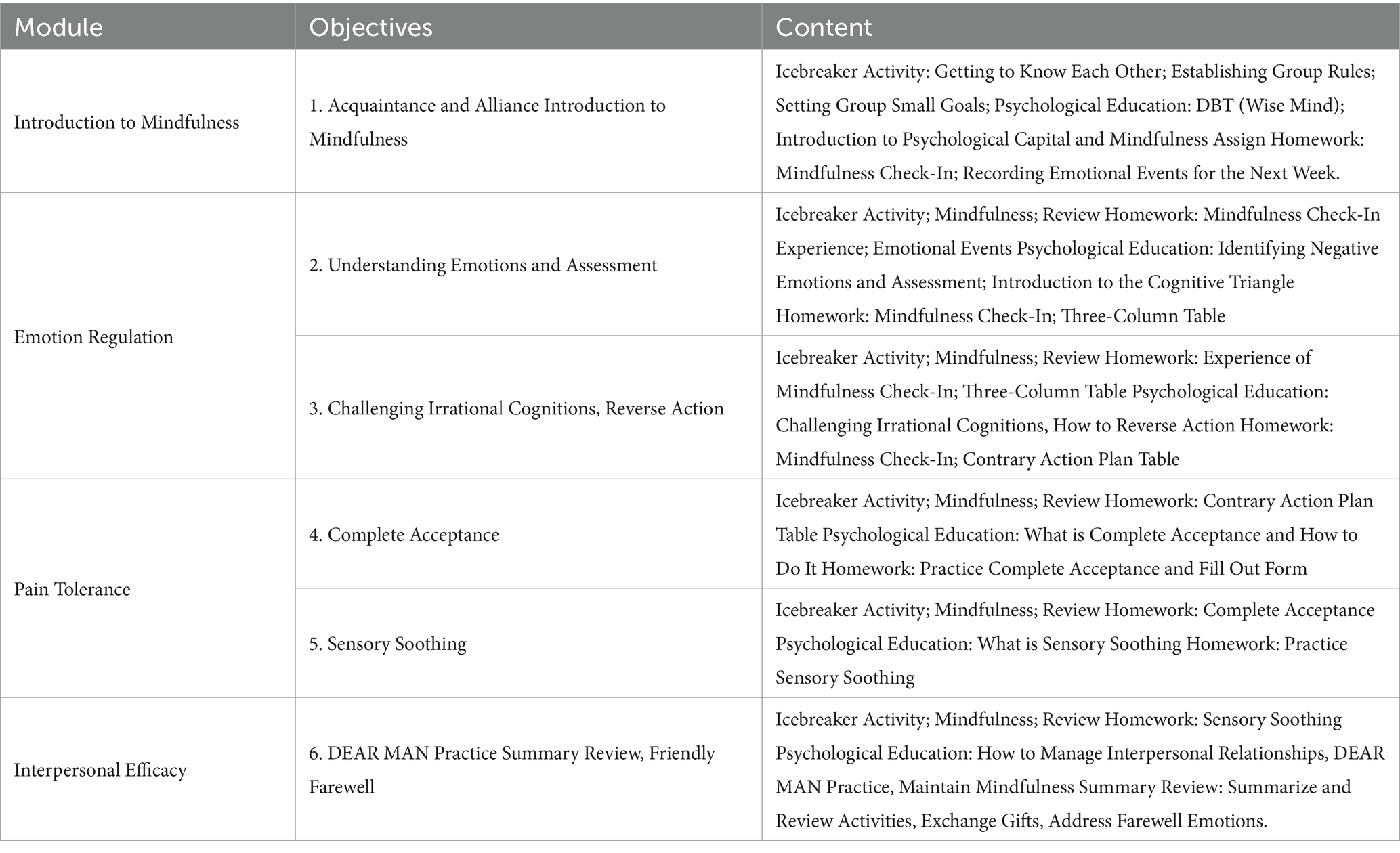
The study’s intervention protocols, which include the particular procedures of group cognitive behavioral therapy (GCBT) and dialectical behavioral therapy (DBT), are listed in Tables 1, 2. During the intervention phase, a weekly medical psychology course covering the fundamentals of mental health, including psychological theories and the diagnosis and treatment of mental diseases, was taken by both the intervention and control groups. The precise intervention procedures utilized in this study to guarantee the independence and scientific validity of the measured intervention effects were not included in this course, which was created to be compatible with standard medical education.
The six-week GCBT intervention takes place once a week on Saturdays, with two-hour sessions. The first week’s objectives were to explain cognitive triangulation theory and build relationships among group members. Following an icebreaker exercise to help members get to know one another, create group rules, and set goals, participants received psychoeducation on the Cognitive Triangle and were given an assignment to document unpleasant emotional experiences. The purpose of the second week was to help members recognize basic emotions, introduce the three-column scale, go over the assignment from the previous week, help members understand basic emotions and automated thinking, and give them a homework assignment that required them to record negative emotions and automated thinking using the three-column scale. Week three’s objectives are to introduce the five-column form and assist group members in challenging automated thinking. They will also discuss last week’s homework and provide homework that requires group members to record events, emotions, and thoughts using the five-column form in order to evaluate logical emotional reactions and behavioral changes. By revisiting assignments to strengthen mastery of the five-column form and promoting regular recording of emotional and cognitive changes, week four further reinforces the use of the form. Week five’s objective was to control emotions through behavioral experiments. After going over the assignments, group members tried to respond practically to upsetting feelings in the behavioral experiments and learned the fundamentals of behavioral regulation of emotions. In order to sustain positive expectations and describe the effectiveness of the intervention, group members summarized the behavioral experiment’s outcomes, reviewed their progress and growth during the intervention, and expressed optimistic expectations for the future in week six. Refer to Table 1.
The four primary modules of the six-week Dialectical Behavior Therapy (DBT) intervention were administered once a week on Sundays for two-hour sessions. The goal of teaching Module 1: Introduction to Mindfulness during the first week is to foster group relationships and introduce mindfulness. Group norms and objectives are established through icebreaker exercises, and psychological instruction on DBT, psychological capital, and mindfulness is given. In order to document emotional experiences for the upcoming week, participants are given homework. Weeks two and three are covered in Module 2: Emotion Regulation. Through a combination of mindfulness exercises, icebreaker games, and instruction on recognizing negative emotions, participants gain an understanding of and ability to evaluate emotions throughout the second week. Emotional events are recorded in a three-column table. The third week is dedicated to confronting illogical thinking. In addition to learning how to challenge illogical thinking, participants are exposed to the idea of “reverse action.” In addition to receiving relevant psychoeducation, participants are given the assignment of developing a reverse action plan. Weeks four and five are dedicated to Module 3: Pain Tolerance. The fourth week is all about total acceptance. Participants gain a deeper grasp of the concept of complete acceptance through psychological education, icebreaker activities, and mindfulness practice. They also perform related assignments. In order to improve pain tolerance, the fifth week’s focus is on sensory soothing. Participants engage in mindfulness exercises, study sensory calming methods, and do associated tasks. The sixth week’s Module 4: Interpersonal Efficacy focuses on enhancing participants’ interpersonal abilities. Members of the group engage in activities that handle farewell emotions, such as summarizing experiences and sharing gifts, as well as practicing the DEAR MAN approach and review tasks. The DBT intervention encourages participants to practice mindfulness exercises daily to enhance their learning. Refer to Table 2.
2.4 Analysis of data
SPSS 26.0 software was used for data processing and analysis in this work. The statistical significance level was set at p < 0.05, and effect sizes were represented using η2 (eta-squared) and Cohen’s d.
3 Results
3.1 Test of homogeneity for baseline attributes
Prior to the intervention, the chi-square test (χ2), the mean ± standard deviation (M ± SD) for ANOVA for normally distributed data, the H-rank-sum test (Kruskal-Wallis test) for skewed data, and the median and its upper and lower quartiles were used to evaluate baseline parameters (e.g., gender, place of birth, being an only child, being a student leader, etc.) of the participants in the three groups. to guarantee that groups’ baseline attributes are uniform. The findings demonstrated that the three groups did not differ significantly on baseline parameters (p > 0.05), suggesting that the distribution of the three groups by gender and place of birth was balanced (refer to Table 3). This provides a solid basis for the investigation of intervention effects that follows.
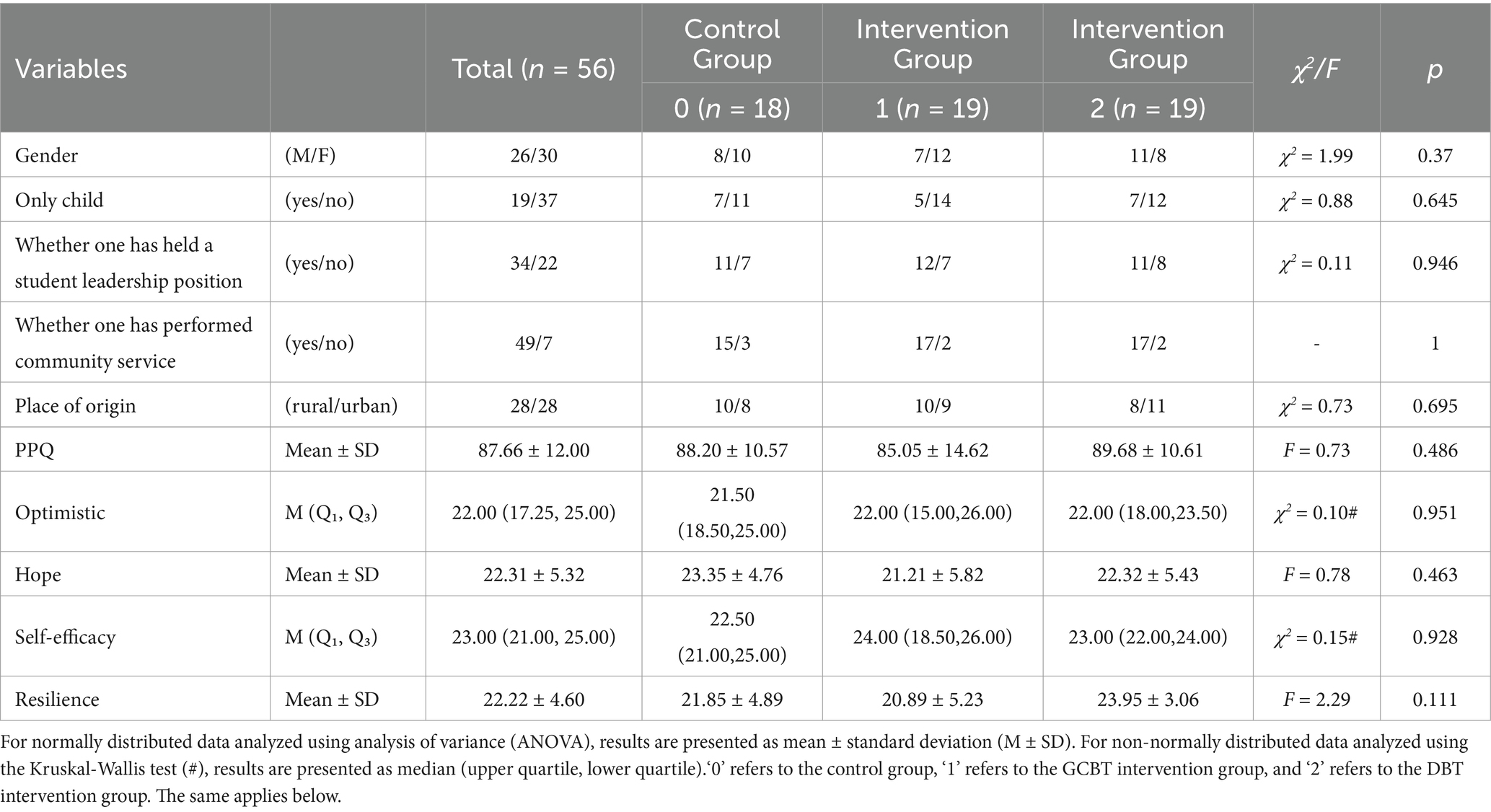
Table 3. Results of demographic variables and scale evaluation before intervention for three groups of participants.
3.2 GCBT and DBT’s intervention effects
Significant differences between the psychological capital measures before and after the GCBT and DBT therapies are displayed in Table 4. In particular, there were parallels between GCBT and DBT therapies in terms of improving medical students’ psychological capital. With effect sizes of 0.567 and 0.667, respectively, at the medium to high effect level, both groups demonstrated a significant improvement in total psychological capital scores (p < 0.001), suggesting that the two interventions had comparable effects on overall psychological capital enhancement. Second, both GCBT and DBT therapies showed significant improvement (p < 0.05) on the optimism and hope dimensions, with similar effects and moderate effect sizes, respectively. Furthermore, the GCBT and DBT intervention groups demonstrated nearly identical improvements (p < 0.001) in the self-efficacy and mental toughness dimensions, with effect sizes of 0.572 and 0.556 and 0.454 and 0.572, respectively, indicating moderate to high effects. In terms of improving several aspects of medical students’ psychological capital, GCBT and DBT demonstrated remarkably similar intervention results overall. This was particularly true for self-efficacy and psychological resilience, which were nearly identical.
Additionally, there were discrepancies between the intervention effects of DBT and GCBT. Self-efficacy had the largest effect size (0.572), indicating a moderate to high intervention effect, whereas the total psychological capital score and its aspects demonstrated significant augmentation (p < 0.05) in the GCBT intervention group. Conversely, the DBT intervention group’s effect sizes on the optimism, hope, and psychological resilience dimensions ranged from 0.405 to 0.667, with the total psychological capital score having the largest effect size at 0.667. The DBT group’s effect sizes on these dimensions were marginally higher than those of the GCBT group, at 0.405, 0.433, and 0.572, respectively. The GCBT group’s effect size (0.572) was greater than the DBT group’s (0.556) on the self-efficacy component, indicating a stronger intervention effect. This suggests that each of the two interventions had its own strengths in different psychological capital dimensions. For example, DBT was marginally more effective than GCBT in enhancing the total psychological capital score, optimism, hope, and psychological resilience, while GCBT had a more significant effect on the self-efficacy dimensions.
3.3 The control group’s effects
Only the total psychological capital score and the optimism dimensions (effect sizes of 0.359 and 0.282, respectively) showed significant improvement (p < 0.05) in the control group; no significant differences were found in the other dimensions of psychological resilience, hope, or self-efficacy (p > 0.05). This implies that there was little change in the control group and that psychological capital was only marginally impacted by regular curriculum-based schooling.
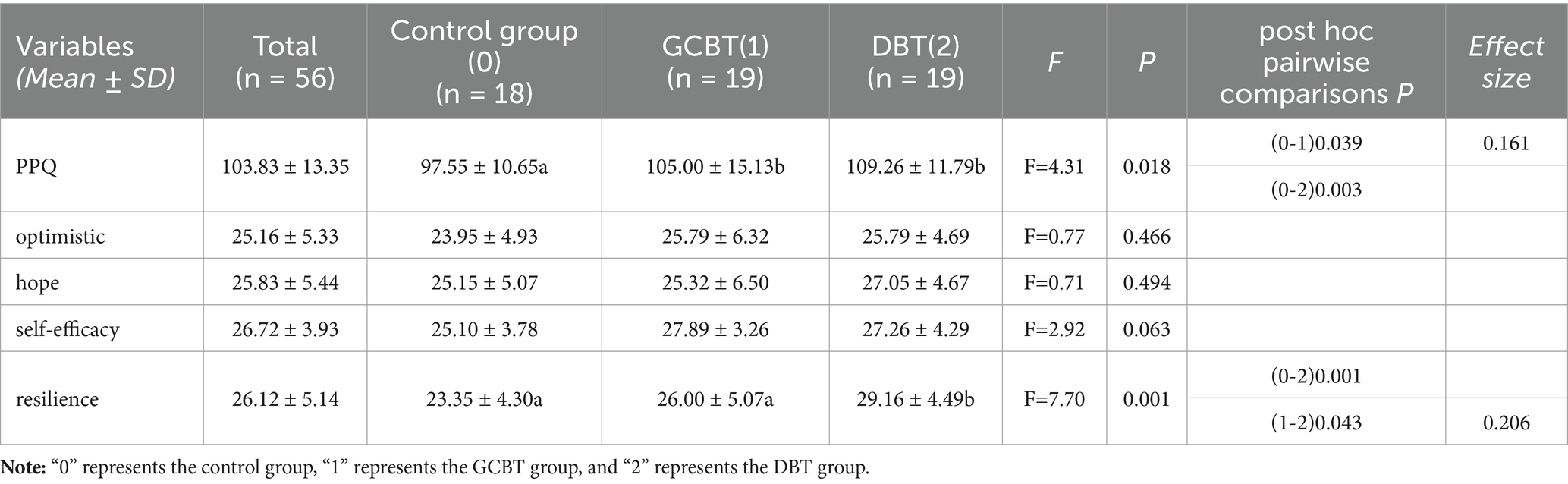
3.4 Results of an ANOVA
Following the intervention, the ANOVA results for the three groups are shown in Table 5. There was a significant difference between the three groups, according to the ANOVA results for the total psychological capital score (F = 4.31, p = 0.018). Subsequent post-hoc analyses revealed significant differences between the control and DBT groups (p = 0.003) and between the control and GCBT groups (p = 0.039, effect size η2 = 0.161). Significant between-group differences were also found by the ANOVA for the mental toughness measure (F = 7.70, p = 0.001). The greater intervention effect of DBT on this dimension was further supported by the substantial differences in mental toughness between the GCBT and DBT groups (p = 0.043, effect size η2 = 0.206) and between the control and DBT groups (p = 0.001).
4 Discussion
The impact of GCBT and DBT in raising medical students’ psychological capital was examined in this study. The study’s findings indicate that while both can successfully improve medical students’ psychological capital, there are some minor variations in particular areas, which may be due to the two interventions’ different theoretical underpinnings and technical foci: DBT focuses more on emotional regulation, pain tolerance, and positive thinking exercises to help people find a balance between stress and emotional swings, while GCBT primarily modifies negative thinking and behavioral responses through cognitive restructuring and behavioral activation (Mehta, 2018; Sehati et al., 2019). In addition to offering theoretical backing for medical students’ psychological capital intervention techniques, this research offers recommendations on how to successfully raise medical students’ psychological capital in the real world (Heikkila et al., 2024; Zhou, 2021).
4.1 Similarities between the outcomes of GCBT and DBT interventions
When it came to improving medical students’ psychological capital and its aspects, GCBT and DBT had striking similarities. This could be because both interventions are grounded in the cognitive-behavioral theoretical framework, which improves medical students’ psychological capital through behavioral and cognitive changes, leading to comparable benefits in raising self-efficacy, optimism, and hope (Yu et al., 2023). This is in line with earlier studies that have demonstrated the substantial benefits of CBT-based intervention strategies in fostering psychological capital and wellbeing (Heikkila et al., 2024). Furthermore, both DBT and GCBT employ a group intervention structure to give medical students social networks and emotional support, which in turn improves a sense of community and social support and fortifies psychological resilience and self-confidence (Bryde Christensen et al., 2021). In addition to fostering connections of mutual support, this group support environment was crucial in helping medical students build their psychological capital. As a result, when it came to improving medical students’ psychological capital and its aspects, GCBT and DBT showed very comparable results.
4.2 Differences between GCBT and DBT therapies’ efficacy
Despite the fact that GCBT and DBT had comparable effects on a number of dimensions, this study found that DBT was marginally more effective than GCBT in terms of optimism, psychological resilience, and hope. This could be because DBT is better at managing emotions and handling high-pressure situations; it improves psychological resilience and optimism by strengthening emotion regulation skills, which help medical students stay optimistic when faced with academic stress (Rabiee et al., 2020; Gillespie et al., 2022). Additionally, medical students receive thorough training in psychological skills through the multi-module integration of DBT (such as emotion regulation, positive thinking, distress tolerance, and interpersonal efficacy), which shows a notable advantage in mental toughness in particular (Ji, 2018). Furthermore, DBT is better than GCBT’s cognitive restructuring technique in the hope component because its dialectical thinking training and reality acceptance techniques support medical students in retaining optimism and constructive coping mechanisms in trying circumstances (Alfonsson et al., 2022). While DBT focuses more on emotion regulation (Li et al., 2022), it is less effective than GCBT at directly boosting self-efficacy. Instead, GCBT’s superiority on self-efficacy may be due to its emphasis on goal setting, cognitive restructuring, and problem solving (Menefee et al., 2022), which helps medical students improve their sense of accomplishment and self-confidence by setting specific goals and adjusting negative self-evaluations. Overall, GCBT was better at increasing self-efficacy, whereas DBT was marginally better at increasing optimism, mental toughness, and hope. Each was successful in a distinct dimension.
4.3 Study limitations and suggestions for more research
There are certain limitations, even though the current study offered insightful information about how GCBT and DBT might be used to improve medical students’ psychological capital. First, the evaluation of the intervention’s long-term benefits was limited by the study’s brief one-month follow-up period. To get more thorough information on the persistence of the intervention, future research could increase the follow-up duration to 3 months or more. Second, the results may not be as broadly applicable as they may be due to the limited sample size. To improve representativeness, future research should extend the sample size to include medical students from a range of socioeconomic backgrounds, genders, and grades. Furthermore, this study did not perform subgroup analyses of demographic characteristics (e.g., gender, years of study) on the impact of the intervention (Simmonds-Buckley et al., 2021). Since the sample size allows for a more thorough examination of the variations in how medical students with various characteristics respond to GCBT and DBT, future research may employ subgroup analysis. Given that all of the data in this study were self-reported by medical students, response bias may have occurred. Subjects may have selected more favorable answers because of social pressure or expectation of the intervention, which would have produced results that were not entirely accurate. To further evaluate the effects of the intervention and lessen response bias from self-report, future research might think about adding objective assessment instruments or observational data (such as eye movements). In order to guarantee the applicability and generalizability of the intervention program in a wider context, future research should take into account the possible influence of cultural variations on intervention effects, as this study was carried out in a particular cultural setting.
4.4 Conclusion and practical application
The findings of this study show that both GCBT and DBT may significantly improve a number of dimensions and effectively raise medical students’ psychological capital. In light of this, it is advised that DBT interventions be prioritized in medical students’ mental health training. This can be done by establishing a special DBT group within the curriculum or by scheduling a DBT module in adaptive training at the start of each semester. The multi-module design of DBT (such as emotion regulation and pain tolerance) is especially well-suited for the psychological needs of medical students in high-pressure settings. For instance, it can be used to teach emotion management skills in the classroom and provide group support during the clerkship or exam season.
Furthermore, as a cognitive intervention technique, GCBT can be utilized in conjunction with DBT and has a remarkable impact on raising medical students’ self-efficacy. By establishing clear objectives and modifying self-evaluation, GCBT modules can be incorporated into career development courses or skills workshops to assist medical students in improving their sense of accomplishment and self-efficacy. In the future, group DBT and GCBT can be combined in medical students’ mental health education to offer all-encompassing psychological support in both group and classroom settings. This will progressively build medical students’ psychological capital, establishing a strong basis for their mental health and professional growth.
Data availability statement
The datasets presented in this article are not readily available because access to the dataset is restricted to authorized research personnel only. The dataset is intended solely for non-commercial academic research purposes, and any sharing or redistribution of the data is strictly prohibited without prior authorization. Requests to access the datasets should be directed to Cexin Dong Njk0NzA5MTExQHFxLmNvbQ==.
Ethics statement
The studies involving humans were approved by the Ethics Committee at Anhui Medical University (protocol number: 84230092). Participants completed an informed consent form, and they were told that if they felt any discomfort while answering questions, they could opt out of the survey at any time without being punished. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
CD: Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Investigation, Methodology. JZ: Writing – review & editing, Data curation, Formal analysis. YW: Data curation, Formal Analysis, Writing – review & editing. DW: Formal analysis, Methodology, Writing – review & editing. ZC: Supervision, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alfonsson, S., Mardula, K., Toll, C., Isaksson, M., and Wolf-Arehult, M. (2022). The self-efficacy in distress tolerance scale (SE-DT): a psychometric evaluation. Borderline Pers. Disord. Emot. Dysregul. 9:23. doi: 10.1186/s40479-022-00195-9
Bryde Christensen, A., Wahrén, S., Reinholt, N., Poulsen, S., Hvenegaard, M., Simonsen, E., et al. (2021). “Despite the differences, we were all the same”. Group cohesion in diagnosis-specific and transdiagnostic CBT groups for anxiety and depression: a qualitative study. Int. J. Environ. Res. Public Health 18:5324. doi: 10.3390/ijerph18105324
Chen, S. H., Lou, X. R., Yin, J., Xie, J. J., Zhang, X. Y., et al. (2022). The impact of medical students’ emotional regulation self-efficacy on academic burnout. Occup. Health 38, 2255–2259. doi: 10.13329/j.cnki.zyyjk.2022.0458
Chen, Y., Wahab, R. B., and Jaladin, R. B. A. M. (2024). Self-deception, psychological capital and depression in Normal university students: a cross-lagged analysis.
Eisner, L., Eddie, D., Harley, R., Jacobo, M., Nierenberg, A. A., and Deckersbach, T. (2017). Dialectical behavior therapy group skills training for bipolar disorder. Behav. Ther. 48, 557–566. doi: 10.1016/j.beth.2016.12.006
Gan, G. G., and Yuen, L. H. (2019). Anxiety, depression and quality of life of medical students in Malaysia. Med J Malaysia 74, 57–61
Gao, L., Zhou, Y. F., and Zhang, Q. M. (2022). The current situation and educational countermeasures of mental health education for medical students. Chin. Sch. Doctor 36, 385–387.
Gillespie, C., Murphy, M., Kells, M., and Flynn, D. (2022). Individuals who report having benefitted from dialectical behaviour therapy (DBT): a qualitative exploration of processes and experiences at long-term follow-up. Borderline Pers. Disord. Emot. Dysregul. 9:8. doi: 10.1186/s40479-022-00179-9
Heikkila, R., Finch, J., Waters, A. M., and Farrell, L. J. (2024). Preliminary effectiveness of a brief school-based HERO intervention: improving the wellbeing of final year adolescent female students. Child Psychiatry Hum. Dev. 55, 575–587. doi: 10.1007/s10578-023-01629-3
Ji, Y. (2018). Research on the intervention of college students’ cognitive emotion regulation on psychological resilience. Master’s thesis, Northeast Normal University.
Li, Y., Storch, E. A., Ferguson, S., Li, L., Buys, N., and Sun, J. (2022). The efficacy of cognitive behavioral therapy-based intervention on patients with diabetes: a meta-analysis. Diabetes Res. Clin. Pract. 189:109965. doi: 10.1016/j.diabres.2022.109965
Linehan, M. M. (1987). Dialectical behavior therapy for borderline personality disorder: theory and method. Bull. Menn. Clin. 51, 261–276
Linehan, M. M. (1993). Cognitive-behavioral treatment of borderline personality disorder. Curr. Psychiatry Rep. 6, 225–231.
Luthans, F., Youssef, C. M., and Avolio, B. J. (2006). Psychological capital: Developing the human competitive edge. New York, United States: Oxford University Press.
Mehta, M. (2018). New advances in cognitive behavioral therapy. J. Indian Assoc. Child Adolesc. Ment. Health 14, 12–30. doi: 10.1177/0973134220180202
Menefee, D. S., Ledoux, T., and Johnston, C. A. (2022). The importance of emotional regulation in mental health. Am. J. Lifestyle Med. 16, 28–31. doi: 10.1177/15598276211049771
Öst, L. G. (2008). Efficacy of the third wave of behavioral therapies: a systematic review and meta-analysis. Behav. Res. Ther. 46, 296–321. doi: 10.1016/j.brat.2007.12.005
Prasath, P. R., Xiong, Y., Zhang, Q., and Jeon, L. (2022). Psychological capital, well-being, and distress of international students. Int. J. Adv. Couns. 44, 529–549. doi: 10.1007/s10447-022-09473-1
Puthran, R., Zhang, M. W., Tam, W. W., and Ho, R. C. (2016). Prevalence of depression amongst medical students: a meta-analysis. Med. Educ. 50, 456–468. doi: 10.1111/medu.12962
Rabiee, N., Nazari, A. M., Keramat, A., Khosravi, A., and Bolbol-Haghighi, N. (2020). Effect of dialectical behavioral therapy on the postpartum depression, perceived stress and mental coping strategies in traumatic childbirth: a randomized controlled trial: test. Int. J. Health Stud. 6, 41–48. doi: 10.22100/ijhs.v6i2.760
Saito, E., Tebbett-Mock, A. A., and McGee, M. (2020). Dialectical behavior therapy decreases depressive symptoms among adolescents in an acute-care inpatient unit. J. Child Adolesc. Psychopharmacol. 30, 244–249. doi: 10.1089/cap.2019.0149
Sehati, M., Nasab, A. A., and Yousefian, Z. (2019). The efficiency of emotion regulation and distress tolerance based on dialectical behavior therapy on anxiety sensitivity and emotion regulation difficulties in women with irritable bowel. J. Soc. Behav. Commun. Health. 3, 298–308. doi: 10.18502/sbrh.v3i1.1034
Simmonds-Buckley, M., Catarino, A., and Delgadillo, J. (2021). Depression subtypes and their response to cognitive behavioral therapy: a latent transition analysis. Depress. Anxiety 38, 907–916. doi: 10.1002/da.23161
Wei, X., Lai, Z., Tan, Z., Ou, Z., Feng, X., Xu, G., et al. (2024). The effect of physical activity on depression in university students: the mediating role of self-esteem and positive psychological capital. Front. Psychol. 15:1485641. doi: 10.3389/fpsyg.2024.1485641
Wu, S., Xu, Z., Zhang, Y., and Liu, X. (2019). Relationship among psychological capital, coping style and anxiety of Chinese college students. Riv. Psichiatr. 54, 264–268. doi: 10.1708/3281.32545
Xu, Q. H., Yu, Q. M., and Ji, S. X. (2023). The relationship between medical students’ emotional management ability, self-esteem, and prosocial behavior. Chin. J. Soc. Med. 40, 167–172.
Yang, ZJ. (2016). The current status of psychological capital and group counseling intervention among vocational school students [Master’s thesis]. Qinghai Normal University.
Yu, Q., Wang, Y. N., and Liu, L. (2022). The status and influencing factors of positive psychological capital among excellent poor college students. Chin. Sch. Health 43, 562–569. doi: 10.16835/j.cnki.1000-9817.2022.04.019
Yu, W., Yao, W., Chen, M., Zhu, H., and Yan, J. (2023). School climate and academic burnout in medical students: a moderated mediation model of collective self-esteem and psychological capital. BMC Psychol. 11:77. doi: 10.1186/s40359-023-01121-6
Yuan, L., Zheng, J. F., and Hou, Y. Q. (2022). The impact of pre-service teachers’ sense of professional mission on learning engagement: the mediating role of professional identity and the moderating role of psychological capital. J. Southwest Univ. 6, 218–227. doi: 10.13718/j.cnki.xdsk.2022.06.019
Zhang, J. (2022). The relationship and intervention of basic psychological needs satisfaction, psychological capital, and academic achievement among junior high school students [Master’s thesis]. Zhejiang Sci-Tech University.
Zhang, K., and Zhang, S. (2010). Positive psychological capital: measurement and its relationship with mental health. Psychol. Behav. Res. 8, 58–64.
Keywords: psychological capital, medical students, group psychological intervention, group cognitive behavioral therapy, dialectical behavior therapy
Citation: Dong C, Zhao J, Wei Y, Wu D and Cai Z (2024) Comparative analysis of cognitive behavioral therapy and dialectical behavior therapy in enhancing psychological capital among medical students: a randomized controlled trial. Front. Psychol. 15:1479310. doi: 10.3389/fpsyg.2024.1479310
Edited by:
Alejandro De La Torre-Luque, Complutense University of Madrid, SpainReviewed by:
Siaw Leng Chan, Universiti Putra Malaysia Bintulu Sarawak Campus, MalaysiaMaría Cantero García, Universidad a Distancia de Madrid, Spain
Copyright © 2024 Dong, Zhao, Wei, Wu and Cai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhu Cai, ODI4MTg0MkBxcS5jb20=
†These authors have contributed equally to this work and share first authorship
 Cexin Dong
Cexin Dong Jinfa Zhao
Jinfa Zhao Yating Wei
Yating Wei Deyuan Wu
Deyuan Wu Zhu Cai1*
Zhu Cai1*